Abstract
Objectives
This study aims to examine patterns and first mentions of reported use of new or uncommon drugs across 13 years, among nationally representative samples in the United States.
Methods
Participants (ages ≥12) in the National Surveys on Drug Use and Health (2005–2017, N = 730,418) were provided opportunities to type in names of new or uncommon drugs they had ever used that were not specifically queried. We examined self-reported use across survey years and determined years of first mentions.
Results
From 2005 to 2017, there were 2,343 type-in responses for use of 79 new or uncommon synthetic drugs, and 54 were first-ever mentions of these drugs. The majority (65.8%) of mentions were phenethylamines (e.g., 2C-x, NBOMe), which were also the plurality of new drug mentions (n = 22; 40.7%). Mentions of 2C-x drugs in particular increased from 30 mentions in 2005 to 147 mentions in 2013. We estimate an upward trend in use of new or uncommon drugs between 2005 and 2017 (p < 0.001).
Conclusion
Although type-in responses on surveys are limited and underestimate prevalence of use, such responses can help inform researchers when new compounds are used. Continued surveillance of use of new and uncommon drugs is needed to inform adequate public health response.
Keywords: new psychoactive substances, phenethylamines, psychedelics, synthetic cathinones, tryptamines
1 |. INTRODUCTION
New psychoactive substances (NPS) continue to emerge throughout the United States and Europe. In fact, dozens of NPS are detected for the first time in Europe every year, with 51 having been discovered in 2017 and over 100 discovered in 2014 (European Monitoring Centre for Drugs and Drug Addiction, 2018). Likewise, at least 36 NPS were discovered in the United States for the first time via drug seizures in 2016/2017 (U.S. Drug Enforcement Administration, 2017; U.S. Drug Enforcement Administration, 2018). Drug identifications from seizures have been the primary source for determining which new drug compounds are diffusing throughout the drug market, but seizure data are epidemiologically limited as confiscations do not necessarily reflect the wide variety of drugs used by the population. Reports of adverse outcomes to Poison Control Centers are another common method of tracking use of various drugs, but reports are limited by their dependence on users experiencing an adverse outcome and by users or health care professionals reporting the adverse outcome (Palamar, Su, & Hoffman, 2016; Warrick et al., 2013). Hospitalization and mortality data are similarly limited due to underreporting and underdetection of use (European Monitoring Centre for Drugs and Drug Addiction, 2017; Slavova et al., 2017). Therefore, further methods of tracking use of new or uncommon drugs are needed. In addition to drug identification data derived from seizures and adverse drug-related outcomes, we believe that survey data can offer additional insights by providing a more comprehensive picture on use of new or uncommon drugs.
Tracking emergence and prevalence of use of new and uncommon drugs is important for informing prevention and educational efforts. For example, the quick emergence of synthetic cannabinoids and synthetic cathinones (“bath salts”) in the United States was associated with tens of thousands of poisonings (American Association of Poison Control Centers, 2016; Cordeiro, Daro, Seung, Klein-Schwartz, & Kim, 2018), suggesting the need for better monitoring of emerging drugs in order to help prevent adverse outcomes associated with use. Surveys are the leading source of gathering data on use of drugs, but they tend to focus heavily on the most common drugs (e.g., cannabis and cocaine) and drugs known to be associated with high rates of dependence (e.g., heroin and methamphetamine; Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2018; Kann et al., 2018; Substance Abuse and Mental Health Services Administration, 2017). Little focus, however, is paid to less common or newly emergent drugs unless there are quick surges in popularity—for example, synthetic cannabinoids and synthetic cathinones (Johnston et al., 2018). This lack of attention represents a problem, given that there are hundreds of potentially dangerous drugs that are new or relatively uncommon. Although some national surveys in the United States have begun including questions about use of some new drug classes (e.g., “synthetic marijuana” and “bath salts”; Johnston et al., 2018), specific drugs within these classes are not queried.
In this paper, we describe patterns and emergence of self-reported use of various new or uncommon drugs, assessed via type-in responses, from 13 consecutive cohorts assessed by a nationally representative survey in the United States. We believe these data can help fill in the gaps with regard to the sparsity of epidemiological data focusing on NPS and other uncommon psychoactive drugs.
2 |. METHODS
2.1 |. Procedure
Data came from the 13 most recent cohorts (2005–2017) of the National Survey on Drug Use and Health (NSDUH), an ongoing cross-sectional survey of noninstitutionalized individuals ages ≥12 in the 50 U.S. states and District of Columbia (Substance Abuse and Mental Health Services Administration, 2017). Each year, NSDUH surveys over 55,000 respondents. We included 2005 as the first year to ensure that results are comparable with the annual European Drug Report, which presents the number of new NPS identified throughout Europe each year by the EU Early Warning System (European Monitoring Centre for Drugs and Drug Addiction, 2018). NSDUH is a nationally representative multistage area probability sample. Surveys are administered via computer-assisted interviewing conducted by an interviewer and audio computer-assisted self-interviewing (ACASI). For the computer-assisted interviewing, interviewers administered a computer-based survey to participants. For the ACASI, respondents were provided with a computer and headphones and asked to complete the survey; interviewers were trained to not look at the screens during administration in order to maintain privacy and confidentiality and to increase honest reporting. The ACASI collected variables including the type-in response data. The weighted interview response rates between 2005 and 2017 ranged from 68.4% to 76.0%.
3 |. DRUG USE VARIABLES
Participants were asked whether they had ever used a variety of common drugs. However, in the section asking about various common psychedelics (e.g., Lysergic acid diethylamide (LSD)), participants were asked whether they had ever used any other “hallucinogens” besides the compounds that were listed for them. Those who answered affirmatively were asked to type in the name(s) of the other hallucinogens they had ever used. They were instructed that if they were not able to spell the drug, they should make their best guess (Center for Behavioral Health Statistics and Quality, 2015). Participants were able to list up to five drugs and were given a similar opportunity to type in names of drugs used that were not queried when asked about stimulants, inhalants, sedatives, analgesics, and about drugs ever injected. However, as of 2015, open-ended questions about use of “other” stimulants, sedatives, and analgesics were no longer included in the survey.
NSDUH coded these responses and provided variables indicating which drugs were typed in by participants. For example, for relevant variables, response #6171 was coded as “4-acetoxy-N,N-dimethyltryptamine, 4-AcO-DMT,” indicating that the participant typed in the name of this compound. We focused on the 79 synthetic psychoactive compounds not directly queried by NSDUH that were listed between 2005 and 2017. The only exception was that in 2006, NSDUH added a question about use of DMT/AMT/Foxy, which was asked after the type-in option for other psychedelics (and in 2015, the question was moved before the open-ended question). Due to N,N-Dimethyltryptamine (DMT’s) popularity as a classic psychedelic and to the survey’s change in design, we did not consider DMT in this analysis. We did, however, still consider type-in responses for AMT and Foxy.
