Abstract
Background:
The United States Department of Agriculture’s Supplemental Nutrition Assistance Program (SNAP) is the country’s largest nutrition assistance program for low-income populations. While SNAP has been shown to reduce food insecurity, research on the diet quality of program participants is inconsistent.
Objective:
This study examined if the community food environment is a potential moderator of the association between SNAP participation and eating behaviors.
Design:
This cross-sectional study utilized participant data from a telephone survey of 2,211 households in four cities in New Jersey. Data were collected from two cross-sectional panels from 2009–10 and 2014. Food outlet data were purchased from commercial sources and classified as supermarkets, small grocery stores, convenience stores, or limited service restaurants.
Participants/setting:
Analysis is limited to 983 respondents (588 SNAP participants) with household incomes below 130% of the Federal Poverty Level.
Main outcome measures:
Eating behaviors assessed as frequency of consum ption of fruit, vegetables, salad, and sugar sweetened beverages (SSB).
Statistical analysis performed:
Interaction and stratified analyses using gamma regression determined the differences in the association between SNAP participation and eating behaviors by the presence or absence of food outlets adjusted for covariates.
Results:
SNAP participation was associated with a higher frequency of consuming SSB (p<0.05) when respondents lived within ¼ –½ mile of a small grocery store, supermarket, and limited service restaurant. SNAP participants who did not live close to a convenience store reported a lower frequency of SSB consumption (p=0.01), while those living more than ½ mile away from a supermarket reported a lower frequency of fruit consumption (p=0.03).
Conclusions:
This study suggests that the community food environment may play a role in moderating the association between SNAP participation and eating behaviors. While SNAP participation is associated with some unhealthy behaviors, this association may only hold true when respondents live in certain food environments.
Keywords: Supplemental Nutrition Assistance Program, dietary behaviors, community food environment, moderation
Introduction
Food insecurity remains a public health problem in the United States with an estimated 15.8 million households, or 13% of the population, being food insecure at least some time during the year.1 The Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program, is the country’s largest nutrition assistance program for low-income populations and is considered the first defense against hunger.2
While SNAP reduces food insecurity,3 many studies find that SNAP participation is associated with unhealthy eating behaviors such as lower fruit and vegetable consumption, higher sugar sweetened beverage (SSB) consumption, and poorer overall diet quality, compared to income-eligible non-participants.4–8 However, other studies have found no difference between participants and income-eligible non-participants9,10 and that SNAP participants may consume more fruit than income-eligible non-participants.3 Interestingly, one study found that SNAP participation was associated with a higher diet quality among participants with low food security while SNAP participation was associated with a lower diet quality among participants with full food security, compared to their non-SNAP participating counterparts.11
There are many factors that influence the shopping behaviors of SNAP participants, such as the price, availability, and accessibility of food.7,12 Research suggests that some SNAP participants may pass the nearest food outlet to shop at one with lower prices and better selection.13 SNAP participants with poor access to a supermarket still spent a majority of their SNAP benefits at those food outlets, comparable to participants who lived close to a supermarket.14 However, other research suggests that the community food environment may also influence the eating behaviors of SNAP participants. While people purchase and consume food from a variety of outlets that sometimes extends beyond their local community food environment,13,15–17 other research indicates that proximity to certain food outlets, such as convenience stores, supermarkets, or restaurants can influence what people eat.18,19 Fruit and vegetable consumption is higher among those who live closer to supermarkets20–23 and SSB consumption is higher among those who live near convenience stores.24–26
Research on the role of the community food environment among SNAP participants is more limited than research among the general population. Gustafson et al. examined the eating behaviors of SNAP participants and their food environment and found that participants who lived within ½ mile of a farmer’s market consumed more fruits, vegetables, grains, and milk.27 A similar study examined the association of food outlets with macronutrient intakes among SNAP participants and reported SNAP participants had a higher consumption of calories and fat when living in counties with multiple gas stations with food marts compared to participants without access to multiple gas stations.28 While these studies limited their population to SNAP participants, they did not examine whether these behaviors were different for income-eligible non-participants. SNAP participation increases a household’s food budget, 29,30 and thus SNAP participants may purchase and consume different foods than the low-income, non-participating population.
Given the mixed results of SNAP participation’s association with eating behaviors and lack of studies examining the role of the food environment on SNAP vs. non-SNAP participants, this study examined how the community food environment moderates the relationship between SNAP participation and eating behaviors. There are two hypotheses based on prior literature regarding eating behaviors and the community food environment. First, the association between SNAP participation and frequency of fruit and vegetable consumption will be stronger among those who live closer to healthy food outlets (supermarkets, small grocery stores), compared to those who do not live close to healthy food outlets. Second, the association between SNAP participation and SSB consumption will be stronger among those living closer to unhealthy food outlets (limited service restaurants, convenience stores), compared to those not living near unhealthy food outlets.
Materials & Methods
Respondent Data
Data on respondents were collected as part of the New Jersey Child Healthy Study examining the role of the food and physical activity environment on children’s health. Data were collected from a telephone survey (both landlines and mobile phones) of a random sample of 2,211 households in four urban, high minority (78.5–95.9% non-white), low-income (median household income $26,000 - $40,428)31 cities in New Jersey: Newark, New Brunswick, Trenton, and Camden. Adults were eligible to complete the phone survey if they had at least one child between the ages of 3–18 years, made food shopping decisions for the household, and lived in one of the four study cities. The household survey was administered to two different panels:panel 1 consisted of 1,408 adults in 2009–2010 and panel 2 included 803 adults in 2014. The phone survey included questions on demographics, eating behaviors, physical activity habits, health status, and employment status. The 30 minute survey was administered in either English or Spanish. Informed consent was obtained at the beginning of the phone survey. The Rutgers and Arizona State University Institutional Review Boards approved the study protocol.
