Highlights
-
•
Ethmoidal fibrosarcoma is an extremely rare tumor.
-
•
Mostly misdiagnosed because of none specifics symptoms, in this case patient didn’t complaint any nasal symptom.
-
•
Treatment is not codified and prognosis is unknown.
Keywords: Fibrosarcoma, Ethmoid, Endoscopy, Navigation, Histopathology
Abstract
Introduction
Ethmoidal fibrosarcoma is an extremely rare tumor which represent less than one percent of all malignancies in this anatomical area, the case of a 13-year-old is reported here.
Presentation of case
A 13-year-old boy, his medical history was marked exclusively before presented to our hospital by an exophthalmia. Rhinoscopic examination showed well-defined pink mass at the level of ethmoid. Computed tomography was performed to showed local and regional extension. Treatment was an endoscopic excision of the tumor using a navigation system. The final diagnosis was made on pathologic examination. Radiotherapy was recommended by multidisciplinary staff but the patient refused.
Discussion
These tumors occur in extremities most frequently and Ethmoidal localization is extremely rare and have no specifics symptoms, so the rhinoscopic examination is necessary for any chronic nasal symptom. Its treatment is not codified because of its rarity and its prognosis is unknown.
Conclusion
It’s important knowledge about this pathology because of its rarity and its therapeutic and prognostic difficulties.
1. Introduction
Fibrosarcoma is a malignant neoplasm of the fibroblastic origin, most commonly occurring from the soft tissue of extremities. Occurrences in the head and neck are not common, accounting for <1% of the malignancies in this anatomical area [1]. Ethmoid sinus location is an extremely rare event [2]. Clinical presentation is not specific. The case of a fibrosarcoma of ethmoid sinus in a 13-year-old boy presenting with exophthalmia is reported here.
2. Case report
A 13-year-old boy presented with a one year history of exophthalmia in the left eye, without any nasal symptoms. There was no history of local trauma or systemic disease, and he was operated on 6 months ago under a rhinoscopic approach when a marsupialization of the cyst was done with pathological examination showing characteristics of an aneurysmal cyst. He was actually admitted for recidivism of the same lesion.
Clinical examination showed exophthalmia of the left eye without loss of visual acuity (Fig. 1).
Fig. 1.
Exophthalmia of the right eye.
Rhinoscopy found a well-defined mass, sitting at the level of the left ethmoidal sinus, smooth and pink. The other side was normal (Fig. 2).
Fig. 2.
Rhinoscopy showing a well-defined mass smooth and pink.
Tomodensitometry showed an oval multiloculated lesion more extensive in the anteroposterior plan replacing the ethmoidal cells measuring 39 × 23 × 35 mm. This lesion has regular walls, duplicated by place. Its content is made of multiple stalls with a liquid level realized by blood outside as it pushes the globe and the right internal muscles without signs of invasion, responsible for an exophthalmia grade I. Inside it fills the nasal fossa and pushes the septum without a free interface. At the top it displaces the ethmoidal roof inward without endocranial invasion. It is responsible for fluid retention at the level of the left maxillary sinus, and through posterior ethmoid cells invasion it is responsible for the narrowing of the optical channel, whereas the frontal and sphenoidal sinuses are free (Fig. 3).
Fig. 3.
Oval lesion replacing the ethmoidal cells measuring 39 × 23 × 35 mm.
