Chikungunya virus (CHIKV) is an alphavirus that is primarily transmitted by Aedes species mosquitoes. Though reports of an illness consistent with chikungunya date back over 200 years, CHIKV only gained worldwide attention during a massive pandemic that began in East Africa in 2004.
KEYWORDS: Chikungunya virus, alphavirus, molecular diagnostics, serology, viral culture
ABSTRACT
Chikungunya virus (CHIKV) is an alphavirus that is primarily transmitted by Aedes species mosquitoes. Though reports of an illness consistent with chikungunya date back over 200 years, CHIKV only gained worldwide attention during a massive pandemic that began in East Africa in 2004. Chikungunya, the clinical illness caused by CHIKV, is characterized by a rapid onset of high fever and debilitating joint pain, though in practice, etiologic confirmation of CHIKV requires the availability and use of specific laboratory diagnostics. Similar to infections caused by other arboviruses, CHIKV infections are most commonly detected with a combination of molecular and serological methods, though cell culture and antigen detection are reported. This review provides an overview of available CHIKV diagnostics and highlights aspects of basic virology and epidemiology that pertain to viral detection. Although the number of chikungunya cases has decreased since 2014, CHIKV has become endemic in countries across the tropics and will continue to cause sporadic outbreaks in naive individuals. Consistent access to accurate diagnostics is needed to detect individual cases and initiate timely responses to new outbreaks.
INTRODUCTION
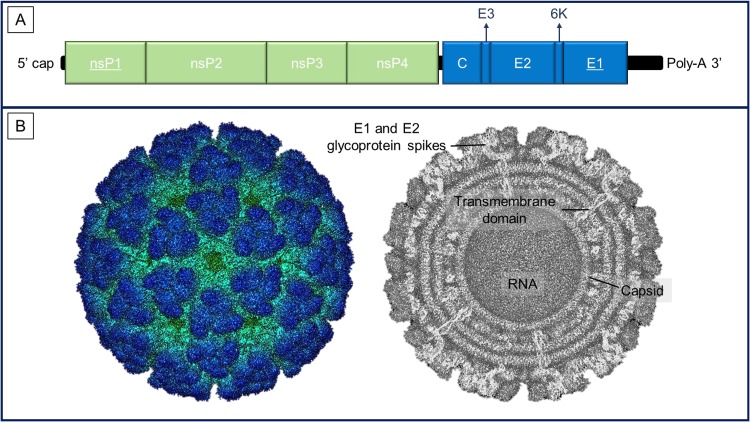
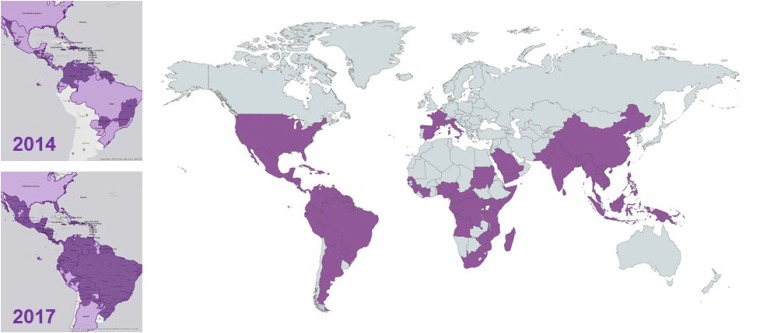
Chikungunya virus (CHIKV) is one of over 30 known viral species in the genus Alphavirus (family Togaviridae). The alphaviruses are enveloped, single-stranded, positive-sense RNA viruses with a genome of approximately 11.8 kb that encodes five structural proteins (capsid, E3, E2, 6K, and E1) and four nonstructural proteins (nsP1, nsP2, nsP3, and nsP4) (Fig. 1) (1, 2). CHIKV is primarily transmitted to humans by the Aedes species mosquitoes Aedes aegypti and Aedes albopictus, though rare reports of blood-borne transmission have been documented (3). Outbreaks had occurred in several countries throughout Africa, Southeast Asia, and Polynesia, but the CHIKV pandemic that began in East Africa in 2004 brought this previously obscure arbovirus to prominence and is unrivaled among pandemics caused by the alphaviruses in terms of size and geographic distribution (Fig. 2) (1, 2).
FIG 1.
(A) Diagram of the CHIKV genome indicating the relative length of the genes encoding nonstructural (green) and structural (blue) proteins. CHIKV molecular diagnostics have predominantly targeted the nsP1 and E1 genes (underlined), accounting for 10 and 14 of the 32 assays referenced in this review, respectively. (B) The structure of the CHIKV virion determined by electron microscopy is shown, highlighting the E1/E2 glycoprotein spikes on the virion surface, transmembrane domains, and the viral capsid (republished from PDBj.org under the Creative Commons Attribution 4.0 International license [190, 191]).
FIG 2.
Countries with autochthonous cases of CHIKV (reported through 16 May 2018, dark purple). Inset maps display the geographical spread of CHIKV in the Americas between 2014 and 2017, though overall case numbers decreased ∼6-fold during this time period. Regions in dark purple reported autochthonous CHIKV transmission at any time through the year shown. Light purple highlights countries with any CHIKV transmission. Countries in gray had no autochthonous cases; asterisks represent imported cases. Maps were modified from those available at CDC.gov and PAHO.org. Notably, the categorization of Cuba differs between these sources, as autochthonous cases have not been reported to PAHO.
CHIKV causes a higher rate of symptomatic infection than other widespread arboviruses, such as dengue virus (DENV) and Zika virus (ZIKV), though there is evidence that the incidence of symptoms is lineage dependent (4, 5). The reported incubation period for CHIKV ranges from 1 to 12 days, and symptomatic infection typically presents as fever and arthralgia, though less common presentations have been described (1, 2, 6). The diagnosis of a CHIKV infection cannot be confirmed based solely on clinical findings (7, 8). Similar to other arboviruses, confirmation is achieved through the use of molecular and/or serological methods, though CHIKV can be isolated in culture, and antigen-based detection has been reported. This review provides an overview of the available CHIKV diagnostics and highlights aspects of basic virology and epidemiology that pertain to viral detection. As a point of clarification, throughout this review the term chikungunya is used to refer to the clinical illness and CHIKV is used to refer to the virus.
HISTORY AND TRANSMISSION
Descriptions of an illness compatible with chikungunya date back to 1779, including potential outbreaks in the Western Hemisphere (9–11), but CHIKV was not identified until the 1950s in what is now southern Tanzania (1, 6, 12). Occasional outbreaks also occurred in Asia from the late 1950s through the latter 20th century (1, 12–14). Phylogenetic studies initially identified three CHIKV lineages: the West African, East/Central/South African (ECSA), and Asian lineages(15, 16). However, in 2004, the Indian Ocean lineage (IOL) emerged from an ECSA strain and caused a large outbreak that began in coastal Kenya and spread to the Comoros, La Réunion, and islands of the Indian Ocean (Fig. 2) (12, 13). This new lineage spread across Asia and the South Pacific, with smaller outbreaks occurring in Western Europe following introductions by returned travelers (12, 17–19). In late 2013, the first cases of chikungunya were identified in St. Martin, and CHIKV quickly spread throughout the Caribbean and the Americas (20). This outbreak was almost exclusively caused by Asian lineage strains, with a small number of ECSA lineage infections being reported in Brazil (12, 14, 21). Although the number of cases declined markedly from 2014 to 2017, CHIKV transmission continues in the Americas (PAHO.org), and outbreaks occur in Asia and Africa, with autochthonous cases being documented in Italy as recently as 2017 (22).
During an outbreak, CHIKV is maintained in a human-mosquito-human cycle of transmission by A. aegypti and A. albopictus mosquitoes, in a pattern similar to that for DENV (1, 23). Attack rates have been relatively low in temperate regions (24), but rates as high as 50 to 75% have been reported during outbreaks in the tropics (25–27). Such high attack rates help explain the occurrence of human coinfections with CHIKV, DENV, and/or ZIKV, which have been reported from the Americas and Asia (7, 28–33), and individuals with these coinfections may present with more severe manifestations (7, 30). A meta-analysis of available publications on CHIKV coinfections revealed that CHIKV-DENV coinfections were most common (44/109 studies), but CHIKV-malaria coinfections were reported in several studies (5/109) (28, 29, 34). During interepidemic periods, CHIKV may be maintained by other mechanisms, leading to persistence in a region and the potential for sporadic outbreaks (35–38).
CHIKV transmission has occurred in regions of endemicity for related alphaviruses, such as O’nyong-nyong virus (ONNV), Mayaro virus (MAYV), Venezuelan equine encephalitis virus (VEEV), and Ross River virus (RRV). Cross protection between alphaviruses has been documented in animal models (39, 40) and humans following natural infection (41) or sequential vaccination (42). In addition to cross protection, there are limited data on the potential for antibody-dependent enhancement (ADE) of alphavirus infections, with in vitro studies of RRV (43, 44) and Sindbis virus (45) suggesting ADE of alphaviruses at low antibody titers. In mice immunized against CHIKV, low IgG titers enhanced CHIKV infection (46, 47), but vaccine-elicited antibodies after RRV vaccination did not enhance CHIKV or RRV infection even at low titers (48). ADE from prior alphavirus exposures has not been documented in human infection (44), and the clinical significance of these experimental findings remain unclear.
ACUTE CLINICAL PRESENTATION AND DIFFERENTIAL DIAGNOSIS
Although it has been reported that a high proportion of CHIKV infections are symptomatic (80 to 97%) (1, 27, 49–51), the ratio of symptomatic to inapparent CHIKV infections (S/I ratio) has varied markedly in the literature (5, 27, 52–56). Factors associated with the S/I ratio include the presence of preexisting neutralizing antibodies to CHIKV (52, 55) and patient age (52, 54, 56, 57). Notably, both negative (54, 57) and positive (52) associations between age and symptomatic infection have been reported. Finally, the S/I ratio appears to be lineage dependent. In a recent reevaluation of the literature, it was found that ∼50% of infections with Asian lineage CHIKV strains versus ∼80% of infections with ECSA lineage strains (predominantly IOL strains) result in symptomatic infections (5). Insufficient data are currently available to estimate the S/I ratio for infections with CHIKV strains of the West African lineage.
The classic triad of symptomatic chikungunya includes an abrupt-onset febrile illness, severe and often debilitating arthralgias, and a rash (Fig. 3) (1, 2, 6). Clinical disease evolves rapidly, and symptomatic patients may present within 2 to 3 days of symptom onset (1, 25, 58–61). Fever can be marked (39 to 40°C) and occurs in the majority of cases (80 to 90%), including atypical cases (62). Arthralgia develops around the time of fever onset and is reported at presentation in 85 to 90% of cases (8, 25, 57–60, 63, 64). Joint involvement is bilateral, though not always symmetric, and most commonly involves the knees, ankles, and joints of the upper extremities (metacarpophalangeal, interphalangeal, and metatarsal joints, elbows, and shoulders) (25, 58, 65, 66). Arthritis with joint swelling and tenderness occurs in ∼30% of cases (25, 65, 67). A skin rash develops in 40 to 60% of cases (1, 2, 25, 64, 65, 68, 69), though this may not be present at the initial visit (65, 70). Rashes are most often maculopapular and may be pruritic, though bullous and purpuric lesions have been reported (8, 25, 62, 69). Headache and gastrointestinal complaints, such as anorexia, nausea, vomiting, and abdominal pain, are also commonly reported in chikungunya cases (25, 57, 65, 66, 69). Hemorrhagic manifestations, however, are rare (∼5% of cases) (25, 59, 67, 71).