We cataloged each new or uncommon synthetic drug reported across all 13 cohorts. Specifically, we first identified the survey year when a specific compound was first ever mentioned on the survey, based on when the drug was assigned its own code for the first time (e.g., #6171 for 4-AcO-DMT). We ensured that neither the drug name nor code number appeared in previous data sets. Specifically, because 2005 was the first cohort in this analysis, we also checked the 2003 and 2004 codebooks (data not formally analyzed) to confirm whether drugs mentioned in 2005 or thereafter were first mentions. After confirming first mentions of specific compounds, we then cataloged all 79 compounds into common classifications guided by previous publications and government reports. Specifically, we ensured that every drug examined had previously been classified into one of the following classes: 2C-x (King, Nutt, & Independent Scientific Committee on Drugs, 2014; Shulgin & Shulgin, 1991; U.S. Drug Enforcement Administration Diversion Control Division, 2017; Yu et al., 2008), DOx (Shulgin & Shulgin, 1991), NBOMe (U.S. Drug Enforcement Administration Diversion Control Division, 2017), other phenethylamines (Greene, 2013; King et al., 2014; Shulgin & Shulgin, 1991), synthetic cathinones (McGraw & McGraw, 2012; Power et al., 2015; Prosser & Nelson, 2012; U.S. Drug Enforcement Administration Diversion Control Division, 2014), tryptamines (Glennon et al., 2000; Shulgin & Shulgin, 1997; U.S. Drug Enforcement Administration Diversion Control Division, 2017; van Hout & Hearne, 2017), synthetic cannabinoids (Deng, Verrico, Kosten, & Nielsen, 2018; U.S. Drug Enforcement Administration Diversion Control Division, 2014), dissociatives (arylcyclohexylamines; Berquist et al., 2018; De Paoli, Brandt, Wallach, Archer, & Pounder, 2013), lysergamides (Brandt et al., 2016; Brandt et al., 2017a; Brandt et al., 2017b; Klinke, Muller, Steffenrud, & Dahl-Sorensen, 2010), and piperazines (U.S. Drug Enforcement Administration Diversion Control Division, 2017). 2C, DOx, NBOMe, and other phenethylamines were further classified into an overall phenethylamine class as per the cited studies. The mention of “synthetic mushrooms” was added to tryptamines as this likely referred to 4-AcO-DMT or a similar tryptamine (Herrmann, Johnson, Johnson, & Vandrey, 2016), and the mention of “synthetic LSD/acid” was added to the lysergamide class (van Hout & Hearne, 2017). After classifying each drug into categories, we then computed counts of mentions for each specific compound and number of counts of all compounds in each class—in total and by survey year. In this report, we (a) describe when specific drugs were mentioned for the first time and (b) present the frequency of individual drugs and drug classes across survey years.
All count statistics described above were computed using unweighted data as we presented frequencies (of these rare drugs) and not percentages. However, we were able to compute prevalence estimates and examine trends over time regarding overall use of new and uncommon drugs examined in this study. This was done using logistic regression by estimating odds of use as a linear function of time as a continuous predictor. In these models, we adjusted for the complex survey design and used sample weights to account for oversampling of young respondents and unit-level and individual-level nonresponse in order to derive nationally representative estimates (Heeringa, West, & Berglund, 2010). This secondary analysis was exempt for review by the New York University Langone Medical Center Institutional Review Board.
4 |. RESULTS
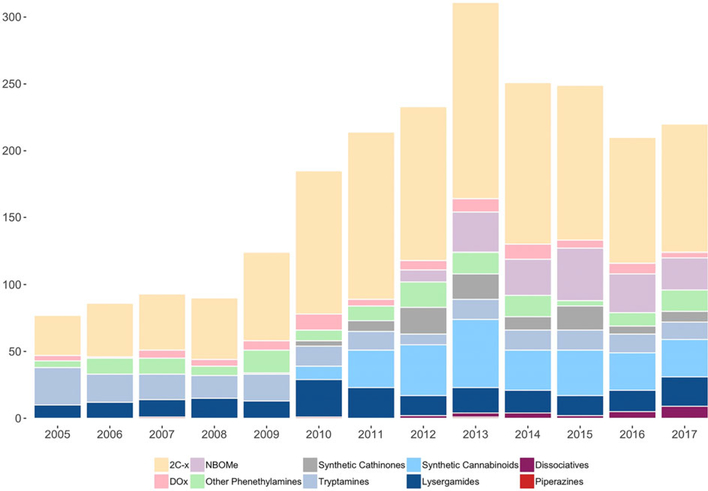
Figure 1 presents the number of mentions of new or uncommon drugs from 2005 to 2017. There were fewer than 100 mentions peryearfrom 2005 to 2008, and there was a steady increase in mentions from 2009 onwards, peaking in 2013 before decreasing slightly. Table 1 presents the frequencies of type-in response mentions for each new or uncommon drug from 2005 to 2017. Two thirds of mentions (65.8%) were phenethylamines, which consisted of 37 drugs. 2C-x compounds were the most prevalent subclass of overall mentions and comprised nearly half (48.9%) of all drug mentions. 2C-x mentions increased from 30 in 2005 to 147 in 2013 and then decreased through 2017. This pattern was driven largely by 2C-B, 2C-E, and 2C-I, which comprised over 9/10 (91.0%) of 2C-x series mentions. With regard to other psychedelic phenethylamines, there were 86 mentions of DOx series drugs and 158 NBOMe mentions. NBOMe compounds were not mentioned until 2012, and 72.2% of these mentions were 25I-NBOMe. Other phenethylamines accounted for another 153 mentions.
FIGURE 1.
Number of new or uncommon drugs reported each year, 2005–2017
TABLE 1.
