Abstract
Background
In recent years, cocaine use has increased in many countries, but only a minority of users seek treatment. Cognitive behavioral therapy (CBT) is seen as first-choice face-to-face treatment. However, a web-based intervention might serve as an alternative.
Aims
To test the efficacy of a web-based self-help intervention, with and without chat counseling, grounded in CBT, at reducing cocaine use in cocaine misusers not in treatment for a substance use disorder.
Methods
Subjects were randomly assigned to (1) a self-help intervention with chat support, (2) a self-help intervention without chat support, or (3) a waiting list control group. The fully-automated self-help program consisted of eight modules based on motivational interviewing, self-control practices and CBT. The primary outcome was the quantity of cocaine use per week. Secondary outcomes included frequency of cocaine and other substance use and mental health symptoms. Linear regression analysis was performed to investigate changes in primary and secondary outcomes.
Results
In total, 416 users registered online for the trial, of whom 311 completed the baseline assessment. Participants were predominantly male (73%) and averaged 33 years old (SD = 7.6). Despite considerable efforts on our part, only 47 of 311 (15.1%) subjects completed the 6-month follow-up assessment. Frequency of cocaine use and severity of cocaine dependence decreased only in the intervention groups. No significant difference in the primary outcome was observed between the study arms, but several differences in secondary outcomes were observed by complete case analyses.
Conclusions
Many cocaine misusers from the general population and not otherwise in treatment could be reached and decreased their cocaine use utilizing a CBT-based online intervention. However, due to the high percentage of dropouts and serious difficulties reaching subjects for follow-up assessments, no conclusions can be drawn regarding study arm differences. Implications for future studies are discussed.
Keywords: Cocaine, Internet, Chat, Self-help, Cognitive Behavioral Therapy, Motivational Interviewing
Highlights
-
•
Chat counseling in addition to web-based self-help in cocaine misusers from the general population was investigated in a RCT.
-
•
Many cocaine misusers were reached and reduced their use with a CBT-based online program with or without chat counseling.
-
•
Due to dropouts and serious difficulties reaching subjects for follow-ups, differences between study arms are inconclusive.
1. Background
Although prevalence rates for cocaine misuse and cocaine dependence remain unclear, the lifetime prevalence of cocaine use has almost doubled in the Swiss general population (among those ages 15–34 years old) over the past fourteen years (Gmel et al., 2014). This is consistent with findings in many other countries in Southern and Western Europe (EMCDDA, 2016). However, the prevalence of cocaine use might be underestimated in general population surveys (Beck et al., 2014; Fendrich et al., 2004). One indication of this stems from wastewater analysis, inferring that cocaine use doubled in most major cities in Switzerland between 2012 and 2017 EMCDDA (European Monitoring Centre for Drugs and Drug Addiction), 2018). Another indication is that, since 2005, cocaine has been reported as the primary substance problem roughly as often as opiates, upon client entry into resident institutions and outpatient units targeting the treatment of substance use disorders (SUDs) (Maffli et al., 2013). It is assumed that the occasional use of cocaine is much more prevalent than addictive use. Nevertheless, some occasional cocaine users switch to more harmful consumption, misuse and abuse (Haasen et al., 2004). Ultimately, and although serious investigations are missing in Switzerland, as well as in other European countries, there must be a sizeable treatment gap in cocaine misusers/abusers.
Outpatient treatment grounded in Cognitive Behavioral Therapy (CBT) has been effective at treating cocaine dependence (De Crescenzo et al., 2018), while intense research on psychopharmacological approaches over the past three decades has failed to identify any compelling evidence of effective medicinal treatments (Indave et al., 2016; Minozzi et al., 2015; Singh et al., 2016). Moreover, certain effective psycho-social interventions, which reward cocaine abstinence — like Contingency Management and the Community Reinforcement Approach — hardly seem feasible in European countries, due to healthcare policies and health insurance-related differences (Schaub et al., 2009; Schaub and Stohler, 2010). Despite the apparent effectiveness of CBT, however, only a small percentage of such individuals currently receive treatment (Haasen et al., 2004).
Web-based interventions that aim to reduce harmful cocaine use might fill an important gap, by providing support for cocaine misusers and those with early dependence who have not responded well to current institution-based treatment. The Internet is a useful tool to reach hidden populations, like illicit drug users (Miller and Sønderlund, 2010). Furthermore, web-based interventions are easy to access and exhibit a remarkably-positive cost-benefit relationship (Curry, 2007), which is an important advantage.
In the first meta-analysis investigating the pooled effectiveness of internet interventions for illicit drug use (excluding cannabis), interventions designed to reduce cocaine and/or amphetamine use were, overall, not significantly better than the control conditions adopted for comparison (n = 481, p = 0.164) (Boumparis et al., 2017). Those studies that did yield an effective decrease in cocaine use involved internet-based community reinforcement, in addition to face-to-face counseling among patients receiving community-based treatment (Brooks et al., 2010); or internet-based CBT plus face-to-face CBT in a methadone maintenance program (Carroll et al., 2014), combined with frequent urinalysis. However, web-based interventions designed to reduce stimulant drug use in individuals recruited from the general population, without being an add-on to face-to-face treatment and not involving urinalysis, generated mixed results (Schaub et al., 2012; Tait, 2014).
To the best of our knowledge, no study to date has investigated the effectiveness of a guided internet-based intervention — whereby participants receive additional online counseling or therapy, or web-based self-help — for the reduction or cessation of cocaine use. Such an intervention could provide better anonymity, while potentially being more effective than an internet intervention involving self-help only. The latter is consistent with results from studies investigating web-based interventions aiming to reduce alcohol (Blankers et al., 2011; Riper et al., 2018) and cannabis use (Schaub et al., 2013; Schaub et al., 2015b) in alcohol and cannabis misusers, respectively, in which superior effects were identified for guided interventions.
The present study aimed to investigate and compare the effectiveness of Snow Control 2.0 (Schaub et al., 2015a) – a web-based self-help intervention with or without tailored chat counseling – at reducing cocaine use in cocaine misusers and those with early cocaine dependence, relative to a six-month waiting list control condition.
2. Methods
2.1. Study interventions
This study had three subject groups, two involving an intervention, and a third, control group. The first intervention (Intervention Group 1) consisted of up to three individual chat-counseling sessions, plus the web-based self-help intervention detailed in the next few paragraphs. The second intervention (Intervention Group 2) was the same as the first, but without chat-counseling sessions. The third group was a waiting list control group (Controls).
2.2. Self-help intervention (Interventions 1 and 2)
The web-based self-help intervention that we offered in this study was a 2015 revision (2.0) of the original Snow Control program developed in 2011 (Schaub et al., 2011). It is grounded in classical CBT for treating cocaine dependence (Petitjean et al., 2014), behavioral self-management (BSM) (McKee et al., 2007), motivational enhancement techniques (MET) (McKee et al., 2007), CBT for depression (Lewinsohn, 1975), and social problem solving (D'zurilla and Nezu, 1990). It has four main components:
-
•
Psychoeducation modules
-
•
Personal companions (as part of the modules)
-
•
A consumption diary, and
-
•
Automated e-mail feedback.
Additionally, the website contains a glossary, a knowledge base, a “Help Me” section, and a contact page.
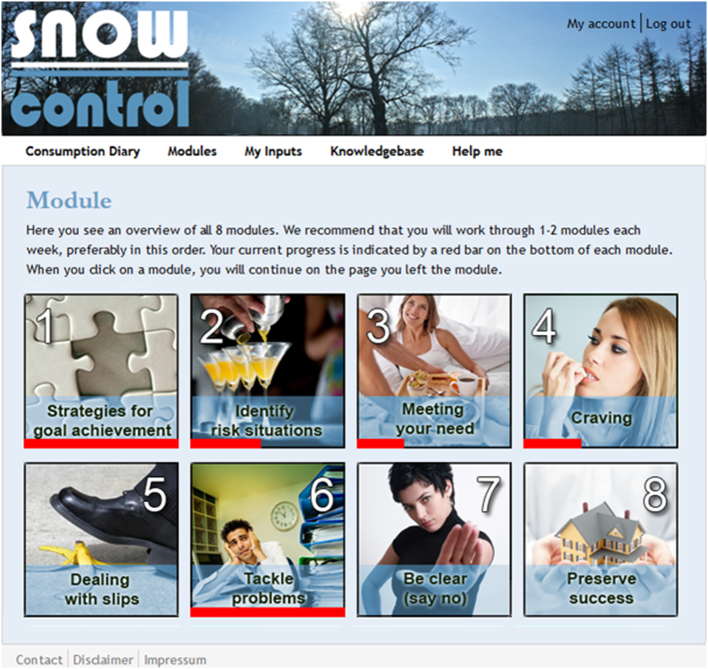
2.3. Modules
The self-help intervention starts with an introductory module (module 0). Upon completion of the introductory module, users are provided with an overview of eight modules (see Fig. 1) and encouraged to work through 1–2 modules per week, at their own pace; preferably in the order in which the modules are presented. Each module consists of a set of pages that can be navigated backwards and forwards. The user is free to enter and leave any module as they wish, and provided with the last page visited upon re-entry. Overall progress within each module is shown as a progress bar on the module overview page, as depicted below.
