Abstract
Objective:
To determine whether prenatal social support was associated with infant adiposity in the first 18 months of life in a low-income, Hispanic sample, known to be at high risk of early child obesity.
Study design:
We performed a longitudinal analysis of 262 low-income, Hispanic mother-infant pairs in the control group of the “Starting Early” child obesity prevention trial. Prenatal social support was measured using an item from the Maternal Social Support Index. We used multilevel modeling to predict weight-for-length z-score (WFLz) trajectories from birth to age 18 months and logistic regression to predict macrosomia and overweight status at ages 6, 12, and 18 months.
Results:
High prenatal social support was independently associated with lower infant adiposity trajectories from birth to age 18 months (B=−0.40 (−0.63, −0.16)), lower odds of macrosomia (aOR 0.35 (0.15, 0.80)), and lower odds of overweight at ages 12 (0.28 (0.10, 0.74)) and 18 months (0.35 (0.14, 0.89)). Prenatal social support was not significantly associated with overweight status at age 6 months.
Conclusions:
Prenatal social support may protect against excessive infant adiposity and overweight in low-income, Hispanic families. Further research is needed to elucidate mechanisms underlying these associations and to inform preventive strategies beginning in pregnancy.
Keywords: Childhood obesity, Obesity prevention, Infancy, Hispanic, Pregnancy
Despite decades of preventive efforts across the United States (US), the prevalence of early child obesity remains alarmingly high,1 particularly in low-income, Hispanic families.2,3 For many children, the onset of obesity occurs well before school entry, and socioeconomic and ethnic disparities in adiposity begin in infancy and persist over time.4 This underscores the importance of early childhood as a critical period in which growth trajectories are established and rapid increases in infant adiposity are noted.5 Numerous risk factors for excessive infant adiposity are identifiable in pregnancy, including maternal socio-demographics (e.g., educational attainment), psychosocial factors (eg, depression and stress) and weight and health-related factors (e.g., maternal obesity, excessive gestational weight gain, gestational diabetes mellitus). Although risk factors for early child obesity have been studied extensively, there has been minimal investigation of resilience factors that are protective against the development of obesity in children with risk exposure.6
Resilience, a construct originating from the field of developmental psychology, refers to the ability to make positive adaptations in response to adversity by utilizing personal, social, and environmental resources.7 Social support, the degree to which one’s needs are satisfied through social relationships, is a component of resilience that has long been known to lead to positive health outcomes.8–10 There is emerging evidence that within low-income communities, adults with more social support have a lower prevalence of obesity.11,12 Additionally, a large body of evidence documents that social support during pregnancy has positive impacts on aspects of maternal and child health known to improve subsequent child weight outcomes, including prenatal nutrition,13 maternal depression,14 birth weight,15 infant feeding,16 and parenting.17 Despite extensive evidence for the role of social support in promoting healthy outcomes generally and in reducing risks related to obesity, there has been limited study of its direct associations with child weight. Cross-sectional studies have suggested that parents’ receipt of social support may be associated with favorable weight outcomes in their children.18–20 However, there have been no longitudinal studies of these relations, limiting the ability to make causal inferences. Therefore, we sought to determine whether prenatal social support was associated with infant adiposity in the first 18 months of life in a low-income, Hispanic sample, known to be at high risk of early child obesity. We hypothesized that high prenatal social support would be associated with lower mean adiposity trajectory and lower prevalence of overweight status in the first 18 months of life.
Methods
We performed a longitudinal cohort analysis examining associations between prenatal social support and infant adiposity from birth to age 18 months. This analysis utilized the control group of a randomized controlled trial (RCT) of the Starting Early Program. Starting Early is a primary-care based child obesity prevention program designed for low-income, Hispanic families, beginning in the third trimester of pregnancy. Participants randomized to the intervention receive individual prenatal and postpartum nutrition and lactation counseling, followed by Nutrition and Parenting Support Groups with a focus on age-appropriate feeding, play, and parenting throughout the first 3 years of life.21 Participants randomized to the control group receive standard prenatal and pediatric primary care. Standard care consists of approximately 8 to 10 prenatal visits during the 3rd trimester, and 9 pediatric visits in the first 18 months of life. Because the intervention is delivered in an environment designed to be supportive, the current analysis is limited to the control group of the RCT. Data for the current analyses were collected between July 2012 and September 2016. The RCT was approved by the institutional review board of New York University School of Medicine and New York City Health and Hospitals and registered on clinicaltrials.gov (NCT01541761).
Sample
Recruitment for Starting Early was conducted in the prenatal and pediatric primary care clinics of a large urban public hospital network. We included women who were at least 18 years old, self-identified as Hispanic, were fluent in English or Spanish, and who had a singleton, uncomplicated pregnancy and intended to receive pediatric care at the study sites. We excluded women with significant medical or psychiatric illness, homelessness, substance abuse, or severe fetal anomalies on ultrasound examination. Women with mild or moderate complications, such as diabetes, depression, or intrauterine growth restriction were not excluded. All infants included in the study were born at ≥34 weeks of estimated gestational age (EGA) as per obstetrics clinical documentation during the delivery hospital admission. Obstetrics providers determined EGA by last menstrual period or first trimester ultrasound, as appropriate for each woman. The analytic sample for the current study included all participants randomized to the control group of the larger RCT who completed the baseline measure of prenatal social support and had at least one set of paired infant anthropometric measures (length and weight) in the first 18 months of life.