Study Sample
Analysis was limited to respondents with household incomes below 130% of the Federal Poverty Level (FPL) who were not missing any data on outcome or explanatory variables. Respondents with household incomes above 130% of the FPL (n=1,161) were dropped as these respondents would not be eligible to participate in SNAP based on household income.32 There were 67 respondents who had missing data on one or more variables and were dropped from the sample, leaving an analytical sample of 983 respondents.
Outcome Variables
Five eating behaviors were chosen for this study based on their association with health outcomes and as indicators of overall diet quality: frequency of consumption of fruit, vegetables, salad, fruit drinks, and regular soda. Fruit drinks and regular soda were combined into a total SSB variable, and were also analyzed separately due to their independent associations with the food environment and sub-populations in the sample.33,34 Participants could report food and beverage consumption frequency by day, week, or month. Frequency of fruit consumption was obtained by the question, “Not counting juice, how often did you eat fruit? Count fresh, frozen, or canned fruit.” Total vegetable consumption was a composite of four questions asking participants to report on frequency of consumption of lettuce/salad, potato, beans, and other vegetables. Salad was also analyzed separately from total vegetable consumption. SSB consumptions was determined by two questions, “How often did you drink fruit flavored drinks such as lemonade, Sunny Delight, Kool-Aid, Gatorade, or sweet iced teas? Do not include 100% fruit juice,” and “How often did you drink regular carbonated soda or soft drinks such as coke, Pepsi, or 7-up? Do not include diet drinks.” These questions were adapted from the Behavior Risk Factor Surveillance Survey and 2009–10 National Health and Nutrition Examination Survey.35,36 Consumption frequency was calculated as number of times per day.
Explanatory Variables
Respondent demographic information was collected via the phone survey, which included age, sex, race/ethnicity, education, income, height, and weight. Race/ethnicity was categorized as, “Non-Hispanic White,” “Non-Hispanic Black,” “Hispanic,” and “Other.” Other included American Indian/Native American/Aleutian or Eskimo, Asian/Pacific Islander, or self-reported other than races listed. Education was categorized into, “less than high school,” “high school or equivalent,” “some college,” or “college graduate.” Income was calculated as a percentage of the FPL and accounted for household size according to the year of data collection.
SNAP participation was determined by the question, “Did anyone in your family living there receive food stamps in 2008/2013?” Participation in Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) was determined by the question, “Did anyone in your family living there receive WIC in 2008/2013?” Respondents who replied with “don’t know” or refused to answer either the SNAP or WIC q uestion were marked as missing and dropped from analysis.
Food outlets were classified based on a previously published protocol.37 Databases of food outlets were purchased from InfoUSA38 and Nielsen39 in 2008, to align with panel 1, and 2014, to align with panel 2. Outlets were classified into six categories of retail outlets based on the food sold in stores, sales volume, and the North American Industry Classification System (NAICS) code.40 Restaurants were classified based on the type of food served and if food was served before or after customers paid the bill. The six retail outlets included supermarkets, small grocery stores, convenience stores, fruit and vegetable markets, meat markets, and meat market with small grocery stores. Restaurants could be classified as either limited service restaurants (LSR) or full service restaurants. For this study, small grocery stores, fruit and vegetable markets, and meat market with small grocery were combined into one variable called small grocery. Only the following four outlets were used in analysis: supermarkets, small grocery, convenience stores, and LSR.
The street network distances between food outlets and respondent’s homes were determined by geographic information system (GIS) mapping using Esri ArcMap with Network Analyst (version 10.3.1). Each year, a custom road/path network was built to include informal pedestrian pathways and exclude highways and on/off ramps. In the four cities in this study, there were more LSR and convenience stores near respondent’s homes and fewer small grocery stores and supermarkets. A ¼ mile radius was used for LSR and convenience stores, as 97% of households had an LSR and 99% had a convenience store within ½ mile consistent with the highly urban setting of the four study cities. A ½ mile radius was used for small grocery stores and supermarkets, as only 8% of households had a supermarket and 16% had a small grocery within ¼ mile.
Statistical Analysis
To assess differences in demographic characteristics and eating behaviors by SNAP participation, t-tests were used for continuous variables and chi-squared for categorical variables.
Multivariable analysis:
Model fit testing based on examination of Akaike’s information criterion (AIC) revealed that gamma regression with a logarithmic link function had the best fit. To interpret the regression coefficients obtained under a logarithmic link function, the antilogarithms of the estimated regression coefficients were computed.41 In gamma regression, the antilogarithm of the regression coefficient, eb, represents the proportional differences in the outcome associated with a 1-unit increase in the independent variable. For this study, eb can be interpreted as the proportional difference in frequency of food and beverage consumption associated with participating in SNAP, compared to frequency of food and beverage consumption among income-eligible adults who do not participate in SNAP. For example, an eb value of 1.50 for a food item would mean a 50% higher frequency of consumption of that food for individuals who participate in SNAP compared to those who do not participate in SNAP. Multivariable models were built based on significant bivariate associations of p<0.10, except for age, sex, race, city of residence, and panel, which were included in all models.