Fig. 1.
Screenshot of the module overview page.
Brief descriptions of the nine modules:
-
0.
Introductory Module
-
•
Introduction to a personal companion (users are presented with six companion profiles and asked to select one)
-
•
Examination of the pros and cons of changing cocaine consumption patterns to address motivation
-
•
Goal setting and introduction to e-mail reminders
-
•
Introduction to the menu item “consumption diary” and its fully-automated progress charts and statistics
-
•
Introduction to the menu item “My Inputs”, where individuals can review their acquired module documents (e.g., a list of the top five strategies for managing cocaine cravings)
-
•
Introduction to the menu item “Help Me” for immediate advice to common problems and access to emergency contacts
-
1.
Module 1: Strategies for goal achievement
-
2.
Module 2: Identifying risky situations
-
3.
Module 3: Meeting your needs
-
4.
Module 4: Cravings
-
5.
Module 5: Dealing with slips
-
6.
Module 6: Tackling problems
-
7.
Module 7: Be clear (say no)
-
8.
Module 8: Maintaining success
2.4. Personal companion
At the beginning of the introductory module, six companions are introduced briefly. Users are asked to choose one virtual companion with whom they, themselves, best identify. The six provided companions vary in their gender, age, sexual orientation, family status, and professional circumstances, to maximize the likelihood that users can find one with whom they can relate. In each module, the personal companion may provide specific advice or examples of useful intervention strategies. Furthermore, users may alternate between different personal companions to gather additional advice and examples.
2.5. Consumption diary
The consumption diary allows users to set goals and monitor their achievements. They enter both their intended consumption (for the upcoming week) and actual consumption (over the previous week) for each day. They are sent weekly reminders to fill out their diary by automated e-mails. A graph shows their progress over time. When diaries are filled out on a weekly basis, users receive two types of automatic feedback: one instantaneously in the website diary, and a second later by e-mail.
The first type of feedback, within the diary, compares their last week's intended and actual cocaine use. If they met their goal, this was considered a success and positive feedback (congratulations) was displayed. If they fell short of their goal, this was considered a failure and compassionate feedback was displayed. Feedback also included an automatic assessment of how ambitious their goal was, based upon the percentage they planned to reduce their consumption, with a < 10% reduction labelled “very moderate”, 10%–20% “moderate”, 20%–30% “standard”, 30%–50% ambitious” and over 50% “very ambitious”. A suggested percentage reduction for the next week's goal was calculated, as either a moderate (10%–20%) or standard (20%–30%) reduction. Moderate reductions were suggested to users who previously had set themselves moderate goals and failed, and to users with very moderate goals (whether they had previously failed or succeeded). Standard reductions were suggested to users who had previously set themselves moderate goals and succeeded, and to those with ambitious or very ambitious goals (whether they had previously failed or succeeded).
The second type of feedback was provided, via e-mail, at some time after users had filled in their last week's consumption data. It consisted of brief positive, neutral or compassionate motivational feedback, depending on whether their cocaine use had reduced, stagnated or increased, from a pool of 3 × 6 different messages.
Another diary feature was the overall end goal, which was set by users during their first week. Users were encouraged (and technically required) to target at least a 40% reduction in weekly cocaine use over the course of the six-week intervention. This was done to decrease the likelihood that users would set their goal at zero (abstinence) and quit after reaching it within the first few weeks, as frequently occurred in the preliminary Snow Control study (Schaub et al., 2012); and to prevent users from setting unduly-modest goals and risking early relapse. Those who sought to achieve cocaine abstinence were encouraged to make similar step-by-step reductions until full abstinence was attained. To avoid severe withdrawal symptoms and potential health risks, abrupt cocaine abstinence was not recommended, contrary to the “cold turkey” technique frequently employed to quit cigarette smoking or chewing tobacco (Bock et al., 2004). Once users achieved their overall goal, they were encouraged to maintain their reduced cocaine use or abstinence, or to further reduce their use successively through week 6.
2.6. Automated e-mails
Four types of automated e-mail were sent:
-
•
Diary feedback (described above)
-
•
Weekly guidance e-mails (roughly 100 words each for motivation)
-
•
Reminder e-mails, reminding users to fill out their diary (repeated once, two days later, if the diary remained uncompleted)
-
•
Reminder e-mails, reminding users to complete the follow-up survey
All texts addressed users personally through their username, were sent via webmaster@snowcontrol.ch, and were signed impersonally by the “SNOW Control Team”.
2.7. Chat-counseling sessions (Intervention 1 only)
Chat-counseling sessions were conducted on the website within a frame at the bottom right corner of the page and scheduled for half an hour each. All written exchanges were recorded for later analysis.
Up to three chat-counseling sessions were initiated, by email, by trained professional therapists, intended to support behavioral changes through MET. Users could discuss the web-based self-help intervention modules and review progress in their consumption diary. Chat-counseling sessions also were used to foster and review socially-rewarding contacts. A more detailed description of the training of the professional therapists and chat-counseling procedures can be found in the study protocol, published elsewhere (Schaub et al., 2015a).
2.8. Technical specifications
Snow Control 2.0 is an SSL-encrypted website based on Drupal 7 (a content management system) with a responsive design for computer screens, tablets and smartphones. Any internet user can register an online account via www.snowcontrol.ch by providing a unique username and e-mail address. Registration is not complete until a verification e-mail link has been clicked and a personal password set.
All user data were acquired via the website and hosted on professionally-managed servers in Switzerland, with ISO27001-certified security regulations. Access to user data was restricted to password-protected accounts. During the trial, security updates were implemented, and minor spelling errors and technical problems fixed.
2.9. Ethics review and data protection
This RCT was executed in compliance with the Helsinki Declaration and approved by the Canton of Zurich Ethics Committee on February 2, 2015 (KEK-ZH-No. 2014-0611). A separate data protection page, the link to which is always visible, provides information about the following: 1) how Snow Control 2.0 adheres to the Swiss Data Protection Law; 2) the extensive use of cookies and the option to disallow them; 3) an explanation about server log-files and confirmation that IP addresses will never combined with any other data that are assessed during participation; and 4) the nonuse of any third party interfaces, like analytical tracking software, social plugins of third parties, etc.
2.10. Subject recruitment
The study population was recruited through the revised Snow Control 2.0 website, to which a promotional link was provided on several websites of local outpatient treatment centers, and websites with nightlife prevention offers. In addition, advertisements were placed in Internet-forums and newspapers. As an incentive, we offered, to all participants who filled out all assessments, a 40 Euro online voucher and participation in a lottery for a 400 Euro online voucher, with the option of donating the corresponding value to a charitable organization.
2.11. Inclusion/exclusion criteria and rationale
For all inclusion and exclusion criteria (see Table 1), we relied on study participants' self-reported data.
Table 1.
Inclusion and exclusion criteria.
| Inclusion criteria | Rationale |
|---|---|
| Minimal age of 18 years | To ensure a minimal age of participation |
| Cocaine use >2 occasions over the last 30 days | To also include occasional users and expand study validity |
| Exclusion criteria | Rationale |
| Participation in other psycho-social or pharmacological treatments for the reduction/cessation of cocaine use | To avoid confounding treatment effects |
| Opioid use over the past 30 days (exception: substitution maintenance treatment for opioid dependence without heroin use) | To avoid confounding drug effects |
| Prior treatment for cardiovascular problems or apoplexy | To prevent subjects with these health problems from entering the study |
2.12. Consent procedure and registration
The entire informed consent and registration procedure could be fully self-administered. The website explained the study's rationale and informed potential users about the following: (1) study inclusion and exclusion criteria (see Table 1); (2) the three different study arms and how each participant had an equal chance of being assigned to any one of them; (3) potential risks of participation; (4) safety arrangements in place, both during and after the study; (5) the inability of Snow Control (with or without chat counseling) to replace face-to-face therapy for problematic cocaine use; and (6) circumstances that would require them to contact their general practitioner or another medical professional. Weekly access to the internet and a certain level of internet literacy was recommended, but not a strict requirement. Moreover, an emergency list was introduced and made accessible throughout the intervention via the menu item “Help Me”. Study participants also were informed that the Canton of Zurich Ethics Committee had approved the study. Furthermore, participants were informed about their right to withdraw from the study at any time without negative consequences, except for the loss of study compensation. After this information was provided, they were directed to the user registration page, where they needed to tick boxes to give informed consent and confirm that they fulfilled all inclusion and exclusion criteria. The entire baseline assessment was web-based and self-administered. Participants who claimed to fulfill the inclusion/exclusion criteria at registration, but then were found not to satisfy them completely, on baseline assessment, still were automatically considered study participants; but, later, during the data analysis phase, the were manually eliminated from the data pool. Completion of the baseline assessment triggered a subject's random assignment and set their study start time.
