Abstract
Background:
Self-management support interventions are widely accepted in chronic kidney disease (CKD) care; however, interventions rarely consider individual behaviors by incorporating a behavioral theoretical framework. The Theoretical Domains Framework (TDF) can be used to facilitate an understanding of patients and their caregivers’ behaviors to successfully self-manage CKD.
Objectives:
(1) To understand behaviors of patients with CKD and their caregivers and identify potential intervention approaches to support CKD self-management and (2) to explore relationships between the 14 TDF domains and CKD self-management.
Design:
Qualitative descriptive study using both content and thematic analysis
Setting:
Purposive criterion was used to recruit participants from across Canada.
Patients:
Canadian patients with CKD and their caregivers.
Measurements:
Focus groups and telephone interviews using a semistructured interview guide.
Methods:
We conducted a secondary analysis of qualitative data collected from focus groups and telephone interviews from July 2017 to January 2018. Two research team members coded the transcribed data to the 14 TDF domains using a modified approach of the Framework Method. We linked the common TDF domains to relevant intervention functions from the Behaviour Change Wheel (BCW) to identify potential intervention approaches. We also identified and mapped relationships between the relevant TDF domains to report emerging themes.
Results:
Six focus groups (37 participants) and 11 telephone interview transcripts were analyzed. Five TDF domains that influenced CKD self-management behavior were identified: environmental context and resources, knowledge, beliefs about capabilities, beliefs about consequences, and social influences. Four BCW intervention functions were identified: education, modeling, persuasion, and environmental restructuring. Four emergent themes, shaped by the populated 14 TDF domains, were identified: What does this mean for me? Help me help myself, How does this make me feel? and Who am I?
Limitations:
The TDF was not used to design the interview guide; therefore, there may be underrepresentation of some TDF domains relevant for self-management.
Conclusion:
Our findings highlight 5 TDF domains that can influence CKD self-management behavior and 4 possible intervention approaches to influence behavior change in patients with CKD and their caregivers. Emergent themes highlight participants’ interpretation of being diagnosed with CKD, their motivations, feelings, values, and altered identity. This work will inform the codesign of a behavior change intervention to enhance patient self-management of CKD.
Keywords: chronic kidney disease, qualitative study, self-management, Theoretical Domains Framework
Abrégé
Contexte:
Les interventions visant à soutenir l’autogestion en santé sont largement acceptées dans le traitement de l’insuffisance rénale chronique (IRC). Cependant, ces interventions tiennent rarement compte des comportements individuels en intégrant un cadre comportemental théorique. Le Theoretical Domains Framework (TDF) pourrait être employé pour faciliter la compréhension des comportements des patients et de leurs fournisseurs de soins en vue d’une autogestion efficace de l’IRC.
Objectif:
1. Comprendre les comportements des patients atteints d’IRC, de même que ceux de leurs fournisseurs de soins, et proposer des approches interventionnelles visant à soutenir l’autogestion de l’IRC.2. Explorer la relation entre les 14 domaines du TDF et l’autogestion de l’IRC.
Type d’étude:
Une étude qualificative et descriptive utilisant à la fois l’analyse de contenu et l’analyse thématique.
Cadre:
Un critère fondé sur l’objectif a été utilisé pour recruter des participants partout au Canada.
Sujets:
Des Canadiens atteints d’IRC et leurs fournisseurs de soins.
Mesures:
Des groupes de discussion et des entretiens téléphoniques menés à l’aide d’un guide d’interview semi-structurée.
Méthodologie:
Nous avons procédé à une analyze secondaire des données qualitatives provenant des groupes de discussion et des entretiens téléphoniques entre juillet 2017 et janvier 2018. Deux chercheurs membres de l’équipe ont codé les données transcrites selon les 14 domaines du TDF à l’aide d’une approche modifiée de The Framework Method. Nous avons relié les domaines courants du TDF aux fonctions d’intervention appropriées du Behaviour Change Wheel (BCW) pour cerner de potentielles approches interventionnelles. Enfin, nous avons établi et cartographié les relations entre les domaines pertinents du TDF pour en dégager les thèmes émergents.
Résultats:
L’analyse porte sur six groupes de discussion (37 participants) et 11 entretiens téléphoniques. Il en est ressorti cinq domaines du TDF ayant influencé l’autogestion de l’IRC (les ressources et le contexte environnemental, les connaissances, les croyances relatives aux capacités, les croyances relatives aux conséquences et les influences sociales) et quatre fonctions d’intervention du BCW (l’éducation, le modelage, la persuasion et le réaménagement du milieu). De plus, quatre thèmes émergents, influencés par les 14 domaines du TDF, ont été mis en lumière: Qu’est-ce que cela signifie pour moi? Aidez-moi à m’aider moi-même., Qu’est-ce que cela me fait ressentir? Qui suis-je?
Limites:
Certains domaines du TDF pertinents pour l’autogestion pourraient être sous-représentés puisque le TDF n’a pas été utilisé pour l’élaboration du guide d’interview.
