Abstract
Adrenal gland injuries after a blunt abdominal trauma are rare events and represent important indicators for severe trauma. Multidetector CT evolution with high volumetric resolution and fast acquisition with the use of multiplanar reformatted (MPR) visualization allows for an accurate and fast diagnosis of the adrenal gland for post-traumatic pathologies. While, before its introduction the diagnosis was made mainly postmortem or during surgery. Adrenal injuries are unilateral up to 90% of the cases involving most commonly the right gland; thoracoabdominal organs injuries are often also associated. Bilateral adrenal lesions are asymptomatic, potentially leading to the development of acute adrenal insufficiency. The purpose of the present review was to determine the prevalence, the mechanism of injury and the different CT appearances of adrenal trauma. Prognosis and management of adrenal injury will also be reviewed.
Keywords: Emergency radiology, trauma imaging, adrenal glands, blunt abdominal trauma, adrenal injuries, hematoma, hemorrhage, multi-detector computed tomography (MDCT)
Introduction
Before the introduction of CT, adrenal gland trauma injuries were difficult to diagnose and were discovered from intra-operative findings or recognized at autopsy.
Nowadays, adrenal gland injuries following blunt abdominal trauma are increasingly recognized in trauma centers thanks to the improving diagnostic possibility of multi-detector computed tomography (MDCT), and the knowledge of the first CT semeiotic sign.
Due to the small size, the deep retroperitoneal position in the upper part of the abdomen with the presence of full fat around, the possibilities of traumatic adrenal injuries were scarce (0.03% to 4.95% of all abdominal blunt or penetrating trauma) (1-6).
Although relatively rare, adrenal injuries can be considered as reliable indicators for evaluating the severity of trauma. In postmortem series, the reported incidence of adrenal hemorrhage or injury in trauma patients is 7–26%, most of these patients died of unrecognized severe abdominal trauma (7,8). These data suggest the correlation between the presence of adrenal injuries and a severe trauma mechanism, recommending mandatory and accurate evaluation of other abdominal organs.
The adrenal injury may not exhibit clear signs or symptoms but can hesitate in subtle but severe problems in particular acute adrenal insufficiency or infection (9).
Patients with bilateral adrenal injury are associated with higher injury severity, morbidity and mortality (4,10) compared to unilateral adrenal injury occurring in 75% to 90% of cases (11-13).
This review aims to describe the first CT signs of adrenal injuries and their correlation with anatomic-pathology.
Anatomy, classification and injury mechanism
Adrenal glands are triangular-shaped endocrine glands located deep within the retroperitoneum on the top of each kidney. The right adrenal gland is locating higher than the left one (14). The adrenal glands have an abundant blood supply via three main arteries: superior, middle and inferior adrenal arteries respectively arising from the inferior phrenic artery, the abdominal aorta, and the renal artery. Venous drainage flows directly into the inferior vena cava on the right and the left renal vein and inferior vena cava on the left side (15).
Anatomopathology of adrenal glands divided them between the outer cortex and inner medulla. The outer cortex produces steroid hormones, and it is divided into three zones with different hormone production (aldosterone, cortisol, and androgens). The medullary part produces epinephrine and norepinephrine, and a miniscule portion of dopamine. The medullary part’s hormone is considered the body’s stress response, increasing cardiac output, and vascular resistance, or a combination of both (16,17).
Mehrazin et al. found that right-sided adrenal gland injuries (78.5%) were more frequent (13); there is also an increased probability of intraglandular bleeding off the right side gland; three theories trying to describe the reasons: direct compression between liver and spine, deceleration force, short term rising of the venous pressure due to the compression of the vena cava (3,5,18-20).
Epidemiology
It has been reported that the incidence rate of the adrenal trauma varied in the past 20 years from 0.15% to 4.95%. The mortality in patients who underwent adrenal trauma is reported to be more than twice for patients incurring a blunt trauma without adrenal injury (6).
Rana et al. found that the adrenal hematoma was present in 1.9% (51 of 2,692) of the patients who underwent CT for trauma, compared with value with the total incidence in all trauma patients (0.8%, 51 of 6,808 patients) (6). Pinto et al. found that only 82 patients (4%) with adrenal injuries in a group of 2,026 emergency multidetector had a CT examination performed in the setting of a major blunt trauma (11).
The same incidence on the total amount of trauma are found by Stawicki et al. (0.15%, 322 out of 210,508 admitted injured patients) (4). Raup et al. demonstrated a lower incidence analyzing more than 1.8 million traumatic patients (0.44%) (21).
