Abstract
Purpose
Diagnostic criteria for monoclonal gammopathy of undetermined significance (MGUS) do not currently include ocular phenotypic changes. Here, we offer a new diagnostic approach that is useful in patients with posteriorly located corneal depositions and present evidence to support the theory that the aqueous humor is a source for monoclonal proteins accumulated in the cornea.
Observations
A 77-year-old woman presented to the clinic with a gradual decrease in visual acuity over 6 months. Slit lamp examination revealed bilateral central guttae consistent with Fuchs corneal dystrophy, peripheral circular band-like corneal opacities in the deep stroma, and bilateral nuclear sclerotic and cortical cataracts. Anterior segment optical coherence tomography confirmed corneal opacities in the posterior stroma and Descemet membrane. Immunological studies revealed increased serum IgG levels of 3220 mg/dL and serum electrophoresis showed an abnormal monoclonal band of 2.4 g/dL identified as IgG lambda by immunofixation electrophoresis. The patient was referred to the hematology clinic where she underwent further systemic workup and was diagnosed with MGUS. Immunofixation electrophoresis of aqueous sampling, which was performed at the time of cataract surgery, confirmed the presence of the IgG lambda gammopathy in the anterior chamber.
Conclusions and importance
Monoclonal gammopathy, although rare, should be included in the differential diagnosis of corneal opacities, as the ocular finding can be the initial manifestation of a systemic disease that can potentially be life-threatening. When corneal biopsy is not feasible due to the location of corneal pathology, aqueous sampling may be an alternative approach towards a clinical diagnosis. We propose a new terminology, “monoclonal gammopathy of ocular significance,” for patients diagnosed with MGUS, however, their only significant clinical finding is ocular manifestation.
Keywords: Cornea, Deposition, Monoclonal gammopathy of undetermined significance, Paraproteinemic keratopathy, Lambda, Immunofixation
Introduction
Monoclonal gammopathies are disorders of B lymphocytes where one (rarely two) plasma cell overproduces an identical type of immunoglobulin, typically composed of a heavy and a light immunoglobulin chain, but occasionally made up of a light chain only (Bence Jones protein) or rarely a heavy chain only.1 The presence of a monoclonal immunoglobulin, and thus a malignant plasma cell clone, is typically heralded by the appearance of a spike in the serum and/or urine electrophoresis. This spike is subsequently typed by immunofixation electrophoresis to identify the type of the heavy chain and the light chain that make up the monoclonal immunoglobulin.1 The most common gammopathies are multiple myeloma and monoclonal gammopathy of undetermined significance (MGUS), both of which primarily affects plasma cells.1,2 MGUS features the same presence of a monoclonal immunoglobulin as multiple myeloma (although at a concentration lower than 3 g/dL), but lacks evidence of any end organ damage such as bone lesions, hypercalcemia, renal insufficiency, anemia, and recurrent bacterial infections and has fewer than 10% clonal plasma cells in the bone marrow.1 Nevertheless, MGUS is considered a premalignant condition since the risk of progressing to multiple myeloma is about 1% per year.2 MGUS is common, with a prevalence of about 3–4% in the population over the age of 50.1
Corneal involvement in gammopathies is very rare (less than 1%) and has a highly variable presentation that may cause misdiagnosis.3 In fact, a recent case series that included a literature review of all published studies of MGUS with paraproteinemic keratopathy defined 17 different patterns among patients with MGUS.4 No cases, to our knowledge, have reported Fuchs corneal dystrophy (FCD) with corneal deposition due to monoclonal gammopathy. We present a case of FCD with bilateral deep stromal opacities, later diagnosed with IgG lambda monoclonal gammopathy. We discuss possible influences of FCD on corneal deposition, alternative approaches to support the diagnosis such as aqueous sampling for detection of monoclonal proteins, and effects of a combination of both conditions on refractive outcomes. We also propose a new terminology for patients with MGUS when ocular findings are the only systemic manifestation of the disease.
