Abstract
The aim of this review was to identify patient-focused interventions that have been trialed to support vulnerable patient populations taking oral anticoagulants (warfarin and the direct-acting oral anticoagulants (DOACs)) such as older persons (65 years and over), those with limited health literacy, and those from culturally and linguistically diverse (CALD) backgrounds. This review also aimed to report on the effects of these interventions on outcomes relevant to the use of anticoagulant therapy. Original articles published between 1 January 1995 and 30 June 2017 were identified using several electronic databases such as Medline, Ovid, Embase, Scopus, Cochrane, and Google Scholar. The following terms were used for the three-tiered search: Tier 1, elderly, aged, older adult, geriatrics; Tier 2, health literacy, literacy, low health literacy, low English proficiency, patient literacy; and Tier 3, ethnicity, ethnic, ethnic groups, CALD, culturally and linguistically diverse, NESB, non-English speaking background, race, racial groups, religion, religious groups, and minority groups. The terms for each tier were combined with the following terms: anticoagulants, anticoagulation, warfarin, apixaban, dabigatran, rivaroxaban, DOACS, new oral anticoagulants, novel oral anticoagulants, patient care, patient knowledge, comprehension, patient education, patient participation, and communication. A total of 41 studies were identified. Most of the interventions identified included older persons taking warfarin who were monitored using the international normalized ratio (INR) and who received patient education. Many interventions reported a significant positive impact on patients’ knowledge, reduction in the number of adverse events caused by hemorrhage, and better INR control. More research on patient-focused interventions is needed that includes patients with limited health literacy, those from CALD backgrounds, and family members and caregivers of patients taking oral anticoagulants.
Keywords: anticoagulants, warfarin, DOACS, medication safety, elderly, health literacy, culturally and linguistically diverse, CALD, patient education, patient knowledge
Introduction
Medication-related problems, such as unsafe medication practices and medication errors, are leading causes of avoidable harm in healthcare systems throughout the world and may be serious enough to cause disability or death.1 Medication problems can occur when patients take high-alert medications, such as oral anticoagulants, which have a high risk of severe harm if used improperly.1–3 Vulnerable patient populations, such as older persons, those with limited health literacy, and those from culturally and linguistically diverse (CALD) backgrounds, are at risk of experiencing medication problems for several reasons. Older persons taking anticoagulants are at risk of adverse events such as bleeding because they often have multiple comorbidities, severe chronic kidney disease, age-related functional and cognitive decline, or polypharmacy, all of which can increase their risk of clinically relevant drug–drug interactions.4,5
Patients with limited health literacy are likely to have little understanding of the use of warfarin6 and may struggle to understand written materials provided to them.7,8 This can reduce their adherence and increase the risk of adverse events such as bleeding.9 In addition, patients from CALD backgrounds may have differing cultural perceptions or beliefs about prescribed treatment. Religious influences, language and communication barriers, inadequate use of interpreters, poor understanding of healthcare services, and socioeconomic barriers can limit their access to the healthcare system.10 The literature shows that patients from CALD backgrounds require information about medication to help them manage their use of medications.11–13 A patient-centered care approach is one way to support these vulnerable patient populations taking oral anticoagulants and to protect them from harm.14,15
Several literature reviews have focused on educational, behavioral, and self-monitoring and self-management interventions for patients taking oral anticoagulant therapy.16–21 We chose to take a narrative review approach to gather different types of evidence from both qualitative and quantitative research22 and to synthesize this information to provide a comprehensive overview of this broad area of research. We used this narrative review approach to ensure the inclusion of full-text articles, published conference abstracts, and studies of populations with limited health literacy and CALD backgrounds. We reasoned that the information gathered from the diverse types of studies of warfarin could be applied to the design of future interventions involving direct-acting oral anticoagulants (DOACs) that are patient focused and cost-effective.
The specific objectives of this review were:
1) to describe the range of interventions developed, implemented, and evaluated to support vulnerable patients using anticoagulant therapies (i.e. warfarin or one of the DOACs);
2) to report on the impact of these interventions on outcomes relevant to the use of anticoagulant therapy.
Definitions
Vulnerable populations
We defined a vulnerable population as those people who are at risk of medication-related problems.4,10,23,24 Studies that included the following people were included: older persons, those with limited health literacy and those from CALD backgrounds.
Older persons
We defined older persons as those aged 65 years or over.25,26
Limited health literacy
The World Health Organization (WHO) defines health literacy as ‘the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health’.27
The articles identified in this review used different tools to measure the level of health literacy.28–31 These included The Rapid Estimate of Adult Literacy in Medicine (REALM) tool32 and the shortened version of the Test of Functional Health Literacy in Adults (S-TOFHLA).33 Newer tools such as the Health Literacy Questionnaire34 are available to access health literacy, however, were not identified in this review.
CALD patients
In Australia, CALD has been defined as those people born overseas in countries other than those classified by the Australian Bureau of Statistics as ‘main English-speaking countries’. Others terms used to describe CALD include ‘ethnic minorities’,10,13 ‘multicultural’, ‘migrant’, and ‘from a non-English speaking background’.35
Methods
A structured search of the literature was performed as described in the following.
Data sources
The following electronic databases were searched to retrieve original articles, review papers, and other publications published from 1 January 1995 to 30 June 2017: Medline, Ovid, Embase, Scopus, the Cochrane Library, and the search platform Google Scholar. This time frame represents the period after which pivotal trials of anticoagulation therapy for stroke prevention in atrial fibrillation were conducted and published, which lead to an increase in the prescribing of these agents as well as exploration into the factors affecting their safe use.20 This time frame also incorporates the advent of alternative anticoagulants (i.e. the DOACs), which are a major focus of the current anticoagulation prescribing.36,37
Search strategy and search terms
A three-tiered search strategy was used for each patient population: older persons (Tier 1); those with low literacy (Tier 2); and those from CALD backgrounds (Tier 3). The search was conducted by combining the US National Library of Medicine Medical Subject Heading terms and specific search terms related to oral anticoagulants and interventions. The following terms were used for each tier. Tier 1 included elderly, aged, older adult, and geriatrics. Tier 2 included health literacy, literacy, low health literacy, low English proficiency, and patient literacy. Tier 3 included ethnicity, ethnic, ethnic groups, CALD, culturally and linguistically diverse, NESB, non-English-speaking background, race, racial groups, religion, religious groups, and minority groups. The terms used for each tier were combined with the following keywords: anticoagulants, anticoagulation, warfarin, apixaban, dabigatran, rivaroxaban, new oral anticoagulants (or NOACs), novel oral anticoagulants, direct acting oral anticoagulant, DOACs, patient care, patient knowledge, comprehension, patient education, patient participation, and communication.
For the Scopus database, because of the number of articles, the term ‘older adult’ was used from Tier 1, ethnicity from Tier 2, and all terms from Tier 3.
Selection criteria
One author performed the search to identify relevant articles. Duplicates were removed, and the articles based on titles and abstracts were screened. For all articles, (including published conference abstracts),31,38 the full-text version was retrieved and assessed according to the objectives of this review. The reference lists of the retrieved articles and review articles were examined manually to identify further relevant studies not identified using the search strategy. The review procedure was verified by the co-researcher.
The studies were selected according to the following criteria: (1) involving a majority of people who were older persons (articles were limited to those including people aged 65 years and over identified using Medline and Embase), limited literacy, from a CALD background, and aged more than 18 years; (2) patient-focused interventions; (3) studies reporting the use of the oral anticoagulants warfarin and DOACs such as apixaban, rivaroxaban, and dabigatran; (4) studies reported in English; (5) original research articles; and (6) articles available in full text.
Case studies and articles without abstracts or full text were excluded. Articles that included programs supporting physicians and patients were excluded to ensure that the outcomes reported in this review reflected the impact of interventions that directly supported only patients. In addition, many studies have addressed the use of anticoagulants through the clinician’s lens by focusing on interventions to optimize the use of these agents. Although this focus is important, it only partially considers the barriers to the use of anticoagulants. What is also needed is a comprehensive range of interventions to support patients’ daily use of these agents and their long-term adherence. Although many resources are available in practice, few actually meet the needs of those patients who are most likely to need anticoagulation therapy but who are also more likely to experience difficulties (i.e. older persons, those with low literacy, and those from CALD backgrounds.
Data extraction
The following data were extracted from the included articles: author, publication year, setting, country, title of publication, trial design, type of intervention, subjects (number of patients, mean age in years, ethnicity/race, health literacy), and key findings ((Table 1, Table 2 and Table 3)).
Table 1.
INR monitoring interventions to support older persons.
