The advances in drug development has improved therapeutic options for patients with cancer. Therapeutic decision-making often includes multiple considerations. Data on the probability of remission, survival and toxicity are readily available from clinical trials. Patient-reported outcomes including quality of life has been increasingly incorporated in trials in recent years. However, patients’ preferences are distinctly understudied. In this focused review, I will discuss some of the studies that have explored preferences of patients with cancer and our attempt to develop a tool to examine therapy preferences.
Value of understanding patients’ preferences
Selection of cancer treatments for an individual patient is complex. Cancer treatments have varying probability of achieving remission and survival. Therapies are often associated with significant risk of toxicities, much higher than therapies used for most other diseases. Different therapies have their unique features such as administration in an outpatient versus inpatient setting, oral versus intravenous route and so on. The complexity and burden of therapy are also very different. As an instance, for older adults with acute myeloid leukemia, currently there are intensive (e.g. a combination of anthracycline and cytarabine, or 7+3) versus low-intensity (e.g. azacitidine) chemotherapy options. These treatments differ in their ability to achieve remission, time necessary to achieve remission and survival.1 Intensive chemotherapy combinations are associated with a high risk of serious toxicities that may result in disability and decline in functional status and quality of life. While intensive chemotherapy is generally given as an inpatient, low-intensity chemotherapy can be administered as outpatient. Intensive chemotherapy may not be available close to home for patients who live far from larger academic hospitals. This may require patients and families to travel further and can add to patients’ and caregivers’ burden.
Given significant differences in efficacy, safety, and treatment characteristics, understanding patients’ preferences are important to allow selection of therapy that meets patients’ expectations and goals of care. Engaging patients’ in therapy selection can also enhance doctor-patient relationship and improve patients’ satisfaction towards medical team and health system.
Measuring patient’s preference of therapy: Literature review
In 1997, a review of literature selected 19 articles from review of more than 1400 abstracts.2 A comprehensive analysis of these articles provided a conceptual framework of patients’ experience and treatment satisfaction.2,3 Although developed for treatment satisfaction rather than patients’ preferences of therapy, this framework provides a broad overview of various factors that come into play when patients seek medical care. Some of these factors include outcomes associated with treatment, safety and convenience of treatment, treatment complexity, burden and cost. These factors can impact patients’ preference of therapy as well.
A few studies have examined patients’ preference of therapy and factors that matter to patients with cancer. For example, a study among older adults with serious illnesses highlighted that the burden of treatment, the anticipated outcome and the likelihood of outcome associated with specific therapies influenced treatment preferences. Factors associated with the burden of treatment included the length of the hospital stay, extent of testing and the invasiveness of interventions. While almost all the patients would choose to receive effective treatment that was associated with a low burden of treatment, only a minority would choose effective but high-burden treatment. Also, a minority of patients would choose treatment that prolongs survival at an expense of functional or cognitive impairment.4
A study in chronic lymphocytic leukemia5 assessed patients’ preference of therapy based on the following attributes: duration of disease control, oral versus intravenous route of administration, risk of diarrhea, risk of serious infection, risk of organ toxicities and out-of-pocket cost. The survey was specifically designed for chronic lymphocytic leukemia, especially to understand patients’ preference of therapies available at the time the study was conducted. Without modification, this survey may not be usable in any other disease or for newer therapies. The survey requires multiple hypothetical scenarios to understand whether patients would prefer one over the other of many available therapies. Individual study participant cannot express the level of interest of one therapy over the other. The survey does not measure various other factors such as caregiver burden that may be important in determining therapy selection.