Conclusion:
Nos résultats mettent en lumière cinq domaines du TDF susceptibles d’influencer les comportements en autogestion de l’IRC et quatre approches interventionnelles qui pourraient entraîner des changements de comportement chez les patients atteints d’IRC et leurs fournisseurs de soins. Les thèmes émergents mettent l’accent sur l’interprétation qu’ont les patients du diagnostic de l’IRC, de même que sur leurs motivations, leurs sentiments, leurs valeurs et leur identité modifiée. Ces travaux éclaireront la co-conception d’une intervention facilitant les changements de comportements, en vue d’améliorer l’autogestion de l’IRC par les patients.
What was known before
Chronic kidney disease (CKD) self-management interventions can reduce modifiable risk factors and slow disease progression. However, prior research has been limited by the lack of a theory-informed approach to identify and understand behaviors in the CKD self-management context. The Theoretical Domains Framework (TDF) is one approach that may assist in developing complex behavioral interventions.
What this adds
Our study applies a theory-informed TDF approach to understand contributors that influence self-management behavior in patients with CKD and their caregivers. Using qualitative methods, we identified 5 TDF domains most common for patients and caregivers to supporting self-management behavior: environmental context and resources, knowledge, beliefs about capabilities, beliefs about consequences, and social influences. We also identified 4 intervention functions (ie, broad approaches by which an intervention can change behavior) from the Behaviour Change Wheel (BCW) for inclusion in a CKD self-management strategy: education, modeling, persuasion, and environmental restructuring. Finally, we describe relationships between the TDF domains and self-management support needs.
Introduction
Chronic kidney disease (CKD) affects about 9% of the population and is a burden on individuals, their families, and the health care system.1 Chronic kidney disease is complex and often coexists with other conditions such as cardiovascular disease and diabetes. It requires an informed, motivated individual along with family, health care, and community supports to successfully manage and slow disease progression. Self-management strategies can support “the individual, in conjunction with family, community, and health care professionals, to manage symptoms, treatments, lifestyle changes, and psychosocial, cultural, and spiritual consequences of health conditions.”2 Self-management entails monitoring as well as developing cognitive, emotional, and behavioral strategies to help individuals maintain a quality of life meaningful to them.3
Similar to other chronic conditions, patients with CKD adopt self-management behaviors to facilitate living with CKD. Although self-management support interventions are widely accepted in CKD care, interventions rarely consider individual behaviors by incorporating a behavioral theoretical framework.4 A behavior change theory that identifies and addresses potential target behaviors in the CKD population could inform the design of a CKD self-management support intervention.
The Theoretical Domains Framework (TDF) is an integrative framework that represents many organizational and individual behavior change theories.5 The TDF has 84 constructs and 14 theoretical domains, relating to individual motivation and capability factors underpinning behavior change (Table 1).5 The TDF can be used to facilitate understanding of patients and their caregivers’ behaviors in self-managing CKD. Furthermore, linking the domains of the TDF to broad categories of interventions (ie, intervention functions) from the Behaviour Change Wheel (BCW) framework can assist in codeveloping a CKD self-management intervention strategy.5 The purpose of this article is to discuss the TDF domains that may influence self-management behavior in patients with CKD and their caregivers and identify potential intervention approaches to support self-management, as well as explore relationships between TDF domains and CKD self-management. This work will inform the codesign of a behavior change intervention to enhance patient self-management of CKD.
Table 1.
Theoretical Domains Framework.5
| Domains | Definition | Theoretical constructs represented within each domain |
|---|---|---|
| Knowledge | An awareness of the existence of something. | • Knowledge (including knowledge of condition/scientific rationale) • Procedural knowledge • Knowledge of task environment |
| Skills | An ability or proficiency acquired through practice. | • Skills • Skills development • Competence • Ability • Interpersonal skills • Practice • Skill assessment |
| Social/professional role and identity | A coherent set of behaviors and displayed personal qualities of an individual in a social or work setting. | • Professional identity • Professional role • Social identity • Identity • Professional boundaries • Professional confidence • Group identity • Leadership • Organizational commitment |
| Beliefs about capabilities | Acceptance of the truth, reality, or validity about an ability, talent, or facility that a person can put to constructive use. | • Self-confidence • Perceived competence • Self-efficacy • Perceived behavioral control • Beliefs • Self-esteem • Empowerment • Professional confidence |
| Optimism | The confidence that things will happen for the best or that desired goals will be attained. | • Optimism • Pessimism • Unrealistic optimism • Identity |
