Abstract
There is limited understanding of the relationship between emotion dysregulation and weight gain among smokers, although available data suggest there are potential relationships that may be of clinical importance. The present study explored a potential mechanism in the relationship between emotion dysregulation and body mass index (BMI). Specifically, the current study examined the indirect effects of emotional eating on the association between emotion dysregulation and BMI among smokers. Participants included 136 (52.2% female; Mage = 42.25, SD = 11.24) adults who were treatment-seeking smokers. Primary analysis included one regression-based model, wherein emotion dysregulation served as the predictor, emotional eating as the intermediary variable, and BMI as the criterion variable. Covariates were age and gender. Results indicated that emotional dysregulation was significantly associated with BMI through emotional eating (a*b = 0.02, SE = .01, CI95% = 0.002, 0.042). The current findings provide initial empirical evidence that greater reported levels of emotion dysregulation may be associated with greater reported levels of emotional eating, which in turn, may be related to higher BMI.
Keywords: Emotion dysregulation, Emotional Eating, Body Mass Index, Smoking
The impact of obesity is not equally distributed in society (Healton, Vallone, McCausland, Xiao, & Green, 2006) with smokers as one group that may be prone to obesity-related problems. Indeed, among smokers, obesity is highly prevalent with over 9 million adult smokers considered obese (Healton et al., 2006). Many smokers may be at risk for weight gain and obesity as a result of the tendency to engage in comorbid problematic health behaviors (e.g., physical inactivity, poor diet; Chiolero, Jacot-Sadowski, Faeh, Paccaud, & Cornuz, 2007). Notably, the combined impact of obesity and smoking is associated with a 3.5 to 5.2 fold increased risk of mortality relative to normal weight non-smokers (Freedman et al., 2006). As such, weight loss and tobacco cessation have been a focus of public health efforts to decrease common negative health consequences associated with these risk factors (Centers for Disease Control and Prevention, 2016; Ma & Xiao, 2010; United States Department of Health and Human Services (USDHHS), 2014).
To better address obesity and weight gain, there is merit in focusing on motivational models of eating behavior (Burgess, Turan, Lokken, Morse, & Boggiano, 2014; Jackson, Lynne Cooper, Mintz, & Albino, 2003). Such an approach recognizes that there are several distinct motives for eating that can vary both between and within individuals (Burgess et al., 2014; Jackson et al., 2003). Of the various motives for eating, emotional eating has emerged as one particularly dysfunctional eating pattern (Ricca et al., 2012; van Strien, Konttinen, Homberg, Engels, & Winkens, 2016) related to weight gain (van Strien et al., 2016). Emotional eating is defined as eating in response to diffuse emotions or in response to clearly labeled emotions (van Strien, Frijters, Bergers, & Defares, 1986b). Emotional eating has been documented as a contributing factor to higher body mass index (a measure of overweight and obesity; [BMI]; Grant & Boersma, 2005; USDHHS, 2012). Indeed, extant work has found that higher levels of emotional eating are associated with weight gain, suggesting emotional processes may, in part, influence eating behavior (Koenders & van Strien, 2011) and subsequent weight gain. For instance, Sung and colleagues (2009) found that emotional eating was an indicator of weight gain at a 4-year follow-up. Moreover, research has shown that people who overconsume food and have higher levels of emotional eating are prone to weight gain, whereas those who overconsume food with lower levels of emotional eating are not prone to weight gain (van Strien, Peter Herman, & Verheijden, 2012).