Case report
A 77-year-old white female was referred to our clinic for gradually decreasing vision in both eyes over the past 6 months. She was known to have FCD and age-related cataract and was referred for surgical management of cataract. She complained of gradually decreasing vision and mild glare but had no systemic symptoms at the time of the presentation. Best corrected visual acuity was 20/30 in the right eye and 20/80 in the left eye. Slit lamp examination demonstrated bilateral peripheral circular band-like, gray-white deep stromal/pre-Descemet opacities with filamentous edges sparing central and perilimbal areas (Fig. 1). In addition, she had confluent guttae in the central cornea without stromal edema and nuclear sclerotic and cortical cataracts in both eyes which were more significant in the left eye. Ultrasound pachymetry revealed central corneal thickness of 571 μm in the right eye and 551 μm in the left eye. Anterior segment optical coherence tomography (OCT) (Visante OCT, Carl Zeiss Meditec, Inc., Dublin, CA) confirmed opacities in deep stromal layers and at the level of Descemet membrane (Fig. 2).
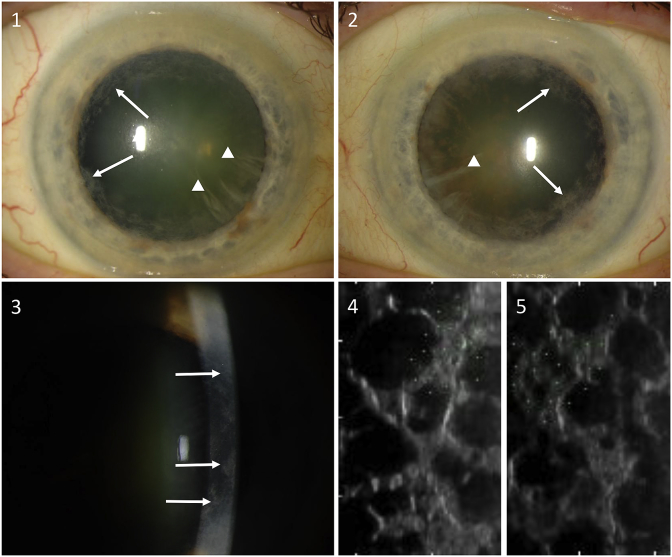
Fig. 1.
Slit-lamp photographs show peripheral circular band-like, gray-white corneal opacities (arrows) and cortical cataracts appearing as wedge-like lenticular opacities (arrowheads) in the right eye (1) and the left eye (2). Direct slit beam shows deep stromal/pre-Descemet opacities (arrows) (3). Specular microscopy images (CellChek XL, Konan Medical USA, Irvine, CA) demonstrate confluent corneal guttae in the right eye (4) and the left eye (5).
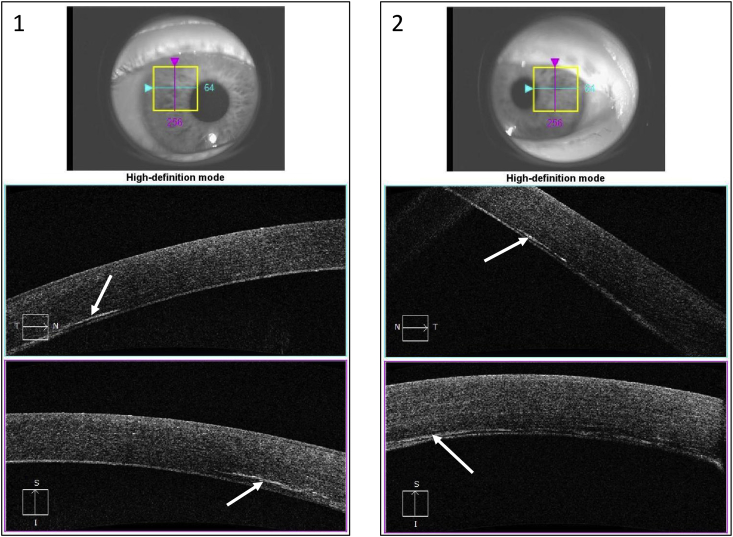
Fig. 2.
Anterior segment optical coherence tomography (Visante OCT, Carl Zeiss Meditec, Inc., Dublin, CA) demonstrates opacities (arrows) in deep stromal layers and at the level of Descemet membrane of the right eye (1) and left eye (2).
Workup for corneal deposits included immunological studies that revealed an increased gamma region by serum protein electrophoresis of 2.4 g/dL (normal, 0.7–1.7 g/dL) and increased immunoglobulin G (IgG) by nephelometry of 3220 mg/dL (normal, 751–1560 mg/dL). The increased gamma region was caused by a monoclonal spike of 1.96 g/dL, which was then identified as IgG lambda by immunofixation electrophoresis. The patient was referred to a hemato-oncologist who established a diagnosis of MGUS, as opposed to multiple myeloma, based on monoclonal spike value less than 3 g/dL, absence of hypermetabolic lytic lesions in skeletal bone survey, increased plasma cell in the bone marrow biopsy but still under 10%, lack of anemia, hypercalcemia, or renal insufficiency. Close clinical observation was recommended without intervention.