Interaction and stratified analysis:
To test for interaction, an interaction term (SNAP participation*presence of food outlet) was included in the multivariable model and then separate, stratified analysis was used to determine the differences in associations between SNAP participation and eating behaviors by presence or absence of food outlets. Preliminary analysis revealed no differences in results when using presence/absence or count of food outlets within a pre-defined radius, so presence/absence was used to be consistent with previous research using these data.42 Two multivariable models were run: one with the subgroup of respondents who had the specific food outlet present within the defined radius and the second with the subgroup who did not have the specific food outlet present within the defined radius.
Sensitivity analysis was conducted which extended the income to 200% of the FPL and there were no significant differences in outcomes. Further sensitivity analysis revealed no differences in demographic variables or outcomes when participants with missing variables were included in the models (data not shown). All analyses were conducted in Stata (version 13.1).43 Individual associations were considered significant at p<0.05. Interactions were considered significant at p<0.10. All confidence intervals (CI) were two-sided and set at 95%.
Results
Of the 983 respondents whose annual household incomes fell under 130% of the FPL, 60% participated in SNAP, 49% were between the ages of 35–54 years, 86% were female, 52% were non-Hispanic black, and 49% had a high school degree or equivalent (Table 1). There were statistically significant differences between participants and nonparticipants in SNAP by age, sex, race/ethnicity, poverty status, and WIC participation. Of respondents’ ages 18–34 years, 66% participated in SNAP compared to only 49% of respondents ages ≥55 years. Female respondents reported a higher rate of SNAP participation (62%) compared to males (47%). Non-Hispanic whites (60%) and non-Hispanic blacks (65%) had a higher percentage of SNAP participation compared to Hispanics (53%). Lastly, respondents with data collected in 2014 had a higher rate of SNAP participation at 72% compared to only 51% of respondents with data collected in 2009–10. In unadjusted analysis, SNAP participants had a higher daily frequency of soda (Mean [M]=0.7, p=0.03), sweetened fruit drinks (M=0.8, p=0.002), and total SSB (M=1.5, p=0.001) consumption compared to income-eligible non-participants (M=0.5, 0.6, 1.1, respectively).
Table 1:
Demographic characteristics and self-reported frequency of consumption of selected food and beverage items by participation in SNAP.a Cross-sectional data of SNAP-eligible respondentsb collected from four New Jersey cities in 2009–10 and 2014 (n=983).
| All SNAP- Income Eligible Respondents (n=983) |
Not SNAP Participantc (n=395) |
SNAP Participant (n=588) |
P-value for difference by SNAP participationd |
|
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age | 0.003 | |||
| 18–34 years | 375 (38) | 129 (33) | 246 (42) | |
| 35–54 years | 486 (49) | 204 (52) | 282 (48) | |
| 55+ years | 122 (12) | 62 (16) | 60 (10) | |
| Sex | 0.001 | |||
| Male | 136 (14) | 72 (18) | 64 (11) | |
| Female | 847 (86) | 323 (82) | 524 (89) | |
| Race/ethnicity | 0.004 | |||
| Non-Hispanic white | 40 (4) | 16 (4) | 24 (4) | |
| Non-Hispanic black | 513 (52) | 181 (46) | 332 (56) | |
| Hispanic | 410 (42) | 192 (49) | 218 (37) | |
| Othere | 20 (2) | 6 (2) | 14 (2) | |
| Education | 0.83 | |||
| Less than high school |
285 (29) | 111 (28) | 174 (30) | |
| High school or equivalent |
478 (49) | 199 (50) | 279 (47) | |
| Some college | 183 (19) | 70 (18) | 113 (19) | |
| College Graduate | 37 (4) | 15 (4) | 22 (4) | |
| Poverty status | <0.001 | |||
| ≤50% poverty level | 272 (28) | 73 (18) | 199 (34) | |
| 50–99% poverty level |
479 (49) | 195 (49) | 284 (48) | |
| 100–130% poverty level |
232 (24) | 127 (32) | 105 (18) | |
| WICf Participation | <0.001 | |||
| No | 710 (72) | 311 (79) | 399 (68) | |
| Yes | 273 (28) | 84 (21) | 189 (32) | |
| Food Outlet Environment |
||||
| Small Grocery | 0.18 | |||
| Absence – ½ mile | 590 (60) | 227 (57) | 363 (62) | |
| Presence – ½ mile | 393 (40) | 168 (43) | 225 (38) | |
| Supermarket | 0.08 | |||
| Absence – ½ mile | 647 (66) | 247 (63) | 400 (68) | |
| Presence – ½ mile | 336 (34) | 148 (37) | 188 (32) | |
| Convenience Store | 0.50 | |||
| Absence – ¼ mile | 169 (17) | 64 (16) | 105 (18) | |
| Presence – ¼ mile | 814 (83) | 331 (84) | 483 (82) | |
| Limited Service | 0.23 | |||
| Restaurant | ||||
| Absence – ¼ mile | 310 (32) | 116 (29) | 194 (33) | |
| Presence – ¼ mile | 673 (69) | 279 (71) | 394 (67) | |
| Panel | <0.001 | |||
| 1 (2009–10) | 572 (58) | 279 (71) | 293 (50) | |
| 2 (2014) | 411 (42) | 116 (29) | 295 (50) | |
| City of Residence | <0.001 | |||
| Camden | 331 (34) | 104 (26) | 227 (39) | |
| Newark | 315 (32) | 127 (32) | 188 (32) | |
| New Brunswick | 122 (12) | 72 (18) | 50 (9) | |
| Trenton | 215 (22) | 92 (23) | 123 (21) | |
|
Food and Beverage Items (Daily Consumption Frequency) |
Mean (SD)h | Mean (SD) | Mean (SD) | p-value |
| Fruit – all | 0.9 (1.1) | 0.9 (1) | 0.9 (1.1) | 0.72 |
| Vegetables - all | 2.2 (1.7) | 2.2 (1.8) | 2.2 (1.6) | 0.79 |
| Salad - all | 0.7 (0.9) | 0.7 (0.9) | 0.7 (0.9) | 0.53 |
| Sugar Sweetened Beverages – all |
1.3 (1.8) | 1.1 (1.5) | 1.5 (2) | 0.001 |
| Soda | 0.6 (1.1) | 0.5 (1) | 0.7 (1.2) | 0.03 |
| Fruit Drinks | 0.7 (1.2) | 0.6 (1) | 0.8 (1.3) | 0.002 |
SNAP = Supplemental Nutrition Assistance Program
Incomes under 130% of the Federal Poverty Level
Numbers/percentages for SNAP participation sum by column. Percentages may be over 100% due to rounding.
