Abstract
Background: The purpose of this study was to identify the incidence of upper extremity injuries presenting to emergency departments (EDs) nationally. Methods: The Nationwide Emergency Department Sample (NEDS) database was queried using International Classification of Diseases, Ninth Revision (ICD-9) codes specific for hand/wrist injuries to identify national estimates of ED visits. The incidence, mean age, gender, payer mix, hospital type, location (metropolitan vs nonmetropolitan), and geographic region were recorded. Results: In total, 2 791 257 patients with upper extremity injuries and infections were treated at an ED in 2010. In total, 7.4% resulted in hospital admission; 57% of patients were male. Most common age group affected was 18 to 44 years (44%), followed by those less than 17 years (24%) and 45 to 64 years (21%). The 3 most common injury classifications were soft tissue contusions (37%), fractures (27%), and infections (17%). Thirty-seven percent of patients had private insurance, 21% had Medicaid, 19% were uninsured, 13% Medicare, and 10% other. In total, 63% of visits were seen in nonteaching EDs, 80% were seen in metropolitan cities, and 65% of visits were seen at non–trauma-designated hospitals. Geographically, 37% of visits were in the South, 25% Midwest, 20% Northeast, and 18% in the West. Conclusions: Soft tissue contusion was the most frequent diagnosis. More than half of the patients were male, while the majority of patients were under the age of 44. Ninety-three percent of patients did not require hospital admission. Half had private insurance and the two-thirds of these patients were seen at nonteaching facilities.
Keywords: trauma, infections, hand injuries, emergency care, upper extremity
Introduction
According to the National Center for Health Statistics, there were 37.2 million injury-related emergency department (ED) encounters nationwide during 2013.11 Injuries to the upper extremity remain one of the most common presentations in the ED making up approximately 10% of all traumas nationwide.13,16 These diagnoses range from simple lacerations and cellulitis to complex amputations and limb-threatening necrotizing infections. Injuries to the hand and upper extremity can be quite complex often requiring a fellowship trained hand surgeon to repair complicated neurovascular injuries and restore proper mechanical function to the upper extremity. These injuries result in significant use of ED resources annually. In 2013, traumatic injuries cost the US health care system approximately 92 billion dollars, second only to heart disease.2 According to the Nationwide Emergency Department Sample (NEDS), more than 2.7 million hand- and wrist-related injuries/infections presented to the ED nationwide.12 Over the last 20 years, utilization of EDs has drastically increased, making it imperative to provide proper resident education and resource allocation to cater to the patient populations and injuries that are most commonly encountered in modern clinical practice.19 Injuries to the hand and wrist often result in significant time missed from work. In more severe cases, these injuries may lead to permanent disability. Currently, very little research exists regarding the epidemiology of upper extremity trauma. Furthermore, the existing literature has yet to provide a common consensus regarding the prevalence and anatomical distribution of these injuries. As a result, it is impossible to develop accurate and evidence-driven changes to the current health care infrastructure. All data presented in this study are provided by the NEDS. The NEDS database provides samples from both the State Inpatient Databases (SID) and State Emergency Department Databases (SEDD), which includes discharge data from 945 hospitals in 33 states in addition to the District of Columbia, providing a 20% stratified sample of US hospital–based EDs. Nationwide Emergency Department Sample is part of the Healthcare Cost and Utilization Project (HCUP), which provides data that are generalized to the nation’s population to drive quality improvement measures and medical education.12 The purpose of this study was to perform a cross-sectional descriptive epidemiological study identifying trends in emergent care for patients with upper extremity injuries and infections using data generalizable to the US population.