Type -in mentions of new and uncommon drugs, 2005–2017
| 2C-x | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| 2C-B (Bromo mescaline, Nexus) | 9 | 11 | 19 | 13 | 20 | 34 | 50 | 35 | 33 | 48 | 40 | 33 | 34 | 379 |
| 2C-I (2,5-Dimethoxy-4-iodophenethylamine) | 13 | 17 | 10 | 18 | 30 | 36 | 42 | 41 | 51 | 41 | 40 | 37 | 34 | 410 |
| 2C-E (2–5-Dimethoxy-4-ethyl-phenethylamine) | 4 | 5 | 6 | 12 | 10 | 28 | 29 | 31 | 49 | 22 | 24 | 14 | 19 | 253 |
| 2C-T-2 | 2 | 2 | 4 | 1 | 1 | 4 | 3 | 3 | 1 | 2 | 1 | 1 | 2 | 27 |
| 2C-T-7 (T7, Blue Mystic) | 2 | 4 | 2 | 1 | 2 | 3 | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 21 |
| 2C-D (2,5-Dimethoxy-4-methylphenethylamine) | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 3 |
| 2C-T (2,5-Dimethoxy-4-methylthiophenethylamine) | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 5 |
| 2C-T-21 (2,5-dimethoxy-4-(2-fluoroethylthio)phenethylamine) | 0 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 4 |
| 2C-C (2–5-Dimethoxy-4-chlorophenethylamine) | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 5 |
| 2C-BCB (TCB-2) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 4 |
| 2C-P (4-propyl-2,5-dimethoxyphenethylamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 9 | 2 | 7 | 6 | 4 | 29 |
| 2C-F (2,5-dimethoxy-4-fluorobenzaldehyde) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 2C-C (4-chloro-2,5-dimethoxyphenethylamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 1 | 5 |
| 2C-B-Fly (2C-Bromo-Fly) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 2C-x total | 30 | 40 | 42 | 46 | 66 | 107 | 125 | 115 | 147 | 121 | 116 | 94 | 96 | 1145 |
| DOx | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| DOM (STP) | 4 | 1 | 5 | 1 | 1 | 3 | 1 | 2 | 3 | 6 | 1 | 4 | 1 | 33 |
| DOI (2,5-Dimethoxy-4-iodoamphetamine) | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 2 | 0 | 8 |
| DOC (2,5-dimethoxy-4-chloroamphetamine) | 0 | 0 | 0 | 4 | 0 | 5 | 2 | 2 | 4 | 1 | 3 | 2 | 2 | 25 |
| DOB (2,5-dimethoxy-4-bromoamphetamine) | 0 | 0 | 0 | 0 | 5 | 3 | 1 | 2 | 3 | 3 | 2 | 0 | 1 | 20 |
| DOx Total | 4 | 1 | 6 | 5 | 7 | 12 | 5 | 7 | 10 | 11 | 6 | 8 | 4 | 86 |
| NBOMe | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| 251-NBOMe (2C-l-NBOMe, BOM-CI, Cimbi-5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 23 | 22 | 26 | 20 | 15 | 114 |
| 25C-NBOMe (2C-C-NBOMe, NBOMe-2C-C) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 6 | 3 | 8 | 3 | 3 | 24 |
| 25B-NBOMe (NBOMe-2C-B) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 2 | 2 | 3 | 10 |
| NBOMe, otherwise unspecified | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 4 | 2 | 9 |
| 25D-NBOMe | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| NBOMe Total | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 30 | 27 | 39 | 29 | 24 | 158 |
| Other Phenethylamines | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| MDA (Methylenedioxyamphetamine) | 3 | 10 | 11 | 7 | 14 | 8 | 10 | 19 | 10 | 11 | 2 | 5 | 7 | 117 |
| PMA (Paramethoxyamphetamine) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| DMA (2, 5-Dimethoxyamphetamine) | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 2 | 0 | 0 | 0 | 6 |
| TMA (Trimethoxyamphetamine) | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| PMMA (Paramethoxymethamphetamine) | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 3C-Bromo-Dragonfly (DOB-Dragonfly) | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 1 | 1 | 2 | 0 | 8 |
| MDE (MDEA, 3,4-Methylenedioxy-N-Ethylamphetamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 | 5 |
| 4-FMA (4-Fluoromethamphetamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| 6-APB, Benzo Fury | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| 5-MAPB | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 |
| 6-MAPB | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 4-FA (4-Fluoroamphetamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| 5-APB | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| 3,4-Ethylenedioxy-N-methylamphetamine (EDMA, MDMC) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Other Phenethylamine Total | 5 | 12 | 12 | 7 | 17 | 8 | 11 | 19 | 16 | 16 | 4 | 10 | 16 | 153 |
| Phenethylamine Total | 39 | 53 | 60 | 58 | 90 | 127 | 141 | 150 | 203 | 175 | 165 | 141 | 140 | 1542 |
| Synthetic Cathinones | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| bk-MDMA (Methylone) | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 | 1 | 3 | 2 | 2 | 16 |
| MCAT (Mephedrone) | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 5 | 2 | 2 | 1 | 0 | 2 | 17 |
| Methedrone | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 |
| MDPV (Methylenedioxypyrovalerone) | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 2 | 1 | 2 | 1 | 0 | 11 |
| Bath salts, otherwise unspecified | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 11 | 10 | 6 | 11 | 1 | 4 | 44 |
| Cloud 10 Ultra | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| alpha-PVP (alpha-Pyrrolidinopentiophenone) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 |
| Beta-keto 2C-B (Bk-2C-B) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Synthetic Cathinones Total | 0 | 0 | 0 | 0 | 1 | 4 | 8 | 20 | 19 | 10 | 18 | 6 | 8 | 94 |
| Tryptamines | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| AMT (Alpha-methyltryptamine, IT-290, 3-IT) | 15 | 7 | 5 | 8 | 6 | 1 | 5 | 2 | 0 | 7 | 1 | 1 | 0 | 58 |
| Foxy | 3 | 3 | 3 | 1 | 2 | 3 | 2 | 2 | 2 | 0 | 0 | 1 | 0 | 22 |
| 5-MeO-DiPT (Foxy methoxy) | 3 | 2 | 1 | 4 | 0 | 3 | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 17 |
| 5-MeO-AMT | 3 | 1 | 4 | 1 | 4 | 2 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 20 |
| DiPT (Di-isopropyl-tryptamine) | 2 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| 5-MeO-DMT | 1 | 5 | 4 | 2 | 4 | 2 | 3 | 1 | 3 | 2 | 1 | 1 | 3 | 32 |
| DPT (Dipropyltryptamine) | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 6 |
| 5-MeO-T (5-methoxytryptamine) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 4-AcO-DMT (4-HO-DMT, 4-acetoxy-N,N-dimethyltryptamine) | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 3 | 2 | 9 | 5 | 3 | 27 |
| 5-MeO, otherwise unspecified | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 2 | 1 | 0 | 1 | 2 | 8 |
| 4-HO-DiP (4-HO-DiPT, 4-Hydroxy-N,N-diisopropyltryptamine) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| 4-Hydroxy-MIPT (4-HO-MiPT) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 |
| 4-HO-MET (N-Ethyl-4-hydroxy-N-methyltryptamine) | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 4 |
| 5-MeO-MiPT | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 1 | 1 | 4 |
| 4-MeO-DMT | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| 5-MeO-DALT (N,N-diallyl-5-methoxytryptamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| 4-HO-DET (CZ-74, Ethocin) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| 4-AcO-MET (4-Acetoxy-MET, Metacetin) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Synthetic mushrooms (unspecified) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Tryptamine Total | 28 | 21 | 19 | 17 | 20 | 15 | 14 | 8 | 15 | 15 | 15 | 14 | 13 | 214 |
| Synthetic Cannabinoids | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| Synthetic cannabinoids (e.g., K2, Spice, JWH-018) | 0 | 0 | 0 | 0 | 0 | 9 | 28 | 33 | 49 | 29 | 33 | 25 | 26 | 232 |
| CP 55,940 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Synthetic cannabis, otherwise unspecified | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 1 | 1 | 3 | 2 | 12 |
| AM-2201 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| Synthetic Cannabinoids Total | 0 | 0 | 0 | 0 | 0 | 10 | 28 | 38 | 51 | 30 | 34 | 28 | 28 | 247 |
| Lysergamides | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| LSA | 10 | 12 | 13 | 15 | 13 | 27 | 23 | 14 | 18 | 16 | 12 | 14 | 20 | 207 |
| ALD-52 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| LSZ (Lysergic acid 2,4-dimethylazetidide) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 3 |
| LAH (LSH, Lysergic acid hydroxyethylamide) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| AL-LAD (6-allyl-6-nor-LSD) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 |
| IP-LSD | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| Synthetic LSD/acid (unspecified) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Lysergamides Total | 10 | 12 | 13 | 15 | 13 | 28 | 23 | 15 | 19 | 17 | 15 | 16 | 22 | 218 |
| Dissociatives | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| 3-MeO-2-Oxo-PCE (MXE, Methoxetamine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 4 | 2 | 4 | 9 | 23 |
| Cl-400 (Eticyclidine, PCE) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 3-MeO-PCP (3-Methoxyphencyclidine) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Dissociative Total | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 4 | 2 | 5 | 9 | 25 |
| Piperazines | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
| BZP (Benzylpiperazine) | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 3 |
| Piperazines Total | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 3 |
| Total | 77 | 86 | 93 | 90 | 124 | 185 | 214 | 233 | 311 | 251 | 249 | 210 | 220 | 2343 |
Note. NSDUH staff classified typed-in responses into precoded response options for previously reported drugs and coded new responses for first reported drugs. The drug names listed above represent NSDUH classification–some of which contain full chemical names or street names and others do not. We did not make major edits to response options for transparency.