2.13. Randomization and group allocation
After the baseline assessment, participants were randomly assigned, in approximately a 1:1:1 ratio, to one of the three study arms. As we offered full transparency in all three study arms, we anticipated that some participants might decide to register another account, in an effort to change their assignment and access a different study arm. In such cases, the participant remained in their initially-assigned study arm for the remainder of the day, based upon his or her IP address.
2.14. Power calculation
We expected small-to-medium effect sizes of at least 0.30 (Cohen's d) between t0 and t2, when we compared the reduction of the amount of cocaine used by participants in intervention group 2 (web-based self-help intervention without chat counseling) against waiting list controls. When we compared intervention group 1 and the waiting list controls, we expected to the reduction of cocaine use in this active group to, if anything, be slightly higher than in intervention group 2; as such, we considered the former comparison to be more relevant, and based our sample size estimate on it. A sample size of n = 144 in each study group was expected to generate 95% confidence and 80% power (F-test, df = 2, α = 5%) to detect this difference, based upon calculations. Thus, we aimed to recruit a total of 432 (3 × 144) study participants overall (Schaub et al., 2015a).
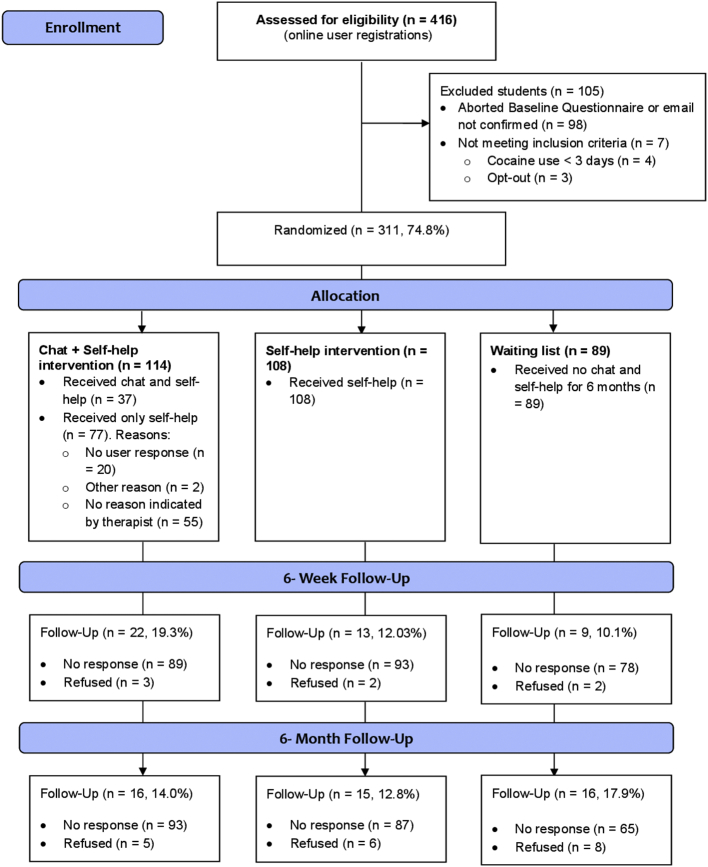
2.15. Trial flow
Fig. 2 provides an overview of the trial's flow. If participants successfully completed the baseline assessment (t0), they were randomly assigned to one of the three study arms and informed accordingly (no blinding). Subjects in study arms 1 and 2 were started on the introductory module, while controls (arm 3) were informed that they would be placed on a waiting list and given access to the web-based self-help intervention in six months.
Fig. 2.
CONSORT-EHEALTH trial flowchart: overview of participant flow.
The follow-up assessments at t1 and t2 were performed in three steps: As the first step, participants received an automatic email with an invitation to either the 6-week (t1) or 6-month (t2) follow-up assessment, each also announcing either the end of the program or study, respectively. If participants failed to fill out either of the web-based assessments after three reminders, as a second step they were contacted via a pre-announcement SMS and subsequent telephone call to be interviewed by study collaborators. Study collaborators tried this up to four times. Only participants who could not be reached after a minimum of four times were considered non-responders. If participants were reached, but refused the telephone interview, as a third step, they were offered an interview limited to the primary outcome only. If they also refused this and had not completed their questionnaire on-line in the interim, they were considered an “active refuser”.
2.16. Outcome measures
All outcomes were measured via web-based questionnaires that had not explicitly been validated for online use. Some questionnaires were mandatory (see Table 2), which means that the participant could not proceed without responding to all questions. None of the responses could be edited or re-submitted by users after their initial entry.
Table 2.
Overview of measurements and instruments.
| Assessments/instruments | Baseline | 6-week follow-up | 6-month follow-up | Mandatory3 |
|---|---|---|---|---|
| Socio-demographics | x | Yes | ||
| Quantity of cocaine use1) | x | x | x | Yes |
| Past 7 days cocaine use | x | x | x | Yes |
| Cocaine-free days1) | x | x | x | Yes |
| Severity of Dependence Scale (SDS) | x | x | x | Yes |
| FDA | x | x | x | No |
| Mental Health Inventory (MHI-5) | x | x | No | |
| Adult Self-Report Scale (ASRS) | x | No | ||
| Working Alliance Inventory (WAI-SR2)) | x | No | ||
| Client Satisfaction Questionnaire (CSQ-4) | x | No |
1) 7-day point estimates of the quantity, in grams, and frequency of cocaine use were derived from the consumption diary, assessed daily utilizing data from the preceding seven days.
2) This instrument only was applied to Intervention Group 1 (self-help plus chat therapy).
3) ‘Mandatory’ means the user could not proceed without giving complete answers.
The primary outcome measure was the weekly quantity of cocaine used, in grams, which is considered a novel measure for this type of intervention in problematic cocaine users (Robinson et al., 2014). In addition, the following secondary outcome measures were assessed: (1) the number of days on which cocaine was used over the past 30 days, calculated using the timeline follow-back assessment (Robinson et al., 2014); (2) Severity of Dependence Scale (SDS), a 5-item questionnaire that provides a score indicating one's severity of cocaine dependence (Gossop et al., 1995); (3) Substance History Questionnaire (German: Fragebogen Substanzanamnese, FDA), to ascertain the individual subject's lifetime and past-month frequency of use and patterns of use, in accordance with the ICD-10; this measure was derived from the European Addiction Severity Index (EuropeASI) (Gsellhofer et al., 1997); (4) short version of the Mental Health Inventory (MHI-5) (Rumpf et al., 2001) to assess recent mental distress and self-diagnosed depression; (5) Adult Self-Report Scale (ASRS), an adult self-screening questionnaire for attention deficit hyper-activity disorder (ADHD) (Kessler et al., 2005); (6) Working Alliance Inventory (WAI-SR), a 12-item self-report questionnaire that consists of three subscales initially designed to assess the working alliance between a patient and therapist (Wilmers et al., 2008); in the current study, its composite score was used as a global measurement of working alliance; and (7) client satisfaction with the intervention, investigated using the Client Satisfaction Questionnaire (CSQ-4), a brief, user-friendly instrument that has been tested in numerous studies with diverse client samples (Schmidt et al., 1989). For a complete list of these measurements and instruments, see Table 2.
Further markers were created for study arms 1 and 2. Retention was assessed as the percentage of days on which the consumption diary was filled out; and participation in the self-help intervention, as the number of completed modules or extent of progression through each module. Further measurement details can be found in the study protocol (Schaub et al., 2015a).
2.17. Data analysis
Data were initially examined for outliers. Then, baseline differences were identified between participants in the three study arms by Pearson chi-square analysis for categorical variables, and by analysis of variance (ANOVA) for continuous variables. The same tests were applied to examine whether participants who answered the 6-month follow-up questionnaires differed from those who were lost to follow-up.
Due to our low follow-up rates, which made reliable multiple imputations impossible, we abandoned our a priori decision to conduct intention-to-treat (ITT) analyses, electing to proceed solely employing complete case analyses and, again deviating from our study protocol (Schaub et al., 2015a), to additionally analyze the data available at 6 weeks (intervention completion), where low follow-up rates had already crystallized.
First, we conducted Generalized Estimating Equation (GEE) analyses to investigate longitudinal changes in primary and secondary outcomes over the study period of six months. Next, we computed differences between the baseline and follow-up assessments for primary and secondary outcome variables, and assessed for differences between study arms using linear regression models. In all models, we included the corresponding baseline variables as a control variable. Results with a Type I error rate of p < 0.05 during two-sided tests were considered statistically significant.
Finally, we compared treatment participation (percentage of module completion), treatment retention (proportion of days diary filled out), and client satisfaction for study arms 1 and 2 using chi-square analysis and t-tests at week 6.
All analyses were performed using the statistical software programs SPSS version 22 and R version 3.3.
3. Results
3.1. Study participation
Recruitment had to be stopped without reaching the target sample size of 432 (Schaub et al., 2015a), as the third-party funding was depleted and the maximal project time afforded by the funding organization ended. The progression of study participants is depicted in Fig. 2. Between October 2015 and 2017, a total of 416 users registered an online account. Of these,
311 (74.8%) successfully confirmed their email address, completed the baseline assessment, and were eligible for study participation. They were randomly allocated to one of the three study arms.
