Short abstract
Background
The impact of middle turbinate resection (MTR) on olfaction remains a point of debate in the current literature. Few studies have objectively evaluated olfactory cleft airflow following MTR; thus, the mechanism by which MTR may impact olfaction is poorly understood. It is not known whether the postsurgical changes in airway volume, flow, and resistance increase odorant transport or disrupt the patterns of normal airflow. Computational fluid dynamics can be used to study the nasal airway and predict responses to surgical intervention.
Objective
To evaluate the functional impact of MTR on nasal airflow, resistance, and olfaction.
Methods
Five maxillofacial computed tomography scans of patients without signs of significant sinusitis or nasal polyposis were used. Control models for each patient were compared to their corresponding model after virtual total MTR. For each model, nasal airway volume, nasal resistance, and air flow rate were determined. Odorant transport of 3 different odorants in the nasal cavity was simulated based on the computed steady airflow field.
Results
Total airflow significantly increased following bilateral MTR in all patient models (P < .05). Consistent with our airflow results, we found a decrease in nasal resistance following MTR. MTR significantly increased area averaged flux to the olfactory cleft when compared to controls for phenylethyl alcohol (high-sorptive odorant). Results for carvone (medium sorptive) were similarly elevated. MTR impact on limonene, a low flux odorant, was equivocal.
Conclusion
MTR increases nasal airflow while decreasing the nasal resistance. Overall, olfactory flux increased for high sorptive (phenylethyl alcohol) and medium sorpitve (l-carvone) odorants. However, the significant variation observed in one of our models suggests that the effects of MTR on the nasal airflow and the resultant olfaction can vary between individuals based on individual anatomic differences.
Keywords: middle turbinate resection, middle turbinectomy, olfaction, nasal airflow, computational fluid dynamics
Introduction
There is no clear consensus regarding the physiologic impact of middle turbinate resection (MTR) during functional endoscopic sinus surgery (FESS). MTR is frequently performed to enhance surgical exposure.1 The risks and benefits of MTR have been debated in the literature for many years. Those who favor resection cite improved intraoperative visualization, increased ease of postoperative examination, improved long-term patency, and decreased formation of synechiae.2–4 Conversely, those who favor preservation argue that resection obscures intraoperative landmarks and increases the risk of iatrogenic frontal sinusitis, nasal crusting, and empty nose syndrome (ENS).2,5
Computational fluid dynamics (CFD) has recently been applied to study the nasal airway and predict responses to surgical intervention. Several CFD studies in the literature have looked specifically at the impact of MTR. Studies by Zhao and Dayal reported increased airway volume and decreased nasal resistance following MTR.6,7 Using a partial middle turbinectomy model, Zhao et al. found that despite changes in overall airflow and nasal resistance, there were no significant differences in streamlines, air flux distribution, and wall shear stress distribution between MTR and control models.6 In contrast, Dayal et al. analyzed the effect of total middle turbinectomy and found significant impairment in nasal air-conditioning capacity, as well as changes in regional airflow distribution.7 Di et al. found that bilateral MTR increases velocity in the region of the sphenopalatine ganglion, which may contribute to the headache seen in patients with ENS.8
The impact of MTR on olfaction is an important component of this debate that has yet to be clearly defined in the literature.7,9,10 Friedman et al. assessed olfaction in patients before and after MTR using the University of Pennsylvania smell identification test (UPSIT) and found no significant change in UPSIT score.11 Soler et al. compared patients who underwent bilateral MTR during FESS with those who did not and found that the bilateral MTR group had improved olfaction based on the Smell Identification Test when compared with controls.9 The mechanism by which MTR impacts olfaction is poorly understood. Although some believe that increased airway volume leads to increased odorant transport to the olfactory cleft, others postulate that MTR could disrupt the patterns of normal airflow and increase the risk of crusting and drying within the olfactory region.1,12
The goal of our study was to determine the functional impact of MTR on nasal airflow, resistance, and olfaction. We used CFD analysis to analyze nasal airflow and odorant delivery patterns throughout the nasal cavity after virtual total middle turbinectomy. Olfactory function was analyzed by examining the particle pathway flow pattern to the olfactory cleft region and quantifying the odorant transport before and after MTR.