Measures
Dependent variables
All anthropometric data for infant subjects were obtained by medical record review of the birth hospitalization and subsequent well child visits. We generated weight-for-length z-scores (WFLz) for each infant at birth and each well child visit using the World Health Organization (WHO) Anthro macro.22 Anthropometric data flagged by the Anthro macro22 as potentially implausible were manually reviewed by authors MK and MM and kept if deemed plausible within the context of other growth data in the child’s medical record and clinical documentation by the provider.23–25 If these data were inconsistent with other growth data in the medical record or if there were no other data in the record with which to compare, they were removed and coded as missing. We used WFLz over time as our first main outcome. WFLz is frequently used as a measure of adiposity in infants, and can be interpreted as degree of adiposity relative to a large, multinational and multiethnic sample of infants growing in optimal environmental conditions. Ideal and proportional growth for a healthy infant would be represented by WFLz that remains stable and within two standard deviations of the median throughout the first 2 years of life. Our second set of main outcomes was categorical weight status at four time points (birth, 6 months, 12 months, and 18 months of age), based on WHO definitions and reference standards: macrosomia was defined as birth weight ≥4 kilograms and overweight at 6, 12, and 18 months of age was defined as WFLz >2.22 Anthropometric measurements used to determine categorical weight status at the 6, 12, and 18 month time points were taken from the medical record of a well child visit within 45 days of the given date. In cases with multiple measurements within the designated 90-day window, the measurement closest in time to the 6, 12, or 18 month birthday was used, respectively. Infants were excluded from the age specific analysis if they did not have anthropometric data available within the specified 90-day window of the given age.
Independent variables
Prenatal social support, socio-demographic and psychosocial factors were collected during an in-person baseline survey administered by trained, bilingual research assistants during the third trimester of pregnancy.
Primary predictor
Prenatal social support was assessed using an item from the Maternal Social Support Index (MSSI),26 which asks, “How many people can you count on in times of need?” and allows numerical responses. It does not ask for further specification of who provides support, such as a family member, friend, or spouse. This item of the MSSI has been shown to be independently associated with maternal depression26 and parenting stress27 in prior studies. This item reflects perceived availability of social support, a subconstruct of social support that has stronger ties to positive health outcomes than measures of actual or received support.9 We visually examined the frequency distribution of responses to this item, which revealed a non-normal distribution and right skew. Exploratory analyses demonstrated that the relation between the number of people to count on and infant adiposity was non-linear with minimal added effect on the outcome as the number of people to count on increased beyond the lowest quartile of the distribution (0 or 1 person to count on). Dichotomizing the predictor at the lowest quartile resulted in multilevel and logistic regression models with lower values for the Akaike information criterion (AIC)28 than models utilizing other cut points for the predictor (quintiles, quartiles, median split). This confirmed that the best model fit was achieved when the predictor was dichotomized at the lowest quartile. Based on these results and prior literature utilizing the same dichotomization,29–33 we classified women with 0 or 1 person to count on in times of need as having low prenatal social support and those with ≥2 people to count on in times of need as having high prenatal social support.
Socio-demographic factors
Socio-demographic factors, including maternal age, nativity (US born versus foreign born), education level (less than high school versus high school graduate), and marital status (married or living with partner versus other) were collected during the prenatal assessment.
Psychosocial factors
Prenatal household food insecurity was measured by the Core Food Security Module from the US Department of Agriculture (USDA).34 Families were classified as “food secure” if they reported fewer than 3 food-insecure conditions and as “food insecure” if they reported 3 or more as recommended by the USDA. Depressive symptoms were measured prenatally using the Patient Health Questionnaire-9 and defined as present if the score was 5 or above.35
Maternal health and weight-related factors
Maternal pre-pregnancy height and weight were collected from medical record review from the earliest first trimester prenatal visit. Maternal pre-pregnancy BMI was calculated using the formula BMI=kg/m2 and subjects were classified as having pre-pregnancy overweight or obesity if their BMI was 25 or above.36 Gestational weight gain (GWG) was calculated by subtracting pre-pregnancy weight from weight recorded when the participant was admitted for delivery. GWG was categorized as inadequate, adequate, or excessive according to the Institute of Medicine definitions.37 Gestational diabetes was determined by medical record review of prenatal visits and 2-hour oral glucose tolerance test results.38
Statistical analyses
We used descriptive statistics to characterize the sample and frequency distributions of key study variables. We used χ2 and t-tests to examine bivariate associations between maternal socio-demographic, psychosocial, and health/weight-related factors and prenatal social support. Maternal characteristics associated with prenatal social support (P < .20) were included in subsequent multivariable models. Relations between maternal characteristics and WFLz trajectory were examined using multilevel modeling, and excessive GWG was the only variable with p<0.20 that had not already been selected for inclusion in multivariable models based upon association with the predictor in the previous set of analyses. Because gestational weight gain reflects a dynamic process and theoretically may be a mechanism by which prenatal social support could influence infant birth weight and subsequent growth trajectory, we did not include this in multivariable models.