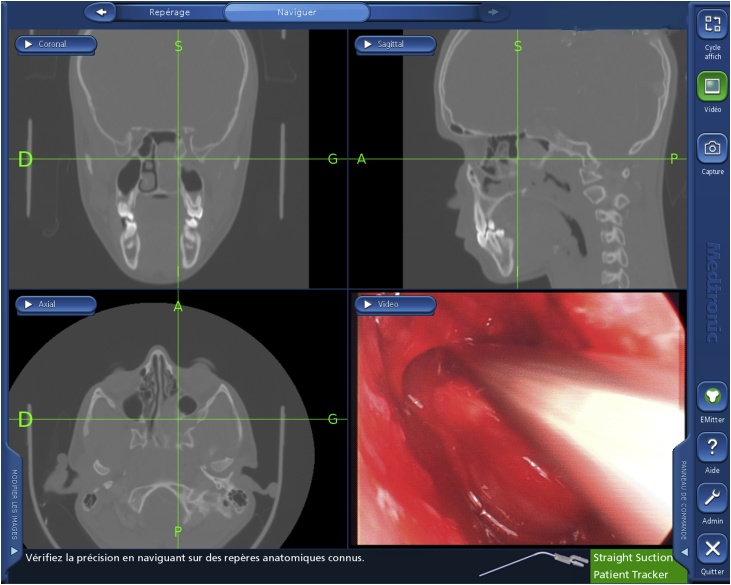
Surgical intervention involved the total excision of the tumor with all its walls, in addition to the orbital medial wall and its periorbital by endoscopic approach. This was assisted by ENT navigation system which was helpful to determine the skull base, the orbit and the carotid canal because landmarks are modified by the tumor (Fig. 4).
Fig. 4.
Navigation showing internal orbital wall in the three plan of space.
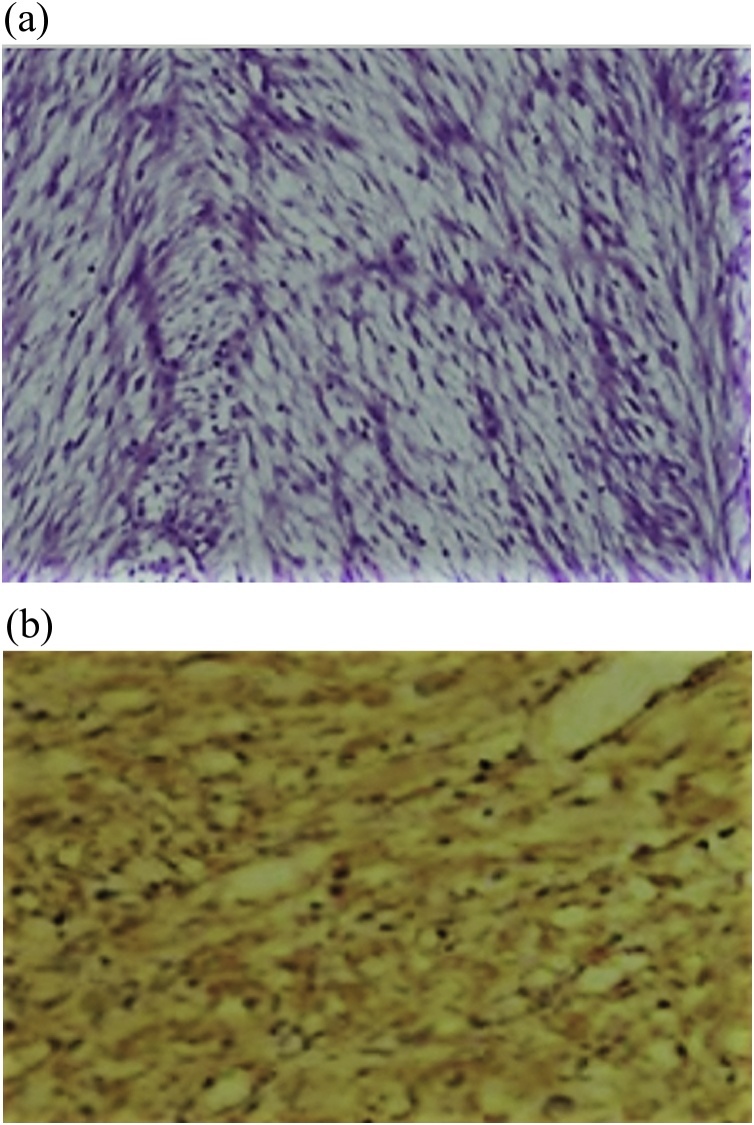
Histopathology found fusocelular carcinomatous proliferation in the herring bone with calcification, presence of multinucleate elements showing atypia estimated at 3/10 fields. Those tissues are negative for desmin and CD 34 and positive for vimentin (Fig. 5).
Fig. 5.
(a): proliferation in herring bone with multinucleate elements, (b): The tumor cells were positive for vimentin.
