Introduction
Intuitive eating (IE) refers to a pattern of eating behaviors that is based on the body’s internal ability to regulate its nutritional needs [1], IE is conceptualized as containing four facets unconditional permission to eat, eating for physical rather than emotional reasons, reliance on hunger and satiety cues, and body-food choice congruence [2]. Overall, IE can be understood as eating based on physiological need or desire versus emotional state or dietary restrictions, a trust in the body’s regulation of how much to eat, and a tendency to choose foods that are good for the body. As such, IE tends to be the conceptual antithesis of popular dieting approaches and eating paradigms which involve calorie restriction or external rules and regulations of food intake.
Previous research has shown many beneficial relationships between IE and psychosocial factors [3], including positive associations with body image and related constructs (i.e., body acceptance, body dissatisfaction, body preoccupation). The acceptance model of IE [4-6] posits that having higher levels of body acceptance leads to the development of IE behaviors. In one study that compared the acceptance model of IE across multiple age groups, the final path from body appreciation to IE was confirmed for emerging (18-25 years), early (26-39 years), and middle (40-65 years) adult women [4]. These studies assume that body image predicts IE, however, they are typically cross-sectional and therefore unable to determine causal pathways with certainty or rule out bidirectional IE-body image relationships. In fact, there is a related group of literature that suggests that IE can predict body image. When IE – or other similar nondiet approaches – are used as interventions in prospective studies, it is often observed that body image improves [7-11]. In a review of relevant intervention studies, improvements in body satisfaction and decreases in body preoccupation were observed [12]. In some studies, these improvements in positive body image (i.e., decreased body dissatisfaction) were sustained at 2-year follow-up [12].
These intervention studies promote IE as a potential alternative to standard behavioral weight loss (BWL) approaches and potential predictor of weight-related outcomes. In addition to IE’s impact on psychosocial factors (e.g., body image), improvements in physiological health (e.g., blood pressure, cholesterol) have been observed in non-diet based interventions [13, 14]. Further, many studies have found a relationship between IE and body mass index (BMI), such that individuals who eat more intuitively display lower BMIs [14].
The fact that BMI is associated with IE is problematic given that BMI is also linked to body image. Specifically, previous research shows a negative association of BMI with body appreciation and a positive association of BMI with shape and weight concern [15, 16]. Thus, BMI could serve as a confounding factor in the IE-body image relationship given its dual associations with both constructs. Further, as demographic factors such as sex and race-ethnicity display differential relationships with body image, they may also impact the relationship between IE and body image [17, 18]. Based on the potential clinical utility of IE in the realm of obesity treatment and/or prevention, it is important to develop a detailed understanding of how IE is associated with these relevant psychosocial and physical factors.
The primary goal of the present study was to determine whether IE is associated with body image after adjusting for objectively measured BMI in a sample of adults. If IE and body image are uniquely related over and above the influence of BMI, it is also important to begin to understand which factors may affect this relationship. BMI may also serve as a moderator of the IE-body image relationship – along with other key demographic variables. Therefore, a secondary aim of this study was to determine whether BMI, sex, and/or race-ethnicity moderated any observed relationships between IE and body image. Without previous research considering the role of objectively measured BMI in the IE-body image relationship to inform the existing project, no a priori hypotheses regarding the primary or secondary aim were made.
Method
Participants
Participants were public university students or community members enrolled in larger, ongoing studies [19, 20]. Ongoing studies were two arms of a behavioral weight loss trial which investigated the efficacy of an acceptance-based behavioral treatment for obesity and evaluated relationships among cognitive, self-regulatory, and physiological factors of obesity. The primary study arm (K23DK103941-01A1) was open to any community members who met eligibility criteria; the secondary study arm (U54GM104938) was directly targeted toward American Indian individuals. Participants in both behavioral weight loss study arms had overweight/obesity (BMI ≥27.0 kg/m2 considered eligible). Detailed inclusion/exclusion are available in the trial methods report [19] and at ClinicalTrials.gov [20]. All measures used for the current study were collected at baseline assessments prior to the initiation of treatment.
