Abstract
Background
The hippocampus, an essential structure for learning and memory, has a reduced volume in preterm born (gestational age < 37 weeks) individuals with very low birth weight (VLBW: birth weight < 1500 g), which may affect memory function. However, the hippocampus is a complex structure with distinct subfields related to specific memory functions. These subfields are differentially affected by a variety of neuropathological conditions, but it remains unclear how these subfields may be affected by medical complications following preterm birth which may cause aberrant brain development, and the consequences of this on learning and memory function in children with VLBW.
Methods
Children born preterm with VLBW (n = 34) and term-born controls from the Norwegian Mother and Child Cohort Study (MoBa) (n = 104) underwent structural MRI and a neuropsychological assessment of memory function at primary school age. FreeSurfer 6.0 was used to analyze the volumes of hippocampal subfields which were compared between groups, as was memory performance. Correlations between abnormal hippocampal subfields and memory performance were explored in the VLBW group.
Results
All absolute hippocampal subfield volumes were lower in the children with VLBW compared to MoBa term-born controls, and the volumes of the left and right dentate gyrus and the right subiculum remained significantly lower after correcting for total intracranial volume. The VLBW group had inferior working memory performance and the score on the subtest Spatial Span backwards was positively correlated to the volume of the right dentate gyrus.
Conclusions
Hippocampal subfield volumes seem to be differently affected by early brain development related to preterm birth. The dentate gyrus appears particularly susceptible to adverse effects of preterm birth. Reduced working memory function among children with VLBW was associated with smaller volume of right dentate gyrus. This finding demonstrates alterations in hippocampal structure-function relationships associated with early brain development related to preterm birth.
Keywords: Preterm birth, Very low birth weight, Hippocampus, Memory function, Structural MRI, Hippocampal subfields, Norwegian Mother and Child Cohort Study (MoBa)
Abbreviations: ASHS, Automatic Segmentation of Hippocampal Subfields; CA, Cornu Ammonis; DG, Dentate Gyrus; GC-DG, Granule cell layer of Dentate Gyrus; HATA, Hippocampal-Amygdaloid Transition Area; HPA, Hypothalamic-Pituitary-Adrenal; ICV, Intracranial Volume; ML, Molecular Layer (of the Hippocampus); MoBa, the national Norwegian Mother and Child Cohort; MPRAGE, Magnetization-prepared rapid acquisition with gradient echo; NESPY, Developmental Neuropsychological assessment; NISS, Neonatal Infant Stressor Scale; REY, Rey-Osterrieth Complex Figures Test; WASI, Wechsler Abbreviated Scale of Intelligence; WISC, Wechsler Intelligence Scale for Children; WPPSI, Wechsler Preschool and Primary Scale of Intelligence
Highlights
-
•
Hippocampal subfield volumes are reduced in very low birth weight (VLBW) children.
-
•
Especially the volumes of the dentate gyrus (DG) were smaller in the VLBW children.
-
•
Reduced working memory function was reported in the preterm group.
-
•
Working memory was positively associated with the right DG in the VLBW group.
1. Introduction
The hippocampus is a complex, heterogeneous structure in the medial temporal lobe. It consists of several anatomically and functionally specialized subfields that are tightly interconnected. Typically, it is divided into the subiculum, presubiculum, parasubiculum, the cornu ammonis (CA) fields 1–4 and the dentate gyrus (DG) (Duvernoy et al., 2013). The hippocampi have been related to episodic memory, the ability to remember experiences occurring in a specific context, e.g. a particular time and place (Burgess et al., 2002; Tulving and Markowitsch, 1998) and is therefore important for the formation of episodic memory (Bohbot et al., 2006; Gadian et al., 2000; Scoville and Milner, 2000). The involvement of the hippocampus in working memory is however debated (Baddeley et al., 2011). Impaired working memory has been reported in patients with temporal lobe epilepsy due to hippocampal sclerosis (Winston et al., 2013) and disrupted deactivation of the hippocampus with increasing working memory load is associated with impaired working memory performance in this patient group (Stretton et al., 2012). Disconnection of the hippocampal-prefrontal cortical circuits has been shown to impair spatial working memory performance in rats when muscimol was infused bilaterally into the ventral hippocampus (Wang and Cai, 2006). Some argue that the hippocampus is more involved in working memory function up until early adolescence (Finn et al., 2010) when a more mature memory system involving the fronto-parietal cortex evolves (Nosarti and Froudist-Walsh, 2016). Nevertheless, we have reported a relationship between the volume of right hippocampus and working memory ability in VLBW young adults born in the 1980s (Aanes et al., 2015).
Prior studies show that the specific hippocampal subfields have specialized functions in memory processes. For example, the CA2/3 and CA4/DG are more involved in encoding, learning and recall over shorter time intervals, while CA1 and subiculum are output structures mainly related to retrieval functions and associated with delayed episodic memory (Eldridge et al., 2005; Mueller et al., 2011; Zammit et al., 2017). Also, irradiation induced hypoplasia of the neonatal DG in rats influenced spatial behavior (Xavier and Costa, 2009).