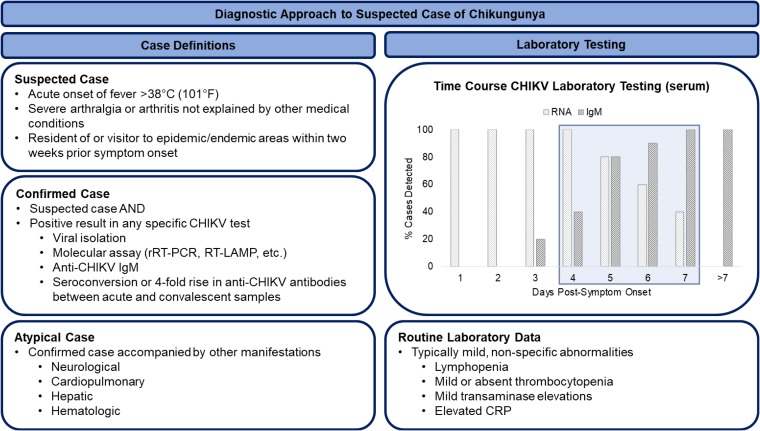
FIG 3.
Case definitions and diagnostic approach to suspected chikungunya cases. The proposed time course for CHIKV diagnosis using serum was derived from published reports (103–106). The sensitivity of RNA detection in serum declines between days 4 and 7 as anti-CHIKV IgM becomes detectable. Anti-CHIKV IgG may become detectable at a similar time point (105). RT-LAMP, reverse transcription–loop-mediated isothermal amplification; CRP, C-reactive protein.
Host factors also affect the clinical presentation of CHIKV infections. It has been observed that young children present with arthralgia less frequently than older children and adults (52, 54, 57, 72). Patients older than 65 years of age may present a more complicated clinical picture during acute chikungunya, with more frequent manifestations other than arthralgia, including high rates of neurological complaints (73). Limited data are available from immunocompromised hosts, but chikungunya manifestations and severity do not appear to differ among solid organ transplant recipients (74). Atypical chikungunya cases, defined as cases with predominant manifestations other than fever and arthralgia, have been reported (Fig. 3) and are estimated to occur in ∼1% of symptomatic cases (62, 75). The incidence of severe and atypical disease has a bimodal distribution, with peaks occurring among neonates and older adults, who often have comorbid illnesses (57, 62, 64, 72, 75). In a large series of such cases from La Réunion, patients with cardiovascular disease (heart failure, arrythmias, and pericarditis) and neurological disease accounted for >50% of individuals with atypical cases (62). Neurological manifestations have included meningoencephalitis, Guillain-Barré syndrome, optic neuropathy, and retinitis, among others (33, 62, 75).
Clinical diagnosis does not reliably differentiate CHIKV infections from other etiologies on the differential, such as other alphaviruses (MAYV, ONNV), flaviviruses (most commonly DENV and ZIKV), and nonviral pathogens, which include, but are not limited to, Plasmodium species, Leptospira, rickettsia, and Salmonella. In settings of CHIKV cotransmission with DENV and ZIKV, a presumptive diagnosis of chikungunya was correct in only 10 to 40% of cases (7, 8, 31). Clinical prediction algorithms have been evaluated to differentiate CHIKV infections from infections with other etiologies, but these have not been independently validated in separate cohorts (59, 63, 66, 72, 76). Results from routine laboratory tests are generally not specific for chikungunya. Abnormal results that have been observed in cases include lymphopenia (<500 to <1,000 × 106 lymphocytes/liter) without leukopenia, mild thrombocytopenia (>100,000 × 106 platelets/liter), mild transaminase elevations (transaminase levels 2 to 3 times the upper limit of normal), and an elevated C-reactive protein level (Fig. 3) (25, 59, 60, 66, 71). Moderate to severe thrombocytopenia favors the diagnosis of dengue rather than chikungunya, particularly if hemorrhagic signs are present (59, 60, 66, 76). However, these laboratory findings occur in other diseases on the differential and do not provide accurate diagnostic information.
CHIKV DIAGNOSTICS
Biosafety.
CHIKV is a risk group 3 pathogen and requires biosafety level 3 (BSL-3) precautions, based on a number of cases associated with laboratory exposures (77, 78), and it is a category C priority pathogen according to the National Institute of Allergy and Infectious Diseases (NIAID) (79). CHIKV infections among laboratory personnel from fieldwork, work with infected mosquitoes, and isolation of live virus from field materials have been reported (80, 81). There have been no case reports of laboratory transmission from blood products; however, a nurse reported acquiring CHIKV by drawing the blood of an infected patient (80). As such, continued caution is recommended when handling infected blood products or live virus in the laboratory due to the potential for transmission. These factors have limited the number of facilities that can safely work with live virus and impacted the testing that is currently available.
Because of the geographic spread of CHIKV, diagnostic approaches that can be practiced in available, low-biosafety-level facilities are needed. As whole-virus preparations are needed for many applications, such as the plaque reduction neutralization test (PRNT), varied strategies of viral inactivation have been studied. It has been reported that standard heat inactivation protocols with a 30-min incubation at 56°C are insufficient for CHIKV, which may require incubations over 2 h to be fully inactivated (82). Complete inactivation of CHIKV was achieved by 1,5-iodonaphthyl azide (INA) treatment. However, a reduction in the capacity to bind to anti-CHIKV antibodies was observed (83). Recent work showed that treatment with UV at 0.09 J/cm2 was sufficient to inactivate an Asian strain of CHIKV. The resulting inactivated virus was replication deficient, but the procedure did not affect the integrity of the virus, and structural epitopes were unaltered (84).
Viral culture.
Despite their use for decades as the “gold standard” for viral detection in clinical virology, cell culture and viral isolation are no longer commonly used for routine diagnostic purposes (85). The procedure requires time for viral growth and subsequent identification as well as specialized equipment and skilled laboratory staff for performance (86). However, the benefit of cell culture is that it allows for biological amplification of the virus and the isolation of strains from human infections. These isolates permit further characterization of viral species and provide invaluable resources to clarify immune responses and perform fundamental basic virology research with contemporaneous strains (86, 87).
Although molecular methods, detailed below, provide a highly sensitive means of detection, false negatives may occur in specimens with low levels of virus, reverse transcription-PCR (RT-PCR) inhibitors, or strains that harbor mutations in target regions. Inoculation of suspected arbovirus-containing human samples onto cell cultures may allow for replication of the virus to high titers, followed by confirmation using immunofluorescence or RT-PCR (6, 88, 89). Furthermore, the semiunbiased nature of viral culture has allowed detection of coinfections with unexpected viral pathogens while simultaneously documenting that these are replicating viruses in the human host (90, 91). The isolation of CHIKV can be performed from serum collected up to 7 days after illness onset, and the virus has also been isolated from human cerebrospinal fluid (CSF) (92) and pools of adult female A. aegypti mosquitoes (93).
Both mosquito and mammalian cell culture systems have been used to isolate CHIKV and study viral replication and pathogenesis (79, 94). It has been shown that CHIKV establishes a persistent noncytopathic infection in A. albopictus C6/36 mosquito cells, while it causes strong cytopathic effects (CPE) and apoptosis in mammalian cells (94–96). CHIKV culture in C6/36 cells permits viral titers that are 100-fold higher than those in Vero cells, though C6/36 cells may not be readily available in clinical diagnostic laboratories (95). In addition to Vero cells (93, 97), CHIKV has been isolated on other mammalian cell lines, including LLC-MK2 (90), BHK-21 (98, 99), and 293T (100) cells. Also, a combination of successive passages in different cell types has been described (101). Notably, C6/36 cell lines are significantly more permissive for more recent CHIKV isolates, suggesting that the increased infectivity and the recent epidemic may derive from evolution of the CHIKV genome beyond simply the E1-A226V substitution (101).
Molecular testing.
Molecular testing remains central to the confirmation of chikungunya (Fig. 3). The viral load in acute CHIKV infections can exceed 11.0 log10 copies/ml of serum, particularly in neonates (7, 70, 102), and the sensitivity of RNA detection remains high through the first 4 to 5 days of illness in most series (103–107). A variety of molecular assays for CHIKV have been published or are commercially available (see Table S1 in the supplemental material). Reported assays include conventional RT-PCR (69, 108–112), real-time RT-PCR (rRT-PCR) (102, 105, 113–120), isothermal methods (110, 121–124), and multiplex assays (125–138). No molecular gold standard by which to evaluate reported assays in practice exists, and the decision to implement a particular test depends on the relative advantages and disadvantages of the method along with the capabilities in a given laboratory.
Consistent with molecular diagnostics in general, real-time methods for CHIKV have proven more sensitive than conventional RT-PCR (112, 115, 116, 121), though this has not been shown in all studies (111). Comparisons between real-time methods have not demonstrated clear differences in assay performance (105, 118, 124, 132, 136), and CHIKV detection in published multiplex assays does not appear to be decreased relative to that in monoplex tests (125, 126, 133, 135, 137, 138). Multiplex assays facilitate testing for a set of pathogens in all patients, and the utility of this approach has been demonstrated in regions with transmission of multiple arboviruses and/or malaria (7, 34). Evaluations of assay exclusivity have been variable. At a minimum, CHIKV molecular tests should be evaluated against DENV, ZIKV, and a panel of alphaviruses that includes MAYV and ONNV, which is the alphavirus most closely related to CHIKV and which may cross-react in molecular assays (124, 136).
Few independent comparisons of available molecular assays have been reported (106), and in a large external quality assessment (EQA) of molecular testing for CHIKV, laboratory performance was not associated with the use of a particular assay or commercial reagents (139). Notably, in this assessment, 50% of laboratories (30/60) failed to meet the acceptable performance standard (≤1 false-negative result and no false-positive results in a set of 12 samples) (139). These findings highlight the complexity of molecular testing in general and the ongoing need for assay harmonization across laboratories. An earlier study demonstrated that the distribution of a preformulated CHIKV rRT-PCR significantly improved sensitivity at participating sites (140). A molecular reference reagent has also been developed for use in the FDA approval process (141, 142), though no molecular test has received FDA approval for CHIKV detection, and use of this reagent outside of the development process has not been reported.
Serum and plasma are the most common specimen types used for CHIKV RNA detection, and all reported methods require nucleic acid extraction for optimal performance. One rRT-PCR using cell culture supernatants without extraction was evaluated, but it remains unclear if this protocol can be applied to clinical samples (114). Given the high viral loads observed in acute CHIKV infections, there has not been the impetus to evaluate alternative specimen types as has been done for ZIKV infections, where average viral loads are significantly lower (7). CHIKV RNA has been amplified from a large number of specimen types other than serum/plasma (143, 144), though most published data describe the testing of CSF, in which both CHIKV RNA and antigen have been detected (33, 143, 145, 146). The viral load in CSF appears to be lower than that in serum, but the duration of CHIKV RNA detection in CSF may be prolonged (143, 145). Finally, both dried blood spots and dried serum spots have been evaluated as specimen types for CHIKV RNA detection by rRT-PCR (147, 148). Both specimens demonstrated ∼93% sensitivity compared to serum, indicating that these represent a reasonable specimen for use in resource-limited areas or to improve patient acceptance of sample collection, such as with small children.
Serological testing.
Serological testing provides diagnostic information and valuable insight into the immune responses to CHIKV infection. CHIKV-specific IgM and IgG antibodies develop in response to infection, and several methods for the detection of these isotypes during the acute and convalescent phases of infection have been reported. Commercial and in-house enzyme-linked immunosorbent assays (ELISAs) to detect antibodies against whole viral antigen have been the preferred methods. Commercial ELISAs from several companies (including IBL, EuroImmun, InBios, and Abcam) have demonstrated acceptable performance (149), though these may cross-react with other alphaviruses, such as ONNV and MAYV (150). EQA studies of CHIKV serology have also been performed. These generally demonstrate poor sensitivity for anti-CHIKV IgM detection, though they demonstrated better performance for IgG assays (139, 151). In the most recent EQA, commercial IFAs offered the best sensitivity overall, and in-house ELISAs were more sensitive than commercial ELISAs (139).