The basis for the differences observed by the authors in the incidence rates could be put in relation with the current trends of CT utilization in an emergency department. On the one hand, the tendency to recommend CT even though the patient is very low risk, is continuously increasing, on the other hand, this increasing numbers of CT scans could raise the chances for early diagnosis of adrenal injuries (12,13,22,23).
Raup et al. (21) in the case mentioned above series with one and sometimes both the adrenal glands affected, reported that a percentage as high as 90.2% was caused by blunt trauma, 8.3% by penetrating, and 1.5% by unclassified injury, the incidence of the adrenal trauma being 0.44%. According to the literature data, vehicle crashes identified in the studies were the most prevalent (4,24). Increased mortality was associated with older age, higher Injury Severity Score (ISS), penetrating injuries, and injuries to other vital organs (21). Isolated adrenal injury in blunt trauma cases is rare (1.5%) but linked to the simultaneous presence of other associated injuries (50.9% ribs, 50.0% thorax, 41.6% liver, 30.9% vertebrae, 27.8% kidney, and 22.0% spleen) (21) (Figures 1,2). A bilateral adrenal hemorrhage is a rare event described in published series of either traumatic or non-traumatic conditions (5,6,13). Panda et al. (10) in contrast with the previous literature cited, observed a relatively high incidence of bilateral adrenal hematoma. Bilateral adrenal hematomas are more frequent in patients having lower Glasgow Coma Scale (GCS); having a higher ISS, ICU recovery time and worse outcomes. This is in part or ascribed to the adrenal insufficiency in the form of hyperkalemia and hypotension or to the associated intra-abdominal organ injuries.
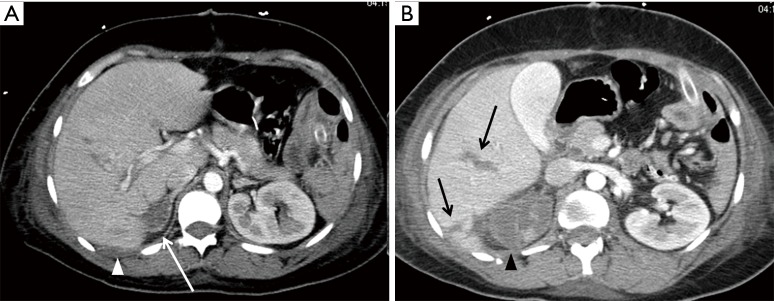
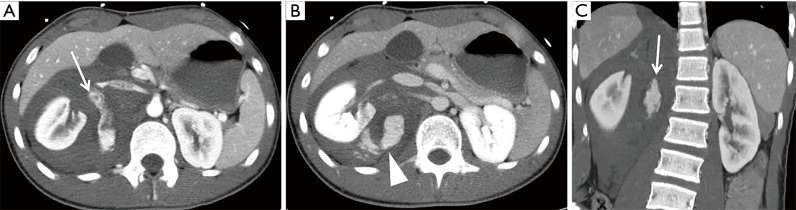
Figure 1.
Contrast enhanced multi-detector computed tomography (CE-MDCT) shows lacerations of the right lobe of the liver (VI segment) (black arrow), devascularization of the right kidney (black arrowhead), and hematoma of the right adrenal gland (white arrow). (A) A subtle perihepatic fluid collection is seen (white arrowhead).
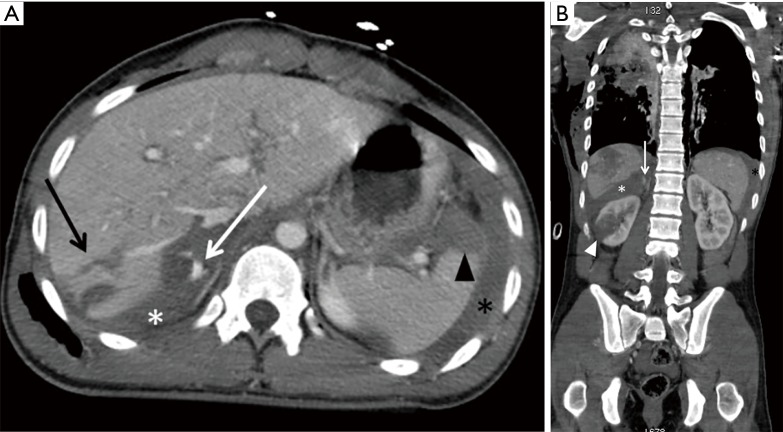
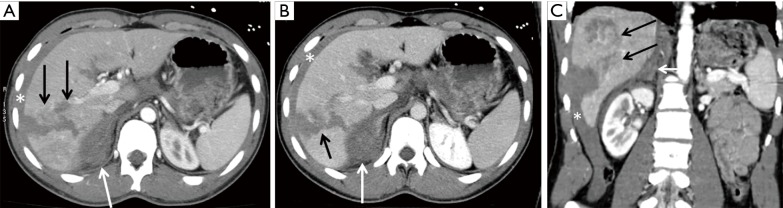
Figure 2.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan; (B) coronal reconstruction. CT shows lacerations of the right lobe of the liver (black arrows), contusion of the spleen (black arrowhead), laceration of the right kidney (white arrowhead) and right adrenal hemorrhage (white asterisk), with a little focus of active bleeding (white arrow). Perisplenic fluid collection is also seen (black asterisk).