| Beliefs about consequences | Acceptance of the truth, reality, or validity about outcomes of a behavior in a given situation. | • Outcome expectancies • Characteristics of outcome expectancies • Beliefs • Anticipated regret • Consequents |
| Reinforcement | Increasing the probability of a response by arranging a dependent relationship or contingency, between the response and a given stimulus. | • Reward (proximal/distal) valued/not valued (probable/improbable) • Incentives • Punishment • Consequents • Reinforcement • Contingencies • Sanctions |
| Intentions | A conscious decision to perform a behavior or a resolve to act in a certain way. | • Stability of intentions • Stages of change model • Transtheoretical model/stages of change |
| Goals | Mental representation of outcomes or end states that an individual want to achieve. | • Goals (distal/proximal) • Goal priority • Goal/target setting • Goals (autonomous/controlled) • Action planning • Implementation intention |
| Memory, attention and decision processes | The ability to retain information, focus selectively on aspects of the environment and choose between 2 or more alternatives. | • Memory • Attention • Attention control • Decision making • Cognitive overload/tiredness |
| Environmental context and resources | Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence, and adaptive behavior. | • Environmental stressors • Resources/material resources • Barriers and facilitators • Organizational culture/climate • Person and environment interaction • Salient event/critical incidents |
| Social influences | Those interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviors. | • Social pressure • Social norms • Group conformity • Social comparison • Group norms • Social support • Intergroup conflict • Power • Group identity • Slienation • Modeling |
| Emotion | A complex reaction pattern, involving experiential, behavioral, and physiological elements, by which the individual attempts to deal with a personally significant matter or event. | • Anxiety • Fear • Affect • Stress • Depression • Positive/negative affect • Burn-out |
| Behavioral regulation | Anything aimed at managing or changing objectively observed or measured actions. | • Self-monitoring • Breaking habit • Action planning |
Methods
Design
This work is part of a larger multiphase study to design, implement, and evaluate an eHealth self-management intervention for patients with CKD. We used a qualitative descriptive approach and content and thematic analysis6 to perform a secondary analysis of data previously collected to understand patient and caregiver preferences and needs for CKD self-management. Focus groups and telephone interviews were conducted with patients with CKD and their caregivers between July 2017 and January 2018. Methods used in the initial study have been reported.7 An amendment using the nonidentifiable primary data set (ie, transcripts) received ethical approval in June 2018 from the Conjoint Health Research Ethics Board at the University of Calgary (REB 17-0908). We reported our study according to the Consolidated Criteria for Reporting Qualitative studies checklist.8
Participant Selection and Recruitment
Patients were eligible to participate in the focus groups or telephone interviews if they were English speaking, ≥18 years old with an awareness of their level of kidney function (reported as CKD categories 1-5 and not on renal replacement therapy), regardless of etiology or duration of CKD. Informal caregivers such as family members or friends of people with CKD were also eligible.
Participants were purposively recruited using 2 methods including the various CKD and primary care clinics in Alberta and Ontario (ie, e-mails and newsletters) and through advertisement (ie, print and social media) by the Kidney Foundation of Canada and the Canadians Seeking Solutions and Innovations to Overcome CKD (Can-SOLVE CKD) Network.9
Participant Characteristics
Six focus group and 11 telephone interview transcripts were analyzed. A total of 48 participants (33 patients and 15 caregivers), with a greater number of females (n = 30) than males (n = 18), were included. Most participants (n = 26) were below the age of 65 years, with the majority having a secondary level of education (n = 30). Patient participants reported various estimated glomerular filtration rate (eGFR) levels; most were between 30 and 60 mL/min/1.73 m2 (n = 9), and 30% of patient participants did not know their eGFR level. Most patients (n = 23) had been diagnosed in the last 10 years. Further details regarding demographics are reported in Table 2 and have been reported elsewhere.7
Table 2.
Participant Characteristics (n = 48).
| Characteristics | Patients (n = 33) No. (%) |
Caregivers (n = 15) No. (%) |
|---|---|---|
| Gender | ||
| Male | 13 (40) | 5 (33) |
| Female | 20 (60) | 10 (67) |
| Age (years) | ||
| Below 50 | 10 (30) | 0(0) |
| 50-64 | 8 (24) | 8 (53) |
| 65-74 | 8 (24) | 4 (27) |
| ≥75 | 7 (22) | 3 (20) |
| Geographical location (population) | ||
| <500 000 (rural) | 13 (39) | 11 (73) |
| ≥500 000 (urban) | 20 (61) | 4 (26) |
| Level of education | ||
| Primary (≤grade 12) | 7 (21) | 3 (20) |
| Secondary (college, university, trade school) | 21 (64) | 9 (60) |
| Postsecondary graduate | 4 (12) | 2 (13) |
| No response | 1 (3) | 1 (7) |
| Self-reported patient clinical characteristics (n = 33) | ||
| Duration of CKD diagnosis (years) | ||
| ≤5 | 13 (40) | |
| 6-10 | 10 (30) | |
| ≥11 | 9 (27) | |
| Unknown | 1 (3) | |
| Severity of CKD (eGFR [mL/min/1.73 m2]) | ||
| 30-60 | 9 (27) | |
| 15-29 | 7 (21.5) | |
| <15 | 7 (21.5) | |
| Unknown | 10 (30) | |
Note. CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate.