| Authors, reference, setting, country | Title | Trial design | Patient intervention | Number of patients Mean age (years) |
Key finding(s) |
|---|---|---|---|---|---|
| Amruso et al.,39
Two community pharmacies, USA |
Ability of clinical pharmacists in a community pharmacy setting to manage anticoagulation therapy | Retrospective observational study | Clinical pharmacists monitored patients’ INRs using point-of-care analyzers, made dosage adjustments as needed, and provided patient education |
n = 50, Age >65 years: n = 42 (84%) |
• During the 6 months of initial therapy with warfarin, majority of INRs were in desired therapeutic ranges • A total of 15 bleeding episodes were reported, of which 10 were minor and 5 were significant. Significant bleeding episodes required referral • The patient satisfaction rate with the service (n = 11) was of above average to excellent |
| Harrison et al.,40
15 community pharmacies, New Zealand |
Anticoagulation management by community pharmacists in New Zealand: An evaluation of a collaborative model in primary care | Prospective cohort study | Pharmacist-led anticoagulation care using point-of-care INR testing and a computer decision support system for dose adjustments |
n = 671 Median age: 72 (age range from 13 to 97) |
• A subgroup analysis (n = 221) of patients who completed 16 and 26 weeks in the pharmacist-led service showed a significant increase in mean TTR compared with under GP-led care (p < 0.001) |
| Shaw et al.,41
15 community pharmacies, New Zealand |
A community pharmacist-led anticoagulation management service: Attitudes towards a new collaborative model of care in New Zealand | Observational descriptive study (qualitative study) | A collaborative community pharmacist-led anticoagulation management service (CPAMS) |
n = 412 patients completed the questionnaire Aged 65 years or over: 70.6% |
• The majority of patients reported: improved access of the service and convenience felt that it saved them time, a preference for capillary testing, found it helpful to receive a printed dose calendar and the immediacy of the test result and dose, found the pharmacist was able to help them with other aspects of their health care, had confidence that test results were reliable |
| Jackson et al.,42
16 rural, community pharmacies, Australia |
Improving the outcomes of anticoagulation in rural Australia: An evaluation of pharmacist-assisted monitoring of warfarin therapy | Prospective cohort study and patient satisfaction questionnaires | Rural Community Pharmacist training and INR monitoring of warfarin therapy, using POC testing via a portable CoaguChek S monitor compared with conventional laboratory testing |
n = 137 Median age: 72 |
• The pharmacy-based INR values (from a total of 120 tests) were significantly correlated with the laboratory INR values p < 0.0001) • Responses from satisfaction questionnaire revealed a majority of patients were satisfied with the monitoring by a pharmacist, rated the quality of the service as good or excellent, found that the monitoring service helped them to deal more effectively with warfarin, believed that the service should be available to all patients on warfarin and had a preference for the service to be provided in the pharmacy followed by the home and general practitioner’s surgery |
| Hodge et al.,43
Anticoagulation clinics, Australia |
Coordinated anticoagulation management in a rural setting. Australian family physician | Prospective cohort and survey | A Victorian rural program that incorporated an anticoagulation clinic, point of care INR testing in remote centers, development of anticoagulation dosing protocols for GP use and, a comprehensive patient education program |
n = 227 Median age: 72 |
• At one remote site, INRs were tested every 14 days resulting in a significantly higher median proportion of time in therapeutic range (78% of time, p = 0.0004) compared with Horsham (main site) • Patients consistently praised the program, and felt more comfortable taking warfarin after undertaking the education |
| Jackson et al.,44 Home-based follow-up of patients discharged from a 450-bed acute care teaching hospital, Australia | Improving the outcomes of anticoagulation: an evaluation of home follow-up of warfarin initiation. | Open-label RCT | A post-discharge home follow-up service by a pharmacist including home monitoring (HM), POC INR testing, telephone communication with the patient’s GP about the INR results and dosage changes, and counseling with a warfarin educational booklet and a double-sided A4 warfarin document |
n = 128 Mean age for home monitoring: 70 Mean age for usual care: 72.5 |
• The percentage of patients with a therapeutic INR with HM at day 8 after discharge was significantly higher compared with usual care (p < 0.002) • Bleeding events 3 months after discharge was significantly lower compared with usual care (p < 0.01) • There was a significant decrease in total bleeding (p = 0.009), major bleeding (p = 0.05), and minor bleeding (p = 0.01) events within 90 days of initial discharge in the HM group compared with usual care |
| Stafford et al.,45
Home setting involving patients discharged from 8 hospitals across 5 metropolitan, rural and remote regions of Australia |
Clinical outcomes of a collaborative, home-based postdischarge warfarin management service | Prospective, nonrandomized controlled cohort study | A collaborative home-based post-discharge (PDS) warfarin management service that involved point-of-care INR monitoring, warfarin education and a home medicines review (HMR) in the first 8 to 10 days post-discharge compared with usual care (UC) |
n = 129 Usual care mean age: 66.2 Intervention mean age: 67.7 |
• The PDS (n = 129) was associated with statistically significantly decreased rates of combined major and minor hemorrhagic events to day 90 (5.3% versus 14.7%; p = 0.03) and day 8 (0.9% versus 7.2%; p = 0.01) compared with UC (n = 139) • The rate of combined hemorrhagic and thrombotic events to day 90 also decreased significantly (6.4% versus 19.0%; p = 0.008) and persistence with warfarin therapy improved significantly (95.4% versus 83.6%; p = 0.004) • No significant differences in readmission and death rates or INR control were demonstrated |
| Stafford et al.,46
Home setting, Australia |
The benefits of pharmacist-delivered warfarin education in the home. | A prospective, nonrandomized, controlled cohort trial | A home-based post-discharge warfarin management service, including warfarin education, a HMR and point-of-care INR monitoring by trained pharmacists, during two or three home visits, compared with usual care (community-based post-discharge care). |
n = 268 Intervention group, mean age: 67.7 Usual care group, mean age: 66.2 |
• There was a significant increase in mean warfarin knowledge scores (measured by OAK test) at day 8 compared with the intervention patients’ baseline of 64.5% (95% CI = 61.0-68.5%) and 78.0%, (95% CI = 74.5-81.5%; p < 0.001), respectively • The intervention patients also scored significantly higher than the usual care patients at day 8 (65.0%, 95% CI = 61.5-68.0%; p < 0.001), but not at day 90 |
| Khan et al.,47
University based anticoagulation clinic, United Kingdom |
The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation | Single-center, RCT | An anticoagulation programme consisting of education with weekly home self-monitoring of the INR versus education and anticoagulation clinic care versus control group (usual anticoagulation clinic) |
n = 125 Mean age: 73 |
• There was a significant increase in percentage time within the therapeutic range for the 6 months following education (p = 0.054) and following education and self-monitoring (p = <0.001) compared with control • QOL measurements and health beliefs about warfarin were mostly unchanged with education or education and self-monitoring |
| Matchar et al.,48 28 Veteran Affairs medical centers with anticoagulation clinics, USA |
Effect of home testing of international normalized ratio on clinical events | Prospective, randomized, nonblinded trial | Point-of-care INR devices with weekly self-testing at home compared with high-quality testing in a clinic |
n = 2922 Mean age: Self-testing group, 66.6 (9.7) Clinic-testing group, 67.4 (9.4) |
• The difference in time to the first primary event (stroke, major bleeding episode, or death) between the self-testing group and clinic-testing group was not significant (p = 0.14) • The self-testing group had a small but significant improvement in TTR (p < 0.001), QOL (p < 0.001), and patient satisfaction with anticoagulation therapy (p = 0.002) |
| Waterman et al,49
8 outpatient health centers, USA |
Patient and physician satisfaction with a telephone-based anticoagulation service | Observational descriptive study (survey) | A multidisciplinary (physician, nurse, pharmacist, research associate, administrative assistant), telephone-based anticoagulation service (ACS) compared with physician management |
n = 215 Mean age: 73 years |
Patients at ACS-available health centers were significantly: • more satisfied with the timeliness of getting blood test results (p = 0.02); • more likely to know what a safe INR value was (p = 0.001); • felt safer taking warfarin (p = 0.04). |
| Witt et al.,50
Large nonprofit, group-model health maintenance organization, USA |
Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy | Retrospective, observational cohort study, 6 months in duration | Clinical Pharmacy Anticoagulation Service (CPAS) consisting of pharmacy technicians, clinical pharmacists and clinical pharmacy specialists |
n = 6,645 Intervention (CPAS) group, mean age:67.5 Control group, mean age: 68.1 |
• Patients in the CPAS group significantly spent more time within their target INR range compared with the control group (p < 0.001) • Patients in the CPAS group were 39% less likely to experience any anticoagulation therapy-related complication (hazard ratio = 0.61; 95% CI = 0.42-0.88) • Differences in the occurrence rates of major bleeding and fatal adverse events between the study groups were not statistically significant after adjustment for age, gender, and indication for anticoagulation therapy • The CPAS had the greatest impact on reducing thromboembolic complications (hazard ratio, 0.82; 95% CI = 0.56–1.20) |
| Wittkowsky et al.,51
Two university-affiliated anticoagulation Clinics, USA |
Outcomes of oral anticoagulant therapy managed by telephone versus in-office visits in an anticoagulation clinic setting | A retrospective, observational cohort study | Telephone-based management of INR compared with office managed patients within an anticoagulation clinic |
n = 234 Intervention, Mean age: 65.28 Control (office-based), Mean age: 66.26 |
• Telephone follow up can be successfully used to manage warfarin therapy in patients who are unable to present in person to an anticoagulation clinic • Monitoring outcomes (i.e. time in therapeutic range and clinic visits per patient-year) were similar between groups |
| Levine et al.,52
three family medicine clinics in a primary care network, Canada |
Monitoring of international normalized ratios: Comparison of community nurses with family physicians | A retrospective cohort analysis | A nurse-run, community-based anticoagulation program compared to a family physician monitoring the patient’s INR |
n = 556 Mean age: 74 |
• The percentage of INR values being out of range and the time between sequential INR readings did not differ significantly (p = 0.115) before and after implementation of nurse monitoring • Nurse-led monitoring of INR is as effective as traditional physician monitoring |
| Taylor et al.,53
An anticoagulant clinic, United Kingdom (UK) |
Evaluation of a nurse specialist anticoagulant service | Prospective cohort study | A nurse specialist service (NSAS) compared with a consultant anticoagulant service (CAS) |
Group A CAS n = 110 >65, n = 65, 59% Group A NSAS n = 124 >65, n = 72, 58% Group B CAS, n = 122 >65, n = 79 75% NSAS, n = 129 >65, n = 66, 51% |
• The NSAS was as good as the CAS in maintaining therapeutic control and better at documenting relevant clinical details, in reducing the number of drugs taken and in improving some aspects of patient knowledge for patients on long-term anticoagulation |
| Hassan et al.,54
An anticoagulation clinic at Staten Island University Hospital, USA |
Telephone-based anticoagulation management in the homebound setting: A retrospective observational study | Retrospective, observational study | Telephone-based dose-adjustments of warfarin in homebound patients |
n = 406 Age: 65–75 (n = 111,24.33%) Age:75–85 (n = 190, 51.34%) Age: >85 (n = 57, 14.51%) |
• Telephone management of warfarin therapy in the homebound setting is feasible |
| Grunau et al.,55
A Canadian primary care practice, Canada |
Patient self-management of warfarin therapy: Pragmatic feasibility study in Canadian primary care | A pragmatic open-label randomized crossover trial | Patient self-management (PSM) of warfarin that included outpatient laboratory monitoring and training compared with physician management |
n = 11 Mean age: 73 |
• No significant difference in proportion of INR values within therapeutic range (p = 0.82), between PSM and physician-management groups. • The improvement in patient satisfaction was not significant • Ten of the 11 patients preferred PSM to physician management and elected to continue with strategy after study completion (p=0.001)) |
| Jenner et al.,56
The Clinical Pharmacy Anticoagulation and Anemia Service (CPAAS) at Kaiser Permanente Colorado (KPCO), USA |
An Education program for patient self-management of warfarin | Prospective, open-label pilot study | A PSM education program with a dosing algorithm that released venipuncture INR results to patients via a secure, online Website |
n = 44 Mean age: 71 |
• The mean competency score improved significantly (p < 0.001) • The proportion achieving a passing score increased significantly (p < 0.001) • The warfarin PSM education program for patients with AF was feasible • High levels of self-reported comfort with warfarin PSM was reported |
| Simmons et al.,57
Kaiser Permanente Colorado, USA |
Pilot study of a novel patient self-management program for warfarin therapy using venipuncture-acquired international normalized ratio monitoring | Prospective, open-label, 3-month, pilot study. | A PSM program consisting of patients receiving dosing decision support tools during a 2-hour live PSM training class to adjust their warfarin dosage |
n = 44 Mean age: 71 (n = 39, that successfully completed the 90-day study) |
• No significant difference in TTR occurred between the 90 days before PSM program participation and the 90 days of PSM (p = 0.65) • The mean number of INR tests performed for each patient significantly increased after PSM program (p < 0.01) |
AF, atrial fibrillation; CI, confidence interval; INR, international normalized ratio; QOL, quality of life; TTR, time in target INR range.
Table 2.
Patient education interventions to support older persons.