We used multilevel modeling (MLM) with random slopes and intercepts (i.e., mixed procedure in Stata SE 14; Stata Corp, College Station, TX) to model the effects of prenatal social support and time on infant WFLz from birth to age 18 months. This method allowed us to test for differences in infant adiposity between those with low and high social support using all available anthropometric data, which were collected at varying time intervals for each infant. We began by specifying an unconditional growth model (WFLz conditioned on time alone) and added unstructured covariance to account for naturally occurring correlations between the intercept (model predicted WFLz at age 0) and slope (model predicted change in WFLz over time). We then added a population-level squared term for age to account for a nonlinear effect of time. We used AIC and the likelihood ratio test to assess model fit. We fit two pre-specified MLMs to determine effects of prenatal social support on infant WFLz. In Model 1, infant WFLz was conditioned on time (infant age in months), time-squared, and prenatal social support. Model 2 was the same as Model 1 with additional adjustment for significant covariates from the prior bivariate analyses (maternal age, nativity, food insecurity, and pre-pregnancy weight status). To estimate the effect of prenatal social support on change in WFLz over time, a time by social support interaction term was added to each model in a second step.
For our categorical outcome, we performed separate unadjusted and adjusted logistic regression analyses for each age to determine if prenatal social support was associated with macrosomia and overweight status at ages 6, 12, and 18 months.
Results
Of the 267 participants randomized to the control group of the parent RCT, all gave valid responses to the social support measure and 262 had infants with at least one set of anthropometric measures in the first 18 months of life. The 5 women whose infants did not have anthropometric data did not differ on any baseline characteristics from those whose infants did have anthropometric data. Table 1 summarizes baseline characteristics and differences by social support level. The majority of participant mothers were born outside of the US (80%) and 30% had not completed high school. Pre-pregnancy overweight/obesity was present in 65% of women. Responses to the social support measure ranged from 0 to 30 people to count on in times of need, with a median of 3 and interquartile range of 2 to 5. Twenty percent of women reported low social support (fewer than 2 people to count on). As shown in Table 1, this was associated with older age, birth outside of the US, food insecurity, and pre-pregnancy overweight or obese status. Prenatal social support was not associated with education, marital status, depressive symptoms, excessive GWG, or gestational diabetes mellitus.
Table 1.
Baseline maternal characteristics and associations with prenatal social support.*
| Total sample (n=262) n (%) | Low social support (n=52) n (%) | High social support (n=210) n (%) | p-value† | |
|---|---|---|---|---|
| Socio-demographic factors | ||||
| Age in years, mean (SD) | 27.9 (5.8) | 29.5 (5.3) | 27.5 (5.8) | 0.03 |
| Born outside of US | 211 (80%) | 50 (96%) | 161 (77%) | <0.01 |
| Completed high school | 185 (70%) | 33 (63%) | 152 (72%) | 0.21 |
| Married or living as married | 188 (72%) | 40 (77%) | 148 (70%) | 0.35 |
| Psychosocial factors | ||||
| Food insecure | 87 (33%) | 27 (52%) | 60 (29%) | <0.01 |
| Depressive symptoms | 87 (33%) | 20 (38%) | 67 (32%) | 0.37 |
| Weight-related factors | ||||
| Pre-pregnancy Overweight/obesity | 170 (65%) | 42 (81%) | 128 (61%) | 0.01 |
| Excessive GWG‡ | 74 (29%) | 19 (37%) | 55 (27%) | 0.30 |
| Gestational diabetes mellitus | 10 (4%) | 2 (4%) | 8 (4%) | >0.99 |
Prenatal social support was measured by maternal response to “How many people can you count on in times of need?” with low social support defined as 0–1 person to count on and high social support defined as ≥2 people to count on.
P-values were determined by t-tests and χ2 analyses measuring differences between women with low and high prenatal social support.
n=259 total; GWG, gestational weight gain. Excessive gestational weight gain is defined by the Institute of Medicine as >40 pounds for women with pre-pregnancy underweight, >35 pounds for women with pre-pregnancy normal weight, >25 pounds for women with pre-pregnancy overweight, and >20 pounds for women with pre-pregnancy obesity.33
Anthropometric data for the 262 infants included 2540 sets of paired anthropometric observations (weight and length) with an average of 10 observations per infant (range 1 to 19) over the first 18 months of life. The correlation between random intercepts and slopes in unadjusted and adjusted MLMs was negative and significant, indicating that on average, infants born smaller grew faster than those born bigger. Model fit was improved by the addition of unstructured covariance that allowed for this correlation (Model 1 independent level and slope effects: AIC 7241; unstructured covariance: 7227) and a squared term for time (LR test significant, χ2 91.7, p<0.01).
