Abstract
Purpose: We examined risk of myocardial infarction and all-cause death associated with the extent of coronary artery disease ascertained by coronary angiography in patients with diabetes mellitus. We hypothesized that risks of myocardial infarction and death were associated with extent of coronary artery disease in diabetes patients.
Patients and methods: We conducted a cohort study of patients with type 1 and type 2 diabetes, who underwent coronary angiography from 2004 to 2012. Patients were stratified according to extent of coronary artery disease: 0-, 1-, 2- or 3-vessel disease or diffuse vessel disease. Endpoints were myocardial infarction, all-cause death, and major adverse cardiovascular events (MACE), defined as the composite of myocardial infarction, cardiac death, or ischemic stroke. Adjusted incidence and mortality rate ratios (IRRsadj) were calculated using patients with 0-vessel disease as the reference group. Median follow-up was 3 years for a total of 45,164 person-years.
Results: The study included 12,594 diabetes patients. Of these, 3,147 (25.0%) had 0-vessel disease, 1,195 (9.5%) had diffuse vessel disease, 3,001 (23.8%) had 1-vessel disease, 2,220 (17.6%) had 2-vessel disease, and 3,031 (24.1%) had 3-vessel disease. The myocardial infarction rate was 0.4 per 100 person-years (95% CI: 0.3–0.5) in patients with 0-vessel disease. Using patients with 0-vessel disease as reference, the risk of myocardial infarction increased according to the number of diseased vessels (diffuse vessel disease: 1.4 per 100 person-years, IRRadj 3.87, 95% CI: 2.41–6.23; 1-vessel disease: 1.9 per 100 person-years, IRRadj 4.99, 95% CI: 3.33–7.46; 2-vessel disease: 2.7 per 100 person-years, IRRadj 7.14, 95% CI: 4.78–10.65; and 3-vessel disease: 4.3 per 100 person-years, IRRadj 11.42, 95% CI: 7.76–16.82; ptrend<0.001). Similar associations were observed for all-cause death and MACE.
Conclusion: The extent of coronary artery disease is a major risk factor for myocardial infarction and death in patients with diabetes mellitus.
Keywords: coronary angiography, epidemiology, Western Denmark Heart Registry, death
Introduction
Only a few studies with either short-term follow-up after coronary angiography (CAG) or long-term follow-up after coronary computed tomography have examined the association between extent of coronary artery disease (CAD) and clinical outcomes in patients with diabetes mellitus.1–3 We hypothesized that the risk of myocardial infarction (MI) and death is associated with the extent of CAD in diabetes patients. If so, a differentiated characterization of the extent of CAD may have a perspective for more individualized preventive treatment strategies for diabetes patients than currently used.
Assessment of CAD by CAG has been described as a valid prognostic tool in risk stratification of diabetes patients.4 In the current study, we conducted a median follow-up of 3 years in diabetes patients undergoing CAG to evaluate whether increasing extent of obstructive CAD is associated with incremental MI and death rates.
Material and methods
Data sources
Each Danish resident is assigned a unique and permanent 10-digit personal identifier at birth or upon immigration. This identifier is included in every Danish health registry and enables accurate long-term follow-up data with minimal risk of loss to follow-up. The Western Denmark Heart Registry (WDHR) is a clinical database containing information on all patients referred for diagnostic, invasive, and surgical procedures since 1999 in Western Denmark (population: 3.3 million people).5,6 The WDHR has collected data on >240,000 CAGs, including a detailed description of the presence and extent of CAD. In addition to the WDHR, we used the following databases in the current study: the Civil Registration System, which collects data on all Danish residents’ vital status (dead, alive, or emigrated); the Danish National Patient Registry, which includes all inpatient and outpatient hospital diagnoses in Denmark; and the Danish National Health Service Prescription Database, which registers data on all reimbursed prescriptions redeemed at Danish pharmacies.7–9 According to Danish law, observational registry-based studies require no approval from local or national ethics committees.
Diabetes
Diabetes patients, with type 1 or type 2 diabetes patients, were identified through the WDHR and the Danish National Health Service Prescription Database.5,6,9 In the WDHR, diabetes patients are classified according to their diabetes treatment (insulin ± oral glucose-lowering treatment, oral glucose-lowering treatment, or nonpharmacological dietary treatment) at the time of CAG intervention. To confirm this information and to include newly diagnosed diabetes patients, we also used the Danish National Health Service Prescription Database to identify patients who had redeemed of ≥1 prescription for anti-diabetes treatment (insulin or non-insulin diabetes medication) within 6 months before and 1 month after CAG. Relevant Anatomical Therapeutic Chemical codes are provided in the supplementary material, Table S1.
Table S1.
