Abstract
Vernet syndrome, often referred to as jugular foramen syndrome, is a rare clinical entity characterised by a set of signs and symptoms caused by dysfunction of IX, X and XI cranial nerves. Although paraganglioma of the head and neck is the most frequent aetiology, it may also be caused by meningioma, VIII cranial nerve schwannoma, pontocerebellar cistern metastases, head and neck trauma, infections and very rarely by cholesteatoma which extends to the petrous apex. The authors describe a case of a patient with a jugulotympanic paraganglioma in which evolution ends up in Vernet syndrome. The patient preferred a ‘wait and scan’ strategy. With the lack of data available to develop an unequivocal algorithm for paraganglioma management, we always consider not only age but also comorbidities, prior treatment and progression of the lesion. Each case has to be addressed individually and treatment should be discussed in detail with every patient.
Keywords: ear, nose and throat/otolaryngology; neurological injury
Background
This clinical case alerts us to a rare syndrome due to a rare disease (jugulotympanic paraganglioma). Despite its slow progression, we have to bear in mind that it may be a potentially life-threatening disease and hence we highlight the importance of long-term follow-up.
Case presentation
The authors describe a case of a 72-year-old woman diagnosed with a left tympanic paraganglioma in the year 2000. At that time, she presented dysphonia due to ipsilateral vocal fold paralysis and pulsatile tinnitus. She denied loss of taste, shoulder weakness or dysphagia. Physical examination presented a red lump with bulging of the tympanic membrane and complete paralysis of the left vocal fold (figures 1 and 2). MRI revealed a large expansive, extraparenchymal lesion centred in the left jugular foramen which widened and infiltrated the temporal bone and extended not only intracranially but also extracranially. It was a heterogeneous lesion, predominantly hypointense in T1 and hyperintense in T2, which turned up clearer with contrast. Linear structures outstandingly hypointense at T1 and T2—corresponding to vascular structures—corroborated the diagnosis of a jugulotympanic tumour.
Figure 1.

Bulging red mass behind tympanic membrane.
Figure 2.

Left vocal fold paralysis.
She was offered surgery but refused and preferred a conservative strategy.
The patient remained stable and 16 years later reported an onset of dysphagia and impairment of the left shoulder elevation and of the rotation of the head to the right side. She also experienced taste loss (of the posterior one-third of the tongue) and an absence of the gag reflex on the left side.
Investigations
The patient did a CT scan that revealed a neoformation centred in the left jugular fossa, invading its borders and infiltrating the adjacent bone. It caused deviation of the jugular bulb (reducing its calibre) and involved the glossopharyngeal, spinal accessory and vagus nerves. The MRI exhibited an increase of the lesion dimensions, mainly its intracranial component (34.2×25×33 mm) distorting the anterior aspect of the left cerebellar hemisphere and the brainstem as well. Furthermore, also diverting the V, VII and VIII cranial nerves in their emerging zones. There were no signs of oedema of the pons or cerebellum or enlargement of the ventricular system (figure 3).
Figure 3.
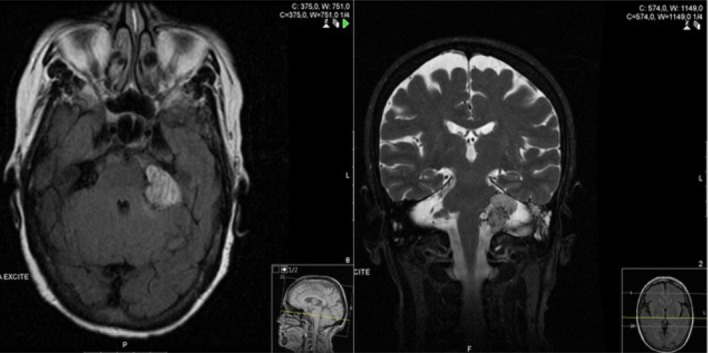
Paraganglioma adjacent to the medial left cerebellar peduncle.
Outcome and follow-up
Then due to a symptomatic growing mass, the therapeutic possibilities (surgery or radiotherapy) were discussed and offered to the patient. She refused both possibilities and preferred active surveillance. Until now, the clinical picture is stable and despite some symptoms referred to by the patient, she considers her life acceptable.