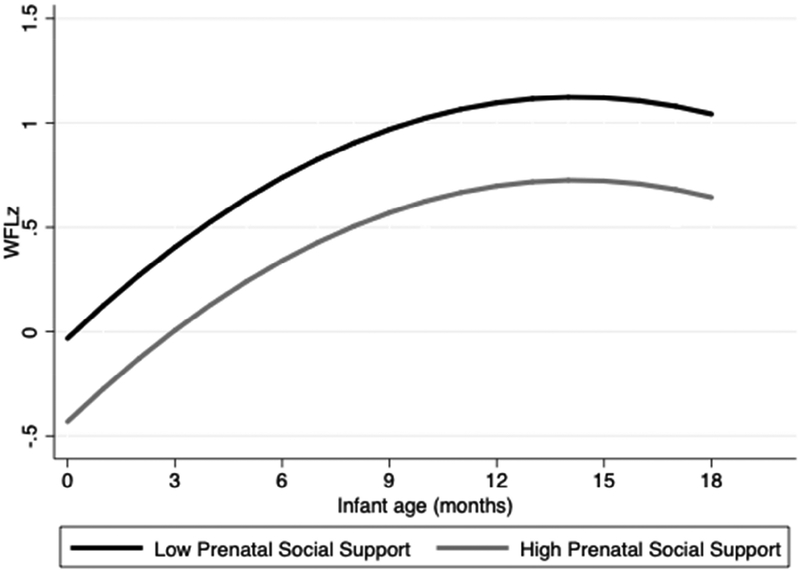
Effects of time and prenatal social support on infant WFLz are shown in Table II. Infant age had a significant and positive linear effect on adiposity that was similar in both models (B=0.16, 95% CI 0.14, 0.18). This indicates that mean WFLz trajectories for the whole sample, regardless of prenatal social support, increased over time. The magnitude of this increase, however, became smaller over time, as indicated by the negative effect of the quadratic term in the model. Prenatal social support had a significant effect on WFLz in unadjusted and adjusted models. Infant adiposity trajectories for those with low and high prenatal social support are depicted in the Figure. Over the first 18 months of life, infants born to mothers with high prenatal social support had mean WFLz 0.4 units lower than infants born to mothers with low social support (Model 1: B=−0.45, 95% CI −0.67, −0.22; Model 2: B=−0.40, 95% CI −0.63, −0.16). A time by social support interaction term was not significant and did not improve model fit (Model 1: LR χ2 0.29, p=0.59; Model 2: LR χ2 0.28, p=0.60) suggesting that the effect of prenatal social support on WFLz did not change significantly over time. A conservative approach to model selection39 adopts the simpler model and adjusts the inference accordingly. With that approach the differential between low and high prenatal social support remains significant at the 0.05 level.
Table 2.
Multilevel models of time and prenatal social support effects on infant weight-for-length z-score (WFLz) from birth to age 18 months in 262 mother-infant pairs.
| Model 1 | Model 2* | |||
|---|---|---|---|---|
| B (SE) | 95% CI | B (SE) | 95% CI | |
| Intercept | 0.002 (0.11) | −0.21, 0.21 | 0.09 (0.28) | −0.47, 0.64 |
| Time (age in months) | 0.16 (0.01) | 0.14, 0.18 | 0.16 (0.01) | 0.14, 0.18 |
| Time squared | −0.006 (0.0006) | 0.007, −0.005 | −0.006 (0.0006) | −0.007, −0.005 |
| High social support† | −0.45 (0.11) | −0.67, −0.22 | −0.40 (0.12) | −0.63, −0.16 |
Adjusted for maternal age, birth country, food insecurity, and pre-pregnancy weight status.
High social support was defined as having at least two people to count on in times of need; A time by social support interaction term was not significant and did not improve model fit when added to either model.
Figure.
Predicted mean adiposity trajectories for 262 infants born to mothers with low and high prenatal social support, controlling for maternal age, nativity, pre-pregnancy weight status, and food insecurity.
Prenatal social support was also associated with differences in categorical infant weight status, as shown in Table 3. Infants born to mothers with high prenatal social support had a lower prevalence of macrosomia than those born to mothers with low prenatal social support (9% vs. 25%, χ2 9.99, p<0.01). Of note, all 4 low birth weight infants in the sample (2%) were in the high social support group, but this was not a statistically significant finding (2% vs. 0%, χ2 1.00, p=0.32) and overall prevalence of low birth weight was much lower in our sample than national estimates (7% for Hispanics and 8% overall).40 The prevalence of overweight was lower at ages 6, 12, and 18 months for infants born to mothers with high social support as compared with low social support. This difference did not reach statistical significance at age 6 months, but was significant at age 12 months (9% vs. 27%, χ2 8.43, p<0.01) and 18 months (13% vs. 34%, χ2 7.89, p<01). These differences persisted after adjustment for relevant covariates with the odds of overweight significantly lower for infants whose mothers had high social support compared with those who had low social support (12 months aOR 0.28, 95% CI 0.10, 0.74; 18 months aOR 0.35, 95% CI 0.14, 0.89).
Table 3.
Prenatal social support effect on infant weight status from birth to age 18 months.
| Age | n | Full sample n (%) | Low social support n (%) | High social support n (%) | OR† | 95% CI | aOR‡ | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| % Overweight* | Birth | 262 | 32 (12%) | 13 (25%) | 19 (9%) | 0.30 | 0.14, 0.65 | 0.35 | 0.15, 0.80 |
| 6 months | 216 | 15 (7%) | 4 (10%) | 11 (6%) | 0.64 | 0.19, 2.12 | 0.60 | 0.16, 2.14 | |
| 12 months | 188 | 23 (12%) | 9 (27%) | 14 (9%) | 0.26 | 0.10, 0.68 | 0.28 | 0.10, 0.74 | |
| 18 months | 160 | 28 (18%) | 11 (34%) | 17 (13%) | 0.29 | 0.12, 0.71 | 0.35 | 0.14, 0.89 |
Overweight defined as ≥4kg at birth (i.e., macrosomia) and as weight-for-length z-score ≥2 at subsequent ages, according to World Health Organization reference standards.
Odds ratios estimated by logistic regression.
Adjusted odds ratios estimated by multiple logistic regression adjusted for maternal age, birth country, food insecurity, and pre-pregnancy weight status.