To address visual complaints, we performed cataract surgery alone as corneal opacities were peripheral and edema was mild. Corneal biopsy for histopathologic (histological and immunohistochemical examination) diagnosis of the lesions was not planned due to deep location of opacities. During cataract surgery, samples of aqueous humor, lens capsule, and lens material were collected and submitted for analysis. Histopathologic studies of the lens capsule and lens material did not show any abnormal protein deposition using immunohistochemical stains. Protein electrophoresis and nephelometry were not able to detect any immunoglobulins. However, immunofixation electrophoresis revealed the presence of a faint band in the G lane with a corresponding, albeit fainter, band in the lambda lane, thus confirming the IgG lambda gammopathy described in the serum.
Visual acuity in the operated eye improved from 20/80 to 20/20 with +0.75 of spherical correction at 1 month, reaching 20/20 without correction at 5 months. Corneal thickness measured at the apex using the Pentacam corneal topography system (Oculus, Inc., Arlington, WA) was 564 μm preoperatively, 612 μm at 1 month, and 580 μm at 5 months (Fig. 3).
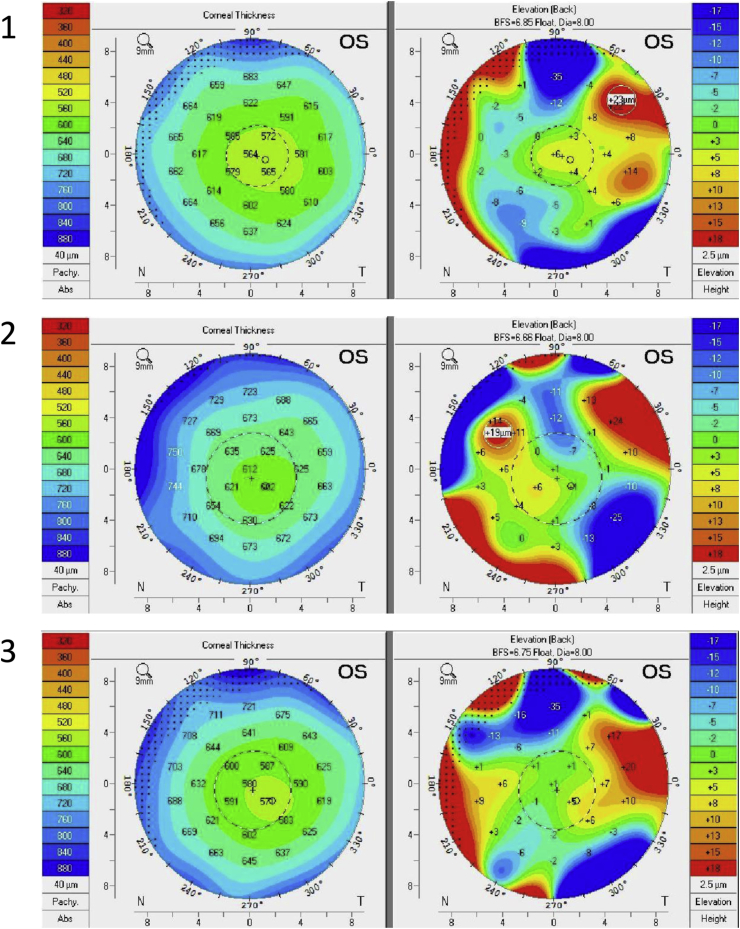
Fig. 3.
Corneal thickness and posterior elevation maps using the Pentacam corneal topography system (Oculus, Inc., Arlington, WA) in the left eye preoperatively (1), at 1-month postoperative visit (2), and at 5 months postoperative visit (3).
Discussion
This report demonstrates that aqueous sampling for protein electrophoresis can be used as an alternative diagnostic approach in cases that a corneal biopsy is not feasible. Further, our results emphasize that immunofixation electrophoresis should always follow protein electrophoresis since its sensitivity is significantly greater. In this case report, we present further evidence to support the theory that the aqueous humor is indeed a source for monoclonal proteins. Finally, although complex due to concurrent corneal pathology, we highlight the importance of considering the complete visual axis in such patients since cataract surgery significantly improved visual acuity in this patient.
