Abstract
Objective:
We reviewed medical records and conducted a nationwide survey to characterize the clinical features and determine the prevalence of biliary tract disease in girls and women with Rett syndrome (RTT).
Methods:
Sixty-two individuals with RTT and biliary tract disease were identified from the membership of Rett Syndrome Organization (RS.O) and patient files of the principal investigator. Medical records of 46 individuals were reviewed for presenting features, diagnostic tests, and treatment outcomes of biliary tract disease. We designed a questionnaire that probed the frequency of risk factors and treatment outcomes of biliary tract disease in RTT. The questionnaire was completed by 271 parents whose daughters met the clinical criteria for RTT and/or had MECP2 mutations and participated in the Natural History of Rett Syndrome Study.
Results:
Presenting symptoms identified by record review included abdominal pain (94%), irritability (88%), weight loss (64%), and vomiting (52%). Biliary dyskinesia, cholecystitis, and cholelithiasis, were identified in 90%, 77%, and 70%, respectively, by cholescintigraphy, surgical pathology, and abdominal ultrasound. The prevalence of biliary tract disease was 4.4% (n=12) in the RTT cohort. Risk factors included older age (p<0.001) and a positive family history (p<0.01). Diagnoses included cholecystitis (n=5), biliary dyskinesia (n=6), and cholelithiasis (n=7). Ten individuals underwent surgery; seven had resolution of symptoms after surgical intervention.
Conclusion:
Biliary tract disease is not unique to RTT, but may be under-recognized because of the cognitive impairment of affected individuals. Early diagnostic evaluation and intervention may improve the health and quality of life of individuals affected with RTT and biliary tract disease.
Keywords: Cholecystitis, cholelithiasis, biliary dyskinesia, MECP2, gallbladder
INTRODUCTION
Rett syndrome (RTT), an X-linked neurodevelopmental disorder localized to the MECP2 gene, is a leading cause of intellectual disability in children (1). RTT affects approximately 1 in 10,000 females worldwide; it may be associated with severe neonatal encephalopathy in males (2). The disorder is recognized clinically between 6 and 18 months of age in girls who plateau in their developmental milestones and lose purposeful hand skills coincident with the onset of hand stereotypies. Growth of the head slows and other neurological signs such as loss of language, motor apraxia, and seizures evolve. The diagnosis of classical RTT is based on strict adherence to the diagnostic criteria put forth by the Rett Syndrome Diagnostic Workgroup (3).
Although neurological symptoms predominate, girls with RTT exhibit a myriad of gastrointestinal problems. Chewing and swallowing dysfunction, gastroesophageal reflux, gastroparesis, gas bloating, and constipation frequently complicate the clinical course of this disorder and predispose girls with RTT to nutritional deficits, protein-energy malnutrition, and growth failure (4, 5). Although these features of RTT are recognized, the pattern of biliary tract disease has not been characterized fully in this disorder.
A preliminary report from Rett Syndrome Organization (RS.O) suggested that girls and women with RTT were susceptible to poorly characterized “abdominal crises” that had a potentially life-threatening impact on the health and well-being of affected individuals. Anecdotal evidence from RS.O indicated that biliary tract disorders may have been responsible, in part, for these events. As a consequence, RS.O leadership approached members of the Rett Natural History Study (RNHS) consortium to examine the problem of biliary tract disease in RTT. RS.O collected reports from families whose daughters had evidence of gallbladder disease. The mission of RS.O was to seek professional review of their daughters’ medical records for information about biliary tract disease and promote awareness about this potential complication of RTT. We designed this study, therefore, in conjunction with RS.O to characterize the prevalence, clinical features, and clinical outcome of biliary tract disease in girls and women with RTT.
SUBJECTS AND METHODS
Study Design
The study was designed in two parts: 1) a retrospective review of medical records to characterize the clinical features of biliary tract disease in a group of girls and women with RTT, and 2) a prospective survey questionnaire (See Appendix, Supplemental Digital Content 1, which represents the survey questionnaire administered to the parents of girls and women with RTT who participated in the Natural History of Rett Syndrome Study) to determine the prevalence of biliary tract disease in a large cohort of girls and women with RTT.
The study was approved by the Baylor College of Medicine Institutional Review Board. Written informed consent was obtained from the parents and/or legal guardians of girls and women with RTT for the review of their medical records. Written parental consent was waived for completion of the survey questionnaire. The assent of girls and women with RTT was waived because of their cognitive impairment.