Data Collection
Six focus groups and 11 telephone interviews were held across Canada. A research team member (M.D.) with experience in qualitative research conducted the focus groups and telephone interviews using a semistructured interview guide (Supplementary Material, Appendix 1).7 The interview guide was not informed by the TDF, but was guided by previous published self-management literature and input from 2 Can-SOLVE CKD patient partners from a national CKD patient-oriented research network.9 The interview guide focused on experiences managing CKD and patients and caregivers’ preferences and needs to self-manage CKD. All focus groups and telephone interviews were audio recorded and transcribed by a transcriptionist with qualitative experience who signed a pledge of confidentiality.
Analysis
Two research team members (M.D., S.B.) completed all analysis phases; M.D. is a clinician-researcher with experience in qualitative research, and S.B. is a qualitative research trainee. Comparison of participant views (ie, patients and caregivers) or evaluation of TDF perspectives between focus group and telephone interview participants was beyond the scope of this article.
Coding data to the TDF
The content analysis plan followed a modified approach of the Framework Method outlined by Gale et al.10 Using a deductive approach, the research team members familiarized themselves with the data by reviewing the anonymized transcripts. The process involved using printed versions of the transcripts with key phrases highlighted and comments written in the margins reflecting initial thoughts. After familiarization, the 2 research members independently analyzed a single telephone interview and focus group transcript by coding (ie, categorizing phrases or passages of the transcripts) to the 14 TDF domains (Table 1). The research team members convened and compared codes applied to the transcripts, at which time data were recategorized under agreed upon TDF domains. Next, the team members independently analyzed 2 more telephone interviews along with an additional focus group, followed by another meeting to reach consensus on the coding framework through discussion on aspects from the data that fit categories based on the 14 TDF domains. This version of the coding framework was systematically applied to all subsequent transcripts. At this point, all transcripts were transferred into NVivo 12 (QSR International Pty Ltd. Version 12, 2018) to facilitate further analysis. To determine the most commonly reported TDF domains from the 14 domains, the frequency of TDF domain coded phrases were calculated.
Identifying intervention functions
To identify potential interventions that might be appropriate for individuals with CKD, the common cited TDF domains were mapped by 2 research team members (M.D., S.B.) to intervention functions identified by Michie and illustrated in the BCW, a comprehensive approach to behavior analysis.5 Intervention functions are broad approaches by which an intervention can change behavior and include education, persuasion, incentivization, coercion, training, restriction, environmental restructuring, modeling, and enablement.5
Thematic analysis
Using an inductive approach, the 2 team members identified and mapped interactions between the 14 TDF domains to highlight relationships between the TDF domains and present meaningful themes reflecting main concepts emerging from the data. All discrepancies were resolved through consensus discussion involving a third team member (B.H).
Results
Common TDF Domains
The 5 most common TDF domains (defined as greater than 100 coded phrases) were environmental context and resources (304 coded phrases), knowledge (160 coded phrases), beliefs about capabilities (121 coded phrases), beliefs about consequences (112 coded phrases), and social influences (105 coded phrases). The 5 TDF domains are interconnected and the relationships between these domains have been incorporated into a conceptual framework shown in Figure 1. The domains represented in each level build on the previous ones and collectively they result in CKD self-management. The domains that were reflected least often (ie, fewer than 20 coded phrases) were goals set with a health care provider or individually, and memory, attention, and decision processes (problems making decisions due to the medication and illness). Table 3 reports the 14 TDF domain frequencies.
Figure 1.
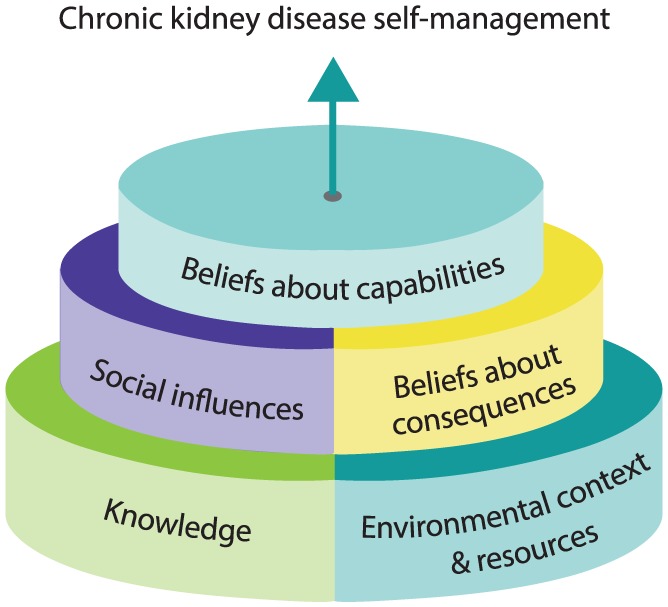
Conceptual framework of the relationship between the most common Theoretical Domains Framework domains.
Table 3.