Anatomical therapeutic chemical codes used in the Danish National Health Service prescription database
| Medication | Anatomical therapeutic chemical (ATC) code |
|---|---|
| Insulin | A10A |
| Non-insulin diabetes medication | A10B |
| Statins | C10AA |
| Aspirin | B01AC22, N02BA01 |
| Adenosine diphosphate receptor inhibitors | B01AC04, B01AC22, B01AC24 |
| Angiotensin-converting enzyme inhibitors | C09A, C09B |
| Angiotensin II receptor blockers | C09C, C09D |
| Beta-blockers | C07 |
| Calcium channel blockers | C08C, C08D |
Coronary artery disease
Patients were stratified according to extent of CAD, ie the number of coronary arteries with obstructive CAD (defined as ≥50% angiographic stenosis): 0-, 1-, 2- or 3-vessel disease (VD), or diffuse VD (ie nonobstructive CAD, defined as <50% stenosis in >1 coronary vessel).
Patient selection
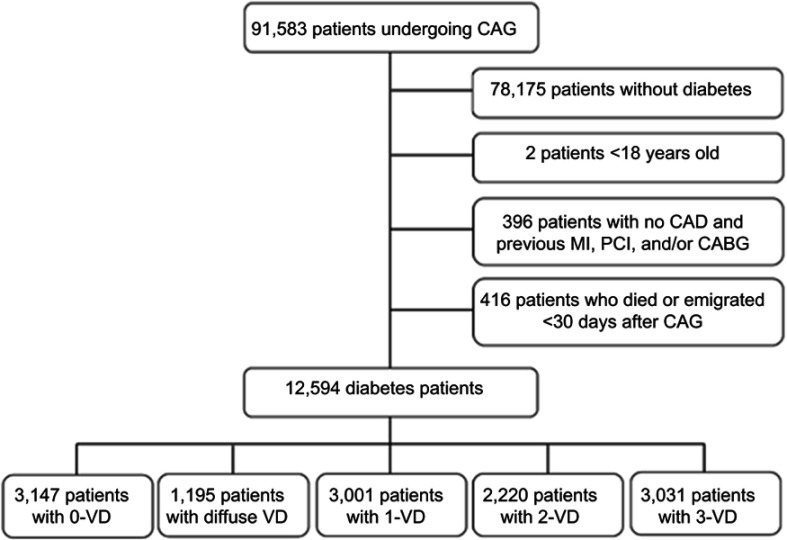
All diabetes patients with a CAG procedure registered in the WDHR from July 1, 2004 to July 30, 2012 were included in the study (Figure 1). Patients without diabetes were excluded (N=82,980). For patients who underwent multiple CAG examinations during the study period the first CAG was regarded as the index procedure. Patients classified as having no CAD despite previous MI, percutaneous coronary intervention, and/or coronary artery bypass grafting were excluded due to risk of misclassification (N=396). Patients who died or emigrated <30 days after CAG (N=416) also were excluded. All patients were ≥18 years old.
Figure 1.
Flowchart of selection of diabetes patients who underwent coronary angiography in Western Denmark between July 1, 2004 and July 30, 2012.
Abbreviations: CAG, coronary angiography; CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; VD, vessel disease.
Comorbidity
Comorbidities were evaluated using the Charlson Comorbidity Index score based on ICD-10 codes (supplementary material, Table S2) registered in the Danish National Patient Registry. We used a 5-year look-back period of patient history before the study inclusion date.10 A modified Charlson Comorbidity Index score (excluding “diabetes” and “diabetes with end-organ damage”) was estimated for each patient on the date of the index CAG.
Table S2.
ICD-10 codes used in the Charlson Comorbidity Index (CCI) score based on data in the Danish National Patient Registry, including weights of each item included in the CCI
| Disease | Weight | ICD-10 codes |
|---|---|---|
| Myocardial infarctiona | 1 | I21, I22, I23 |
| Congestive heart failure | 1 | I50, I11.0, I13.0, I13.2 |
| Peripheral vascular disease | 1 | I70-I74, I77 |
| Cerebrovascular disease | 1 | I60-I69, G45, G46 |
| Dementia | 1 | F00-F03, F05.1, G30 |
| Chronic pulmonary disease | 1 | J40-J47, J60-J67, J68.4, J70.1, J70.3, J84.1, J92.0, J96.1, J98.2, J98.3 |
| Connective tissue disease | 1 | M05, M06, M08, M09, M30-M36, D86 |
| Ulcer disease | 1 | K22.1, K25-K28 |
| Mild liver disease | 1 | B18, K70.0-K70.3, K70.9, K71, K73, K74, K76.0 |
| Diabetes I and II | 1 | E10.0, E10.1, E10.9, E11.0, E11.1, E11.9 |
| Hemiplegia | 2 | G81, G82 |
| Moderate to severe kidney disease | 2 | I12, I13, N00-N05, N07, N11, N14, N17-N19, Q61 |
| Diabetes with end-organ damage | 2 | E10.2-E10.8, E11.2-E11.8 |
| Any tumor | 2 | C00-C75 |
| Leukemia | 2 | C91-C95 |
| Lymphoma | 2 | C81-C85, C88, C90, C96 |
| Moderate to severe liver disease | 3 | B15.0, B16.0, B16.2, B19.0, K70.4, K72, K76.6, I85 |
| Metastatic solid tumor | 6 | C76-C80 |
| AIDS | 6 | B21-B24 |
Notes: aICD-10 code I21 was used as a primary or secondary discharge diagnosis during an acute hospitalization for myocardial infarction events 30 days or more after coronary angiography.