There were 94 mentions of synthetic cathinones (“bath salts”), with the first report of methylone occurring in 2009. Unspecified bath salts were almost half (46.8%) of these mentions. Tryptamines accounted for 9.1% of all mentions and contained a wide variety of compounds mentioned (n = 19). Synthetic cannabinoids made up 1/10 (10.5%) of mentions, although specific compounds were rarely mentioned. Lysergamides made up 9.3% of all mentions, and new dissociatives comprised 1.1%.
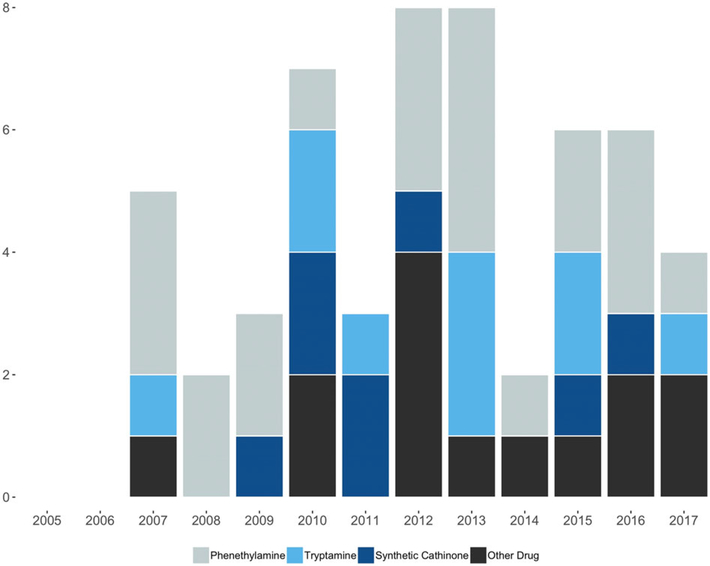
Figure 2 presents the number of first mentions from 2005 to 2017. There were no first mentions of new or uncommon drugs in 2005/2006. Mentions thereafter staggered but increased to eight in 2012 and in 2013 and then decreased in a staggered manner through 2017. Phenethylamines were the plurality of new drug mentions (40.7%, n = 22). Table 2 presents a list of the 54 first mentions in ascending order by year of first mention.
FIGURE 2.
Number of first mentions of new or uncommon drugs reported each year, 2005–2017
TABLE 2.
First mentions of new and uncommon drugs by Year (n = 54)
| Year | New or uncommon drug | Drug class |
|---|---|---|
| 2007 | 2C-T | Phenethylamine |
| 2007 | 4-AcO-DMT; 4-HO-DMT | Tryptamine |
| 2007 | BZP | Piperazine |
| 2007 | DOI | Phenethylamine |
| 2007 | PMMA | Phenethylamine |
| 2008 | 2C-T-21 | Phenethylamine |
| 2008 | DOC | Phenethylamine |
| 2009 | 3C-Bromo-Dragonfly | Phenethylamine |
| 2009 | bk-MDMA (Methylone) | Synthetic cathinone |
| 2009 | DOB | Phenethylamine |
| 2010 | 2C-BCB | Phenethylamine |
| 2010 | 4-HO-DiPT | Tryptamine |
| 2010 | 4-HO-MiPT | Tryptamine |
| 2010 | CP 55,940 | Synthetic cannabinoid |
| 2010 | MCAT (Mephedrone) | Synthetic cathinone |
| 2010 | Methedrone | Synthetic cathinone |
| 2010 | Synthetic cannabinoids | Synthetic cannabinoid |
| 2011 | 4-HO-MET | Tryptamine |
| 2011 | Bath salts, otherwise unspecified | Synthetic cathinone |
| 2011 | MDPV | Synthetic cathinone |
| 2012 | 25C-NBOMe | Phenethylamine |
| 2012 | 25I-NBOMe | Phenethylamine |
| 2012 | 2C-F | Phenethylamine |
| 2012 | 3-MeO-2-Oxo-PCE (MXE) | Dissociative |
| 2012 | AM-2201 | Synthetic cannabinoid |
| 2012 | CI-400 | Dissociative |
| 2012 | Cloud 10 Ultra | Synthetic cathinone |
| 2012 | Synthetic cannabis, otherwise unspecified | Synthetic cannabinoid |
| 2013 | 25B-NBOMe | Phenethylamine |
| 2013 | 2C-C | Phenethylamine |
| 2013 | 2C-P | Phenethylamine |
| 2013 | 4-FMA | Phenethylamine |
| 2013 | 4-MeO-DMT | Tryptamine |
| 2013 | 5-MeO-DALT | Tryptamine |
| 2013 | 5-MeO-MiPT | Tryptamine |
| 2013 | LSZ | Lysergamide |
| 2014 | LAH | Lysergamide |
| 2014 | 4-FA | Phenethylamine |
| 2015 | 4-AcO-MET | Tryptamine |
| 2015 | 4-HO-DET | Tryptamine |
| 2015 | 5-MAPB | Phenethylamine |
| 2015 | AL-LAD | Lysergamide |
| 2015 | alpha-PVP | Synthetic cathinone |
| 2015 | NBOMe, otherwise unspecified | Phenethylamine |
| 2016 | 1P-LSD | Lysergamide |
| 2016 | 2C-B-Fly | Phenethylamine |
| 2016 | 3-MeO-PCP | Dissociative |
| 2016 | 6-MAPB | Phenethylamine |
| 2016 | 6-APB, Benzo Fury | Phenethylamine |
| 2016 | Bk-2C-B | Synthetic cathinone |
| 2017 | 25D-NBOMe | Phenethylamine |
| 2017 | 5-APB | Phenethylamine |
| 2017 | Synthetic LSD/acid (unspecified) | Lysergamide |
| 2017 | Synthetic mushrooms (unspecified) | Tryptamine |
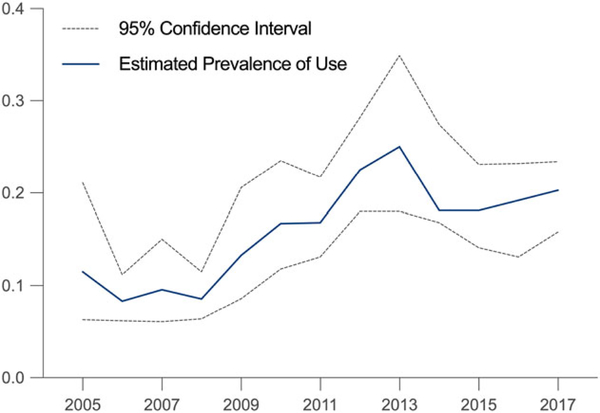
Finally, we examined trends in self-reported use of any new or uncommon drug examined in this study. We detected a significant upward trend in use between 2005 and 2017 (p < 0.001). More specifically, as shown in Figure 3, 0.12% reported use in 2005, and this steadily increased to 0.25% through 2013 before slightly decreasing in more recent years. Mentions of most drug classes were too rare to permit examining trends over time with confidence, but 2C-x and overall phenethylamine use demonstrated similar trends over time compared with the trend in use of any drug examined (Table SS1). It should be noted that a quarter of those reporting use of a new or uncommon drug reported using more than one. Specifically, 75.7% reported using one, but 16.5% reported using two; 4.7% reporting using three, and 3.1% reported using four-six.