New advances in automated magnetic resonance imaging (MRI)-processing software (Iglesias et al., 2015; Yushkevich et al., 2015) make it possible to examine hippocampal subfields in larger study populations. Studies based on this software have linked CA1 and subiculum to delayed visual and verbal memory in older adults (Zammit et al., 2017), the left CA-field to verbal memory in healthy adults (Aslaksen et al., 2018), and the CA1 and CA2–3 to better delayed recall. Although this software was developed for analyzing adult brains, it has also proved to be reliable in investigating the development of hippocampal subfields in typically developing children and adolescents (Krogsrud et al., 2014) where longitudinal decreases in volumes of CA2–3 and CA4/DG were associated with verbal learning (Tamnes et al., 2014).
The hippocampus is known to be vulnerable to different pathologies (Walker et al., 2007), and studies have shown that the hippocampal subfields are differently affected by pathological conditions, such as reduced volumes of CA1–3 and DG reported in major depressive disorder (Huang et al., 2013; Travis et al., 2015), smaller CA4/DG in Post-Traumatic Stress Disorder (PTSD) (Hayes et al., 2017) and smaller CA4/DG in first episode schizophrenia and smaller CA1 in chronic schizophrenia (see review by (Nakahara et al., 2018). Reduced hippocampal subfield volumes are also seen in survivors of pediatric brain tumors (Decker et al., 2017) and patients with temporal lobe epilepsy (Sone et al., 2016). In addition, the subiculum and DG volumes decline with normal ageing (Small, 2001) while Alzheimer's disease typically affects the CA1-field (de Flores et al., 2015).
The hippocampus and its related memory functions are also affected in individuals born preterm (born before gestational week 37) with very low birth weight (VLBW: BW <1500 g) (see Nosarti and Froudist-Walsh, 2016 for a review). Being born preterm with VLBW increases the risk of perinatal brain injury followed by aberrant brain development (Nosarti et al., 2002; Volpe, 2009). Individuals with VLBW may be exposed to hypoxic-ischemic episodes as neonates (Volpe, 2012) to which the hippocampus is particularly vulnerable (Busl and Greer, 2010; Nakamura et al., 1986; Ørbo et al., 2018). In addition to hypoxia, the hippocampus is sensitive to stress hormones and undernutrition during its development in utero (Schmidt-Kastner and Freund, 1991; Sizonenko et al., 2006), which are all factors that may be present in the preterm born neonate. Thus, injury to the immature hippocampus and/or impaired hippocampal growth and development may add to the neurodevelopmental burden of preterm born individuals (Jacob et al., 2011).
Studies have shown that compared to term-born controls, individuals born preterm with VLBW have smaller hippocampal volumes from infancy through adulthood (Nosarti and Froudist-Walsh, 2016). We have previously reported reduced hippocampal volume in a cohort of participants born preterm with VLBW in young adulthood (Bjuland et al., 2014) which was related to memory function measured by a comprehensive test battery (Aanes et al., 2015). Additionally, we have found reduced global hippocampal volumes in an overlapping sample of the same cohort as in this study (Sølsnes et al., 2015; Sølsnes et al., 2016; Sripada et al., 2018). However, the studies conducted in the preterm population so far have treated the hippocampi as homogenous structures and looked at global hippocampal volume when comparing to term-born controls and relating to memory function. Thus, little is known about how medical complications of preterm birth may affect the development and growth of specific subfields of the hippocampi and how this may have functional consequences with regard to memory and learning in children with VLBW.
The aim of this study was to explore any differences in volumes of hippocampal subfields and memory function between school-aged children born preterm with VLBW compared to term-born controls. Secondly, to examine if hippocampal subfield volumes were associated with neonatal risk factors, such as birth weight, gestational age, and total number of days in the neonatal intensive care unit (NICU) and days in need of mechanical ventilation in the preterm born group with VLBW. Thirdly, we investigate structure-function relationships between hippocampal subfields and memory test scores in the VLBW group for the volumes and test scores where significant group differences were present.
We hypothesized that the individuals with VLBW would have smaller hippocampal subfield volumes and lower memory test scores compared to the term-born controls. We also hypothesized that there would be an association between neonatal risk factors and hippocampal subfield volumes, and between inferior memory performance and reduced hippocampal subfield volumes.
2. Material and methods
2.1. Participants
The original cohort has been thoroughly described in Sølsnes et al. (2015), and a brief description is given below.
2.1.1. VLBW group
Preterm-born children with VLBW born at or admitted to the Neonatal Intensive Care Unit (NICU) at St. Olav University Hospital in Trondheim, Norway between 2003 and 2007 were included in the study. Exclusion criteria were severe cerebral palsy, severe sensory impairments (deafness or blindness) and/or any contraindications for MRI. Sixty-three children, aged 6 to 11 years, were eligible and 57 agreed to participate. Of these, 10 did not want to participate in MRI and completed the neuropsychological assessment only while two participants had MRI but did not participate in neuropsychological assessment. MRI-scans of 10 participants were excluded due to movement artifacts or disrupted scanning, leaving 39 children with MRI-scans of good quality. Of these, 34 had successful automated subfield segmentation of the hippocampi while 32 had both volumetrics and neuropsychological assessment of memory function.