Van Strien and colleagues (2012) suggested in order to implement optimal weight-related interventions, emotional eating should be addressed. Given the experience of negative emotions has been linked to emotional eating and subsequent overeating (Sultson, Kukk, & Akkermann, 2017), inadequate regulation of such negative emotions (i.e., emotion dysregulation) may be one clinically important risk-factor of emotional eating. Emotion dysregulation involves difficulties engaging a set of abilities wherein one can observe, understand, evaluate, and differentiate one’s emotions and subsequently access strategies to regulate emotions and control behavioral responses (Gratz & Roemer, 2004a). Facets of emotion dysregulation (e.g. emotional non-acceptance, difficulty engaging in goal directed behavior, limited access to emotion regulation strategies) have been linked to both smoking (Adams, Tull, & Gratz, 2012; Rogers et al., 2018) and weight gain (Sainsbury et al., 2018). Available research among adults who are obese, suggests that emotion dysregulation is independently related to eating in response to aversive states even after accounting for negative affectivity (Gianini, White, & Masheb, 2013). Moreover, extant neuroimaging work has found that smokers exhibit abnormal brain functions in brain regions (e.g., prefrontal cortex; Bechara et al., 2001; Galvan, Poldrack, Baker, McGlennen, & London, 2011; Goldstein & Volkow, 2011; Lubman, Yucel, & Pantelis, 2004; Sutherland, McHugh, Pariyadath, & Stein, 2012) consistently associated with emotion regulation (McRae et al., 2010; Mocaiber et al., 2011; Moratti, Saugar, & Strange, 2011; Ochsner et al., 2004). This data highlights that smokers may have greater susceptibility to difficulties with emotion dysregulation.
Theoretically, broadly in line with past work, smokers who have difficulties regulating emotions may be more likely to engage in emotional eating as a coping mechanism in response to aversive states (Gianini et al., 2013). Moreover, because of increased levels of emotional eating, such individuals may be at a greater risk of weight gain (Koenders & van Strien, 2011; Sung et al., 2009; van Strien et al., 2012). However, to our knowledge, no study has examined the indirect relationship between emotion dysregulation and BMI through emotional eating generally, or among smokers. The proposed model may shed empirical and theoretical light on intermediary variables related to weight gain and other comorbid health behaviors among this high-risk group of smokers with elevated anxiety sensitivity.
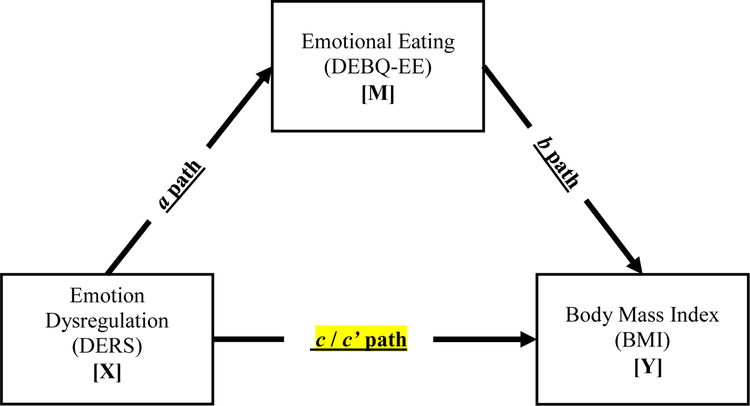
Together, the present study tested the hypothesis that emotional eating would exert an indirect effect on the relationship between emotion dysregulation and BMI (Figure 1). It was hypothesized that higher levels of emotion dysregulation would be related to greater levels of emotional eating, which in turn, would be related to an increase in BMI. It was further hypothesized that the effects of emotion dysregulation on BMI indirectly through emotional eating would be evident over and above two theoretically-relevant covariates: gender and age (Prentice & Jebb, 2001).
Figure 1.
Conceptual model
Note. a path = Effect of X on M; b path = Effect of M on Y, controlling for X; c path = Total effect of X on Y; c’ path= Direct effect of X on Y controlling for M. A single path was conducted (X) on the outcome (Y). Covariates included age and gender.
Method
Measures
Demographic Questionnaire.
A demographic questionnaire was used to measure age and gender of the study participants.
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004).
The DERS is a 36-item self-report questionnaire used to assess how often respondents experience dysregulated emotional states. Items are measured on a 5-point Likert-type scale from 1 (almost never) to 5 (almost always). The DERS yields a total score (Cronbach’s α = .93 in the current sample) as well as six subscale scores: Non-Acceptance of Emotional Responses, Difficulties Engaging in Goal-Directed Behavior, Impulse Control Difficulties, Lack of Emotional Awareness, Access to Emotion Regulation Strategies, and Lack of Emotional Clarity. The DERS demonstrates strong psychometric properties, including high test-retest reliability, high internal consistency, and good construct and predictive validity (Gratz & Roemer, 2004; Whiteside et al., 2007).