Methods
The NEDS database was queried using common International Classification of Diseases, Ninth Revision (ICD-9) codes specific for hand/wrist injuries and infections presenting between January 1, 2010, and December 31, 2010, to identify national estimates of ED visits for these related diagnoses. Injury diagnoses within the NEDS database are categorized as vascular, infection, fractures, dislocations, burns, tendon, crush injury, nerve injury, amputation, laceration, abrasion, and contusion. We selected data pertaining to the incidence by injury type, age, gender, payer mix, hospital type (teaching vs nonteaching), location (metropolitan vs nonmetropolitan), and geographic region (north, south, east, and west) for use in this study. We further stratified the 3 most common types of injuries (contusion, fracture, infection/inflammation) by anatomical location and age. Fractures and contusions involving multiple anatomical locations (ie, fingers and hand, wrist and hand, etc) were excluded from this portion of the analysis. Frequency of infections/inflammatory pathologies of the wrist and hand were combined due to ICD-9 coding of synovitis and tenosynovitis. Statistical analysis using one-way analysis of variance (ANOVA) test was performed comparing frequencies of specific injuries by payer status as well as geographic region. P value < .05 was considered statistically significant.
Results
A query of the NEDS database resulted in a weighted estimate of 2 791 257 records of traumatic hand/wrist pathology treated at an ED in the United States in 2010. Of these visits, only 207 109 (7.4%) resulted in hospital admission. Fifty-seven percent of patients were male, while the remaining 43% of patents were female. The NEDS database stratified patient age into specific groups. The most frequent pathological classification was soft tissue contusion (33%), followed by fractures of the extremity (27%). The other diagnoses included infection/inflammation (17%), burns (4.5%), laceration (4.3%), crush (3.2%), abrasion (2.4%), foreign body (2.3%), amputation (2%), tendon (0.9%), nerve (0.7%), and vascular (0.6%). Table 1 depicts the incidence by age and location (wrist, hand, fingers) for the 3 most common types of hand/wrist injuries (contusion, fractures, infection). Figure 1 depicts the frequency of ED visits sorted by age. Figure 2 depicts the payer mix. Figure 3 depicts the frequency of ED visits by region (north, south, east, and west). Roughly two-thirds or 63% of these visits were seen in nonteaching EDs. Eighty percent of these ED visits were seen at hospitals in large metropolitan cities. Sixty-five percent of these visits were seen at non–trauma-designated hospitals. There was no statistical significant difference seen among the 3 most common injury types when compared by payer status (Table 2). Although there appeared to be an increased frequency of injuries in the Southern states, this also did not reach statistical significance (Table 3).
Table 1.
Frequency by Age and Location (Wrist, Hand, Fingers) for the 3 Most Common Types of Hand/Wrist Injuries (Contusion, Fractures, Infection).
| Age | Contusion |
Fractures |
Infection/inflammation |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| W | H | F | T | W | H | F | T | W/H | F | T | |
| ≤17 | 42 391 | 107 936 | 99 057 | 249 384 | 7047 | 30 587 | 108 998 | 146 632 | 30 540 | 28 014 | 58 554 |
| 18-44 | 73 479 | 258 136 | 98 112 | 429 727 | 26 718 | 81 641 | 130 055 | 238 414 | 154 429 | 67 602 | 222 031 |
| 45-64 | 33 235 | 78 630 | 32 900 | 144 765 | 11 255 | 18 732 | 77 089 | 107 076 | 94 185 | 32 964 | 127 149 |
| 65-84 | 17 979 | 39 518 | 19 337 | 76 834 | 5 551 | 7 567 | 28 107 | 41 225 | 38 553 | 7742 | 46 295 |
| ≥85 | 5844 | 12 197 | 2513 | 20 554 | 2256 | 2243 | 5662 | 10 161 | 9843 | 1167 | 11 010 |
| All ages | 172 929 | 486 417 | 242 096 | 921 264 | 42 697 | 140 770 | 349 911 | 533 358 | 327 550 | 137 489 | 461 592 |
Note. W = wrist; H = hand; F = fingers; T = sum of all locations.
Figure 1.
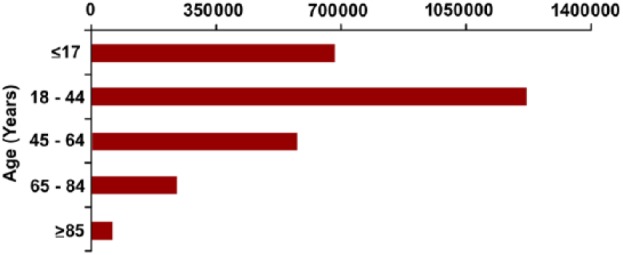
Frequency of hand and wrist pathology by age.
Figure 2.