FIGURE 3.
Estimated prevalence of use of any new or uncommon drug, 2005–2017
5 |. DISCUSSION
From an epidemiological perspective, data based on drug seizures and adverse outcomes resulting from use are largely limited by the fact that they may not capture the wide variety of drugs actually used among the general population. As such, we conducted the first study assessing self-reported use of various new or uncommon drugs based on type-in responses from multiple cohorts of individuals assessed through nationally representative surveys in the United States.
In general, our survey results show that a large majority of the NSDUH drug mentions were phenethylamines. 2C-x compounds, in particular, comprised the majority of phenethylamine mentions, driven primarily by mentions of 2C-B, 2C-E, and 2C-I. These trends are similar to those reported in several DEA National Forensic Laboratory Information System (NFLIS) reports, showing that the national number of 2C-x seizures sharply increased from 28 reports in 2006 to 1,530 in 2015, with a peak of 2,113 reports in 2013 (U.S. Drug Enforcement Administration Diversion Control Division, 2017; U.S. Drug Enforcement Administration Office of Diversion Control, 2013). The same patterns were reported in studies based on Poison Control Center data, which also noted that 2C-B, 2C-E, and 2C-I were the primary drivers of 2C-x exposures (Forrester, 2013; Forrester, 2014; Srisuma, Bronstein, & Hoyte, 2015). Whereas these three 2C-x subclasses also accounted for 90% of 2C-x NFLIS seizures in 2011, NBOMe compounds accounted for 91% of 2C-x-related seizures by 2015 (U.S. Drug Enforcement Administration Diversion Control Division, 2017). It should be noted that NFLIS categorizes NBOMe with 2C-x compounds, as NBOMe is a derivative of 2C, whereas our NSDUH study presents these as separate subclasses. We did observe that the number of NSDUH mentions of NBOMe, which was first noted in 2012, increased thereafter. The first NBOMe seizures, as per NFLIS, were reported in 2011 (U.S. Drug Enforcement Administration Diversion Control Division, 2017).
With regard to tryptamine use, NSDUH and NFLIS tryptamine trends were somewhat similar for more recent years but differed in years prior to 2010. For example, our findings demonstrate that tryptamine mentions appear to trend downwards between 2005 and 2012 and then remain steady at slightly higher levels between 2013 and 2016. By comparison, NFLIS data show that total tryptamine seizures spiked upwards from 42 reports in 2005 to 4,046 in 2011 but then decreased in 2012 before remaining steady at approximately 1,000 reports between 2013 and 2015. It should be noted that DMT was the most commonly seized tryptamine by a large margin between 2006 and 2010, and the second most seized tryptamine between 2011 and 2015, but we had to exclude DMT in our analyses. Nonetheless, the overall trends are similar.
Synthetic cannabinoids and synthetic cathinones represent two of the more prevalent groups of NPS used in the United States (Miech et al., 2018), and the majority of NPS discovered each year tend to fall into one of these classes (European Monitoring Centre for Drugs and Drug Addiction, 2018). Mentions of drugs in these classes were rare relative to phenethylamine mentions. Specifically, the results showed that the first mentions were in 2010, with a peak in 2013. This trend is comparable with that based on NFLIS reports, which found that the first synthetic cannabinoid seizures occurred in 2009 (15 reports), with numbers spiking upwards thereafter and peaking in 2014 at approximately 33,000 reports before dipping slightly in 2015 to just under 30,000 reports (U.S. Drug Enforcement Administration Diversion Control Division, 2011; U.S. Drug Enforcement Administration Diversion Control Division, 2014). As it pertains to synthetic cathinones, we observed an increase in mentions from 2009 to 2012 and then a decrease. The number of National Poison Control Center cases has similarly trended downwards between 2011 and 2016 (American Association of Poison Control Centers, 2016), although the number of NFLIS reports during a similar period has trended upwards (from 142 reports in 2010 to 19,490 in 2015; U.S. Drug Enforcement Administration Diversion Control Division, 2011, 2014).
It should be noted that there were no reports of use of novel opioids via the type-in response option on this survey. There were some type-in reports of fentanyl use over the years, but these responses were listed as “Actiq, Fentanyl, Duragesic, Sublimaze”, so we could not determine whether use was of synthetic, illicitly manufactured fentanyl, or misuse of prescriptions. NSDUH has also started specifically querying fentanyl use in recent years. No other novel opioids or fentanyl analogs were typed-in by participants. There have been tens of thousands of deaths related to exposure to these compounds in the United States in recent years (Jones, Einstein, & Compton, 2018), so we believe use was underreported. Underreporting may be due, in part, to the fact that exposure to or misuse of fentanyl, its analogs, and/or other opioid NPS is often unknown, given that they are common adulterants in drugs such as heroin.
The apparent underreporting of use of NPS such as synthetic cannabinoids, synthetic cathinones, and novel opioids demonstrates that type-in responses must be considered with caution (Kroutil, Vorburger, Aldworth, & Colliver, 2010; Palamar, Martins, Su, & Ompad, 2015). It is unknown why drugs such as 2C are more commonly typed in when compared with more prevalent new or uncommon drugs, though one potential explanation is that many such drugs were still legal at the time of survey administration. Consequently, these drugs may not have instinctively come to mind while participants were completing the survey. In similar fashion, when prompted to type in names of other hallucinogens, stimulants, or inhalants, and about drugs ever injected, synthetic cannabinoids, in particular, may not have been considered because they lack salient characteristics that fit in any of these categories. Inclusion of questions about “other” drugs smoked might have led to increased reporting of use of synthetic cannabinoids. Also, drug class names were more commonly typed in for these two classes as opposed to specific compound names. There are now hundreds of synthetic cannabinoid compounds in circulation (European Monitoring Centre for Drugs and Drug Addiction, 2018; U.S. Drug Enforcement Administration, 2018), and mixtures of these compounds, which are often mislabelled (Zamengo, Frison, Bettin, & Sciarrone, 2014), are most often sold in the United States in packages under names such as Spice and K2. Thus, the popularization of these drugs, coupled with ever-shifting mixtures of components, makes it difficult for users to become aware of the specific compounds they are using. Instead, these drugs are often simply grouped together as “synthetic marijuana” or “Spice” drugs. A somewhat similar situation occurred regarding “bath salts,” but it appears more common for users to be aware of which compound(s) they are using.