Methods
Medical Records
The membership of RS.O, the family based organization for RTT awareness and advocacy, were solicited directly by the administrative staff of RS.O for participation in the review of the medical records of girls and women with RTT who had biliary tract disease. The names and contact information for each individual were submitted with parental permission by the RS.O staff to the principal investigator. Additional case reports also were solicited from families within the principal investigator’s clinical practice. Each individual met the consensus criteria for classic or variant RTT. All age, ethnic, and racial groups were eligible for study participation. Two of the investigators (KJM, JL) obtained written parental permission for the review of their daughter’s medical records. Documents were requested from physician offices and hospitals. Medical records were reviewed for demographic information, presenting symptoms, physical findings, laboratory and diagnostic tests, surgical procedures, pathological findings, and clinical outcomes. Data of interest were considered to be present or absent only if clearly specified in the medical records. Available data were recorded on pre-designed computerized spreadsheets for analysis. Data of interest were collected over a period of 13 years from 2003 to 2016.
Survey Questionnaire
Survey questionnaires were developed by two of the investigators (KJM, JL) to characterize the frequency, risk factors, and treatment outcomes of biliary tract disease in RTT (Appendix). The survey was a 40-point questionnaire that queried demographics, genetic mutations, family history, symptoms, laboratory and diagnostic tests, surgical procedures, and clinical outcomes. Reponses to questions were coded in a “yes”, no”, or “don’t know” format. Responses were grouped based on answers to two primary questions: 1) has your child been evaluated for biliary tract disease, and 2) does your child have biliary tract disease. Demographic information for the entire cohort was summarized, followed by further analysis of those individuals whose responses were “yes” to one or both primary questions.
Participants for the survey were recruited through the multicenter Rett Natural History Study (RNHS) at one of six US sites (Houston, TX; Birmingham, AL; Chicago, IL; New Brunswick, NJ; Oakland, CA; Miami or Tampa, FL) by members of the RNHS consortium. The RNHS consortium, which was comprised of physicians, nurses, dietitians, and genetic counsellors from the participating sites, is part of the Rare Diseases Clinical Research Network, an initiative of the Office of Rare Diseases Research, National Center for Advancing Translational Sciences. Approval to conduct the RNHS was obtained from the Institutional Review Boards at each investigative site and written informed consent was obtained from all families who participated in the RNHS.
Individuals who met the clinical diagnostic criteria for RTT and/or had a mutation in the MECP2 gene were eligible for enrollment (3). The diagnosis of the RTT phenotype was performed by a study neurologist or geneticist with clinical experience in RTT. Consensus criteria were used to categorize participants as having classic RTT, atypical RTT, or a mutation in MECP2 but not fulfilling clinical criteria for RTT (3). All participants had MECP2 testing; participants with clinical RTT were included even if they lacked a mutation. All mutations were classified on the basis of the severity of the mutation: mild (R133C, R294X, R306C, 3’ truncations), moderately severe (T158M, all others except mild and severe), and severe (R106W, R255X, R270X, large deletions) (6). All age, racial, and ethnic groups were eligible for study. Further details have been published previously (7). Data were collected over a period of 18 months from November, 2012, to May, 2014, to capture a representative cohort from all study sites.
Statistical analysis
Descriptive statistics were used to summarize the demographic, clinical, diagnostic, and treatment variables of the RTT participants contained within the medical records and survey questionnaires (MiniTab, v.18, MiniTab, Inc., State College, PA). Nonparametric (Kruskal-Wallis) and Fisher’s Exact tests were used to detect differences in continuous and discrete outcome variables, respectively, between individuals with and without biliary tract disease from the questionnaire.