Clinical symptoms
Adrenal gland trauma has no specific clinical presentation. Abdominal pain, nausea, vomiting, hypo- or hypertension, agitation, mental status alteration, and mild fever are the most common presenting symptoms. Timely clinical diagnosis is complicated causing the possibility of a severe medical mistake as retroperitoneal persistent hemorrhage and hematoma could eventually evolve into an abscess (19). It is important to recognize early signs of bilateral adrenal lesions potentially leading to the development of acute adrenal insufficiency, a condition that involves the destruction of 90% or more of each gland (25).
Bilateral adrenal gland injury may lead to adrenal insufficiency with “endocrine-related syndromes”: sudden decrement of adrenal steroid production with hemodynamic shock, related to a laboratory triad of hypoglycemia, hyperkalemia, and hyponatremia, acidosis-hypotension and lethargy may be present too. This endocrine-related syndrome if misdiagnosed could lead to death if misdiagnosed (2,19).
Some factors seem to be predisposing to adrenal hemorrhage: thromboembolic disease, coagulopathy, pregnancy, and burns (2,26). In patients with adrenal insufficiency and enlargement of adrenals suggestive of bilateral hemorrhage, a test for anticardiolipin and anti-β2 glycoprotein-I antibodies should be performed to prevent the fatal manifestation of the antiphospholipid syndrome (27).
The poor clinical evidence of adrenal gland lesions and the severe consequence of the related endocrine syndrome suggest the mandatory use of CT investigation in traumatic patients and a meticulous evaluation of CT signs of adrenal lesions.
CT features
MDCT has fast volumetric imaging acquisition, broad patient’s coverage and higher spatial resolution (28).
MDCT with its thin-section allows the use of multiplanar reformatted (MPR) algorithm for images reconstruction; location and shape of adrenal lesions are accurately defined together with the view of possible local and vascular injuries and other organs associated traumatic lesions (29).
US has a reduced sensitivity comparing to CT in traumatic patients’ evaluation with a fundamental role in the unstable patient with F.A.S.T. scan for detecting hemoperitoneum (9,30).
Adrenal injuries essential CT aspect is around hematoma (approximately 80% of cases of adrenal trauma) with a slightly hyperdense aspect (mean attenuation of 56 HU ±10) (Figure 3) (19,31,32). After contrast media (CM) administration the hematoma does not enhance remaining slightly hypodense, a capsule with a thin hyperdense peripheral rim could be observed (Figure 4). Hematoma’s size can vary from 3 to more than 10 cm (32) (Figure 5). CT signs of active bleeding consist in hyperdense spots in dynamic phase scans after CM administration; the presence of active bleeding is rare but required urgent embolization if diagnosed (19,32) (Figure 2).
Figure 3.

Contrast enhanced multi-detector computed tomography (CE-MDCT), axial scan. CT shows right adrenal hematoma, expanding the gland (white arrow).
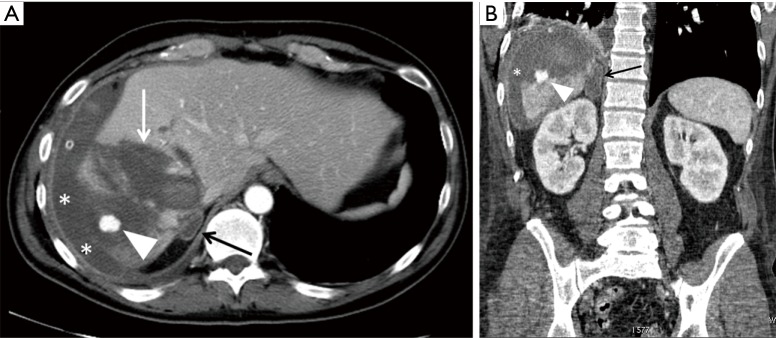
Figure 4.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan; (B) coronal reconstruction. CT shows a subtle right adrenal hematoma, with a thin enhanced peripheral rim (black arrow). A huge hepatic laceration is seen (white arrow) with a traumatic intrahepatic pseudoaneurysm (white arrowhead). A subcapsular hepatic hematoma is also appreciable (white asterisk).