2.1.2. Control subjects
The control subjects were recruited from the national Norwegian Mother and Child Cohort Study (MoBa) managed by the Norwegian Institute of Public Health (Magnus et al., 2006) in a collaboration project with the Center for the Study of Human Cognition (CSHC), Department of Psychology, University of Oslo. We invited age-matched (aged 6 to 12 years) non-disabled term born children living in the same geographical area as the VLBW participants (central Norway). Those with factors known to affect function of the central nervous system, including neurological or psychiatric illness, serious head trauma, and those with a birth weight < 2500 g or MRI contraindications were excluded from participation. Invitation letters were sent to a total of 643 MoBa participants, of whom 203 responded and 143 children agreed to participation. Of these, 22 did not want to participate in MRI and scans from 17 controls had to be excluded due to movement artifacts or disrupted scanning, leaving 104 participants with MRI-scans of good quality. The youngest participants (5–6 years of age) were the most likely to decline MRI or to be excluded due to movement artifacts. Of those with high quality MRI, all had successful automated segmentation of the hippocampi and neuropsychological assessment of memory function.
2.2. Neuropsychological assessment
The neuropsychological assessment was performed by trained research assistants and PhD students, blinded to previous medical history and MRI findings, but not to group adherence due to small differences in the assessment battery for cognitive function (IQ) between the two groups. Since the term born control group was part of a larger multicenter study, they received an abbreviated IQ test battery, see below for details.
2.2.1. Cognitive assessment
The complete version of the Wechsler Intelligence Scale for Children, 4th edition (WISC-IV) (Wechsler, 2003) was used to assess cognitive abilities and provide Full scale IQ in the preterm group with VLBW. The Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999) was used to assess cognitive abilities in control children older than 6.5 years of age, while two control children younger than 6.5 years completed a short form of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-III) (Wechsler, 2002), both providing an estimated Full scale IQ.
2.2.2. Neuropsychological assessment of memory functions
Subtests from different neuropsychological test batteries were used to assess several aspects of memory function. The subtest Spatial Span (from the Wechsler Memory Scale (Wechsler, 1997)) and the Digit Span subtest (from the WISC-IV) were used to evaluate visual and verbal working memory, respectively. Narrative memory was tested using a story from A developmental NEuroPSYchological assessment (NEPSY- 2nd edition) (Korkman and Kemp, 2002), where the children listen to a story and are later asked to recall it (free recall) and to answer specific questions from the story (queued recall). Only a subgroup (n = 39) of the controls completed this test. Visual memory was assessed using the Rey-Osterrieth Complex Figure Test (REY) (Meyers and Meyers, 2004), which is a complex geometrical drawing that assesses visuo-spatial abilities and delayed visuospatial memory. In this study, we included the copy score at baseline and the delayed recall score after 30 min. Raw scores adjusted for age were used in the analyses.
2.3. Neonatal variables
Neonatal variables known to represent risk factors for poor long-term neurological outcome after preterm birth were registered. These included birth weight, gestational age at birth, number of days on mechanical ventilator, and total days spent in NICU.
2.4. Socioeconomic status
Socioeconomic status (SES) was calculated according to Hollinghead's two factor index of social position, based on education and occupation of one parent, or the mean index of both parents (Hollinghead, 1957). SES scores were missing for one VLBW and three control children, and mean SES in the respective group was imputed for these participants.
2.5. MR-imaging
2.5.1. Image acquisition
The cerebral MRI-data was acquired with a sagittal 3D T1-weighted magnetization prepared rapid acquisition gradient echo (MPRAGE) sequence (repetition time (TR) = 2400 ms, echo time (TE) 3.61 ms, inversion time (TI) = 1000 ms, flip angle 8°, 160 slices, voxel sizes of 1.25 × 1.25 × 1.20 mm3, and field of view (FOV) 240 × 240 mm2) at a 1.5 Tesla Siemens Avanto scanner with a 12-channel head coil. A parallel imaging technique (iPAT) acquiring multiple T1-scans within a short scan time of 4 min 18 s enabled us to discard the scans with too low quality and average those with sufficient quality. The average total scan time was 30 min. All MPRAGEs were visually inspected by trained personnel before further processing.
2.5.2. Hippocampal subfield segmentation
The images were processed using the freely available FreeSurfer image analysis suite version 6.0 (http://surfer.nmr.mgh.harvard.edu) (Dale et al., 1999; Fischl et al., 2002; Fischl et al., 2004) with the hippocampal subfield segmentation module (Iglesias et al., 2015). In addition to motion correction, removal of non-brain tissue, Talairach transformation and segmentation of subcortical white matter and deep gray matter volumes (Fischl et al., 2002; Fischl et al., 2004; Reuter et al., 2010; Segonne et al., 2004), the new automatic algorithm segments the hippocampus into 12 subfields based on Bayesian inference from a new high-resolution probabilistic atlas generated from ex vivo MRI data (Iglesias et al., 2015). This method shows strong correlations with manual delineations and segments into the following hippocampal subfields in each hemisphere: CA1, CA2/3, CA4, the molecular layer (ML), the granule cell layer of the dentate gyrus (GC-DG), subiculum, presubiculum, parasubiculum, fimbria, the hippocampal-amygdaloid transition area (HATA), hippocampal tail, and hippocampal fissure. The whole hippocampus consists of all fields except for the hippocampal fissure. The method has not yet been validated for children. However, a previous FreeSurfer version has been used to investigate hippocampal subfields in typically developing children aged 4 to 22 years (Krogsrud et al., 2014; Tamnes et al., 2013), and Herten et al. (2018) found acceptable agreement between the global hippocampal volume from the FreeSurfer 6.0 subfield segmentation method and manual segmentation in children between 5 and 16.4 years (Herten et al., 2018). However, further studies validating this procedure for specific hippocampal subfields in children are needed.