IgM capture ELISAs may provide improved performance, and two separate groups have described in-house assays whose results demonstrated high concordance with PRNT results from the CDC (152, 153). PRNTs are highly accurate but labor-intensive and require BSL-3 facilities. Although rarely performed in clinical laboratories, PRNT remains in use for diagnosis when available due to its high specificity (103). Attempts have been made to develop versions of the PRNT using noninfectious virus replicon particles or chimeric viruses that do not require enhanced biosafety procedures (154, 155). Commercial, rapid diagnostic tests for anti-CHIKV IgM and IgG have been developed (e.g., SD Bioline and OnSite Chik) but have very low sensitivity and specificity (150, 156–158).
An important consideration for the use of serological testing is the extended duration of antibody detection following acute infection. CHIKV-specific IgM levels tend to peak at between 4 and 20 days after symptom onset, but these may not wane for 11 to 14 months (103) and CHIKV-specific IgM has been detected as late as 18 months postinfection by direct ELISA (143). Therefore, anti-CHIKV IgM detection in the acute phase of infection can provide only a presumptive diagnosis. CHIKV-specific IgG remains detectable long after infection and may indicate lifetime protection. IgG generally rises after IgM, though IgG antibodies to CHIKV E2 epitopes have been detected as early as 6 days after the onset of symptoms (159). In addition to serum and plasma, anti-CHIKV antibodies have been detected in CSF from patients with neurological manifestations (sensitivity, 80%; specificity, 87%) (145).
Other methodologies have recently been developed to simplify and/or improve upon traditional ELISAs. Serum spotted onto filter paper demonstrated 98.2% concordance with frozen samples when evaluated for serological testing on St. Martin (148). The use of multiple antigenic E2 peptides (160, 161), the preparation of E1 or E2 proteins (162–164), or the use of recombinant monoclonal E2 antibodies (165) has shown high specificity compared to whole-virus detection. Seroreactivities to E1 and E2 differ slightly, with high specificities for both by IgM capture ELISA but higher sensitivity for E2 than for E1 (90% compared to 78%) (166). The use of such reagents in capture ELISAs may eliminate the biohazard risk associated with the use of whole-virus preparations (166, 167). Additionally, these assays are more specific and may resolve issues related to cross-reactivity among alphaviruses. ONNV polyclonal antibodies weakly neutralize CHIKV, but the misdiagnosis of CHIKV for ONNV is possible, as between 71 and 86% of monoclonal antibodies to CHIKV also neutralized ONNV (41). Highly specific epitope-blocking ELISAs to the E2 protein do not show significant cross-reactions with other alphaviruses (168) yet identify antibodies that cross-protect between CHIKV lineages (159).
Antigen detection.
Antigen capture assays are also in development, though these are used less commonly than antigen-based methods for DENV. An immunochromatographic assay using monoclonal antibodies against the E1 protein was developed to detect CHIKV antigen in serum (169), but this test was found to be sensitive only for the ECSA lineage (89%) and not for the Asian lineage (33%) (170). Another antigen capture ELISA reported 96% concordance with real-time RT-PCR results for acute-phase samples from 200 subjects in India (146), and a test for whole CHIKV antigen in acute-phase samples had an overall agreement of 94% with RT-PCR (171). As these assays continue to develop and improve, antigen-based detection may provide rapid methods for CHIKV diagnostic confirmation and expand testing to laboratories without the capacity for molecular methods.
PROGNOSIS, OUTCOME, AND PREVENTION
Several agents have demonstrated activity against CHIKV in vitro, and monoclonal antibodies have shown efficacy in animal models (172–175), but currently, there is no specific antiviral treatment for CHIKV and management remains symptomatic. With the exception of joint pain, the symptoms of acute chikungunya typically resolve over a few days to 1 week (1, 68). Approximately 50% of patients have chronic arthralgia and/or arthritis at 3 to 6 months, and over 25% of patients may still have symptoms at 12 months, which negatively impacts quality of life during recovery (68, 176–180). Although significant heterogeneity regarding the rate of chronic joint pain following chikungunya exists in the literature, older age (>35 to 60 years) and preexisting joint disease have been consistently associated with this outcome (176, 177). Persistent joint symptoms may occur more often in women (177, 179), and one meta-analysis observed a nonsignificant trend toward more frequent chronic manifestations following infections with ECSA lineage strains (50%) than following infections with Asian lineage strains (36%) (178).
During recent outbreaks, mortality from CHIKV infections (attributable and associated) has been 14 to 80/100,000 inhabitants (181–183). Disease severity and excess deaths increase markedly in individuals >70 years old, and in the Dominican Republic, patients over 80 years old experienced a case fatality rate of 4.5% (62, 181, 182, 184). There are data indicating that the CHIKV viral load at presentation is associated with disease severity. Average viral loads are highest among neonates and the elderly, and viral loads are higher in hospitalized cases (7, 65, 66, 102, 184). However, the clinical applicability of these findings remains to be established.
Vector control is the primary mode of CHIKV prevention, though published data support the concept that a CHIKV vaccine could be highly efficacious and provide lasting immunity. Long-term protection against a following infection by CHIKV has been observed in areas of endemicity (185, 186), and a number of candidate vaccines have demonstrated promising results in preclinical studies. A few vaccines have now entered phase I and II clinical trials; however, the design and completion of phase III trials will be a significant challenge in the setting of a low number of cases during interepidemic periods. A complete discussion of CHIKV candidate vaccines is beyond the scope of this minireview, and these have recently been reviewed elsewhere (187–189).
CONCLUSION
Although the number of chikungunya cases has decreased since 2014, CHIKV has become endemic in countries across the tropics and has the capacity to cause sporadic outbreaks in naive individuals. This creates new challenges for CHIKV detection and surveillance as clinical cases become less frequent and may be misdiagnosed if accurate laboratory tests do not remain available. Furthermore, decreased case numbers conceal the need for improved diagnostics and prognostics that could identify individuals at high risk for chronic disease or poor outcomes and target prevention efforts to curb future explosive outbreaks.
Supplementary Material
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/JCM.00350-19.
REFERENCES
- 1.Powers AM. 2010. Chikungunya. Clin Lab Med 30:209–219. doi: 10.1016/j.cll.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Weaver SC, Lecuit M. 2015. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med 372:1231–1239. doi: 10.1056/NEJMra1406035. [DOI] [PubMed] [Google Scholar]
- 3.Staples JE, Fischer M. 2014. Chikungunya virus in the Americas—what a vectorborne pathogen can do. N Engl J Med 371:887–889. doi: 10.1056/NEJMp1407698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appassakij H, Khuntikij P, Kemapunmanus M, Wutthanarungsan R, Silpapojakul K. 2013. Viremic profiles in asymptomatic and symptomatic chikungunya fever: a blood transfusion threat? Transfusion 53:2567–2574. doi: 10.1111/j.1537-2995.2012.03960.x. [DOI] [PubMed] [Google Scholar]
- 5.Bustos Carrillo F, Collado D, Sanchez N, Ojeda S, Lopez Mercado B, Burger-Calderon R, Gresh L, Gordon A, Balmaseda A, Kuan G, Harris E. 2019. Epidemiological evidence for lineage-specific differences in the risk of inapparent chikungunya virus infection. J Virol 93:e01622-18. doi: 10.1128/JVI.01622-18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva JVJ, Ludwig-Begall LF, de Oliveira-Filho EF, Oliveira RAS, Durães-Carvalho R, Lopes TRR, Silva DEA, Gil LHVG. 2018. A scoping review of Chikungunya virus infection: epidemiology, clinical characteristics, viral co-circulation complications, and control. Acta Trop 188:213–224. doi: 10.1016/j.actatropica.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waggoner JJ, Gresh L, Vargas MJ, Ballesteros G, Tellez Y, Soda KJ, Sahoo MK, Nunez A, Balmaseda A, Harris E, Pinsky BA. 2016. Viremia and clinical presentation in Nicaraguan patients infected with Zika virus, chikungunya virus, and dengue virus. Clin Infect Dis 63:1584–1590. doi: 10.1093/cid/ciw589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silva MMO, Tauro LB, Kikuti M, Anjos RO, Santos VC, Goncalves TSF, Paploski IAD, Moreira PSS, Nascimento LCJ, Campos GS, Ko AI, Weaver SC, Reis MG, Kitron U, Ribeiro GS. 18 December 2018. Concomitant transmission of dengue, chikungunya and Zika viruses in Brazil: clinical and epidemiological findings from surveillance for acute febrile illness. Clin Infect Dis doi: 10.1093/cid/ciy1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carey DE. 1971. Chikungunya and dengue: a case of mistaken identity? J Hist Med Allied Sci 26:243–262. [DOI] [PubMed] [Google Scholar]
- 10.Kuno G. 2015. A re-examination of the history of etiologic confusion between dengue and chikungunya. PLoS Negl Trop Dis 9:e0004101. doi: 10.1371/journal.pntd.0004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halstead SB. 2015. Reappearance of chikungunya, formerly called dengue, in the Americas. Emerg Infect Dis 21:557–561. doi: 10.3201/eid2104.141723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weaver SC, Forrester NL. 2015. Chikungunya: evolutionary history and recent epidemic spread. Antiviral Res 120:32–39. doi: 10.1016/j.antiviral.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Vignuzzi M, Higgs S. 2017. The bridges and blockades to evolutionary convergence on the road to predicting chikungunya virus evolution. Annu Rev Virol 4:181–200. doi: 10.1146/annurev-virology-101416-041757. [DOI] [PubMed] [Google Scholar]
- 14.Burt FJ, Chen W, Miner JJ, Lenschow DJ, Merits A, Schnettler E, Kohl A, Rudd PA, Taylor A, Herrero LJ, Zaid A, Ng LFP, Mahalingam S. 2017. Chikungunya virus: an update on the biology and pathogenesis of this emerging pathogen. Lancet Infect Dis 17:e107–e117. doi: 10.1016/S1473-3099(16)30385-1. [DOI] [PubMed] [Google Scholar]