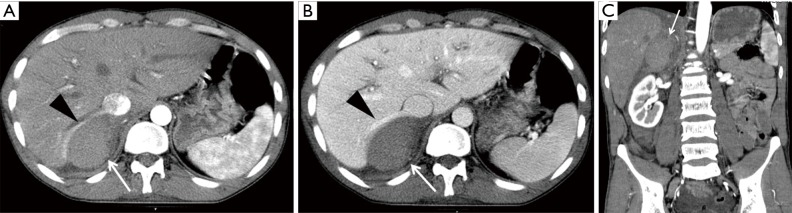
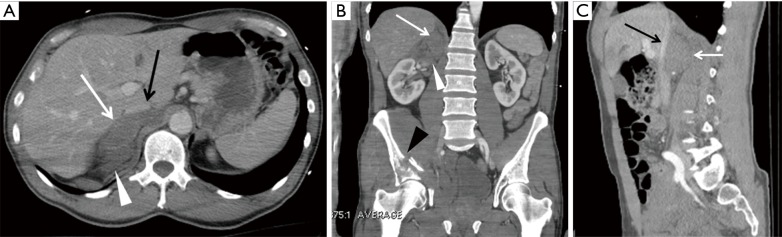
Figure 5.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan, arterial phase; (B) axial scan, venous phase; (C) coronal reconstruction, arterial phase. CT demonstrates a large right adrenal hematoma (white arrow) displacing the inferior vena cava and the right hepatic vein (black arrowhead).
Others possible findings include irregular hemorrhage (Figure 6), normal adrenal gland swelling, active extravasation of contrast material from the adrenal vessels (Figure 7). Adrenal hemorrhages may also be seen in the form of adrenal gland enlargement (Figure 8) and amorphous solid mass.
Figure 6.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan, arterial phase; (B) axial scan, venous phase; (C) coronal reconstruction, arterial phase. CT shows a huge retroperitoneal hemorrhage. A large focus of active bleeding is seen, which is already well evident in the arterial phase (white arrow) and enlarge in the arterial phase (white arrowhead). The active bleeding is due to the right adrenal artery tearing.
Figure 7.
Contrast enhanced multi-detector computed tomography (CE-MDCT), axial scans. CT shows a right adrenal irregular hemorrhage (white arrow) obliterating the gland. A right hepatic lobe laceration (black arrow), laceration of the spleen (black arrowhead) and perihepatic and perisplenic fluid collection (white asterisk) are also seen.
Figure 8.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan, arterial phase; (B) axial scan, venous phase; (C) coronal reconstruction, arterial phase. CT shows right adrenal hematoma as an adrenal gland enlargement (white arrow). Laceration of the right hepatic lobe (black arrow) and a subtle perihepatic fluid collection (white asterisk) are also seen.
Some cases of adrenal rupture have also been reported (24). Delays in diagnosis or misdiagnosis are often fatal for patients (33). In between 20% and 50% of the patients, the patients with bilateral adrenal hemorrhage had presented life-threatening adrenal insufficiency. In the event of sepsis, bilateral adrenal hemorrhage causes death in more than 90% of cases (34).
Associated CT findings include stranding of the periadrenal fat (93%) (Figures 9,10), retroperitoneal hemorrhage (22%), and thickened diaphragmatic crura (10%) (Figure 10) (2,5,6). The change of attenuation of retroperitoneal fat around the adrenal gland is due to blood infiltration, considering a diagnostic sign for adrenal hemorrhage, that sign could contribute to the indistinct appearance of the adrenal gland. CT sign consists of thin lacelike strands of soft tissue attenuation within the low-attenuation retroperitoneal fat (35) to more evident hyperdense tissue in the adrenal space.
Figure 9.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan; (B) coronal reconstruction; (C) sagittal reconstruction. CT shows a right adrenal hematoma, enlarging the gland (white arrow). Inferior vena cava is compressed and displaced (black arrow). It is also appreciable the periadrenal fat tissue thickening (white arrowhead). There is also a fracture of the right hemipelvis (black arrowhead).
Figure 10.
Contrast enhanced multi-detector computed tomography (CE-MDCT). (A) Axial scan; (B) sagittal reconstruction. CT shows a right adrenal hematoma (white asterisk), associated with stranding of the periadrenal fat tissue (white arrow). It is also appreciable thickening of the right diaphragmatic crus (black asterisk). A large intrahepatic hematoma is also seen (black arrow).