Chi-squared analysis used to determine p-value of difference among groups for categorical variables and t-tests were used to determine differences among eating behaviors.
Other included American Indian/Native American/Aleutian or Eskimo, Asian/Pacific Islander, or self-reported other than races listed.
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children
SD = Standard deviation
In adjusted, multivariable analysis (Table 2), SNAP participation was significantly associated with a 29% higher frequency of fruit drinks (p=0.02) and 20% higher frequency of total SSB consumption (p=0.04). Presence of convenience stores within ¼ mile was associated with a 20% lower frequency of total SSB consumption (p=0.04) and a 27% lower frequency of fruit drink consumption (p=0.02). Lastly, presence of a LSR within ¼ mile was associated with a 16% higher frequency of vegetable consumption (p=0.01).
Table 2:
Associations of self-reported frequency of consumption of selected food and beverage items with participation in SNAPa (yes/no) and with presence of various food outlets. Cross-sectional data of SNAP-eligible respondentsb collected from four New Jersey cities in 2009–10 and 2014 (n=983).c,d
| Food and beverage items (Daily Consumption Frequency) |
Association with SNAP Participation (vs. not participating) |
Presence of Small Grocery within ½ mile |
Presence of Supermarket within ½ mile |
Presence of Convenience Store within ¼ mile |
Presence of LSRe within ¼ mile |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| proportional difference (eb) (95% CI) f,g |
p- value |
proportional difference (eb) (95% CI) f,g |
p- value |
proportional difference (eb) (95% CI) f,g |
p- value |
proportional difference (eb) (95% CI) f,g |
p- value |
proportional difference (eb) (95% CI) f,g |
p- value |
|
| Fruit – all | 0.88 (0.75, 1.03) |
0.11 | 1.10 (0.94, 1.28) |
0.24 | 1.04 (0.88, 1.22) |
0.64 | 1.02 (0.84, 1.23) |
0.86 | 1.11 (0.95, 1.30) |
0.19 |
| Vegetables – all |
0.96 (0.86, 1.06) |
0.42 | 0.97 (0.87, 1.07) |
0.51 | 0.97 (0.87, 1.09) |
0.65 | 0.96 (0.85, 1.09) |
0.53 | 1.16 (1.04, 1.28) |
0.01 |
| Salad | 0.91 (0.76, 1.08) |
0.29 | 0.98 (0.83, 1.16) |
0.84 | 1.03 (0.85, 1.23) |
0.79 | 1.00 (0.81, 1.24) |
0.98 | 1.17 (0.99, 1.39) |
0.07 |
| Sugar Sweetened Beverages – all |
1.20 (1.01, 1.44) |
0.04 | 0.94 (0.79, 1.11) |
0.48 | 1.01 (0.85, 1.22) |
0.88 | 0.80 (0.65, 0.99) |
0.04 | 1.09 (0.92, 1.31) |
0.32 |
| Soda | 1.04 (0.80, 1.35) |
0.79 | 0.92 (0.73, 1.17) |
0.51 | 0.95 (0.74, 1.23) |
0.72 | 0.92 (0.68, 1.24) |
0.59 | 1.13 (0.88, 1.45) |
0.35 |
| Fruit Drinks |
1.29 (1.04, 1.60) |
0.02 | 0.95 (0.77, 1.18) |
0.66 | 1.05 (0.84, 1.32) |
0.64 | 0.73 (0.57, 0.95) |
0.02 | 1.07 (0.86, 1.33) |
0.56 |
SNAP= Supplemental Nutrition Assistance Program
Incomes below 130% of the Federal Poverty Line
Separate models were run for each food item and each food outlet
Each model used gamma regression and was adjusted for age, sex, race/ethnicity, education, city of residence, panel (year of collection), participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and income
LSR=Limited Service Restaurant
eb = antilogarithm of regression coefficient and represents the proportional difference in frequency of food or beverage consumption with participation in SNAP vs those who do not participate
95% CI=95% Confidence Interval
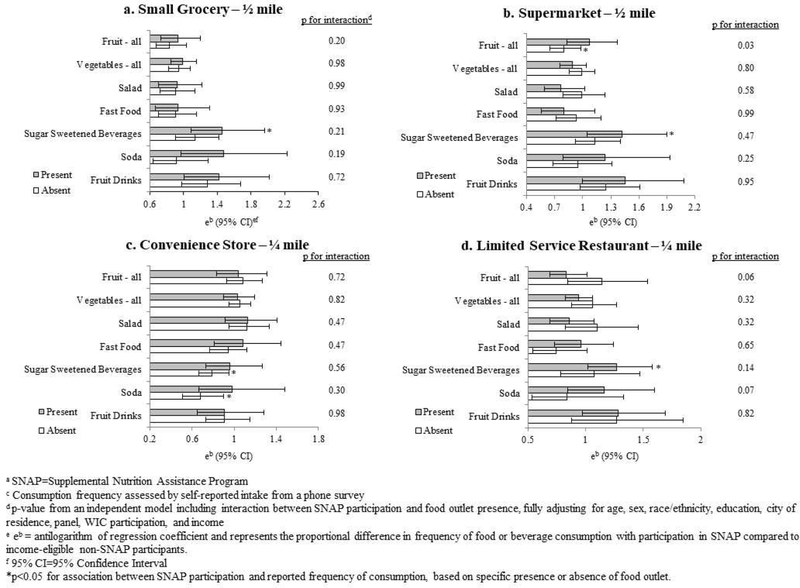
Stratified analyses (Figure 1, complete data found in Tables 3–6 – suggested as supplementary online tables) revealed differences in the association between SNAP participation and eating behaviors, depending on whether specific food outlets were present or absent in the community food environment. Among those living within a ½ mile of a small grocery store, SNAP participation was associated with a 42% higher consumption of fruit drinks (eb=1.42, CI: 10 1.00, 2.02) and 46% higher consumption of total SSB (eb=1.46, CI: 1.09, 1.96), compared to income eligible non-SNAP participants.