| Authors, reference, setting, country | Title | Trial design | Patient Intervention | Number of patients Mean age (years) |
Key finding(s) |
|---|---|---|---|---|---|
| Fatima et al.,58
Cardiology and thrombosis clinics, inpatient hospital wards, Canada |
Development and validation of a decision aid for choosing among antithrombotic agents for atrial fibrillation | Prospective cohort study | A patient decision aid booklet. Stroke prevention options: 1) no treatment, aspirin and anticoagulants, 2) warfarin vs DOACs, and 3) DOAC vs DOAC |
n = 81 Mean age: 75.2 |
• Mean decisional conflict score was low • Mean knowledge score improved (p < 0.001) • Mean helpfulness score in making a treatment choice was high 6.2, standard deviation 0.9 on a scale from 1 to 7 • Information was rated as good or excellent in terms of clarity or comprehensiveness • The most preferred presentation format of the decision aid was verbal (74%), 51 (63%) participants found the pictograms to be helpful in addition to the pie charts |
| Holbrook et al.,59
four family practices and one geriatric day clinic, Canada |
Influence of decision aids on patient preferences for anticoagulation therapy: a randomized trial | Randomized trial (no control) | Six combinations of decision aid format (decision board versus decision booklet with audiotape versus interactive computer program) and graphic presentation of outcome probability data (pie chart or pictogram). Stroke prevention options: Aspirin versus warfarin versus no therapy |
n = 98 Mean age: 73.6 |
• Knowledge (maximum score 10) of AF and the treatment benefits and harms associated with anticoagulant therapy for AF increased (p < 0.01) regardless of the format or graphic presentation • 96% of the participants felt that the decision aid helped them make their treatment choice • Number of patients choosing warfarin decreased after treatment names were revealed |
| Hong et al.,60
An internal medicine and cardiology clinic, Canada |
Validation of a patient decision aid for choosing between dabigatran and warfarin for atrial fibrillation | Prospective cohort study | A patient decision aid (a paper booklet) Stroke prevention options: warfarin versus dabigatran |
n = 35 Mean age: 62.7 |
• The mean total decisional conflict score was low 18.9 (SD 14.2) • The difference in mean knowledge score improved significantly 4.60 (SD 1.48) to 6.42 (SD 0.80) • The DA was understandable by the majority of participants (68.6%), and helpful in making a treatment decision by all of the participants |
| Man-Son-Hing et al.,61
14 medical centers that participated in the Stroke Prevention in Atrial Fibrillation (SPAF) III trial, United States and Canada |
A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: a randomized controlled trial | RCT | Audio booklet (AB) decision aid (paper booklet, personal worksheet, and audiotape) versus usual care. Stroke prevention options: Aspirin versus warfarin. |
n = 287 Mean Age intervention:65, Mean age usual care:67 |
• More patients in the AB group made a choice about antithrombotic therapy than in the control group (p = 0.02) • Patients in the AB group were more knowledgeable and had more realistic expectations about the risk of stroke and hemorrhage • Decisional conflict and satisfaction were similar for the two groups |
| McAlister et al.62
102 community-based primary care practices, Canada |
Impact of a patient decision aid on care among patients with nonvalvular atrial fibrillation: A cluster randomized trial | Prospective, multicenter, two-arm, cluster RCT | A home self-administered antithrombotic decision aid (Paper booklet and audiotape versus control (usual care) Stroke prevention options: No warfarin versus warfarin |
n = 434 Mean age: 72 |
• There was a significant absolute improvement in the number of patients receiving appropriate care compared with the control group at 3 months (p = 0.03) • Very-high-risk patients were significantly more knowledgeable about their personal biannual stroke risk without treatment (p = 0.03) • Patients were significantly more knowledgeable in estimating the potential benefits and risks of warfarin such as their relative risk reduction with warfarin (p = 0.001) and mean estimate of the biannual bleeding risk with warfarin (p = 0.03) • Total Decisional Conflict Scale score was significantly lower in the intervention group • The beneficial effect of the decision aid did not significantly persist after 12 months between the intervention and control (p = 0.44) |
| Thomson et al.,63
40 General Practices, England |
A patient decision aid to support shared decision-making on anti-thrombotic treatment of patients with atrial fibrillation: randomised controlled trial | Two-armed open exploratory RCT | Computerized decision aid Comprised of 2 components: (1) individualized risks and benefits, (2) shared decision-making section compared with evidence-based paper guidelines applied as direct advice Stroke prevention options: warfarin versus aspirin therapy |
n = 109 Mean age (SD) for the decision aid group:73.1 (6.7) Mean age for the guidelines group: 73.7 (6.2) |
• Decision conflict was lower in the computerized decision aid group immediately after the clinic; mean difference 20.18 (95% CI = 20.34-20.01) • Participants not already on warfarin who were in the decision aid group were much less likely to start warfarin than participants not already on warfarin in the guidelines arm (OR = 0.01 95% CI = 0.001–0.16) • Knowledge about warfarin improved in the decision aid and guideline groups post-clinic, however, declined again in both groups by 3 months |
| Giuliano et al.,64
772-bed community teaching hospital, USA |
Can a short video improve apixaban knowledge in an inpatient setting? | Prospective, quasi-experimental study | 2 Apixaban videos; (i) for the treatment and prevention of DVT/PE (ii) for the prevention of stroke in AF |
n = 33, Mean age: 69.6 |
• Knowledge Scores significantly increased by 19.7% from the pre-test to the immediate post-test time point (p < 0.001) • Patients previously receiving apixaban or another anticoagulant were less likely to improve scores compared with new patients (p < 0.05) • For n = 22, there was no significant difference of knowledge from pre-test to 1 month post-test/follow-up (p = 0.11) |
| Moore et al.,65
University of North Carolina Medical Center, USA |
Impact of video technology on efficiency of pharmacist-provided anticoagulation counseling and patient comprehension |
Prospective, open, parallel-group study | Prerecorded informational videos provided on a tablet device coupled with ‘Teach-back’ questions compared with a control group which received face-to-face counseling |
n = 40 Mean age: 66 |
• The mean counseling time for a pharmacist was significantly reduced in the video group (p < 0.001) • Following adjustment, mean total time was reduced 8.71 (95% CI = 5.15–12.26) minutes (adjusted p < 0.001) in Restart participants (have taken warfarin therapy previously) and 2.31 (−2.19–6.81) minutes (adjusted p = 0.472) in New Start (warfarin-naïve) participants receiving video counseling • Patient comprehension (measured by the Oral Anticoagulation Knowledge (OAK) test) post counselling did not differ between informational videos and traditional face-to-face (oral) counselling |
| Mazor et al.,66
anticoagulation clinic located in an academic health center, USA |
Patient education about anticoagulant medication: is narrative evidence or statistical evidence more effective? | Randomized clinical trial | Three versions of videos incorporating narrative evidence, statistical evidence or both into patient education about warfarin | n = 317 for those who completed baseline and post-intervention questionnaires, more than 50% of participants were over 65 years of age for each intervention arm | • Compared with patients in the control group, patients who watched any video showed significant gains on the knowledge test (p < 0.001), greater positive shifts in their beliefs in the importance of laboratory testing (p = 0.010), and in their beliefs that taking warfarin is beneficial (p = 0.012) • Narrative evidence had a greater impact than statistical evidence on beliefs about the importance of lab testing (p = 0.05) and on knowledge (p = 0.006) when baseline knowledge was included as a covariate |
| Fairbairn-Smith et al.,67
Anticoagulant monitoring clinic UK |
Effect of provision of the NHS NPSA oral anticoagulant therapy patient information pack upon patients’ knowledge and anticoagulation control | Prospective cohort study | The NHS National Patient Safety Agency (NPSA) patient information booklet |
n = 24, Mean age: 68 |
• Knowledge improved significantly for the ability to name side effects of warfarin (p < 0.01), ability to describe what would happen to their INR subsequent to omitting a dose of warfarin (p < 0.01) • Anticoagulation control indicated by TTR, significantly improved (p < 0.05) |
| Lane et al.,68
AF outpatient clinic at the City Hospital, UK. |
Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy: Effects of an educational intervention programme The West Birmingham Atrial Fibrillation Project | Prospective cohort study | An information booklet. |
n = 33 patients out of 93 that completed the follow-up assessment 8 weeks later, Mean age: 68.0 |
• Patient’s knowledge of the target INR range and factors that may affect INR levels improved significantly (p = 0.001 and p = 0.014), respectively) for those who completed both questionnaires • Few patients were aware of the benefit of stroke prevention associated with anticoagulants at baseline (21%) or after the educational intervention (27%) • The intervention had little effect on increasing awareness of the bleeding risks associated with anticoagulants, although three in five people appeared to appreciate these risk |
| Masnoon et al.,69
A General teaching hospital, Australia |
A study of consumer retention of key information provided by clinical pharmacists during anticoagulant counselling | Prospective cohort study | Patient education about the anticoagulant warfarin through pharmacist counseling |
n = 22, Mean age: 69.0 |
• Immediately after counseling before discharge from hospital, participants were significantly able to recall the majority of key information elements than was observed 6 weeks after counseling, average (mean ± SD) of 79.9 ±14.6% (71.0 ±11.7%; p = 0.02) • From the three information elements that were considered critical (adverse effects, INR monitoring and drug interactions), recall of adverse effects was found to be the greatest • The two most poorly recalled information elements were mechanism of action of warfarin and diet interactions with warfarin therapy, both immediately after and 6 weeks after counseling • Indication for warfarin use was the most recalled element at immediately after and 6 weeks after counseling |
| Metlay et al.,70
Hospital USA |
Patient reported receipt of medication instructions for warfarin is associated with reduced risk of serious bleeding events | Prospective cohort study | Patient report of receipt of medication instructions |
n = 2347 Majority of patients >75 years of age (65%) |
• The rate of warfarin-related hospitalization for bleeding was substantially lower for patients who reported receiving medication instructions from a physician or nurse and a pharmacist |
| Beyth et al.,71
University teaching hospital, USA |
A multicomponent intervention to prevent major bleeding complications in older patients | RCT | Multicomponent comprehensive program of management of warfarin therapy- patient education about warfarin, training to increase patient participation in their care, self-monitoring of prothrombin time using a portable home monitor, guideline-based management of warfarin dosing Duration: 6 months |
n = 325 Mean age: 75 |
• Major bleeding at 6 months. Overt bleeding that led to the loss of at least 2.0 units of blood in 7 days or less or was otherwise life-threatening • Major bleeding was significantly more common at 6 months in the usual care group than in the intervention group (p = 0.0498, log-rank test) • Death and recurrent venous thromboembolism occurred with similar frequency in both groups at 6 months in the intervention group versus usual care groups (p = 0.2) • Throughout 6 months, the proportion of total treatment time during which the INR was within the therapeutic range was significantly higher in the intervention group than in the usual care group (56% versus 32%; p < 0.001) • The proportion of total treatment time during which the INR was within the therapeutic range was significantly higher in the intervention group than in the usual care group (p < 0.001) |
| Mitchiner et al.72
Community teaching hospital, USA |
Evaluation of the B-SAFE campaign to reduce clinically significant warfarin-drug interactions among fee-for-service Medicare beneficiaries | Prospective before and after study | B-SAFE Campaign to educate patients who take warfarin about the risk of serious drug–drug interactions and other adverse drug events that can occur while on these medications |
n = 65 Before intervention: Study hospital, Age > 70, n = 48 Control hospital, Age > 70, n = 11 After the intervention: Study hospital, Age >70, n = 61, Control hospital, Age > 70, n = 33 |
• The authors observed a marginally significant decline in the rate of warfarin-related drug interactions (OR = 0.66; 95% CI = 0.33–1.29) among Fee-for-Service Medicare patients admitted for bleeding complications to the hospital targeted by the B-SAFE campaign • Patient exposure to the B-SAFE campaign may have resulted in a decrease in the rate of clinically significant warfarin-related drug interactions |
| Clarkesmith et al.,73 Hospital outpatients clinic, UK |
Educational intervention improves anticoagulation control in atrial fibrillation patients: The TREAT randomised trial | RCT | A one-off group (1–6 patients) theory-driven educational intervention Content: DVD that included patient narratives, educational booklet, self-monitoring diary and worksheet and group discussion compared with usual care |
n = 97 Mean age: 72.9 |
• Patients had significantly higher TTR than usual care at 6 months (76.2% versus. 71.3%; p = 0.035); suggesting improved adherence, however, not at 12 months (76.0% versus. 70.0%; p = 0.44) • At 6 months, knowledge scores significantly predicted TTR (r = 0.245; p = 0.04) • There was improved patient’s understanding of the necessity of warfarin and perception of treatment harm. The intervention group significantly viewed medication as less harmful than the usual care group (p < 0.05) • Patients’ perception of the general harm and overuse of medication, as well as the perceived necessity of their AF specific medications predicted TTR at 6 and 12 months • QOL increased in the intervention group at the 1 month follow up. At all subsequent follow ups there were no significant differences in QOL scores between groups |
| Davy et al.,38 no setting mentioned, France | Higher persistence but lower compliance with direct oral anticoagulants treatment for atrial fibrillation following a personalized therapeutic information: paradoxical results of the MONACO study | Randomized, parallel, single blind, placebo control, usual care noninterventional study | Personalized therapeutic information for patients (group A active) recently prescribed rivaroxaban on days 15, 30, and 45 including 3 phone calls, paper booklets offer and Website suggestions |
n = 196 Mean age: 70 |
• At 1 year, persistence was higher in A group, 98% (90/92) versus 76% (76/92) (p < 0.001) • However, compliance (primary outcome, measured per-protocol by design) was paradoxically slightly lower, at 7.4 ± 0.8 versus 7.6 ± 1.1 (p = 0.02) • Knowledge results were mostly similar in the two groups |
AF, atrial fibrillation; B-SAFE, Bring a list of all your medications with you, Standard dose, time and monitoring, Adverse effects, Fall and injury precautions, Evaluate and examine; CI, confidence interval; DOAC, direct-acting oral anticoagulant; INR, international normalized ratio; OR, odds ratio; QOL, quality of life; RCT, randomized controlled trial; r, correlation coefficient; TTR, time in therapeutic range (proportion of time spent within therapeutic INR range).