An analysis of a prospective study among older adults starting chemotherapy highlighted that health outcomes such as function, freedom from pain and freedom from symptoms are more important than survival to many patients.6
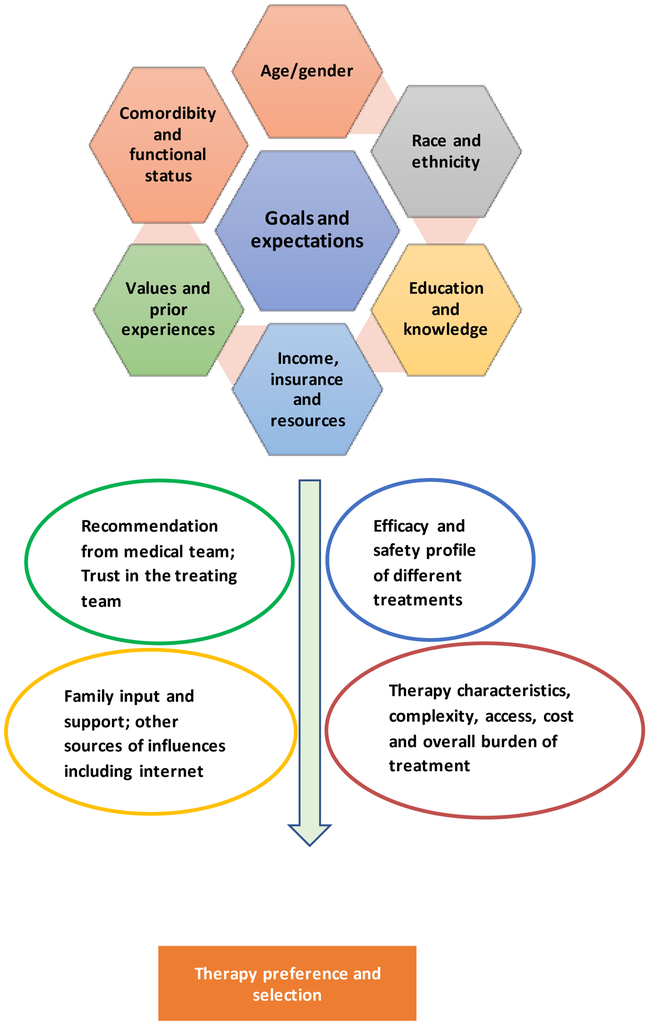
These studies provide important information about the preferences and values of patients with cancer. Based on these studies, my own personal experience as well as discussion with several health care providers involved in the care of patients with cancer, I have put together a theoretical framework of factors and processes that affect therapy preferences of a cancer patient (figure 1). These factors include:
Patient’ s characteristics such as demographic factors, functional status, cognitive status, available resources, and prior experiences. Such factors shape individual’s goals of care, and expectations from treatment. These factors also determine the relative importance a patient places on several attributes of treatment.
Attributes of treatment such as safety, effectiveness and various characteristics of treatment. These may be considered the primary determinants of preference of one over the other therapy option.
Sources of information including recommendations from the medical team, opinion of family and friends, and information from internet and publications. These sources of information can influence decision about pursuing specific treatment.
Figure 1.
Theoretical framework of factors and processes that affect therapy preferences and selection
A multitude of these factors affect patient’s preference of therapy. For instance, younger fit patients with children, who have strong family and financial support may desire cure even at an expense of serious toxicities. Conversely, older adults who have poor health, low financial or family support and suffer social isolation may prefer to avoid toxicities and high out-of-pocket cost even if the choice of therapy leads to suboptimal outcomes. Additionally, older adults with less family support may prefer receiving therapy closer to home.
Development of a therapy preference scale
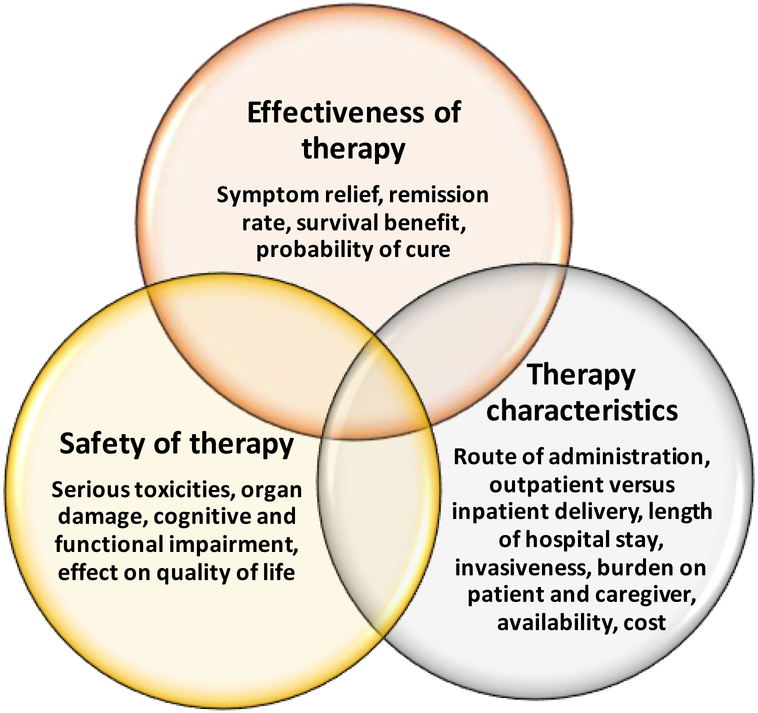
The following attributes of treatment are important to patients and are key determinants of preference of one over the other specific treatment (figure 2):
Efficacy of the treatment as measured by rates of remission, symptom palliation, improvement in survival and possibility of cure.
Safety of the treatment as measured by risk of serious toxicities as well as the impact of treatment on functional and cognitive status of patients.