Dutch Eating Behavior Questionnaire-Emotional Eating Subscale (DEBQ; Van Strien et al., 1986).
The DEBQ is a 33-item self-report measure used to assess 3 subscale facets: restrained eating, emotional eating, and external eating. Items are rated on a 5-point Likert-type scale ranging from 1 (never) to 5 (very often). In the current study the emotional eating subscale (13 items: e.g. “Do you have the desire to eat when you feel lonely?”) was used. The DEBQ-EE has strong psychometric properties (Van Strien et al., 1986) and internal consistency in the present study was excellent (Cronbach’s α = .96).
Body Mass Index (BMI).
Height and weight were collected from all participants and calculated based on objective measurements taken by a trained research assistant using a scale and stadiometer. Participants were asked to remove their shoes prior to measurement and any heavy clothing. BMI was calculated per World Health Organization recommendations ([weight (pounds)][height (inches)2 × 703]); (WHO), 2000).
Procedures
The present sample included adults who were treatment-seeking daily smokers recruited through community advertisements in Dallas, Texas from January 2010 to January 2014 as part of a larger randomized control trial examining exercise as a possible mechanism to assist in smoking cessation in adults who were sedentary with elevated anxiety sensitivity (Smits et al., 2012). Eligibility criteria included: (1) adults who were daily smokers (at least 1 year of smoking, a minimum of 10 cigarettes per day); (2) elevated anxiety sensitivity (a score of ≥ 20 on the 16-item Anxiety Sensitivity Index; Reiss, Peterson, Gursky, & McNally, 1986); (3) sedentary (exercising less than twice a week for 30 minutes or less at a moderate intensity); and (4) motivated to quit (reporting at least a 5 on a 10-point scale). Participants deemed eligible were randomized for an in-person baseline appointment. Informed consent was obtained from all participants. Protocol procedures were approved by the Institutional Review Board at Southern Methodist University. A comprehensive list of exclusion criteria and study procedures are provided in the study protocol (Smits et al., 2012). The current study is a secondary analysis of data from all participants who completed the baseline assessment.
Data Analytic Strategy
Sample descriptive statistics and zero-order correlations among study variables were examined (see Table 1). Primary analysis included one regression-based model (see Table 2). Specifically, emotion dysregulation served as the predictor with emotional eating as the intermediary variable and BMI as the criterion variable in the model. Covariates were age and gender.
Table 1.
Descriptive Statistics and Bivariate Correlations between Study Variables (N = 136)
| Variable | Mean/n (SD/%) |
1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1. Gendera | 136 (52.2%) | – | ||||
| 2. Agea | 42.25 (11.24) | −.105 | – | |||
| 3. DERS-Totalb | 71.43 (19.43) | .078 | −.281** | – | ||
| 4. DEBQ-EEc | 2.00 (0.86) | .264** | .070 | .268** | – | |
| 5. BMId | 26.86 (4.93) | −.088 | .242** | −.037 | .191* | – |
Note.
p < .01,
p < 05.
Covariate;
Predictor;
Intermediary Variable;
Criterion; Gender: % listed as females (Coded: 0 = male and 1 = female); DERS-Total = Difficulties with Emotion Regulation Scale – Total Score (Gratz & Roemer, 2004b); DEBQ-EE = Dutch Eating Behavior Questionnaire – Emotional Eating Subscale (van Strien, Frijters, Bergers, & Defares, 1986a); BMI = Body Mass Index; 1 = Gender; 2 = Age; 3 = DERS-Total; 4 = DEBQ-EE; 5 = BMI.
Table 2.