Despite biases with regard to type-in responses on surveys, we believe such information can assist epidemiologists in detecting emergence and patterns of use of new and uncommon drugs. We also believe reporting on Poison Control and other adverse-event-based data could be improved as it relates to exposure to new or uncommon drugs. Annual national Poison Control Center reports, for example, do not list many specific compounds and simply classify numerous stimulants as “hallucinogenic amphetamines” (Gummin et al., 2017). Similarly, stimulant drug-related deaths reported by the Centers for Disease Control and Prevention are collapsed into a “psychostimulant” category (Seth, Scholl, Rudd, & Bacon, 2018). Collection and/or reporting of data on adverse effects of specific new or uncommon drugs in such systems could improve public health response.
In the grander scheme, there is also a need for the collection and analysis of data on use of new and uncommon drugs that are not dependent on an adverse outcomes or confiscation. Social media platforms and websites where “psychonauts” report on effects of use of various NPS have been put forth as important sources of information (Deluca et al., 2012), but purposive targeting of psychonauts may not yield data generalizable to the overall population. Surveys administered systematically to the overall population would provide more generalizable information, although as reported in this study, use of most new or uncommon drugs would be rare. An alternative scheme potentially worth consideration could be the systematic administration of surveys to “at-risk” populations. For example, electronic dance music nightclub/party attendees have consistently been shown to report high prevalence of use of new and/or uncommon drugs (Palamar, Acosta, Sherman, Ompad, & Cleland, 2016; Palamar, Barratt, Ferris, & Winstock, 2016). Understanding prevalence obtained through such surveys may help us better understand diffusion of such drugs throughout the general population.
6 |. LIMITATIONS
NSDUH only surveyed individuals living in households, noninstitutionalized group quarters (e.g., dormitories and shelters), and civilians residing at military bases. Homeless individuals (who do not use shelters), military personnel on active duty, and residents of institutional group quarters, such as hospitals and jails, were not surveyed by NSDUH, which can limit generalizability. The change in survey design in 2015, which dropped open-ended questions about use of “other” stimulants, sedatives, or analgesics, could have also affected responses; however, almost all (99.2%; 1651 of 1664) responses in previous years were typed into the categories that remained, giving us confidence that the change in questions did not likely have a large impact on reporting. The lack of a question querying use of “any type of drug not asked about” is another limitation. In addition, these open-ended questions queried ever use, so recency of use cannot be determined.
Type-in responses are limited because not providing questions about specific drugs tends to lead to severe underreporting (Kroutil et al., 2010; Palamar, Martins, et al., 2015). We believe substantial underreporting occurred not only because respondents were not specifically asked about these dozens of drugs but also because many individuals are simply unaware what drugs they have used. Use of “mystery” (unknown) pills and powders, for example, is common (Palamar, Acosta, et al., 2016), and moreover, consumption of adulterants present in common drugs is prevalent. For example, various studies suggest drugs like ecstasy commonly contain synthetic cathinones (bath salts), whereas drugs said to be LSD have been found to be NBOMe (Brunt et al., 2016; Martins et al., 2017; Palamar, Salomone, Vincenti, & Cleland, 2016). Many respondents also reported use of drug classes but not specific compounds within the class. For example, it is unknown which synthetic cathinone or synthetic cannabinoid users of bath salts or Spice drugs actually used. However, we also classified specific drugs into categories so lack if specific drug compound name was not a major limitation in most cases.
7 |. CONCLUSION
Given the limitations of seizure data and data on adverse events related to drug use, we believe surveys can add to our understanding of emergence and patterns of use of new and uncommon drugs. Indeed, type-in responses on surveys tend to lead to biased estimates of use, but data on use that did not necessarily result in adverse outcomes are needed nonetheless. Monitoring the extent of use of new or emerging drugs can guide public health efforts, particularly those targeting synthetic cannabinoids and synthetic cathinones—two of the most commonly used classes of NPS associated with tens of thousands of poisonings in the United States as evidenced by survey, Poison Control, and emergency department data. Even though prevalence of use of synthetic cannabinoids and synthetic cathinones has decreased in recent years (Kann et al., 2018; Miech et al., 2018; Oliver et al., 2018), these compounds continue to emerge at an alarming rate (European Monitoring Centre for Drugs and Drug Addiction, 2018). Moreover, some of these compounds are highly potent and dangerous (Dalton, Wang, & Zavitsanou, 2009; Watterson & Olive, 2017), leaving users at risk for dependence or other serious adverse outcomes.
It is important to note that synthetic cannabinioids and synthetic cathinones were less commonly mentioned in our study than 2C-x. We believe we are the first to examine 2C-x use on a repeated national survey and have determined that use of these compounds has increased in popularity despite having remained relatively unrecognized by epidemiologists. More research is needed to determine the extent to which use of 2C-x and related compounds leads to adverse effects and need for treatment in order to gauge potential impact on public health. We also detected increasing use of NBOMe, a class that includes compounds known to be particularly dangerous, especially when ingested unknowingly (e.g., in purported LSD). Finally, we detected use of other drug classes that carry less capacity for harm, such as tryptamines and lysergamides (Gable, 2004; Nutt, King, & Phillips, 2010). Despite a lower public health impact, health care professionals may still benefit from knowing that these drugs are used at an appreciable rate in the event of adverse outcomes arising from use.
Ultimately, different drug classes (or compounds within specific classes) are associated with differing degrees of danger and may each require a different degree of public health attention. Nevertheless, continued research is needed on all drug classes examined in this paper. Although the epidemiology of NPS use is only in its infancy, there is an abundance of literature (e.g., case studies) regarding adverse effects (and their treatment) of many of the compounds examined here. Although small case studies do have value, any preventative or harm reduction measures targeting such compounds require more systematic research and surveillance.
Supplementary Material
ACKNOWLEDGMENT
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Numbers K01DA038800 and R01DA044207 (PI: Palamar). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding information
National Institute on Drug Abuse, Grant/Award Numbers: K01DA038800 and R01DA044207
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of the article.