Discussion
Vernet syndrome is characterised by a set of signs and symptoms triggered by the involvement of the cranial nerves IX, X, XI.1
The jugular foramen is located posteriorly to the carotid canal, being formed anteriorly by the petrous portion of the temporal bone and posteriorly by the occipital bone.2
The following signs and symptoms can be present: dysphonia (either persistent or positional) with vocal fold paralysis, soft palate asymmetry, dysphagia, loss of taste in the posterior portion of the tongue, decreased secretions of the parotid gland, loss of choking reflex and sternocleidomastoid and trapezius weakness.3 4 Vernet Syndrome, many times referred to as Jugular Foramen Syndrome, was first described by Vernet in 1917.5
The most common symptoms are hoarseness and dysphagia and in fact, they were present in our patient. Although pain is also common our patient did not have any symptom. Collet Sicard is another skull base syndrome, which though having the same features as Vernet syndrome, it is also characterised by hypoglossal nerve dysfunction with consequent unilateral paralysis and tongue atrophy.1 6
The cranial nerves descending in the jugular foramen are glossopharyngeal (IX), vagus (X) and spinal accessory (XI) nerves. The compression of these cranial nerves caused the following signs/symptoms: dysphagia, left vocal fold paralysis and an impairment of the elevation of the left shoulder and of the rotation of the head to the right side.
Although paraganglioma of the head and neck is by far the most frequent aetiology, it may also be caused by meningioma, schwannoma of the VIII cranial nerve, metastases in the pontocerebellar cistern, head and neck trauma, infections (some rare infections caused by varicella zoster virus), cholesteatoma extending to the petrous apex or jugular vein thrombosis.2 7 8
Paragangliomas are hypervascular neoformations originating from cells of the paraganglionic system. They usually present a benign behaviour with a slow-growing pattern.9 Only 3% of extra-adrenal cases correspond to the head and neck region.10
Of all paragangliomas of the head and neck, the most frequent are carotid, followed by the jugulotympanic and vagal. Jugular foramen paragangliomas are indeed a truly therapeutic challenge due to the noble locations, namely in the lateral skull base and intracranial region, which make it difficult to control the tumour with low morbidity. The clinical picture is generally related to the dysfunction of the cranial nerves involved by the neoformation. Therefore, they may present a variety of symptoms, including dysfunction of VII (facial paralysis), VIII (tinnitus, hearing loss), X (dysphonia) and XI (shoulder weakness pain) cranial nerves.9 When they cause IX, X, XI cranial nerve dysfunction, they are responsible for the Vernet syndrome. Head and neck paragangliomas usually present a substantial gap time (30.5 months) between the onset of symptoms and the diagnosis, because of its low growth rate (0.8 mm/year).11
Fisch modified classification is frequently used to lead us to a more accurate approach. The classification Fisch A corresponds to a tumour which is limited to the middle ear; classification B corresponds to a tumour limited to the tympanomastoid segment of temporal bone; classification C corresponds to a tumour involving the infralabyrinthine compartments and classification D corresponds to the intracranial extension.12 13
Surgery has been the traditional approach to this pathology. Once the main goal of treatment is the total tumour eradication with minimal damage, the surgical approach for Fisch A and B tumours is a good option as surgery can thus be achieved with low complication rates.14 On the contrary, for patients with Fisch C and D lesions, surgery is associated with high morbidity. This way other forms of management are being increasingly considered as they actually offer an alternative: observation (‘wait and scan’ approach), radiotherapy or a combination of surgical debulking and further radiation. Certain factors must be take into consideration when choosing a particular approach, namely patient’s age, comorbidities, hearing status, cranial nerves function and tumour size should be taken into account for surgery.9 Thus, young age, secreting tumours, significant intracranial mass effect, progression after radiation, facial paralysis, malignant transformation and low risk of cranial nerve injury.9
In this case study, the 72-year-old patient had a growing type D Fisch lesion without facial paralysis and signs of cerebral trunk compression. Therefore, surgical risk and morbidity were high. In fact, at this moment, the ‘wait and scan’ approach seems to be a sustainable strategy option. As there isn’t an ideal approach, all the possibilities with corresponding risks and benefits have to be discussed with the patient.