Indirect Effect of Emotion Dysregulation on BMI via Emotional Eating.
| X | Path | R2 | b | SE | t | p | CI (I) | CI (U) |
|---|---|---|---|---|---|---|---|---|
| 1 | DERS-Total → DEBQ-EE (a) | .161 | 0.013 | 0.004 | 3.585 | <.001 | 0.059 | 0.020 |
| DEBQ-EE → BMI (b) | .103 | 1.241 | 0.521 | 2.384 | .019 | 0.211 | 2.271 | |
| DERS-Total → BMI (c’) | −0.007 | 0.023 | −0.301 | .764 | −0.052 | 0.039 | ||
| DERS-Total → BMI (c) | .064 | 0.009 | 0.022 | 0.421 | .675 | −0.035 | 0.054 | |
| DERS-Total → DEBQ-EE → BMI (a*b) | 0.016 | 0.010 | 0.002 | 0.042 |
Note. N for analyses is 136 cases. The standard error and 95% CI for the indirect effects (a*b) are obtained through bootstrapping with 10,000 re-samples. a path = Effect of X on M; b paths = Effect of M on Yi; c’ paths= Direct effect of X on Yi controlling for M; c paths = Total effect of X on Yi. DERS-Total =Difficulties with Emotion Regulation Scale – Total Score (Gratz & Roemer, 2004b); DEBQ-EE = Dutch Eating Behavior Questionnaire – Emotional Eating Subscale (van Strien et al., 1986a); BMI = Body Mass Index.
Analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). An indirect effect is the product of path a (the association between the predictor [x] and the proposed explanatory intermediary variable [m]) and path b (the association between the proposed intermediary variable [m] and the dependent variable [y], controlling for x). As recommended, the confidence intervals around the point-estimate were constructed using 10,000 bootstrap re-samplings, and 95-percent confidence intervals (CIs) were estimated (Hayes, 2009; Preacher & Hayes, 2004, 2008). The indirect pathway is considered statistically significant if the 95% CIs around a*b does not include zero (Preacher & Hayes, 2008; Zhao, Lynch, & Chen, 2010). To further strengthen the interpretation of results, alternative models were tested by reversing the proposed intermediary variable with the predictor variable (Preacher & Hayes, 2004).
Of the 136 participants, we were missing emotion dysregulation data (n = 8), emotional eating data (n = 11), and BMI data (n = 8). Little’s MCAR test was conducted and was non-significant, indicating that there is no evidence that the data are systematically biased. Hence, missing data was imputed using the expectation-maximization algorithm in SPSS 21.0. In cases in which the N is small and the proportion of missing cases is large, it is recommended that analyses be repeated both with and without the missing data imputed in order to increase confidence in the results (Tabachnick & Fidell, 2013). Thus, analyses were conducted with the imputed dataset and the non-imputed raw dataset. Results from the dataset with imputed missing data, were identical in terms of significant and non-significant findings to results from the raw, non-imputed, dataset; thus, below we report the results from the expectation-maximization data set.
Results
Participants
Data was collected as part of a larger randomized controlled trial examining the efficacy of two smoking cessation interventions (Smits et al., 2016). Specifically, the larger study examined a standard treatment for smoking cessation + exercise as a potentially useful mechanism for smoking cessation compared to standard treatment for smoking cessation + health control. Participants for the larger trial included sedentary, males and females with elevated anxiety sensitivity, ages 18 to 65, who have been daily smokers for at least one year and are currently smoking an average of at least 10 cigarettes per day (see Smits et al., 2016). Given the current study is a secondary analysis from the larger trial, eligibility criteria were maintained from the larger trial. Participants included 136 adults who were treatment-seeking (52.2% female, Mage = 42.3 years, SD = 11.24). Participants were primarily White (74.1%), fewer were Black/African American (20.7%), Asian (2.2%), or other (3%). In the current sample, the average BMI was 26.8. Twenty-three percent fell within the obese range defined as a BMI of 30 or greater, 39.1% were within the overweight range as defined as a BMI between 25–29.9, 34.4% fell within the healthy weight range as defined as a BMI between 18.5–24.9, and 2.3% fell within the underweight range defined as a BMI below 18.5 (Centers for Disease Control and Prevention, 2016).
Bivariate Relations
Correlations for all study variables are presented in Table 1. Emotion dysregulation was not significantly correlated with BMI. Emotional eating was positively correlated with emotion dysregulation (r = .27, p < .01) and BMI (r = .19, p < .05).