Overall, participants were considered eligible for the current study if they were a) 18-65 years of age and b) spoke English fluently. Study exclusion criteria included: a) < 18 years old or > 65 years old, b) currently pregnant, c) history of a neurological disorder, and d) non-English speaking. Additionally, clinical trial exclusion criteria particularly relevant to the current study included: a) history of bariatric surgery or planning to get surgery within the next 12 months, or b) history of or current eating disorder. All participants provided informed consent prior to initiating the study and were appropriately compensated.
Measures
Intuitive Eating.
IE was measured with the Intuitive Eating Scale-2 (IES-2) [2]. The IES-2 is a 23-item self-report instrument with response options from 1 (Strongly Disagree) to 5 (Strongly Agree). The IES-2 provides a total IE score as well as scores for four IE subscales: Unconditional Permission to Eat (Unconditional Permission; 6 items), Reliance on Hunger and Satiety Cues (Hunger Reliance; 8 items), Eating for Physical Rather than Emotional Reasons (Physical Reasons; 6 items), and Body-Food Choice Congruence (Congruence; 3 items). Each score is represented as an average of responses to relevant items and higher scores represent greater levels of IE. The IES-2 has previously displayed good reliability and validity in both women (α = .87) and men (α = .89) [2]. The IES-2 subscales have previously displayed good reliability as well, ranging from .81 (Unconditional Permission, women) to .93 (Physical Reasons, women). In the current study the IES-2 total scale displayed good reliability (men α = .83, women α = .86) and the reliabilities of the subscales were adequate or above (Unconditional Permission men α = .73 to Congruence women α = .90).
Body Image.
Our body image construct was measured in terms of one’s concern with his/her body. Specifically, body concern was measured with the Eating Disorder Examination-Questionnaire (EDE-Q 6.0)[21]. The EDE-Q 6.0 is a 28-item self-report instrument designed to measure behaviors and cognitions commonly associated with eating pathology. Each item has response options on a Likert-type scale from 0-6 and scores are calculated as an average of responses. The EDE-Q provides scores for Restraint, Eating Concern (EC), Weight Concern (WC), and Shape Concern (SC). Pathological cognitions related to body image were of most interest in the current study. Therefore, the items on the WC and SC subscales were averaged to create a combined Body Concern scale. The combination of these two scales to create a single Body Concern scale was supported as the WC and SC subscales were significantly correlated (r = .90, p < .001) and the combined scale displayed good reliability in the current sample (α = .91). The goal of the combined scale was to reduce multiple testing, to reduce Type I error, and to present results in a parsimonious manner.
Body Mass Index and Covariates.
BMI was measured with research-grade scales: Tanita scale (TANITA Body Fat Analyzer Model TBF-105 K930599) or Seca scale (Model 813) and calculated to the nearest hundredth as kg/m2. Height was measured to the nearest .1 cm and weight was measured to the nearest .1 kg. Obesity classes were defined according to the Centers for Disease Control and Prevention (CDC) as follows: healthy weight = 18.5-24.9 kg/m2, overweight = 25.0-29.9 kg/m2, Class I obesity = 30.0-34.9 kg/m2, Class II obesity = 35.0-39.9 kg/m2 [22]. Participants’ age, sex, and race-ethnicity were measured via self-report questionnaire. Sex and race-ethnicity were dummy coded with reference groups of male and white, respectively. For moderation analyses described below, race-ethnicity was coded as a dichotomous variable (0=white, 1=racial/ethnic minority status).
Procedure
This study was approved by the university IRB and was administered according to APA ethical standards. Participants’ BMI was measured in lab by trained research personnel. The remaining study variables (i.e., IE, Body Concern, demographics and covariates) were measured in lab via online self-report measures. For those participants enrolled in larger studies all data for this project were collected prior to receiving study treatment.
Data Analysis.
All data were checked to assure they met the assumptions of normality and were appropriate for analyses. Within-person, within-scale data imputation was performed when individuals were missing ≤ 10% of scale data on the IES-2 or EDE-Q 6.0. Data were analyzed with hierarchical linear regressions which considered the relationships between total and subscale IE scores with Body Concern after controlling for covariates. A regression analysis was performed for each set of predictors (i.e., total IE, IE subscales) with the outcome (i.e., Body Concern). Covariates included age, sex, race-ethnicity, and BMI. Of note, given that study participants came from multiple settings, stratified analyses were performed to explore the patterns of results among the undergraduate versus overweight/obese treatment-seeking adult samples.