Methods
Institutional review board approval was obtained from both Virginia Commonwealth University and The Ohio State University. Five maxillofacial computed tomography (CT) scans of patients without signs of significant sinusitis or nasal polyposis were used. CT scans were obtained with slices of 0.06 mm thickness.
A total of 5 control models, one from each patient, were created from the CT scans using Amira (Amira 5.0, Visage Imaging Inc.) based on the Hounsfield unit threshold. After necessary smoothing and manual artifact correction, Amira automatically generates 3-dimensional surface that encompasses the nasal airway based on the preset thresholds. For the virtual surgery models, bilateral total middle turbinectomy was simulated by converting the bony and soft tissue volume of the middle turbinate into air space using Amira. Complete removal of the middle turbinate was confirmed in axial, sagittal, and coronal planes. Virtual total middle turbinectomy was performed to about 1 to 2 mm inferior to the skull base.
ICEM CFD (Ansys, Inc., Canonsburg, PA) was applied to generate the computational mesh for individual control and virtual surgery models. A typical initial nasal cavity mesh contained between 0.6 million and 1.5 million finite elements. Then, the initial meshes were refined by gradient adaptation until grid independence of the solutions was achieved. After the grid adaptation, the final nasal cavity mesh ranged from 0.7 million to 2.2 million finite elements.
The numerical simulation of nasal airflow and odorant transport was conducted using the commercial software package FLUENT 16.2 (Ansys, Inc.). The protocol used in the current study is based on our previous publications.12–14 Specifically, a physiologically realistic pressure drop of 15 Pa between the nostrils and the nasopharynx was applied for all models. This pressure drop of 15 Pa was chosen to simulate restful breathing during routine daily life.15–17 We focused on modeling only laminar airflow in the nasal cavity because previous studies have indicated that nasal flow is mostly laminar at the resting breathing flow rate.18 The governing equations for the conservation of mass and momentum were solved by FLUENT 16.2 (Ansys, Inc.) using the finite volume method. A second-order upwind scheme was used for discretization. The SIMPLE algorithm was used for pressure–velocity coupling. The simulations were performed as steady state. The convergence criteria of each variable are 1E-4. Increasing the convergence criteria to 1E-5 had been found to have a negligible effect on the simulation results.19
Odorant transport in the nasal cavity is then simulated based on the computed steady airflow field. The uptake of odorant into the mucosal lining involving absorption, diffusion, and removal of odorant molecules can be described to a first approximation by a dimensionless mass transport at the mucosal wall. The uncoupled governing equation of odorant convection and diffusion in the air phase is solved followed by our previous work.12 Three different odorants were studied, including phenylethyl alcohol (PEA;high sorptive), l-cavone (medium sorptive), and d-limonene (low sorptive). The olfactory region was segmented based on the CT scans of each individual.
For each model, nasal airway volume was quantified. The nasal resistance and air flow rate were calculated for each model on the right side alone, left side alone, and combined to obtain bilateral ones. Olfactory flux for each molecule was simulated in both the control and virtual surgery models. Paired 2-tailed t test was used for the statistical analysis. The analyses were carried out in IBM SPSS Statistics 22.0 (IBM Corp.).
Results
Total airflow significantly increased following bilateral MTR in all patient models (P = 4.7E-04). Average airflow in the control models was 1.72E-04 m3/s (standard deviation [SD] = 7.841E-05) versus 2.30E-04 m3/s (SD = 1.01E-04) in the MTR models. Patient 3 represented the only variation in our data set-MTR on the patient’s right side actually resulted in decreased ipsilateral flow compared to the control model (7.51E-05 m3/s vs 7.81E-05 m3/s; Table 1), while the left side and bilateral combined airflow after MTR in patient 3 still resulted in airflow increasing.
Table 1.
Nasal Resistance Before and After Bilateral Middle in Pa·s/mL.
| Resistance (Control) | Resistance (Bilateral) | |
|---|---|---|
| Patient 1 | 0.0849 | 0.0578 |
| Patient 2 | 7.52E-02 | 6.46E-02 |
| Patient 3 | 0.1565 | 0.1375 |
| Patient 4 | 1.49E-01 | 8.81E-02 |
| Patient 5 | 5.25E-02 | 3.98E-02 |
Consistent with our airflow results, we found a decrease in resistance following MTR. Average resistance as measured in Pa·s/mL was 0.10362 (SD = 0.0464) in the control group, versus 0.07756 (SD = 0.078) for the bilateral MTR models. All models demonstrated a decrease in resistance, except the right side of patient 3 (Table 1), while the left side and bilateral combined nasal resistance after MTR in patient 3 still resulted in nasal resistance decreasing.