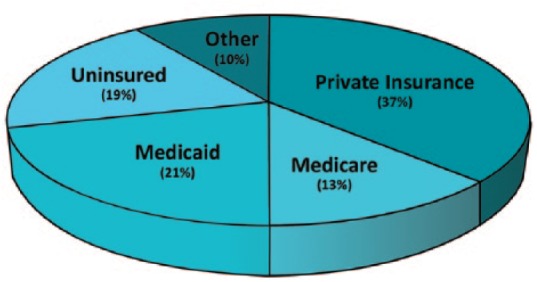
Payer mix of all patients presenting to the emergency department with hand/wrist injuries in 2010. Insurance status categorized as private, Medicare, Medicaid, uninsured, or other.
Figure 3.
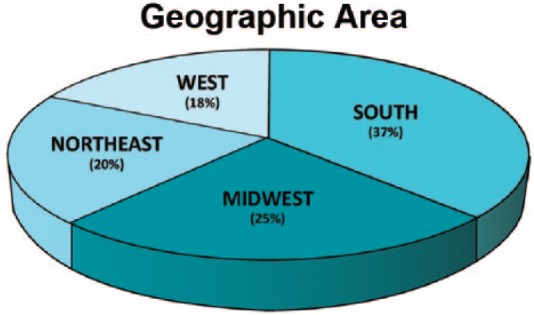
Distribution of patient presentation to US emergency departments by region (north, south, east, and west).
Table 2.
Injury Type by Insurance Type Listed as Percent (P = .132).
| Injury Type | Medicare | Medicaid | Private | Uninsured |
|---|---|---|---|---|
| Fracture | 15 | 20 | 46 | 18 |
| Contusion | 13 | 28 | 38 | 18 |
| Infection | 16 | 24 | 36 | 14 |
Table 3.
Injury Type by Geographical Region Listed as Percent (P = .09).
| Injury Type | Northeast | Midwest | South | West |
|---|---|---|---|---|
| Fracture | 19 | 26 | 35 | 20 |
| Contusion | 21 | 26 | 39 | 14 |
| Infection | 21 | 22 | 40 | 17 |
Discussion
Few studies have been published to investigate the epidemiological trends of upper extremity injuries in the United States. Consequently, it is difficult to determine resource allocation, health care staff education, and community prevention measures that accurately represent the distribution of patients utilizing the ED each year. The lack of a uniform and evidence-based approach to drive these endeavors is in part due to delay in the adoption of the electronic medical record (EMR) which now allows for increased accessibility of such data. Ootes et al published the only comprehensive epidemiological study involving all categories of upper extremity injuries in the United States.13 Giustini et al and Polinder et al conducted the only comparable studies in Italy and the Netherlands, respectively.3,15 Other similar epidemiological studies are more limited due to their focus on 1 type of injury, anatomical location, or age group.1,6,7,17,18 The data presented by the previously mentioned studies provide invaluable insight into frequency of injury type by location. However, changes to resource allocation and education should not be guided by such a limited number of studies. Furthermore, the findings of Giustini et al and Polinder et al provide useful information regarding upper extremity injuries, and yet trends seen in Italy and the Netherlands should not be used to guide decision making involving the US population. Decisions regarding changes to public health and education require a large body of evidence to maximize the efficiency of EDs and minimize the occurrence of such injuries in the first place. We aim to add to the existing body of evidence investigating upper extremity injuries and provide insight that can be directly generalized to the US population. Previous studies have shown that injuries to the hand are more common compared with those of the rest of the upper extremity.5,13,15 For this reason, this study was focused on the frequency and patient demographics involving injuries of the wrist, hand, and digits.
The most frequent injury classification in this study was soft tissue contusion (33%), which differs from the data presented by other studies. Finger lacerations were found to be the most common injury by anatomical location by Ootes et al13 while they were found to be less frequent in this study than soft tissue contusions, fractures, and infection/inflammatory processes of the hand, wrist, and digits, with the exception of fractures of the wrist (Table 1). The data reported by Giustini et al support the findings of Ootes et al with open wound to the finger being the most common injury to the hand/wrist (20.8%), followed by contusion of the finger (8.3%).3,13
The increased incidence of ED visits in the South compared with other regions (Figure 3) may be due to warmer climate, increasing the amount of time spent doing home improvement activities or outside participating in recreational activities. This reasoning is supported by the findings of Ootes et al. They reported that most upper extremity injuries occur at home (45.4%), followed by place of recreation or sport (16.2%).13 Further investigation into factors associated to the mechanism of injury and patient demographics may illuminate a more precise reason for such findings.