Primary Analyses
Results of the indirect analysis are presented in Table 2. Higher reported levels of emotional dysregulation were positively associated with greater reported levels of emotional eating (a path: b = 0.01, SE = 0.00, p < .001). The total effects model with emotion dysregulation predicting BMI, was not significant. The full model with emotional eating was significant (R2 = 0.10, F(4, 113) = 3.74, p = .007). Specifically, higher reported levels of emotional eating were positively associated with higher BMI (b path: b = 1.24, SE = 0.52, p = .019). A test for the indirect effects indicated that higher reported levels of emotion dysregulation was associated with higher levels of BMI, indirectly through the greater reported levels of emotional eating (a*b = 0.02, SE = .01, CI95% = 0.002, 0.042).
Temporal Ordering
To further strengthen our interpretation of results and aid in specificity, a reverse model was run for emotion dysregulation. Specifically, BMI remained the criterion variable, emotional eating was the predictor and emotion dysregulation served as the intermediary variable. The indirect effect of emotional eating on BMI through emotion dysregulation was non-significant (a*b = −0.05, SE = 0.18, CI95% = −0.445, 0.310).
Discussion
As hypothesized, results indicated that emotion dysregulation had an indirect effect on BMI through emotional eating. Higher reported levels of emotion dysregulation were linked to higher reported levels of emotional eating, which in turn, were related to higher BMI levels. The observed effects were evident after adjusting for gender and age. Further, the temporal ordering test supported this model. These findings are consistent with previous studies suggesting emotional eating is associated with emotion dysregulation (Gianini et al., 2013) and increased weight gain (Grant & Boersma, 2005;Koenders & van Strien, 2011; Sung et al., 2009; van Strien et al., 2016; van Strien et al., 2012) and extends this work among a sample of sedentary smokers with high anxiety sensitivity.
The present study offers a better understanding of one potential intermediary variable concerning how emotion dysregulation may affect BMI. Results suggest that emotion dysregulation may not in it of itself be related to higher BMI levels, but instead, among smokers, emotion dysregulation may contribute to alternative maladaptive coping methods such as emotional eating to neutralize aversive emotional states. These data are consistent with affect-oriented models which suggest that maladaptive eating behaviors (e.g., binge episodes) are often triggered in response to aversive emotional states and utilized as a form of affect regulation (Pearson, Wonderlich, & Smith, 2015). Interestingly, further support for this perspective comes from the bivariate relation between emotion dysregulation and emotional eating that shared only 7% of variance. These data indicate emotion dysregulation is not isomorphic with emotional eating. Overall, from an integrative theoretical perspective, repeated use of eating for emotional reasons may influence BMI. Finally, given emotion dysregulation exerted an indirect effect on BMI through emotional eating in the absence of an association between emotion dysregulation and BMI, it is important to note that other paths not part of this formal model may be important to consider (Hayes, 2009). For example, it could be that more than one indirect path may carry the relationship between emotion dysregulation and BMI, and those paths may operate in opposite directions. For example, emotion dysregulation may be related to both emotional eating (Gianini et al., 2013) and restrictive eating (e.g., restriction of energy intake; American Psychiatric Association, 2013; Lavender et al., 2015). Specifically, emotional eating has been found to be associated with higher BMI (Koenders & van Strien, 2011; Sung et al., 2009) whereas restrictive eating has been found to be associated with lower BMI (American Psychiatric Association, 2013).
Clinically, results from the present study may facilitate future development of targeted weight management programs for smokers with reported difficulties regulating their emotions. Although efficacious weight management programs exist for smokers and non-smokers, more generally (Murphy, Rohsenow, Johnson, & Wing, 2018), no tailored weight-loss interventions exist for current smokers. Thus, it may be beneficial to understand and clinically address emotion dysregulation to enhance psychological flexibility to facilitate change in eating behavior as a weight loss intervention for smokers. Cognitive-behavioral therapy may be one promising approach to target emotion dysregulation. For example, Fairburn and colleagues (2003) have proposed a transdiagnostic cognitive-behavioral therapy (CBT) to target dysfunctional mood modulatory behavior to improve eating behavior and disorders. Dialectical behavior therapy (DBT) may also be beneficial in targeting emotional eating to facilitate weight loss, with one study finding that individuals enrolled in DBT reported between 7.6% and 10.1% loss in body weight as well reduction in emotional distress and frequency of emotional eating (Glisenti & Strodl, 2012). Future work may benefit from exploring the impact of CBT or DBT tactics in improving weight loss among smokers through reductions in emotional eating facilitated by improvement in adaptive emotion regulation tactics.