We analyzed flux to the olfactory region using PEA, carvone, and limonene. The flux value was divided by the olfactory region’s surface area to control for variations between models. We were unable to perform odorant analysis on the left side for patient 1, due to preexisting, anatomic obstruction of the olfactory cleft.
On average, for PEA, MTR significantly increased area averaged flux to the olfactory cleft when compared to controls (1.6327E-08 kg/m2s vs 1.0013E-08 kg/m2s; P = .0208). The only variation in this trend occurred with patient 3 on the left side only, where we saw a decrease in area averaged flux following middle turbinectomy (3.8411E-10 kg/m2s vs 2.8611E-9 kg/m2s).
Results for carvone were similar to PEA but did not approach significance (P = 0.051) (Table 2). On average, middle turbinectomy increased flux to the olfactory area in comparison with control (1.1502E-08 kg/m2s vs 9.0524E-09 kg/m2s). Again only 1 model differed from this trend. Flux decreased after middle turbinectomy in the left side of patient 3 (3.0125E-09 kg/m2s vs 9.3293E-09 kg/m2s in the control).
Table 2.
Olfactory Flux for High Sorptive (PEA), Medium Sorptive (Carvone), and Low Sorptive (Limonene) Odorants Before and After MT.
| PEA Control | PEA MT | Carvone Control | Carvone MT | Limonene Control | Limonene MT | |
|---|---|---|---|---|---|---|
| Patient 1 left | NA | NA | NA | NA | NA | NA |
| Patient 1 right | 1.88525E-08 | 2.41034E-08 | 1.88166E-08 | 1.99627E-08 | 9.76418E-10 | 9.67E-10 |
| Patient 2 left | 4.1656E-12 | 6.32282E-10 | 6.76702E-10 | 3.46807E-09 | 8.74115E-10 | 9.12E-10 |
| Patient 2 right | 5.41546E-08 | 7.30622E-08 | 2.8573E-08 | 3.20965E-08 | 9.89712E-10 | 9.93E-10 |
| Patient 3 left | 2.86111E-09 | 3.84108E-10 | 9.32932E-09 | 3.01252E-09 | 9.60478E-10 | 9.01E-10 |
| Patient 3 right | 4.22393E-13 | 8.55335E-11 | 1.28611E-10 | 1.22502E-09 | 7.69804E-10 | 7.71E-10 |
| Patient 4 left | 9.38517E-10 | 9.88376E-09 | 1.7826E-09 | 7.74328E-09 | 4.32777E-10 | 4.24E-10 |
| Patient 4 right | 7.57941E-10 | 2.60587E-09 | 1.09607E-09 | 2.42055E-09 | 2.93233E-10 | 3.44E-10 |
| Patient 5 left | 7.90489E-09 | 2.65548E-08 | 1.05737E-08 | 1.79652E-08 | 9.48634E-10 | 9.61E-10 |
| Patient 5 right | 4.6412E-09 | 9.63101E-09 | 1.0495E-08 | 1.56251E-08 | 9.61681E-10 | 9.74E-10 |
Abbreviations: MT, middle turbinectomy; NA, not applicable; PEA, phenylethyl alcohol.
For limonene, middle turbinectomy resulted in a slight increase in flux to the olfactory region but was statistically significant (P = 0.341) (8.0521E-10 kg/m2s vs 8.0076E-10 kg/m2s; Table 2). A decrease in flux following middle turbinectomy was noted on the right side for patient 1, the left side for patient 3, and the left side for patient 4.