Figure 1:
Stratified analysis of the association between SNAPa participation and reported frequency of consumptionc, based on presence or absence of a food outlet, and the significance of the interaction between SNAP participation and food outlet presence from four New Jersey cities 2009–2010 and 2014.
When there was no supermarket within ½ mile, SNAP participation was associated with a 20% lower frequency of fruit consumption (eb=0.80, CI: 0.65, 0.98), compared to income-eligible non-participants. For those who lived within ½ mile of a supermarket, SNAP participation was associated with a 45% higher frequency of fruit drinks (eb=1.45, CI: 1.00, 2.08) and 42% higher frequency of SSB consumption (eb=1.42, CI: 1.05, 1.90), compared to income-eligible non-participants.
Among respondents not living within ¼ mile of a convenience store, SNAPparticipation was associated with a 21% lower frequency of total SSB consumption (eb=0.79, CI: 0.66, 0.95) and 32% lower frequency of soda consumption (eb=0.68, CI: 0.51, 0.90).
Lastly, respondents who lived within ¼ mile of a LSR had a significant association between SNAP participation and a higher frequency of total SSB consumption (eb=1.27, CI:1.02, 1.58), compared to income-eligible non-participants. There was no association between vegetable and salad frequency consumption and SNAP participation irrespective of presence or absence of investigated food outlets.
Discussion
This study examined how the community food environment influences the relationship between SNAP participation and consumption of foods and beverages, and may help clarify the mixed findings of previous studies that examined the association between SNAP participation and eating behaviors. Interaction and stratified analyses revealed that SNAP participation was associated with a higher consumption of SSB when respondents lived close to a small grocery store, supermarket, and LSR. There was a significant association between SNAP participation and lower SSB consumption when respondents did not live close to a convenience store. There was a significant association between SNAP participation and a lower frequency of fruit consumption when respondents did not live near a supermarket.
The published research on SNAP participation and consuming SSB is mixed with some studies finding SSB consumption higher among SNAP participants,6,44 and other studies finding no significant association when compared to income-eligible non-participants.9,10 Based on findings in the current study, this discrepancy could be due to varying community food environments among study participants. While SNAP participation was associated with a 20% higher SSB consumption in the overall sample, this association disappeared when respondents did not live close to food outlets, and only remained when respondents lived close to grocery stores, supermarkets, and LSR—outlets that sell SSB and often at low prices.45 Past research has found that among low-income and SNAP participants, an increase in food spending is associated with an increase in SSB consumption.46 Because SNAP increases the purchasing power for food compared to income-eligible non-participants, and SNAP participants have higher at-home food spending than income-eligible non-participants,29,30,47 an increase in the food budget could lead to higher SSB consumption.
The positive association between food outlets and SSB consumption also aligns with previous research. A study among adolescents found that living within ½ or 1 mile of restaurants, convenience stores, and grocery stores was associated with a higher SSB consumption.25 Gustafson et al. reported that shopping at supermarkets was associated with a higher SSB consumption.48
Many studies have examined the association between fruit and vegetable intake and the community food environment, and the results are generally consistent—those who live near supermarkets, farmer’s markets, or healthy food stores consume more20,21,23,28,49 while those who live near convenience stores and restaurants consume less.17,49,50 These findings align with the current study’s result that SNAP participation was associated with a lower frequency of fruit consumption when respondents did not live near a supermarket. If SNAP participants do not live near supermarkets, which are usually SNAP-authorized retailers and sell fruit at affordable prices, they may be choosing to spend their benefit dollars at SNAP-authorized convenience stores or small grocery stores that are more accessible, but usually sell lower quality produce and at higher prices, and sometimes do not sell any fresh produce.51,52
While evidence exists that the consumer food environment—such as price and accessibility—influences shopping behaviors, 12 a review by Gustafson et al. found that the consumer-level food environment was not associated with dietary behavior.53 It is possible that enacting incentive or restrictive policies could help improve SNAP participant’s diet within a given food environment. To improve the consumption of fruits and vegetables among SNAP participants, a pilot project by the United States Department of Agriculture, the Healthy Incentives Pilot (HIP), provided 30 cents to participants for every SNAP dollar spent on fruits and vegetables. The money was immediately credited to the SNAP participant’s Electronic Benefit Transfer card and could be used to purchase any SNAP-authorized food or beverage. The pilot results revealed that HIP participants consumed more fruits and vegetables than non-participants, spent more SNAP benefit dollars on fruits and vegetables than non-participants, and even spent more total money on fruits and vegetables than non-participants.54 This types of incentive may be effective in improving fruit and vegetable purchases among SNAP participants, even among those who do not live near supermarkets.