There are several limitations to consider in the present study. First, the data were cross-sectional in nature. Thus, the findings do not permit testing of temporal sequencing. Future work is needed to determine the directional effects of these associations using prospective designs. Second, as the variables were assessed via self-report, there is the possibility that the observed relations were in part a function of shared method variance. Future research would benefit by employing a multi-method assessment approach to cross-index the nature of the relations observed in the present study. Third, the current study examined one potential intermediary variable (i.e., emotional eating) in the absence of an association between emotion dysregulation and BMI. Future work should examine other potential intermediary variables that may operate in the opposite direction of emotional eating (e.g., restrictive eating) to better understand the total effect of emotion dysregulation and BMI. Finally, our sample consisted of community-recruited, sedentary, daily cigarette smokers with elevated anxiety sensitivity. Future studies may benefit by sampling from other populations to ensure the generalizability of the results to nonsmokers and mixed smoker status samples.
Overall, the current study serves as an initial exploration into the association between emotion dysregulation, emotional eating, and BMI. There was empirical evidence of indirect associations of emotion dysregulation on BMI via emotional eating. Accordingly, if replicated and extended using alternative research designs, weight loss interventions for smokers may benefit from consideration of emotion regulation therapeutic tactics aimed to reduce emotional eating.
Highlights.
Extant work identified emotional eating and emotion dysregulation as related to BMI
Results found emotion dysregulation is associated with BMI through emotional eating
Clinically, results may inform future weight loss program development for smokers
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: All other authors declare that they have no conflicts of interest.
REFERENCES
- (WHO), W. H. O. (2000). Obesity: Preventing and managing the global epidemic. Switzerland: World Health Organization. [PubMed] [Google Scholar]
- Adams CE, Tull MT, & Gratz KL (2012). The Role of Emotional Nonacceptance in theRelation between Depression and Recent Cigarette Smoking. The American Journal on Addictions, 21(4), 293–301. doi: doi: 10.1111/j.1521-0391.2012.00238.x [DOI] [PubMed] [Google Scholar]
- Association AP (2013). Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington, DC: Americna Psychiatric Association. [Google Scholar]
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, & Nathan PE (2001). Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia, 39(4), 376–389. [DOI] [PubMed] [Google Scholar]
- Burgess EE, Turan B, Lokken KL, Morse A, & Boggiano MM (2014).Profiling motives behind hedonic eating. Preliminary validation of the Palatable Eating Motives Scale. Appetite, 72, 66–72. doi: 10.1016/j.appet.2013.09.016 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, C. (2016). Defining Adult Overweight and Obesity. Overweight & Obesity. [Google Scholar]
- Chiolero A, Jacot-Sadowski I, Faeh D, Paccaud F, & Cornuz J (2007). Association of Cigarettes Smoked Daily with Obesity in a General Adult Population. Obesity, 15(5), 1311–1318. doi: doi: 10.1038/oby.2007.153 [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R(2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther, 41(5), 509–528. doi: 10.1016/S0005-7967(02)00088-8 [DOI] [PubMed] [Google Scholar]
- Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, & Ron E (2006). The Mortality Risk of Smoking and Obesity Combined. American Journal of Preventive Medicine, 31(5), 355–362. doi: 10.1016/j.amepre.2006.07.022 [DOI] [PubMed] [Google Scholar]
- Galvan A, Poldrack RA, Baker CM, McGlennen KM, & London ED (2011). Neural correlates of response inhibition and cigarette smoking in late adolescence. Neuropsychopharmacology, 36(5), 970–978. doi: 10.1038/npp.2010.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianini LM, White MA, & Masheb RM (2013). Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eating Behaviors, 14(3), 309–313. doi: 10.1016/j.eatbeh.2013.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glisenti K, & Strodl E (2012). Cognitive Behavior Therapy and Dialectical Behavior Therapy for Treating Obese Emotional Eaters. Clinical Case Studies, 11(2), 71–88. doi: 10.1177/1534650112441701 [DOI] [Google Scholar]