Discussion
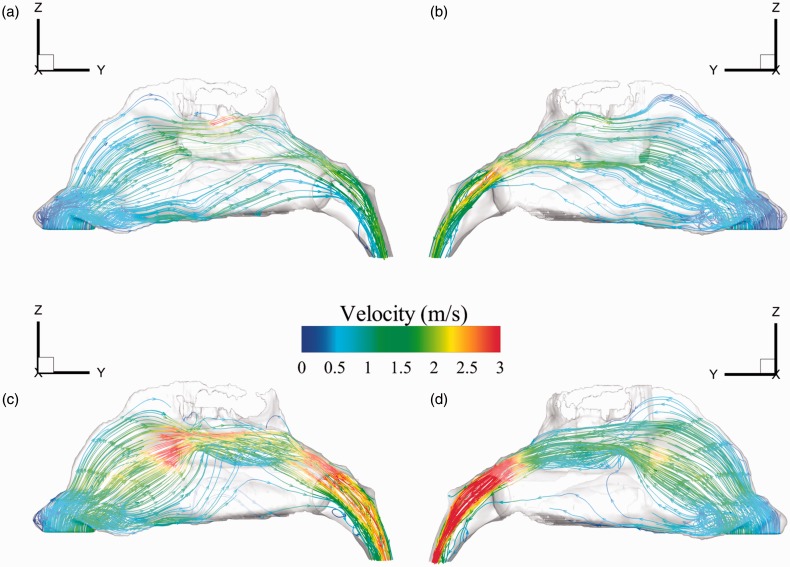
The impact of middle turbinectomy on olfaction remains a point of debate in the current literature.9–11 Previous studies have proposed different mechanisms by which MTR affects odorant transport to the olfactory cleft; however, objective evaluations of odorant transport following MTR are scarce. Overall, our data suggest that middle turbinectomy results in an increase in total nasal airflow, a decrease in total resistance, and improved odor absorption for high and medium sorptive odors. Nasal cavity volume increased significantly after MTR (2.29E-05 vs 2.69E-05, t = −12.3, P < .05). As expected, in 4 of 5 patients, MTR models with increased cavity volume demonstrated decreased total nasal resistance and increased total nasal airflow (Figure 1). In analyzing changes to olfaction, we compared area averaged flux to the olfactory cleft before and after MTR. There was an increase in olfactory flux for high sorptive (PEA) and medium sorpitve (l-carvone) odorants, while our data for limonene, a low flux odorant, were equivocal. The significant increase in area averaged flux to the olfactory cleft for PEA supports previous studies that found that highly sorptive odorants are most susceptible to local airflow.20
Figure 1.
Increased nasal airflow and decreased resistance in control models (a—right and b—left) and after middle turbinectomy (c—right and d—left). Data included from patient 4 represent similar findings to all other patients except patient 3.
These findings contradict a previous study by Zhao et al. that also utilized CFD modeling to calculate odorant uptake flux in a single patient who underwent middle turbinectomy for concha bullosa. The flux to the olfactory region remained constant before and after middle turbinectomy in this study.6 Similarly, Lee et al. examined the effects of varying degrees of resection of the middle turbinate on nasal airflow and olfaction and found a progressive decrease in flow to the olfactory region as the volume of middle turbinectomy increased.21 However, in our particle flow pathway analysis, MTR led to an increase in airflow to the space created by MTR and also increased airflow to the olfactory region in 4 of our 5 patients (Figure 1). Interestingly, Damm et al. identified the nasal segment in the upper meatus below the cribriform plate as 1 of the 2 nasal segments that contributes to individual differences in odor thresholds.22 Analysis of airflow patterns in our models before and after MTR suggests that removal of the middle turbinate may positively impact olfaction in part by improving access to this region. However, additional factor should also be taken into account, such as the distribution of olfactory epithelium on MT. It is likely that the contradicting outcome in previous literature is due to the balance between the loss of olfactory epithelium on the middle turbinate after resection and to which extent the improvement of the airflow can compensate.