The multidisciplinary team deciding on the treatment options included surgeons, oncologists, radiotherapists and radiologists. The decision was made to treat the patient with radiotherapy, but the patient refused. The alternative was to closely monitor the patient, with monthly clinical and endoscopic examinations. No recidivism was actually found after one year of follow-up.
3. Discussion
Fibrosarcomas may develop in any mesenchymal tissue in which fibroblasts are present; they are most frequently located in the extremities and the trunk. Fibrosarcoma can arise in soft tissues or within bone. In the head and neck region, soft tissue sarcomas are extremely rare, accounting for less than 1% of all neoplasms [3].
It is more frequent in the fifth and sixth decades of age but cases in children and adolescents were also described in the literature [4,5].
Infantile fibrosarcoma includes less than one percent of childhood tumors and about 10 percent of soft tissues sarcomas [6,7].
Some authors have mentioned a cut‑off age of 2 years [8,9], whereas others have suggested a cut‑off age up to 5 years [10,11].
2 years was suggested to be the cut‑off age for infantile fibrosarcoma by the World Health Organization (WHO) [12].
Early signs and symptoms are unfortunately vague and may mimic minor upper respiratory infections. The most common presentation for sinonasal fibrosarcomas includes nasal airway obstruction, pain, epistaxis and hypoesthesia, not one of these symptoms was present in our patient [13].
Pathologic examination is the only way of diagnosis after imaging studies. Histologically, sinonasal fibrosarcomas are composed of hypercellular tumors with spindle shaped thin cells arranged in typical herring bone pattern [14]. When this histologic picture is diffuse and uniform, diagnosis can be made even without ancillary studies [15]. These tumors are negative for pancytokeratin, desmin, S100 and SMA. They are only positive for vimentin [16].
Surgery remains the mainstay for the treatment of fibrosarcomas. Wide local excision with radical margins is generally recommended [17,18]. Adjuvant radiotherapy is also used in positive surgical margins or macroscopically incomplete excision [19]. In this case the patient refused radiotherapy so the multidisciplinary decision was to opt for a complete surgical excision with a monthly follow-up.
The greatest advantage of endoscopic surgery assisted by navigation for malignant tumors is the reduction in morbidity and length of stay, but surgical margins are not always controlled.
4. Conclusion
Fibrosarcoma is very rare tumor, especially head and neck localization, symptoms are not specific, so the rhinoscopic examination is necessary when investigating any chronic nasal symptom or exophthalmia. Its treatment and prognosis is not codified because of its rarity.
Conflicts of interest
Authors do not declare any conflict of interest.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study is exempt from ethnical approval in our institution.
Consent
Written informed consent was obtained from the patient's parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
Author contribution
Dr Zouhair and dr chaouki have participated in the papers writing and images treatement, Pr Rouadi, Pr Abada, Pr Roubal and Pr Mahtar in the rereading and final approval of the manuscript upon submission.
Registration of research studies
None.
Guarantor
Zouhair Najib.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgement
Authors have no acknowledgement.