Upper extremity trauma was most frequent in ages 18 to 44, which differs from those reported by other studies. Giustini et al report the most frequent age group presenting with upper extremity injuries in Italy is 10 to 14 years of age, while Polinder et al report the highest incidence in males and females 0 to 14 years of age in the Netherlands.5,19 These differences may be inherent differences between European and American patient populations and will require additional comparative studies to determine a more definitive reason. Furthermore, additional information regarding the mechanism of injury would help elucidate the reason behind such differences.
Insurance status of patients presenting to US EDs for upper extremity trauma has not been previously reported in other similar large-scale epidemiologic studies. More than half of the patients in this study did not have private insurance (63%). In addition, the incidence of uninsured patients in this study is 19%, which coincides with the national average (16.3%) reported by the US Census Bureau in 2010.11 Insurance status is of particular importance in upper extremity trauma. Uninsured patients have not been reported to have higher rates of trauma compared with insured counterparts. However, increased morbidity and mortality have been associated with lack of insurance when investigating trauma patients, which is thought to be associated with deceased health literacy, delay in proper treatment, and administration of fewer diagnostic tests.4,5,16
Only a small proportion of patients in this study (7.4%) required hospital admission for the management of their injuries, suggesting that most injuries to the upper extremity are not limb threatening when treated appropriately. This coincides with the values reported by Giustini et al. Their study reported an overall hospital admission rate of 10% for upper extremity injuries, and that this rate varied significantly between injuries to the hand (5.1%) and injuries to the arm (17.4%).3 The precise reason for these differences was not reported but is likely due to the higher morbidity and mortality associated with neurovascular compromise of the proximal extremity compared with that of the hand and fingers. In addition, injuries to the upper and lower extremities are the most common reason for hospitalization in patients presenting with nonfatal trauma. More than one-third of the patients requiring hospitalization for conditions involving the extremities had either serious or limb-threatening injuries.2,9,10
As a result of the large pool of patients and sampling from hospitals ranging in size and trauma rating from all regions of the country, the NEDS database serves as a useful tool to provide data that more closely represent the trends seen nationwide. However, the NEDS database, like other similar databases, has limitations. The fact that the database used only has data for the year 2010, as well as the amount of time between data collection and publication, is a major limitation. As a result, these data may not fully represent current trends despite the many benefits of the NEDS database. Due to the retrospective nature of this database, there may be instances of incorrect ICD-9 input so that it is possible the data do not perfectly match the trends seen clinically. In addition, the direct mechanism and setting in which the injury occurred were not reported by this database and, for this reason, were not included in the study. Mackenzie and Fowler reported that the most common cause for injury to the extremity in a civilian population was falling, and was seen in 30% of upper extremity injuries, followed by industrial work–related accidents and motor vehicle–related accidents.9 Ameri et al report similar findings in their epidemiologic study of upper extremity fractures. They found that falls were the most common cause of fracture for all anatomical locations (shoulder, humerus, forearm, and wrist) except the hand in which direct impact was more common.1 Despite the previously mentioned limitations, the data included in this study provide useful information, serving as additional support to bolster the current knowledge while providing new insight regarding insurance status and geographic location. Collectively, the existing studies in addition to those to be published in the future will help drive change to the US health care system.