- 15.Powers AM, Brault AC, Tesh RB, Weaver SC. 2000. Re-emergence of chikungunya and O'nyong-nyong viruses: evidence for distinct geographical lineages and distant evolutionary relationships. J Gen Virol 81:471–479. doi: 10.1099/0022-1317-81-2-471. [DOI] [PubMed] [Google Scholar]
- 16.Volk SM, Chen R, Tsetsarkin KA, Adams AP, Garcia TI, Sall AA, Nasar F, Schuh AJ, Holmes EC, Higgs S, Maharaj PD, Brault AC, Weaver SC. 2010. Genome-scale phylogenetic analyses of chikungunya virus reveal independent emergences of recent epidemics and various evolutionary rates. J Virol 84:6497–6504. doi: 10.1128/JVI.01603-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonilauri P, Bellini R, Calzolari M, Angelini R, Venturi L, Fallacara F, Cordioli P, Angelini P, Venturelli C, Merialdi G, Dottori M. 2008. Chikungunya virus in Aedes albopictus, Italy. Emerg Infect Dis 14:852–854. doi: 10.3201/eid1405.071144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moro ML, Gagliotti C, Silvi G, Angelini R, Sambri V, Rezza G, Massimiliani E, Mattivi A, Grilli E, Finarelli AC, Spataro N, Pierro AM, Seyler T, Macini P. on behalf of the Chikungunya Study Group. 2010. Chikungunya virus in north-eastern Italy: a seroprevalence survey. Am J Trop Med Hyg 82:508–511. doi: 10.4269/ajtmh.2010.09-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gould EA, Gallian P, De Lamballerie X, Charrel RN. 2010. First cases of autochthonous dengue fever and chikungunya fever in France: from bad dream to reality! Clin Microbiol Infect 16:1702–1704. doi: 10.1111/j.1469-0691.2010.03386.x. [DOI] [PubMed] [Google Scholar]
- 20.Leparc-Goffart I, Nougairede A, Cassadou S, Prat C, de Lamballerie X. 2014. Chikungunya in the Americas. Lancet 383:514. doi: 10.1016/S0140-6736(14)60185-9. [DOI] [PubMed] [Google Scholar]
- 21.Souza TM, Azeredo EL, Badolato-Correa J, Damasco PV, Santos C, Petitinga-Paiva F, Nunes PC, Barbosa LS, Cipitelli MC, Chouin-Carneiro T, Faria NR, Nogueira RM, de Bruycker-Nogueira F, Dos Santos FB. 2017. First report of the East-Central South African genotype of chikungunya virus in Rio de Janeiro, Brazil. PLoS Curr 9:ecurrents.outbreaks.4200119978d62ccaa454599cd2735727. doi: 10.1371/currents.outbreaks.4200119978d62ccaa454599cd2735727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vairo F, Mammone A, Lanini S, Nicastri E, Castilletti C, Carletti F, Puro V, Di Lallo D, Panella V, Varrenti D, Scaramozzino P, di Caro A, Scognamiglio P, Capobianchi MR, Ippolito G, Chikungunya Lazio Outbreak Group. 2018. Local transmission of chikungunya in Rome and the Lazio region, Italy. PLoS One 13:e0208896. doi: 10.1371/journal.pone.0208896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsetsarkin KA, Vanlandingham DL, McGee CE, Higgs S. 2007. A single mutation in Chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog 3:e201. doi: 10.1371/journal.ppat.0030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rezza G, Nicoletti L, Angelini R, Romi R, Finarelli AC, Panning M, Cordioli P, Fortuna C, Boros S, Magurano F, Silvi G, Angelini P, Dottori M, Ciufolini MG, Majori GC, Cassone A, for the CHIKV Study Group. 2007. Infection with chikungunya virus in Italy: an outbreak in a temperate region. Lancet 370:1840–1846. doi: 10.1016/S0140-6736(07)61779-6. [DOI] [PubMed] [Google Scholar]
- 25.Borgherini G, Poubeau P, Staikowsky F, Lory M, Le Moullec N, Becquart JP, Wengling C, Michault A, Paganin F. 2007. Outbreak of chikungunya on Reunion Island: early clinical and laboratory features in 157 adult patients. Clin Infect Dis 44:1401–1407. doi: 10.1086/517537. [DOI] [PubMed] [Google Scholar]
- 26.Sergon K, Njuguna C, Kalani R, Ofula V, Onyango C, Konongoi LS, Bedno S, Burke H, Dumilla AM, Konde J, Njenga MK, Sang R, Breiman RF. 2008. Seroprevalence of chikungunya virus (CHIKV) infection on Lamu Island, Kenya, October 2004. Am J Trop Med Hyg 78:333–337. doi: 10.4269/ajtmh.2008.78.333. [DOI] [PubMed] [Google Scholar]
- 27.Sergon K, Yahaya AA, Brown J, Bedja SA, Mlindasse M, Agata N, Allaranger Y, Ball MD, Powers AM, Ofula V, Onyango C, Konongoi LS, Sang R, Njenga MK, Breiman RF. 2007. Seroprevalence of chikungunya virus infection on Grande Comore Island, Union of the Comoros, 2005. Am J Trop Med Hyg 76:1189–1193. doi: 10.4269/ajtmh.2007.76.1189. [DOI] [PubMed] [Google Scholar]
- 28.Raut CG, Rao NM, Sinha DP, Hanumaiah H, Manjunatha MJ. 2015. Chikungunya, dengue, and malaria co-infection after travel to Nigeria, India. Emerg Infect Dis 21:908–909. doi: 10.3201/eid2105.141804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Salam N, Mustafa S, Hafiz A, Chaudhary AA, Deeba F, Parveen S. 2018. Global prevalence and distribution of coinfection of malaria, dengue and chikungunya: a systematic review. BMC Public Health 18:710. doi: 10.1186/s12889-018-5626-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mukherjee S, Dutta SK, Sengupta S, Tripathi A. 2017. Evidence of dengue and chikungunya virus co-infection and circulation of multiple dengue serotypes in a recent Indian outbreak. Eur J Clin Microbiol Infect Dis 36:2273–2279. doi: 10.1007/s10096-017-3061-1. [DOI] [PubMed] [Google Scholar]
- 31.Sanchez-Carbonel J, Tantalean-Yepez D, Aguilar-Luis MA, Silva-Caso W, Weilg P, Vasquez-Achaya F, Costa L, Martins-Luna J, Sandoval I, Del Valle-Mendoza J. 2018. Identification of infection by chikungunya, Zika, and dengue in an area of the Peruvian coast. Molecular diagnosis and clinical characteristics. BMC Res Notes 11:175. doi: 10.1186/s13104-018-3290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carrillo-Hernández MY, Ruiz-Saenz J, Villamizar LJ, Gómez-Rangel SY, Martínez-Gutierrez M. 2018. Co-circulation and simultaneous co-infection of dengue, chikungunya, and Zika viruses in patients with febrile syndrome at the Colombian-Venezuelan border. BMC Infect Dis 18:61. doi: 10.1186/s12879-018-2976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Acevedo N, Waggoner J, Rodriguez M, Rivera L, Landivar J, Pinsky B, Zambrano H. 2017. Zika virus, chikungunya virus, and dengue virus in cerebrospinal fluid from adults with neurological manifestations, Guayaquil, Ecuador. Front Microbiol 8:42. doi: 10.3389/fmicb.2017.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waggoner J, Brichard J, Mutuku F, Ndenga B, Heath CJ, Mohamed-Hadley A, Sahoo MK, Vulule J, Lefterova M, Banaei N, Mukoko D, Pinsky BA, LaBeaud AD. 2017. Malaria and chikungunya detected using molecular diagnostics among febrile Kenyan children. Open Forum Infect Dis 4:ofx110. doi: 10.1093/ofid/ofx110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Althouse BM, Guerbois M, Cummings DAT, Diop OM, Faye O, Faye A, Diallo D, Sadio BD, Sow A, Faye O, Sall AA, Diallo M, Benefit B, Simons E, Watts DM, Weaver SC, Hanley KA. 2018. Role of monkeys in the sylvatic cycle of chikungunya virus in Senegal. Nat Commun 9:1046. doi: 10.1038/s41467-018-03332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tsetsarkin KA, Chen R, Weaver SC. 2016. Interspecies transmission and chikungunya virus emergence. Curr Opin Virol 16:143–150. doi: 10.1016/j.coviro.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jain J, Kushwah RBS, Singh SS, Sharma A, Adak T, Singh OP, Bhatnagar RK, Subbarao SK, Sunil S. 2016. Evidence for natural vertical transmission of chikungunya viruses in field populations of Aedes aegypti in Delhi and Haryana states in India—a preliminary report. Acta Trop 162:46–55. doi: 10.1016/j.actatropica.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Mavale M, Parashar D, Sudeep A, Gokhale M, Ghodke Y, Geevarghese G, Arankalle V, Mishra AC. 2010. Venereal transmission of chikungunya virus by Aedes aegypti mosquitoes (Diptera: Culicidae). Am J Trop Med Hyg 83:1242–1244. doi: 10.4269/ajtmh.2010.09-0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gardner J, Anraku I, Le TT, Larcher T, Major L, Roques P, Schroder WA, Higgs S, Suhrbier A. 2010. Chikungunya virus arthritis in adult wild-type mice. J Virol 84:8021–8032. doi: 10.1128/JVI.02603-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Partidos CD, Paykel J, Weger J, Borland EM, Powers AM, Seymour R, Weaver SC, Stinchcomb DT, Osorio JE. 2012. Cross-protective immunity against O'nyong-nyong virus afforded by a novel recombinant chikungunya vaccine. Vaccine 30:4638–4643. doi: 10.1016/j.vaccine.2012.04.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blackburn NK, Besselaar TG, Gibson G. 1995. Antigenic relationship between chikungunya virus strains and O'nyong nyong virus using monoclonal antibodies. Res Virol 146:69–73. doi: 10.1016/0923-2516(96)80591-7. [DOI] [PubMed] [Google Scholar]
- 42.McClain DJ, Pittman PR, Ramsburg HH, Nelson GO, Rossi CA, Mangiafico JA, Schmaljohn AL, Malinoski FJ. 1998. Immunologic interference from sequential administration of live attenuated alphavirus vaccines. J Infect Dis 177:634–641. doi: 10.1086/514240. [DOI] [PubMed] [Google Scholar]
- 43.Lidbury BA, Mahalingam S. 2000. Specific ablation of antiviral gene expression in macrophages by antibody-dependent enhancement of Ross River virus infection. J Virol 74:8376–8381. doi: 10.1128/JVI.74.18.8376-8381.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Linn ML, Aaskov JG, Suhrbier A. 1996. Antibody-dependent enhancement and persistence in macrophages of an arbovirus associated with arthritis. J Gen Virol 77:407–411. doi: 10.1099/0022-1317-77-3-407. [DOI] [PubMed] [Google Scholar]
- 45.Flynn DC, Olmsted RA, Mackenzie JM Jr, Johnston RE. 1988. Antibody-mediated activation of Sindbis virus. Virology 166:82–90. doi: 10.1016/0042-6822(88)90149-3. [DOI] [PubMed] [Google Scholar]
- 46.Hallengärd D, Kakoulidou M, Lulla A, Kümmerer BM, Johansson DX, Mutso M, Lulla V, Fazakerley JK, Roques P, Le Grand R, Merits A, Liljeström P. 2014. Novel attenuated Chikungunya vaccine candidates elicit protective immunity in C57BL/6 mice. J Virol 88:2858–2866. doi: 10.1128/JVI.03453-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lum FM, Couderc T, Chia BS, Ong RY, Her Z, Chow A, Leo YS, Kam YW, Renia L, Lecuit M, Ng L. 2018. Antibody-mediated enhancement aggravates chikungunya virus infection and disease severity. Sci Rep 8:1860. doi: 10.1038/s41598-018-20305-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holzer GW, Coulibaly S, Aichinger G, Savidis-Dacho H, Mayrhofer J, Brunner S, Schmid K, Kistner O, Aaskov JG, Falkner FG, Ehrlich H, Barrett PN, Kreil TR. 2011. Evaluation of an inactivated Ross River virus vaccine in active and passive mouse immunization models and establishment of a correlate of protection. Vaccine 29:4132–4141. doi: 10.1016/j.vaccine.2011.03.089. [DOI] [PubMed] [Google Scholar]
- 49.Queyriaux B, Simon F, Grandadam M, Michel R, Tolou H, Boutin JP. 2008. Clinical burden of chikungunya virus infection. Lancet Infect Dis 8:2–3. doi: 10.1016/S1473-3099(07)70294-3. [DOI] [PubMed] [Google Scholar]