However, the 6-week and 6-month follow-up assessments were completed by only 44 (14.1%) and 47 (15.1%) of the participants, respectively, despite the three-step assessment procedure. By study arm, 22 (19.3%) participants in the intervention group with chat, 13 (12.0%) in the intervention group without chat, and nine (10.1%) controls completed the 6-week assessment. The follow-up rates for the 6-month assessment were similarly low: just 16 (14.0%) respondents in study arm 1, 15 (12.8%) in study arm 2, and 16 (17.9%) in study arm 3.
3.2. Participants' baseline characteristics
Participants' baseline characteristics are summarized in Table 3. Subjects were predominantly male (73%) and averaged 33 years old (SD = 7.6). Overall, 93.3% screened higher than the cut-off ≥3 on the SDS-scale for cocaine dependence, and 69.9% indicated at least one occasion of risky alcohol use within the past 30 days, defined as the consumption of five or more standard drinks. In addition, 83.4% screened positive for clinically-relevant depressive symptoms on the MHI-5 (<70), and 34.4% for adult ADHD at baseline on the ASRS. The only significant difference between the three study arms was detected for gender (Χ22 = 7.740, P = 0.02), with both intervention groups tending to have a greater percentage of male participants than the control group (Table 3).
Table 3.
Baseline characteristics of participants.
| Characteristics | Intervention 1 (Chat and self-help) (n = 114) |
Intervention 2 (Self-help only) (n = 108) |
Control group (Waiting list) (n = 89) | Total (n = 311) |
test value | P |
|---|---|---|---|---|---|---|
| Sex, n (%) | X22 = 7.740 | 0.02 | ||||
| Female | 30 (26.3) | 21 (19.4) | 33 (37.1) | 84 (27) | ||
| Male | 84 (73.7) | 87 (80.6) | 56 (62.9) | 227 (73) | ||
| Age in years, M (SD) | 33.5 (8.1) | 33.3 (7.4) | 32.3 (7.2) | 33.1 (7.6) | F2 = 0.679 | 0.51 |
| Age range, n (%) | X28 = 4.962 (n = 310) | 0.76 | ||||
| ≤20 years | 7 (6.2) | 4 (3.7) | 6 (6.7) | 17 (5.5) | ||
| 21–25 years | 10 (8.8) | 11 (10.2) | 8 (9) | 29 (9.3) | ||
| 26–30 years | 24 (21.2) | 20 (18.5) | 23 (25.8) | 73 (21.7) | ||
| 31–35 years | 28 (24.8) | 32 (29.6) | 27 (30.3) | 95 (28.2) | ||
| 36+ years | 44 (38.9) | 41 (38) | 25 (28.1) | 117 (34.7) | ||
| Highest education, n (%) | X28 = 9.276 | 0.32 | ||||
| Primary school | 6 (5.5) | 7 (6.6) | 9 (10.2) | 22 (7.3) | ||
| Apprenticeship | 43 (39.4) | 53 (50) | 30 (34.1) | 126 (41.6) | ||
| Secondary school | 13 (11.9) | 10 (9.4) | 16 (18.2) | 39 (12.9) | ||
| Technical college | 27 (24.8) | 23 (21.7) | 19 (21.6) | 69 (22.8) | ||
| University | 20 (18.3) | 13 (12.3) | 14 (15.9) | 47 (15.5) | ||
| Origin, n (%) | ||||||
| Canton of Zurich | 48 (42.1) | 30 (27.8) | 36 (40.4) | 114 (36.7) | X26 = 10.421 | 0.11 |
| Other Cantons | 46 (40.4) | 60 (55.6) | 44 (49.4) | 150 (48.2) | ||
| Germany | 17 (14.9) | 17 (15.7) | 9 (10.1) | 43 (13.8) | ||
| Other countries | 3 (2.6) | 1 (0.9) | 0 (0) | 4 (1.3) | ||
| SDSa, M (SD) | 8.3 (2.6) | 8.2 (2.7) | 8.7 (2.7) | 8.4 (2.7) | F2 = 0.918 | 0.40 |
| Weekly quantity of cocaine use, in grams, M (SD) | 3.5 (3.4) | 4.0 (3.6) | 4.1 (3.7) | 3.8 (3.5) | F2 = 0.890 | 0.41 |
| Days of cocaine use over past 30 days, n (%) | 11.7 (7.9) | 11.9 (7.8) | 13.3 (8.2) | 12.2 (7.9) | F2 = 1.085 | 0.34 |
| Number of years of cocaine use, M (SD) | 6.6 (5.4) | 7.1 (6.3) | 6.9 (6.3) | 6.9 (5.9) | F2 = 0.170 (n = 300) | 0.84 |
| Days of other substance use over past 30 days, M (SD) | ||||||
| Risky alcohol useb | 8.2 (8.8) | 6.6 (7.9) | 6.6 (8.2) | 7.2 (8.3) | F2 = 0.903 (n = 215) | 0.41 |
| Cannabinoids | 6.1 (9.9) | 6.3 (10.5) | 7.9 (11.3) | 6.6 (10.5) | F2 = 0.572 (n = 207) | 0.57 |
| Amphetamines | 0.9 (2.3) | 2.1 (4.9) | 2.6 (6.9) | 1.9 (4.9) | F2 = 2.003 (n = 206) | 0.14 |
| Relaxants | 2.7 (7.4) | 2.5 (8.5) | 0.9 (4.6) | 2.2 (7.2) | F2 = 0.967 (n = 179) | 0.38 |
| Hallucinogens | 0.1 (0.2) | 0.2 (0.5) | 0.2 (0.9) | 0.1 (0.6) | F2 = 0.938 (n = 176) | 0.39 |
| Heroin | 0.5 (3.8) | 0.0 (0.1) | 0 (0) | 0.2 (2.3) | F2 = 1.016 (n = 176) | 0.36 |
| Methadone | 0 (0) | 0.5 (3.7) | 0.6 (4.3) | 0.4 (3.2) | F2 = 0.578 (n = 174) | 0.56 |
| MHI-5c, M (SD) | 49.4 (18.7) | 50.5 (17.1) | 49.4 (18.8) | 49.8 (18.1) | F2 = 0.130 | 0.88 |
| ADHDd, n (%) | 40 (25.4) | 32 (31.1) | 34 (40.5) | 106 (35.3) | X22 = 1.793 | 0.41 |
aSeverity of Dependence Scale (SDS) scores range from 0 to 15, with a screening cut-off of ≥3 for cocaine dependence. b Risky alcohol use was defined as five or more standard drinks per day. A standard drink was defined as 5 cl spirits, 15–20 cl wine, or 22–45 cl beer. cMental Health Inventory (MHI-5): higher values represent improved symptoms. MHI-5 values range from 0 to 100 with a cut-off of <70 for clinically-relevant symptoms. d ADHD according to the World Health Organization Adult ADHD Self-Report Scale (ASRS) designed for ADHD screening in the general population.
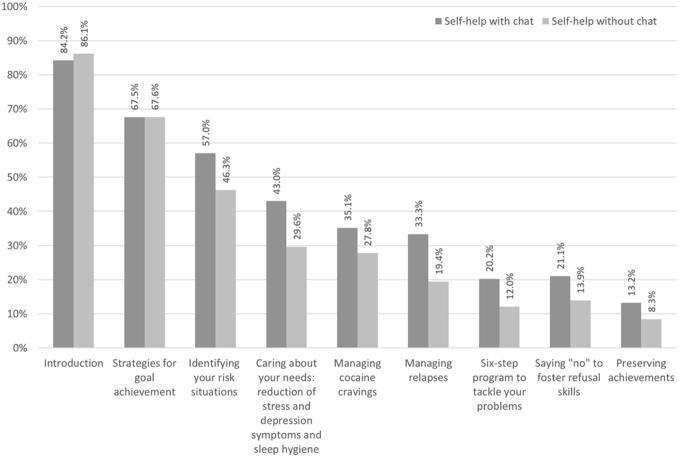
3.3. Intervention attrition, participation, retention and satisfaction
There were no systematic differences with respect to baseline characteristics in participants who responded at follow-up and those who failed to respond to follow-up across the three study arms. Concerning intervention participation (module completion rate), there were differences between Intervention Group 1 (self-help with chat) and Intervention Group 2 (self-help without chat). As Fig. 3 depicts, module completion rates were higher for participants receiving intervention 1 than 2, despite the introduction and module 1 (Strategies for goal achievement). Participants in Intervention Group 1 not only completed more modules (M = 3.43, SD = 2.80 versus M = 2.71, SD = 2.44), they also read a larger proportion of the modules that they did not complete, relative to participants in the other intervention group (Fig. 3). In addition, they exhibited significantly-higher intervention retention (t220 = 2.514, P < 0.00), filling out their diary on 29.4% of days, versus just 18.9% in Intervention Group 2. Out of 114 participants who partook of intervention 1 and were offered chat counseling, 37 (32.5%) participated in one or more chat-counseling sessions. They seemed particularly motivated, relative to those who were offered chat options but did not use them, completing significantly more modules (M = 5.35, SD = 2.63, N = 37 versus M = 2.51, SD = 2.39, N = 77; t112 = −5.756, P < 0.00), and responding significantly more (t112 = 5.713, P < 0.00) at follow-up assessment (37.8%) than those in Intervention Group 1 who did not book a chat appointment (2.6%); however, they did not differ in any of the other assessed variables, including retention rate (t112 = 8.347, P = 0.14).