Table 3.
Intervention to support those patients with limited literacy and from a CALD background.
| Authors, reference, setting, country | Title | Trial design | Patient intervention | Number of patients Mean age (years) |
Key finding(s) |
|---|---|---|---|---|---|
| Collins et al.,28
Public hospital, Ireland |
Pharmacist’s counseling improves patient knowledge regarding warfarin, irrespective of health literacy level | Prospective cohort study | Pharmacist counseling and a warfarin booklet |
n = 43 Mean age: 65.72 Health literacy (REALM): Adequate, n = 26, 60.5% Limited, n = 17, 39.5% |
• Warfarin knowledge at baseline improved significantly within 24 h of verbal counseling (p < 0.05) • Warfarin knowledge within 24 h of counseling decreased significantly after 28 to 56 days of counseling (p < 0.05) • Score improvement following verbal counselling was similar in those with adequate health literacy; and those with limited health literacy |
| Castelli et al.,31
Academic medical center, USA |
Effect of a rivaroxaban patient assistance kit (R-PAK) for patients discharged with rivaroxaban: a randomized controlled trial | Prospective, randomised, controlled trial | R-PAK with counseling at discharge The R-PAK contained an individualized medication box with dividers to indicate twice-daily or once-daily dosing, a patient’s guide to rivaroxaban, and a date of transition reminder card |
n = 25 Control, Mean age: 61 Intervention, Mean age:54 Health literacy score based on a single item screening tool for: - R-PAK: 12% not at risk - Control:13% not at risk |
• No difference in baseline assessment of health literacy status • Proper transition to daily administration on day 22 was no different between the groups (p < 0.891) • Adherence was reported in 99.8% of R-PAK patients and 97.65% of control patients (p < 0.074) |
| Schillinger et al.,29
Cardiologist-supervised, pharmacist-staffed anticoagulation clinic at San Francisco General Hospital (SFGH), USA |
Language, literacy and communication regarding medication in an anticoagulation clinic: a comparison of verbal versus visual assessment | Prospective cohort study | A visual aid consisting of a digitized color menu of warfarin pills Bilingual research assistants asked patients to (1) verbalize their prescribed weekly warfarin regimen and (2) identify this regimen from a digitized color menu of warfarin pills and Coumadin pills |
n = 220 Median age = 59 Age/ethnicity: Asian, n = 87 (39%) Black, n = 31 (14%) Latino, n = 61 (28%) White, n = 41 (19%) Health literacy (s-TOFHLA) of English and Spanish speaking patients: n = 178 Inadequate, n = 86, 39%, Marginal, n = 23, 11%, Adequate, n = 69, 31% |
• There was a significant difference in concordance between verbal and visual modes with clinicians regarding the weekly warfarin regimen • 50% of patients achieved verbal concordance and 66% achieved visual concordance with clinicians regarding the weekly warfarin regimen (p < 0.001) • Verbal concordance was lower for Cantonese than English speakers (38% versus 56%, OR = 0.48, 95% CI = 0.23–0.97, p = 0.04) • Verbal concordance was lower for patients with inadequate versus adequate health literacy (42% versus 64%, OR = 0.41, 95% CI = 0.21–0.78, p < 0.01) • When patients reported their regimen from verbal to visual modes, there was greater patient–provider concordance across all patient subgroups, especially for those patients with communication barriers such as Cantonese speakers compared with English speakers (45% versus 16% raw improvement, OR = 4.38, 95% CI = 2.02–9.48, p < 0.001) • Neither language nor health literacy were associated with visual discordance |
| Machtinger et al.,30
Cardiologist-supervised, pharmacist-staffed anticoagulation clinic at a general hospital and an affiliated public hospital USA |
A visual medication schedule to improve anticoagulation control: a randomized, controlled trial | Randomized controlled trial | A computer-generated visual medication schedule (VMS) of the updated warfarin dose from the clinic pharmacist |
n = 147, Mean age:61 Ethnicity: Asian, n = 59 (40%), White, n = 46 (31%), Hispanic, n = 25 (17%), Black, n = 17 (12%) Health literacy (s- TOFHLA): Inadequate, n = 58, 63% Marginal, n = 11, 12% Adequate, n = 31, 33% |
• Anticoagulation control was achieved more rapidly with intervention subjects than control subjects • The benefit of the intervention was significant among subjects with baseline regimen discordance but not among subjects with baseline concordance (median, 28 versus 49 days; HR = 1.92; 95% CI = 1.08–3.39) but not among subjects with baseline concordance (median, 28 versus 35 days; HR = 1.14; 95% CI = 0.71–1.83) |
| Lee et al.,75
Single university-affiliated medical center USA |
Feasibility study of a mobile health intervention for older adults on oral anticoagulation therapy |
Prospective, quasi-experimental study with a single-arm pre–post design | Mobile health (mHealth) applications containing modules for warfarin therapy |
n = 18 Mean age: 67 Ethnicity: Caucasian, n = 9 (50%), Hispanic, n = 7 (39%), Other, n = 2, (11%). Patients were English or Spanish speaking |
• Anticoagulation knowledge significantly improved from baseline to follow-up (p = 0.007) • Participants reported they were generally satisfied with the mHealth intervention, its ease of use and its usefulness |
CI, confidence interval; HR hazard ratio; OR odds ratio; REALM, The Rapid Estimate of Adult Literacy in Medicine tool; s-TOFHLA, abbreviated version of the short-form test of functional health literacy in adults - English and Spanish versions; TTR, time spent in target INR range.
Results
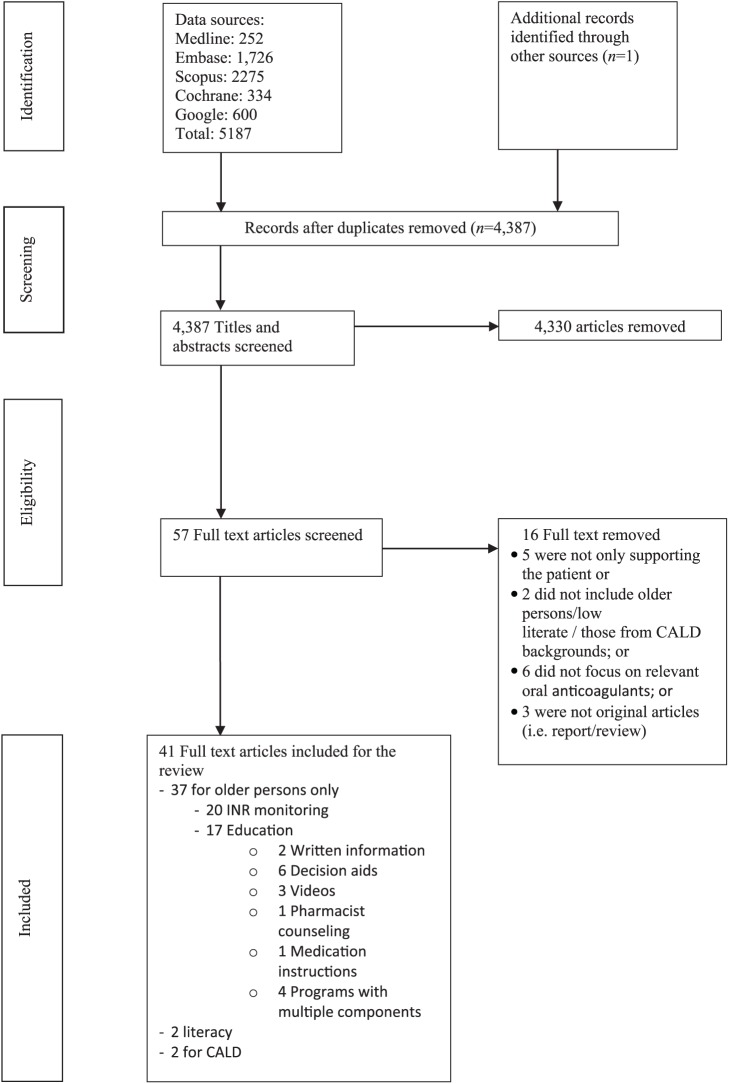
A total of 41 articles were included in the review (Figure 1). Most patient-focused interventions targeted older persons (n = 37). For older persons, the most common intervention trialed involved monitoring of the international normalized ratio (INR) (n = 20). Other interventions involved patient education and included written information (n = 2), decision aids (DAs) (n = 6), videos (n = 3), pharmacist counseling (n = 1), medication instructions (n = 1), and programs with multiple components (n = 4). Only two interventions for patients with limited health literacy and patients from CALD backgrounds were identified.
Figure 1.
Flow chart of the search strategy and results.
Studies about DAs included warfarin and the DOACs together, and one study incorporated a video and included the DOAC apixaban. These studies had limitations such as exclusion of non-English-speaking patients, difficulty recruiting warfarin-naïve participants, small sample size, and not being randomized controlled trials (RCTs).
Interventions for older persons
The main interventions to support older persons included INR monitoring (Table 1) and patient education through written and unwritten information (Table 2).
INR monitoring of patients taking warfarin
The INR monitoring of the use of warfarin may occur through self-monitoring or patient self-management (PSM) and is important for minimizing the risk of hemorrhagic or thromboembolic complications. Self-monitoring is defined as the training of a patient to use point-of-care (POC) testing via a portable device to perform the INR test and inform their healthcare provider of the result. The physician or another healthcare provider uses the results obtained by the participant to adjust the anticoagulant dose as required. PSM is defined as the patient obtaining INR values directly according to a predetermined dose–INR schedule and adjusting the warfarin dose independently.18,55
This review found that various INR monitoring models were beneficial in supporting older persons. These included POC testing (n = 10)39,40–48 led by pharmacists in the community39-41 and in rural43 and home44–46 settings, along with home self-monitoring (n = 2)47,48; telemonitoring using venipuncture testing (n = 6)49,50–54 led by a multidisciplinary team,44 pharmacists,50,51 and nurses52–54; and PSM using venipuncture testing (n = 3) through the use of nomograms,55 a dosing algorithm,56 or an online messaging system.57
However, some of these models of INR monitoring were beneficial only for certain patients. POC testing was suitable for patients who had limited access to an anticoagulant clinic,48,51 for those with erratic INR control, and for frail people with a caregiver who could assist by performing the test at home.47,48,51 PSM using venipuncture-acquired INR monitoring was shown to be feasible and suitable for those patients with stable INR control,57 who had a preference for PSM over physician management,55 and who were comfortable changing the warfarin dose on their own.56
Only two studies were RCTs that found benefits of education, home self-monitoring,47 and the role of a pharmacist follow-up service after discharge that included home monitoring44 in supporting older persons. Most of the other studies were prospective or observational.
Decision aids
The most commonly reported patient-focused intervention that included both warfarin and DOACs was the use of decision aids (DAs; n = 6).58–63 DAs can support patients by making their decisions explicit, providing information about options and associated benefits/harms, and helping to clarify congruence between decisions and personal values.17 Three of the six articles identified were RCTs61–63 (Table 2).
One prospective study (n = 81) had the objective of validating a DA to assist patients in choosing between antithrombotic agents for AF.58 This validated DA was unique because it presented and compared information between all antithrombotic treatment options for atrial fibrillation, such as warfarin and DOACs, was accessible for clinical use through a website, and was developed using the standard criteria of the International Patient Decision Aid Standards.58 It also involved pretesting to refine the DA, which indicates that it was tailored to the needs of older persons.58 The DA presented descriptions related to atrial fibrillation and charts depicting important outcomes for comparisons between: (1) no treatment, aspirin, and anticoagulants; (2) warfarin versus DOACs; and (3) dabigatran, rivaroxaban, and apixaban.58
Overall, the DAs were available in a variety of formats such as paper booklets,58,60 decision board,59 computerized DA,63 and a combination of formats, such as a decision booklet with audiotape,59,63 a 29-page paper booklet with a personal worksheet, and a 20-minute audiotape that guided the patient through the booklet and worksheet.61 One DA contained a graphic presentation of outcome probability data for the benefits and harms as a pie chart or pictogram.59
Videos
Three studies trialed the use of videos as a format for educating older persons taking warfarin65,66 and the DOAC apixaban.64 One study (n = 40) showed that, compared with face-to-face counseling, informational videos coupled with teach-back questions significantly reduced pharmacist time spent on anticoagulation counseling on discharge without compromising short-term patient comprehension, primarily in patients with prior warfarin use. However, this study found a nonsignificant reduction in patients using warfarin for the first time.65 Another study reported that the use of narrative evidence in the form of patient anecdotes was more effective than statistical evidence on certain outcomes, such as beliefs about the importance of laboratory testing, and on knowledge when baseline knowledge was included as a covariate.66
Educational videos that are indication-specific may improve short-term knowledge (less than 6 months).64 However, the studies involving videos did not specifically target older persons in their inclusion criteria and did not explain whether the target population was involved in the development of the videos. This suggests that the videos may not have acknowledged the needs of older persons and that the videos may not have been tailored to their needs.
