Abstract
Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T-cell lymphoma (PCAT) is a rare and heterogeneous entity with less than 100 published cases to date. A 68-year-old man was following up for an inflammatory lichen–lupus overlap dermatosis of 3 years duration. Treatment with methotrexate was started, observing a dramatic change in the skin lesions that became infiltrated plaques and generalized ulcerated tumours distributed over trunk and extremities. Histological study showed marked epidermotropism of CD8 positive cells and monoclonality was demonstrated by the polymerase chain reaction. Diagnosis of PCAT was concluded. Treatment with polychemotherapy was indicated. The PCAT is characterized by a rapid clinical history of generalized papules, plaques, nodules and tumours with frequent ulceration and necrosis. Although it has no pathognomonic clinical features, there are clinical, histological and prognostic data that define them as a group and differentiate them from other lymphomas. Exceptionally, there are cases reported which have been triggered following treatment with immunosuppressive drugs. In our patient we think that PCAT was triggered by the transformation of a pre-existing dermatosis, which had never showed a lymphoproliferative profile in biopsies before. A possible pathogenic mechanism is that in some inflammatory dermatoses, chronic antigenic stimulation in a situation of iatrogenic immunosuppression may favour the development of a malignant clonal T cell.
Keywords: Cutaneous oncology, cutaneous T-cell lymphoma, lymphomas, treatment of lymphoma
Introduction
Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T-cell lymphoma (PCAT), a rare and heterogeneous entity is a subtype of cutaneous T-cell lymphoma. It was first described in 1999 by Berti et al.[1] With less than 100 published cases to date, it is currently classified as a provisional entity according to the latest World Health Organization/European Organization for Research and Treatment of Cancer (WHO/EORTC) classification.[2]
Clinical case
A 68-year-old man was being followed up for a histopathologically proven inflammatory lichen–lupus dermatosis of 3 years duration. Due to the loss of response to oral retinoids, methotrexate was started, observing a dramatic change in the skin lesions that became infiltrated plaques and generalized tumours distributed over the trunk and extremities, some of which were ulcerated [Figure 1]. A biopsy was performed, showing in the superficial dermis a dense proliferation of small to medium-sized cells, with slightly enlarged and irregular nuclei, affecting and erasing the entire interface, with marked epidermotropism, focally infiltrating some hair follicles and blood vessels [Figure 2a]. Necrotic keratinocytes were observed. Immunohistochemical techniques showed a CD8 positive [Figure 2b], CD4 positive, BF1 positive, Granzima positive, TIA1 positive [Figure 2c and d], CD30 negative, CD56 negative, Epstein–Barr RNA negative, Ki67 with nuclear positivity in more than 50% of the lymphoid cellularity and focal immunopositivity for perforin. Monoclonality was proved by means of a Genomic Identification Analysis study of the clonal reordering of the hypervariable regions of the TCR-G gene and TCR-B by polymerase chain reaction and capillary electrophoresis. Studies for evaluation of extension of disease with haemogram, serologies including human T-lymphotropic virus type I and 2, bone marrow biopsy and computed tomography scan did not found any alterations. Diagnosis of PCAT was concluded. Treatment with cyclophosphamide + doxorubicin + vincristine + prednisone (CHOP) was indicated. After five sessions the lesions improved. At present, the patient continues in follow up.
Figure 1.

(a) Multiple papulonodular erythematous lesions and tumour with crustal surface located in lower extremities. (b) Some lesions had arcuate morphology and left residual hyper- and hypopigmentation
Figure 2.
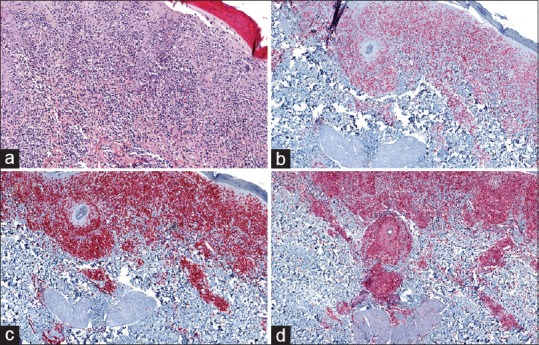
(a) HE 4× abundant cells of lymphoid strain densely arranged in superficial dermis. (b) Positivity for CD8. (c) Positivity for CD3. (d) Positivity for TIA
Commentary
The PCAT is characterized by a rapid clinical history of generalized papules, plaques, nodules and tumours which frequently present with central ulceration and necrosis.[3,4] Although it has no pathognomonic clinical features, there are data that define them as a group. The principal differential diagnosis must be made with fungoid CD8 positive mycosis based on the following criteria:
Absence of previous cutaneous lesions of mycosis fungoides is mandatory for the diagnosis[1,2,3]
In PCAT histology highlights epidermotropism, along with a dermal and angiocentric infiltrate with a cytotoxic immunohistochemistry pattern CD8 positive, EVB negative, CD56 negative and monoclonality.[3,4] The histopathology of mycosis fungoides tends to be less pagetoid with more pleomorphic and convoluted nuclei and most importantly without necrotic keratinocytes
In PCAT, there is rapid progression and poor prognosis with no response to conventional therapies for CD4 positive lymphomas,[1,2,3] while current evidence suggest that mycosis CD8 positive cases have the same clinical behaviour and prognosis as more common CD4 positive cases.[4]
Exceptionally, there are cases reported that have been triggered following treatment with immunosuppressive drugs.[5] In our patient we think that PCAT was triggered by the transformation of a pre-existing dermatosis, which had never showed a lymphoproliferative profile in biopsies before, shortly after initiating treatment with methotrexate. A possible pathogenic mechanism is that in some inflammatory dermatoses, chronic antigenic stimulation in a situation of iatrogenic immunosuppression may favour the development of a malignant clonal T cell.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Berti E, Tomasini D, Vermeer MH, Meijer CJLM, Alessi E, Willemze R. Primary cutaneous CD8 positive epidermotropic cytotoxic T-cell lymphoma: A distinct clinicopathologic entity with an aggressive clinical behaviour. Am J Pathol. 1999;155:483–92. doi: 10.1016/S0002-9440(10)65144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paulli M, Berti E. Cutaneous T cell lymphomas (including rare subtypes): Current concepts, II. Haematologica. 2004;89:1372–88. [PubMed] [Google Scholar]
- 4.Guitart J, Martinez-Escala ME, Subtil A, Duvic M, Pulitzer MP, Olsen EA, et al. Primary cutaneous aggressive epidermotropic cytotoxic T-cell lymphomas: Reappraisal of a provisional entity in the 2016 WHO classification of cutaneous lymphomas. Mod Pathol. 2017;30:761–72. doi: 10.1038/modpathol.2016.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson WT, Leeman-Neill RJ, Patel P, Ho J, Grandinetti LM, Jedrych J, et al. Fatal case of primary cutaneous aggressive T-OOcell lymphoma switching from a CD4+ to a CD8+ phenotype: Progressive disease with bexarotene and romidepsin treatment. Am J Dermatopathol. 2016;38:832–7. doi: 10.1097/DAD.0000000000000609. [DOI] [PubMed] [Google Scholar]