TDF Domain Frequencies.
| TDF domain | No. of coded phrases | No. of participants mentioning domain (n = 48) |
|---|---|---|
| Environmental context and resources | 304 | 42 |
| Knowledge | 160 | 40 |
| Beliefs about capabilities | 121 | 36 |
| Beliefs about consequences | 112 | 28 |
| Social influences | 105 | 31 |
| Emotion | 82 | 36 |
| Social and professional role and identity | 61 | 30 |
| Behavioral regulation | 58 | 26 |
| Intentions | 44 | 24 |
| Reinforcement | 28 | 13 |
| Optimism | 28 | 13 |
| Skills | 27 | 17 |
| Goals | 14 | 7 |
| Memory, attention, and decision making | 8 | 8 |
Note. TDF = Theoretical Domains Framework.
Intervention Functions
Table 4 shows the 5 most common TDF domains mapped to 4 applicable intervention functions. These intervention functions include education, modeling, persuasion, and environmental restructuring. Education and modeling apply to all 5 TDF domains. Education involves increasing a person’s knowledge and understanding, while modeling provides an example for a person to aspire to or imitate. Persuasion comprises using communication to encourage a person to take action, for example, information from a credible source. Environmental restructuring involves changing the physical or social context, for example, adding objects to the environment (eg, Web-based tool), access to health care resources, and prompts to influence behavioral change.
Table 4.
TDF Domains and Relevant Intervention Functions.
| TDF domains | No. of times coded | Intervention functionsa | |||
|---|---|---|---|---|---|
| Education | Modeling | Persuasion | Environmental restructuring | ||
| Environmental context and resources | 304 |

|
|||
| Knowledge | 160 | ||||
| Beliefs about capabilities | 121 | ||||
| Beliefs about consequences | 112 | ||||
| Social influences | 105 | ||||
Note. TDF = Theoretical Domains Framework.
Intervention functions: Broad categories of potential intervention approaches.
Themes
Four emergent themes, shaped by the populated 14 TDF domains, were identified: What does this mean for me? Help me help myself, How does this make me feel? and Who am I? Sample quotes for each of the themes and related domains are presented in Table 5.
Table 5.
Themes, Relevant TDF Domains, and Descriptions With Illustrative Quotes.
| Theme | TDF domain | Description | Quotes |
|---|---|---|---|
| What does this mean for me? | Knowledge | Lack of knowledge around CKD awareness and disease-specific knowledge. | “I really don’t know what GFR means . . . and what the numbers mean. Like is a low number good? Is the higher number good? What is it. all I know is what my number is.” (FG 2 Patient 4) “I needed my questions addressed, I needed to know why and what can I do.” (INT Patient 13) |
| Intentions | Unmatched timing of information: “readiness to learn” versus “CKD category.” | “I think for me, and perhaps other people you are speaking to, there are stages of understanding.” (INT Patient 23) “There needs to be more continuing education when you have this condition because things do change, not only the information, you change as you evolve into your condition and stage of life.” (INT Patient 21) |
|
| Help me help myself. | Beliefs about capabilities | Developing self-efficacy and self-confidence. | “Everyone is proactively looking after their own condition and searching out information . . . these are great things that self-managers do.” (FG 1 Patient 9) “Some people they don’t want to speak up and they don’t want to ask questions. They say here is what the doctor said so that’s it. Well, that’s wrong, you got to ask questions.” (FG 5 Patient 1) “You have to stay disciplined, you know because you’re health comes first.” (FG 2 Patient 2) |
| Behavior regulation | Identifying individualized self-monitoring techniques. | “I set a timer for him, like on his watch so that he has his meals and snacks and everything.” (FG 2 Caregiver 1) “I make a record of my sugar and my blood pressure and keeping a record of that.” (FG 2 Patient 5) |
|
| Skills | Acquiring skills with repeated practice. | “We are experts at looking after ourselves, but we aren’t experts at looking after anybody else” (FG 1 Patient 2) “I research the whole thing (medications) because I don’t want to make my body worse.” (FG 3 Patient 8) |
|
| How does this make me feel? | Social influences | Optimizing social supports. | “It was just so difficult for me because I live alone.” (FG 3 Patient 7) “You can share your challenges and you can hear other people going through similar things and you don’t feel as isolated.” (FG 3 Patient 6) “Suddenly I couldn’t do sports and I wasn’t working. So, it’s like suddenly my whole social world was pretty much gone.” (INT Patient 23) |
| Optimism | Recognizing positive and negative feelings. | “Life goes on, absolutely, and this disease makes you stronger. You don’t dwell on it.” (FG 3 Patient 8) “No matter what you do it’s going to get worse either way.” (INT Patient 4) |
|
| Beliefs about consequences | Expectations about outcomes based on restrictions disease places on individual and consequences of performing a behavior. | “Diet, it becomes a frustration for me. I can’t have this, I can’t have that. I need clearance of everything that goes in my mouth and I hate it.” (FG 4 Patient 2) “Every aspect (of life) like financial, physical, social, emotional is affected.” (INT Patient 23) |
|
| Environmental Context and Resources | Circumstances of an individual’s situation or environment that encourages or discourages the development of skills and confidence. | “The kidney foundation has a very user friendly, simple manual.” (FG 1 Patient 2) “I prefer my information to come from like my doctor. I find reading online, yeah I don’t know what’s reliable and what’s not and then when you find something quite medical like that, it’s hard to kind of decipher how it applies to you. So, I find what’s most useful is kind of what is given to me by my physician.” (FG 1 Patient 4) |
|
| Who am I? | Social/professional role and identity | Identifying with a new or altered role. | “It’s all about coping as far as I’m concerned . . . it’s always trying to find my new normal as depending on where my kidneys are at and so for me my whole journey has been around balancing and trying to figure it out.” (FG 1 Patient 2) “I developed a line which said, normal is whatever the day is because it never is the same twice in our house.” (FG 1 Caregiver 1) |
Note. TDF = Theoretical Domains Framework; CKD = chronic kidney disease; GFR = glomerular filtration rate; FG = focus group; INT = telephone interview.