RESULTS
Medical record review
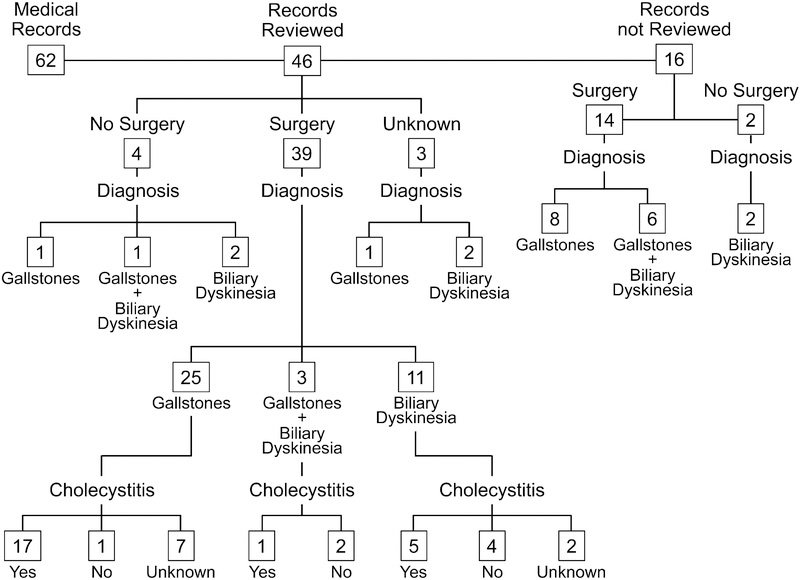
Sixty-two individuals with RTT and biliary tract disease were identified based on parental report. The medical records of 46 individuals from this group were reviewed (Figure 1). The medical records of 16 individuals escaped review because of unknown contact information or failure to obtain parental permission. Of those 16 individuals whose medical records were unavailable, 14 had surgery, two did not. Gallstones were reported to be present in eight individuals who underwent surgery. The outcome of six individuals who had surgery was unknown. Two individuals who did not have surgery had gallstones, based on parental report.
Figure 1.
Flowchart of medical record review: 46 medical records were reviewed to determine the clinical outcome of biliary tract disease in girls and women with Rett syndrome
Of the 46 records providing documentation (See Table, Supplemental Digital Content 2, which describes the clinical features of biliary tract disease in 46 girls and women with RTT identified by medical record review), the majority of individuals with RTT and biliary tract disease were Caucasian. The median age at which individuals presented with symptoms was 21 y. Presenting symptoms included abdominal pain, irritability, weight loss, and vomiting. The median duration of symptoms was 2.5 months. The family history was positive for biliary tract disorders in nearly two-thirds of the group. Presenting temperature, pulse and blood pressure were normal (data not shown). The median height and weight z-scores were more than two standard deviations below the mean, but the body mass index z-score was nearly zero. The abdominal exam was noteworthy for the presence of right upper quadrant abdominal pain and abdominal distention. The CBC and liver panel were normal; however, the upper third quartile values for two or more lab tests including AST, ALT, alkaline phosphatase, or total bilirubin exceeded reference values in 5 individuals. Gallstones were documented in 28 (70%) of the available abdominal ultrasound reports; 4 (15%) identified a dilated common bile duct. Gallstones were documented in 4 (67%) of the available CT scan reports and a delay in gallbladder emptying was documented in 19 (90%) of the available cholecystokinin-stimulated hepatobiliary iminodiacetic acid (CCK-HIDA) scan reports. The median age at diagnosis was 21 y.
Cholecystectomy was performed in 39 (85%) individuals; four did not have surgery and three had an unknown course. Laparoscopic surgery was performed in 32 (81%) individuals. The median age at which surgery was performed was 21 y. Of those individuals who had surgery, 25 (64%) had gallstones, 11 (28%) had biliary dyskinesia, and three had both disorders. Of those individuals who did not undergo surgery, one had gallstones, two had biliary dyskinesia, and one had both diagnoses. The clinical outcome of three of the individuals who did not have surgery was unknown. The one patient with gallstones alone who did not have surgery remained asymptomatic for two years. Cholecystitis was documented in 24 (77%) available pathology reports; the severity of disease was listed as mild in 6, moderate in 3, and erosive in one case. Cholelithiasis was documented in 20 (65%) available pathology reports.
When both groups were summarized as a whole, cholelithiasis was identified by parental report, abdominal ultrasound, CT scan, and/or pathology report in 41 (66%) individuals, while biliary dyskinesia was identified by parental report and /or CCK-HIDA scan in 19 (31%). Surgery was performed in 53 (85%) individuals. The median age (1st, 3rd quartile) at the time of surgery was 21 y (15, 26). Death due to a respiratory complication of cholecystectomy was reported by the parent of one individual.