- 50.Gerardin P, Guernier V, Perrau J, Fianu A, Le Roux K, Grivard P, Michault A, de Lamballerie X, Flahault A, Favier F. 2008. Estimating chikungunya prevalence in La Reunion Island outbreak by serosurveys: two methods for two critical times of the epidemic. BMC Infect Dis 8:99. doi: 10.1186/1471-2334-8-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Burt FJ, Rolph MS, Rulli NE, Mahalingam S, Heise MT. 2012. Chikungunya: a re-emerging virus. Lancet 379:662–671. doi: 10.1016/S0140-6736(11)60281-X. [DOI] [PubMed] [Google Scholar]
- 52.Yoon IK, Alera MT, Lago CB, Tac-An IA, Villa D, Fernandez S, Thaisomboonsuk B, Klungthong C, Levy JW, Velasco JM, Roque VG Jr, Salje H, Macareo LR, Hermann LL, Nisalak A, Srikiatkhachorn A. 2015. High rate of subclinical chikungunya virus infection and association of neutralizing antibody with protection in a prospective cohort in the Philippines. PLoS Negl Trop Dis 9:e0003764. doi: 10.1371/journal.pntd.0003764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bloch D, Roth NM, Caraballo EV, Munoz-Jordan J, Hunsperger E, Rivera A, Perez-Padilla J, Rivera Garcia B, Sharp TM. 2016. Use of household cluster investigations to identify factors associated with chikungunya virus infection and frequency of case reporting in Puerto Rico. PLoS Negl Trop Dis 10:e0005075. doi: 10.1371/journal.pntd.0005075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Balmaseda A, Gordon A, Gresh L, Ojeda S, Saborio S, Tellez Y, Sanchez N, Kuan G, Harris E. 2016. Clinical attack rate of chikungunya in a cohort of Nicaraguan children. Am J Trop Med Hyg 94:397–399. doi: 10.4269/ajtmh.15-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Galatas B, Ly S, Duong V, Baisley K, Nguon K, Chan S, Huy R, Ly S, Sorn S, Som L, Buchy P, Tarantola A. 2016. Long-lasting immune protection and other epidemiological findings after chikungunya emergence in a Cambodian rural community, April 2012. PLoS Negl Trop Dis 10:e0004281. doi: 10.1371/journal.pntd.0004281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nakkhara P, Chongsuvivatwong V, Thammapalo S. 2013. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans R Soc Trop Med Hyg 107:789–796. doi: 10.1093/trstmh/trt083. [DOI] [PubMed] [Google Scholar]
- 57.Ray P, Ratagiri VH, Kabra SK, Lodha R, Sharma S, Sharma BS, Kalaivani M, Wig N. 2012. Chikungunya infection in India: results of a prospective hospital based multi-centric study. PLoS One 7:e30025. doi: 10.1371/journal.pone.0030025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kularatne SA, Gihan MC, Weerasinghe SC, Gunasena S. 2009. Concurrent outbreaks of chikungunya and dengue fever in Kandy, Sri Lanka, 2006-07: a comparative analysis of clinical and laboratory features. Postgrad Med J 85:342–346. doi: 10.1136/pgmj.2007.066746. [DOI] [PubMed] [Google Scholar]
- 59.Lee VJ, Chow A, Zheng X, Carrasco LR, Cook AR, Lye DC, Ng LC, Leo YS. 2012. Simple clinical and laboratory predictors of chikungunya versus dengue infections in adults. PLoS Negl Trop Dis 6:e1786. doi: 10.1371/journal.pntd.0001786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bonifay T, Vesin G, Bidaud B, Bonnefoy C, Dueymes M, Nacher M, Djossou F, Epelboin L. 19 October 2018. Clinical characteristics and predictive score of dengue vs. chikungunya virus infections. Med Mal Infect. doi: 10.1016/j.medmal.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 61.Paternina-Caicedo A, De la Hoz-Restrepo F, Díaz-Quijano F, Caicedo-Torres W, Auxiliadora Badillo-Viloria M, Bula-Anichiarico D, Alvis-Guzmán N, Mattar S, Constenla D, Pinzón-Redondo H. 2018. Features of dengue and chikungunya infections of Colombian children under 24 months of age admitted to the emergency department. J Trop Pediatr 64:31–37. doi: 10.1093/tropej/fmx024. [DOI] [PubMed] [Google Scholar]
- 62.Economopoulou A, Dominguez M, Helynck B, Sissoko D, Wichmann O, Quenel P, Germonneau P, Quatresous I. 2009. Atypical chikungunya virus infections: clinical manifestations, mortality and risk factors for severe disease during the 2005-2006 outbreak on Reunion. Epidemiol Infect 137:534–541. doi: 10.1017/S0950268808001167. [DOI] [PubMed] [Google Scholar]
- 63.Macpherson C, Noel T, Fields P, Jungkind D, Yearwood K, Simmons M, Widjaja S, Mitchell G, Noel D, Bidaisee S, Myers TE, LaBeaud AD. 2016. Clinical and serological insights from the Asian lineage chikungunya outbreak in Grenada, 2014: an observational study. Am J Trop Med Hyg 95:890–893. doi: 10.4269/ajtmh.16-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lindsey NP, Staples JE, Fischer M. 2018. Chikungunya virus disease among travelers—United States, 2014-2016. Am J Trop Med Hyg 98:192–197. doi: 10.4269/ajtmh.17-0668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Staikowsky F, Talarmin F, Grivard P, Souab A, Schuffenecker I, Le Roux K, Lecuit M, Michault A. 2009. Prospective study of chikungunya virus acute infection in the island of La Reunion during the 2005–2006 outbreak. PLoS One 4:e7603. doi: 10.1371/journal.pone.0007603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Thiberville SD, Boisson V, Gaudart J, Simon F, Flahault A, de Lamballerie X. 2013. Chikungunya fever: a clinical and virological investigation of outpatients on Reunion Island, south-west Indian Ocean. PLoS Negl Trop Dis 7:e2004. doi: 10.1371/journal.pntd.0002004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jain J, Nayak K, Tanwar N, Gaind R, Gupta B, Shastri JS, Bhatnagar RK, Kaja MK, Chandele A, Sunil S. 2017. Clinical, serological, and virological analysis of 572 chikungunya patients from 2010 to 2013 in India. Clin Infect Dis 65:133–140. doi: 10.1093/cid/cix283. [DOI] [PubMed] [Google Scholar]
- 68.Taubitz W, Cramer JP, Kapaun A, Pfeffer M, Drosten C, Dobler G, Burchard GD, Loscher T. 2007. Chikungunya fever in travelers: clinical presentation and course. Clin Infect Dis 45:e1–e4. doi: 10.1086/518701. [DOI] [PubMed] [Google Scholar]
- 69.Danis-Lozano R, Díaz-González EE, Trujillo-Murillo KDC, Caballero-Sosa S, Sepúlveda-Delgado J, Malo-García IR, Canseco-Ávila LM, Salgado-Corsantes LM, Domínguez-Arrevillaga S, Torres-Zapata R, Gómez-Cruz O, Fernández-Salas I. 2017. Clinical characterization of acute and convalescent illness of confirmed chikungunya cases from Chiapas, S. Mexico: a cross sectional study. PLoS One 12:e0186923. doi: 10.1371/journal.pone.0186923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dutta SK, Pal T, Saha B, Mandal S, Tripathi A. 2014. Copy number variation of chikungunya ECSA virus with disease symptoms among Indian patients. J Med Virol 86:1386–1392. doi: 10.1002/jmv.23794. [DOI] [PubMed] [Google Scholar]
- 71.Nkoghe D, Kassa RF, Bisvigou U, Caron M, Grard G, Leroy EM. 2012. No clinical or biological difference between chikungunya and dengue fever during the 2010 Gabonese outbreak. Infect Dis Rep 4:e5. doi: 10.4081/idr.2012.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Laoprasopwattana K, Kaewjungwad L, Jarumanokul R, Geater A. 2012. Differential diagnosis of chikungunya, dengue viral infection and other acute febrile illnesses in children. Pediatr Infect Dis J 31:459–463. doi: 10.1097/INF.0b013e31824bb06d. [DOI] [PubMed] [Google Scholar]
- 73.Godaert L, Bartholet S, Gazeuse Y, Brouste Y, Najioullah F, Kanagaratnam L, Cesaire R, Fanon JL, Drame M. 2018. Misdiagnosis of chikungunya virus infection: comparison of old and younger adults. J Am Geriatr Soc 66:1768–1772. doi: 10.1111/jgs.15492. [DOI] [PubMed] [Google Scholar]
- 74.Rosso F, Rodríguez S, Cedano JA, Mora BL, Moncada PA, Velez JD. 2018. Chikungunya in solid organ transplant recipients, a case series and literature review. Transpl Infect Dis 20:e12978. doi: 10.1111/tid.12978. [DOI] [PubMed] [Google Scholar]
- 75.Cerny T, Schwarz M, Schwarz U, Lemant J, Gerardin P, Keller E. 2017. The range of neurological complications in chikungunya fever. Neurocrit Care 27:447–457. doi: 10.1007/s12028-017-0413-8. [DOI] [PubMed] [Google Scholar]
- 76.Carabali M, Lim JK, Palencia DC, Lozano-Parra A, Gelvez RM, Lee KS, Florez JP, Herrera VM, Kaufman JS, Rojas EM, Villar LA. 2018. Burden of dengue among febrile patients at the time of chikungunya introduction in Piedecuesta, Colombia. Trop Med Int Health 23:1231–1241. doi: 10.1111/tmi.13147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Centers for Disease Control and Prevention. 2009. Biosafety in microbiological and biomedical laboratories. Centers for Disease Control and Prevention, Atlanta, GA. [Google Scholar]
- 78.Scherer WF, Eddy GA, Monath TP. 1980. Laboratory safety for arboviruses and certain other viruses of vertebrates. Am J Trop Med Hyg 29:1359–1381. [DOI] [PubMed] [Google Scholar]
- 79.Sourisseau M, Schilte C, Casartelli N, Trouillet C, Guivel-Benhassine F, Rudnicka D, Sol-Foulon N, Le Roux K, Prevost M-C, Fsihi H, Frenkiel M-P, Blanchet F, Afonso PV, Ceccaldi P-E, Ozden S, Gessain A, Schuffenecker I, Verhasselt B, Zamborlini A, Saïb A, Rey FA, Arenzana-Seisdedos F, Desprès P, Michault A, Albert ML, Schwartz O. 2007. Characterization of reemerging chikungunya virus. PLoS Pathog 3:e89. doi: 10.1371/journal.ppat.0030089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mascarenhas M, Garasia S, Berthiaume P, Corrin T, Greig J, Ng V, Young I, Waddell L. 2018. A scoping review of published literature on chikungunya virus. PLoS One 13:e0207554. doi: 10.1371/journal.pone.0207554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tomori O, Monath TP, O'Connor EH, Lee VH, Cropp CB. 1981. Arbovirus infections among laboratory personnel in Ibadan, Nigeria. Am J Trop Med Hyg 30:855–861. doi: 10.4269/ajtmh.1981.30.855. [DOI] [PubMed] [Google Scholar]
- 82.Huang YJ, Hsu WW, Higgs S, Vanlandingham DL. 2015. Temperature tolerance and inactivation of chikungunya virus. Vector Borne Zoonotic Dis 15:674–677. doi: 10.1089/vbz.2015.1795. [DOI] [PubMed] [Google Scholar]
- 83.Sharma A, Gupta P, Maheshwari RK. 2012. Inactivation of chikungunya virus by 1,5 iodonapthyl azide. Virol J 9:301. doi: 10.1186/1743-422X-9-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mathew AM, Mun AB, Balakrishnan A. 2018. Ultraviolet inactivation of chikungunya virus. Intervirology 61:36–41. doi: 10.1159/000490567. [DOI] [PubMed] [Google Scholar]
- 85.De Serres G, Skowronski DM, Wu XW, Ambrose CS. 2013. The test-negative design: validity, accuracy and precision of vaccine efficacy estimates compared to the gold standard of randomised placebo-controlled clinical trials. Euro Surveill 18(37)::pii=20585. doi: 10.2807/1560-7917.ES2013.18.37.20585. [DOI] [PubMed] [Google Scholar]