What does this mean for me?
Participants were seeking to understand CKD in relation to their illness experiences and personal situations. Two TDF domains corresponded to this theme: knowledge and intentions. Participants wanted credible CKD-specific information, along with information about diet, symptoms, travel, and medications that were relevant and tailored to their circumstance (eg, their individual comorbidities, lifestyle, occupational/social roles). Intentions were reflected in participants’ comments about the preferred timing of the information, for example, their “readiness” to learn independent of their CKD category or number of years since diagnosis.
Help me help myself
Participants reported that they felt they could actively manage their CKD if they had the knowledge and resources available to them. This theme encompassed three TDF domains. First, beliefs about capabilities (self-efficacy, self-confidence) as evidenced by participants’ references to being proactive and advocating for themselves and others. Examples of this were questions that patient participants asked about their medical condition, medications, and participating in physical activity. Second, behavior regulation (self-monitoring) which involved reminders (eg, alarms to take their medication) or tracking (eg, keeping a diary to record blood pressure). Finally, acquiring skills by repeated practice and applying new knowledge. For example, patient participants acquired new skills such as how use the Internet, how to communicate effectively with health care providers, and understanding their lab results.
How does this make me feel?
Participants discussed the emotions and feelings that were prevalent throughout the stages of CKD that corresponded to 4 common TDF domains. Social influences in the form of social supports such as support groups, family members, health care providers, and spiritual groups were important to help participants cope with the stigma and isolation related to living with CKD. Optimism included both positive (eg, being open to change) and negative feelings (eg, helplessness). Beliefs about consequences were mainly expectations about disease and treatment outcomes (eg, financial, physical, and emotional) and the consequences of performing a behavior (eg, taking medications that caused side effects). Finally, environmental context and resources were key factors contributing to their confidence in managing their personal health. Environmental context and resources included having access to or lack of access to health care professionals (HCPs), community supports, Internet (eg, Google, YouTube), along with access to their medical records (eg, lab results).
Who am I?
The fourth theme represented how people with CKD or those that care for them identified themselves in their “new” or “altered” roles. The TDF domain social/professional role and identity was relevant where participants had to modify their role to accommodate the “new normal.” Examples include reverse caregiver role (mutual support between patient and caregiver) and taking on the role of patient or caregiver in addition to their previous multiple roles (eg, wife/husband, parent, employee).
Discussion
Few studies of self-management interventions have considered behavior change theories in the development of their intervention.4 We undertook a deductive and inductive analysis of qualitative data to understand contributors of self-management behavior and identify intervention functions to inform the future development of a CKD self-management strategy. We coded self-management experiences of patients with CKD and their caregivers to the 14 TDF domains, resulting in identifying 5 TDF domains most common to supporting self-management for patients and caregivers: environmental context and resources, knowledge, beliefs about capabilities and consequences, and social influences. We also found 4 applicable intervention functions (ie, education, modeling, persuasion, and environmental restructuring) by linking the common TDF domains to relevant BCW intervention functions to identify potential intervention approaches. Four themes emerged around self-management behavior based on the 14 TDF domains: What does this mean for me? Help me help myself, How does this make me feel? and Who am I?
The TDF has been used in implementation studies within the health care setting.11,12 Most of these studies applied the TDF to identify barriers and facilitators to changing behavior at the organizational and system levels, with individual behavior change mainly focusing on HCPs. To our knowledge, this is the first study to explore potential contributors to behavior change using the TDF for patients with CKD and caregivers. The TDF allowed us to explore individual and environmental factors that contribute to the complexities of self-management behaviors.
Our findings extend those of prior studies in several ways. Past studies investigating CKD self-management interventions to slow further kidney function progression have focused on behaviors such as medication adherence, lifestyle changes (eg, engaging in physical activity, dietary modifications), and medical monitoring (eg, blood pressure, blood glucose). For individuals to optimally perform these behaviors, they need to be knowledgeable about CKD, its implications, and management to slow CKD progression. Previous researchers have discussed the need for CKD-specific information, building self-confidence, and providing social support.13-15 Our findings highlight that knowledge is important to patients and their caregivers to self-manage CKD; however, other contributors including environmental context and resources, beliefs about capabilities, beliefs about consequences, and social influences are also relevant.