Written information
Two studies in the UK67,68 showed that patient information booklets significantly improved older person’s knowledge, such as the ability to name side effects of warfarin and to describe what would happen to their INR after omitting a dose of warfarin,67 the target INR range, and factors that may affect INR level. The limitations of one study included a lack of patients’ perceptions on the usefulness of the booklet and that only 33 (35.5%) of patients were able to complete the follow-up questionnaire.68
The studies that described the use of booklets had several limitations. The development of the booklets was not explained, which suggests that the authors did not tailor the booklets according to the needs of the participants. Although one booklet68 significantly improved patients’ knowledge of the target INR and factors that may affect INR levels, it had little effect on awareness of the bleeding risks associated with anticoagulants. In addition, patients’ perceptions of the value of the booklets were not determined.
Pharmacist counseling
Before hospital discharge, pharmacists play an important role in educating patients about their medications through counseling. One study highlighted the importance of pharmacists educating patients about the critical information for warfarin counselling and the need for regular counseling sessions.69 One limitation of this study was its small sample size (n = 22).
Medication instructions
Another intervention involved patients receiving instructions about medication use from either a physician or nurse, plus a pharmacist after the patient had filled the prescription for warfarin.70 These patients had a reduced risk of experiencing hospitalization because of warfarin-related bleeding over the next 2 years. The instructions may have included statements such as: things the patient should and should not do when taking the medication; written or spoken instructions; and instructions received from the doctor, nurse, or pharmacist.70
Overall, although most studies targeted older persons, only six studies specifically targeted this population in their inclusion criteria and rationale: two programs,71,72 one INR monitoring intervention,47 two DAs,59,60 and a medication instruction intervention.70 Older persons were targeted because they are at increased risk of unstable control of anticoagulation 47 and warfarin-related bleeding complications71 or because they are representative of the population with atrial fibrillation for whom anticoagulation is recommended to prevent strokes.59,60 Older persons are also at significantly greater risk of an adverse drug event compared with younger patients.72 One study70 did not mention the reason for targeting older persons, although it highlighted the importance of patients taking warfarin receiving medication instructions from a physician or nurse and a pharmacist because those patients who could recall receiving instructions had a lower rate of warfarin-related hospitalization for bleeding.70 These studies did not describe the development of the interventions and therefore may not have tailored the interventions to the needs of older persons.
Programs with multiple components
One RCT71 evaluated a program with multiple components, including patient education and training to self-monitor their INR levels. Another RCT73 evaluated a complex educational–behavioral intervention to support older persons taking oral anticoagulants. Another program (n = 97) was unique because it was theory driven and was based on the relevant current literature and clinical guidelines74; it also involved the patients during the development of the intervention and had a multidisciplinary process involving patients, psychologists, and cardiologists.73 The program was compared with usual care, which comprised a standard yellow booklet and included an ‘expert patient’-focused DVD based on patient narratives, along with an educational booklet, self-monitoring diary, and worksheet. Critical elements in the development process included the use of clinical guidelines, appropriate theoretical models, patient input, and appropriate evaluation tools.73,74 One limitation of this program was that 12 months after initiation of warfarin, there was no significant difference in the time in target INR range (TTR) between the intervention and control groups. This lack of difference suggested that the program needs to be repeated at regular intervals to refresh information and reinforce behavioral changes.74
Other programs included a patient education campaign that involved tool kits with large print booklets, posters, bookmarks, pamphlets, and postcards.72 Another program included personalized therapeutic information, including phone calls on days 15, 30, and 45, paper booklet offerings, and website suggestions.38
Interventions for patients with limited health literacy
Hospital pharmacist counseling with a booklet
One study (n = 34) trialed the use of hospital pharmacist counseling and a warfarin booklet28; 39.5% of patients (n = 17) in this study had limited health literacy (Table 3). The intervention significantly improved warfarin knowledge within 24 h of verbal counselling.28 However, the knowledge score decreased significantly after 28 to 56 days of counseling.28
Rivaroxaban patient assistance kit
Another study, a prospective RCT (n = 25), trialed the effect of a rivaroxaban patient assistance kit (R-PAK) with pharmacist counseling for patients discharged with rivaroxaban compared with the standard rivaroxaban group who were discharged with no kit. The aim was to determine whether the use of the kit increased proper dose transition and overall patient adherence. Proper transition to daily administration on day 22 did not differ between the groups, and adherence did not differ between the R-PAK patients and those patients taking rivaroxaban with no discharge kit.31 However, in that study, health literacy was assessed based on a single-item health literacy screening tool. Most patients stated they rarely or never required help to read instructions, pamphlets, or other written materials from their doctor or pharmacy, meaning that their rate of health literacy was high.31
The authors of these two studies specifically targeted patients with limited health literacy because they are more likely to have little knowledge about warfarin, an increased risk of bleeding complications, and may not understand patient educational brochures about anticoagulants.28,31 Furthermore, DOACs such as rivaroxaban have a short half-life, which requires a change in medication dosage and frequency on day 22 to prevent venous thromboembolism. This may increase the risk of patient error, especially for patients with limited health literacy.31 The development of the visual aid, booklet, and R-PAK was not described, which suggests that these interventions may not have been tailored to the needs of those with limited health literacy despite the intentions of the authors.
A limitation of these health literacy studies was that they assessed health literacy using different tools and that most of the patients had an adequate29,30 or high level of health literacy.31
Interventions for patients from CALD backgrounds
Two studies showed that the use of a visual aid29,30 and a mobile health application75 supported patients from a CALD background group by improving their anticoagulation control more rapidly than that observed in control subjects30 and increased their knowledge of warfarin therapy75 (Table 3).
Visual aids
Visual aids29,30 have been used to specifically target patients from CALD backgrounds and those with limited health literacy. The visual aids were used to overcome potential communication and language barriers in this target group and to thereby reduce or prevent nonadherence and ensure clinician–patient concordance with the prescribed warfarin regimen.
In a prospective cohort study (n = 220), English-speaking and Spanish-speaking patients from varied cultural backgrounds were asked to verbally indicate their weekly warfarin regimen and to identify this regimen from a digitized color menu of warfarin pills.29 Health literacy was assessed using the S-TOFHLA, the shortened form of a test of functional health literacy in adults.33
Another RCT (n = 147)30 evaluated the use of a computer-generated visual medication schedule of digitized images of the patient’s warfarin regimen printed on a 7-day calendar in combination with a brief 2-minute ‘teach-back’ session.30 The visual schedule was translated into Spanish and Cantonese. The study found that CALD patients benefitted from the translated texts. Patients were categorized as having regimen concordance if there was no patient–clinician discrepancy in the total weekly dosage of warfarin.30
Mobile health applications
One study of the use of a mobile health application for patients from CALD backgrounds and older persons found the mobile application may enhance self-management skills in terms of medication adherence and self-care with anticoagulation therapy.75 These patient groups were specifically targeted because they may struggle following a multicomponent treatment regimen that may affect their diet and activities. In addition, adherence of patients from CALD backgrounds, such as older Hispanic people, has been shown to be poor because of inadequate knowledge about warfarin therapy, especially about Latin foods containing a high amount of vitamin K.75 This intervention was tailored to the needs of older persons by having a simple layout, large navigation buttons and a component (‘Message to tell doctors’) to increase effective communication with their doctor on matters such as INR results, medication reminders, and symptom monitoring.75 It was also tailored to CALD participants by allowing them to invite family members, including grandchildren or children, to the training sessions and by providing a list of foods that Hispanic people commonly eat, along with data from the US Department of Agriculture on the amounts of vitamin K in foods.75
Interventions that included a combination of patient populations
Four studies included patient populations with several characteristics. One study that involved pharmacist counseling included older persons with limited health literacy.28 Two studies describing the use of visual aids included CALD populations with limited health literacy.29,30 One study that evaluated a mobile health application included older English-speaking and Spanish-speaking people.75
Comparison of the impact of patient-focused interventions on outcomes
A variety of outcomes were assessed after the interventions. These included knowledge, anticoagulation control, adverse effects, decisional conflict, mortality, QOL, and patient satisfaction and persistence with warfarin therapy.
Impact on knowledge
Most interventions were effective in improving knowledge. These interventions included DAs,58–63 written information,67,68 a program,73 a video,64 patient education by a pharmacist,46,69 and a mobile health application.75 Several DAs significantly improved knowledge about warfarin.58–62 One RCT (n = 98) conducted in Canada reported significant improvements in the mean knowledge score for atrial fibrillation, treatment options, and outcomes regardless of the format or graphic presentation of the DA.59 The intervention with the longest follow up was conducted in an anticoagulation clinic (n = 24) and showed that after 6 months of using a written booklet, patients’ knowledge about the side effects of warfarin and the consequences of a missed dose of warfarin on the INR increased significantly.67 In a RCT lasting 6 months (n = 97), the educational intervention comprising a DVD with patient narratives, educational booklet, self-monitoring diary, worksheet, and a group discussion, knowledge scores significantly predicted TTR.73
An intervention using a mobile health application showed a significant increase in anticoagulation knowledge from the baseline to the 3-month follow-up for participants taking warfarin.75 An intervention including a video about apixaban produced a significant improvement in knowledge about apixaban from before to immediately after the intervention; however, there was no significant change in knowledge at 1 month after the intervention or at the follow up. The study also found that the scores were less likely to improve in patients who had previously received apixaban or another anticoagulant compared with new patients.64
Some of these studies had several limitations. The time frame for the decrease in knowledge retention varied from 28 days28 to 6 weeks69 or 3 months.46 The content of knowledge provided to educate patients and the instruments used to measure knowledge varied between studies, and this may have affected the outcomes. The main topics for patient education included the indications and duration of warfarin use, dosing, administration time and actions in the event of missed doses, target INR range, side effects, interactions with other drugs and herbs, and lifestyle issues such as alcohol and diet. Knowledge improved in several areas, such as the purpose of the medication and the identification of adverse effects,64,67,69 patients’ understanding of when to seek emergency attention,64 management of missed doses,64,67 and target INR range.67 The instruments used for some studies28,46,65,69 included the Oral Anticoagulation Knowledge test,76 the Anticoagulation Knowledge Assessment tool,77 and a tool described by Taylor et al.78
Impact on anticoagulation control (INR monitoring)
Most studies that showed a significant improvement in anticoagulation control, as indicated by the TTR, involved POC testing.40,43,44,47,48 One unique finding from one RCT (n = 125),47 was the benefits of education alone in improving TTR. Other interventions that found a significant improvement in anticoagulation control included a written information booklet,67 programs,71,73 and a telemonitoring service led by pharmacists.50 Another RCT (n = 147) showed that patients using a computer-generated visual medication schedule achieved anticoagulation control more rapidly than control subjects.30 The benefit of the intervention was significant for patients with baseline regimen discordance but not for those with baseline concordance.30
Impact on adverse events such as hemorrhagic or thromboembolic complications
Two studies involved a post-discharge home-based service by a pharmacist, including POC INR monitoring, warfarin education,44,45 and a home medicines review.45 These interventions reduced the rate of adverse effects of warfarin. In one randomized controlled cohort study (n = 129), inclusion of a post-discharge service was associated with significantly lower rates of combined major and minor hemorrhagic events to 90 days post-discharge and at 8 days post-discharge compared with usual care (n = 139). In addition, the rate of combined hemorrhagic and thrombotic events to day 90 was also significantly lower, and persistence with warfarin therapy improved significantly. The second open-label RCT (n = 128) showed a significantly lower rate of bleeding events 3 months after discharge in the intervention group compared with patients in usual care. Other studies included two PSM programs,55,57 POC testing,47,48 telemonitoring,50,51 and a multicomponent program that included patient education about warfarin, training to increase patient participation in their care, self-monitoring of prothrombin time using a portable home monitor, and guideline-based management of warfarin dosing.71
Impact on decisional conflict
Most of the DAs assisted older persons with becoming more confident and comfortable with their treatment decision.58–60,62,63 However, in a recent Cochrane review,19 data from two trials were pooled, and the random-effects analysis favored usual care in terms of reducing decisional conflict.61,62
Decisional conflict has been measured using a variety of tools, which makes it difficult to compare the outcomes. In one review,79 some of the studies reported decisional conflict outcome using the p value,61–63 whereas other studies reported no p value.59,60
In contrast to other reviews,19,79 our review found one new study on a DA.58 This study reported a low decisional conflict score of 7.2 (SD 10.8) on a scale of 1 to 100, which suggested that participants felt informed, clear about their values, supported and certain when making a decision.58 Another finding of this study was that there was no significant correlation between the years of education and total Decision Conflict Scale score.58 In addition, our review included one study63 that was excluded from a meta-analysis19 because it did not have a usual care arm. This study found a significant decrease in decisional conflict in the computerized decision aid group immediately after a shared decision-making clinic compared with the evidence-based paper guidelines applied as direct advice.