- 86.Patramool S, Bernard E, Hamel R, Natthanej L, Chazal N, Surasombatpattana P, Ekchariyawat P, Daoust S, Thongrungkiat S, Thomas F, Briant L, Misse D. 2013. Isolation of infectious chikungunya virus and dengue virus using anionic polymer-coated magnetic beads. J Virol Methods 193:55–61. doi: 10.1016/j.jviromet.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 87.Hudu SA, Alshrari AS, Syahida A, Sekawi Z. 2016. Cell culture, technology: enhancing the culture of diagnosing human diseases. J Clin Diagn Res 10:DE01–DE05. doi: 10.7860/JCDR/2016/15837.7460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Staples JE, Breiman RF, Powers AM. 2009. Chikungunya fever: an epidemiological review of a re-emerging infectious disease. Clin Infect Dis 49:942–948. doi: 10.1086/605496. [DOI] [PubMed] [Google Scholar]
- 89.Dash M, Mohanty I, Padhi S. 2011. Laboratory diagnosis of chikungunya virus: do we really need it? Indian J Med Sci 65:83–91. doi: 10.4103/0019-5359.104781. [DOI] [PubMed] [Google Scholar]
- 90.Cherabuddi K, Iovine NM, Shah K, White SK, Paisie T, Salemi M, Morris JG Jr, Lednicky JA. 2016. Zika and chikungunya virus co-infection in a traveller returning from Colombia, 2016: virus isolation and genetic analysis. JMM Case Rep 3:e005072. doi: 10.1099/jmmcr.0.005072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lednicky J, De Rochars VM, Elbadry M, Loeb J, Telisma T, Chavannes S, Anilis G, Cella E, Ciccozzi M, Okech B, Salemi M, Morris JG Jr.. 2016. Mayaro virus in child with acute febrile illness, Haiti, 2015. Emerg Infect Dis 22:2000–2002. doi: 10.3201/eid2211.161015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schuffenecker I, Iteman I, Michault A, Murri S, Frangeul L, Vaney MC, Lavenir R, Pardigon N, Reynes JM, Pettinelli F, Biscornet L, Diancourt L, Michel S, Duquerroy S, Guigon G, Frenkiel MP, Brehin AC, Cubito N, Despres P, Kunst F, Rey FA, Zeller H, Brisse S. 2006. Genome microevolution of chikungunya viruses causing the Indian Ocean outbreak. PLoS Med 3:e263. doi: 10.1371/journal.pmed.0030263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mulyatno KC, Susilowati H, Yamanaka A, Soegijanto S, Konishi E. 2012. Primary isolation and phylogenetic studies of chikungunya virus from Surabaya, Indonesia. Jpn J Infect Dis 65:92–94. [PubMed] [Google Scholar]
- 94.Ghosh A, Alladi PA, Narayanappa G, Vasanthapuram R, Desai A. 2018. The time course analysis of morphological changes induced by Chikungunya virus replication in mammalian and mosquito cells. Acta Virol 62:360–373. doi: 10.4149/av_2018_403. [DOI] [PubMed] [Google Scholar]
- 95.Li YG, Siripanyaphinyo U, Tumkosit U, Noranate N, An A, Tao R, Kurosu T, Ikuta K, Takeda N, Anantapreecha S. 2013. Chikungunya virus induces a more moderate cytopathic effect in mosquito cells than in mammalian cells. Intervirology 56:6–12. doi: 10.1159/000339985. [DOI] [PubMed] [Google Scholar]
- 96.Long KM, Heise MT. 2015. Protective and pathogenic responses to chikungunya virus infection. Curr Trop Med Rep 2:13–21. doi: 10.1007/s40475-015-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ang SK, Lam S, Chu JJ. 2016. Propagation of chikungunya virus using mosquito cells. Methods Mol Biol 1426:87–92. doi: 10.1007/978-1-4939-3618-2_8. [DOI] [PubMed] [Google Scholar]
- 98.Zhang X, Huang Y, Wang M, Yang F, Wu C, Huang D, Xiong L, Wan C, Cheng J, Zhang R. 2018. Differences in genome characters and cell tropisms between two chikungunya isolates of Asian lineage and Indian Ocean lineage. Virol J 15:130. doi: 10.1186/s12985-018-1024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Carletti F, Marsella P, Colavita F, Meschi S, Lalle E, Bordi L, Di Lallo D, Panella V, Di Caro A, Nicastri E, Scognamiglio P, Lanini S, Vairo F, Capobianchi MR, Ippolito G, Castilletti C. 2017. Full-length genome sequence of a chikungunya virus isolate from the 2017 autochthonous outbreak, Lazio Region, Italy. Genome Announc 5:e01306-17. doi: 10.1128/genomeA.01306-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chalaem P, Chusri S, Fernandez S, Chotigeat W, Anguita J, Pal U, Promnares K. 2016. Characterization of a chikungunya virus strain isolated from banked patients' sera. Virol J 13:150. doi: 10.1186/s12985-016-0606-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wikan N, Sakoonwatanyoo P, Ubol S, Yoksan S, Smith DR. 2012. Chikungunya virus infection of cell lines: analysis of the East, Central and South African lineage. PLoS One 7:e31102. doi: 10.1371/journal.pone.0031102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Laurent P, Le Roux K, Grivard P, Bertil G, Naze F, Picard M, Staikowsky F, Barau G, Schuffenecker I, Michault A. 2007. Development of a sensitive real-time reverse transcriptase PCR assay with an internal control to detect and quantify chikungunya virus. Clin Chem 53:1408–1414. doi: 10.1373/clinchem.2007.086595. [DOI] [PubMed] [Google Scholar]
- 103.Chua CL, Sam IC, Chiam CW, Chan YF. 2017. The neutralizing role of IgM during early chikungunya virus infection. PLoS One 12:e0171989. doi: 10.1371/journal.pone.0171989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chusri S, Siripaitoon P, Silpapojakul K, Hortiwakul T, Charernmak B, Chinnawirotpisan P, Nisalak A, Thaisomboonsuk B, Klungthong C, Gibbons RV, Jarman RG. 2014. Kinetics of chikungunya infections during an outbreak in southern Thailand, 2008-2009. Am J Trop Med Hyg 90:410–417. doi: 10.4269/ajtmh.12-0681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Panning M, Grywna K, van Esbroeck M, Emmerich P, Drosten C. 2008. Chikungunya fever in travelers returning to Europe from the Indian Ocean region, 2006. Emerg Infect Dis 14:416–422. doi: 10.3201/eid1403.070906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yap G, Pok KY, Lai YL, Hapuarachchi HC, Chow A, Leo YS, Tan LK, Ng LC. 2010. Evaluation of chikungunya diagnostic assays: differences in sensitivity of serology assays in two independent outbreaks. PLoS Negl Trop Dis 4:e753. doi: 10.1371/journal.pntd.0000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gibney KB, Fischer M, Prince HE, Kramer LD, St George K, Kosoy OL, Laven JJ, Staples JE. 2011. Chikungunya fever in the United States: a fifteen year review of cases. Clin Infect Dis 52:e121–e126. doi: 10.1093/cid/ciq214. [DOI] [PubMed] [Google Scholar]
- 108.Hasebe F, Parquet MC, Pandey BD, Mathenge EG, Morita K, Balasubramaniam V, Saat Z, Yusop A, Sinniah M, Natkunam S, Igarashi A. 2002. Combined detection and genotyping of Chikungunya virus by a specific reverse transcription-polymerase chain reaction. J Med Virol 67:370–374. doi: 10.1002/jmv.10085. [DOI] [PubMed] [Google Scholar]
- 109.M Naresh Kumar CV, Anthony Johnson AM, R Sai Gopal DV. 2007. Molecular characterization of chikungunya virus from Andhra Pradesh, India & phylogenetic relationship with Central African isolates. Indian J Med Res 126:534–540. [PubMed] [Google Scholar]
- 110.Lakshmi V, Neeraja M, Subbalaxmi MV, Parida MM, Dash PK, Santhosh SR, Rao PV. 2008. Clinical features and molecular diagnosis of Chikungunya fever from South India. Clin Infect Dis 46:1436–1442. doi: 10.1086/529444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sharma S, Dash PK, Santhosh SR, Shukla J, Parida M, Rao PV. 2010. Development of a quantitative competitive reverse transcription polymerase chain reaction (QC-RT-PCR) for detection and quantitation of chikungunya virus. Mol Biotechnol 45:49–55. doi: 10.1007/s12033-009-9238-9. [DOI] [PubMed] [Google Scholar]
- 112.Reddy V, Ravi V, Desai A, Parida M, Powers AM, Johnson BW. 2012. Utility of IgM ELISA, TaqMan real-time PCR, reverse transcription PCR, and RT-LAMP assay for the diagnosis of chikungunya fever. J Med Virol 84:1771–1778. doi: 10.1002/jmv.23406. [DOI] [PubMed] [Google Scholar]
- 113.Lanciotti RS, Kosoy OL, Laven JJ, Panella AJ, Velez JO, Lambert AJ, Campbell GL. 2007. Chikungunya virus in US travelers returning from India, 2006. Emerg Infect Dis 13:764–767. doi: 10.3201/eid1305.070015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pastorino B, Bessaud M, Grandadam M, Murri S, Tolou HJ, Peyrefitte CN. 2005. Development of a TaqMan RT-PCR assay without RNA extraction step for the detection and quantification of African chikungunya viruses. J Virol Methods 124:65–71. doi: 10.1016/j.jviromet.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 115.Edwards CJ, Welch SR, Chamberlain J, Hewson R, Tolley H, Cane PA, Lloyd G. 2007. Molecular diagnosis and analysis of chikungunya virus. J Clin Virol 39:271–275. doi: 10.1016/j.jcv.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 116.Santhosh SR, Parida MM, Dash PK, Pateriya A, Pattnaik B, Pradhan HK, Tripathi NK, Ambuj S, Gupta N, Saxena P, Lakshmana Rao PV. 2007. Development and evaluation of SYBR green I-based one-step real-time RT-PCR assay for detection and quantification of chikungunya virus. J Clin Virol 39:188–193. doi: 10.1016/j.jcv.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 117.Panning M, Hess M, Fischer W, Grywna K, Pfeffer M, Drosten C. 2009. Performance of the RealStar chikungunya virus real-time reverse transcription-PCR kit. J Clin Microbiol 47:3014–3016. doi: 10.1128/JCM.01024-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chen H, Parimelalagan M, Takei F, Hapuarachchi HC, Koay ES, Ng LC, Ho PS, Nakatani K, Chu JJ. 2016. Development of 2,7-diamino-1,8-naphthyridine (DANP) anchored hairpin primers for RT-PCR detection of chikungunya virus infection. PLoS Negl Trop Dis 10:e0004887. doi: 10.1371/journal.pntd.0004887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chen H, Takei F, Koay ES, Nakatani K, Chu JJ. 2013. A novel DANP-coupled hairpin RT-PCR for rapid detection of chikungunya virus. J Mol Diagn 15:227–233. doi: 10.1016/j.jmoldx.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 120.Chiam CW, Chan YF, Loong SK, Yong SS, Hooi PS, Sam IC. 2013. Real-time polymerase chain reaction for diagnosis and quantitation of negative strand of chikungunya virus. Diagn Microbiol Infect Dis 77:133–137. doi: 10.1016/j.diagmicrobio.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 121.Parida MM, Santhosh SR, Dash PK, Tripathi NK, Lakshmi V, Mamidi N, Shrivastva A, Gupta N, Saxena P, Babu JP, Rao PV, Morita K. 2007. Rapid and real-time detection of chikungunya virus by reverse transcription loop-mediated isothermal amplification assay. J Clin Microbiol 45:351–357. doi: 10.1128/JCM.01734-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Priye A, Bird SW, Light YK, Ball CS, Negrete OA, Meagher RJ. 2017. A smartphone-based diagnostic platform for rapid detection of Zika, chikungunya, and dengue viruses. Sci Rep 7:44778. doi: 10.1038/srep44778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Telles JN, Le Roux K, Grivard P, Vernet G, Michault A. 2009. Evaluation of real-time nucleic acid sequence-based amplification for detection of chikungunya virus in clinical samples. J Med Microbiol 58:1168–1172. doi: 10.1099/jmm.0.010736-0. [DOI] [PubMed] [Google Scholar]