Medication
Records of treatment with statins, aspirin, adenosine diphosphate (ADP) receptor inhibitors, angiotensin-converting-enzyme (ACE) inhibitors/angiotensin II receptor blockers, β-blockers, and calcium channel blockers were ascertained from the Danish National Health Service Prescription Database (anatomical therapeutic chemical codes are provided in the supplementary material, Table S1).9 Treatment was defined as reimbursement for a redeemed prescription between 6 months before and 1 month after the index CAG date.
Myocardial infarction
MI diagnoses were obtained from the Danish National Patient Registry (Supplementary Material, Table S2). Follow-up began 30 days after CAG, as an MI diagnosis has shown less validity during the first 30 days after CAG (due to interhospital patient transfers and initial double registration of MI).11
All-cause death
Information on all-cause death was obtained from the Civil Registration System. The Civil Registration System is virtually complete, with approximately 0.3% persons lost to follow-up.12
Major adverse cardiovascular events
Major adverse cardiovascular events (MACE) were defined as the composite of MI, ischemic stroke, and cardiac death. Ischemic stroke was ascertained from the Danish National Patient Registry (ICD-10 codes: DI-63-64). Cardiac death was obtained from death certificates (ICD-10 codes: DI-20-25, DI-46, DI-47.2, DI-50, R-96) from the Danish Register of Causes of Death.13
Statistical analyses
Follow-up began 30 days after the index CAG. For MI, follow-up continued until first MI, death, emigration, or end of follow-up (December 31, 2012), whichever occurred first. For death, follow-up continued until death, emigration, or end of follow-up. For MACE, follow-up continued until MI, ischemic stroke, death, emigration, or end of follow-up. Due to lack of access to death certificates in 2012, patient inclusion was restricted to June 30, 2011 and end of follow-up was December 31, 2011 for MACE. We estimated event rates for MI, death, and MACE per 100 person-years and constructed cumulative incidence proportion curves corresponding to the seventy-fifth percentile of follow-up. As the data did not meet criteria for proportional hazards, we subsequently estimated incidence rate ratios (IRRs) and adjusted IRRs (IRRsadj) for the clinical endpoints using modified Poisson regression with the event as the outcome and the natural log of person-years as the offset.14 Patients with 0-VD were used as reference. IRRs were adjusted for age, sex, smoking status, hypertension, modified Charlson Comorbidity Index score, and also for treatment with aspirin, statins, ADP receptor inhibitors, β-blockers, ACE inhibitors, angiotensin II receptor blockers, and calcium channel blockers. Since we were using a modified Poisson regression, adjusting for death as a competing risk was not relevant. We conducted a log-rank test for trend for each endpoint, stratified by CAD extent. We performed complete case analyses in the multivariable regression analyses. In these analyses, we only had missing values for smoking (11%). We also conducted a subgroup analysis for elective patients (N=7,664). Statistical analyses were conducted using Stata/IC software version 13.1 (Statacorp LP, College Station, Texas, USA).
Results
A total of 12,594 diabetes patients underwent CAG during the study period. Among these patients, 3,147 (25.0%) had 0-VD, 1,195 (9.5%) had diffuse VD, 3,001 (23.8%) had 1-VD, 2,220 (17.6%) had 2-VD, and 3,031 (24.1%) had 3-VD (Figure 1). Median follow-up-time was 3.0 years (Q1-Q3: 1.1–5.0 years), for a total of 45,164 person-years. None were lost to follow-up.
Baseline characteristics
Diabetes patients with obstructive CAD (1-3 VD) were more often male, older, active smokers, and with reimbursed prescriptions for aspirin, statins, β-blockers, calcium channel blockers, ACE-inhibitors, and ADP receptor inhibitors than patients without obstructive CAD (Table 1). Furthermore, patients with obstructive CAD were more likely to undergo acute or subacute CAG.
Table 1.