Additionally, sensitivity analyses were performed in which sex, race-ethnicity, and continuous BMI were considered as potential moderators in the relationship between IE and Body Concern. First, a moderation analysis was performed for each potential moderator with total IE. Next, potential moderators that displayed significant interactions with total IE were further probed via moderation analyses with IE subscales that were significant in primary regression analyses. For all moderation analyses with BMI, significant interactions were probed with the pick-a-point approach utilizing empirically validated and clinically meaningful BMI (kg/m2) cut-offs for weight status (i.e., 18.50, 25.00, 30.00, 35.00, 40.00) [22]. A priori significance level was set at α = .05 for all analyses. All analyses were conducted using SPSS version 24. Moderation analyses were conducted using PROCESS version 3.1.
Results
Participants
The total sample from the larger studies included 191 adults. Key variables for the current study were administered to a subset of these participants (n = 158). Within this sample, participants were retained for analyses if they had complete data for IE, Body Concern, and covariates after imputation was performed. The final sample consisted of 136 adults who were 34.4 ± 14.8 years old, 73% female, and 56% Caucasian. Of the final sample, 43% were undergraduate students and 57% were overweight/obese treatment-seeking adults. All weight categories were represented (18.5 – 50.7 kg/m2), with 18.4% of the sample falling in the overweight category and 58.1% of the sample falling in the obese category. Sample characteristics and average levels of IE and Body Concern can be observed in Table 1. Stratified primary analyses for the IE Total-Body Concern relationship indicated negative regression coefficients for both the undergraduate (β = −.56, p < .001) vs. overweight/obese treatment-seeking samples (β = −.21, p = .071), though the relationship fell short of significance in the overweight/obese sample. This pattern supports the need for our a priori-planned moderation analyses using BMI as an effect modifier. For parsimony, all results presented below are from the aggregate sample. Greater detail about the stratified demographic characteristics and primary analyses can be found in Supplementary Tables S1-S3.
Table 1.
Participant Characteristics
| n = 136 M (SD) or N (%) |
|
|---|---|
| Demographics & History | |
| Age (years) | 34.38 (14.75) |
| Gender (female) | 94 (72.9) |
| Race-Ethnicity | |
| African American | 8 (5.9) |
| American Indian/Alaska Native | 32 (23.5) |
| Asian/Pacific Islander | 2 (1.5) |
| Caucasian | 76 (55.9) |
| Hispanic | 4 (2.9) |
| Other | 2 (1.5) |
| Multiple race/ethnicity | 12 (8.8) |
| BMI (kg/m2) | 31.08 (6.95) |
| Healthy weight (< 25.00) | 32 (23.5) |
| Overweight (25.00-29.99) | 25 (18.4) |
| Class I obesity (30.00-34.99) | 38 (27.9) |
| Class II obesity (35.00-39.99) | 28 (20.6) |
| Class III obesity (≥ 40.00) | 13 (9.6) |
| Intuitive Eating (IES-2; possible range 1-5)a | |
| Total | 3.22 (0.56) |
| Unconditional Permission to Eat (Unconditional Permission) | 3.30 (0.72) |
| Eating for Physical Rather than Emotional Reasons (Physical Reasons) | 3.21 (0.92) |
| Reliance on Hunger and Satiety Cues (Hunger Reliance) | 3.15 (0.77) |
| Body-Food Choice Congruence (Congruence) | 3.25 (0.90) |
| Body Concern (EDE-Q 6.0; possible range 0-6)b | 2.76 (1.55) |
Note. BMI = body mass index; EDE-Q = Eating Disorder Examination-Questionnaire;
IES-2 = Intuitive Eating Scale-2
Higher scores on the IES-2 and its subscales represent greater levels of IE.
Higher scores on the EDE-Q 6.0 represent greater levels of body concern.