Indeed, corneal deposition of monoclonal proteins presents with variable clinical signs and symptoms in the literature.3, 4, 5 A proposed cause for such variability in appearance is the diversity of the light chain structure itself,6 and patient-specific factors such as corneal endothelial viability that may modulate deposition.7 In the absence of clinically evident corneal opacity, confocal microscopy can be used to reveal structural changes throughout all corneal layers except the endothelium.8 We hypothesize that endothelial dysfunction secondary to FCD may have contributed to the posterior locus of the deposits in our patient. It is unclear, however, why the central cornea was spared, although thickened Descemet membrane and guttae may have prevented the transition of the proteins into the central cornea. To our knowledge, this is the first case report of paraproteinemic keratopathy in a patient with FCD. Further studies are needed to understand the possible role of FCD in the pathophysiology of paraproteinemic keratopathy, particularly in cases with posterior deposition.
Diagnosis of paraproteinemic keratopathy is usually made by identification of monoclonal gammopathy in serum using protein electrophoresis and abnormal protein deposition on corneal biopsy specimen using immunohistochemical stains.3 When located anteriorly, a corneal biopsy can be easily performed for histopathologic diagnosis. However, when located posteriorly, a corneal biopsy is usually not feasible. In cases with central corneal involvement affecting vision significantly, a penetrating or lamellar keratoplasty is usually planned, and histopathologic evaluation of the corneal button confirms the diagnosis. In our case, we were unable to perform a biopsy as the opacities were located in the deep stroma. We submitted the anterior lens capsule and lens material collected during the cataract extraction for histologic and immunohistochemical studies to support the diagnosis; however, no sign of abnormal protein deposition was seen in these tissues.
Although the source of monoclonal proteins is difficult to determine, posterior deposition of the abnormal proteins has been postulated to arise from the high aqueous concentration of the monoclonal protein.9 Our case highlights the importance of a multifaceted approach to maximize sensitivity in detection of monoclonal proteins and offer evidence to support the theory that the aqueous is the source of monoclonal proteins that accumulate within the corneal layers. IgG and kappa light chains appear in aqueous samples of patients with multiple myeloma using protein electrophoresis,10,11 but in a comparable case with deep corneal opacities associated with B-cell lymphoma, protein electrophoresis of an aqueous sample did not demonstrate monoclonal protein.12 In our case, protein electrophoresis and nephelometry of aqueous also revealed no band; however, immunofixation electrophoresis showed a faint band of IgG and lambda light chain. The principles of these techniques differ from each other. Protein electrophoresis is a technique separating particles in a liquid sample based on their electrical charge. Nephelometry detects particles in a liquid sample by measuring the scattered light when a laser beam passes through the liquid, and the particles deflect the light. Immunofixation electrophoresis is a two-step approach and takes place after proteins are separated using protein electrophoresis to identify a specific protein. A fluorescent antibody against a certain protein is added and glows if the targeted protein is present in the sample. Immunofixation electrophoresis has a higher sensitivity (limit of detection of approximately 100 mg/L) than protein electrophoresis (limit of detection of 500 mg/L) and therefore a negative protein electrophoresis result does not exclude a monoclonal gammopathy.13 We suggest negative results with protein electrophoresis should always be followed by immunofixation electrophoresis.
The refractive outcome of cataract surgery in this case varied over several months, likely reflecting a process associated with FCD. Both a change in posterior corneal curvature and density of the cornea with altered hydration may contribute to refractive changes. Whether peripheral corneal deposition contributed to visual aberrations postoperatively remains unclear.
Recently, a new terminology “monoclonal gammopathy of renal significance” was proposed to be used in patients who do not meet hematologic criteria for multiple myeloma but demonstrate renal pathology secondary to monoclonal proteins.14 Such classification distinguishes patients who demonstrate pathology or require treatment from patients with truly benign MGUS. Authors suggested that the term MGUS should be limited to those cases where no connection to end organ damage can be demonstrated.14 We propose the term “monoclonal gammopathy of ocular significance” when only ocular disease can be demonstrated, but the patient is healthy otherwise. We believe that such a classification is necessary to distinguish patients with ocular involvement in the setting of MGUS from patients with no ocular involvement. It would also be important to differentiate them from patients with ocular involvement but in the setting of more serious gammopathies, such as multiple myeloma. This classification may also be utilized in research studies to achieve uniformity when selecting the study participants.