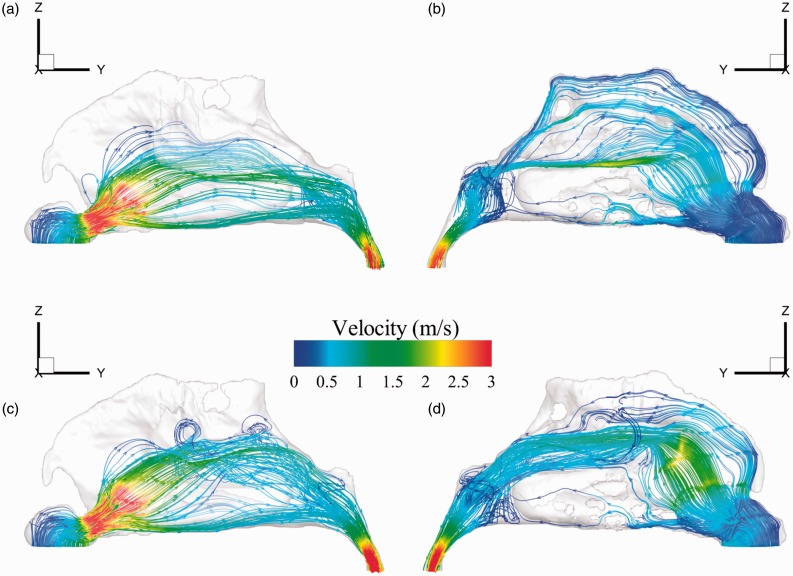
Patient 3 was a notable exception to our overall findings. Patient 3 had a decrease in nasal airflow following MTR on the right side, while the left side and the total combined bilateral airflow increased. Particle pathway flow pattern demonstrates increased turbulent flow being formed in the middle airway on the right side (Figure 2c), potentially contributing to the decrease in airflow on the right side. Interestingly, although the patient’s left side did show an increased nasal airflow, there is a preferential increase in airflow to the middle airway in the space previously occupied by the middle turbinate. The particle pathway flow pattern distribution along the olfactory region is significantly reduced (Figure 2d). This likely contributed to the decrease in the odorant flux seen on the left side for PEA and carvone. This particular patient’s variation from the other 4 patients’ findings suggest that the effects of MTR on nasal airflow and olfaction can vary between individuals based on individual anatomic differences and the MTR effects may be hard to predict. And we did not notice any significant anatomical anomaly in patient 3 while comparing to others.
Figure 2.
Flow simulations before (a—right and b—left) and after (c—right and d—left) middle turbinectomy in patient 3. On the left side, turbulent flow inferior to the olfactory cleft and a resulting decrease in airflow to the left olfactory cleft are evident following middle turbinectomy (d). Only the right side of Patient 3, out of all the study models, demonstrated decreased airflow/increased nasal resistance after MTR while the left side and bilateral combined total airflow in Patient 3 still demonstrated increased airflow/decreased nasal resistance, as similarly observed in all other patients. The right side variation in Patient 3 following MTR may be explained by the increased turbulence seen in the middle nasal cavity (c).
We recognize several limitations in this study. Importantly, clinical data on the patient’s preoperative and postoperative olfactory function were not included as part of the study. A recent study by Soler et al. analyzed patient responses to a Smell Identification Test and found that patients with MTR were more likely to show improvements in olfaction compared to patients with turbinate preservation.9 Future studies correlating objective evaluation of odorant transport with subjective reports of olfaction in patients are needed to determine if CFD analysis of odorant transport directly correlates with patient’s experience.
Conclusion
Nasal airflow and olfaction are complex processes, likely influenced by a variety of anatomic factors. Our study suggests that MTR generally appears to increase nasal airflow while decreasing the nasal resistance. This may result in increased airflow to the olfactory region. However, MTR had varying effects on olfactory uptake within our data set. The effects of MTR will likely vary between patients due to unique anatomic differences. Future CFD and clinical studies are needed to further elucidate the exact role of the middle turbinate on airflow and olfaction. CFD modeling studies using preoperative and postoperative scans on patients undergoing FESS, correlated with objective clinical olfactory data would further explain these processes. CFD modeling could be a useful adjunct to predict which patients may be negatively impacted by middle turbinectomy, both in terms of nasal airflow and olfaction.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research is partly supported by NIH (National Institute on Deafness and Other Communication Disorders [NIDCD] R01 DC013626) to K.Z.