Discussion
We found that high prenatal social support, a component of resilience, independently predicted lower infant adiposity over the first 18 months of life. Mothers with high prenatal social support were approximately one third as likely to have a newborn with macrosomia or a 12 or 18 month old with overweight. These findings add to the mounting evidence that the prenatal period represents a critical time to target for child obesity prevention and that resilience factors during this period can have significant and lasting effects on child growth trajectories.41,42
The role of social support has been well-studied during pregnancy, primarily as it relates to adverse perinatal outcomes (e.g., low birth weight, preterm birth, Apgar scores, operative delivery)15,43,44 and the prenatal behaviors and maternal conditions that affect these outcomes (e.g., smoking,13 diet and physical activity,45 depression32). This body of evidence developed from studies aiming to understand the role of social support in preventing perinatal morbidity, and has not previously focused on infant adiposity and child obesity risk. Many of these studies have targeted populations at highest risk of low birth weight and other poor pregnancy outcomes (adolescents, African Americans, women with poor prenatal care or chronic medical illness),46 not necessarily populations at high risk of early child obesity. However, low prenatal social support was more than twice as prevalent in our sample of low-income, Hispanic women as compared with other studies using similar categorical measures in other demographic groups.29,47 There is a strong and well-documented socioeconomic gradient in obesity prevalence in the US3 and these findings suggest that prenatal social support, although protective against infant adiposity overall, may be more scarce for the most vulnerable children. In the context of the growing obesity epidemic that disproportionately impacts Hispanic young children,1 evidence that prenatal social support is protective against adiposity in infancy begins to fill several important gaps in the literature.
Our finding that social support was protective against macrosomia is important because birth weight is known to be associated with subsequent infant growth and macrosomia is highly predictive of early child obesity, particularly in Hispanic children.48–50 Because the association of birth weight with prenatal social support has been studied almost exclusively in women with high risk of delivering low birth weight infants, birth weight has most frequently been characterized as low birth weight versus healthy birth weight, without analysis of its association to high birth weight (i.e., macrosomia). In contrast, our sample was limited to relatively healthy, low risk pregnancies with a high prevalence of pre-pregnancy overweight and obesity, strong predictors of macrosomia. This differential pattern of risk between our study cohort and that of prior studies likely played a role in the directionality of our birth weight findings, in which prenatal social support significantly protected against macrosomia but did not significantly alter the odds of low birth weight.
We also found that differences in weight between infants with differential exposure to prenatal social support persisted well beyond birth. Infants born to mothers with high social support had less adiposity over the first year and a half of life and lower odds of overweight status at ages 12 and 18 months. There are a number of possible explanations for these lasting effects, which will require empirical testing in future studies. The metabolic and neuroendocrine programming that occur in utero exert strong influence on birth weight,51,52 and high birth weight is highly associated with early child obesity.50 Thus, the effects of prenatal social support on postnatal growth may simply be the consequences of its effects on prenatal growth and birth weight. However, there are also numerous post-partum maternal behaviors and environmental conditions known to be associated with prenatal social support that impact mother-infant pairs more broadly and may play a role in supporting healthy growth. Prenatal social support has been associated with lower rates of post-partum depression,14,53 healthier infant attachment,53 less parenting stress,54 and higher rates of breastfeeding16 and responsive parenting.17 All of these factors have favorable effects on subsequent child obesity risk in the literature,55,56 but just as the prenatal social support literature has not focused on child weight outcomes, few studies of child obesity have included measures of prenatal social support. The pathophysiology of child obesity is complex and its developmental origins are multifactorial, so further study of these associations and pathways are needed.
The effects of prenatal social support must be considered in the context of effects of social support more generally, that may impact maternal health and well-being prior to pregnancy. Social support has been linked to decreased morbidity and mortality from a broad range of conditions over the entire life course,10,57,58 and several studies have found that women who feel supported have a lower prevalence of overweight and obesity than those who lack social support. Though this literature has primarily included white and African American samples,11,12,59,60 pre-pregnancy maternal obesity is known to be a strong predictor of child obesity regardless of race or ethnicity.61 Our bivariate results show that overweight/obesity was significantly less prevalent among women with high social support. This is important given high rates of obesity among Hispanic women of childbearing age36 and the impact this has on both their own health and the health and obesity risk of their children.62
We found that marital status was not significantly associated with prenatal social support. Moreover, although we did not ascertain who provided social support, of the 16 participants in the larger trial who reported having no one to count on in times of need, 11 were married. This highlights an important distinction between structure and function that has often been raised in the social support literature.9 Structural aspects of social networks and measures of these structural components (e.g., marital status, number of people living at home, number of social contacts) are quite different from the functional role of those social networks, which may or may not include the provision of social support.9,10 Although it is clear that prenatal social support provided by an intimate partner can have positive effects on perinatal outcomes,44,63,64 simply having a partner does not guarantee the provision of adequate support or the health benefits associated with it.
Our findings should be considered in the context of several limitations. First, although we have longitudinal data for infant adiposity, we only have data for social support at a single point in time. Trajectories of social support over the course of pregnancy and early infancy have not been extensively studied, but it is likely that social support is not static. Therefore, future studies of social support should include repeated measures, particularly when studying outcomes that vary over time. Second, the MSSI item used to measure social support is composed of a single question that does not capture the multidimensional nature of social support, despite its predictive power as an independent measure in prior studies. Further study of associations between infant weight and different dimensions of maternal social support measured over time is warranted. Third, our findings may not be generalizable to other populations, as our sample was composed of low-income, Hispanic families. An additional limitation in generalizability stems from the exclusion criteria of the larger trial. Pregnant women with significant medical or psychiatric illness or those who are homeless may be at the highest risk of low social support but were excluded from our study, potentially decreasing the variation of social support in our sample. Future studies should include more vulnerable populations to appropriately capture experiences across the spectrum of social support. Lastly, social support may exert its effects, at least in part, by moderating or “buffering” the adverse effects of stress on health.10 Because our study did not include a measure of maternal stress, we were unable to analyze social support as a moderator in this way, and the inclusion of stress measures is an important consideration for future studies.