- Goldstein RZ, & Volkow ND (2011). Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci, 12(11), 652–669. doi: 10.1038/nrn3119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant PG, & Boersma H (2005). Making sense of being fat: A hermeneutic analysis of adults’ explanations for obesity. Counselling and Psychotherapy Research, 5(3), 212–220. doi: doi: 10.1080/17441690500310429 [DOI] [Google Scholar]
- Gratz KL, & Roemer L (2004a). Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi: 10.1023/b:joba.0000007455.08539.94 [DOI] [Google Scholar]
- Gratz KL, & Roemer L (2004b). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology & Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420. doi: 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Methodology in the social sciences. New York, NY: The Guilford Press. [Google Scholar]
- Healton CG, Vallone D, McCausland KL, Xiao H, & Green MP (2006). Smoking, obesity, and their co-occurrence in the United States: cross sectional analysis. BMJ, 333(7557), 25–26. doi: 10.1136/bmj.38840.608704.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson B, Lynne Cooper M, Mintz L, & Albino A (2003). Motivations to eat: Scale development and validation. Journal of Research in Personality, 37(4), 297–318. doi: 10.1016/S0092-6566(02)00574-3 [DOI] [Google Scholar]
- Koenders PG, & van Strien T (2011). Emotional Eating, Rather Than Lifestyle Behavior, Drives Weight Gain in a Prospective Study in 1562 Employees. Journal of Occupational and Environmental Medicine, 53(11), 1287–1293. doi: 10.1097/JOM.0b013e31823078a2 [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, & Mitchell JE (2015). Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review, 40, 111–122. doi: 10.1016/j.cpr.2015.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubman DI, Yucel M, & Pantelis C (2004). Addiction, a condition of compulsive behaviour? Neuroimaging and neuropsychological evidence of inhibitory dysregulation. Addiction, 99(12), 1491–1502. doi: 10.1111/j.1360-0443.2004.00808.x [DOI] [PubMed] [Google Scholar]
- Ma J, & Xiao L (2010). Obesity and depression in US women: results from the 2005–2006 National Health and Nutritional Examination Survey. Obesity (Silver Spring), 18(2), 347–353.doi: 10.1038/oby.2009.213 [DOI] [PubMed] [Google Scholar]
- McRae K, Hughes B, Chopra S, Gabrieli JD, Gross JJ, & Ochsner KN (2010). The neural bases of distraction and reappraisal. J Cogn Neurosci, 22(2), 248–262. doi: 10.1162/jocn.2009.21243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocaiber I, Sanchez TA, Pereira MG, Erthal FS, Joffily M, Araujo DB, et al. (2011). Antecedent descriptions change brain reactivity to emotional stimuli: a functional magnetic resonance imaging study of an extrinsic and incidental reappraisal strategy. Neuroscience, 193, 241–248. doi: 10.1016/j.neuroscience.2011.07.003 [DOI] [PubMed] [Google Scholar]
- Moratti S, Saugar C, & Strange BA (2011). Prefrontal-occipitoparietal coupling underlies late latency human neuronal responses to emotion. J Neurosci, 31(47), 17278–17286. doi: 10.1523/jneurosci.2917-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy CM, Rohsenow DJ, Johnson KC, & Wing RR (2018). Smoking and weight loss among smokers with overweight and obesity in Look AHEAD. Health Psychology, 37(5), 399–406. doi: 10.1037/hea0000607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochsner KN, Ray RD, Cooper JC, Robertson ER, Chopra S, Gabrieli JD, et al. (2004). For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage, 23(2), 483–499. doi: 10.1016/j.neuroimage.2004.06.030 [DOI] [PubMed] [Google Scholar]
- Pearson CM, Wonderlich SA, & Smith GT (2015). A risk and maintenance model for bulimia nervosa: From impulsive action to compulsive behavior. Psychol Rev, 122(3), 516–535. doi: 10.1037/a0039268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. doi: 10.3758/bf03206553 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Reserch and Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Prentice AM, & Jebb SA (2001). Beyond body mass index. Obesity Reviews, 2(3), 141–147. doi: doi: 10.1046/j.1467-789x.2001.00031.x [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, & McNally RJ (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther, 24, 1–8. [DOI] [PubMed] [Google Scholar]