Hemorrhage can occur within some benign lesions or normal adrenal glands after trauma, causing the gland to increase rapidly in size. In the evaluation of incidental adrenal lesions, it is essential to evaluate the growth rate, eventually comparing the current exam to the previous one if present, if not 4–6 months are commonly suggested.
Over time, hematomas tend to decrease in size and attenuation, although adrenal enlargement can be observed in the first few weeks following trauma (36). Within weeks to months, the hematomas decrease in size tending to become centrally hypoattenuating. Months to years later, calcification can take the shape of a shrunken and densely calcified small adrenal gland following the complete reabsorption of hematoma. If the hematoma does not completely reabsorb and persists, an organized, chronic hematoma appears as a mass with a low-density center, with or without calcifications. Such masses are termed ‘‘adrenal pseudocysts’’ (33). The presence of calcifications can affect enhancing components on postcontrast CT.
The CT appearance of post hemorrhage pseudocysts is similar to other adrenal cysts; however, since they are usually the result of old hemorrhage, pseudocysts are more likely than endothelial cysts to contain septations, blood products, and soft tissue nodules. Pseudocysts are also more likely to contain calcifications (20–56% incidence) than endothelial cysts (9.5%); the calcifications are usually located within the cyst wall and can be very thick (37,38). The presence of a thickened irregular, enhancing wall in post hemorrhaging pseudocyst can be mistaken for a cystic neoplasm (39).
Differential diagnosis
Since adrenal gland trauma is uncommon (<5% of all adrenal trauma), in the absence of other abdominal organ injuries, there should be careful consideration for the possibility of a different diagnosis such as adenoma, carcinoma, myelolipoma, metastasis, pheochromocytoma or tuberculosis.
A systematic review of all the abdominal imaging studies revealed that adrenal incidentalomas occurred in the range from 1% to 4% (40-43).
It is not always easy to differentiate traumatic adrenal lesions, traumatic lesions in the pathologic gland or gland enlargements not related to the trauma.
Preexisting adrenal disorders can predispose the adrenal to injury and hemorrhage with minor trauma (44).
The primary tumor, such as the adrenocortical carcinoma, often appears as very large heterogeneous necrotic mass growing over time. While hematomas tend not to demonstrate on CT appreciable enhancement, the primary tumors and the metastatic disease typically demonstrate early enhancement and delayed wash-out of intravenous contrasts, differing in this aspect from the adenomas tending wash-out faster. In case of diagnostic doubts, MR should be considered for better tissue characterization.
Positron emission tomography seems to have a role in evaluating active cellular metabolism (32).
Treatment and prognosis
Because of the rarity and heterogeneity of the clinical presentation and prognosis of traumatic adrenal injury, no specific guidelines exist.
The management of a patient with adrenal gland injury may be operative or non-operative according to the patients’ hemodynamic status, the severity of the adrenal injury, and the presence and severity of the other lesions.
Adrenal trauma should carefully be considered because of the possibility of significant hemorrhage requiring transfusion.
Electrolyte disturbances including hyponatremia, hyperkalemia, hypoglycemia, hypocalcemia and hypermagnesemia, acidosis, hypotension, and lethargy (19) associated with adrenal insufficiency in acute settings due to bilateral adrenal hemorrhage may be an early and fatal manifestation. Diagnosis of bilateral adrenal hemorrhage in these patients can be made rapidly by a CT scan of the abdomen to start the treatment with glucocorticoids and mineralocorticoids. In patients with adrenal insufficiency and enlargement of adrenals suggestive of bilateral hemorrhage, a test for anticardiolipin and anti-β2glycoprotein I antibodies should be performed to prevent the fatal manifestation of the antiphospholipid syndrome (27).
Adrenal injuries can usually be managed conservatively, but when acute bleeding symptoms that require rapid treatment are suspected, surgery or interventional radiology procedures are needed (2,45).
Adrenalectomy should be reserved for cases with extensive parenchymal damage with the goal of saving even a minor part especially if both glands are involved (46).
Adrenal traumatic hemorrhages management through transcatheter angiographic embolization, both in adult and in pediatric patients are reported in the literature (19,47). Transcatheter embolization is often a chance in a hemodynamically unstable patient to rapidly solve an active source of bleeding (48). Isolated adrenal injuries are not fatal and do not require surgery, and thus they should be managed conservatively.
When a definitive diagnosis is not possible on the initial scan, short-interval follow-up (6–12 weeks) CT imaging is a reasonable recommendation aimed at ensuring appropriate and definitive diagnosis.