Conclusions
In the absence of a distinct pattern in presentation, we recommend a high index of suspicion for monoclonal gammopathy in patients with unexplained stromal opacities. Aqueous sampling can be an alternative approach to support the diagnosis when a corneal biopsy is not possible.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support.
Conflicts of interest
The authors have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2019.100471.
Contributor Information
Sezen Karakus, Email: skaraku1@jhmi.edu.
John D. Gottsch, Email: jgottsch@jhmi.edu.
Patrizio Caturegli, Email: pcat@jhmi.edu.
Allen O. Eghrari, Email: allen@jhmi.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Rajkumar S.V., Dimopoulos M.A., Palumbo A. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–e548. doi: 10.1016/S1470-2045(14)70442-5. [DOI] [PubMed] [Google Scholar]
- 2.Kyle R.A., Therneau T.M., Rajkumar S.V. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346:564–569. doi: 10.1056/NEJMoa01133202. [DOI] [PubMed] [Google Scholar]
- 3.Garibaldi D.C., Gottsch J., de la Cruz Z. Immunotactoid keratopathy: a clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemias. Surv Ophthalmol. 2005;50:61–80. doi: 10.1016/j.survophthal.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Lisch W., Wasielica-Poslednik J., Kivelä T. The hematologic definition of monoclonal gammopathy of undetermined significance in relation to paraproteinemic keratopathy (an American ophthalmological society thesis) Trans Am Ophthalmol Soc. 2016;114:T7. [PMC free article] [PubMed] [Google Scholar]
- 5.Milman T., Kao A.A., Chu D. Paraproteinemic keratopathy: the expanding diversity of clinical and pathologic manifestations. Ophthalmology. 2015;122:1748–1756. doi: 10.1016/j.ophtha.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 6.Lisch W., Saikia P., Pitz S. Chameleon-like appearance of immunotactoid keratopathy. Cornea. 2012;31:55–58. doi: 10.1097/ICO.0b013e31821ddd0c. [DOI] [PubMed] [Google Scholar]
- 7.Graichen D.F., Perez E., Jones D.B. kappa-Immunoglobulin corneal deposits associated with monoclonal gammopathy. Immunohistochemical and electron microscopic findings. Ger J Ophthalmol. 1994;3:54–57. [PubMed] [Google Scholar]
- 8.Aragona P., Allegra A., Postorino E.I. Corneal structural changes in nonneoplastic and neoplastic monoclonal gammopathies. Investig Ophthalmol Vis Sci. 2016;57:2657–2665. doi: 10.1167/iovs.15-18594. [DOI] [PubMed] [Google Scholar]
- 9.Ormerod L.D., Collin H.B., Dohlman C.H. Paraproteinemic crystalline keratopathy. Ophthalmology. 1988;95:202–212. doi: 10.1016/s0161-6420(88)33200-8. [DOI] [PubMed] [Google Scholar]
- 10.Steuhl K.P., Knorr M., Rohrbach J.M. Paraproteinemic corneal deposits in plasma cell myeloma. Am J Ophthalmol. 1991;111:312–318. doi: 10.1016/s0002-9394(14)72315-3. [DOI] [PubMed] [Google Scholar]
- 11.Green E.D., Morrison L.K., Love P.E. A structurally aberrant immunoglobulin paraprotein in a patient with multiple myeloma and corneal crystal deposits. Am J Med. 1990;88:304–311. doi: 10.1016/0002-9343(90)90159-b. [DOI] [PubMed] [Google Scholar]
- 12.Matoba A.Y., Chevez-Barrios P., Jones D.B. Atypical corneal immunoglobulin deposition in a patient with dysproteinemia. Cornea. 2010;29:105–107. doi: 10.1097/ICO.0b013e31819e34ab. [DOI] [PubMed] [Google Scholar]
- 13.Willrich M.A.V., Murray D.L., Kyle R.A. Laboratory testing for monoclonal gammopathies: focus on monoclonal gammopathy of undetermined significance and smoldering multiple myeloma. Clin Biochem. 2018;51:38–47. doi: 10.1016/j.clinbiochem.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Leung N., Bridoux F., Hutchison C.A. International Kidney and Monoclonal Gammopathy Research Group. Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant. Blood. 2012;120:4292–4295. doi: 10.1182/blood-2012-07-445304. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.