Impact on mortality and quality of life
Three studies measured mortality and showed no impact on mortality compared with the control group or comparison group.45,48,71 Three studies47,48,73 measured QOL as an outcome. One program73 showed that QOL increased in the intervention group at the 1-month follow up but not at 12 months. The second study48 showed small but significant improvement in QOL at the 2-year follow up only in the patient group that undertook home monitoring with the self-testing. The third study47 showed no change in QOL apart from the emotional role limitation (i.e. limitation in usual role activities because of emotional problems), however, the authors stated that this result was probably due to chance.
Impact on other outcomes
Patient satisfaction
Older persons expressed patient satisfaction with several interventions such as INR monitoring, DAs and videos. These included INR monitoring by pharmacists in an anticoagulation clinic,39 community pharmacy,41 and rural pharmacy settings,42 and by a multidisciplinary telemonitoring service.49 The patients in these studies were satisfied with the accessibility of the service,41 convenience,41 time saved, immediacy of the blood test results and dose,41,49 and monitoring service by a pharmacist.39,42 Patients were also satisfied with the DAs58–60 and a video about apixaban.64 Older participants and those from CALD backgrounds reported they were generally satisfied with the intervention using a mobile health application because of its ease of use and usefulness.75
Beliefs about medication and persistence with warfarin therapy
In a study of older persons, the group given a theory-driven educational intervention group was significantly more likely to view medication as less harmful than the usual care group, and patients’ perceptions of general harm predicted TTR at 6 and 12 months.73 In addition, persistence with warfarin therapy improved significantly in patients using a collaborative home-based, post-discharge warfarin management service45 (n = 129).
Verbal and visual concordance, and patient–provider concordance
CALD patients and patients with limited health literacy were categorized as having verbal concordance if there was no patient–clinician discrepancy in the total weekly dosage of warfarin when the patient verbalized the regimen. Patients were categorized as having visual concordance if there was no patient–clinician discrepancy in the total weekly warfarin dosage when the patient identified the regimen from the digitized pill menu or a visual aid.29 In this study that was conducted in an anticoagulation clinic at a San Francisco hospital, shifting from verbal to visual modes was associated with greater patient–provider concordance across all patient subgroups and especially for those with communication barriers such as Cantonese speakers. Clinician–patient discordance regarding the patients’ warfarin regimen was common, but occurred less frequently when patients used a visual aid.29 Another study conducted in the USA involved patients of various ethnicities (n = 147, Asian (40%), White (31%), Hispanic (17%), and Black (12%)) with poor anticoagulant control, most of whom had limited health literacy. Use of a visual medication schedule combined with brief counselling reduced the time to anticoagulation control.30
Overall, most interventions did not specifically seek to include vulnerable patient groups as part of their recruitment process. Most of the interventions were not tailored to address the needs of each vulnerable patient group, and most of the authors failed to acknowledge the needs of each group or to describe the development of the interventions. Nonetheless, these studies were included according to this review’s search criteria because we felt that the lessons learned from their strategies could be applied to vulnerable patient groups in future studies.
Only a few interventions specifically targeted vulnerable patient populations based on the inclusion criteria and rationale of their studies. Of these studies, only one described how the intervention was developed and considered the participants’ needs by tailoring the intervention to address them.75 The interventions that specifically targeted older persons included two programs71,72; one INR monitoring intervention47; decision aids59,60 (one of which ensured that at least half the sample would be 65 years or older60); and a mobile health application that included participants who were 55 years and older.75 Other interventions specifically targeted patients with limited health literacy; these included pharmacist counselling with a booklet28 and a R-PAK.31 Visual aids29,30 specifically targeted patients with limited health literacy and those from a CALD background. In addition, the mobile health application75 also specifically targeted both older persons and patients from CALD backgrounds.
Discussion
This review has described a range of interventions to support vulnerable patient groups taking anticoagulants such as warfarin or a DOAC and identified the outcomes of these interventions when used with anticoagulant therapy. This review has revealed several important findings.
We found that more interventions had been trialed to support older persons compared with those with limited literacy and from CALD backgrounds. Some of these interventions were comprehensive multimodal programs that were successful. By contrast, a significant finding of this review was that fewer studies have focused on supporting patients with limited health literacy and patients from CALD backgrounds; such studies were also simpler and, in most cases, unidimensional. Moreover, it was difficult to determine which intervention was the best because of differences in methodology. Some of the interventions differed in their advantages and disadvantages and were suitable for certain patients only.
Another interesting finding was that few interventions specifically targeted vulnerable patient groups in their inclusion criteria and rationale. We identified only six studies47,59,60,70–72 describing interventions that specifically targeted older persons and two studies of interventions that specifically targeted those with limited health literacy.28,31 The findings from one study28 highlight the importance of assessing health literacy because of the positive correlation between health literacy and warfarin knowledge. This relationship between health literacy and knowledge was also highlighted in one study of patients with hypertension.80 The authors concluded that it is important to ensure health education interventions are literacy sensitive because patient knowledge can link health literacy to self-efficacy, self-care, and health outcomes for patients.80
Only three studies of interventions have specifically targeted several vulnerable patient populations at the same time, such as patients from CALD backgrounds and older persons with chronic diseases who were taking warfarin75 or patients from CALD backgrounds and those with limited health literacy.29,30 These findings suggest that there is a need for more interventions that specifically target vulnerable patient populations.
This review also identified studies describing interventions that did not specifically target vulnerable patient populations groups; however, we included these according to our search criteria. The advantage of some of these reports was that they described how the interventions were developed according to patients’ needs, meaning that they were tailored to address those needs. For example, a paper that describes a unique and successful multicomponent program73 revealed how it was developed using critical elements such as patient input to tailor it to the needs of older persons. The beneficial impact of this program on outcomes such as knowledge and anticoagulation control suggest that future programs to support vulnerable patient groups should be developed based on a similar process, albeit with regular and long-term follow up and repetition at regular intervals.
Another program provided personalized therapeutic information that supported older persons and found improved drug persistence with the DOAC rivaroxaban. This result may have occurred because the program prevented less-compliant patients from stopping taking DOACs for futile reasons. The authors suggested that these patients should be the target of educational programs.38
This review also identified a DA that was unique because it included all antithrombotic choices (i.e. warfarin and the DOACs) and was tailored to the needs of older persons.58 The advantages of including all treatment choices are that the DA can assist patients who may have felt overwhelmed by having to decide on one treatment and it allows older persons to become engaged in shared decision-making with their doctor to help them select the most suitable anticoagulant in a systematic way, in alignment with their values and preferences.81 Similar to another review,17 we found that DAs improved older persons’ knowledge about oral anticoagulants, helped participants feel informed and clear about their values and supported when making a decision. The implications of our findings suggest that future DAs should be developed in a similar way with the same features. However, although studies of DAs were beneficial in improving older persons’ knowledge of the oral anticoagulants and confidence with their treatment decisions, one study reported a limitation: when the names of the treatment options were revealed, it was clear that some participants had chosen a less-effective treatment (aspirin instead of warfarin).59 The authors of this study suggested that, to optimize treatment, it is important for clinicians to allow patients time to express their preferences and rationale for treatment options at the time of prescribing.59
Similar to the unique DA, this review also found a paper that described a video that included the DOAC, apixaban, to support older persons.64 The advantages of videos in supporting older persons are the ability to increase patients’ knowledge about oral anticoagulants, to strengthen their beliefs in the importance of laboratory testing and the benefits of taking warfarin, to convey a large amount of complex information, to be watched several times at home with the family, and to be helpful to those patients who have difficulty reading written material, such as people with limited health literacy and from CALD backgrounds who cannot read English.66 Considering similar findings noted in another review,21 we suggest that videos should incorporate narrative evidence such as patient anecdotes into physician–patient dialogues or educational materials to increase the effectiveness of the message.66 One of the potential problems of using a video is that knowledge may not be retained beyond 1 month, which is problematic because many patients, such as older persons with chronic atrial fibrillation, need to take oral anticoagulants beyond 1 month. In addition, patients may not be motivated or empowered to watch the video again after discharge from the hospital.64
Several INR monitoring models were also identified to support older persons who take warfarin. The advantage of using POC INR measuring devices to support older persons in self-testing compared with venous plasma testing is that it allows for more frequent home monitoring of the INR through weekly self-testing.47 This, in turn, can lead to better anticoagulation control, better dosage advice, and improved concordance.47 POC INR monitoring promotes patient engagement in their own care and may improve clinical outcomes because out-of-range INR values can be identified and treated more quickly.48 However, there are some disadvantages in using POC INR monitoring devices, including the resources required for extensive training of nurse clinicians or specialized physicians, cost of test strips, fear of self-testing or needles, and difficulty learning the technique to perform the test.47,55
Another model that used technology to support older persons with INR monitoring was telephone anticoagulation services. Studies using this model reported benefits such as accessibility, convenience, follow up via the telephone for patients unable to present in person to an anticoagulation clinic, patient satisfaction, and improved clinical outcomes such as fewer anticoagulation complications.51 A telephone service also allows for a large number of patients to be managed by a few anticoagulation providers over a wide geographic area,50 in the home setting,54 and in the anticoagulation clinic setting.51 However, some of these studies were limited because they were not RCTs and did not measure outcomes such as medical costs.49,51
In some PSM models using venipuncture, older persons were able to review their INR laboratory results on the same day the test was performed and communicate with healthcare practitioners using a secure online messaging system, My Health Manager.56,57 These models have several advantages: the prompt receipt of INR results, unlike in other studies, in which INR results were communicated to patients in person or via mail55; no additional costs for finger-stick monitoring devices and testing strips; and no need to acquire the skill necessary to perform finger-stick INR tests.57
Another finding of our review was the beneficial role of multidisciplinary teams and allied health professionals in supporting older persons across different healthcare settings and during the transition of care between settings. Examples include pharmacist-led INR monitoring in collaboration with general practitioners,44,45 post-discharge warfarin services, and pharmacist-led education69 during the transition of care from the hospital to the home setting. The advantage of using pharmacists for INR monitoring and patient education is that they are conveniently located in a variety of healthcare settings such as the community, hospital, and home, and during transitions of care, which can optimize patient safety. Providing support to vulnerable patients during transitions of care is important because, as noted by the WHO, patients are at increased risk of medication errors during this time.1
Several authors have suggested that some INR monitoring models are suitable for certain older persons. POC testing and telephone-based management models can be considered for older persons who do not wish to travel or have difficulty traveling to an anticoagulation clinic, particularly those with erratic INR control who require frequent monitoring, frail people with a caregiver who could perform the test at home,47 and those limited by physical disability and geographic distance,48,51 such as people in rural or remote settings42 who are unable to wait for a face-to-face visit and INR blood withdrawal in an anticoagulation clinic.51 In the study of a venipuncture PSM model, patients needed to have access to online software such as My Health Manager.56 Overall, these findings highlight the important role of a caregiver and the accessibility and convenience of managing INR monitoring using certain models such as those applicable to the home setting, which could be useful for older persons with limited mobility or transportation problems.36
Other interventions that supported older persons involved written information in the form of patient information booklets.67,68 The lack of impact of one booklet on certain aspects of anticoagulants and of input from patients about their perceptions of the value of the booklets68 suggests that written information alone is insufficient to increase patients’ knowledge of anticoagulants and that, ideally, patients should have input into the development of a resource. A similar result was found in another study, in which patients and/or their caregivers viewed the supply of a booklet as inadequate and thought both verbal and written information were equally important.82 These findings are important because a lack of knowledge regarding warfarin can influence anticoagulation control and the rate of adverse outcomes.21
Another important finding of this review was that the beneficial impact of several interventions on outcomes, such as knowledge, anticoagulant control (TTR), and decisional conflict, were short term and the length of follow up was brief. These findings highlight the importance of regular and long-term follow up and the need to repeat interventions at regular intervals.