In patients who had a traumatic unilateral or bilateral adrenal hematoma, it is necessary to determine whether the lesion is a neoplastic process complicated by hemorrhage. For these patients, careful imaging analysis is necessary to identify an underlying adrenal cyst or neoplasm as the cause of the hemorrhage. CT performed with and without intravenous contrast material is of value to distinguish between an uncomplicated hematoma and an underlying neoplastic process of the adrenal gland. MR imaging allows a better tissue characterization and relatively precise timing of the blood. Serial imaging can help to understand the clinical evolution of the clot properly. In children, US or CEUS maybe have a role too. Finally, for the distinction between benign and malignant masses in the adrenal lesion in order to decide which further management to follow, either needle biopsy or excision biopsy or conservative management is required (39,49).
Conclusions
Knowledge of CT features of common patterns of adrenal injury consequent in a traumatic patient is essential for radiologists to avoid misdiagnosis or unnecessary surgical interventions.
Adrenal lesions in traumatic patients are rare but often associated with severe trauma dynamics and with others organ injuries considering the adrenal lesions as an indicator of severe trauma.
CT patterns could be varied and not always is possible to separate the previous condition to post-traumatic changes. Generally growing of adrenal dimension with a slightly hyperdense aspect is suggestive for post-traumatic adrenal hematoma. No contrast media enhancement is evident in adrenal hematoma; the presence of dynamic enhancement after contrast media administration is to be considered as active bleeding and handled immediately with surgery or endovascular treatment.
When CT diagnosis is not clear the use of MRI is useful to evaluate a better characterization of tissues and blood presence and timing; MRI may have a role also in the follow-up of stable patients. Sometimes PET imaging is necessary to evaluate metabolic activity.
Especially in a pediatric patient, US or CEUS may be considered useful in the follow-up.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Elsayes KM, Mukundan G, Shirkhoda A, et al. Adrenal masses: MR imaging features with pathologic correlation. Radiographics 2004;24 Suppl 1:S73-86. 10.1148/rg.24si045514 [DOI] [PubMed] [Google Scholar]
- 2.Sinelnikov AO, Abujudeh HH, Chan D, et al. CT manifestations of adrenal trauma: experience with 73 cases. Emerg Radiol 2007;13:313-8. 10.1007/s10140-006-0563-z [DOI] [PubMed] [Google Scholar]
- 3.To’o KJ, Duddalwar VA. Imaging of traumatic adrenal injury. Emerg Radiol 2012;19:499-503. 10.1007/s10140-012-1063-y [DOI] [PubMed] [Google Scholar]
- 4.Stawicki SP, Hoey BA, Grossman MD, et al. Adrenal gland trauma is associated with high injury severity and mortality. Curr Surg 2003;60:431-6. 10.1016/S0149-7944(02)00796-1 [DOI] [PubMed] [Google Scholar]
- 5.Burks DW, Mirvis SE, Shanmuganathan K. Acute adrenal injury after blunt abdominal trauma: CT findings. AJR Am J Roentgenol 1992;158:503-7. 10.2214/ajr.158.3.1738984 [DOI] [PubMed] [Google Scholar]
- 6.Rana AI, Kenny PJ, Lockhart ME, et al. Adrenal gland hematomas in trauma patients. Radiology 2004;230:669-75. 10.1148/radiol.2303021345 [DOI] [PubMed] [Google Scholar]
- 7.Porter JM, Muscato K, Patrick JR. Adrenal haemorrhage: a comparison of traumatic and nontraumatic deaths. J Natl Med Assoc 1995;87:569-71. [PMC free article] [PubMed] [Google Scholar]
- 8.Sevitt S. Post-traumatic adrenal apoplexy. J Clin Pathol 1955;8:185-94. 10.1136/jcp.8.3.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinto A, Scaglione M, Pinto F, et al. Adrenal injuries: spectrum of CT findings. Emerg Radiol 2003;10:30-3. [DOI] [PubMed] [Google Scholar]