Body Image
After controlling for BMI and other covariates (i.e., Step 2), a significant negative association was found for total IE scores with Body Concern (β = −.442, p < .001). The magnitude of this relationship was a medium effect (f2 = .26), with Total IE uniquely explaining 13% of the variance in Body Concern. Additionally, significant associations were found for some IE subscales with Body Concern. Specifically, Unconditional Permission was negatively associated with Body Concern (β = −.319, p < .001), as was Physical Reasons (β = −.383, p < .001). Neither Hunger Reliance (β = .053, p = .469) nor Congruence (β = −.085, p = .284) were significantly associated with Body Concern. Together, the four IE subscales displayed a large effect (f2 = .42) on Body Concern and uniquely explained 19% of the variance in the outcome. These results can be seen in Table 2.
Table 2.
Associations of IE with Body Concern
| Model 1: Total IE (n = 136) |
Model 2: IE Subscales (n = 136) |
|||
|---|---|---|---|---|
| R2 | ΔR2 | R2 | ΔR2 | |
| Step 1a | .348 | -- | .348 | -- |
| Step 2 | .482 | .133* | .540 | .192* |
| β | P | B | P | |
| Age | .032 | .702 | .019 | .805 |
| Sexb | .196 | .008* | .141 | .056 |
| Race/Ethnicityc | - | - | - | - |
| African American vs. White | .002 | .977 | .011 | .864 |
| American Indian/Alaska Native vs. White | .096 | .207 | .123 | .098 |
| Asian/Pacific Islander vs. White | .054 | .413 | .051 | .414 |
| Hispanic vs. White | −.077 | .251 | −.010 | .880 |
| Multiple race/ethnicity vs. White | .212 | .004* | .283 | <.001* |
| Other race/ethnicity vs. White | .072 | .274 | .065 | .302 |
| BMI | .092 | .282 | .048 | .569 |
| Total IE | −.442 | <.001* | - | - |
| Unconditional Permission | - | - | −.319 | <.001* |
| Physical Reasons | - | - | −.383 | <.001* |
| Hunger Reliance | - | - | .053 | .469 |
| Congruence | - | - | −.085 | .284 |
Note:
Significant at p < .05; BMI = body mass index;
Unconditional Permission = Intuitive Eating Scale-2 Unconditional Permission to Eat subscale score; Physical Reasons = Intuitive Eating Scale-2 Eating for Physical Rather than Emotional Reasons subscale score;
Hunger Reliance = Intuitive Eating Scale-2 Reliance on Hunger and Satiety Cues subscale score; Congruence = Intuitive Eating Scale-2 Body-Food Choice Congruence subscale score;
Only covariates (age, sex, race/ethnicity, BMI) were entered on Step 1. For parsimony, specific beta coefficients of covariates are only presented for Step 2.
Sex was coded as follows: 0=Male, 1=Female
Race/Ethnicity was dummy coded with “White” as the reference group (i.e., White=0).
Moderation Analyses.
BMI emerged as a significant moderator in the relationship between total IE and Body Concern (b = .079, p = .011), with the interaction term displaying a small effect (f2 = .05). Specifically, a significant negative relationship between total IE and Body Concern was observed at healthy weight (b = −2.10, p < .001), overweight (b = −1.58, p < .001), Class I obesity (b = −1.19, p < .001), and Class II obesity levels (b = −.79, p = .005). However, the relationship between IE and Body Concern was non-significant at Class III obesity level (b = −.39, p = .314). Overall, it was observed that the slope of the negative relationship between IE and Body Concern decreased in magnitude with increasing BMI, as indicated by the differences in slopes and significance levels of the regression lines. Notably, the Class III obesity cell size was small (n=13), and therefore may have been underpowered, though the non-significant result is consistent with the pattern of decreasing slopes with increasing obesity severity. The results of this moderation analysis are depicted in Figure 1.
Figure 1. Simple Slopes Analysis of BMI Status as a Moderator of the Relationship between Intuitive Eating and Body Concern.