Fig. 3.
Module completion rate (yes vs. no) for intervention 1 (self-help with chat) and intervention 2 (self-help without chat).
Overall, the number of modules completed was associated with the number of cocaine-use days at baseline. Participants in Intervention Groups 1 and 2 who reported fewer baseline-use days, completed slightly more modules than those who reported more use days at baseline (t307 = 1.904, P = 0.048).
Concerning satisfaction with the intervention, as measured using the CSQ-4, there were no differences between participants who were offered chat counseling and those offered self-help only (complete case analysis, CCA: t22 = 0.252, P = 0.80).
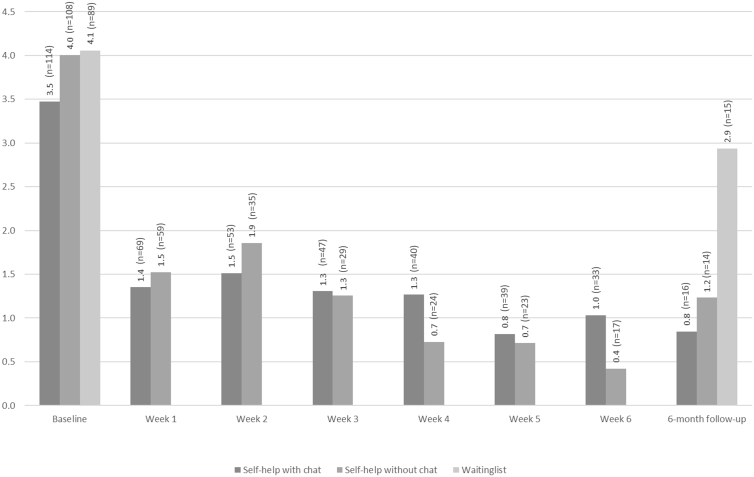
3.4. Main outcome
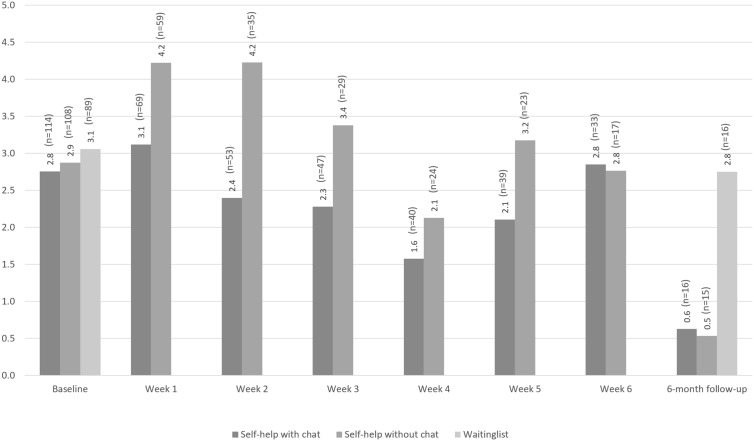
Fig. 4 depicts the mean quantity of cocaine used per week (main outcome) and Fig. 5 the mean numbers of cocaine use days per week, both based on CCA. Within all three study arms, there were significant reductions in the quantity of cocaine use over time (Table 4). However, frequency of cocaine use only decreased significantly in the two intervention groups and not in controls (Table 4). There were no significant differences in the magnitude of change in the quantity of cocaine use per week between any of the three study arms, either between baseline and 6-week follow-up, or between baseline and 6-month follow-up (Table 5).
Fig. 4.
Weekly quantity of cocaine use, in grams, according to baseline, consumption diary and follow-up estimates for all three study arms, based on complete case analysis.
Fig. 5.
Cocaine use days per week, according to baseline, consumption diary and follow-up estimates for all three study arms, based complete case analysis.
Table 4.
Number of participants and mean and standard deviation changes in primary and secondary outcomes between baseline, 6-week and 6-month follow-up (complete case analysis).
| Intervention 1 |
Intervention 2 |
Control group |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Chat and self-help) |
(self-help only) |
(waiting list) |
||||||||||
| Baseline n = 114 | 6 weeks n = 22 |
6 months n = 16 | P | Baseline n = 108 | 6 weeks n = 13 |
6 months n = 15 |
P | Baseline n = 89 |
6 weeks n = 9 |
6 months n = 16 |
P | |
| Weekly quantity of cocaine use, in grams M (SD) | 3.47 (3.38) | 0.35 (0.57) | 0.85 (1.04) | <0.001 | 4.00 (3.59) | 1.43 (2.23) | 1.23 (2.18) | <0.001 | 4.06 (3.68) | 2.33 (2.35) | 2.94 (4.80) | <0.001 |
| Frequency of cocaine use in days per month M (SD) | 11.67 (7.94) | 4.36 (5.89) | 3.00 (2.80) | <0.001 | 11.97 (7.80) | 7.38 (7.64) | 3.03 (4.18) | <0.001 | 13.26 (8.17) | 12.56 (10.67) | 11.00 (10.70) | 0.67 |
| SDS a (Range 0–15) M (SD) | 8.32 (2.57) | 6.26 (2.88) | 5.93 (3.22) | <0.001 | 8.22 (2.71) | 6.21 (2.72) | 5.50 (2.73) | <0.001 | 8.72 (2.76) | 7.47 (2.96) | 8.33 (3.39) | 0.21 |
| MHI-5bM (SD) | 49.43 (18.70) | – | 55.33 (19.71) | 0.03 | 50.53 (17.06) | – | 45.13 (20.84) | 0.61 | 49.37 (18.86) | – | 39.13 (16.75) | 0.72 |
| Alcohol use days, last 30 days M (SD) | 13.29 (16.59) | 9.39 (6.01) | 4.30 (5.19) | <0.001 | 12.75 (8.81) | 7.79 (7.98) | 6.50 (8.12) | 0.003 | 11.84 (8.60) | 9.50 (9.73) | 8.00 (3.69) | 0.048 |
| Alcohol use days, last 30 days (risky c) M (SD) | 8.20 (8.80) | 2.74 (3.68) | 1.40 (3.27) | <0.001 | 6.60 (7.94) | 3.63 (6.25) | 3.38 (5.97) | 0.04 | 6.59 (8.23) | 6.56 (9.25) | 2.86 (3.98) | 0.11 |
Note. Generalized Estimating Equation (GEE) models per study arm for each primary and secondary outcome with time as predictor.
Severity of Dependence Scale (SDS) scores range from 0 to 15 with a screening cut-off of ≥3 for cocaine dependence.
Mental Health Inventory (MHI-5): higher values represent improved symptoms. MHI-5 values range from 0 to 100 with a cut-off of <70 for clinically-relevant symptoms. c Risky alcohol use was defined as five or more standard drinks per day.
Table 5.
Intervention effects for primary and secondary outcomes based on complete case analysis between baseline (T1), 6-week (T2) and 6-month (T3) follow-up.