Baseline characteristics of diabetes patients at the time of coronary angiography, Denmark, 2004–2012
| 0-VD (N=3,147) |
Diffuse VD (N=1,195) | 1-VD (N=3,001) |
2-VD (N=2,220) |
3-VD (N=3,031) |
Total (N=12,594) |
|
|---|---|---|---|---|---|---|
| Follow-up, years | 3.0 (1.1–5.0) | 2.1 (1.0–4.0) | 3.0 (1.1–5.1) | 3.0 (1.1–5.1) | 3.0 (1.1–4.0) | 3.0 (1.1–5.0) |
| Age, years | 61 (53–69) | 65 (59–73) | 65 (59–73) | 67 (61–75) | 68 (62–75) | 65 (59–73) |
| Male sex, % | 51.0 | 64.1 | 68.1 | 72.1 | 75.1 | 66.0 |
| Current smoking, % | 23.0 | 24.1 | 30.0 | 28.0 | 25.1 | 26.1 |
| Hypertension, % | 79.0 | 86.0 | 80.0 | 81.1 | 83.1 | 81.1 |
| MI <30 days after CAG, % | 1.1 | 3.0 | 23.0 | 20.1 | 18.1 | 14.0 |
| Medical treatment | ||||||
| Aspirin, % | 65.0 | 76.0 | 83.1 | 85.1 | 87.1 | 79.1 |
| Statins, % | 73.1 | 85.0 | 88.0 | 89.1 | 89.0 | 84.1 |
| ADP-inhibitors, % | 4.0 | 7.1 | 44.1 | 41.1 | 31.1 | 27.0 |
| blockers, % | 56.1 | 64.0 | 74.1 | 78.1 | 80.0 | 71.0 |
| ACE-inhibitors, % | 47.1 | 53.0 | 54.1 | 57.1 | 60.0 | 54.1 |
| Calcium channel blockers, % | 35.1 | 42.1 | 37.0 | 42.0 | 46.0 | 40.0 |
| ARBs, % | 30.0 | 34.0 | 28.1 | 26.1 | 28.0 | 29.0 |
| Modified Charlson Comorbidity Index score | ||||||
| 0, % | 59.0 | 51.0 | 58.1 | 54.1 | 51.1 | 55.1 |
| 1, % | 24.1 | 25.1 | 22.0 | 24.1 | 26.1 | 24.1 |
| 2, % | 10.1 | 14.1 | 11.1 | 12.1 | 13.0 | 12.0 |
| ≥3, % | 5.1 | 8.0 | 7.1 | 7.0 | 8.1 | 7.0 |
| Procedural indication | ||||||
| STEMI, % | 2.1 | 1.0 | 17.1 | 14.1 | 11.0 | 10.0 |
| NSTEMI, % | 7.0 | 10.1 | 19.0 | 24.0 | 28.1 | 18.1 |
| Unstable AP, % | 2.0 | 2.0 | 1.1 | 2.0 | 1.0 | 1.1 |
| Stable AP, % | 50.1 | 55.1 | 42.1 | 44.0 | 43.0 | 46.0 |
| Arrhythmia, % | 2.1 | 2.0 | 2.0 | 1.1 | 2.0 | 2.0 |
| Valve disease, % | 9.1 | 7.1 | 7.0 | 5.1 | 3.1 | 6.1 |
| Cardiomyopathy, % | 9.1 | 7.1 | 4.1 | 4.0 | 6.1 | 6.1 |
| Unspecified chest pain, % | 5.1 | 5.1 | 1.1 | 0.1 | 0.1 | 2.1 |
| Other, % | 9.0 | 6.1 | 3.1 | 3.0 | 2.0 | 4.1 |
| Procedural priority | ||||||
| Acute/subacute, % | 23.0 | 24.0 | 45.1 | 47.1 | 48.1 | 39.0 |
| Elective, % | 76.1 | 75.1 | 54.0 | 52.0 | 51.0 | 60.1 |
Notes: Data are presented as median (Q1–Q3), mean (Q1–Q3), or %.
Abbreviations: VD, vessel disease; MI, myocardial infarction; CAG, coronary angiography; ADP, adenosine diphosphate; ACE, angiotensin-converting enzyme; ARB, angiotensin-II receptor blocker; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; AP, angina pectoris.
Clinical endpoints
During the follow-up period, 949 patients had an MI and 2,443 patients died. Numbers of events stratified by extent of CAD are summarized in Table 2. Cumulative 5-year incidence proportion curves for MI, death, and MACE are displayed in Figure 2.
Table 2.