- 124.Patel P, Abd El Wahed A, Faye O, Pruger P, Kaiser M, Thaloengsok S, Ubol S, Sakuntabhai A, Leparc-Goffart I, Hufert FT, Sall AA, Weidmann M, Niedrig M. 2016. A field-deployable reverse transcription recombinase polymerase amplification assay for rapid detection of the chikungunya virus. PLoS Negl Trop Dis 10:e0004953. doi: 10.1371/journal.pntd.0004953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dash PK, Parida M, Santhosh SR, Saxena P, Srivastava A, Neeraja M, Lakshmi V, Rao PV. 2008. Development and evaluation of a 1-step duplex reverse transcription polymerase chain reaction for differential diagnosis of chikungunya and dengue infection. Diagn Microbiol Infect Dis 62:52–57. doi: 10.1016/j.diagmicrobio.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 126.Mishra B, Sharma M, Pujhari SK, Ratho RK, Gopal DS, Kumar CN, Sarangi G, Chayani N, Varma SC. 2011. Utility of multiplex reverse transcriptase-polymerase chain reaction for diagnosis and serotypic characterization of dengue and chikungunya viruses in clinical samples. Diagn Microbiol Infect Dis 71:118–125. doi: 10.1016/j.diagmicrobio.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 127.Naze F, Le Roux K, Schuffenecker I, Zeller H, Staikowsky F, Grivard P, Michault A, Laurent P. 2009. Simultaneous detection and quantitation of chikungunya, dengue and West Nile viruses by multiplex RT-PCR assays and dengue virus typing using high resolution melting. J Virol Methods 162:1–7. doi: 10.1016/j.jviromet.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 128.Kulesh DA, Jahrling J, Lee JS, Groebner JL, Turell MJ, O’Guinn ML, Smith DR. 2009. Development of field-based real-time reverse transcription-polymerase chain reaction assays for detection of chikungunya and O'nyong-nyong viruses in mosquitoes. Am J Trop Med Hyg 81:679–684. doi: 10.4269/ajtmh.2009.09-0138. [DOI] [PubMed] [Google Scholar]
- 129.Pongsiri P, Praianantathavorn K, Theamboonlers A, Payungporn S, Poovorawan Y. 2012. Multiplex real-time RT-PCR for detecting chikungunya virus and dengue virus. Asian Pac J Trop Med 5:342–346. doi: 10.1016/S1995-7645(12)60055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Saha K, Firdaus R, Chakrabarti S, Sadhukhan PC. 2013. Development of rapid, sensitive one-tube duplex RT-PCR assay for specific and differential diagnosis of chikungunya and dengue. J Virol Methods 193:521–524. doi: 10.1016/j.jviromet.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 131.Cecilia D, Kakade M, Alagarasu K, Patil J, Salunke A, Parashar D, Shah PS. 2015. Development of a multiplex real-time RT-PCR assay for simultaneous detection of dengue and chikungunya viruses. Arch Virol 160:323–327. doi: 10.1007/s00705-014-2217-x. [DOI] [PubMed] [Google Scholar]
- 132.Chen H, Parimelalagan M, Lai YL, Lee KS, Koay ES, Hapuarachchi HC, Ng LC, Ho PS, Chu JJ. 2015. Development and evaluation of a SYBR green-based real-time multiplex RT-PCR assay for simultaneous detection and serotyping of dengue and chikungunya viruses. J Mol Diagn 17:722–728. doi: 10.1016/j.jmoldx.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pabbaraju K, Wong S, Gill K, Fonseca K, Tipples GA, Tellier R. 2016. Simultaneous detection of Zika, chikungunya and dengue viruses by a multiplex real-time RT-PCR assay. J Clin Virol 83:66–71. doi: 10.1016/j.jcv.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 134.Simmons M, Myers T, Guevara C, Jungkind D, Williams M, Houng HS. 2016. Development and validation of a quantitative, one-step, multiplex, real-time reverse transcriptase PCR assay for detection of dengue and chikungunya viruses. J Clin Microbiol 54:1766–1773. doi: 10.1128/JCM.00299-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Waggoner JJ, Gresh L, Mohamed-Hadley A, Ballesteros G, Davila MJ, Tellez Y, Sahoo MK, Balmaseda A, Harris E, Pinsky BA. 2016. Single-reaction multiplex reverse transcription PCR for detection of Zika, chikungunya, and dengue viruses. Emerg Infect Dis 22:1295–1297. doi: 10.3201/eid2207.160326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Waggoner JJ, Ballesteros G, Gresh L, Mohamed-Hadley A, Tellez Y, Sahoo MK, Abeynayake J, Balmaseda A, Harris E, Pinsky BA. 2016. Clinical evaluation of a single-reaction real-time RT-PCR for pan-dengue and chikungunya virus detection. J Clin Virol 78:57–61. doi: 10.1016/j.jcv.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wu W, Wang J, Yu N, Yan J, Zhuo Z, Chen M, Su X, Fang M, He S, Zhang S, Zhang Y, Ge S, Xia N. 2018. Development of multiplex real-time reverse-transcriptase polymerase chain reaction assay for simultaneous detection of Zika, dengue, yellow fever, and chikungunya viruses in a single tube. J Med Virol 90:1681–1686. doi: 10.1002/jmv.25253. [DOI] [PubMed] [Google Scholar]
- 138.Santiago GA, Vazquez J, Courtney S, Matias KY, Andersen LE, Colon C, Butler AE, Roulo R, Bowzard J, Villanueva JM, Munoz-Jordan JL. 2018. Performance of the Trioplex real-time RT-PCR assay for detection of Zika, dengue, and chikungunya viruses. Nat Commun 9:1391. doi: 10.1038/s41467-018-03772-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jacobsen S, Patel P, Schmidt-Chanasit J, Leparc-Goffart I, Teichmann A, Zeller H, Niedrig M. 2016. External quality assessment studies for laboratory performance of molecular and serological diagnosis of chikungunya virus infection. J Clin Virol 76:55–65. doi: 10.1016/j.jcv.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 140.Panning M, Charrel RN, Donoso Mantke O, Mantke OD, Landt O, Niedrig M, Drosten C. 2009. Coordinated implementation of chikungunya virus reverse transcription-PCR. Emerg Infect Dis 15:469–471. doi: 10.3201/eid1503.081104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Anez G, Heisey DA, Rios M. 2014. Complete coding region sequence of a chikungunya virus strain used for formulation of CBER/FDA RNA reference reagents for nucleic acid testing. Genome Announc 2:e00587-14. doi: 10.1128/genomeA.00587-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Añez G, Jiang Z, Heisey DAR, Kerby S, Rios M, Drebot M, Holloway K, Lindsay R, Makowski K, Dugenny S, Petrich D, Kramer LD, Zink S, St George K, Dean A, Zeng L, Linnen J, Bres V, Powers A, Ledermann J, Weaver S, Langsjoen R, Seymour R. 2015. Collaborative study for the characterization of a chikungunya virus RNA reference reagent for use in nucleic acid testing. Vox Sang 109:312–318. doi: 10.1111/vox.12297. [DOI] [PubMed] [Google Scholar]
- 143.Grivard P, Le Roux K, Laurent P, Fianu A, Perrau J, Gigan J, Hoarau G, Grondin N, Staikowsky F, Favier F, Michault A. 2007. Molecular and serological diagnosis of chikungunya virus infection. Pathol Biol (Paris) 55:490–494. doi: 10.1016/j.patbio.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 144.Bandeira AC, Campos GS, Rocha VF, Souza BS, Soares MB, Oliveira AA, Abreu YC, Menezes GS, Sardi SI. 2016. Prolonged shedding of chikungunya virus in semen and urine: a new perspective for diagnosis and implications for transmission. IDCases 6:100–103. doi: 10.1016/j.idcr.2016.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kashyap RS, Morey SH, Chandak NH, Purohit HJ, Taori GM, Daginawala HF. 2010. Detection of viral antigen, IgM and IgG antibodies in cerebrospinal fluid of chikungunya patients with neurological complications. Cerebrospinal Fluid Res 7:12. doi: 10.1186/1743-8454-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shukla J, Khan M, Tiwari M, Sannarangaiah S, Sharma S, Rao PV, Parida M. 2009. Development and evaluation of antigen capture ELISA for early clinical diagnosis of chikungunya. Diagn Microbiol Infect Dis 65:142–149. doi: 10.1016/j.diagmicrobio.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 147.Andriamandimby SF, Heraud JM, Randrianasolo L, Rafisandratantsoa JT, Andriamamonjy S, Richard V. 2013. Dried-blood spots: a cost-effective field method for the detection of chikungunya virus circulation in remote areas. PLoS Negl Trop Dis 7:e2339. doi: 10.1371/journal.pntd.0002339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Matheus S, Huc P, Labeau B, Bremand L, Enfissi A, Merle O, Flusin O, Rousset D, Leparc-Goffart I. 2015. The use of serum spotted onto filter paper for diagnosing and monitoring chikungunya virus infection. J Clin Virol 71:89–92. doi: 10.1016/j.jcv.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 149.Litzba N, Schuffenecker I, Zeller H, Drosten C, Emmerich P, Charrel R, Kreher P, Niedrig M. 2008. Evaluation of the first commercial chikungunya virus indirect immunofluorescence test. J Virol Methods 149:175–179. doi: 10.1016/j.jviromet.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 150.Prat CM, Flusin O, Panella A, Tenebray B, Lanciotti R, Leparc-Goffart I. 2014. Evaluation of commercially available serologic diagnostic tests for chikungunya virus. Emerg Infect Dis 20:2129–2132. doi: 10.3201/eid2012.141269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Niedrig M, Zeller H, Schuffenecker I, Drosten C, Emmerich P, Rumer L, Donoso-Mantke O. 2009. International diagnostic accuracy study for the serological detection of chikungunya virus infection. Clin Microbiol Infect 15:880–884. doi: 10.1111/j.1469-0691.2009.02851.x. [DOI] [PubMed] [Google Scholar]
- 152.Wasonga C, Inoue S, Kimotho J, Morita K, Ongus J, Sang R, Musila L. 2015. Development and evaluation of an in-house IgM-capture ELISA for the detection of chikungunya and its application to a dengue outbreak situation in Kenya in 2013. Jpn J Infect Dis 68:410–414. doi: 10.7883/yoken.JJID.2014.482. [DOI] [PubMed] [Google Scholar]
- 153.Galo SS, Gonzalez K, Tellez Y, Garcia N, Perez L, Gresh L, Harris E, Balmaseda A. 2017. Development of in-house serological methods for diagnosis and surveillance of chikungunya. Rev Panam Salud Publica 41:e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Glasker S, Lulla A, Lulla V, Couderc T, Drexler JF, Liljestrom P, Lecuit M, Drosten C, Merits A, Kummerer BM. 2013. Virus replicon particle based chikungunya virus neutralization assay using Gaussia luciferase as readout. Virol J 10:235. doi: 10.1186/1743-422X-10-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Erasmus JH, Needham J, Raychaudhuri S, Diamond MS, Beasley DW, Morkowski S, Salje H, Fernandez Salas I, Kim DY, Frolov I, Nasar F, Weaver SC. 2015. Utilization of an Eilat virus-based chimera for serological detection of chikungunya infection. PLoS Negl Trop Dis 9:e0004119. doi: 10.1371/journal.pntd.0004119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Johnson BW, Goodman CH, Holloway K, de Salazar PM, Valadere AM, Drebot MA. 2016. Evaluation of commercially available chikungunya virus immunoglobulin M detection assays. Am J Trop Med Hyg 95:182–192. doi: 10.4269/ajtmh.16-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kosasih H, Widjaja S, Surya E, Hadiwijaya SH, Butarbutar DP, Jaya UA, Nurhayati, Alisjahbana B, Williams M. 2012. Evaluation of two IgM rapid immunochromatographic tests during circulation of Asian lineage chikungunya virus. Southeast Asian J Trop Med Public Health 43:55–61. [PubMed] [Google Scholar]