| T1-T2 |
T1-T3 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean a | P b | dc | 95% CI | Meana | P b | dc | 95% CI | |||||
| Self-help with chat (n = 114) vs. self-help without chat (n = 108) | ||||||||||||
| Quantity of cocaine use | −1.02 | −0.37 | −1.06 | – | 0.34 | −2.23 | −0.74 | −1.46 | – | 0.02 | ||
| Frequency of cocaine use | −3.19 | −0.63 | −1.32 | – | 0.08 | −1.34 | −0.18 | −0.88 | – | 0.53 | ||
| SDS | 0.07 | 0.03 | −0.56 | – | 0.61 | −0.71 | −0.23 | −0.93 | – | 0.48 | ||
| MHI-5 | – | – | – | – | 13.40 | 0.65 | −0.09 | – | 1.36 | |||
| Alcohol use days, last 30 days | 4.70 | 0.047 | 0.66 | 0.00 | – | 1.30 | −0.88 | −0.14 | −1.11 | – | 0.85 | |
| Alcohol use days, last 30 days (risky) | −1.20 | −0.18 | −0.86 | – | 0.51 | 0.24 | 0.08 | −1.02 | – | 1.16 | ||
| Self-help with chat (n = 114) vs. waiting list (n = 89) | ||||||||||||
| Quantity of use | −1.46 | −0.47 | −1.25 | – | 0.33 | −1.68 | −0.44 | −1.14 | – | 0.29 | ||
| Frequency of use | −0.94 | −0.13 | −0.90 | – | 0.65 | −6.69 | 0.046 | −0.74 | −1.43 | – | 0.00 | |
| SDS | −0.81 | −0.31 | −0.92 | – | 0.30 | −1.47 | −0.46 | −1.17 | – | 0.28 | ||
| MHI-5 | – | – | – | – | 12.03 | 0.69 | −0.06 | – | 1.39 | |||
| Alcohol use days, last 30 days | −3.36 | −0.37 | −1.05 | – | 0.33 | −6.04 | −1.00 | −2.04 | – | 0.18 | ||
| Alcohol use days, last 30 days (risky) | −7.18 | 0.005 | −1.06 | −1.81 | – | −0.24 | −2.83 | −0.73 | −1.84 | – | 0.49 | |
| Self-help without chat (n = 114) vs. waiting list (n = 89) | ||||||||||||
| Quantity of use | −0.44 | −0.18 | −1.03 | – | 0.68 | 0.55 | 0.16 | −0.58 | – | 0.88 | ||
| Frequency of use | 2.25 | 0.28 | −0.58 | – | 1.12 | −5.35 | −0.64 | −1.34 | – | 0.10 | ||
| SDS | −0.88 | −0.36 | −1.01 | – | 0.31 | −0.75 | −0.22 | −0.92 | – | 0.50 | ||
| MHI-5 | – | – | – | – | −1.38 | −0.07 | −0.76 | – | 0.63 | |||
| Alcohol use days, last 30 days | −8.06 | 0.01 | −0.85 | −1.58 | – | −0.08 | −5.17 | −0.96 | −2.01 | – | 0.21 | |
| Alcohol use days, last 30 days (risky) | −5.98 | 0.02 | −1.09 | −1.86 | – | −0.26 | −3.07 | −0.74 | −1.81 | – | 0.44 | |
| Self-help with and without chat combined (n = 222) vs. waiting list (n = 89) | ||||||||||||
| Quantity of use | −3.60 | −0.74 | −1.48 | – | 0.02 | −0.64 | −0.18 | −0.80 | – | 0.44 | ||
| Frequency of use | 0.24 | 0.04 | −0.70 | – | 0.77 | −6.04 | 0.02 | −0.73 | −1.34 | – | −0.10 | |
| SDS | −0.84 | −0.33 | −0.88 | – | 0.23 | −0.61 | −0.17 | −0.78 | – | 0.45 | ||
| MHI-5 | – | – | – | – | 5.11 | 0.25 | −0.36 | – | 0.85 | |||
| Alcohol use days, last 30 days | −5.41 | 0.04 | −0.62 | −1.25 | – | 0.03 | −5.60 | −0.96 | −1.90 | – | 0.05 | |
| Alcohol use days, last 30 days (risky d) | −6.60 | 0.004 | −1.04 | −1.71 | – | −0.33 | −2.96 | −0.82 | −1.78 | – | 0.21 | |
Note. Linear regression models with differences between baseline and follow-up as outcome and study arms as predictors.
aNegative values indicate greater symptom reduction in the first group or groups relative to the second group, b = controlling for pre-treatment scores (T1), c = Cohen's d,d Risky alcohol use was defined as five or more standard drinks per day.
3.5. Secondary outcomes
Significant changes over time were observed for all secondary outcomes for different study arms based on CCA (Table 4). Participants who received intervention 1 (self-help and chat) scored lower on the severity on dependence scale (SDS) (P < 0.001), reported higher mental health (MHI) (P = 0.03), and decreased both their overall (P < 0.001) and risky alcohol use (P < 0.001). Participants who received intervention 2 (self-help without chat) also decreased in their dependency scores (P < 0.001), and both overall (P = 0.003) and risky alcohol use (P = 0.04), but did not exhibit any improvement in their mental health. Contrary to participants receiving either intervention, waiting list controls showed a significant improvement only in overall alcohol use (P = 0.048), and not in the severity of dependence, their mental health, or risky alcohol use (Table 4). Significant differences between the three study arms were detected in the frequency of cocaine use, as well as in alcohol use patterns in the CCA at follow-up. At 6-month follow-up, participants who received intervention 1 reduced their frequency of cocaine use more than controls (Cohens' d (d) = −0.74, CI: −1.43;0.00, P = 0.046). Also, relative to waiting list controls, greater reductions were detected in days of risky alcohol use over the past 30 days in both Intervention Group 1 (d = −1.06, confidence interval (CI): −1.81; −0.24, P = 0.005) and Intervention Group 2 participants (d = −1.09, CI: −1.86; −0.26, P = 0.02) at 6-week follow-up. Participants in Intervention Group 2 also exhibited greater reductions in overall alcohol use over the last 30 days than both participants in Intervention Group 1 (d = 0.66, CI: 0.00;1.30, P = 0.047) and controls (d = −0.85, CI: −1.58; −0.08, P = 0.01) at 6-week follow-up. Lastly, significant differences were detected between the two intervention groups combined and controls in the frequency of cocaine use at 6-month follow-up and overall alcohol use and risky alcohol use at 6-week follow-up. Participants who received the intervention reported 1) less frequent cocaine use (d = −6.04, CI: −1.34;-0.10, P = 0.02), 2) less overall alcohol use (d = −5.41, CI: −1.25; 0.03, P = 0.04), and 3) less risky alcohol use (d = −6.60, CI: −1.71; −0.33, P = 0.004) (Table 5).
3.6. Safety
Over the course of the entire study, only three of 308 (1.6%) participants contacted one of the outpatient addiction clinics from the Arud Centers for Addiction Medicine. None had to be treated as an emergency case; one wished to be referred for inpatient cessation treatment. Moreover, none of the involved therapists, psychiatrists or researchers became aware of any adverse or serious adverse events related to the Snow Control 2.0 study, as reported by other addiction counseling services.
4. Discussion
4.1. Principal findings
For the present study, we recruited a considerable number of cocaine misusers and cocaine users with early cocaine dependence, as well as high levels of comorbidity from risky drinking, depression symptoms, and ADHD, who otherwise were not yet in treatment for a theory-based and pretested internet intervention. Significant decreases in cocaine use were observed for all study arms. However, the frequency of cocaine use decreased only in the two active intervention groups. Moreover, while participants receiving self-help plus chat reported similar improvements to the self-help only group in the severity of their cocaine dependence, and their overall and risky alcohol use, improvements in mental health were observed exclusively in the self-help plus chat group. Meanwhile, waiting list controls exhibited improvement solely in overall alcohol use, and in none of the other secondary outcomes (severity of dependence, mental health, risky alcohol use).
Although the within-study group comparisons indicate superiority of the two active conditions over the control condition, we cannot appropriately answer questions regarding their superiority reducing weekly quantity of cocaine use in grams (main outcome) or for some of the secondary outcomes, because a very high dropout rate compromised the statistical power of the study. Moreover, the large quantity of missing data and inherent bias secondary to losses to follow-up rendered any meaningful data imputation process virtually impossible.
Accessing participants for follow-up assessments was very difficult, resulting in very low follow-up rates, between 13 and 18%, including some active follow-up refusals (6% overall). In similarly-designed studies, we achieved much higher follow-up rates of 38% among cannabis misusers (Schaub et al., 2013; Schaub et al., 2015b) and 61–62% follow-up rates in alcohol misusers (Boß et al., 2018; Schaub et al., 2016), with almost no active study-participation refusals. While cannabis use is punished by fine in Switzerland, narcotics laws dictate that possession of cocaine use results in penalization and criminalization. For some participants, their cocaine use reported in the diary even reached quantities, in later weeks that would no longer count as possession, but as cocaine dealing, such that they might have increasingly feared prosecution. This could explain why we initially reached many cocaine misusers, but many of them dropped out later and were difficult to reach for follow-up assessments. The perceived increased risk of serious criminalization, in combination with comparatively-high mistrust levels in cocaine misusers (Williamson et al., 1997), might have increased the drop-out rates; for example, cocaine users typically know that the police intercept mobile phones on spec and many initially provided their mobile phone number for follow-up assessments in case they could not be reached by e-Mail. A further explanation might be the frequently-observed comorbidity with ADHD (34.4% screen positive) that might have increased intervention dropouts and decreased reliability with follow-up appointments (Soendergaard et al., 2016). However, we assume that there might be other unknown, but important reasons that need to be identified. A detailed content analysis of the chat sessions might have provided additional insights into the dropout problems and difficulties with follow-up, but would have gone beyond the scope of the present study. As for the chat rates, they were – contrary to the dropout and follow-up problems – superior (32%) to those we observed in our very similarly-designed study involving cannabis misusers (21% (Schaub et al., 2013; Schaub et al., 2015b)). Ultimately, we must admit that it was very difficult for us to entice cocaine misusers into guided self-help who were from the general population and not otherwise in treatment for their cocaine problem.