Number of events and rates of myocardial infarction, death and major adverse cardiovascular events in patients with diabetes, by extent of coronary artery disease
| Events (N) |
Rate per 100 person-years(95%CI) | Unadjusted IRR (95%CI) |
Adjusted IRRa (95%CI) |
|
|---|---|---|---|---|
| Myocardial infarction | ||||
| 0-VD | 41 | 0.4 (0.3–0.5) | 1 | 1 |
| Diffuse VD | 46 | 1.4 (1.0–1.8) | 3.80 (2.50–5.79) | 3.87 (2.41–6.23) |
| 1-VD | 203 | 1.9 (1.7–2.2) | 5.36 (3.83–7.49) | 4.99 (3.33–7.46) |
| 2-VD | 213 | 2.7 (2.4–3.1) | 7.56 (5.41–10.57) | 7.14 (4.78–10.65) |
| 3-VD | 446 | 4.3 (4.0–4.8) | 12.07 (8.76–16.63) | 11.42 (7.76–16.82) |
| All-cause death | ||||
| 0-VD | 359 | 3.1 (2.8–3.5) | 1 | 1 |
| Diffuse VD | 172 | 5.0 (4.3–5.8) | 1.61 (1.34–1.93) | 1.35 (1.11–1.66) |
| 1-VD | 507 | 4.6 (4.3–5.1) | 1.48 (1.29–1.70) | 1.31 (1.12–1.54) |
| 2-VD | 506 | 6.1 (5.6–6.7) | 1.96 (1.71–2.25) | 1.69 (1.45–1.98) |
| 3-VD | 899 | 8.1 (7.6–8.6) | 2.58 (2.29–2.92) | 2.01 (1.73–2.33) |
| MACE | ||||
| 0-VD | 141 | 1.7 (1.4–2.0) | 1 | 1 |
| Diffuse VD | 79 | 3.5 (2.8–4.3) | 2.06 (1.56–2.71) | 1.62 (1.20–2.17) |
| 1-VD | 316 | 4.0 (3.6–4.4) | 2.37 (1.94–2.90) | 1.98 (1.58–2.47) |
| 2-VD | 344 | 5.7 (5.2–6.4) | 3.43 (2.81–4.18) | 2.87 (2.31–3.58) |
| 3-VD | 697 | 8.7 (8.1–9.4) | 5.21 (4.34–6.25) | 3.96 (3.21–4.87) |
Notes: aAdjusted for age, sex, modified Charlson Comorbidity Index score, hypertension, smoking status, and for treatment with aspirin, statins, adenosine diphosphate receptor inhibitors, β-blockers, ACE-inhibitors, angiotensin-II receptor blockers, and calcium channel blockers, using patients with 0-VD as reference.
Abbreviations: VD, vessel disease; IRR; incidence rate ratio; MACE, major adverse cardiovascular events.
Figure 2.

Cumulative incidences of myocardial infarction (A), all-cause death (B), and MACE (C) in diabetes patients with 0-vessel disease, diffuse VD, 1-VD, 2-VD, and 3-VD. The follow-up period represents the seventy-fifth percentile.
Abbreviations: VD, vessel disease; MACE, major adverse cardiovascular events.
We observed an incremental increase in the MI event rate per 100 person-years by extent of CAD (Table 2). Patients with 0-VD (0.4 MI per 100 person-years) had the lowest risk and patients with 3-VD (4.3 MI per 100 person-years) had the highest risk. Using patients with 0-VD as reference, the risk of MI increased by number of diseased vessels (Table 2; ptrend<0.001).
For all-cause death, event rates also increased according to the number of diseased vessels (Table 2). Patients with 0-VD had the lowest risk (3.1 deaths per 100 person-years) and patients with 3-VD the highest risk (8.1 deaths per 100 person-years). Using patients with 0-VD as reference, the risk of death increased by number of diseased vessels (Table 2; ptrend<0.001).
For MACE, we similarly observed increasing event rates by extent of CAD (Table 2). Patients with 0-VD had the lowest risk (1.7 deaths per 100 person-years) and patients with 3-VD the highest risk (8.7 deaths per 100 person-years). Using patients with 0-VD as reference, the risk of MACE increased by number of diseased vessels (Table 2; ptrend<0.001).
For both MI, death, and MACE, the curves, and thus the risk, for different extents of CAD continued to diverge, rather than stabilize, over at least a 5-year period (Figure 2).
Subgroup analysis of patients undergoing elective CAG, yielded similar results of both MI and death (Table 3).
Table 3.