REFERENCES
- American Association of Poison Control Centers. (2016). AAPCC—Bath salts data. Alexandria, VA: https://aapcc.s3.amazonaws.com/files/library/Bath_Salts_Web_Data_through_11.2016.pdf. [Google Scholar]
- Berquist MD, Hyatt WS, Bauer-Erickson J, Gannon BM, Norwood AP, & Fantegrossi WE (2018). Phencyclidine-like in vivo effects of methoxetamine in mice and rats. Neuropharmacology, 134(Pt A), 158–166. 10.1016/j.neuropharm.2017.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt SD, Kavanagh PV, Westphal F, Elliott SP, Wallach J, Colestock T, … Halberstadt AL (2017a). Return of the lysergamides. Part II: Analytical and behavioural characterization of N(6) -allyl-6-norlysergic acid diethylamide (AL-LAD) and (2′S,4′S)-lysergic acid 2,4-dimethylazetidide (LSZ). Drug Testing and Analysis, 9(1), 38–50. 10.1002/dta.1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt SD, Kavanagh PV, Westphal F, Elliott SP, Wallach J, Stratford A, … Halberstadt AL (2017b). Return of the lysergamides. Part III: Analytical characterization of N(6) -ethyl-6-norlysergic acid diethylamide (ETH-LAD) and 1-propionyl ETH-LAD (1P-ETH-LAD). Drug Testing and Analysis, 9(10), 1641–1649. 10.1002/dta.2196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt SD, Kavanagh PV, Westphal F, Stratford A, Elliott SP, Hoang K, … Halberstadt AL (2016). Return of the lysergamides. Part I: Analytical and behavioural characterization of 1-propionyl-d-lysergic acid diethylamide (1P-LSD). Drug Testing and Analysis, 8(9), 891–902. 10.1002/dta.1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunt TM, Nagy C, Bucheli A, Martins D, Ugarte M, Beduwe C, & Ventura VM (2016). Drug testing in Europe: Monitoring results of the Trans European Drug Information (TEDI) Project. Drug Testing and Analysis, 9, 188–198. 10.1002/dta.1954 [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (2015). 2016 National Survey on drug use and health (NSDUH): CAI specifications for programming. Rockville, MD: Substance Abuse and Mental Health Services Administration; https://www.samhsa.gov/data/sites/default/files/NSDUHmrbCAIquex2016.pdf [Google Scholar]
- Cordeiro SK, Daro RC, Seung H, Klein-Schwartz W, & Kim HK (2018). Evolution of clinical characteristics and outcomes of synthetic cannabinoid receptor agonist exposure in the United States: Analysis of National Poison Data System data from 2010 to 2015. Addiction, 113(10), 1850–1861. 10.1111/add.14281 [DOI] [PubMed] [Google Scholar]
- Dalton VS, Wang H, & Zavitsanou K (2009). HU210-induced downregulation in cannabinoid CB1 receptor binding strongly correlates with body weight loss in the adult rat. Neurochemical Research, 34(7), 1343–1353. 10.1007/s11064-009-9914-y [DOI] [PubMed] [Google Scholar]
- De Paoli G, Brandt SD, Wallach J, Archer RP, & Pounder DJ (2013). From the street to the laboratory: Analytical profiles of methoxetamine, 3-methoxyeticyclidine and 3-methoxyphencyclidine and their determination in three biological matrices. Journal of Analytical Toxicology, 37(5), 277–283. 10.1093/jat/bkt023 [DOI] [PubMed] [Google Scholar]
- Deluca P, Davey Z, Corazza O, Di Furia L, Farre M, Flesland LH, … Schifano F (2012). Identifying emerging trends in recreational drug use; outcomes from the Psychonaut Web Mapping Project. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 39(2), 221–226. 10.1016/j.pnpbp.2012.07.011 [DOI] [PubMed] [Google Scholar]
- Deng H, Verrico CD, Kosten TR, & Nielsen DA (2018). Psychosis and synthetic cannabinoids. Psychiatry Research, 268, 400–412. 10.1016/j.psychres.2018.08.012 [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction (2017). High-risk drug use and new psychoactive substances. Luxembourg: EMCDDA Rapid Communication, Publications Office of the European Union; http://www.emcdda.europa.eu/publications/rapid-communications/high-risk-drug-use-and-nps_en [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. (2018). European Drug Report 2018. http://www.emcdda.europa.eu/publications/edr/trends-developments/2018.
- Forrester MB (2013). 2C series phenethylamine derivative exposures in Texas. Substance Abuse, 34(1), 81–82. 10.1080/08897077.2012.715623 [DOI] [PubMed] [Google Scholar]
- Forrester MB (2014). NBOMe designer drug exposures reported to Texas poison centers. Journal of Addictive Diseases, 33(3), 196–201. 10.1080/10550887.2014.950027 [DOI] [PubMed] [Google Scholar]
- Gable RS (2004). Comparison of acute lethal toxicity of commonly abused psychoactive substances. Addiction, 99(6), 686–696. 10.1111/j.1360-0443.2004.00744.x [DOI] [PubMed] [Google Scholar]
- Glennon RA, Dukat M, Grella B, Hong SS, Costantino L, Teitler M, … Mattson MV (2000). Binding of beta-carbolines and related agents at serotonin (5-HT(2) and 5-HT(1A)), dopamine (D(2)) and benzodiazepine receptors. Drug and Alcohol Dependence, 60(2), 121–132. 10.1016/S0376-8716(99)00148-9 [DOI] [PubMed] [Google Scholar]
- Greene SL (2013). Benzofurans and benzodifurans In Dargan PI, & Wood DM (Eds.), Novel psychoactive substances classification, pharmacology and toxicology (pp. 383–392). Cambridge, MA: Academic Press; 10.1016/B978-0-12-415816-0.00016-X [DOI] [Google Scholar]
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, & Banner W (2017). 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clinical Toxicology (Philadelphia, Pa.), 55(10), 1072–1252. 10.1080/15563650.2017.1388087 [DOI] [PubMed] [Google Scholar]
- Heeringa S, West BT, & Berglund PA (2010). Applied survey data analysis. Boca Raton, FL: Chapman & Hall/CRC; 10.1201/9781420080674 [DOI] [Google Scholar]
- Herrmann E, Johnson P, Johnson M, & Vandrey R (2016). Novel Drugs of Abuse: Cannabinoids, stimulants, and hallucinogens In Preedy V (Ed.), Neuropathology of drug addictions and substance misuse Volume 1: Foundations of understanding, tobacco, alcohol, cannabinoids and opioids. Cambridge, MA: Academic Press. [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, & Schulenberg JE (2018). Monitoring the future national survey results on drug use: 1975–2017: Overview, key findings on adolescent drug use. Ann Arbor: The University of Michigan Institute for Social Research; Retrieved from Ann Arbor: http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2017.pdf [Google Scholar]
- Jones CM, Einstein EB, & Compton WM (2018). Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA, 319(17), 1819–1821. 10.1001/jama.2018.2844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, … Ethier KA (2018). Youth Risk Behavior Surveillance—United States, 2017. MMWR Surveillance Summaries, 67(8), 1–114. 10.15585/mmwr.ss6708a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, Nutt DJ, & Independent Scientific Committee on Drugs. (2014). Deaths from “legal highs”: A problem of definitions. Lancet, 383(9921), 952 10.1016/S0140-6736(14)60479-7 [DOI] [PubMed] [Google Scholar]
- Klinke HB, Muller IB, Steffenrud S, & Dahl-Sørensen R (2010). Two cases of lysergamide intoxication by ingestion of seeds from Hawaiian Baby Woodrose. Forensic Science Intenational, 197(1–3), e1–e5. 10.1016/j.forsciint.2009.11.017 [DOI] [PubMed] [Google Scholar]
- Kroutil LA, Vorburger M, Aldworth J, & Colliver JD (2010). Estimated drug use based on direct questioning and open-ended questions: responses in the 2006 National Survey on Drug Use and Health. International Journal of Methods in Psychiatric Research, 19(2), 74–87. 10.1002/mpr.302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins D, Barratt MJ, Pires CV, Carvalho H, Vilamala MV, Espinosa IF, & Valente H (2017). The detection and prevention of unintentional consumption of DOx and 25x-NBOMe at Portugal’s Boom Festival. Human Psychopharmacology, 32(3). 10.1002/hup.2608 [DOI] [PubMed] [Google Scholar]