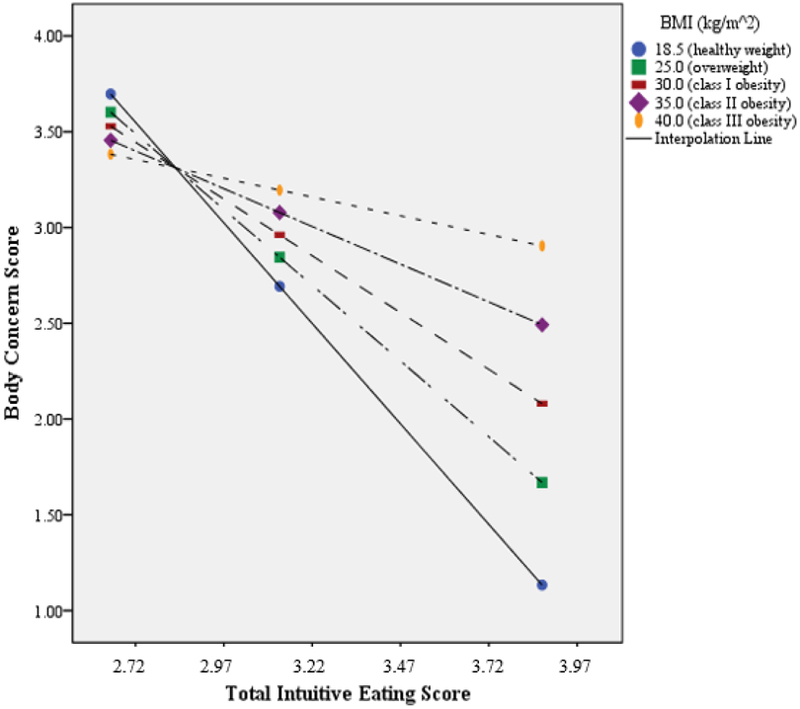
Note: BMI = body mass index
To follow-up on the significant interaction between total IE and BMI, moderation analyses were performed for IE subscales that displayed significant associations with Body Concern in the primary regression analysis (i.e., Unconditional Permission, Physical Reasons). The relationship between Unconditional Permission and Body Concern was significantly moderated by BMI (b = .060, p = .004) and the effect size was small (f2 = .07). Significant negative associations between Unconditional Permission and Body Concern were specifically observed at healthy (b = −1.31, p<.001), overweight (b = −.92, p < .001), and Class I obese BMIs (b= −.62, p < .001), whereas the relationship was non-significant at Class II (b = −.31, p = .112) and Class III obese BMIs (b = −.01, p = .961). As with the total IE scores, the magnitude of the Unconditional Permission-Body Concern relationship was greatest at healthy BMI levels and decreased with increasing BMI, becoming non-significant for those with Class II and III obesity.
The relationship between Physical Reasons and Body Concern was also significantly moderated by BMI (b = .038, p = .023) with a small effect size (f2 = .04) and showed a similar pattern of effects. Physical Reasons and Body Concern displayed a significant negative relationship for those at healthy weight (b = −1.21, p < .001), overweight (b = −.96, p < .001), Class I obesity (b = −.77, p < .001), and Class II obesity levels (b = −.58, p < .001), but at not Class III obesity levels (b = −.39, p = .061). Once again, the magnitude of the relationship displayed a decrease with increasing BMI as consistent with previous analyses.
No significant interaction between total IE and race-ethnicity (i.e., white vs. racial/ethnic minority status) was observed in association with Body Concern (b = −.16, p = .685). Likewise, total IE and sex (i.e., male vs. female) did not display a significant interaction in association with Body Concern (b = −.02, p = .966). Neither of the magnitudes of these analyses met the threshold for at least a small effect (f2 < .02).
Discussion
The primary objective of this study was to determine whether IE was associated with body image after controlling for objective BMI. Findings revealed that higher levels of IE were associated with lower levels of shape and weight concerns – independent of BMI – such that eating more intuitively was related to less concern with body shape and weight, regardless of an individual’s actual BMI. Two of the IE subscales – Unconditional Permission and Physical Reasons – were uniquely associated with body image. Therefore, it appears that giving oneself permission to eat freely and eating based on hunger instead of emotion(s) may be the most important aspects of IE in this relationship.