Number of events and rates of myocardial infarction and death in elective patients with diabetes, by extent of coronary artery disease
| Events (N) |
Rate per 100 person-years(95%CI) | Unadjusted IRR (95%CI) |
Adjusted IRRa (95%CI) |
|
|---|---|---|---|---|
| Myocardial infarction | ||||
| 0-VD | 27 | 0.3 (0.2–0.5) | 1 | 1 |
| Diffuse VD | 22 | 0.9 (0.6–1.3) | 2.79 (1.59–4.89) | 2.58 (1.41–4.73) |
| 1-VD | 79 | 1.4 (1.1–1.7) | 4.56 (2.95–7.06) | 4.11 (2.51–6.72) |
| 2-VD | 87 | 2.1 (1.7–2.5) | 6.72 (4.37–10.35) | 6.53 (4.04–10.56) |
| 3-VD | 185 | 3.3 (2.9–3.8) | 10.77 (7.19–16.12) | 10.04 (6.35–15.88) |
| All-cause death | ||||
| 0-VD | 250 | 2.8 (2.5–3.2) | 1 | 1 |
| Diffuse VD | 99 | 3.8 (3.1–4.6) | 1.35 (1.07–1.70) | 1.20 (0.94–1.55) |
| 1-VD | 248 | 4.3 (3.8–4.8) | 1.51 (1.27–1.80) | 1.32 (1.08–1.62) |
| 2-VD | 216 | 4.9 (4.3–5.6) | 1.74 (1.45–2.08) | 1.56 (1.27–1.92) |
| 3-VD | 379 | 6.4 (5.8–7.1) | 2.26 (1.93–2.65) | 1.87 (1.54–2.27) |
| MACE | ||||
| 0-VD | 97 | 1.5 (1.2–1.8) | 1 | 1 |
| Diffuse VD | 44 | 2.5 (1.8–3.3) | 1.72 (1.20–2.46) | 1.44 (1.00–2.08) |
| 1-VD | 144 | 3.3 (2.8–3.9) | 2.29 (1.77–2.97) | 1.88 (1.41–2.52) |
| 2-VD | 150 | 4.5 (3.9–5.4) | 3.18 (2.46–4.11) | 2.74 (2.07–3.64) |
| 3-VD | 298 | 6.7 (6.0–7.5) | 4.64 (3.68–5.85) | 3.69 (2.83–4.80) |
Notes: aAdjusted for age, sex, modified Charlson Comorbidity Index score, hypertension, smoking status, and for treatment with aspirin, statins, adenosine diphosphate receptor inhibitors, β-blockers, ACE-inhibitors, angiotensin-II receptor blockers, and calcium channel blockers, using patients with 0-VD as reference.
Abbreviations: VD, vessel disease; IRR, incidence rate ratio; MACE, major adverse cardiovascular events.
Discussion
The present study’s primary finding is that the extent of CAD ascertained by CAG in diabetes patients was associated with an increased rate of MI, all-cause death, and MACE in our cohort with a median of 3.0 years and a seventy-fifth percentile of 5.0 years follow-up.
The current study expands a previous report based on the same patient cohort.4 The earlier report showed that (i) diabetes patients without CAD have a similar risk of MI as non-diabetes patients without CAD, and (ii) diabetes patients with CAD have a higher risk of MI than non-diabetes patients with CAD. In the current analysis, we extend these results by showing that it is not only the presence but also the extent of CAD that defines the risk of MI and death among diabetes patients. Furthermore, we show that the differences in risk continue to increase, rather than stabilize, over at least a 5-year period. It is important to note that our study included diabetes patients undergoing CAG for a clinical indication. Therefore, our conclusions are not necessarily applicable for asymptomatic patients with diabetes.
A cohort study of US veterans undergoing elective coronary angiography for CAD, also found that increasing extent of CAD was associated with a progressively greater risk of MI and all-cause mortality, both in a mixed cohort (N=37,674) and in a diabetes subgroup (N=15,699).1 The study differed from ours in several important aspects. First, US veterans are not representative of a general CAG cohort, being 90% male, 39% obese, and 26% having posttraumatic stress disorder. At the same time, our study population does not represent ethnic subgroups, since the Danish population is primarily Caucasian. Second, follow-up was limited to 1 year in the US veteran cohort, compared to a median of 3 years and a seventy-fifth percentile of 5 years in our study. Third, the US veterans study included only elective patients, while our cohort consisted of consecutive patients, among whom a high proportion had an acute coronary syndrome. Fourth, it should be noted that the two studies used different definitions of vascular disease. In the study of US veterans, nonobstructive VD was defined as ≥1 stenosis ≥20% but <70% and obstructive VD was defined as any stenosis ≥70% or left main stenosis ≥50%.1 Despite these differences, our study—including our subgroup analysis for elective patients only—and the US veterans study had consistent results, with both finding an incremental risk of adverse cardiac events with increasing extent of CAD.
The CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry followed 1,823 diabetes patients for 5 years, using coronary computed tomography angiography (CCTA).2 Similar to the current study, mortality increased with the extent of CAD in the CONFIRM diabetes cohort. However, the CONFIRM diabetes analysis did not examine MI as an individual endpoint. Instead, MACE (defined as death, MI, unstable angina, or late coronary revascularization) was examined in a subgroup of diabetes patients (N=973) and showed a similar incremental association between CAD extent and MACE occurrence. The CONFIRM diabetes cohort enrolled elective patients, unlike our study, which enrolled all-comers including a high proportion of patients with acute coronary syndromes.