Our study showed that pregnant, low-income Hispanic women with high social support had infants with less adiposity over the first 18 months of life and significantly lower odds of macrosomia and overweight at ages 12 and 18 months. Although many prior studies have examined more conventional measures of prenatal mental health (e.g., depression, self-efficacy) in relation to infant feeding styles and practices,65,66 few have considered the role of social support as a distinct construct. Based on our results, it is plausible that the omission of social support may result in unmeasured confounding, and further study of how social support during the prenatal period may protect against infant adiposity is warranted. We believe that the field would benefit from interdisciplinary research to incorporate measurement of prenatal social support in obesity prevention studies, as well as adequate assessment of child growth outcomes in studies of prenatal social support. Adiposity in infancy is one of the strongest predictors of obesity later in childhood, and understanding factors that protect against excess infant weight gain and obesity is critical to developing effective models of obesity prevention that focus on strength and resilience rather than risk.
Acknowledgments
M.K. was supported in part by the Health Resources & Services Administration (T32HP22238) and the National Center for Advancing Translational Sciences (UL1TR001445 [to the NYU Langone Health CTSI]). This study was also supported by the National Institute of Food and Agriculture, United States Department of Agriculture (2011-68001-30207 [to M.M.]); and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23HD081077 [to R.G.]). The authors declare no conflicts of interest.
List of abbreviations
- WFLz
weight-for-length z-score
- RCT
randomized controlled trial
- EGA
estimated gestational age
- WHO
World Health Organization
- MSSI
Maternal Social Support Index
- US
United States
- USDA
United States Department of Agriculture
- BMI
body mass index
- MLM
multilevel modeling
- AIC
Akaike information criterion
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this study were presented as abstracts as the Pediatric Academic Societies annual meeting, May 5–8, 2018, Toronto, Canada; and ObesityWeek, October 29-November 2, 2017, Washington, DC.
References
- 1.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3):e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292. doi: 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossen LM, Schoendorf KC. Measuring health disparities: Trends in racial-ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001–2010. Ann Epidemiol. 2012;22(10):698–704. doi: 10.1016/j.annepidem.2012.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Isong IA, Rao SR, Bind M-A, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. doi: 10.1542/peds.2017-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polk S, Thornton RJ, Caulfield L, Muñoz A. Rapid infant weight gain and early childhood obesity in low-income Latinos and non-Latinos. Public Health Nutr. 2016;19(10):1777–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kazlauskas E, Gailiene D, Vaskeliene I, Skeryte-Kazlauskiene M. Intergenerational transmission of resilience? Sense of coherence is associated between Lithuanian survivors of political violence and their adult offspring. Front Psychol. 2017;8(SEP):1677. doi: 10.3389/fpsyg.2017.01677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cassel J An epidemiological perspective of psychosocial factors in disease etiology. Am J Public Health. 1974;64(11):1040–1043. doi: 10.2105/AJPH.64.11.1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. [DOI] [PubMed] [Google Scholar]
- 10.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 11.Brogan K, Idalski Carcone A, Jen KLC, Ellis D, Marshall S, Naar-King S. Factors associated with weight resilience in obesogenic environments in female African-American adolescents. J Acad Nutr Diet. 2012;112(5):718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Assari S, Caldwell CH, Zimmerman MA. Low parental support in late adolescence predicts obesity in young adulthood; Gender differences in a 12-year cohort of African Americans. J Diabetes Metab Disord. 2015;14(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harley K, Eskenazi B. Time in the United States, social support and health behaviors during pregnancy among women of Mexican descent. Soc Sci Med. 2006;62(12):3048–3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie R-H, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann Epidemiol. 2009;19(9):637–643. doi: 10.1016/j.annepidem.2009.03.008 [DOI] [PubMed] [Google Scholar]
- 15.Orr ST. Social support and pregnancy outcome: a review of the literature. Clin Obstet Gynecol. 2004;47(4):842. [DOI] [PubMed] [Google Scholar]
- 16.Dennis C-L, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast-feeding duration among primiparous women: a randomized controlled trial. CMAJ. 2002;166(1):21–28. [PMC free article] [PubMed] [Google Scholar]
- 17.Burchinal MR, Follmer A, Bryant DM. The relations of maternal social support and family structure with maternal responsiveness and child outcomes among African American families. Dev Psychol. 1996;32(6):1073–1083. doi: 10.1037/0012-1649.32.6.1073 [DOI] [Google Scholar]
- 18.Gerald LB, Anderson A, Johnson GD, Hoff C, Trimm RF. Social class, social support and obesity risk in children. Child Care Health Dev. 1994;20(3):145–163. [DOI] [PubMed] [Google Scholar]
- 19.Lindberg L, Ek A, Nyman J, Marcus C, Ulijaszek S, Nowicka P. Low grandparental social support combined with low parental socioeconomic status is closely associated with obesity in preschool-aged children: a pilot study. Pediatr Obes. 2016;11(4):313–316. doi: 10.1111/ijpo.12049 [DOI] [PubMed] [Google Scholar]
- 20.Watt TT, Martinez-Ramos G, Majumdar D. Race/ethnicity, acculturation, and sex differences in the relationship between parental social support and children’s overweight and obesity. J Health Care Poor Underserved. 2012;23(4):1793–1805. [DOI] [PubMed] [Google Scholar]
- 21.Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Randomized controlled trial of a primary care-based child obesity prevention intervention on infant feeding practices. J Pediatr. 2016;174:171–177.e2. doi: 10.1016/j.jpeds.2016.03.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO). WHO Anthro (version 3.2.2, January 2011) and macros. 2011. http://www.who.int/childgrowth/software/en/.