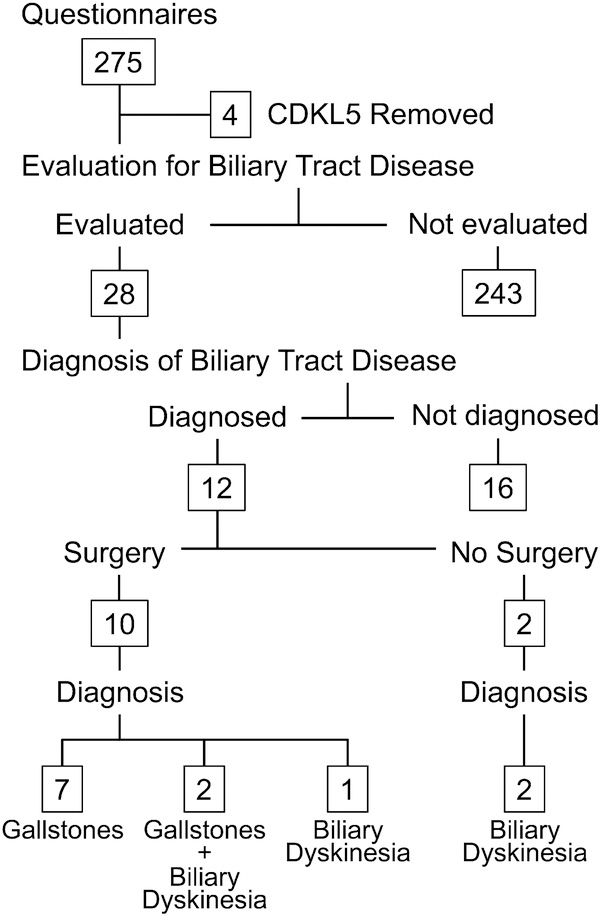
Survey Questionnaires
A total of 275 parents whose children had RTT and/or MECP2 mutations completed the survey (Figure 2). Four questionnaires were excluded because the participants had CDKL5, a rare x-linked genetic disorder that results in severe neurodevelopmental impairment and early onset seizures which were previously thought to be associated with the Hanefeld variant of RTT. The size of the remaining biliary cohort represented approximately 20% of the total NHRS cohort (8). The median (1st, 3rd quartile) age of the individuals in the RTT cohort (n=271) was 11 (7, 19) y. Females comprised 98% of the cohort. Ninety-seven percent of the cohort met the clinical criteria for RTT and 95% of the group was positive for a MECP2 mutation. The severity of the mutations was classified as mild in 24%, moderately severe in 42%, and severe in 29% of the participants. The family history of biliary tract disease was positive in 26% of the RTT cohort.
Figure 2.
Flowchart of survey questionnaire review: 271 questionnaires were reviewed to determine the prevalence of biliary tract disease in girls and women with Rett syndrome
A subset of 28 individuals from the NHRS cohort was evaluated for the presence of biliary tract disorders based on parental concerns for gastrointestinal problems (See Table, Supplemental Digital Content 3, which describes the clinical features of biliary tract disease in individuals with RTT and/or MECP2 mutations from the Natural History of Rett Syndrome Study) (N=28)). Twelve individuals had biliary tract disease identified by one or multiple diagnostic tests; 16 individuals did not. The mean age (p<0.05) and the proportion of participants who had a positive family history (p<0.06) differed between affected and unaffected individuals. The proportion of individuals who were female, those who met the clinical diagnostic criteria for RTT, and the clinical severity of the mutations did not differ between the two groups.
The presence of symptoms, including abdominal pain, irritability, vomiting, and fever, did not differ between individuals who had biliary tract disease and those who did not; none had jaundice. The median duration of symptoms in those who had biliary tract disease was 21 months. Laboratory tests were obtained in eight (29%) individuals within the subset; normal liver function was reported in all individuals evaluated. Diagnostic studies including abdominal ultrasound, abdominal CT scan, and CCK-HIDA scan were obtained in 22 (79%), 8 (29%), and 9 (32%) individuals, respectively, within the subset. Abnormal ultrasound, CT scan, and CCK-HIDA scan results were reported in 8 (36%), 3 (37%), and 5 (56%), respectively, of those individuals evaluated.
The perioperative diagnoses included cholecystitis in five, cholelithiasis in nine, and biliary dyskinesia in five individuals. Cholecystectomy was performed in 10 individuals, nine of whom had a laparoscopic procedure. The median (1st, 3rd quartile) age at surgery was 22 (18, 27) y. Serious post-operative complications, primarily infection, occurred in one individual. The median duration of the follow-up period after surgery was 3 y. Seven individuals reported resolution of biliary tract disease after surgery; one additional individual was newly post-op. Two individuals had persistent, but less severe and less frequent, symptoms including abdominal pain, irritability, and/or vomiting at follow-up.