References
- 1.LaMear WR, Davis WE, Templer JW, et al. Partial endoscopic middle turbinectomy augmenting functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1992; 107(3):382–389. [DOI] [PubMed] [Google Scholar]
- 2.Stewart MG. Middle turbinate resection. Arch Otolaryngol Head Neck Surg. 1998; 124(1):104–106. [DOI] [PubMed] [Google Scholar]
- 3.Morgenstein KM, Krieger MK. Experience in middle turbinectomy. Laryngoscope. 1980; 90:1596–1603. [PubMed] [Google Scholar]
- 4.Havas TE, Lowinger DS. Comparison of functional endonasal sinus surgery with and without partial middle turbinate resection. Ann Otol Rhinol Laryngol. 2000; 109(7):634–640. [DOI] [PubMed] [Google Scholar]
- 5.Nurse LA, Duncavage JA. Surgery of the inferior and middle turbinates. Otolaryngol Clin North Am. 2009; 42(2):295–309. [DOI] [PubMed] [Google Scholar]
- 6.Zhao K, Malhotra P, Rosen D, et al. Computational fluid dynamics as surgical planning tool: a pilot study on middle turbinate resection. Anat Rec (Hoboken). 2014; 297(11):2187–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dayal A, Rhee JS, Garcia GJ. Impact of middle versus inferior total turbinectomy on nasal aerodynamics. Otolaryngol Head Neck Surg. 2016; 155(3):518–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di MY, Jiang Z, Gao ZQ, et al. Numerical simulation of airflow fields in two typical nasal structures of empty nose syndrome: a computational fluid dynamics study. PLoS One. 2013; 8(12):e84243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soler ZM, Hwang PH, Mace J, et al. Outcomes after middle turbinate resection: revisiting a controversial topic. Laryngoscope. 2010; 120(4):832–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choby GW, Hobson CE, Lee S, et al. Clinical effects of middle turbinate resection after endoscopic sinus surgery: a systematic review. Am J Rhinol Allergy. 2014; 28(6):502–507. [DOI] [PubMed] [Google Scholar]
- 11.Friedman M, Caldarelli DD, Venkatesan TK, et al. Endoscopic sinus surgery with partial middle turbinate resection: effects on olfaction. Laryngoscope. 1996; 106(8):977–981. [DOI] [PubMed] [Google Scholar]
- 12.Zhao K, Scherer PW, Hajiloo SA, et al. Effect of anatomy on human nasal air flow and odorant transport patterns: implications for olfaction. Chem Senses. 2004; 29(5):365–379. [DOI] [PubMed] [Google Scholar]
- 13.Li C, Farag AA, Leach J, et al. Computational fluid dynamics and trigeminal sensory examinations of empty nose syndrome patients. Laryngoscope. 2017; 127(6):E176–E184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li C, Jiang J, Kim K, et al. Nasal structural and aerodynamic features that may benefit normal olfactory sensitivity. Chem Senses. 2018; 43(4):229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee TS, Goyal P, Li C, Zhao K. Computational fluid dynamics to evaluate the effectiveness of inferior turbinate reduction techniques to improve nasal airflow. JAMA Facial Plast Surg. 2018; 20(4):263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li C, Farag AA, Maza G, et al. Investigation of the abnormal nasal aerodynamics and trigeminal functions among empty nose syndrome patients. Int Forum Allergy Rhinol. 2018; 8(3):444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otto BA, Li C, Farag AA, et al. Computational fluid dynamics evaluation of posterior septectomy as a viable treatment option for large septal perforations. Int Forum Allergy Rhinol. 2017; 7(7):718–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li C, Jiang J, Dong H, Zhao K. Computational modeling and validation of human nasal airflow under various breathing conditions. J Biomech. 2017; 64:59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Z, Kleinstreuer C. Laminar‐to‐turbulent fluid–nanoparticle dynamics simulations: Model comparisons and nanoparticle‐deposition applications. Int J Numer Methods Biomed Eng. 2011; 27(12):1930–1950. [Google Scholar]
- 20.Zhao K, Dalton P, Yang GC, et al. Numerical modeling of turbulent and laminar airflow and odorant transport during sniffing in the human and rat nose. Chem Senses. 2006; 31:107–118. [DOI] [PubMed] [Google Scholar]
- 21.Lee KB, Jeon YS, Chung SK, et al. Effects of partial middle turbinectomy with varying resection volume and location on nasal functions and airflow characteristics by CFD. Comput Biol Med. 2016; 77:214–221. [DOI] [PubMed] [Google Scholar]
- 22.Damm M, Vent J, Schmidt M, et al. Intranasal volume and olfactory function. Chem Senses. 2002; 27(9):831–839. [DOI] [PubMed] [Google Scholar]