In summary, injuries to the hand and wrist are common and resulted in 2.7 million ED visits in 2010. The majority of patients do not require hospital admission. Less than half had private insurance, and the majority of these patients were seen at nonteaching facility. Development of a registry specific to hand and upper extremity traumas in the United States would aid in making accurate quality improvement measures allowing for increased efficiency of resource allocation and education to both hospital personnel and the community. Such registries already exist in other countries, including the “Hand Trauma Alliance” in Germany and “FESUM” (Fédération des services d’urgences de la main [European Federation of Hand Emergency Services]) in France, Belgium, and Switzerland.8,14
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: Authors are required to ensure the following guidelines are followed, as recommended by the International Committee of Medical Journal Editors, Uniform Requirements for Manuscripts Submitted to Biomedical Journals. Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ameri M, Aghakhani K, Ameri E, et al. Epidemiology of the upper extremity trauma in a traumatic center in Iran. Glob J Health Sci. 2017;9(4):97-105. [Google Scholar]
- 2. Finkelstein EA, Corso PS, Miller TR, et al. The incidence and economic burden of injuries in the United States. J Epidemiol Community Health. 2007;61(10):926. [Google Scholar]
- 3. Giustini M, de Leo A, Leti A, et al. Incidence estimates of hand and upper extremity injuries in Italy. Ann Ist Super Sanita. 2015;51(4):305-312. [DOI] [PubMed] [Google Scholar]
- 4. Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84(10):1605-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945-949. [DOI] [PubMed] [Google Scholar]
- 6. Larsen CF, Brondum V, Skov O. Epidemiology of scaphoid fractures in Odense, Denmark. Acta Orthop Scand. 1992;63(2):216-218. [DOI] [PubMed] [Google Scholar]
- 7. Larsen CF, Mulder S, Johansen AM, et al. The epidemiology of hand injuries in the Netherlands and Denmark. Eur J Epidemiol. 2004;19(4):323-327. [DOI] [PubMed] [Google Scholar]
- 8. Leixnering M, Quadlbauer S, Szolarcz C, et al. Prevention of hand injuries—current situation in Europe. Handchir Mikrochir Plast Chir. 2013;45(6):339-343. [DOI] [PubMed] [Google Scholar]
- 9. Mackenzie EJ, Fowler CJ. Epidemiology. In: Mattox KL, Moore EE, Feliciano DV, eds. Trauma. 6th ed. New York, NY: McGraw-Hill; 2008:25. [Google Scholar]
- 10. Nance ML. National trauma data bank annual report. http://www.facs.org/trauma/ntdb/pdf/ntdb-annual-report-2012.pdf. Published 2012. Accessed August 13, 2017.
- 11. National Hospital Ambulatory Medical Care Survey: 2013 Emergency Department Summary Tables. Tables 1, 4, 14, 24. Date unknown. https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2013_ed_web_tables.pdf. Accessed August 13, 2017.
- 12. NEDS Database Documentation. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2016. www.hcup-us.ahrq.gov/db/nation/neds/nedsdbdocumentation.jsp. Accessed August 13, 2017. [PubMed] [Google Scholar]
- 13. Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand. 2012;7(1):18-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pajardi GE, Cortese PD. The Italian CUMI. Handchir Mikrochir Plast Chir. 2013;45(6):332-334. [DOI] [PubMed] [Google Scholar]
- 15. Polinder S, Iorden GI, Pannneman MJ, et al. Trends in the incidence and cost of injuries to the shoulder, arm, and wrist in the Netherlands between 1986 and 2008. BMC Public Health. 2013;13(1):531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosen H, Fady S, Lipsitz S. Downwardly mobile: the accidental cost of being insured. Arch Surg. 2009;144(11): 1006-1010. [DOI] [PubMed] [Google Scholar]
- 17. Van Onselen EB, Karim RB, Hage JJ, et al. Prevalence and distribution of hand fractures. J Hand Surg Br. 2003;28(5): 491-495. [DOI] [PubMed] [Google Scholar]
- 18. Van Tassel DC, Owens BD, Wolf JM. Incidence estimates and demographics of scaphoid fracture in the U.S. population. J Hand Surg Am. 2010;35(8):1242-1245. [DOI] [PubMed] [Google Scholar]
- 19. Weiss AJ, Wier LM, Stocks C, et al. Overview of Emergency Department Visits in the United States, 2011. HCUP Statistical Brief #174. Rockville, MD: Agency for Healthcare Research and Quality; http://www.hcupus.ahrq.gov/reports/statbriefs/sb174-Emergency-Department-Visits-Overview.pdf. Published June 2014. Accessed August 13, 2017. [PubMed] [Google Scholar]