When the 12 individuals with biliary tract disease were coupled with the entire NHRS cohort, the overall prevalence of biliary tract disease in the girls and young women with RTT was 4.4%. Of all the individuals in the NHRS cohort, those with biliary tract disease differed from those who did not have biliary tract disease with respect to median (1st, 3rd quartile) age [25 (21, 34) vs 10 (7, 17) y, p<0.001] and a positive family history (64% vs 26%, p<0.01). We found no difference between groups for mutation severity (data not shown).
DISCUSSION
Biliary tract disease occurs infrequently in RTT, but if identified, may have a potentially fatal outcome. In this study, the presenting symptoms of biliary tract disease were nonspecific, including abdominal pain, irritability, weight loss, and vomiting. Biliary dyskinesia, cholecystitis, or cholelithiasis, was documented in the medical records of 90%, 77%, and 70%, respectively, of the individuals with RTT. The prevalence of biliary tract disease in a large cohort of girls and women with RTT was 4.4%. Risk factors included older age at diagnosis and a positive family history. Seven of the ten individuals from the large cohort who underwent surgery for cholecystitis, biliary dyskinesia, or cholelithiasis had resolution of symptoms after surgical intervention.
Underlying dysmotility of the gallbladder or obstruction of the cystic duct in conjunction with gallstones formation frequently results in bile stasis and subsequent inflammation of the gallbladder. Starvation, dehydration, or immobilization may aggravate the inflammatory process because these conditions interrupt gallbladder contraction and emptying, leading to further bile stasis. Recurrent attacks of inflammation or obstruction progressively scar the gallbladder, resulting in further loss of function and additional gallstone formation. In the present study, these three disorders existed on a continuum in girls and women with RTT. The increased frequency with which biliary dyskinesia was identified from medical record review and the cohort survey suggests that the underlying motility disturbance of the gastrointestinal tract in RTT acts as a primary contributor to the pathophysiology. Starvation, dehydration, and immobilization, may aggravate biliary tract disease because individuals with RTT have oral motor feeding difficulties, may become dehydrated and undernourished, and are less mobile (4). Not surprisingly, the present study also underscores the increased frequency with which cholecystitis occurred in RTT, as it does in unaffected children (9). Some have argued that cholecystitis is more prevalent in children than previously described, as illustrated in one study whereby 87% of patients who had a pre-operative diagnosis of cholelithiasis by abdominal ultrasound also had a post-operative diagnosis of cholecystitis by pathologic examination (9).
Current trends suggest that the prevalence of biliary tract disease is increasing based on the increasing number of cholecystectomies performed (10–12). The prevalence of cholelithiasis in healthy children, determined by abdominal ultrasound, is estimated to be 1.9%, whereas the prevalence of biliary dyskinesia in children is unknown (13). The prevalence of gallbladder disease leading to surgery in healthy children is reported to be 2% to 4%, but may be as high as 6% in obese children (13–16). In the present study, we surveyed a representative sample of girls and young women who participated in the Natural History of Rett Syndrome study throughout the United States to estimate the prevalence of biliary tract disease in this disorder. We found the prevalence of 4.4% in RTT, determined by parental report, to be similar to that in the general population.
The etiology of symptomatic biliary tract disease in children is changing, with the frequency of hemolytic disease declining and the frequency of other entities rising, including cystic fibrosis, the use of oral contraceptives or total parenteral nutrition, prematurity, congenital malformations of the biliary tract, and intestinal disorders of the ileum (11,12,15,17). Risk factors commonly associated with biliary tract disease in children include older age, female gender, Hispanic ethnicity, obesity, and a positive family history (13,15,17–19). A female predominance of cholelithiasis and biliary dyskinesia has been identified in adolescence in most, but not all studies (9–11,13–15,19–21). In one report, 55% of patients were overweight, obese, or severely obese (15). A positive family history has been reported in as many as 53% of patients with cholelithiasis (13,18,19,22). However, no risk factors have been identified in some studies (12,14,17–19). In the present study, we found the primary risk factors for biliary tract disease to be older age at diagnosis and a positive family history, but not obesity based on BMI estimates, across all mutation groups of clinical severity. In both the smaller number of medical record reviews and the larger cohort of parents surveyed, the median age at diagnosis was 21 to 23 y and nearly two-thirds of the girls and young women with RTT who had confirmed gallbladder disease had a positive family history of biliary tract disease. We are aware of one additional girl with RTT who has a congenital malformation of the gallbladder.