- 23.Van den Broeck J, Argeseanu Cunningham S, Eeckels R, Herbst K. Data cleaning: Detecting, diagnosing, and editing data abnormalities. PLoS Med. 2005;2(10):e267. doi: 10.1371/journal.pmed.0020267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawman HG, Ogden CL, Hassink S, Mallya G, Veur S Vander, Foster GD. Practice of epidemiology comparing methods for identifying biologically implausible values in height, weight, and body mass index among youth. Am J Epidemiol. 2015;182(4). doi: 10.1093/aje/kwv057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lo JC, Maring B, Chandra M, et al. Prevalence of obesity and extreme obesity in children aged 3–5 years. Pediatr Obes. 2014;9(3):167–175. doi: 10.1111/j.2047-6310.2013.00154.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pascoe JM, Ialongo NS, Horn WF, Reinhart MA, Perradatto D. The reliability and validity of the maternal social support index. Fam Med. 1988;20(4):271–276. [PubMed] [Google Scholar]
- 27.Adamakos H, Ryan K, Ullman DG, Pascoe J, Diaz R, Chessare J. Maternal social support as a predictor of mother-child stress and stimulation. Child Abuse Negl. 1986;10(4):463–470. doi: 10.1016/0145-2134(86)90050-5 [DOI] [PubMed] [Google Scholar]
- 28.Akaike H A new look at the statistical model identification. IEEE Trans Autom Control. 1974. doi: 10.1109/TAC.1974.1100705 [DOI] [Google Scholar]
- 29.Lespinasse AA, David RJ, Collins JW, Handler AS, Wall SN. Maternal support in the delivery room and birthweight among African-American women. J Natl Med Assoc. 2004;96(2):187–195. [PMC free article] [PubMed] [Google Scholar]
- 30.Almeida J, Mulready-Ward C, Bettegowda VR, Ahluwalia IB. Racial/Ethnic and nativity differences in birth outcomes among mothers in New York City: the role of social ties and social support. Matern Child Health J. 2014;18(1):90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iguacel I, Michels N, Ahrens W, et al. Prospective associations between socioeconomically disadvantaged groups and metabolic syndrome risk in European children. Results from the IDEFICS study. Int J Cardiol. 2018. doi: 10.1016/j.ijcard.2018.07.053 [DOI] [PubMed] [Google Scholar]
- 32.Sidebottom AC, Hellerstedt WL, Harrison PA, Hennrikus D. An examination of prenatal and postpartum depressive symptoms among women served by urban community health centers. Arch Womens Ment Health. 2014;17(1):27–40. doi: 10.1007/s00737-013-0378-3 [DOI] [PubMed] [Google Scholar]
- 33.Harrison PA, Sidebottom AC. Systematic prenatal screening for psychosocial risks. J Health Care Poor Underserved. 2008;19(1):258–276. doi: 10.1353/hpu.2008.0003 [DOI] [PubMed] [Google Scholar]
- 34.Coleman-Jensen A, Nord M, Andrews M, Carlson S, Alisha Coleman-Jensen MNMA, Carlson S. Household foods security in the United States in 2010, ERR-125. United States Dep Agric Econ Res Serv. 2011;(125):1–29. http://minoritynewsservice.com/images/userfiles/USDAFoodSecurity(1).pdf. [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rasmussen KM, Abrams B, Bodnar L, Butte NF, Catalano PM, Siega-Riz AM. Recommendations for weight gain during pregnancy in the context of the obesity epidemic. Obs Gynecol. 2010;116(5):1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi: 10.2337/dc09-1848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berk R, Brown L, Buja A, Zhang K, Zhao L. Valid post-selection inference. Ann Stat. 2000:1–39. [Google Scholar]
- 40.Martin JA, Hamilton BE, Osterman MJKS, Driscoll AK, Drake P. Births: Final data for 2016 National Vital Statistics Reports. Natl Vital Stat Reports. 2018;67(1):1–55. doi:May 8, 2013 [PubMed] [Google Scholar]
- 41.Whitaker RC, Whitaker RC, Dietz WH, Dietz WH. Role of the prenatal environment in the development of obesity. J Pediatr. 1998;132(5):768–776. [DOI] [PubMed] [Google Scholar]
- 42.Ehrenthal DB, Maiden K, Rao A, et al. Independent relation of maternal prenatal factors to early childhood obesity in the offspring. Obstet Gynecol. 2013;121(1):115–121. [DOI] [PubMed] [Google Scholar]
- 43.Turner RJ, Grindstaff CF, Phillips N. Social support and outcome in teenage pregnancy. J Health Soc Behav. 1990;31(1):43–57. [PubMed] [Google Scholar]
- 44.Feldman PJ, Dunkel-Schetter C, Sandman CA, Wadhwa PD. Maternal social support predicts birth weight and fetal growth in human pregnancy. Psychosom Med. 2000;62(5):715–725. [DOI] [PubMed] [Google Scholar]
- 45.Thornton PL, Kieffer EC, Salabarría-Peña Y, et al. Weight, diet, and physical activity-related beliefs and practices among pregnant and postpartum Latino women: the role of social support. Matern Child Health J. 2006;10(1):95–104. doi: 10.1007/s10995-005-0025-3 [DOI] [PubMed] [Google Scholar]