- 10.Panda A, Kumar A, Gamanagatti S, et al. Are traumatic bilateral adrenal injuries associated with higher morbidity and mortality? A prospective observational study. J Trauma Manag Outcomes 2015;9:6. 10.1186/s13032-015-0026-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinto A, Scaglione M, Guidi G, et al. Role of multidetector row computed tomography in the assessment of adrenal gland injuries. Eur J Radiol 2006;59:355-8. 10.1016/j.ejrad.2006.04.029 [DOI] [PubMed] [Google Scholar]
- 12.Gabal-Shehab L, Alagiri M. Traumatic adrenal injuries. J Urol 2005;173:1330-1. 10.1097/01.ju.0000155459.11926.61 [DOI] [PubMed] [Google Scholar]
- 13.Mehrazin R, Derweesh IH, Kincade MC, et al. Adrenal trauma: Elvis Presley Memorial Trauma Center experience. Urology 2007;70:851-5. 10.1016/j.urology.2007.07.004 [DOI] [PubMed] [Google Scholar]
- 14.Trinci M, Greco F, Ramunno M, et al. Adrenal Gland Injuries. In: Miele V, Trinci M. editors. Diagnostic Imaging in Polytrauma Patients. Basel: Springer International Publishing, 2018:389-407. [Google Scholar]
- 15.Rao RH, Vagnucci AH, Amico JA. Bilateral massive adrenal haemorrhage: early recognition and treatment. Ann Intern Med 1989;110:227-35. 10.7326/0003-4819-110-3-227 [DOI] [PubMed] [Google Scholar]
- 16.Sadler GP, Wheeler MH. Open anterior right adrenalectomy. Oper Tech Gen Surg 2002;4:279-87. 10.1053/otgn.2002.25345 [DOI] [Google Scholar]
- 17.Lucey BC. Adrenal Trauma and Intervention. In: Blake Michael A, Boland Giles WL. editors. Adrenal Imaging. New York City: Humana Press, 2009. [Google Scholar]
- 18.Gómez RG, McAninch JW, Carrol PR. Adrenal gland trauma: diagnosis and management. J Trauma 1993;35:870-4. 10.1097/00005373-199312000-00012 [DOI] [PubMed] [Google Scholar]
- 19.Roupakias S, Papoutsakis M, Tsikopoulos G. Adrenal injuries following blunt abdominal trauma in children: report of two cases. Ulus Travma Acil Cerrahi Derg 2012;18:171-4. 10.5505/tjtes.2012.65390 [DOI] [PubMed] [Google Scholar]
- 20.Woodruff S, Yeung M, Grodski S, et al. Adrenal injuries and incidentalomas in trauma patients at an urban trauma centre. J Curr Surg 2012;2:123-9. [Google Scholar]
- 21.Raup VT, Eswara JR, Vetter JM, et al. Epidemiology of Traumatic Adrenal Injuries Requiring Surgery. Urology 2016;94:227-31. 10.1016/j.urology.2016.03.022 [DOI] [PubMed] [Google Scholar]
- 22.Iuchtman M, Breitgand A. Traumatic adrenal haemorrhage in children: an indicator of visceral injury. Pediatr Surg Int 2000;16:586-8. 10.1007/s003830000423 [DOI] [PubMed] [Google Scholar]
- 23.Schwarz M, Horev G, Freud E, et al. Traumatic adrenal injury in children. Isr Med Assoc J 2000;2:132-4. [PubMed] [Google Scholar]
- 24.Safioleas M, Stamatakos M, Safioleas C, et al. Adrenal rupture after blunt abdominal trauma. Chirurgia (Bucur) 2008;103:107-9. [PubMed] [Google Scholar]
- 25.Chin R. Adrenal Crisis. Crit Care Clin 1991;7:23-42. 10.1016/S0749-0704(18)30321-X [DOI] [PubMed] [Google Scholar]
- 26.Sayit AT, Sayit E, Gunbey HP, et al. Imaging of unilateral adrenal haemorrhages in patients after blunt abdominal trauma: report of two cases. Chin J Traumatol 2017;20:52-5. 10.1016/j.cjtee.2016.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caron P, Chabannier MH, Cambus JP, et al. Definitive adrenal insufficiency due to bilateral adrenal haemorrhage and primary antiphospholipid syndrome. J Clin Endocrinol Metab 1998;83:1437-9. 10.1210/jcem.83.5.4833 [DOI] [PubMed] [Google Scholar]
- 28.Soto JA, Anderson SW. Multidetector CT of Blunt Abdominal Trauma. Radiology 2012;265:678-93. 10.1148/radiol.12120354 [DOI] [PubMed] [Google Scholar]
- 29.Regine G, Stasolla A, Miele V. Multidetector computed tomography of the renal arteries in vascular emergencies. Eur J Radiol 2007;64:83-91. 10.1016/j.ejrad.2007.06.007 [DOI] [PubMed] [Google Scholar]