Policies aimed at restricting allowable purchases with SNAP benefits have also been discussed as a possible measure to improve the diet of SNAP participants.8,55,56 These policy ideas range from restricting certain food items, such as SSB, to only allowing purchases of a specific set of foods, such as in the WIC program. A study by Leschewski and Weatherspoon theorized that restricting a few unhealthy foods, such as SSB, would unlikely alter eating behaviors as they account for a small percentage of total expenditures.56 Restricting all non-WIC food items could result in an improvement in diet quality, but would also require SNAP households to change their total household food expenditures. This could result in unintended consequences, as money previously used for non-food expenses would need to be spent on food items that are no longer covered. This could also result in perceived stigma if households would be required to use two forms of payment within one transaction.
There are limitations to the current study. All respondent variables, including SNAP participation, income, and eating behaviors, were self-reported. SNAP participation was gathered by asking if the respondent participated in the previous year while eating behaviors were asked for the prior month; therefore, it could be the respondent was not currently enrolled in SNAP. There are also many available outlets where participants could have bought food, outside of the food outlets collected in this study. Multiple statistical tests were run on eating behaviors and food outlets with some significant results possibly occurring by chance. The use of a random digit dial for study recruitment would exclude those without a phone. Lastly, all data were cross-sectional, so results only reflect an association between SNAP and eating behaviors.
This study has many strengths. The classification process for food outlets was robust and based on a published protocol, and included more in-depth analysis than what was received from the purchased dataset. Using GIS mapping, classification of food outlet proximity was determined based on distance from each respondent’s household rather than via census tract or block boundaries. The respondents came from a large, diverse sample from four cities that included low-income, minority populations. Lastly, information on WIC participation among respondents was available, allowing for adjustment of this program, which has been shown to also influence eating behaviors.57–59
Conclusion
The role that SNAP plays in shaping food behaviors is complex, and this study suggests that the community food environment may also contribute to shaping eating habits among SNAP participants. While SNAP participation is associated with some unhealthy behaviors, this association may only be significant when respondents live in certain food environments where there is easy access to unhealthy foods. Future research is needed to investigate SNAP participation, the community food environment, and consumer-level food environment longitudinally, to examine how these variables influence eating behaviors over time.
Supplementary Material
Research Snapshot
Research Question:
Does the community food environment act as a potential moderator in the association between SNAP participation and eating behaviors?
Key Findings:
In this cross-sectional study, interaction and stratified analyses revealed that SNAP participation was associated with a higher consumption of sugar sweetened beverages only when respondents lived close to a small grocery store, supermarket, and limited service restaurant.
Acknowledgments
Funding/financial disclosures: Funding support was provided by the Robert Wood Johnson Foundation and the National Institute of Child Health and Human Development 1R01HD071583–01A1.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: There are no conflicts of interest to disclose.
Contributor Information
Cori Lorts, Northern Arizona University, 1100 S. Beaver St., Box 15095, Flagstaff, AZ 86011, Phone: 928-523-4071, Fax: 928-523-0148, Cori.Lorts@asu.edu.
Natasha Tasevska, Arizona State University, 550 N. 3rd Street, Phoenix, AZ 85004-0698, Phone: 602-827-2485, Fax: 602-496-0886.
Marc Adams, Arizona State University, 550 N. 3rd Street, Phoenix, AZ 85004-0698, Phone: 602-827-2470, Fax: 602-496-0886.
Michael J. Yedida, Rutgers University, 112 Paterson Street, 5th Floor, New Brunswick, NJ 08901-1293, Phone: 848-932-4645, Fax: 732-932-0069, myedidia@ifh.rutgers.edu.
David Tulloch, Rutgers University, 93 Lipman Drive, New Brunswick, NJ 08901-8524, Phone: 732-932-1581, Fax: 732-932-1940, dtulloch@crssa.rutgers.edu.
Steven P Hooker, San Diego State University, 5500 Campanile Drive, San Diego, CA 92182-4124, Phone: 619-594-6516, Fax: 619-594-7103, shooker@sdsu.edu.
Punam Ohri-Vachaspati, Arizona State University, 550 N. 3rd Street, Phoenix, AZ 85004-0698, Phone: 602-827-2270, Fax: 602-496-0886, Punam.Ohri-Vachaspati@asu.edu.
References
- 1.Coleman-Jensen A, P RM, Gregory CA, Singh A. Household Food Security in the United States in 2015 United States Department of Agriculture, Economic Research Service; 2016. [Google Scholar]
- 2.Supplemental Nutrition Assistance Program (SNAP). Economic Research Service. United States Department of Agriculture. https://www.ers.usda.gov/topics/food-nutrition-assistance/supplemental-nutrition-assistance-program-snap/. Accessed June 15, 2017.