We performed a two-step quality control as described in Cao et al. (2017), where the subfield segmentations for each individual were first manually inspected to exclude volumes with obvious errors in hippocampal location or subfield assignment. Secondly, we looked for outliers, i.e. volumes >5SD from the mean of each hippocampal subfield, which was the same threshold used by Cao et al. The first step led to the exclusion of two right-sided hippocampal volumes in the control group, while the second step did not reveal any outliers.
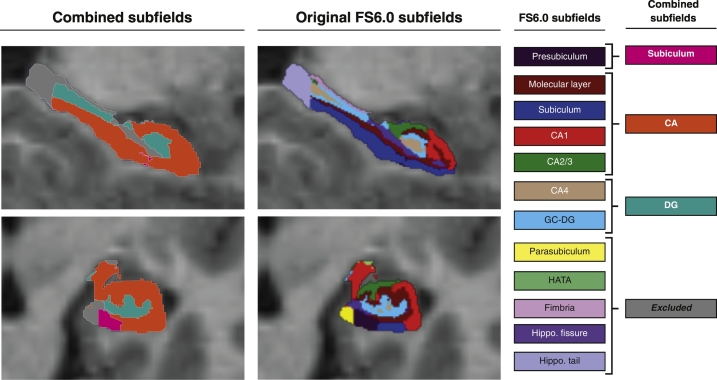
As our segmentations were based on T1-weighted images only, the boundary definitions for smaller subfields (e.g. CA2/3, GC-DG, molecular layer) may be less reliable (Chen et al., 2018; Iglesias et al., 2015; McHugo et al., 2018). Therefore, we regrouped the subfield volumes and combined some of them to create three subfield volumes for each hippocampus: CA-field, Dentate gyrus and Subiculum. This was done in line with the recent suggestions from Mueller et al. (Mueller et al., 2018) in the following way: CA-field: CA1 + CA2/3 + Molecular layer + Subiculum; Dentate gyrus (DG): GC-DG + CA4; Subiculum = Presubiculum (see Fig. 1 for illustration). This reclassification is also more in line with other automated segmentation methods, such as the Automatic Segmentation of Hippocampal Subfields (ASHS) (Yushkevich et al., 2015).
Fig. 1.
Combined hippocampal subfields (left) based on original FreeSurfer 6.0 labels (right). The original subfield labels from FreeSurfer are shown in the left panel and the combined subfields used in the present analyses are shown to the right. The Subiculum is equal to the FreeSurfer label Presubiculum; The CA-field includes the FreeSurfer labels Molecular layer, Subiculum, CA1 and CA2/3; The DG consists of the FreeSurfer labels CA4 and GC-DG; while the HATA, Fimbria, Hippocampal fissure and Hippocampal tail were excluded from analyses. CA = Cornu Ammonis; DG = Dentate gyrus; GC-DG = Granulate cells of the dentate gyrus; HATA = Hippocampal-Amygdaloid Transition Area.
Total intracranial volumes (ICV) used for correction analyses were calculated based on an automated reverse brain mask method with the “new segment” approach from the SPM8 toolbox (release 5236) (www.fil.ion.uclac.uk/spm) (Hansen et al., 2015). The ICV segmentations were visually inspected, and none were rejected.
2.6. Statistical analysis
All statistical analyses were conducted within IBM SPSS Statistics version 25. Differences in group means were analyzed using the Student t-test or Mann-Whitney U test for nonparametric distributions. The group comparisons of neuropsychological test scores and hippocampal subfield volumes were performed with a univariate general linear model with group as fixed factor, adjusted for sex, age at assessment. The neuropsychological test scores were also adjusted for SES. Group differences in hippocampal subfield volumes were both on absolute volumes and with intracranial volume added as a covariate in univariate general linear models. Correlations between neonatal variables and hippocampal volumes were investigated using partial correlation analysis corrected for sex, intracranial volume and age at assessment. The correlation analyses between number of days in NICU and number of days in need of mechanical ventilation and hippocampal volumes were also adjusted for gestational age at birth, i.e. degree of immaturity. Partial correlations were also used to investigate brain structure-function relationships in the VLBW group adjusting for age, sex, SES and total intracranial volume.
2.6.1. Multiple comparisons correction
The Bonferroni method was used to correct for multiple comparisons. Bonferroni adjusted p-values for significance for the memory test scores group comparison was (0.05/11) = 0.0045, for the subfield volume analyses (0.05/6) = 0.0083 and for the possible structure-function relationships (0.05/6) = 0.0083. The Bonferroni corrected p-value for the correlation analyses between neonatal variables and hippocampal subfield volumes was (0.05/24) = 0.002.
Both Bonferroni adjusted significant p-values and uncorrected p-values (significant p < .05) were reported since the likelihood of type II errors (false negative) is increased by the rather conservative Bonferroni method so that real differences between groups may appear non-significant (Perneger, 1998). However, only presenting uncorrected p-values may result in rejecting the null hypothesis too readily (type I error – false positive). By presenting results both with and without Bonferroni adjusted p-values this would enable the reader to make a reasonable conclusion about what to be “true” findings based also on whether the results are biologically plausible in this rather exploratory study.