- McGraw M, & McGraw L (2012). Bath salts: Not as harmless as they sound. Journal of Emergency Nursing, 38(6), 582–588. 10.1016/j.jen.2012.07.025 [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the future national survey results on drug use, 1975–2017: Volume I, Secondary school students. University of Michigan. Ann Arbor: Institute for Social Research; http://www.monitoringthefuture.org/pubs/monographs/mtf-vol1_2017.pdf. 10.3998/2027.42/146530 [DOI] [Google Scholar]
- Nutt DJ, King LA, & Phillips LD (2010). Drug harms in the UK: A multicriteria decision analysis. Lancet, 376(9752), 1558–1565. 10.1016/s0140-6736(10)61462-6 [DOI] [PubMed] [Google Scholar]
- Oliver CF, Palamar JJ, Salomone A, Simmons SJ, Philogene-Khalid HL, Stokes-McCloskey N, & Rawls SM (2018). Synthetic cathinone adulteration of illegal drugs. Psychopharmacology. 10.1007/s00213-018-5066-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Acosta P, Sherman S, Ompad DC, & Cleland CM (2016). Self-reported use of novel psychoactive substances among attendees of electronic dance music venues. The American Journal of Drug and Alcohol Abuse, 42(6), 624–632. 10.1080/00952990.2016.1181179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Barratt MJ, Ferris JA, & Winstock AR (2016). Correlates of new psychoactive substance use among a self-selected sample of nightclub attendees in the United States. The American Journal on Addictions, 25(5), 400–407. 10.1111/ajad.12403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Martins SS, Su MK, & Ompad DC (2015). Self-reported use of novel psychoactive substances in a US nationally representative survey: Prevalence, correlates, and a call for new survey methods to prevent underreporting. Drug and Alcohol Dependence, 156, 112–119. 10.1016/j.drugalcdep.2015.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Salomone A, Vincenti M, & Cleland CM (2016). Detection of “bath salts” and other novel psychoactive substances in hair samples of ecstasy/MDMA/”Molly” users. Drug and Alcohol Dependence, 161, 200–205. 10.1016/j.drugalcdep.2016.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Su MK, & Hoffman RS (2016). Characteristics of novel psychoactive substance Exposures Reported to New York City Poison Center, 2011–2014. The American Journal of Drug and Alcohol Abuse, 42(1), 39–47. 10.3109/00952990.2015.1106551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power JD, Kavanagh P, O’Brien J, Barry M, Twamley B, Talbot B, … Brandt SD (2015). Test purchase, identification and synthesis of 2-amino-1-(4-bromo-2, 5-dimethoxyphenyl)ethan-1-one (bk-2C-B). Drug Testing and Analysis, 7(6), 512–518. 10.1002/dta.1699 [DOI] [PubMed] [Google Scholar]
- Prosser JM, & Nelson LS (2012). The toxicology of bath salts: A review of synthetic cathinones. Journal of Medical Toxicology, 8(1), 33–42. 10.1007/s13181-011-0193-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Scholl L, Rudd RA, & Bacon S (2018). Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morbidity and Mortality Weekly Report, 67(12), 349–358. 10.15585/mmwr.mm6712a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shulgin A, & Shulgin A (1991). Phenethylamines I have known and loved (PiHKAL). Berkley, CA: Transform Press. [Google Scholar]
- Shulgin A, & Shulgin A (1997). Tryptamines I have known and loved (TiHKAL) (1st ed.). Berkley, CA: Transform Press. [Google Scholar]
- Slavova S, Costich JF, Bunn TL, Luu H, Singleton M, Hargrove SL, … Ingram V (2017). Heroin and fentanyl overdoses in Kentucky: Epidemiology and surveillance. The International Journal on Drug Policy, 46, 120–129. 10.1016/j.drugpo.2017.05.051 [DOI] [PubMed] [Google Scholar]
- Srisuma S, Bronstein AC, & Hoyte CO (2015). NBOMe and 2C substitute phenylethylamine exposures reported to the National Poison Data System. Clinical Toxicology (Philadelphia, Pa.), 53(7), 624–628. 10.3109/15563650.2015.1054502 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on drug use and health. Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.pdf [Google Scholar]
- U.S. Drug Enforcement Administration. (2017). 2016 Emerging Threat Report. https://ndews.umd.edu/sites/ndews.umd.edu/files/emerging-threat-report-2016-annual.pdf.
- U.S. Drug Enforcement Administration. (2018). 2017 Emerging Threat Report. https://ndews.umd.edu/sites/ndews.umd.edu/files/deaemerging-threat-report-2017-annual.pdf.
- U.S. Drug Enforcement Administration Diversion Control Division. (2011). National forensic laboratory information system special report: Synthetic cannabinoids and synthetic Cathinones reported in NFLIS, 2009–2011. VA: Springfield; https://www.nflis.deadiversion.usdoj.gov/Reports.aspx [Google Scholar]
- U.S. Drug Enforcement Administration Diversion Control Division. (2014). National forensic laboratory information system special report: Synthetic cannabinoids and synthetic Cathinones reported in NFLIS, 2010–2013. VA: Springfield; https://www.nflis.deadiversion.usdoj.gov/Reports.aspx [Google Scholar]
- U.S. Drug Enforcement Administration Diversion Control Division. (2017). National forensic laboratory information system special report: 2C-phenethylamines, Piperazines, and Trypatmines reported in NFLIS, 2011–2015. VA: Springfield; https://www.nflis.deadiversion.usdo).gov/Reports.aspx [Google Scholar]
- U.S. Drug Enforcement Administration Office of Diversion Control. (2013). National forensic laboratory information system special report: Emerging 2C-phenethylamines, Piperazines, and tryptamines in NFLIS, 2006–2011. VA: Springfield; https://www.nflis.deadiversion.usdoj.gov/Reports.aspx [Google Scholar]
- van Hout MC, & Hearne E (2017). New psychoactive substances (NPS) on cryptomarket for: An exploratory study of characteristics of forum activity between NPS buyers and vendors. International Journal of Drug Policy, 40, 102–110. 10.1016/j.drugpo.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Warrick BJ, Hill M, Hekman K, Christensen R, Goetz R, Casavant MJ, … Smolinske S (2013). A 9-state analysis of designer stimulant, “bath salt,” hospital visits reported to poison control centers. Annals of Emergency Medicine, 62(3), 244–251. 10.1016/j.annemergmed.2012.12.017 [DOI] [PubMed] [Google Scholar]
- Watterson LR, & Olive MF (2017). Reinforcing effects of cathinone NPS in the intravenous drug self-administration paradigm. Current Topics in Behavioral Neurosciences, 32, 133–143. 10.1007/7854_2016_33 [DOI] [PubMed] [Google Scholar]
- Yu B, Becnel J, Zerfaoui M, Rohatgi R, Boulares AH, & Nichols CD (2008). Serotonin 5-hydroxytryptamine(2A) receptor activation suppresses tumor necrosis factor-alpha-induced inflammation with extraordinary potency. Journal of Pharmacology and Experimental Therapeutics, 327(2), 316–323. 10.1124/jpet.108.143461 [DOI] [PubMed] [Google Scholar]
- Zamengo L, Frison G, Bettin C, & Sciarrone R (2014). Understanding the risks associated with the use of new psychoactive substances (NPS): High variability of active ingredients concentration, mislabelled preparations, multiple psychoactive substances in single products. Toxicology Letters, 229(1), 220–228. 10.1016/j.toxlet.2014.06.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.