- 3.Gregory C, Ver Ploeg M, Andrews M, Coleman-Jensen A. Supplemental Nutrition Assistance Program (SNAP) participation leads to modest changes in diet quality United States Department of Agriculture, Economic Research Service; 2013. [Google Scholar]
- 4.Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: a systematic review. Am J Prev Med 2015;49(4):594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen BT, Shuval K, Njike VY, Katz DL. The Supplemental Nutrition Assistance Program and dietary quality among US adults: findings from a nationally representative survey. Mayo Clin Proc 2014;89(9):1211–1219. [DOI] [PubMed] [Google Scholar]
- 6.Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC. Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. Am J Clin Nutr 2012;96(5):977–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chrisinger BW, Kallan MJ, Whiteman ED, Hillier A. Where do U.S. households purchase healthy foods? An analysis of food-at-home purchases across different types of retailers in a nationally representative dataset. Prev Med 2018;112:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lacko AM, Popkin BM, Smith Taillie L. Grocery Stores Are Not Associated with More Healthful Food for Participants in the Supplemental Nutrition Assistance Program. J Acad Nutr Diet 2018. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Todd JE, Ver Ploeg M. Caloric beverage intake among adult supplemental nutrition assistance program participants. Am J Public Health 2014;104(9):e80–e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bleich SN, Vine S, Wolfson JA. American adults eligible for the Supplemental Nutritional Assistance Program consume more sugary beverages than ineligible adults. Prev Med 2013;57(6):894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen BT, Shuval K, Bertmann F, Yaroch AL. The Supplemental Nutrition Assistance Program, food insecurity, dietary quality, and obesity among US adults. Am J Public Health 2015;105(7):1453–1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ver Ploeg M, et al. Access to Affordable and Nutritious Food: Measuring and Understanding Food Deserts and Their Consequences United Stated Department of Agriculture, Economic Research Service; 2009. [Google Scholar]
- 13.Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B. Where Do Americans Usually Shop for Food and How Do They Travel to Get There?: Initial Findings from the National Household Food Acquisition and Purchase Survey United States Department of Agriculture, Economic Research Service; 2015. [Google Scholar]
- 14.Schwartz G, Grindal T, Wilde P, Klerman J, Bartlett S. Supermarket Shopping and The Food Retail Environment among SNAP Participants. J Hunger Environ Nutr 2018;13(2):154–179. [Google Scholar]
- 15.Ver Ploeg M, Wilde PE. How do food retail choices vary within and between food retail environments? Food Policy 2018;79:300–308. [Google Scholar]
- 16.Hillier A, Cannuscio CC, Karpyn A, McLaughlin J, Chilton M, Glanz K. How far do low-income parents travel to shop for food? Empirical evidence from two urban neighborhoods. Urban Geogr 2011;32(5):712–729. [Google Scholar]
- 17.LeDoux TF, Vojnovic I. Examining the role between the residential neighborhood food environment and diet among low-income households in Detroit, Michigan. Appl Geogr 2014;55:9–18. [Google Scholar]
- 18.Ni Mhurchu C, Vandevijvere S, Waterlander W, et al. Monitoring the availability of healthy and unhealthy foods and nonalcoholic beverages in community and consumer retail food environments globally. Obes Rev 2013;14:108–119. [DOI] [PubMed] [Google Scholar]
- 19.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health Place 2012;18(5):1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson PL, Dominguez F, Teklehaimanot S, Lee M, Brown A, Goodchild M. Does distance decay modelling of supermarket accessibility predict fruit and vegetable intake by individuals in a large metropolitan area? J Health Care Poor Underserved 2013;24(10):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dunn RA, Dean WR, Johnson CM, Leidner A, Sharkey JR. The Effect of Distance and Cost on Fruit and Vegetable Consumption in Rural Texas. J Agr Appl Econ 2015;44(4):491–500. [Google Scholar]
- 22.Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health 2002;92(11):1761–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zenk SN, Schulz AJ, Hollis-Neely T, et al. Fruit and vegetable intake in African Americans: income and store characteristics. Am J Prev Med 2005;29(1):1–9. [DOI] [PubMed] [Google Scholar]
- 24.Hearst MO, Pasch KE, Laska MN. Urban v. suburban perceptions of the neighbourhood food environment as correlates of adolescent food purchasing. Public Health Nutr 2012;15(2):299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr 2010;13(11):1757–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn RA, Sharkey JR, Horel S. The effect of fast-food availability on fast-food consumption and obesity among rural residents: an analysis by race/ethnicity. Econ Hum Biol 2012;10(1):1–13. [DOI] [PubMed] [Google Scholar]
- 27.Gustafson A, Lewis S, Perkins S, Wilson C, Buckner E, Vail A. Neighbourhood and consumer food environment is associated with dietary intake among Supplemental Nutrition Assistance Program (SNAP) participants in Fayette County, Kentucky. Public Health Nutr 2013;16(07):1229–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gustafson A, Lewis S, Perkins S, et al. Association Between the Retail Food Environment, Neighborhood Deprivation, and County-Level Dietary Outcomes Among Supplemental Nutrition Assistance Program–Education (SNAP-Ed) Recipients in Kentucky, 2010–2011. J Hunger Environ Nutr 2013;8(3):362–377. [Google Scholar]
- 29.Beatty TK, Tuttle CJ. Expenditure response to increases in in-kind transfers: Evidence from the Supplemental Nutrition Assistance Program. Am J Agric Econ 2014;97(2):390–404. [Google Scholar]
- 30.Kim J Do SNAP participants expand non-food spending when they receive more SNAP Benefits?—Evidence from the 2009 SNAP benefits increase. Food Policy 2016;65:9–20. [Google Scholar]
- 31.U.S. Census Quick Facts. https://www.census.gov/quickfacts/fact/table/. Accessed May 23, 2018.