The finding that eating intuitively is associated with one’s views of his/her body is supported by many previous studies. In particular, numerous interventions have found that IE (or related non-diet approaches) leads to improved body image, either through increased body appreciation or decreased body dissatisfaction [7-11]. Further, the acceptance model of IE [4-6] suggests that body appreciation contributes to the development of IE behaviors. However, these studies have neglected to consider the role of BMI in these relationships, even though it has been associated with both constructs [14-16]. This study contributes to previous literature by displaying that IE was uniquely associated with body image, even after controlling for the effects of an individual’s objective BMI. This finding suggests that IE is a distinctive construct, such that the benefits are IE are not due to the fact that individuals with high IE tend to have lower weights.
Despite the fact that objective BMI did not explain or eliminate the association between IE and body image, BMI did emerge as an important moderator of the relationship. In contrast, no differential associations between IE and body image were observed for male vs. female or white vs. racial/ethnic minority status individuals. The relationship between IE and body image was strongest in individuals of the lowest BMI in our sample (i.e., healthy weight individuals). This pattern was true for both the unconditional permission to eat scale (Unconditional Permission) and the eating for physical vs. emotional reasons scale (Physical Reasons). In individuals of the highest BMI (i.e., those with Class III obesity), the relationship between Physical Reasons and body image was non-significant; further, the relationship between Unconditional Permission and body image was non-significant in individuals with Class II or III obesity. This suggests that eating for physical rather than emotional reasons and giving oneself unconditional permission to eat when and what is desired is only positively related to body image up to a certain BMI.
As IE displayed differential effects based on objective BMI, it is important to understand the nuances in this relationship specific to each weight category. Eating for physical – rather than emotional – reasons is most strongly related to weight/shape concerns in individuals of a healthy weight, with the relationship becoming weaker and eventually non-significant in class III obesity. This effect could indicate that though eating for physical need is generally helpful, it becomes more difficult at higher BMIs due to the decreased satiety and heightened hunger signaling commonly observed in obesity [23, 24]. Eating for physical need may only be useful if one’s physiological signals are not dysregulated by excess adiposity and/or metabolic impairment. Of note, giving oneself unconditional permission to eat is no longer associated with body image in individuals with Class II obesity or greater. This could be due to differences in what this subscale might be measuring at various BMI levels. For instance, the quality and/or quantity of food being consumed by individuals at various weight statuses may differ even if each group is giving themselves unconditional permission to eat when and what is desired.
Accordingly, there may be clinical and research implications of these results. For example, IE could be a useful intervention tool for individuals with impaired body image, helping them develop a healthier view of their bodies and preventing the development of eating pathology. Alternatively, we may be able to target individuals’ views about their bodies in order to help them eat more intuitively, which could be helpful in weight maintenance or obesity prevention. In all of these cases, though, we must consider weight status. Based on the current findings, it appears that IE or body image treatments may be most effective for individuals of healthy weight, implicating their potential utility for the prevention of obesity development. However, prospective studies are needed to understand the relationships between eating intuitively, body image, and BMI over time.
Though this study expounded upon the role of objective BMI in the IE-body image relationship, the directionality and mechanisms of the relationship still are largely unknown [4-6, 25]. There are several conceptualizations of how this relationship may function in either direction: Perhaps having less concern with one’s shape and weight allows a person to be more in tune with his/her internal hunger signals, differentiating them from emotional cues, and also allows a person to give him/herself permission to freely eat when and what is desired [6]. Likewise, perhaps being concerned with one’s body shape/weight disrupts the ability to eat freely and based on physical reasons. Conversely, maybe frequent eating for non-physical (i.e., emotional) reasons or frequently engaging in external dietary restraint leads a person to become concerned with his/her body shape and weight. Otherwise stated, maybe a person who eats intuitively, displaying a trust in his/her body to know when and what to eat, will tend to be less concerned with his/her body shape and weight. An investigation of mediators is needed in order to understand the mechanisms of these relationships and how best to apply these concepts. When considering these possible conceptual mechanisms, though, one must remember that the IE-body image relationship may not be the same for all individuals.