The clinical features of biliary tract disease in children typically are described as colicky abdominal pain localized to the right upper quadrant or epigastric area in at least 85% of affected individuals, nausea and vomiting in approximately 60%, and fatty food intolerance in 10% (13,17,18,20). However, as many as 51% of children with cholelithiasis may be asymptomatic (13,17–19). In the present study, the overarching symptoms of irritability and presumed abdominal pain, reported by parents, were non-specific and did not differentiate between those who had or did not have biliary tract disease. Hence, a high index of suspicion for biliary tract disorders is warranted when parents report nonspecific symptoms without an apparent cause. Our review of medical records suggested that the duration of symptoms was less than 2 months, but based on the cohort survey, symptoms may be present for nearly 2 years. A similarly prolonged period of symptoms has been reported in healthy children with biliary dyskinesia (20).
Laboratory tests are abnormal in less than 50% of symptomatic patients, although white blood cell counts, liver function studies, and pancreatic lipase may be elevated in the presence of complications of biliary tract disease (13,18). In the present study, we found laboratory tests to be of limited value in detecting biliary tract disease. Four of the five individuals with abnormal liver function studies had cholelithiasis alone; the fifth individual had biliary dyskinesia and cholelithiasis. All five individuals underwent cholecystectomy. We did not detect clinical differences between these five individuals and the remainder of the group due to small sample size. The severity of disease in these five individuals could not be assessed; only one of these individuals had an elevated total bilirubin equal to 2 mg/dL, suggestive of an obstructive component. More importantly, the absence of abnormal laboratory values failed to correlate with the extent of pathology found at the time of surgery. It is of concern to us that surgical intervention may be delayed in the presence of nonspecific symptoms and the absence of abnormal laboratory studies, particularly in individuals who are unable to communicate their discomfort and distress.
Abdominal ultrasonography and radionuclide hepatobiliary imaging with cholecystokinin stimulation are the diagnostic procedures of choice for cholelithiasis and biliary dyskinesia, respectively, but both tests fail to detect cholecystitis (15,20,23). In one report, abdominal ultrasounds detected cholelithiasis in 88% and cholecystitis in 5% of patients, but pathology reports provided evidence that 87% of the group had cholecystitis (9). Similarly, in children who had CCK-HIDA scans consistent with the diagnosis of biliary dyskinesia and no mention of cholecystitis, pathology reports identified cholecystitis in 80% or more of these individuals (15,23–25). In the present study, 70% of abdominal ultrasounds documented gallstones, but only 7% reported thickened gallbladder walls consistent with cholecystitis. Similarly, 90% of the reports from CCK-HIDA scans documented an ejection fraction less than 35%, while none documented cholecystitis. In contrast, 77% of the pathology reports provided evidence for chronic cholecystitis. Although the proportions of these diagnostic entities are high, we cannot be certain of their absolute frequency. Medical records often were incomplete and in the survey parents did not recall if tests were performed nor did they always know the results of the studies performed. A more robust data set would better clarify the relationships among these diagnoses.
Laparoscopic cholecystectomy is the treatment of choice for symptomatic cholelithiasis (26). Cholecystectomy results in the resolution of symptoms in 100% of patients; recurrence of symptoms (post-cholecystectomy syndrome) may be observed in 5% of patients (19). Treatment with ursodeoxycholic acid has been proposed as a nonsurgical approach; dissolution primarily of radiolucent gallstones occurs in 7% to 37% of patients, but resolution of symptoms has been reported in 26% to 48% of affected individuals (18,19). Watchful waiting has been advocated for asymptomatic cholelithiasis, with no patients becoming symptomatic during a 1-y period of observation (18). In contrast, laparoscopic surgery has been proposed as an efficacious and durable procedure for biliary dyskinesia, with long-term resolution of symptoms in 34% to 44% of patients (21,23,24). In the present study, 85% of individuals with RTT whose medical records were reviewed and 83% of those identified with biliary tract disease in the NHRS subset underwent surgery. Although long-term follow-up was unavailable for the group whose medical records were reviewed, 70% of affected individuals from the large cohort who underwent surgery remained asymptomatic on average after three years of follow-up.
We acknowledge that this study had several limitations. In attempting to characterize the clinical features of biliary tract disease in RTT, we used a hybrid of methods including a retrospective review of medical records and a prospective survey questionnaire based on parental reporting. As a consequence, the frequency with which the diagnoses of biliary dyskinesia, cholecystitis, and cholelithiasis were made depended on the method of acquisition and the number of individuals assessed. Reliance on retrospective medical record reporting always is unsatisfactory because not every question is asked or recorded and the acquisition of documents often is incomplete. In addition, the validity of data collected from surveys depends on the accuracy of parental recollection. Nevertheless, to our knowledge, this work is the first attempt to synthesize current information about a potentially fatal gastrointestinal disorder in girls and women with RTT syndrome.