Out study extends previous 1-year CAG data out to 5 years and also represents consecutively enrolled patients, many exhibiting acute coronary syndromes, rather than elective patients. Further, we find comparable results in comparison to an elective CCTA cohort. The fact that these studies, despite being performed in different countries, in elective and all-comer cohorts, and using different imaging modalities, strengthen the conclusions and the external validity.
The CAG and CCTA studies described above provide a rationale for performing prospective randomized studies to test individualized primary prophylactic strategies. Only a single randomized clinical trial has examined targeted patient care guided by CCTA vs optimal patient care in asymptomatic diabetes patients.15 The trial did not find screening of CAD beneficial as screening did not reduce the composite rate of all-cause mortality, nonfatal MI, or unstable angina requiring hospitalization at 4 years. However, the trial predominantly included low-risk diabetes patients with normal or nonobstructive CAD, which nearly eliminated the probability of detecting differences in outcomes. Rather than randomizing asymptomatic patients to CCTA or not, we suggest that CCTA should be used for risk stratification before randomization. Based on the current results, it seems likely that asymptomatic patients with diabetes and obstructive 2-VD and 3-VD will benefit from intensive prophylactic medical treatments, eg with novel strategies such as sodium-glucose cotransporter-2 (SGLT-2) inhibitors,16 glucagon-like peptide-1 (GLP-1) analogues,17,18 PCSK9 inhibitors,19 and the monoclonal antibody canakinumab targeting interleukin-1β.20 However, this has to be tested in prospective randomized clinical trials.
The ASCEND (A Study of Cardiovascular Events in Diabetes) study21 recently examined whether aspirin should be used as primary prophylactic treatment in diabetes patients. It showed that the benefits of aspirin with prevention of serious vascular events (12% reduced relative risk) were largely counterbalanced by a high occurrence of major bleeding events (29% higher relative risk), when used for primary prevention in diabetes patients. This questions the use of aspirin as primary prophylaxis in patients with asymptomatic CAD.21 In our study, diabetes patients with 0-VD exhibited a low cardiovascular risk and it may be considered to discontinue treatment with aspirin in these patients. As our results confirm, the 0-VD patients have a very low risk of MI, so they will only have the risk of bleeding complications with aspirin treatment.
As our study relied on registry data, we cannot exclude the possibility of the impact of unmeasured confounding. Another limitation is that we could not differentiate between type of diabetes. As well, we could not establish the duration of diabetes, which is associated with higher extent of CAD and higher risk of major adverse cardiovascular and cerebrovascular events.22–24 The inclusion period lasted from 2004 to 2012. In this period, acute care of acute coronary syndromes was substantially improved by pre-hospital triage based on in-ambulance ECG leading to bypassing of referral hospitals and direct transfer to tertiary hospitals with invasive facilities, and by the introduction of drug-eluting stents. CAG has some important limitations to address. First, CAG does not describe lesion morphology and plaque vulnerability in the vessel wall. Second, it is an invasive procedure, which limits its use as a screening modality. Third, as classification of CAD is based on visual angiographic assessment by the treating physician during CAG, we cannot exclude a minor degree of interobserver variation. Fourth, we stratified CAD according to the number of coronary arteries with obstructive CAD. This is a simplification of a spectrum of CAD and the results must be interpreted in this context. With the current classification we were nevertheless able to identify diabetes patients at low, intermediate, and high risk. We were unable to further stratify patients according to the number of coronary segments/arteries with nonobstructive CAD since only significant lesions are registered in the WDHR. Moreover, we cannot determine which patients received revascularization therapy, which can affect their prognosis. Finally, our study was limited to a seventy-fifth percentile of 5.0 years follow-up and interpretation of our data should be restricted to this period.
Conclusion
Increasing extent of obstructive CAD in diabetes patients was associated with an incremental rate of MI, death, and MACE for at least 5 years. Thus, assessment of CAD extent can assist in identifying diabetes patients at high risk of cardiovascular events, who may benefit the most from primary prophylactic measures.
Data availability
According to the Danish law on personal data, we are not allowed to make the dataset publicly available.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Kevin Kris Warnakula Olesen reports personal fees from Bayer, outside the submitted work. Mr Madsen did not report receiving fees, honoraria, grants or consultancies; the Department of Clinical Epidemiology is, however, involved in studies with funding from various companies as research grants to (and administered by) Aarhus University. Dr Michael Maeng report personal fees from Bayer, personal fees from Novo Nordisk, personal fees from Bristol Myers-Squibb, personal fees from Astra, personal fees from Boehringer-Ingelheim, outside the submitted work. The other authors report no conflicts of interest in this work.