- 158.Rianthavorn P, Wuttirattanakowit N, Prianantathavorn K, Limpaphayom N, Theamboonlers A, Poovorawan Y. 2010. Evaluation of a rapid assay for detection of IgM antibodies to chikungunya. Southeast Asian J Trop Med Public Health 41:92–96. [PubMed] [Google Scholar]
- 159.Chua CL, Sam IC, Merits A, Chan YF. 2016. Antigenic variation of East/Central/South African and Asian chikungunya virus genotypes in neutralization by immune sera. PLoS Negl Trop Dis 10:e0004960. doi: 10.1371/journal.pntd.0004960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bhatnagar S, Kumar P, Mohan T, Verma P, Parida MM, Hoti SL, Rao DN. 2015. Evaluation of multiple antigenic peptides based on the chikungunya E2 protein for improved serological diagnosis of infection. Viral Immunol 28:107–112. doi: 10.1089/vim.2014.0031. [DOI] [PubMed] [Google Scholar]
- 161.Fumagalli MJ, de Souza WM, Esposito DLA, Silva A, Romeiro MF, Martinez EZ, da Fonseca BAL, Figueiredo L. 2018. Enzyme-linked immunosorbent assay using recombinant envelope protein 2 antigen for diagnosis of chikungunya virus. Virol J 15:112. doi: 10.1186/s12985-018-1028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Yathi KK, Joseph JM, Bhasker S, Kumar R, Chinnamma M. 2011. Recombinant CHIK virus E1 coat protein of 11 KDa with antigenic domains for the detection of chikungunya. J Immunol Methods 372:171–176. doi: 10.1016/j.jim.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 163.Verma A, Chandele A, Nayak K, Kaja MK, Arulandu A, Lodha R, Ray P. 2016. High yield expression and purification of chikungunya virus E2 recombinant protein and its evaluation for serodiagnosis. J Virol Methods 235:73–79. doi: 10.1016/j.jviromet.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 164.Chua CL, Chan YF, Sam IC. 2014. Characterisation of mouse monoclonal antibodies targeting linear epitopes on chikungunya virus E2 glycoprotein. J Virol Methods 195:126–133. doi: 10.1016/j.jviromet.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 165.Kumar J, Khan M, Gupta G, Bhoopati M, Lakshmana Rao PV, Parida M. 2012. Production, characterization, and application of monoclonal antibodies specific to recombinant (E2) structural protein in antigen-capture ELISA for clinical diagnosis of chikungunya virus. Viral Immunol 25:153–160. doi: 10.1089/vim.2011.0068. [DOI] [PubMed] [Google Scholar]
- 166.Cho B, Jeon BY, Kim J, Noh J, Kim J, Park M, Park S. 2008. Expression and evaluation of chikungunya virus E1 and E2 envelope proteins for serodiagnosis of chikungunya virus infection. Yonsei Med J 49:828–835. doi: 10.3349/ymj.2008.49.5.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Priya R, Khan M, Rao MK, Parida M. 2014. Cloning, expression and evaluation of diagnostic potential of recombinant capsid protein based IgM ELISA for chikungunya virus. J Virol Methods 203:15–22. doi: 10.1016/j.jviromet.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 168.Goh LY, Kam YW, Metz SW, Hobson-Peters J, Prow NA, McCarthy S, Smith DW, Pijlman GP, Ng LF, Hall RA. 2015. A sensitive epitope-blocking ELISA for the detection of chikungunya virus-specific antibodies in patients. J Virol Methods 222:55–61. doi: 10.1016/j.jviromet.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 169.Okabayashi T, Sasaki T, Masrinoul P, Chantawat N, Yoksan S, Nitatpattana N, Chusri S, Morales Vargas RE, Grandadam M, Brey PT, Soegijanto S, Mulyantno KC, Churrotin S, Kotaki T, Faye O, Faye O, Sow A, Sall AA, Puiprom O, Chaichana P, Kurosu T, Kato S, Kosaka M, Ramasoota P, Ikuta K. 2015. Detection of chikungunya virus antigen by a novel rapid immunochromatographic test. J Clin Microbiol 53:382–388. doi: 10.1128/JCM.02033-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Huits R, Okabayashi T, Cnops L, Barbe B, Van Den Berg R, Bartholomeeusen K, Arien KK, Jacobs J, Bottieau E, Nakayama EE, Shioda T, Van Esbroeck M. 2018. Diagnostic accuracy of a rapid E1-antigen test for chikungunya virus infection in a reference setting. Clin Microbiol Infect 24:78–81. doi: 10.1016/j.cmi.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 171.Jain J, Okabayashi T, Kaur N, Nakayama E, Shioda T, Gaind R, Kurosu T, Sunil S. 2018. Evaluation of an immunochromatography rapid diagnosis kit for detection of chikungunya virus antigen in India, a dengue-endemic country. Virol J 15:84. doi: 10.1186/s12985-018-1000-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Thiberville SD, Moyen N, Dupuis-Maguiraga L, Nougairede A, Gould EA, Roques P, de Lamballerie X. 2013. Chikungunya fever: epidemiology, clinical syndrome, pathogenesis and therapy. Antiviral Res 99:345–370. doi: 10.1016/j.antiviral.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Goh LY, Hobson-Peters J, Prow NA, Gardner J, Bielefeldt-Ohmann H, Pyke AT, Suhrbier A, Hall RA. 2013. Neutralizing monoclonal antibodies to the E2 protein of chikungunya virus protects against disease in a mouse model. Clin Immunol 149:487–497. doi: 10.1016/j.clim.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 174.Broeckel R, Fox JM, Haese N, Kreklywich CN, Sukulpovi-Petty S, Legasse A, Smith PP, Denton M, Corvey C, Krishnan S, Colgin LMA, Ducore RM, Lewis AD, Axthelm MK, Mandron M, Cortez P, Rothblatt J, Rao E, Focken I, Carter K, Sapparapau G, Crowe JE Jr, Diamond MS, Streblow DN. 2017. Therapeutic administration of a recombinant human monoclonal antibody reduces the severity of chikungunya virus disease in rhesus macaques. PLoS Negl Trop Dis 11:e0005637. doi: 10.1371/journal.pntd.0005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tharmarajah K, Mahalingam S, Zaid A. 2017. Chikungunya: vaccines and therapeutics. F1000Res 6:2114. doi: 10.12688/f1000research.12461.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Elsinga J, Gerstenbluth I, van der Ploeg S, Halabi Y, Lourents NT, Burgerhof JG, van der Veen HT, Bailey A, Grobusch MP, Tami A. 2017. Long-term chikungunya sequelae in Curacao: burden, determinants, and a novel classification tool. J Infect Dis 216:573–581. doi: 10.1093/infdis/jix312. [DOI] [PubMed] [Google Scholar]
- 177.van Aalst M, Nelen CM, Goorhuis A, Stijnis C, Grobusch MP. 2017. Long-term sequelae of chikungunya virus disease: a systematic review. Travel Med Infect Dis 15:8–22. doi: 10.1016/j.tmaid.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 178.Paixao ES, Rodrigues LC, Costa M, Itaparica M, Barreto F, Gerardin P, Teixeira MG. 2018. Chikungunya chronic disease: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg 112:301–316. doi: 10.1093/trstmh/try063. [DOI] [PubMed] [Google Scholar]
- 179.Edington F, Varjao D, Melo P. 2018. Incidence of articular pain and arthritis after chikungunya fever in the Americas: a systematic review of the literature and meta-analysis. Joint Bone Spine 85:669–678. doi: 10.1016/j.jbspin.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 180.Huits R, De Kort J, Van Den Berg R, Chong L, Tsoumanis A, Eggermont K, Bartholomeeusen K, Arien KK, Jacobs J, Van Esbroeck M, Bottieau E, Cnops L. 2018. Chikungunya virus infection in Aruba: diagnosis, clinical features and predictors of post-chikungunya chronic polyarthralgia. PLoS One 13:e0196630. doi: 10.1371/journal.pone.0196630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Freitas ARR, Alarcon-Elbal PM, Donalisio MR. 2018. Excess mortality in Guadeloupe and Martinique, islands of the French West Indies, during the chikungunya epidemic of 2014. Epidemiol Infect 146:2059–2065. doi: 10.1017/S0950268818002315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Mavalankar D, Shastri P, Bandyopadhyay T, Parmar J, Ramani KV. 2008. Increased mortality rate associated with chikungunya epidemic, Ahmedabad, India. Emerg Infect Dis 14:412–415. doi: 10.3201/eid1403.070720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Freitas ARR, Alarcón-Elbal PM, Paulino-Ramírez R, Donalisio MR. 2018. Excess mortality profile during the Asian genotype chikungunya epidemic in the Dominican Republic, 2014. Trans R Soc Trop Med Hyg 112:443–449. doi: 10.1093/trstmh/try072. [DOI] [PubMed] [Google Scholar]
- 184.Hoz JM, Bayona B, Viloria S, Accini JL, Juan-Vergara HS, Viasus D. 2015. Fatal cases of chikungunya virus infection in Colombia: diagnostic and treatment challenges. J Clin Virol 69:27–29. doi: 10.1016/j.jcv.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 185.Auerswald H, Boussioux C, In S, Mao S, Ong S, Huy R, Leang R, Chan M, Duong V, Ly S, Tarantola A, Dussart P. 2018. Broad and long-lasting immune protection against various chikungunya genotypes demonstrated by participants in a cross-sectional study in a Cambodian rural community. Emerg Microbes Infect 7:1–13. doi: 10.1038/s41426-017-0010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Nitatpattana N, Kanjanopas K, Yoksan S, Satimai W, Vongba N, Langdatsuwan S, Nakgoi K, Ratchakum S, Wauquier N, Souris M, Auewarakul P, Gonzalez J-P. 2014. Long-term persistence of chikungunya virus neutralizing antibodies in human populations of North Eastern Thailand. Virol J 11:183. doi: 10.1186/1743-422X-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rezza G, Weaver SC. 2019. Chikungunya as a paradigm for emerging viral diseases: evaluating disease impact and hurdles to vaccine development. PLoS Negl Trop Dis 13:e0006919. doi: 10.1371/journal.pntd.0006919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Powers AM. 2018. Vaccine and therapeutic options to control chikungunya virus. Clin Microbiol Rev 31:e00104-16. doi: 10.1128/CMR.00104-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Powers AM. 2019. Licensed chikungunya virus vaccine: a possibility? Lancet 392:2660–2661. doi: 10.1016/S0140-6736(18)32809-5. [DOI] [PubMed] [Google Scholar]
- 190.Kinjo AR, Suzuki H, Yamashita R, Ikegawa Y, Kudou T, Igarashi R, Kengaku Y, Cho H, Standley DM, Nakagawa A, Nakamura H. 2012. Protein Data Bank Japan (PDBj): maintaining a structural data archive and resource description framework format. Nucleic Acids Res 40:D453–D460. doi: 10.1093/nar/gkr811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sun S, Xiang Y, Akahata W, Holdaway H, Pal P, Zhang X, Diamond MS, Nabel GJ, Rossmann MG. 2013. Structural analyses at pseudo atomic resolution of chikungunya virus and antibodies show mechanisms of neutralization. Elife 2:e00435. doi: 10.7554/eLife.00435. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.