2.7. Ethics
This study was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). The Regional Committee for Medical Research and Ethics approved the study protocol (project number: 2010/2359), and written, informed consent was obtained from the caregivers of all participants.
3. Results
3.1. Clinical characteristics
The main clinical characteristics of the two study groups are presented in Table 1. There were, as expected, significant differences in mean birth weight, gestational age and head circumference at birth between the two groups. The mean birth weight and gestational age for the children in the VLBW group were 1031 g (SD 305 g) and 29 weeks, respectively, while the age-matched controls were born at a mean gestation of 40 weeks with a mean birth weight of 3694 g (SD 532 g). Mean age at MRI was slightly lower in the group with VLBW, while mean age for neuropsychological assessment was not statistically different between groups (VLBW: mean age 8.9 years (SD 1.7), controls: mean age 9.4 years (SD 1.2)). The VLBW group received more special education in school and had a lower mean IQ than controls (IQ score 98 versus 107, p = .001). There were no significant group differences regarding sex or SES.
Table 1.
Clinical characteristics of the two study groups.
| VLBW group |
Control group |
p-value | |||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Range | n | Mean (SD) | Range | ||
| Birth weight (grams) | 34 | 1031 (305) | 416–1495 | 104 | 3694 (532) | 2510–5460 | <0.0001 |
| Gestational age (weeks) | 34 | 29.2 (2.5) | 25–34 | 103 | 40.1 (1.3) | 37.1–42.6 | <0.0001 |
| Head circumference at birth (cm) | 31 | 26.5 (2.5) | 22.3–30.0 | 92 | 35.5 (1.5) | 32.0–39.0 | <0.0001 |
| Sex male n | 34 | 18 (53%) | – | 104 | 49 (47%) | – | 0.555 |
| Socioeconomic status (SES)a | 34 | 3.9 (1.0) | 1–5 | 104 | 4.2 (0.9) | 1–5 | 0.056 |
| Clinical data | |||||||
| APGAR 1 min | 34 | 7 | 0–9 | ||||
| APGAR 5 min | 34 | 8 | 1–10 | ||||
| Days in NICU n | 34 | 58 | 8–101 | ||||
| Days on mechanical ventilator n | 34 | 4.7 | 0–47 | ||||
| Age at MRI (years) | 34 | 8.7 (1.7) | 6.1–10.7 | 104 | 9.4 (1.3) | 6.2–12.0 | 0.032 |
| Received special education in school n | 33 | 13 (39%) | – | 100 | 8 (8%) | – | <0.001 |
| Full IQ | 32 | 98 (12) | 74–132 | 104 | 107 (13) | 74–135 | 0.001 |
Subject characteristics; Student's t-test was used for parametric data, Mann-Whitney U test for non-parametric data, Pearson Chi-Square for categorical data. Abbreviations: VLBW = very low birth weight; NICU = neonatal intensive care unit; MRI = magnetic resonance imaging; IQ = intelligence quotient.
SES was calculated according to Hollinghead's two factor index of social position, based on education and occupation of one parent, or the mean index of both parents.
Neonatal MRI was not performed as a routine in clinics in Norway when these children were born. However, based on neonatal ultrasonography two of the 34 participants with VLBW had pathological ultrasound findings: one had intraventricular hemorrhage (IVH) grade I and one IVH grade III. The preterm born neonate with IVH grade III had a cerebral MRI performed before discharge from the NICU, described as normal, except for small amounts of blood in the ventricles. Overall, this is a sample of preterm born children who did not present with gross brain pathology in the neonatal period.
3.2. Memory assessment
The children born preterm with VLBW had significantly lower scores than the controls on Digit span forward and total and Spatial span backwards and total, which measure verbal and visual working memory. There were no significant differences between the two groups in narrative memory, measured by NEPSY story, or delayed visual memory measured by the Rey-Osterrieth Complex Figure Test (Table 2). When correcting for multiple comparisons, Spatial span backward and total remained significantly reduced in the VLBW group.
Table 2.
Memory results in the two study groups.