Knowledge, environmental context, and resources provide a foundation for CKD self-management, along with the impacts of social influences and beliefs about consequences. These influence an individual’s beliefs about their capabilities, where the patient has confidence in their ability to do tasks to achieve positive results that are meaningful to them (ie, self-efficacy).16 Self-efficacy has been positively associated with self-management; therefore, supporting patient self-efficacy may facilitate successful CKD self-management.17 Addressing these 5 modifiable contributors may support patients in adopting and/or maintaining CKD self-management regimens.
There is a growing emphasis on person-centered care where patient preferences guide their health care,18 and self-management plays a key role in providing patient-centric care for individuals with CKD. Our themes demonstrate a behavioral-based account that speaks to participants’ interpretation of being diagnosed with CKD, their motivations, feelings, values, and altered identity. Each of the emergent themes include either “me” or “I” (eg, Help me help myself) to reflect the centrality of the participant’s voice. In addition, emphasis was not just on the diagnosis of CKD and the physical and medical needs, but on other factors that influence self-management including their environmental context, social influences, consequences, and capabilities. Our findings support the growing awareness that health care providers and researchers should recognize that not only physiological and physical states influence a patient’s actions, but their emotional status and personal context that are often equally or more important to the patient.19
We found that 4 intervention functions (ie, education, modeling, persuasion, and environmental restructuring) may be relevant for addressing 1 or more of the TDF domains. Some of the intervention functions can apply to a much wider range of TDF domains than others (ie, education and modeling can be used to address all 5 TDF domains). Designing a self-management intervention using a combination of these intervention functions may increase the capacity of patients and their caregivers to effectively self-manage CKD. Many CKD self-management interventions have used education as a component.20 Interactive and multifaceted features (eg, in-person teaching, written information, telephone follow-up) have also been reported to be effective in improving self-management.21 There is evidence in the chronic disease literature that positive role models (ie, peers with similar backgrounds and disease concerns) can increase an individual’s self-efficacy.16 Chronic kidney disease self-management intervention literature speaks to modeling, specifically related to the aid of peer support groups, individual peer support, and/or peers providing components of a self-management intervention.22,23
Along with education and modeling, persuasion and environmental restructuring were identified as possible intervention functions for bringing about behavior change. Many studies have reported using HCPs as the main provider of the self-management intervention, including nurses, dieticians, and social workers, to influence behavior change.4 Fewer studies have discussed concepts around environmental restructuring. For example, shopping tours of grocery store4 or cooking classes in the community.24 Education, modeling, persuasion, and environmental restructuring are practical intervention approaches that can be considered for a CKD patient self-management support intervention.
Limitations
Although this work is novel in the area of CKD self-management, there are limitations. First, performing a secondary analysis on data that were not structured around a priori TDF questions and resulted in some difficulty operationalizing the TDF. As a result, some domains may be underrepresented or not explored, even though they may be important in the self-management process (eg, goals, emotions). Second, we did not analyze the data according to participant role (ie, patient or caregiver) or gender; self-management needs may differ for these sub-groups. In addition, although the domains and associated constructs were well described, application to individual patient and caregiver experiences in some instances were challenging, and results therefore may vary depending on interpretation. Finally, the data were collected from a Canadian population and findings may not be applicable to other settings.
Conclusions
The TDF provided a systematic framework for assessment of CKD self-management behaviors and possible intervention approaches to influence behavior change in patients with CKD and their caregivers. These results will be used to inform the active components of an eHealth intervention to support self-management.
Supplemental Material
Supplemental material, Supplementary_Material_Appendix_1 for Understanding Adults With Chronic Kidney Disease and Their Caregivers’ Self-Management Experiences: A Qualitative Study Using the Theoretical Domains Framework by Sarah Baay, Brenda Hemmelgarn, Helen Tam-Tham, Juli Finlay, Meghan J. Elliott, Sharon Straus, Heather Beanlands, Gwen Herrington and Maoliosa Donald in Canadian Journal of Kidney Health and Disease
Acknowledgments
The authors would like to thank Sarah Gil who assisted in designing Figure 1.
Footnotes
Ethics Approval and Consent to Participate: An amendment using the nonidentifiable primary data set (ie, transcripts) received ethical approval in June 2018 from the Conjoint Health Research Ethics Board at the University of Calgary (REB 17-0908). Secondary consent was not required for this study.
Consent for Publication: All coauthors reviewed and approved the final manuscript for publication.
Availability of Data and Materials: Data and materials may be made available upon written request to the corresponding author. Reasonable requests for data access will be assessed in consultation with Conjoint Health Research Ethics Board.
