A 70-year-old Spanish man was referred to our emergency room (ER) for acute generalized epileptic seizures, which had developed over the previous 24 h. Two years before, the patient had been diagnosed with multiple nocardial brain abscesses that had been successfully treated without recurrence and complications during follow-up. The patient’s medical history also included type 2 diabetes mellitus, high blood pressure, persistent lymphopenia (CD4 T lymphocyte count of 120 cells/µl), and hypogammaglobulinemia, with a bone marrow biopsy with no significant findings. Seven months prior to this admission, he had undergone liver transplantation due to presinusoidal portal hypertension without clear filiation. The immunosuppressive treatment included prednisone, tacrolimus, and mycophenolate mofetil. He also received trimethoprim-sulfamethoxazole prophylaxis.
The patient reported a 7-day persistent fever. He did not complain of headache or mention other neurological symptoms. He had no history of head trauma. The results of the physical examination, including a neurological examination, were unremarkable. Laboratory test results revealed a leukocyte count of 4,700 cells/µl with 800 lymphocytes/µl. The C-reactive protein level was 7.6 mg/dl. The serum creatinine level was within the normal range, but liver function was altered, with elevated gamma-glutamyl transpeptidase (754 U/liter) and alkaline phosphatase (714 U/liter). While in the ER, he suffered a new generalized tonic-clonic seizure. A magnetic resonance imaging (MRI) of the head demonstrated the presence of an epidural abscess with osteomyelitis of the frontal bone (Fig. 1A). The patient was admitted to the hospital for further evaluation, and treatment with levetiracetam and meropenem was prescribed. Surgical drainage of the epidural abscess was performed. A sample was sent to the microbiology laboratory for staining and bacterial (aerobic and anaerobic), fungal, and mycobacterial culture. Based on the Gram stain (Fig. 1B), Ziehl-Neelsen and direct auramine-rhodamine stains of the sample were performed (Fig. 1C and D). Seven days later, the causative pathogen was isolated on culture.
FIG 1.
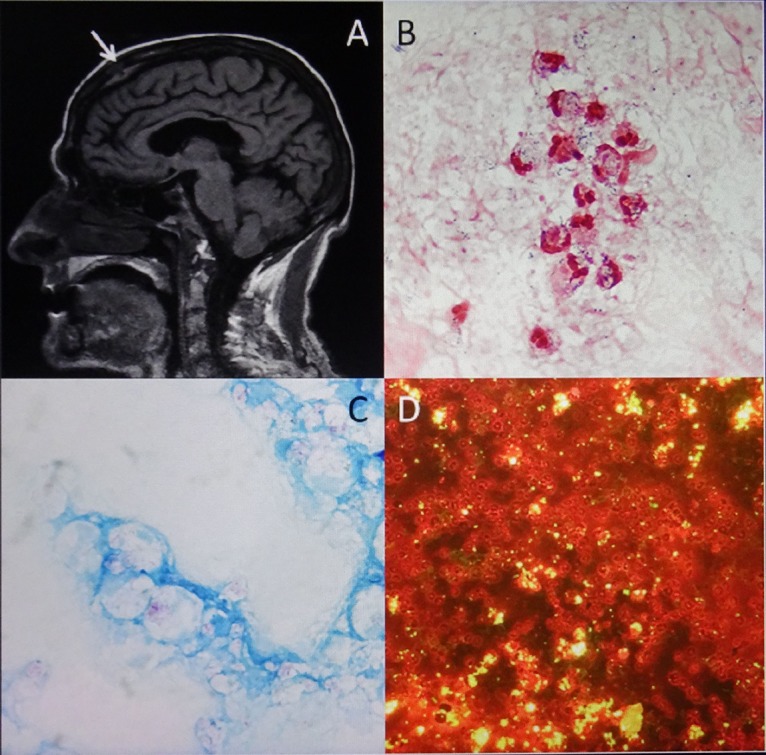
(A) MRI of the head, revealing epidural abscess with osteomyelitis of the frontal bone (arrow). (B, C, D) Direct Gram stain (magnification, ×1,000), Ziehl-Neelsen stain (magnification, ×1,000), and auramine-rhodamine stain (magnification, ×200) of the epidural abscess specimen.
For answer and discussion, see https://doi.org/10.1128/JCM.00649-18 in this issue.