| Memory test | n | VLBW group |
Control group |
p-value | |||
|---|---|---|---|---|---|---|---|
| Mean (SE) | 95 % CI | n | Mean (SE) | 95 % CI | |||
| Digit Span | |||||||
| Forward | 32 | 6.2 (0.3) | 5.6– 6.7 | 104 | 7.0 (0.2) | 6.7 – 7.3 | 0.018 |
| Backward | 32 | 5.0 (0.3) | 4.6 – 5.6 | 104 | 5.6 (0.1) | 5.4 – 5.9 | 0.065 |
| Total | 32 | 11.2 (0.4) | 10.4– 12.1 | 104 | 12.6 (0.2) | 12.1 – 13.1 | 0.008 |
| Spatial Span | |||||||
| Forward | 32 | 6.6 (0.3) | 6.0 – 7.2 | 7.0 (0.2) | 6.7 – 7.4 | 0.249 | |
| Backward | 32 | 5.4 (0.3) | 4.8– 5.9 | 102 | 6.7 (0.2) | 6.4 – 7.0 | <0.001 |
| Total | 32 | 12.0 (0.5) | 11.0 – 12.9 | 13.8 (0.3) | 13.2 – 14.3 | 0.002 | |
| NEPSY Narrative memory | |||||||
| Free recall | 32 | 18.6 (1.1) | 16.4 – 20.9 | 19.5 (1.0) | 17.5 – 21.5 | 0.564 | |
| Cued recall | 32 | 4.8 (0.5) | 3.9 – 5.7 | 4.7 (0.4) | 3.9 – 5.5 | 0.862 | |
| Total | 32 | 23.5 (0.8) | 21.9 – 25.0 | 39 | 24.2 (0.7) | 22.9 – 25.6 | 0.465 |
| REY Visuospatial memory | |||||||
| Copy | 31 | 22.3 (1.2) | 19.9 – 24.7 | 92 | 23.5 (0.7) | 22.1 – 24.9 | 0.413 |
| Delayed recall | 31 | 12.4 (1.1) | 10.3 – 14.6 | 92 | 11.0 (0.6) | 9.8 – 12.3 | 0.266 |
General linear model with group as fixed factor and socioeconomic status and sex and age at assessment as covariates.
Abbreviations: VLBW = very low birth weight; SE = Standard Error; CI = Confidence Interval; NEPSY = A Developmental NEuroPSYchological Assessment; REY = Rey-Osterrieth Complex Figure Test.
3.3. Hippocampal total and subfield volumes
The children born with VLBW had significantly lower absolute total hippocampal volumes bilaterally compared to controls. In addition, all absolute hippocampal subfield volumes were significantly smaller in the VLBW group. Total ICV was also lower in the VLBW group, and when correcting for this, the volume reduction of the total right hippocampus as well as the left and right DG and the right subiculum remained significant (Table 3). When correcting for multiple comparisons, only Right DG volume remained significantly lower in the VLBW group. The absolute volumes of all the twelve hippocampal subfields segmented by FreeSurfer for the two groups are shown in Supplemental material (Table S1) while the absolute combined subfields are shown in Table S2.
Table 3.
Hippocampal total and subfield volumes (mm3) in the two study groups.
| VLBW group |
Control group |
p-value | |||||
|---|---|---|---|---|---|---|---|
| N | Mean (SE) | 95% CI | n | Mean (SE) | 95% CI | ||
| Total Hippocampal volumes | |||||||
| Left hippocampal volume | 34 | 3314 (42) | 3230–3397 | 104 | 3409 (24) | 3363–3456 | 0.055 |
| Right hippocampal volume | 34 | 3340 (41) | 3259–3420 | 102 | 3443 (23) | 3397–3488 | 0.032 |
| Hippocampal subfield volumes | |||||||
| Left CA-field | 34 | 1761 (24) | 1713–1810 | 104 | 1811 (14) | 1784–1838 | 0.081 |
| Right CA-field | 34 | 1813 (24) | 1766–1861 | 102 | 1844 (13) | 1818–1871 | 0.275 |
| Left DG | 34 | 521 (8) | 504–538 | 104 | 545 (5) | 536–555 | 0.015 |
| Right DG | 34 | 527 (8) | 512–542 | 102 | 553 (4) | 544–561 | 0.004 |
| Left Subiculum | 34 | 313 (6) | 301–325 | 104 | 325 (3) | 318–331 | 0.112 |
| Right Subiculum | 34 | 291 (5) | 280–302 | 102 | 306 (3) | 300–312 | 0.019 |
| Total intracranial volume (cm3) | 34 | 1454 (21) | 1412–1496 | 104 | 1519 (12) | 1495–1542 | 0.009 |
General linear model with group as fixed factor, and sex and age at MRI and intracranial volume as covariates. Abbreviations: VLBW = very low birth weight; SE = standard error; CI = confidence interval; CA = Cornu Ammonis; DG = Dentate gyrus.
3.4. Associations between hippocampal subfield volumes and neonatal variables in the VLBW group
No significant correlations were found between birthweight, gestational age, or number of days in NICU and hippocampal subfield volumes. Correlations were found between several hippocampal subfield volumes and days on mechanical ventilator for the 15 subjects with VLBW who were in need of ventilator. The greatest effects were found for Left CA (r = −0.630, p = .012) and Right Subiculum (r = −0.620, p = .14) and days on mechanical ventilation. The correlations remained significant after removing one outlier with 47 days on ventilator but did not survive Bonferroni correction.
3.5. Associations between reduced hippocampal subfield volumes and inferior memory scores in the VLBW group
The volume of the right DG was positively correlated with the Spatial span backward subtest (r = 0.444, p = .018). However, this was not significant after Bonferroni correction. No other suggested structure-function relationship was found for hippocampal subfield volumes and memory test scores that were lower in the VLBW group than in the control group.
4. Discussion
In this study, children with VLBW born 2003–2007 had smaller absolute hippocampal subfield volumes bilaterally than age-matched term-born controls at a mean age of 9 years. When correcting for ICV, the hippocampal volume reductions were limited to DG bilaterally and right subiculum. Lower working memory performance was found in the VLBW group, while other memory functions did not differ between the two groups. A positive association was found between reduced score on the working memory subtest Spatial Span backwards and reduced right DG volume, suggesting a possible structure-function relationship in the preterm born group of children with VLBW.