This is particularly unfortunate, since we registered almost daily, new cocaine users from our target group without any recruitment efforts when we finished our study and made our intervention available as an unguided self-help intervention not requiring study participation. This registration tendency continued, at a somewhat lower level, but still at a much higher rate than during the active study recruitment period, for the next 12 months after recruitment was terminated. Thus, the need for an intervention like Snow Control is continuous. This raises the ethical question: is it ethical to continue providing Snow Control after only demonstrating within-group differences? We hold that, as long as the treatment gap for cocaine misusers exists and there are no more attractive and effective online or offline alternatives, Snow Control should remain online.
Limitations of the current study that merit consideration can be summarized as follows: First, we did not succeed at attaining the higher participation rates or more complete follow-up initially intended with the study protocol. Second, we did not reach our target sample size and, thus, the study is underpowered. Third, we did not validate cocaine use, since we did not want to limit study participation to those willing to provide, for example, urine or hair samples, and did not want to restrict the study's external validity.
4.2. Implications for future studies
Given our experience with the current study, alternative ways need to be developed to assess the treatment of cocaine misusers, and we believe that our experience should be considered a starting point. A qualitative study is warranted to investigate why so many participants dropped out of our intervention groups and why, beyond the reason described earlier regarding fear of prosecution, it was so hard to reach participants for follow-up assessments. Although we had experience in a previous study involving cocaine misusers (Schaub et al., 2012), and developing the intervention involved piloting with individuals from the target population (Schaub et al., 2015a), we did not expect these problems to be of this magnitude. Moreover, these problems were less pronounced during the first couple of years of the study and became more explicit during the last year of recruitment, with no obvious reason for this trend.
Some authors suggest employing a more user-centered design and individualization in programs for addicts to improve their commitment and adherence (Fleming et al., 2016; de Beurs et al., 2017). In this way, a similar program could permit participants to choose their favorite counselor within a team introduced online, and their preferred mode of communication (chat vs. mailing system vs. additional phone calls, etc.). The introduction of serious gaming and persuasive technology could further augment results (Fleming et al., 2016), but these have not been tested for internet interventions targeting cocaine users, to date.
Additionally, more effective data collection approaches are needed for future similar studies to reduce the rate of participant dropout. We recommend linking follow-up assessments (data collection) with therapeutic content that might be perceived as meaningful and useful by participants (e.g., a pre-announced booster module that aims to preserve long-term success).
Replicating the study in a different setting – e.g., in a country like Portugal, where the possession of small amounts of cocaine is not criminalized or penalized – should also be considered. This might help to prevent some cocaine users with high levels of mistrust in authority, as well as those whose cocaine use approaches the quantities associated with dealing in other countries, from dropping out. Similarly, replication in countries like the U.S., where contingency management is widely accepted and could be combined with online CBT, could be worthwhile and might increase intervention adherence.
5. Conclusions
Many cocaine misusers from the general population and not otherwise in treatment were reached utilizing a CBT-based online intervention and reduced their cocaine use. However, due to the high percentage of dropouts and serious difficulties reaching them for follow-up assessments, no conclusions can be drawn regarding inter-group study arm differences.
Abbreviations
ANOVA analysis of variance
ARUD Arud Centers for Addiction Medicine
ASRS Adult ADHD Self-Report Scale
BSM behavioral self-management
CBT cognitive behavioral therapy
CC complete cases
CCA complete case analyses
CRA community reinforcement approach
CSQ-4 customer satisfaction questionnaire
EuropeASI European Addiction Severity Index
EMCDDA European Monitoring Centre for Drugs and Drug Addiction
FDA Fragebogen Substanzanamnese (questionnaire for the assessment of substance use history)
ISGF Swiss Research Institute for Public Health and Addiction
ITT intention-to-treat
MET motivational enhancement techniques
MHI-5 mental health inventory
MI motivational interviewing
N/A not applicable
RCT randomized controlled trial
SDS severity of dependence scale
SPSS statistical package for the social sciences
SSL secure sockets layer
TLFB time-line follow back
WAI-SR Working Alliance Inventory - Short Revised
Conflicts of interest
The current authors created the intervention. Otherwise, the authors have no competing interests to declare. This trial is registered at Current Controlled Trials and is traceable as ISRCTN12205466.
Author contributions
MPS was responsible for the study design. MPS, AW and RPC prepared the first draft of the paper. MPS, AW, LS, and SH contributed to the development of the interventions for study arms one and two. AW programmed and implemented the study website, Snow Control 2.0. All the authors helped to recruit subjects and approved the final version of the manuscript submitted for publication.
Acknowledgments
The Swiss National Science Foundation [grant number 100019_156507/1] provided funding for this study. The authors wish to extend particular appreciation to the staff of the Arud centers for addiction medicine in Zurich, Switzerland and to their clients, who voluntarily participated in the pilot testing of arms 1 and 2 of the Snow Control 2.0 study. Moreover, special thanks go to Tantiana Imhof, Ivana Ilieva and Julia Vollrath-Roediger for their tremendous work following up the study participants.
Contributor Information
Michael P. Schaub, Email: michael.schaub@isgf.uzh.ch.
Raquel Paz Castro, Email: raquel.paz@isgf.uzh.ch.
Andreas Wenger, Email: andreas.wenger@isgf.uzh.ch.
Christian Baumgartner, Email: christian.baumgartner@isgf.uzh.ch.
Lars Stark, Email: l.stark@arud.ch.
David D. Ebert, Email: david.ebert@fau.de.
Boris B. Quednow, Email: quednow@bli.uzh.ch.
Severin Haug, Email: severin.haug@isgf.uzh.ch.
References
- Beck F., Guignard R., Legleye S. Does computer survey technology improve reports on alcohol and illicit drug use in the general population? A comparison between two surveys with different data collection modes in France. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0085810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beurs D., van Bruinessen I., Noordman J., Friele R., van Dulmen S. Active involvement of end users when developing web-based mental health interventions. Front. Psychiatry. 2017;8 doi: 10.3389/fpsyt.2017.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankers M., Koeter M.W.J., Schippers G.M. Internet therapy versus internet self-help versus no treatment for problematic alcohol use: a randomized controlled trial. J. Consult. Clin. Psychol. 2011;79(3):330–341. doi: 10.1037/a0023498. [DOI] [PubMed] [Google Scholar]
- Bock B.C., Graham A.L., Sciamanna C.N., Krishnamoorthy J., Whiteley J., Carmona-Barros R.…Abrams D.B. Smoking cessation treatment on the internet: content, quality, and usability. Nicotine Tob. Res. 2004;6(2):207–219. doi: 10.1080/14622200410001676332. [DOI] [PubMed] [Google Scholar]
- Boß L., Lehr D., Schaub M.P., Paz Castro R., Riper H., Berking M., Ebert D.D. Efficacy of a web-based intervention with and without guidance for employees with risky drinking: results of a three-arm randomized controlled trial. Addiction. 2018;113(4):635–646. doi: 10.1111/add.14085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boumparis N., Karyotaki E., Schaub M.P., Cuijpers P., Riper H. Internet interventions for adult illicit substance users: a meta-analysis. Addiction. 2017;112(9):1521–1532. doi: 10.1111/add.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks A.C., Ryder D., Carise D., Kirby K.C. Feasibility and effectiveness of computer-based therapy in community treatment. J. Subst. Abus. Treat. 2010;39(3):227–235. doi: 10.1016/j.jsat.2010.06.003. [DOI] [PubMed] [Google Scholar]
- Carroll K.M., Kiluk B.D., Nich C., Gordon M.A., Portnoy G.A., Marino D.R., Ball S.A. Computer-assisted delivery of cognitive-behavioral therapy: efficacy and durability of CBT4CBT among cocaine-dependent individuals maintained on methadone. Am. J. Psychiatry. 2014;171(4):436–444. doi: 10.1176/appi.ajp.2013.13070987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry S.J. eHealth research and healthcare delivery. Beyond intervention effectiveness. Am. J. Prev. Med. 2007;32(5 SUPPL) doi: 10.1016/j.amepre.2007.01.026. [DOI] [PubMed] [Google Scholar]