In summary, physicians should maintain a high index of suspicion for biliary tract disease in older girls and young women with RTT who have unexplained irritability and abdominal symptoms, particularly in individuals whose family history is positive for biliary tract disease. Prompt evaluation and early intervention may restore health and improve the quality of life of individuals affected with this disorder.
Supplementary Material
Supplemental Digital Content 1. Appendix. Parent Survey: Biliary Tract (Gallbladder) Disease and Cancer in Rett Syndrome
Supplemental Digital Content 2. Table 1. Clinical features of biliary tract disease in 46 girls and women with Rett syndrome identified by medical record review
Supplemental Digital Content 3. Table 2. Clinical features of biliary tract disease in individuals with Rett syndrome and/or MECP2 mutations from the Natural History of Rett Syndrome Study (n=28)
WHAT IS KNOWN/WHAT IS NEW.
What is known?
Gastrointestinal problems complicate the clinical course of girls and women with Rett syndrome (RTT).
The prevalence and clinical features of biliary tract disease in RTT has not been fully characterized.
What is new?
The prevalence of biliary tract disease was 4.4% in a large RTT cohort.
Risk factors included older age and a positive family history of biliary tract disease.
Diagnostic evaluation and surgical intervention resulted in resolution of symptoms in seven of ten individuals after surgical intervention.
Acknowledgments
Financial disclosures: The authors report the following financial disclosures: Drs. Motil, Skinner, Percy, Neul, Glaze, and Ms. Barrish, Lane, Geerts, Annese, and McNair received research support from NIH (NCRR U54 RR019478, U54 HD06122). Ms. Lane receives funds from RS.O in her capacity as a medical/nursing consultant.
Funding Sources: Funding for this project was provided by Rett Syndrome Organization (RS.O), the Rett Syndrome Association of Illinois, The Blue Bird Circle, the National Institutes of Health (NICHD U54 HD061222, NCRR U54 RR019478, and the Office of Rare Diseases Research). The views expressed in written materials or publications do not necessarily reflect the official policies of the Department of Health and Human Services, nor does mention by trade names, commercial practices, or organizations imply endorsement by the U.S. Government. This work is also a publication of the USDA/ARS Children’s Nutrition Research Center, Baylor College of Medicine, Houston, TX, and has been funded in part with federal funds from the US Department of Agriculture, Agricultural Research Service (Cooperative Agreement Number 58-3092-5-000). The content of this publication does not necessarily reflect the views or policies of the US Department of Agriculture, nor does mention of trade names commercial products, or organizations imply endorsement by this agency.
Abbreviations:
- MECP2
methyl-CpG-binding protein 2
- NCRR
National Center for Research Resources
- NIH
National Institutes of Health
- RDCRN
Rare Disease Clinical Research Network
- RS.O
Rett Syndrome.org
- RTT
Rett syndrome
REFERENCES
- 1.Amir RE, Van den Veyver IB, Schultz R, et al. Influence of mutation type and X chromosome inactivation on Rett syndrome phenotypes. Ann Neurol 2000;47:670–9. [PubMed] [Google Scholar]
- 2.Laurvick CL, de Klerk N, Bower C, et al. Rett syndrome in Australia: a review of epidemiology. J Pediatr 2006;148:347–52. [DOI] [PubMed] [Google Scholar]
- 3.Neul JL, Kaufmann WE, Glaze DG, et al. Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol 2010;68:944–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motil KJ, Caeg E, Barrish JO, et al. Gastrointestinal and nutritional problems occur frequently in girls and women with Rett syndrome. J Pediatr Gastroenterol Nutr 2012;55:292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tarquinio DC, Motil KJ, Hou W, et al. Growth failure and outcome in Rett syndrome: specific growth references. Neurology 2012;79:1653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cuddapah VA, Pillai RB, Shekar KV, et al. Methyl-CpG-binding protein 2 (MECP2) mutation type is associated with disease severity in Rett syndrome. J Med Genet 2014; 51:152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tarquinio DC, Hou W, Berg A, et al. The longitudinal course of epilepsy in Rett syndrome and related disorders. Brain 2017;140:306–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tarquinio DC, Hou W, Neul JL, et al. The course of awake breathing disturbance across the lifespan in Rett syndrome. Brain Dev 2018;40:515–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blackwood BP, Grabowski J. Chronic cholecystitis in the pediatric population: an underappreciated disease process. Gastroenterol Hepatol 2017;10:125–30. [PMC free article] [PubMed] [Google Scholar]