4.1. Hippocampal volumes in the VLBW group
Reduced hippocampal volume is a common finding in the preterm population (see Nosarti and Froudist-Walsh, 2016 for a review). We have previously reported reduced hippocampal volumes in a cohort of young adults born with VLBW in the 1980s (Aanes et al., 2015; Bjuland et al., 2014). However, there have been great advances in neonatal intensive care since then and the results may not be representative for cohorts born in the 2000s. Still, reductions in global hippocampal volume and shape-alterations have been reported at term-equivalent age (Thompson et al., 2013) and at age 7 years (Thompson et al., 2014) for preterm individuals born in the same decade as this study population. As far as we know, though, no one has investigated specific hippocampal subfield alterations in the preterm population. We found smaller volumes of the CA-fields, DG and subiculum bilaterally in the VLBW group when compared to term-born controls. The volume reduction of bilateral DG and the right subiculum remained significant when correcting for ICV.
4.2. The role of the different hippocampal subfields
The Cornu Ammonis (CA), and predominantly the CA1-subfield, is particularly vulnerable to ischemia (Walker et al., 2007), which is believed to underlie some of the aberrant brain development in the preterm-born individuals (Volpe, 2012). The children with VLBW had lower volumes of the CA-field compared to term-born controls, although not significant after correcting for ICV. In our study, a weak correlation was found between CA-field volumes and days on mechanical ventilation. Thus, we speculate that the children in the VLBW group with the most immature lung function may have more episodes with hypoxia-ischemia in the neonatal period, influencing growth the CA-subfield. Further and larger studies are needed to confirm or reject this speculation since only a very limited number of children with VLBW on mechanical ventilator were included in our study.
The dentate gyrus (DG) receives input from entorhinal cortex and projects to the CA3 (Amaral et al., 2007), and has been reported to be vulnerable to both physical and psychological stress resulting in apoptosis and impaired neurogenesis (Morris, 2007), and to hypoglycemia resulting in neuronal necrosis (Auer, 1986, Auer, 2010). Both of these mechanisms are possible explanations alone or together for the reduced DG volumes seen in the VLBW group. Being born very preterm is certainly a stressful event in terms of different physical and psychological stressors, for instance painful procedures like intubation and intravenous access. In fact, the Neonatal Intensive Stressor Scale (NISS) (Newnham et al., 2009), which quantifies the accumulated stress the preterm baby is exposed to, is associated with regional alterations in brain structure and function at term-equivalent age, including functional alterations in the temporal lobe which the authors argue reflect alterations in the hippocampus due to stress (Smith et al., 2011). Stress also exacerbates the effects of other neurological insults commonly seen in preterm babies such as hypoxia and ischemia (Morris, 2007). Hypoglycemia is also a frequent complication of preterm birth and is linked to several neurodevelopmental abnormalities (Sharma et al., 2017). In our study, the left DG volume was negatively correlated with days on mechanical ventilation (p = .025), meaning that more days in need of respiratory assistance were associated with smaller DG in the VLBW group. Mechanical ventilation is ranked as one of the most stressful procedures in the NISS (Newnham et al., 2009) which may explain the significant association. However, as mentioned above further and larger studies including information on stress, hypoglycemia etc. are needed to confirm this speculation.
The subiculum was also reduced in the children in the VLBW group compared to term-born controls, although only the right subiculum remained significantly reduced after including total intracranial volume in the analysis. The subiculum is a structure which receives input from CA1 and entorhinal cortex and projects to several cortical and subcortical areas (Aggleton and Christiansen, 2015; Matsumoto et al., 2018), and may play a crucial role in organizing hippocampal output. It is mainly related to retrieval functions (Eldridge et al., 2005) and thought to be involved in spatial navigation, memory and regulation of the hypothalamic-pituitary-adrenal (HPA)-axis (O’Mara et al., 2009). The key role in regulation of the HPA-axis through its connection with hypothalamic regions and a high-density of glucocorticoid binding sites (Herman and Mueller, 2006) makes early stress a plausible explanation for the reduced volumes seen in the VLBW group. In fact, some argue that the subiculum is responsible for the hippocampal interaction in the HPA-axis. Studies of psychological stress also report reduced subicular volumes (Teicher et al., 2012). The subiculum is also vulnerable to hypoxic-ischemic episodes (Stark, 2007), and we found negative associations between days on mechanical ventilator and subicular volumes in the VLBW group. We therefore speculate that the normal development of subiculum is negatively affected by medical conditions associated with preterm birth.
4.3. Memory function in children born with VLBW
The lower visual and verbal working memory performance in the children with VLBW compared to term-born controls are in line with previous studies in the preterm population (Anderson, 2014). We found no group-differences in narrative memory or visual delayed memory assessed with the NEPSY-story and Rey-Osterrieth Complex Figure Test (REY), respectively. This is in agreement with Brunnemann et al. (2013) who found no visual memory deficits in a group of preterm individuals compared to term-born controls when assessed with REY at age 9 (Brunnemann et al., 2013). Our results partly align with Omizzolo et al. (2013) who report deficits in visual immediate memory and verbal working memory at age 7 assessed with similar tests to spatial span and digit span in our study (Omizzolo et al., 2013). However, they also found deficits in short delay verbal memory, which we did not assess, and in visual delayed memory. The inconsistency in visual delayed memory could be due to differences in tests as Omizzolo et al. used a Dot locations subtest.