- De Crescenzo F., Ciabattini M., D'Alò G.L., De Giorgi R., Del Giovane C., Cassar C., Janiri L., Clark N., Ostacher M.J., Cipriani A. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: a systematic review and network meta-analysis. PLoS Med. 2018;26(15):12. doi: 10.1371/journal.pmed.1002715. (e1002715) [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'zurilla T.J., Nezu A.M. Development and preliminary evaluation of the social problem-solving inventory. Psychol. Assess. 1990;2(2):156. [Google Scholar]
- EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) 2018. (Wastewater analysis and drugs: a European multi-city study) [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. (2016). European Drug Report 2016: Trends and Developments. European Monitoring of Drugs and Drugs Addiction. doi: 10.2810/88175. [DOI]
- Fendrich M., Johnson T.P., Wislar J.S., Hubbell A., Spiehler V. The utility of drug testing in epidemiological research: results from a general population survey. Addiction. 2004;99(2):197–208. doi: 10.1111/j.1360-0443.2003.00632.x. [DOI] [PubMed] [Google Scholar]
- Fleming T.M., de Beurs D., Khazaal Y., Gaggioli A., Riva G., Botella C., Baños R.M., Aschieri F., Bavin L.M., Kleiboer A., Merry S., Lau H.M., Riper H. Maximizing the impact of e-therapy and serious gaming: time for a paradigm shift. Frontiers in Psychiatry. 2016;7 doi: 10.3389/fpsyt.2016.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gmel G., Kuendig H., Notari L., Gmel C. 2014. Suchtmonitoring Schweiz - Konsum von Alkohol, Tabak und illegalen Drogen in der Schweiz im Jahr 2013. (Lausanne) [Google Scholar]
- Gossop M., Darke S., Griffiths P., Hando J., Powis B., Hall W., Strang J. The severity of dependence scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90(5):607–614. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- Gsellhofer B., Fahrner E.-M., Weiler D., Vogt M., Hron U., Platt J. In: European Addiction Severity Index EuropASI - Deutsche Version nach dem amerikanischen Original von T. McLellan, 5. Ed., 1992, und der europäischen Version EuropASI von. Kokkevi A., Hartgers Ch., Blanken P., Fahrner E.-M., Pozzi G., Tempesta E., Uchtenh A., editors. 1997. [Google Scholar]
- Haasen C., Prinzleve M., Zurhold H., Rehm J., Güttinger F., Fischer G.…Krausz M. Cocaine use in Europe – A multi-centre study. Eur. Addict. Res. 2004;10(4):139–146. doi: 10.1159/000079834. [DOI] [PubMed] [Google Scholar]
- Indave B.I., Minozzi S., Pani P.P., Amato L. Antipsychotic medications for cocaine dependence. Cochrane Database Syst. Rev. 2016;(3) doi: 10.1002/14651858.CD006306.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Adler L., Ames M., Demler O., Faraone S., Hiripi E.…Walters E.E. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol. Med. 2005;35(2):245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P.M. The behavioral study and treatment of depression. In: Hersen M., Eisler R.M., Miller P.M., editors. Progress in Behavioral Modification. vol. 1. Academic Press; New York: 1975. pp. 19–65. [Google Scholar]
- Maffli E., Delgrande Jordan M., Schaaf S., Dickson-Spillmann M., Künzi U. 2013. Act-info Jahresbericht 2012. (Bern) [Google Scholar]
- McKee S.A., Carroll K.M., Sinha R., Robinson J.E., Nich C., Cavallo D., O'Malley S. Enhancing brief cognitive-behavioral therapy with motivational enhancement techniques in cocaine users. Drug Alcohol Depend. 2007;91(1):97–101. doi: 10.1016/j.drugalcdep.2007.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller P.G., Sønderlund A.L. Using the internet to research hidden populations of illicit drug users: a review. Addiction. 2010;105(9):1557–1567. doi: 10.1111/j.1360-0443.2010.02992.x. [DOI] [PubMed] [Google Scholar]
- Minozzi, S., Amato, L., Pani, P. P., Solimini, R., Vecchi, S., De Crescenzo, F., … Davoli, M. (2015). Dopamine agonists for the treatment of cocaine dependence. The Cochrane Database of Systematic Reviews, (5), CD003352. doi: 10.1002/14651858.CD003352.pub4. [DOI] [PMC free article] [PubMed]
- Petitjean S.A., Dürsteler-MacFarland K.M., Krokar M.C., Strasser J., Mueller S.E., Degen B., Farronato N.S. A randomized, controlled trial of combined cognitive-behavioral therapy plus prize-based contingency management for cocaine dependence. Drug Alcohol Depend. 2014;145:94–100. doi: 10.1016/j.drugalcdep.2014.09.785. [DOI] [PubMed] [Google Scholar]
- Riper H., Hoogendoorn A., Cuijpers P., Karyotaki E., Boumparis N., Mira A. Effectiveness and treatment moderators of internet interventions for adult problem drinking: an individual patient data meta-analysis of 19 randomised controlled trials. PLoS Med. 2018;15(12) doi: 10.1371/journal.pmed.1002714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson S.M., Sobell L.C., Sobell M.B., Leo G.I. Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use. Psychology of addictive behaviors. 2014;28(1):154. doi: 10.1037/a0030992. [DOI] [PubMed] [Google Scholar]
- Rumpf H.-J., Meyer C., Hapke U., John U. Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res. 2001;105(3):243–253. doi: 10.1016/s0165-1781(01)00329-8. [DOI] [PubMed] [Google Scholar]
- Schaub M., Stohler R. Behandlung der Kokainabhängigkeit – ein multimodales Unterfangen. Swiss Medical Forum. 2010;10(25):437–440. [Google Scholar]
- Schaub M., Berthel T., Stohler R. 2009. Behandlung der Kokainabhängigkeit in der Schweiz: Ausmass und Erfahrung bei der Implementierung von in der internationalen wissenschaftlichen Literatur publizierten Therapieansätzen. Resultate einer Netzwerkumfrage. Abhängigkeiten, (3) pp. 72–80. [Google Scholar]
- Schaub M., Sullivan R., Stark L. Snow control - an RCT protocol for a web-based self-help therapy to reduce cocaine consumption in problematic cocaine users. BMC Psychiatry. 2011;11 doi: 10.1186/1471-244X-11-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M., Sullivan R., Haug S., Stark L. Web-based cognitive behavioral self-help intervention to reduce cocaine consumption in problematic cocaine users: randomized controlled trial. J. Med. Internet Res. 2012;14(6):e166. doi: 10.2196/jmir.2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M.P., Haug S., Wenger A., Berg O., Sullivan R., Beck T., Stark L. Can reduce--the effects of chat-counseling and web-based self-help, web-based self-help alone and a waiting list control program on cannabis use in problematic cannabis users: a randomized controlled trial. BMC Psychiatry. 2013;13(1):305. doi: 10.1186/1471-244X-13-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M.P., Maier L.J., Wenger A., Stark L., Berg O., Beck T.…Haug S. Evaluating the efficacy of a web-based self-help intervention with and without chat counseling in reducing the cocaine use of problematic cocaine users: the study protocol of a pragmatic three-arm randomized controlled trial. BMC Psychiatry. 2015;15 doi: 10.1186/s12888-015-0518-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M.P., Wenger A., Berg O., Beck T., Stark L., Buehler E., Haug S. A web-based self-help intervention with and without chat counseling to reduce cannabis use in problematic cannabis users: three-arm randomized controlled trial. J. Med. Internet Res. 2015;17(10) doi: 10.2196/jmir.4860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M.P., Blankers M., Lehr D., Boss L., Riper H., Dekker J.…Ebert D.D. Efficacy of an internet-based self-help intervention to reduce co-occurring alcohol misuse and depression symptoms in adults: study protocol of a three-arm randomised controlled trial. BMJ Open. 2016;6(5) doi: 10.1136/bmjopen-2016-011457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt J., Lamprecht F., Wittmann W.W. Zufriedenheit mit der stationären Versorgung: Entwicklung eines Fragebogens und erste Validitätsuntersuchungen. Psychotherapie, Psychosomatik. Medizinische Psychologie. 1989;39(7):248–255. [PubMed] [Google Scholar]
- Singh M., Keer D., Klimas J., Wood E., Werb D. Topiramate for cocaine dependence: a systematic review and meta-analysis of randomized controlled trials. Addiction. 2016;111(8):1337–1346. doi: 10.1111/add.13328. [DOI] [PubMed] [Google Scholar]
- Soendergaard H.M., Thomsen P.H., Pedersen P., Pedersen E., Poulsen A.E., Nielsen J.M.…Soegaard H.J. Treatment dropout and missed appointments among adults with attention-deficit/hyperactivity disorder: associations with patient-and disorder-related factors. The Journal of Clinical Psychiatry. 2016;77(2):232–239. doi: 10.4088/JCP.14m09270. [DOI] [PubMed] [Google Scholar]
- Tait R.J., McKetin R., Kay-Lambkin F., Carron-Arthur B., Bennett A., Bennett K.…Griffiths K.M.A. A Web-Based Intervention for Users of Amphetamine-Type Stimulants: 3-Month Outcomes of a Randomized Controlled Trial. JMIR Ment. Health. 2014;1(1):e1. doi: 10.2196/mental.3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson S., Gossop M., Powis B., Griffiths P., Fountain J., Strang J. Adverse effects of stimulant drugs in a community sample of drug users. Drug Alcohol Depend. 1997;44(2–3):87–94. doi: 10.1016/s0376-8716(96)01324-5. [DOI] [PubMed] [Google Scholar]
- Wilmers F., Munder T., Leonhart R., Herzog T., Plassmann R., Barth J., Linster H.W. Die deutschsprachige Version des Working Alliance Inventory - short revised (WAI-SR) - Ein schulenübergreifendes, ökonomisches und empirisch validiertes Instrument zur Erfassung der therapeutischen Allianz. Klinische Diagnostik Und Evaluation. 2008;1(3):343–358. [Google Scholar]