In addition to the discussed bidirectionality between IE and body image, the observed interrelationships between IE, BMI, and body image raise further complexities, such as whether IE may moderate the relationship between BMI and body image. In short, there is much to be learned about the relationships between these factors, and more robust, non-cross-sectional study designs are needed to empirically explore the options. Longitudinal studies that assess changes in all three of these variables (i.e., IE, BMI, and body concern) utilizing mixed models to determine how change in one impacts the others are essential to untangling the complex relationships between these variables and their corresponding pathways.”
Though this study made an important contribution to the literature, it had limitations that should be addressed. Firstly, due to the cross-sectional study design no conclusions about the directionality or causality of the relationships between IE, BMI, and body image may be drawn. Secondly, the use of data collected for larger, ongoing studies did not allow for the measurement of specific covariates that would be useful additions to this study (e.g., perceived weight status) [26, 27]. In addition, the specific aspect of body image that this study considered was body concern, so results may vary if body image was defined and measured in a different way (e.g., body dissatisfaction, body appreciation). Further, while BMI is a commonly used measure of weight status, it is not as accurate as more advanced techniques (e.g., dual-energy X-ray absorptiometry) for determining actual adiposity levels. Additionally, the current study may not have been adequately powered to detect interaction effects between IE and sex or race-ethnicity. While the observed effect sizes (f2 < .02) suggest that any significant effects may be limited in their clinical utility, better-powered studies should be utilized in order to fully assess the role of potential demographic moderators of the IE-body image relationship. With larger sample sizes and greater participant diversity, future studies should also utilize more nuanced and culturally-sensitive coding metrics as opposed to the current approach of white vs. racial/ethnic minority status. Lastly, this study consisted of a nonclinical sample, so these results should be replicated in a population that includes individuals with clinically significant levels of weight and shape concerns.
In conclusion, this study found that eating intuitively – particularly giving oneself unconditional permission to eat and eating for physical, rather than emotional, reasons – was uniquely associated with lower levels of body concern, or a more positive body image in a sample of adults. Further, it was found that these relationships were strongest in individuals of a healthy weight. These findings support previous literature and contribute evidence that BMI is important to consider in the IE-body image relationship. However, the questions of directionality and causality still stand. With future research, IE- or body image-based interventions may be powerful tools for improving physical health and mental well-being through obesity and eating disorder prevention and/or weight loss maintenance.
Supplementary Material
Highlights.
Intuitive eating (IE) was associated with less negative body image, adjusting for measured BMI.
Unconditional Permission & Physical Reasons were the most important facets in this relationship.
The IE-body image relationship was strongest at healthy weight and decreased with increasing BMI.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interests: none.
References
- 1.Tribole E and Resch E, Intuitive eating: A revolutionary program that works. 2012: Macmillan [Google Scholar]
- 2.Tylka TL and Kroon Van Diest AM, The Intuitive Eating Scale–2: Item refinement and psychometric evaluation with college women and men. Journal of Counseling Psychology, 2013. 60(1): p. 137. [DOI] [PubMed] [Google Scholar]
- 3.Bruce LJ and Ricciardelli LA, A systematic review of the psychosocial correlates of intuitive eating among adult women. Appetite, 2016. 96: p. 454–472. [DOI] [PubMed] [Google Scholar]
- 4.Augustus-Horvath CL and Tylka TL, The acceptance model of intuitive eating: a comparison of women in emerging adulthood, early adulthood, and middle adulthood. Journal of Counseling Psychology, 2011. 58(1): p. 110. [DOI] [PubMed] [Google Scholar]