Characteristics of treatment such as route and frequency of administration, outpatient versus inpatient delivery, and overall burden of therapy. Availability of therapy only in specialized centers, invasiveness of interventions, caregiver burden, and cost can greatly add to the burden associated with a therapy.
Figure 2. Key domains of the proposed therapy preference scale.
The small overlap of three domains where a therapy is associated with high efficacy, high safety and low therapy burden represents an ideal therapy for a patient. In most of the real scenarios, patients identify the most important factor from these domains and select a therapy that has the highest likelihood of achieving the most desired outcome while balancing other outcomes to the extent possible.
Based on the information, I have developed a multidimensional “therapy preference scale” (supplemental file) that includes measures of above domains as well as independent global items to compare relative importance of one factor over the other. We are in the process of field testing and validating the scale. While the scale measures attributes of treatment that patients consider to chose therapy, patients’ characteristics and sources of information provide context to understand the reason for preference of a specific therapy and should be simultaneously studied.
Purpose of a therapy preference scale
While oncologists may have a general understanding of patients’ preferences, a scale is needed to capture preferences of an individual patient with cancer in clinical practice or research setting. A multidimensional scale may also allow us to develop deeper understanding of relative importance of various factors to patients. In real-world practice, chemotherapy is underutilized, particularly in older adults. For instance, 33% of patients with acute myeloid leukemia aged 71-80 years and 41% of patients aged ≥81 years did not receive chemotherapy.7 While low utilization of chemotherapy has multiple reasons, one factor could be lack of understanding of patients’ preference about therapy and poor communication between patients and physicians.8,9 A therapy preference scale can fill this need and facilitate communication in a clinical setting and allow selection of therapy that will likely meet a patient’s goals of care. Examination of preferences of patients from diverse background and subsequently patients’ satisfaction of therapy can also help future patients learn from perspective of patients who have already gone through cancer treatments. The scale may also provide useful insights regarding patients’ perspective and values that could guide drug development and drug approval process, to some extent. As the cost of cancer therapy continues to increase, the scale can be used to determine the value of various treatments from the perspective of patients. Future studies in this field are needed to validate the scale and explore various utilities of this scale.
Acknowledgements:
This work was supported by the National Institute of General Medical Sciences, 1 U54 GM115458, which funds the Great Plains IDeA-CTR Network, and the Fred and Pamela Buffett Cancer Center Support Grant from the National Cancer Institute (P30 CA036727). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest: VRB reports receiving consulting fees from Pfizer, CSL Behring, Agios, and Incyte, and research funding from Incyte.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Bhatt VR, Gundabolu K, Koll T, Maness LJ. Initial therapy for acute myeloid leukemia in older patients: Principles of care. Leuk Lymphoma 2010, 59(1):29–41. [DOI] [PubMed] [Google Scholar]
- 2.Weaver M, Patrick DL, Markson LE, Martin D, Frederic I, Berger M. Issues in the measurement of satisfaction with treatment. Am J Manag Care 1997, 3:579–94. [PubMed] [Google Scholar]
- 3.Revicki DA. Patient assessment of treatment satisfaction: methods and practical issues. Gut 2004, 53: iv40–iv44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002, 346:1061–6. [DOI] [PubMed] [Google Scholar]
- 5.Mansfield C, Masaquel A, Sutphin J, Weiss E, Gutierrez M, Wilson J, et al. Patients' priorities in selecting chronic lymphocytic leukemia treatments. Blood Adv. 2017, 2(24):2176–2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soto Perez De Celis E, Li D, Sun CL, Kim H, Twardowski P, Fakih M, et al. Patient-defined goals and preferences among older adults with cancer starting chemotherapy (CT). J Clin Oncol 2018, 36: (suppl; abstr 10009). [Google Scholar]
- 7.Bhatt VR, Shostrom V, Gundabolu K, Armitage JO. Utilization of initial chemotherapy for newly diagnosed acute myeloid leukemia in the United States. Blood Adv 2018, 2(11):1277–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LeBlanc TW, Fish LJ, Bloom CT, El-Jawahri A, Davis DM, Locke SC, et al. Patient experiences of acute myeloid leukemia: A qualitative study about diagnosis, illness understanding, and treatment decision- making. Psychooncology 2017, 26(12)2063–2068. [DOI] [PubMed] [Google Scholar]
- 9.Nicholson S, Abel GA, Fathi AT, Steensma DP, LeBlanc TW, DeAngelo DJ, et al. Perceptions of prognosis and treatment risk in older patients with acute myeloid leukemia (AML). J Clin Oncol 2017, 35(31_suppl):43. [Google Scholar]