Supplementary Materials
References
- 1.Maddox TM, Stanislawski MA, Grunwald GK, et al. Nonobstructive coronary artery disease and risk of myocardial infarction. Jama. 2014;312(17):1754–1763. doi: 10.1001/jama.2014.14681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blanke P, Naoum C, Ahmadi A, et al. Long-term prognostic utility of coronary CT angiography in stable patients with diabetes mellitus. JACC Cardiovascular Imaging. 2016;9(11):1280–1288. doi: 10.1016/j.jcmg.2015.12.027 [DOI] [PubMed] [Google Scholar]
- 3.Saely CH, Aczel S, Marte T, Langer P, Drexel H. Cardiovascular complications in Type 2 diabetes mellitus depend on the coronary angiographic state rather than on the diabetic state. Diabetologia. 2004;47(1):145–146. doi: 10.1007/s00125-003-1274-6 [DOI] [PubMed] [Google Scholar]
- 4.Olesen KKW, Madsen M, Egholm G, et al. Patients with diabetes without significant angiographic coronary artery disease have the same risk of myocardial infarction as patients without diabetes in a real-world population receiving appropriate prophylactic treatment. Diabetes Care. 2017;40(8):1103–1110. doi: 10.2337/dc16-2388 [DOI] [PubMed] [Google Scholar]
- 5.Schmidt M, Maeng M, Madsen M, Sorensen HT, Jensen LO, Jakobsen CJ. The Western Denmark Heart Registry: its influence on cardiovascular patient care. Journal of the American College of Cardiology. 2018;71(11):1259–1272. doi: 10.1016/j.jacc.2017.10.110 [DOI] [PubMed] [Google Scholar]
- 6.Schmidt M, Maeng M, Jakobsen CJ, et al. Existing data sources for clinical epidemiology: the Western Denmark Heart Registry. Clinical Epidemiology. 2010;2:137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clinical Epidemiology. 2015;7:449–490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scandinavian Journal of Public Health. 2011;39(7 Suppl):30–33. doi: 10.1177/1403494811401482 [DOI] [PubMed] [Google Scholar]
- 9.Johannesdottir SA, Horvath-Puho E, Ehrenstein V, Schmidt M, Pedersen L, Sorensen HT. Existing data sources for clinical epidemiology: the Danish National database of reimbursed prescriptions. Clinical Epidemiology. 2012;4:303–313. doi: 10.2147/CLEP.S37587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 11.Egholm G, Madsen M, Thim T, et al. Evaluation of algorithms for registry-based detection of acute myocardial infarction following percutaneous coronary intervention. Clin Epidemiol. 2016;8:415–423. doi: 10.2147/CLEP.S108906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. European Journal of Epidemiology. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 13.Helweg-Larsen K. The Danish register of causes of death. Scandinavian Journal of Public Health. 2011;39:26–29. doi: 10.1177/1403494811399958 [DOI] [PubMed] [Google Scholar]
- 14.Zou G. A modified poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 15.Muhlestein JB, Lappe DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. Jama. 2014;312(21):2234–2243. doi: 10.1001/jama.2014.15825 [DOI] [PubMed] [Google Scholar]
- 16.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. The New England Journal of Medicine. 2015;373(22):2117–2128. doi: 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 17.Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with Type 2 diabetes. The New England Journal of Medicine. 2016;375(19):1834–1844. doi: 10.1056/NEJMoa1607141 [DOI] [PubMed] [Google Scholar]
- 18.Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in Type 2 diabetes. The New England Journal of Medicine. 2016;375(4):311–322. doi: 10.1056/NEJMoa1603827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–1722. doi: 10.1056/NEJMoa1615664 [DOI] [PubMed] [Google Scholar]
- 20.Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–1131. doi: 10.1056/NEJMoa1707914 [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S86–S104. doi: 10.2337/dc18-S009 [DOI] [PubMed] [Google Scholar]
- 22.Kim JJ, Hwang BH, Choi IJ, et al. Impact of diabetes duration on the extent and severity of coronary atheroma burden and long-term clinical outcome in asymptomatic type 2 diabetic patients: evaluation by Coronary CT angiography. European Heart Journal Cardiovascular Imaging. 2015;16(10):1065–1073. doi: 10.1093/ehjci/jev106 [DOI] [PubMed] [Google Scholar]
- 23.Fox CS, Sullivan L, D’Agostino RB Sr., Wilson PW. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart study. Diabetes Care. 2004;27(3):704–708. [DOI] [PubMed] [Google Scholar]
- 24.Wannamethee SG, Shaper AG, Lennon L. Cardiovascular disease incidence and mortality in older men with diabetes and in men with coronary heart disease. Heart (British Cardiac Society). 2004;90(12):1398–1403. doi: 10.1136/hrt.2003.026104 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to the Danish law on personal data, we are not allowed to make the dataset publicly available.