Author Contributions: Each of the coauthors contributed to conception, design, acquisition of data, analysis, and interpretation of data and in drafting and revising manuscript for important intellectual content to varying degrees, but with equal effort.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is a project of the Can-SOLVE CKD Network, supported by the Canadian Institutes of Health Research under Canada’s Strategy for Patient-Oriented Research. They had no role in the design and conduct of the study; data collection, analysis, and interpretation; or preparation, review, or approval of the manuscript.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD: Meghan J. Elliott  https://orcid.org/0000-0002-5434-2917
https://orcid.org/0000-0002-5434-2917
References
- 1. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Richard AA, Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh. 2011;43(3):255-264. doi: 10.1111/j.1547-5069.2011.01404.x. [DOI] [PubMed] [Google Scholar]
- 3. Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177-187. [DOI] [PubMed] [Google Scholar]
- 4. Donald M, Kahlon BK, Beanlands H, et al. Self-management interventions for adults with chronic kidney disease: a scoping review. BMJ Open. 2018;8(3):e019814. doi: 10.1136/bmjopen-2017-019814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London, England: Siverback Publishing; 2014. [Google Scholar]
- 6. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398-405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 7. Donald M, Beanlands H, Straus S, et al. Identifying needs for self-management interventions in patients with chronic kidney disease and their caregivers: a qualitative study. American Journal of Kidney Diseases. 2019;pii: S0272-6386(19)30163-5. doi: 10.1053/j.ajkd.2019.02.006. [DOI] [Google Scholar]
- 8. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 9. Levin A, Adams E, Barrett BJ, et al. Canadians seeking solutions and innovations to overcome chronic kidney disease (Can-SOLVE CKD): Form and function. Can J Kidney Health Dis. 2018;5:1-12. doi:10.1177/2054358117749530. [DOI] [PMC free article] [PubMed]
- 10. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Phillips CJ, Marshall AP, Chaves NJ, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc. 2015;8:139-146. doi: 10.2147/JMDH.S78458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Costantini L, Beanlands H, McCay E, Cattran D, Hladunewich M, Francis D. The self-management experience of people with mild to moderate chronic kidney disease. Nephrol Nurs J. 2008;35(2):147-155; quiz 156. [PubMed] [Google Scholar]
- 14. Johnson ML, Zimmerman L, Welch JL, Hertzog M, Pozehl B, Plumb T. Patient activation with knowledge, self-management and confidence in chronic kidney disease. J Ren Care. 2016;42(1):15-22. doi: 10.1111/jorc.12142. [DOI] [PubMed] [Google Scholar]
- 15. Bowling CB, Vandenberg AE, Phillips LS, McClellan WM, Johnson TM, II, Echt KV. Older patients’ perspectives on managing complexity in CKD self-management. Clin J Am Soc Nephrol. 2017;12(4):635-643. doi: 10.2215/CJN.06850616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1-7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 17. Curtin RB, Walters BA, Schatell D, Pennell P, Wise M, Klicko K. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis. 2008;15(2):191-205. doi: 10.1053/j.ackd.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 18. Naldemirci O, Lydahl D, Britten N, Elam M, Moore L, Wolf A. Tenacious assumptions of person-centred care? exploring tensions and variations in practice. Health (London). 2018;22(1):54-71. doi: 10.1177/1363459316677627. [DOI] [PubMed] [Google Scholar]
- 19. Grey M, Schulman-Green D, Knafl K, Reynolds NR. A revised self- and family management framework. Nurs Outlook. 2015;63(2):162-170. doi: 10.1016/j.outlook.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 20. Zimbudzi E, Lo C, Misso ML, et al. Effectiveness of self-management support interventions for people with comorbid diabetes and chronic kidney disease: a systematic review and meta-analysis. Syst Rev. 2018;7(1):84. doi: 10.1186/s13643-018-0748-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lopez-Vargas PA, Tong A, Howell M, et al. Patient awareness and beliefs about the risk factors and comorbidities associated with chronic kidney disease: a mixed-methods study. Nephrology (Carlton). 2017;22(5):374-381. doi: 10.1111/nep.12829. [DOI] [PubMed] [Google Scholar]
- 22. Chen SH, Tsai YF, Sun CY, Wu IW, Lee CC, Wu MS. The impact of self-management support on the progression of chronic kidney disease: a prospective randomized controlled trial. Nephrol Dial Transplant. 2011;26(11):3560-3566. doi: 10.1093/ndt/gfr047. [DOI] [PubMed] [Google Scholar]
- 23. Hughes J, Wood E, Smith G. Exploring kidney patients’ experiences of receiving individual peer support. Health Expect. 2009;12(4):396-406. doi: 10.1111/j.1369-7625.2009.00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. deBrito-Ashurst I, Perry L, Sanders TA, et al. The role of salt intake and salt sensitivity in the management of hypertension in South Asian people with chronic kidney disease: a randomised controlled trial. Heart. 2013;99(17):1256-1260. doi: 10.1136/heartjnl-2013-303688. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Material_Appendix_1 for Understanding Adults With Chronic Kidney Disease and Their Caregivers’ Self-Management Experiences: A Qualitative Study Using the Theoretical Domains Framework by Sarah Baay, Brenda Hemmelgarn, Helen Tam-Tham, Juli Finlay, Meghan J. Elliott, Sharon Straus, Heather Beanlands, Gwen Herrington and Maoliosa Donald in Canadian Journal of Kidney Health and Disease