- 5.Tylka TL and Homan KJ, Exercise motives and positive body image in physically active college women and men: Exploring an expanded acceptance model of intuitive eating. Body image, 2015. 15: p. 90–97. [DOI] [PubMed] [Google Scholar]
- 6.Avalos LC and Tylka TL, Exploring a model of intuitive eating with college women. Journal of Counseling Psychology, 2006. 53(4): p. 486. [Google Scholar]
- 7.Bacon L, et al. , Evaluating a" non-diet'wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. International Journal of Obesity, 2002. [DOI] [PubMed] [Google Scholar]
- 8.Bacon L, et al. , Size acceptance and intuitive eating improve health for obese, female chronic dieters. Journal of the American Dietetic Association, 2005. 105(6): p. 929–936. [DOI] [PubMed] [Google Scholar]
- 9.Bush HE, et al. , Eat for life: a work site feasibility study of a novel mindfulness-based intuitive eating intervention. American Journal of Health Promotion, 2014. 28(6): p. 380–388. [DOI] [PubMed] [Google Scholar]
- 10.Humphrey L, Clifford D, and Morris MN, Health at every size college course reduces dieting behaviors and improves intuitive eating, body esteem, and anti-fat attitudes. Journal of nutrition education and behavior, 2015. 47(4): p. 354–360. e1. [DOI] [PubMed] [Google Scholar]
- 11.Cole RE and Horacek T, Effectiveness of the My Body Knows When intuitive-eating pilot program. American journal of health behavior, 2010. 34(3): p. 286–297. [DOI] [PubMed] [Google Scholar]
- 12.Schaefer JT and Magnuson AB, A review of interventions that promote eating by internal cues. Journal of the Academy of Nutrition and Dietetics, 2014. 114(5): p. 734–760. [DOI] [PubMed] [Google Scholar]
- 13.Cadena-Schlam L and López-Guimerà G, Intuitive eating: an emerging approach to eating behavior. Nutrición hospitalaria, 2014. 31(3): p. 995. [DOI] [PubMed] [Google Scholar]
- 14.Van Dyke N and Drinkwater EJ, Review article relationships between intuitive eating and health indicators: literature review. Public health nutrition, 2014. 17(08): p. 1757–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rø Ø, Reas DL, and Rosenvinge J, The impact of age and BMI on Eating Disorder Examination Questionnaire (EDE-Q) scores in a community sample. Eating behaviors, 2012. 13(2): p. 158–161. [DOI] [PubMed] [Google Scholar]
- 16.Swami V, Hadji-Michael M, and Furnham A, Personality and individual difference correlates of positive body image. Body image, 2008. 5(3): p. 322–325. [DOI] [PubMed] [Google Scholar]
- 17.Fallon EA, Harris BS, and Johnson P, Prevalence of body dissatisfaction among a United States adult sample. Eating behaviors, 2014. 15(1): p. 151–158. [DOI] [PubMed] [Google Scholar]
- 18.Chithambo TP and Huey SJ, Black/white differences in perceived weight and attractiveness among overweight women. Journal of Obesity, 2013. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkins MA, et al. , Cognitive and Self-regulatory Mechanisms of Obesity Study (COSMOS): Study protocol for a randomized controlled weight loss trial examining change in biomarkers, cognition, and self-regulation across two behavioral treatments. Contemporary clinical trials, 2018. 66: p. 20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawkins MA, NCT02786238. 2016. [Google Scholar]
- 21.Fairburn CG and Beglin SJ, Assessment of eating disorders: Interview or self- report questionnaire? International journal of eating disorders, 1994. 16(4): p. 363–370. [PubMed] [Google Scholar]
- 22.CDC. Defining Adult Overweight and Obesity. Overweight and Obesity 2016 June 16, 2016. [cited 2017 May 11, 2017]. [Google Scholar]
- 23.Sumithran P, et al. , Long-Term Persistence of Hormonal Adaptations to Weight Loss. New England Journal of Medicine, 2011. 365(17): p. 1597–1604. [DOI] [PubMed] [Google Scholar]
- 24.Sumithran P and Proietto J, The defence of body weight: a physiological basis for weight regain after weight loss. Clinical Science, 2013. 124(4): p. 231–241. [DOI] [PubMed] [Google Scholar]
- 25.Schoenefeld SJ and Webb JB, Self-compassion and intuitive eating in college women: Examining the contributions of distress tolerance and body image acceptance and action. Eating Behaviors, 2013. 14(4): p. 493–496. [DOI] [PubMed] [Google Scholar]
- 26.Daly M, Robinson E, and Sutin AR, Does knowing hurt? Perceiving oneself as overweight predicts future physical health and well-being. Psychological science, 2017. 28(7): p. 872–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haynes A, et al. , A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. 2018. p. 347–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