References
- 1.Cecchetto G., Carli M., Alaggio R., Dall’Igna P., Bisogno G., Scarzello G. Fibrosarcoma in pediatric patients: results of the Italian Cooperative Group studies (1979‑1995) J. Surg. Oncol. 2001;78:225–231. doi: 10.1002/jso.1157. [DOI] [PubMed] [Google Scholar]; Cecchetto G, Carli M, Alaggio R, Dall’Igna P, Bisogno G, Scarzello G, et al, Fibrosarcoma in pediatric patients: Results of the Italian Cooperative Group studies (1979‑1995). J Surg Oncol 78 (2001) 225‑31. [DOI] [PubMed]
- 2.Mansouri H., Rzin M., Marjani M., Sifat H., Hadadi K., Hassouni K. Fibrosarcoma of the maxillary sinus. Indian J. Otolaryngol. Head Neck Surg. 2006;58:104–105. doi: 10.1007/BF02907759. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mansouri H, Rzin M, Marjani M, Sifat H, Hadadi K, Hassouni K, et al, Fibrosarcoma of the maxillary sinus. Indian J Otolaryngol Head Neck Surg 58 (2006) 104‑5. [DOI] [PMC free article] [PubMed]
- 3.Rajendran R., Sivapathasundharam B. 6th ed. Elsevier Company; New Delhi: 2009. Shafer’s Textbook of Oral Pathology; pp. 155–157. [Google Scholar]; Rajendran R, Sivapathasundharam B, Shafer’s textbook of oral pathology. 6th ed. New Delhi: Elsevier Company (2009) 155-157
- 4.Dehner L.P. Tumors of the mandible and maxilla in children II. A study of 14 primary and secondary malignant tumors. Cancer. 1973;32:112–120. doi: 10.1002/1097-0142(197307)32:1<112::aid-cncr2820320115>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]; Dehner LP, Tumors of the mandible and maxilla in children II. A Study of 14 Primary and Secondary Malignant Tumors. Cancer 32 (1973) 112‑120. [DOI] [PubMed]
- 5.Blocker S., Koenig J., Ternberg J. Congenital fibrosarcoma. J. Pediatr. Surg. 1987;22:665–670. doi: 10.1016/s0022-3468(87)80123-9. [DOI] [PubMed] [Google Scholar]; Blocker S, Koenig J, Ternberg J, Congenital fibrosarcoma. J Pediatr Surg 22 (1987) 665‑670. [DOI] [PubMed]
- 6.Celkan T., Ozkan A., Apak H., Ibrahimi B., Dervisoglu S., Yuksel L. Two different clinical presentation of infantile fibrosarcoma. Turk. J. Cancer. 2000;30:81–86. [Google Scholar]; Celkan T, Ozkan A, Apak H, Ibrahimi B, Dervisoglu S, Yuksel L,et al, Two different clinical presentation of infantile fibrosarcoma. Turkish Journal of cancer 30 (2000) 81-86.
- 7.Dixon N.E., Morales J., Escalon E. Congenital fibrosarcoma: report of one case treated with presurgical chemotherapy. Int. Pediatr. 2003;18(2):8791. [Google Scholar]; Dixon NE, Morales J, Escalon E,et al, Congenital fibrosarcoma:Report of one case treated with presurgical chemotherapy. Int Pediatr 18(2) (2003) 8791.
- 8.Enzinger F.M., Weiss S. Mosby; St Louis: 1995. Soft Tissue Tumours; pp. 231–239. [Google Scholar]; Enzinger FM, Weiss S, Soft tissue tumours. St Louis: Mosby 1995 (231-39).
- 9.Cecchetto G., Carli M., Alaggio R., Dall’Igna P., Bisogno G., Scarzello G. Fibrosarcoma in pediatric patients: results of the Italian cooperative group studies (1979–1995) J. Surg. Oncol. 2001;78:225–231. doi: 10.1002/jso.1157. [DOI] [PubMed] [Google Scholar]; Cecchetto G, Carli M, Alaggio R, Dall’Igna P, Bisogno G, Scarzello G, et al, Fibrosarcoma in pediatric patients: Results of the Italian Cooperative Group Studies (1979‑1995). J Surg Oncol 78 (2001) 225‑231. [DOI] [PubMed]
- 10.Hays D.M., Mirabal V.Q., Karlan M.S., Patel H.R., Landing B.H. Fibrosarcomas in infants and children. J. Pediatr. Surg. 1970;5:176–183. doi: 10.1016/0022-3468(70)90274-5. [DOI] [PubMed] [Google Scholar]; Hays DM, Mirabal VQ, Karlan MS, Patel HR, Landing BH, Fibrosarcomas in infants and children. J Pediatr Surg 5 (1970) 176‑183. [DOI] [PubMed]
- 11.Chung E.B., Enzinger F.M. Infantile fibrosarcoma. Cancer. 1976;38:729–739. doi: 10.1002/1097-0142(197608)38:2<729::aid-cncr2820380216>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]; Chung EB, Enzinger FM, Infantile Fibrosarcoma. Cancer 38 (1976) 729‑739. [DOI] [PubMed]
- 12.Coffin C.M., Fletcher J.A. Infantile fibrosarcoma. In: Fletcher C.D., Unni K.K., Mertens F., editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press; Lyon, France: 2002. pp. 98–100. [Google Scholar]; Coffin CM, Fletcher JA, Infantile Fibrosarcoma. In: Fletcher CD, Unni KK, Mertens F, editors. World Health Organization Classification of Tumours. Pathology and genetics of tumours of soft tissue and bone. Lyon, France: IARC Press (2002) 98‑100.