- 32.Am I Eligible for SNAP? Supplemental Nutrition Assistance Program (SNAP). https://www.fns.usda.gov/snap/eligibility. Accessed May 21, 2017.
- 33.Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatr 2013;167(1):14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS) Survey Atlanta, Georgia: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire: Hyattsville, MD: U.S: Department of Health and Human Services, Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 37.Ohri-Vachaspati P, Martinez D, Yedidia MJ, Petlick N. Improving data accuracy of commercial food outlet databases. Am J Health Promt 2011;26(2):116–122. [DOI] [PubMed] [Google Scholar]
- 38.InfoUSA. https://www.infousa.com/. Accessed July 22, 2017.
- 39.Nielsen. http://www.nielsen.com/us/en.html. Accessed July 22, 2017.
- 40.US Census Bureau, North American Industry Classification System (NAICS). http://www.census.gov/eos/www/naics/. Accessed October 16, 2016.
- 41.Hardin JW, Hilbe JM, Hilbe J. Chapter 6: The gamma family. Generalized linear models and extensions: Stata press; 2007. [Google Scholar]
- 42.Ohri-Vachaspati P, Lloyd K, DeLia D, Tulloch D, Yedidia MJ. A closer examination of the relationship between children’s weight status and the food and physical activity environment. Prev Med 2013;57(3):162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stata [computer program]. Version 13.1 College Station, TX: StataCorp; 2013. [Google Scholar]
- 44.Hilmers A, Chen T-A, Dave JM, Thompson D, Cullen KW. Supplemental Nutrition Assistance Program participation did not help low income Hispanic women in Texas meet the dietary guidelines. Prev Med 2014;62:44–48. [DOI] [PubMed] [Google Scholar]
- 45.Vilaro MJ, Barnett TE. The rural food environment: a survey of food price, availability, and quality in a rural Florida community. Food and Public Health 2013;3(3):111–118. [Google Scholar]
- 46.Mabli J, Castner L, Ohls J, Fox MK, Crepinsek MK, Condon E. Food expenditures and diet quality among low-income households and individuals Mathematica Policy Research; 2010. [Google Scholar]
- 47.Wilde PE, Troy LM, Rogers BL. Food stamps and food spending: An Engel function approach. Am J Agric Econ 2009;91(2):416–430. [Google Scholar]
- 48.Gustafson A, Christian JW, Lewis S, Moore K, Jilcott S. Food venue choice, consumer food environment, but not food venue availability within daily travel patterns are associated with dietary intake among adults, Lexington Kentucky 2011. Nutr J 2013;12(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Neighborhood retail food environment and fruit and vegetable intake in a multiethnic urban population. Am J Health Promt 2009;23(4):255–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kruger DJ, Greenberg E, Murphy JB, DiFazio LA, Youra KR. Local concentration of fast-food outlets is associated with poor nutrition and obesity. Am J Health Promt 2014;28(5):340–343. [DOI] [PubMed] [Google Scholar]
- 51.Laska MN, Caspi CE, Pelletier JE, Friebur R, Harnack LJ. Peer Reviewed: Lack of Healthy Food in Small-Size to Mid-Size Retailers Participating in the Supplemental Nutrition Assistance Program, Minneapolis–St. Paul, Minnesota, 2014. Prev Chronic Dis 2015;12:E135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andreyeva T, Blumenthal DM, Schwartz MB, Long MW, Brownell KD. Availability and prices of foods across stores and neighborhoods: the case of New Haven, Connecticut. Health Affairs 2008;27(5):1381–1388. [DOI] [PubMed] [Google Scholar]
- 53.Gustafson A, Hankins S, Jilcott S. Measures of the consumer food store environment: a systematic review of the evidence 2000–2011. J Community Health 2012;37(4):897–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bartlett S, Associates A. Evaluation of the Healthy Incentives Pilot (HIP), Final Report United States Department of Agriculture, Food and Nutrition Service, Office of Policy Support; 2014. [Google Scholar]
- 55.Klerman JA, Collins AM, Olsho LE. Improving nutrition by limiting choice in the Supplemental Nutrition Assistance Program. Am J Prev Med 2017;52(2S2):S171–S178. [DOI] [PubMed] [Google Scholar]
- 56.Leschewski AM, Weatherspoon DD. The Supplemental Nutrition Assistance Program: Current and Proposed Restricted Food Expenditures. Am J Prev Med 2018;55(3):e70–e77. [DOI] [PubMed] [Google Scholar]
- 57.Schultz DJ, Shanks CB, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for women, infants, and children food package revisions on participants: a systematic review. J Acad Nutr Diet 2015;115(11):1832–1846. [DOI] [PubMed] [Google Scholar]
- 58.Andreyeva T, Tripp AS. The healthfulness of food and beverage purchases after the federal food package revisions: The case of two New England states. Prev Med 2016;91:204–210. [DOI] [PubMed] [Google Scholar]
- 59.Okeke JO, Ekanayake RM, Santorelli ML. Effects of a 2014 Statewide Policy Change on Cash-Value Voucher Redemptions for Fruits/Vegetables Among Participants in the Supplemental Nutrition Program for Women, Infants, and Children (WIC). Matern Child Health J 2017;21(10):1874–1879. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.