- Ricca V, Castellini G, Fioravanti G, Lo Sauro C, Rotella F, Ravaldi C, et al. (2012). Emotional eating in anorexia nervosa and bulimia nervosa. Comprehensive Psychiatry, 53(3), 245–251. doi: 10.1016/j.comppsych.2011.04.062 [DOI] [PubMed] [Google Scholar]
- Rogers AH, Bakhshaie J, Viana AG, Manning K, Mayorga NA, Garey L, et al. (2018). Emotion dysregulation and smoking among treatment-seeking smokers. Addictive Behaviors, 79, 124–130. doi: 10.1016/j.addbeh.2017.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sainsbury K, Evans EH, Pedersen S, Marques MM, Teixeira PJ, Lähteenmäki L, et al. (2018). Attribution of weight regain to emotional reasons amongst European adults with overweight and obesity who regained weight following a weight loss attempt. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. doi: 10.1007/s40519-018-0487-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JA, Zvolensky MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, et al. (2016). The Efficacy of Vigorous-Intensity Exercise as an Aid to Smoking Cessation in Adults With High Anxiety Sensitivity: A Randomized Controlled Trial. Psychosom Med, 78(3), 354–364. doi: 10.1097/psy.0000000000000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JA, Zvolensky MJ, Rosenfield D, Marcus BH, Church TS, Frierson GM, et al. (2012). The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with elevated anxiety sensitivity: Study protocol for a randomized controlled trial. Trials, 13, 207. doi: 10.1186/1745-6215-13-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultson H, Kukk K, & Akkermann K (2017). Positive and negative emotional eating have different associations with overeating and binge eating: Construction and validation of the Positive-Negative Emotional Eating Scale. Appetite, 116, 423–430. doi: 10.1016/j.appet.2017.05.035 [DOI] [PubMed] [Google Scholar]
- Sung J, Lee K,& Song Y-M (2009). Relationship of eating behavior to long-term weight change and body mass index: The Healthy Twin study. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, 14(2), e98–e105. doi: 10.1007/bf03327806 [DOI] [PubMed] [Google Scholar]
- Sutherland MT, McHugh MJ, Pariyadath V, & Stein EA (2012). Resting state functional connectivity in addiction: Lessons learned and a road ahead. Neuroimage, 62(4), 2281–2295. doi: 10.1016/j.neuroimage.2012.01.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabacnick BG, & Fidell LS (2013). Using multivariate statistics (6th ed). Boston, MA: Allyn & Bacon/Pearson Education. [Google Scholar]
- USDHHS, U. S. D. o. H. H. S. (2012). What Are Overweight and Obesity? , from https://www.nhlbi.nih.gov/health/health-topics/topics/obe
- USDHHS, U. S. D. o. H. H. S. (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. US Department of Health and Human Services, CDC. 2014 [Google Scholar]
- van Strien T, Frijters JER, Bergers GPA, & Defares PB (1986a). The Dutch Eating Behavior Questionnaire (DEBQ) for Assessment of Restrained Emotional, and External Eating Behavior. International Journal of Eating Disorders, 5(2), 295–315. [Google Scholar]
- van Strien T, Frijters JER, Bergers GPA, & Defares PB (1986b). The Dutch Eating Behavior Questionnaire (Debq) for Assessment of Restrained, Emotional, and External Eating Behavior (Vol. 5). [Google Scholar]
- van Strien T, & Koenders PG (2012). How do life style factors relate to general health and overweight? Appetite, 58(1), 265–270. doi: 10.1016/j.appet.2011.10.001 [DOI] [PubMed] [Google Scholar]
- van Strien T, Konttinen H, Homberg JR, Engels RCME, & Winkens LHH (2016). Emotional eating as a mediator between depression and weight gain. Appetite, 100, 216–224. doi: 10.1016/j.appet.2016.02.034 [DOI] [PubMed] [Google Scholar]
- van Strien T, Peter Herman C, & Verheijden MW (2012). Eating style, overeating and weight gain. A prospective 2-year follow-up study in a representative Dutch sample. Appetite, 59(3), 782–789. doi: 10.1016/j.appet.2012.08.009 [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. [Google Scholar]