Finally, only two interventions, a mobile health application75 and a multicomponent program,74 were tailored to the needs of the vulnerable patient groups. These had a beneficial impact on outcomes such as improved knowledge, better anticoagulation control, and improved beliefs about medication. By contrast, several interventions were not tailored to the vulnerable patient groups and used a variety of INR monitoring models, DAs, videos, and booklets; however, they still had a positive impact on the same outcomes. These findings suggest that tailored and nontailored information can be used to support vulnerable patient populations to optimize patient outcomes. If tailored information is developed, healthcare professionals should be trained in individualizing interventions and responding to patients’ specific needs. Healthcare professionals should also learn how to provide a suite of resources that are culturally relevant7 or adopt a culturally competence approach83 and to consider each patient’s health and computer literacy.75,84
Limitations
There are several limitations of this review. We excluded non-English language papers, selected only full-text articles, and set an age limit of 65 years for older persons and included only studies in which the majority of participants were over 65 years of age. Setting a lower age limit may have incorporated more articles. The articles were selected by one reviewer who could have introduced some bias towards the results.
This review shows that several studies used different tools to measure warfarin knowledge28,46,65,69 and health literacy.28–30 In addition, the studies differed on a number of aspects: methodology, inclusion and exclusion criteria, sample size, setting, duration and type of study (i.e. only eight studies were RCTs),30,47,44,61–63,71,73 follow up, patient medical conditions, and inclusion of participants with a history of taking warfarin or a DOAC or those just starting medication. These differences made it difficult to compare the clinical outcomes across the trials and limited the generalizability of the results to other settings and countries. In addition, for two studies, it was difficult to determine the effectiveness of each component of the programs.71,72
Future research
Future research is needed to develop patient-focused interventions that target patients from CALD backgrounds and those with limited health literacy who are taking oral anticoagulants, and to include caregivers and family members. To optimize the treatment of these patient groups, healthcare professionals should be trained in developing interventions that are literacy sensitive and culturally appropriate. Other strategies that could be trialed for patients with limited health literacy taking oral anticoagulants may include the use of plain language and teach-back by providers,85 involvement of consumers when developing materials to ensure understanding of patient information,86 and clearly presented health educational materials and visual aids.87 For patients from CALD backgrounds taking oral anticoagulants, other strategies that could be explored include multilingual resources and staff,13 encouraging patients to ask questions,88 development of culturally appropriate information,7 providing interpreters and bilingual-link workers, and using pictorial flashcards.10
More studies are also required to determine whether interventions that specifically target vulnerable patient populations by acknowledging their needs and being tailored lead to better patient outcomes compared with interventions that are not customized. Larger RCTs are needed of interventions that include all the antithrombotics, use technology such as mobile health applications, and involve multidisciplinary and multicomponent programs with critical elements such as patient input and regular postintervention follow up to achieve a long-lasting impact on patient outcomes.
To enhance knowledge retention of information by vulnerable patients, who are often prone to recent memory loss, a repeated interactive session using text messaging and other smart phone applications such as FaceTime could be studied. Future studies should also ensure that healthcare professionals are trained in individualizing interventions and responding accordingly. In addition, future interventions should consider exploring patient outcomes such as mortality, QOL, and adherence, and their cost-effectiveness. Finally, further research is required for standardizing information about oral anticoagulants and the tools used to measure health literacy and knowledge about anticoagulant use.
Conclusion
Although most of the interventions trialed supported older persons, only a few specifically targeted them. This review identified a major gap in the literature showing that limited interventions have been trialed to support patients from CALD backgrounds and those with limited health literacy. Further research is needed to include patients with limited health literacy and those from CALD backgrounds as well as family members and caregivers of patients taking oral anticoagulants. It may be advantageous to determine whether patient outcomes differ between tailored and nontailored interventions. Future interventions should explore patient outcomes fully, such as mortality, quality of life and adherence, and the cost-effectiveness of interventions.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: AY and BB have no conflicts of interest to declare.
ORCID iD: Angela Yiu  https://orcid.org/0000-0003-2934-4440
https://orcid.org/0000-0003-2934-4440
Contributor Information
Angela Yiu, Graduate School of Health – Pharmacy, University Technology of Sydney, Level 4, Building 7, 67 Thomas Street, Ultimo, NSW 2007, Australia.
Beata Bajorek, Graduate School of Health – Pharmacy, University of Technology Sydney and Pharmacy Department, Royal North Shore Hospital, Australia.
References
- 1. World Health Organization. Medication without harm - global patient safety challenge on medication safety. Geneva: WHO, 2017. [Google Scholar]
- 2. Piazza G, Nguyen TN, Cios D, et al. Anticoagulation-associated adverse drug events. Am J Med 2011; 124: 1136–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Runciman WB, Roughead EE, Semple SJ, et al. Adverse drug events and medication errors in Australia. Int J Qual Health Care 2003; 15(Suppl.1): i49–i59. [DOI] [PubMed] [Google Scholar]
- 4. Forbes HL, Polasek TM. Potential drug–drug interactions with direct oral anticoagulants in elderly hospitalized patients. Ther Adv Drug Saf 2017; 8: 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bajorek B. A review of the safety of anticoagulants in older people using the medicines management pathway: weighing the benefits against the risks. Ther Adv Drug Saf 2011; 2: 45–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fang MC, Machtinger EL, Wang F, et al. Health literacy and anticoagulation-related outcomes among patients taking warfarin. J Gen Intern Med 2006; 21: 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilson FL, Racine E, Tekieli V, et al. Literacy, readability and cultural barriers: critical factors to consider when educating older African Americans about anticoagulation therapy. J Clin Nurs 2003; 12: 275–282. [DOI] [PubMed] [Google Scholar]
- 8. Diamantouros A, Bartle W, Geerts W. Patient information about warfarin: an assessment of accuracy and readability. JAMA Intern Med 2013; 173: 582–583. [DOI] [PubMed] [Google Scholar]
- 9. Diug B, Evans S, Lowthian J, et al. The unrecognized psychosocial factors contributing to bleeding risk in warfarin therapy. Stroke 2011; 42: 2866–2871. [DOI] [PubMed] [Google Scholar]
- 10. Alhomoud F, Dhillon S, Aslanpour Z, et al. Medicine use and medicine-related problems experienced by ethnic minority patients in the United Kingdom: a review. Int J Pharm Pract 2013; 21: 277–287. [DOI] [PubMed] [Google Scholar]
- 11. Dilworth TJ, Mott D, Young H. Pharmacists’ communication with Spanish-speaking patients: a review of the literature to establish an agenda for future research. Res Social Adm Pharm 2009; 5: 108–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. El Samman F, Chaar BB, McLachlan AJ, et al. Medicines and disease information needs of older Arabic-speaking Australians. Australas J Ageing 2013; 32: 28–33. [DOI] [PubMed] [Google Scholar]
- 13. Mohammad A, Saini B, Chaar BB. Exploring culturally and linguistically diverse consumer needs in relation to medicines use and health information within the pharmacy setting. Res Social Adm Pharm 2015; 11: 545–559. [DOI] [PubMed] [Google Scholar]
- 14. Coulter A, Roberts S, Dixon A. Delivering better services for people with long-term conditions, https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf. (2013, accessed February 2018).
- 15. Coleman K, Austin BT, Brach C, et al. Evidence on the chronic care model in the new millennium. Health aff (Project Hope) 2009; 28: 75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wofford JL, Wells MD, Singh S. Best strategies for patient education about anticoagulation with warfarin: a systematic review. BMC Health Serv Res 2008; 8: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Library 2017; 4:1–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Heneghan CJ, Garcia-Alamino JM, Spencer EA, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Library 2016; 7: 1–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Clarkesmith DE, Pattison HM, Khaing PH, et al. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev 2017; 4: 1–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clarkesmith DE, Pattison HM, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Library 2013; 6: 1–62. [DOI] [PubMed] [Google Scholar]
- 21. Nasser S, Mullan J, Bajorek B. Challenges of older patients’ knowledge about warfarin therapy. J Prim Care Community Health 2012; 3: 65–74. [DOI] [PubMed] [Google Scholar]
- 22. Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005; 10(Suppl. 1): 6–20. [DOI] [PubMed] [Google Scholar]
- 23. Eassey D, Smith L, Krass I, et al. Consumer perspectives of medication-related problems following discharge from hospital in Australia: a quantitative study. Int J Qual Health Care 2016; 28: 391–397. [DOI] [PubMed] [Google Scholar]
- 24. Parekh N, Ali K, Davies K, et al. Can supporting health literacy reduce medication-related harm in older adults? London: SAGE Publications, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Orimo H, Ito H, Suzuki T, et al. Reviewing the definition of “elderly”. Geriatr Gerontol Int 2006; 6: 149–158. [Google Scholar]
- 26. World Health Organization. Health statistics and information systems, http://www.who.int/healthinfo/survey/ageingdefnolder/en/. (2018, accessed 1 February 2017).
- 27. World Health Organization. Track 2: Health literacy and health behaviour, http://www.who.int/healthpromotion/conferences/7gchp/track2/en/. (2018, accessed 1 July 2017).