- 13.Bailey B.J., Johnson J.T., Kohul R.I., Pillsbury H.C., Tardy M.E. Lippincott; 1993. Neoplasms of the Nose and Paranasal Sinuses. Head and Neck Surgery Otolarygology; p. 105. [Google Scholar]; Bailey BJ, Johnson JT, Kohul RI, Pillsbury HC, Tardy ME, Neoplasms of the nose and paranasal sinuses. Head and Neck Surgery Otolarygology: Lippincott (1993) 105.
- 14.Frankenthaler R., Ayala A.G., Hartwick R.W., Goepfert H. Fibrosarcoma of the head and neck. Laryngoscope. 1990;100:799–802. doi: 10.1288/00005537-199008000-00001. [DOI] [PubMed] [Google Scholar]; Frankenthaler R, Ayala AG, Hartwick RW, Goepfert H, Fibrosarcoma of the head and neck. Laryngoscope 100 (1990) 799‑802. [DOI] [PubMed]
- 15.Lyos A.T., Goepfert H., Luna M.A., Jaffe N., Malpica A. Soft tissue sarcoma of the head and neck in children and adolescents. Cancer. 1996;77:193–200. doi: 10.1002/(SICI)1097-0142(19960101)77:1<193::AID-CNCR31>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]; Lyos AT, Goepfert H, Luna MA, Jaffe N, Malpica A, Soft tissue sarcoma of the head and neck in children and adolescents. Cancer 77 (1996) 193‑200. [DOI] [PubMed]
- 16.Coffin C.M., Jaszcz W., O’Shea P.A., Dehner L.P. So‑called congenital‑infantile fibrosarcoma: does it exist and what is it? Pediatr. Pathol. 1994;14:133–150. doi: 10.3109/15513819409022033. [DOI] [PubMed] [Google Scholar]; Coffin CM, Jaszcz W, O’Shea PA, Dehner LP, So‑called congenital‑infantile fibrosarcoma: Does it exist and what is it? Pediatr Pathol 14 (1994) 133‑50. [DOI] [PubMed]
- 17.Pe´ rez-Ordo´ n˜ ez B., Huvos A.G. Nonsquamous lesions of nasal cavity, paranasal sinuses, and nasopharynx. In: Gnepp D.R., editor. Diagnostic Surgical Pathology of the Head and Neck. W.B. Saunders Company; Philadelphia: 2001. pp. 79–139. [Google Scholar]; Pe´ rez-Ordo´ n˜ ez B, Huvos AG, Nonsquamous lesions of nasal cavity, paranasal sinuses, and nasopharynx. In: Gnepp DR (ed) Diagnostic surgical pathology of the head and neck. W.B. Saunders Company, Philadelphia (2001) 79–139
- 18.Shah J.P. Fibrosarcoma of nasal cavity. N. Y. State J. Med. 1977;77:983–984. [PubMed] [Google Scholar]; Shah JP, Fibrosarcoma of nasal cavity. N Y State J Med 77 (1977) 983–984 [PubMed]
- 19.Koka V., Vericel R., Lartigau E., Lusinchi A., Schwaab G. Sarcomas of nasal cavity and paranasal sinuses: chondrosarcoma, osteosarcoma and fibrosarcoma. J. Laryngol. Otol. 1994;108:947–953. doi: 10.1017/s0022215100128609. [DOI] [PubMed] [Google Scholar]; Koka V, Vericel R, Lartigau E, Lusinchi A, Schwaab G, Sarcomas of nasal cavity and paranasal sinuses: chondrosarcoma, osteosarcoma and fibrosarcoma. J Laryngol Otol 108 (1994) 947–953 [DOI] [PubMed]