- 46.Valero De Bernabé J, Soriano T, Albaladejo R, et al. Risk factors for low birth weight: A review. Eur J Obstet Gynecol Reprod Biol. 2004;116(1):3–15. doi: 10.1016/j.ejogrb.2004.03.007 [DOI] [PubMed] [Google Scholar]
- 47.Almeida J, Molnar BE, Kawachi I, Subramanian SV. Ethnicity and nativity status as determinants of perceived social support: Testing the concept of familism. Soc Sci Med. 2009;68(10):1852–1858. doi: 10.1016/j.socscimed.2009.02.029 [DOI] [PubMed] [Google Scholar]
- 48.Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: A Systematic review. Am J Prev Med. 2016;50(6):761–779. [DOI] [PubMed] [Google Scholar]
- 49.Woo Baidal JA, Criss S, Goldman RE, Perkins M, Cunningham C, Taveras EM. Reducing Hispanic children’s obesity risk factors in the first 1000 days of life: a qualitative analysis. J Obes. 2015;2015:945918. doi: 10.1155/2015/945918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu ZB, Han SP, Zhu GZ, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12(7):525–542. [DOI] [PubMed] [Google Scholar]
- 51.Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11(4):496–506. doi: 10.1038/oby.2003.69 [DOI] [PubMed] [Google Scholar]
- 52.Stout SA, Espel EV, Sandman CA, Glynn LM, Davis EP. Fetal programming of children’s obesity risk. Psychoneuroendocrinology. 2015;53:29–39. doi: 10.1016/j.psyneuen.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ohara M, Okada T, Aleksic B, et al. Social support helps protect against perinatal bonding failure and depression among mothers: a prospective cohort study. Nat Publ Gr. 2017;7(1):9546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lu M-H, Wang G-H, Lei H, Shi M-L, Zhu R, Jiang F. Social support as mediator and moderator of the relationship between parenting stress and life satisfaction among the Chinese parents of children with ASD. J Autism Dev Disord. 2018;48(4):1181–1188. doi: 10.1007/s10803-017-3448-y [DOI] [PubMed] [Google Scholar]
- 55.Hughes SO, Power TG, Liu Y, Sharp C, Nicklas TA. Parent emotional distress and feeding styles in low-income families. The role of parent depression and parenting stress. Appetite. 2015;92(C):337–342. doi: 10.1016/j.appet.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 56.Parks EP, Kazak A, Kumanyika S, Lewis L, Barg FK. Perspectives on stress, parenting, and children’s obesity-related behaviors in black families. Health Educ Behav. 2016;43(6):632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cohen S, McKay G. Social support, stress and buffering hypothesis: A theoretical analysis Handbook of psychology and health. In: Baum A, Taylor SE, Singer JE, eds. Hillsdale, NJ; 1984. [Google Scholar]
- 58.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- 59.Serlachius A, Elovainio M, Juonala M, et al. High perceived social support protects against the intergenerational transmission of obesity: The Cardiovascular Risk in Young Finns Study. Prev Med (Baltim). 2016;90:79–85. [DOI] [PubMed] [Google Scholar]
- 60.Ali SM, Lindström M. Socioeconomic, psychosocial, behavioural, and psychological determinants of BMI among young women: differing patterns for underweight and overweight/obesity. Eur J Public Health. 2005;16(3):324–330. doi: 10.1093/eurpub/cki187 [DOI] [PubMed] [Google Scholar]
- 61.Flores G, Lin H. Factors predicting overweight in US kindergartners. Am J Clin Nutr. 2013;97(6):1178–1187. [DOI] [PubMed] [Google Scholar]
- 62.Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. Am J Clin Nutr. 2010;91(6):1560–1567. [DOI] [PubMed] [Google Scholar]
- 63.Luecken LJ, Lin B, Coburn SS, MacKinnon DP, Gonzales NA, Crnic KA. Prenatal stress, partner support, and infant cortisol reactivity in low-income Mexican American families. Psychoneuroendocrinology. 2013;38(12):3092–3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Crnic KA, Greenberg MT, Ragozin AS, Robinson NM, Basham RB. Effects of stress and social support on mothers and premature and full-term infants. Child Dev. 1983;54(1):209–217. [PubMed] [Google Scholar]
- 65.Barrett KJ, Thompson AL, Bentley ME. The influence of maternal psychosocial characteristics on infant feeding styles. Appetite. 2016;103:396–402. doi: 10.1016/j.appet.2016.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Goulding AN, Rosenblum KL, Miller AL, et al. Associations between maternal depressive symptoms and child feeding practices in a cross-sectional study of low-income mothers and their young children. Int J Behav Nutr Phys Act. 2014;11(1):1–11. doi: 10.1186/1479-5868-11-75 [DOI] [PMC free article] [PubMed] [Google Scholar]