- 28. Collins S, Barber A, Sahm LJ. Pharmacist’s counselling improves patient knowledge regarding warfarin, irrespective of health literacy level. Pharmacy 2014; 2: 114–123. [Google Scholar]
- 29. Schillinger D, Machtinger EL, Wang F, et al. Language, literacy, and communication regarding medication in an anticoagulation clinic: a comparison of verbal vs. visual assessment. J Health Commun 2006; 11: 651–664. [DOI] [PubMed] [Google Scholar]
- 30. Machtinger EL, Wang F, Chen L-L, et al. A visual medication schedule to improve anticoagulation control: a randomized, controlled trial. Jt Comm J Qual Patient Saf 2007; 33: 625–635. [DOI] [PubMed] [Google Scholar]
- 31. Castelli M, Saint C, Crannage AJ, et al. Effect of a rivaroxaban patient assistance kit (R-PAK) for patients discharged with rivaroxaban: a randomized controlled trial. Pharmacotherapy Conference: 2016 Annual Meeting of the American College of Clinical Pharmacy, ACCP 2016, United states 2016; 36: e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 1993; 25: 391–395. [PubMed] [Google Scholar]
- 33. Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999; 38: 33–42. [DOI] [PubMed] [Google Scholar]
- 34. Osborne RH, Batterham RW, Elsworth GR, et al. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013; 13: 658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Smith V, Schaffer E. Chronic disease management in culturally and linguistically diverse communities: a review of the literature. 2014. [Google Scholar]
- 36. Brieger D, Amerena J, Attia JR, et al. National heart foundation of Australia and cardiac society of Australia and New Zealand: Australian clinical guidelines for the diagnosis and management of atrial fibrillation 2018. Med J Aust 2018; 209: 1209–1266. [DOI] [PubMed] [Google Scholar]
- 37. Steffel J, Verhamme P, Potpara TS, et al. The 2018 European heart rhythm association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J 2018; 39: 1330–1393. [DOI] [PubMed] [Google Scholar]
- 38. Davy JM, Tapiero A, Fournie JM, et al. Higher persistence but lower compliance with direct oral anticoagulants treatment for atrial fibrillation following a personalized therapeutic information: Paradoxical results of the MONACO study. Europace 2017; 19(Suppl. 3): iii47. [Google Scholar]
- 39. Amruso NA. Ability of clinical pharmacists in a community pharmacy setting to manage anticoagulation therapy. J Am Pharm Assoc 2004; 44: 467–471. [DOI] [PubMed] [Google Scholar]
- 40. Harrison J, Shaw JP, Harrison JE. Anticoagulation management by community pharmacists in New Zealand: an evaluation of a collaborative model in primary care. Int J Pharm Pract 2015; 23: 173–181. [DOI] [PubMed] [Google Scholar]
- 41. Shaw J, Harrison J, Harrison J. A community pharmacist-led anticoagulation management service: attitudes towards a new collaborative model of care in New Zealand. Int J Pharm Pract 2014; 22: 397–406. [DOI] [PubMed] [Google Scholar]
- 42. Jackson SL, Peterson GM, Bereznicki LR, et al. Improving the outcomes of anticoagulation in rural Australia: an evaluation of pharmacist-assisted monitoring of warfarin therapy. J Clin Pharm Ther 2005; 30: 345–353. [DOI] [PubMed] [Google Scholar]
- 43. Hodge K, Janus E, Sundararajan V, et al. Coordinated anticoagulation management in a rural setting. Aust fam physician 2008; 37: 280–283. [PubMed] [Google Scholar]
- 44. Jackson SL, Peterson G, Vial J, et al. Improving the outcomes of anticoagulation: an evaluation of home follow-up of warfarin initiation. J Intern Med 2004; 256: 137–144. [DOI] [PubMed] [Google Scholar]
- 45. Stafford L, Peterson GM, Bereznicki LRE, et al. Clinical outcomes of a collaborative, home-based postdischarge warfarin management service. Ann Pharmacother 2011; 45: 325–334. [DOI] [PubMed] [Google Scholar]
- 46. Stafford L, van Tienen EC, Bereznicki LR, et al. The benefits of pharmacist-delivered warfarin education in the home. Int J Pharm Pract 2012; 20: 384–389. [DOI] [PubMed] [Google Scholar]
- 47. Khan TI, Kamali F, Kesteven P, et al. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol 2004; 126: 557–564. [DOI] [PubMed] [Google Scholar]
- 48. Matchar DB, Jacobson A, Dolor R, et al. Effect of home testing of international normalized ratio on clinical events. N Eng J Med 2010; 363: 1608–1620. [DOI] [PubMed] [Google Scholar]
- 49. Waterman AD, Banet G, Milligan PE, et al. Patient and physician satisfaction with a telephone-based anticoagulation service. J Gen Intern Med 2001; 16: 460–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Witt DM, Sadler MA, Shanahan RL, et al. Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest 2005; 127: 1515–1522. [DOI] [PubMed] [Google Scholar]
- 51. Wittkowsky AK, Nutescu EA, Blackburn J, et al. Outcomes of oral anticoagulant therapy managed by telephone vs in-office visits in an anticoagulation clinic setting. Chest. 2006; 130: 1385–1389. [DOI] [PubMed] [Google Scholar]
- 52. Levine MA, Shao W, Klein D. Monitoring of international normalized ratios: comparison of community nurses with family physicians. Can Fam Physician 2012; 58: e465–e471. [PMC free article] [PubMed] [Google Scholar]
- 53. Taylor FC, Gaminara E, Cohen H, et al. Evaluation of a nurse specialist anticoagulant service. Clin Lab Haematol 1997; 19: 267–272. [DOI] [PubMed] [Google Scholar]
- 54. Hassan S, Naboush A, Radbel J, et al. Telephone-based anticoagulation management in the homebound setting: a retrospective observational study. Int J Gen Med 2013; 6: 869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Grunau BE, Wiens MO, Harder KK. Patient self-management of warfarin therapy: pragmatic feasibility study in Canadian primary care. Can Fam Physician 2011; 57: e292–e298. [PMC free article] [PubMed] [Google Scholar]
- 56. Jenner KM, Simmons BJ, Delate T, et al. An education program for patient self-management of warfarin. Perm J 2015; 19(4): 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Simmons BJ, Jenner KM, Delate T, et al. Pilot study of a novel patient self-management program for warfarin therapy using venipuncture-acquired international normalized ratio monitoring. Pharmacotherapy 2012; 32: 1078–1084. [DOI] [PubMed] [Google Scholar]
- 58. Fatima S, Holbrook A, Schulman S, et al. Development and validation of a decision aid for choosing among antithrombotic agents for atrial fibrillation. Thromb Res 2016; 145: 143–148. [DOI] [PubMed] [Google Scholar]
- 59. Holbrook A, Labiris R, Goldsmith CH, et al. Influence of decision aids on patient preferences for anticoagulant therapy: a randomized trial. CMAJ 2007; 176: 1583–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hong C, Kim S, Curnew G, et al. Validation of a patient decision aid for choosing between dabigatran and warfarin for atrial fibrillation. J Popul Ther Clin Pharmacol 2013; 20: e229–e237. [PubMed] [Google Scholar]
- 61. Man-Son-Hing M, Laupacis A, O’Connor AM, et al. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: a randomized controlled trial. JAMA 1999; 282: 737–743. [DOI] [PubMed] [Google Scholar]
- 62. McAlister FA, Man-Son-Hing M, Straus SE, et al. Impact of a patient decision aid on care among patients with nonvalvular atrial fibrillation: a cluster randomized trial. CMAJ 2005; 173: 496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Thomson RG, Eccles MP, Steen IN, et al. A patient decision aid to support shared decision-making on anti-thrombotic treatment of patients with atrial fibrillation: randomised controlled trial. Qual Saf Health Care 2007; 16: 216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Giuliano C, Nofar T, Edwin SB. Can a short video improve apixaban knowledge in an inpatient setting? P T 2017; 42: 256–260. [PMC free article] [PubMed] [Google Scholar]
- 65. Moore SJ, Blair EA, Steeb DR, et al. Impact of video technology on efficiency of pharmacist-provided anticoagulation counseling and patient comprehension. Ann Pharmacother 2015; 49: 631–638. [DOI] [PubMed] [Google Scholar]
- 66. Mazor KM, Baril J, Dugan E, et al. Patient education about anticoagulant medication: is narrative evidence or statistical evidence more effective? Patient Educ Couns 2007; 69: 145–157. [DOI] [PubMed] [Google Scholar]
- 67. Fairbairn-Smith L, Cope W, Robinson B, et al. Effect of provision of the NHS NPSA oral anticoagulant therapy patient information pack upon patients’ knowledge and anticoagulant control. J Thromb Haemost 2011; 9: 231–233. [DOI] [PubMed] [Google Scholar]
- 68. Lane DA, Ponsford J, Shelley A, et al. Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy: effects of an educational intervention programme: the West Birmingham atrial fibrillation project. Int J Cardiol 2006; 110: 354–358. [DOI] [PubMed] [Google Scholar]
- 69. Masnoon N, Sorich W, Alderman CP. A study of consumer retention of key information provided by clinical pharmacists during anticoagulant counselling. J Pharm Pract Res 2016; 46: 227–244. [Google Scholar]
- 70. Metlay JP, Hennessy S, Localio AR, et al. Patient reported receipt of medication instructions for warfarin is associated with reduced risk of serious bleeding events. J Gen Intern Med 2008; 23: 1589–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Beyth RJ, Quinn L, Landefeld CS. A multicomponent intervention to prevent major bleeding complications in older patients receiving warfarin. a randomized, controlled trial. Ann Intern Med 2000; 133: 687–695. [DOI] [PubMed] [Google Scholar]
- 72. Mitchiner JC, Korzeniewski SJ, Betten D, et al. Evaluation of the B-SAFE campaign to reduce clinically significant warfarin-drug interactions among fee-for-service medicare beneficiaries. Am J Med Qual 2012; 27: 518–523. [DOI] [PubMed] [Google Scholar]
- 73. Clarkesmith DE, Pattison HM, Lip GY, et al. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One [Electronic Resource] 2013; 8: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Clarkesmith DE, Pattison HM, Borg Xuereb C, et al. Developing a complex educational–behavioural intervention: the TREAT intervention for patients with atrial fibrillation. Healthcare 2016; 4: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lee J-A, Evangelista LS, Moore AA, et al. Feasibility study of a mobile health intervention for older adults on oral anticoagulation therapy. Gerontol Geriatric Med 2016; 2: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zeolla MM, Brodeur MR, Dominelli A, et al. Development and validation of an instrument to determine patient knowledge: the oral anticoagulation knowledge test. Ann Pharmacother 2006; 40: 633–638. [DOI] [PubMed] [Google Scholar]
- 77. Briggs AL, Jackson TR, Bruce S, et al. The development and performance validation of a tool to assess patient anticoagulation knowledge. Res Social Adm Pharm 2005; 1: 40–59. [DOI] [PubMed] [Google Scholar]
- 78. Taylor FC, Ramsay ME, Tan G, et al. Evaluation of patients’ knowledge about anticoagulant treatment. BMJ Qual Saf 1994; 3: 79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. O’Neill ES, Grande SW, Sherman A, et al. Availability of patient decision aids for stroke prevention in atrial fibrillation: a systematic review. Am Heart J 2017; 191: 1–11. [DOI] [PubMed] [Google Scholar]
- 80. Osborn CY, Paasche-Orlow MK, Bailey SC, et al. The mechanisms linking health literacy to behavior and health status. Am J Health Behav 2011; 35: 118–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. National Institute for Health and Care Excellence (NICE). Medicines optimisation overview, https://pathways.nice.org.uk/pathways/medicines-optimisation (2018, accessed 1 February 2018).
- 82. Bajorek BV, Ogle SJ, Duguid MJ, et al. Management of warfarin in atrial fibrillation: views of health professionals, older patients and their carers. Med J Aust 2007; 186: 175–180. [DOI] [PubMed] [Google Scholar]
- 83. Cantarero-Arévalo L, Kassem D, Traulsen JM. A culturally competent education program to increase understanding about medicines among ethnic minorities. Int J Clin Pharm 2014; 36: 922–932. [DOI] [PubMed] [Google Scholar]
- 84. Australian Commission on Safety and Quality in Health Care. Health literacy: taking action to improve safety and quality, https://www.safetyandquality.gov.au/wp-content/uploads/2014/08/Health-Literacy-Taking-action-to-improve-safety-and-quality.pdf. (2014, accessed 25 July 2018).
- 85. Koh HK, Rudd RE. The arc of health literacy. JAMA 2015; 314: 1225–1226. [DOI] [PubMed] [Google Scholar]
- 86. Aker J, Beck M, Papay JI, et al. Consumers better understand and prefer simplified written drug information: an evaluation of 2 novel formats versus the current CMI. Ther Innov Regul Sci 2013; 47: 125–132. [DOI] [PubMed] [Google Scholar]
- 87. Sudore RL, Schillinger D. Interventions to improve care for patients with limited health literacy. J Clin Outcomes Manag 2009; 16: 20–29. [PMC free article] [PubMed] [Google Scholar]
- 88. Nadar S, Begum N, Kaur B, et al. Patients’ understanding of anticoagulant therapy in a multiethnic population. J R Soc Med 2003; 96: 175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]