- 30.Rhea JT, Garza DH, Novelline RA. Controversies in emergency radiology CT versus ultrasound in the evaluation of blunt abdominal trauma. Emerg Radiol 2004;10:289-95. [DOI] [PubMed] [Google Scholar]
- 31.Mahajan A, Rao V, Thakur M, et al. Adrenal injury after blunt abdominal trauma: correlation between CT findings and injury severity score. ECR 2010, Poster No.: C-1176. doi: 10.1594/ecr2010/C-1176. [DOI]
- 32.Jordan E, Poder L, Courtier J, et al. Imaging of nontraumatic adrenal haemorrhage. AJR Am J Roentgenol 2012;199:W91-8. 10.2214/AJR.11.7973 [DOI] [PubMed] [Google Scholar]
- 33.Lee MJ, Kim AG, Jang JE, et al. A case of traumatic bilateral adrenal haemorrhage mimicking bilateral adrenal adenomas. YUJM 2012;29:35-37. [Google Scholar]
- 34.Sacerdote MG, Johnson PT, Fishman EK. CT of the adrenal gland: the many faces of adrenal haemorrhage. Emerg Radiol 2012;19:53-60. 10.1007/s10140-011-0989-9 [DOI] [PubMed] [Google Scholar]
- 35.Turgut AT, Onur MR, Akpinar E, et al. Congenital and Acquired Nonneoplastic Adrenal Diseases. In: Dogra S, MacLennan GT. editors. Genitourinary Radiology: Male Genital Tract, Adrenal and Retroperitoneum. London: Springer-Verlag London, 2013:211-30. [Google Scholar]
- 36.Schek J, Macht S, Klasen-Sansone J, et al. Clinical impact of hyperattenuation of adrenal glands on contrast-enhanced computed tomography of polytraumatised patients. Eur Radiol 2014;24:527-30. 10.1007/s00330-013-3050-4 [DOI] [PubMed] [Google Scholar]
- 37.Guo YK, Yang ZG, Li Y, et al. Uncommon adrenal masses: CT and MRI features with histopathologic correlation. Eur J Radiol 2007;62:359-70. 10.1016/j.ejrad.2006.12.011 [DOI] [PubMed] [Google Scholar]
- 38.Rozenblit A, Morehouse HT, Amis ES. Cystic adrenal lesions: CT features. Radiology 1996;201:541-8. 10.1148/radiology.201.2.8888255 [DOI] [PubMed] [Google Scholar]
- 39.Kawashima A, Sandler CM, Ernst RD, et al. Imaging of nontraumatic haemorrhage of the adrenal gland. Radiographics 1999;19:949-63. 10.1148/radiographics.19.4.g99jl13949 [DOI] [PubMed] [Google Scholar]
- 40.Dunnick NR, Korobkin M. Imaging of adrenal Incidentalomas: current status. AJR Am J Roentgenol 2002;179:559-68. 10.2214/ajr.179.3.1790559 [DOI] [PubMed] [Google Scholar]
- 41.Bovio S, Cataldi A, Reimondo G, et al. Prevalence of adrenal incidentaloma in a contemporary computerized tomography series. J Endocrinol Invest 2006;29:298-302. 10.1007/BF03344099 [DOI] [PubMed] [Google Scholar]
- 42.Young WF., Jr Management approaches to adrenal incidentalomas. A view from Rochester, Minnesota. Endocrinol Metab Clin North Am 2000;29:159-85. 10.1016/S0889-8529(05)70122-5 [DOI] [PubMed] [Google Scholar]
- 43.Young WF., Jr Clinical practice. The incidentally discovered adrenal mass. N Engl J Med 2007;356:601-10. 10.1056/NEJMcp065470 [DOI] [PubMed] [Google Scholar]
- 44.Daly KP, Ho CP, Persson DL, et al. Traumatic retroperitoneal injuries: review of multidetector CT findings. Radiographics 2008;28:1571-90. 10.1148/rg.286075141 [DOI] [PubMed] [Google Scholar]
- 45.Lee YS, Jeong JJ, Nam KH, et al. Adrenal injury following blunt abdominal trauma. World J Surg 2010;34:1971-4. 10.1007/s00268-010-0537-x [DOI] [PubMed] [Google Scholar]
- 46.Liao CH, Lin J, Fu CY, et al. Adrenal gland trauma: is extravasation an absolute indication for intervention? World J Surg 2015;39:1312-9. 10.1007/s00268-015-2953-4 [DOI] [PubMed] [Google Scholar]
- 47.Igwilo OC, Sulkowski RJ, Shah MR, et al. Embolization of traumatic adrenal haemorrhage. J Trauma 1999;47:1153-5. 10.1097/00005373-199912000-00032 [DOI] [PubMed] [Google Scholar]
- 48.Ierardi AM, Petrillo M, Patella F, et al. Interventional radiology of the adrenal glands: current status. Gland Surg 2018;7:147-65. 10.21037/gs.2018.01.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wedmid A, Palese M. Diagnosis and treatment of the adrenal cyst. Curr Urol Rep 2010;11:44-50. 10.1007/s11934-009-0080-1 [DOI] [PubMed] [Google Scholar]