- 10.Matta SR, Kovacic K, Yan K, et al. Trends of cholecystectomies for presumed biliary dyskinesia in children in the United States. J Pediatr Nutr 2018;66:808–10. [DOI] [PubMed] [Google Scholar]
- 11.Walker SK, Maki AC, Cannon RM, et al. Etiology and incidence of pediatric gallbladder disease. Surgery 2013; 154:927–33. [DOI] [PubMed] [Google Scholar]
- 12.Miltenburg DM, Schaffer R, Breslin T, et al. Changing indications for pediatric cholecystectomy. Pediatrics 2000;105:1250–3. [DOI] [PubMed] [Google Scholar]
- 13.Wesdorp I, Bosman D, de Graaff A, et al. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr 2000;31:411–7. [DOI] [PubMed] [Google Scholar]
- 14.Kaechele V, Wabitsch M, Thiere D, et al. Prevalence of gallbladder stone disease in obese children and adolescents: influence of the degree of obesity, sex, and pubertal development. J Pediatr Gastroenterol Nutr 2006;42:66–70. [DOI] [PubMed] [Google Scholar]
- 15.Mehta S, Lopez ME, Chumpatazi BP, et al. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 2012;129:e82–e88. [DOI] [PubMed] [Google Scholar]
- 16.Nunes MM, Medeiros CC, Silva LR. Cholelithiasis in obese adolescents treated at an outpatient clinic. J Pediatr (Rio J) 2014;90:203–8. [DOI] [PubMed] [Google Scholar]
- 17.Bogue CO, Murphy AJ, Gerstle JT, et al. Risk factors, complications and outcomes of gallstones in children: a single center review. J Pediatr Gastroenterol Nutr 2010;50:303–8. [DOI] [PubMed] [Google Scholar]
- 18.Tuna Kirasclioglu C, Cuhaci Cakir B, Bayram G, et al. Risk factors, complications and outcome of cholelithiasis in children: a retrospective, single-centre review. J Paediatr Child Health 2016;52:944–9. [DOI] [PubMed] [Google Scholar]
- 19.Della Corte C, Falchetti D, Nebbia G, et al. Management of cholelithiasis in Italian Children: A national multicenter study. World J Gastroenterol 2008;14:1383–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santucci NR, Hyman PE, Harmon CM, et al. Biliary dyskinesia in children: a systematic review. J Pediatr Gastroenterol Nutr 2017;64:186–93. [DOI] [PubMed] [Google Scholar]
- 21.Mahida JB, Sulkowski JP, Cooper JN, et al. Prediction of symptom improvement in children with biliary dyskinesia. J Surg Res 2015;198:393–9. [DOI] [PubMed] [Google Scholar]
- 22.Frybova B, Drabec J, Lochmannova J, et al. Cholelithiasis and choledocolithiasis in children; risk factors for development. PLos One 2018;13:e0196475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lai SW, Rothenberg SS, Kay SM, et al. Outcomes of laparoscopy cholecystectomy for biliary dyskinesia in children. J Laparoendosc Adv Surg Tech A 2017;27:845–50. [DOI] [PubMed] [Google Scholar]
- 24.Siddiqui S, Newbrough S, Alterman D, et al. Efficacy of laparoscopic cholecystectomy in the pediatric population. J Pediatr Surg 2008;43:109–13. [DOI] [PubMed] [Google Scholar]
- 25.Hofeldt M, Richmond B, Huffman K, et al. Laparoscopic cholecystectomy for treatment of biliary dyskinesia is safe and effective in the pediatric population. Am Surg 2008;74:1069–72. [PubMed] [Google Scholar]
- 26.Esposito C, Gonzalez Sabin MA, Corcione F, et al. Results and complications of laparoscopic cholecystectomy in childhood. Surg Endosc 2001;15:890–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Appendix. Parent Survey: Biliary Tract (Gallbladder) Disease and Cancer in Rett Syndrome
Supplemental Digital Content 2. Table 1. Clinical features of biliary tract disease in 46 girls and women with Rett syndrome identified by medical record review
Supplemental Digital Content 3. Table 2. Clinical features of biliary tract disease in individuals with Rett syndrome and/or MECP2 mutations from the Natural History of Rett Syndrome Study (n=28)