Learning points.
We describe a case of a rare syndrome due to a rare disease which can be life threatening.
With the lack of available data to develop an algorithm for its management, we consider not only age but also the presence of comorbidities, prior treatments and the lesion progression rate.
The tumour localisation (based on clinical signs and symptoms) is important to determine further investigation and the best management.
Each case has to be addressed individually, and treatment options discussed in detail with every patient.
Footnotes
Contributors: FM, PO, JP and AC: participated in an active way on management of clinical case and contributed equally to manuscript writing and revision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Ammar H, Fouda R. An unusual cause of hoarseness. Case Rep Child Meml Hosp Chic 2012;2012:bcr0220125761 10.1136/bcr.02.2012.5761 [DOI] [Google Scholar]
- 2. Caldemeyer KS, Mathews VP, Azzarelli B, et al. The jugular foramen: a review of anatomy, masses, and imaging characteristics. Radiographics 1997;17:1123–39. 10.1148/radiographics.17.5.9308106 [DOI] [PubMed] [Google Scholar]
- 3. Robbins KT, Fenton RS. Jugular foramen syndrome. J Otolaryngol 1980;9:505–16. [PubMed] [Google Scholar]
- 4. Jaiswal M, Bhaskar MK, Mittal RS, et al. Positional hoarseness: an unusual symptom in jugular foramen mass. BMJ Case Rep 2016;2016:bcr2016215805 10.1136/bcr-2016-215805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. V M. Paralysies laryngees associees. Paris Medical 1917:152–70. [Google Scholar]
- 6. Wilson H, Johnson DH. Jugular foramen syndrome as a complication of metastatic cancer of the prostate. South Med J 1984;77:92–3. 10.1097/00007611-198401000-00029 [DOI] [PubMed] [Google Scholar]
- 7. Lee M, Heo Y, Kim T. Vernet’s Syndrome Associated with Internal Jugular Vein Thrombosis. J Stroke Cerebrovasc Dis 2019;28:344–6. 10.1016/j.jstrokecerebrovasdis.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 8. Ferreira J, Franco A, Teodoro T, et al. Vernet syndrome resulting from varicella zoster virus infection-a very rare clinical presentation of a common viral infection. J Neurovirol 2018;24:379–81. 10.1007/s13365-018-0622-8 [DOI] [PubMed] [Google Scholar]
- 9. Moore MG, Netterville JL, Mendenhall WM, et al. Head and Neck Paragangliomas: An Update on Evaluation and Management. Otolaryngol Head Neck Surg 2016;154:597–605. 10.1177/0194599815627667 [DOI] [PubMed] [Google Scholar]
- 10. Wasserman PG, Savargaonkar P. Paragangliomas: classification, pathology, and differential diagnosis. Otolaryngol Clin North Am 2001;34:845–62. [DOI] [PubMed] [Google Scholar]
- 11. Carlson ML, Sweeney AD, Wanna GB, et al. Natural history of glomus jugulare: a review of 16 tumors managed with primary observation. Otolaryngol Head Neck Surg 2015;152:98–105. 10.1177/0194599814555839 [DOI] [PubMed] [Google Scholar]
- 12. Sivalingam S, Konishi M, Shin SH, et al. Surgical management of tympanojugular paragangliomas with intradural extension, with a proposed revision of the Fisch classification. Audiol Neurootol 2012;17:243–55. 10.1159/000338418 [DOI] [PubMed] [Google Scholar]
- 13. Shin SH, Sivalingam S, De Donato G, et al. Vertebral artery involvement by tympanojugular paragangliomas: management and outcomes with a proposed addition to the fisch classification. Audiol Neurootol 2012;17:92–104. 10.1159/000330724 [DOI] [PubMed] [Google Scholar]
- 14. Prasad SC, Mimoune HA, D’Orazio F, et al. The role of wait-and-scan and the efficacy of radiotherapy in the treatment of temporal bone paragangliomas. Otol Neurotol 2014;35:922–31. 10.1097/MAO.0000000000000386 [DOI] [PubMed] [Google Scholar]