4.4. The relationship between hippocampus and neonatal variables
Days in need of mechanical ventilation in the neonatal period was negatively correlated with most hippocampal subfields, meaning that more days in need of respiratory assistance were associated with smaller hippocampal subfield volumes. However, the number of neonates requiring mechanical ventilation was low and included only 15 preterm born children. The associations did not survive Bonferroni correction. These findings have to be confirmed in larger study samples before generalization of results. However, the association is interesting and worth mentioning, since it is biological plausible. We speculate further that children in the VLBW group with the most immature lung function may have experienced more episodes with hypoxia-ischemia and stress in the neonatal period, which may then affect the developing hippocampus (Sizonenko et al., 2006), including the CA-fields and the subiculum (Stark, 2007) to a greater extent.
4.5. The relationship between hippocampus and memory function in children born with VLBW
In our study, we found a positive association between scores on the visual working memory test Spatial Span backwards and the right DG volume in the VLBW group, implying that a larger right DG provides better visual working memory in the preterm population. This is a novel finding which has not been reported before. However, this finding needs to be confirmed in larger studies since the association did not survive correction for multiple comparisons. One could speculate whether this finding might indicate a reorganization of memory functions in the VLBW study group. The right hippocampus is thought to be more involved in spatial memory and the left in verbal and more general episodic memory (Burgess et al., 2002; Suthana et al., 2011). However, spatial memory includes representations within working, short-term memory and long-term memory. Thus, we can speculate that the relationship between right DG and the working memory subtest Spatial Span in this study could be due/is linked to the spatial element of the test. Actually, it has been argued that the backward version of the Spatial Span task involves specific spatial processes and is more a task of spatial memory than visual working memory (Mammarella and Cornoldi, 2005).
4.6. Strengths and limitations
Strengths of this study include a large normative control sample from the Norwegian Mother-and Child cohort and thorough clinical assessment with standardized memory testing and quantitative cerebral MRI of the children in both study groups. To our knowledge, no one has reported hippocampal subfield volumes in the preterm population with VLBW and related them to memory function before. A novelty of the study is the use of a new algorithm for hippocampal subfield segmentation. However, this algorithm has not been thoroughly validated in pediatric populations.
The study has some limitations that need to be considered. First, the rather small sample size of preterm individuals and a possible selection bias in the control group as they were recruited through the national MoBa birth cohort study may limit generalization of results. There is also quite large variability in age among the study participants (participants between 6 and 12 years of age), which we have tried to adjust for by covarying with age in all analyses. Also, the hippocampus is found to be larger in boys than girls (Tamnes et al., 2014) and we did not explore any sex differences in this study due to the limited sample size of children with VLBW. The administration of different IQ-assessments in the VLBW group and control group is another limitation with less demanding abbreviated versions of the test in the control group. Thus, the differences in general cognitive ability must be interpreted with caution. However, the results are in line with other studies of preterm born individuals born in the 2000s which report IQ scores in the same range as in this study (Omizzolo et al., 2013). The memory tests used in this study do not constitute a comprehensive test battery of different aspects of memory function, thus we may have overlooked possible relations to hippocampal subfield volumes.
MRI pathology involving other brain structures than the hippocampi could also influence memory function in the preterm group with VLBW. MRI results in childhood from the same study population have been reported by our research group (Sølsnes et al., 2015, Sølsnes et al., 2016), showing smaller cortical surface area bilaterally in the frontal, temporal and parietal lobes, as well as increased cortical thickness in the frontal and occipital regions and reduced cortical thickness in the posterior parietal regions, in the individuals born preterm with VLBW compared with term-born controls (Sølsnes et al., 2015). The individuals born with VLBW also had reduced volumes of thalamus, globus pallidus, corpus callosum, cerebral white matter, ventral diencephalon, and brain stem, and larger ventricular system than the controls (Sølsnes et al., 2016). It is therefore not possible to differentiate the specific effects of hippocampal involvement on neuropsychological functioning in these preterm born children with VLBW.
Finally, the automated segmentation method used in this study has limitations. Although it overcomes some of the potential problems with manual segmentation; being laborious, less reproducible and with potential bias (Mueller et al., 2018), there are some important short comings. First, only T1-weighted data acquired on a 1.5 T scanner with a resolution of 1.25 × 1.25 × 1.20 mm3 was used. Though, studies have shown that the method is appropriate and reliable in datasets with different resolution and contrast (Iglesias et al., 2015; Whelan et al., 2016), it would have been better to use higher resolution scans and a combination of T1 and T2-weighted images (Iglesias et al., 2015). The accuracy of the automated methods on lower resolution structural data has been questioned (Wisse et al., 2014). However, this method has shown good correlations with manual methods (de Flores et al., 2015; Schmidt et al., 2018) and high test-retest reliability for all subfields except for the hippocampal fissure (Whelan et al., 2016). We also excluded the smaller subfields that are less reliable (hippocampal fissure, parasubiculum, HATA and fimbria). There is also a debate on definitions of subfields and placement of subfield boundaries (Wisse et al., 2017), and therefore a disagreement exists in different manual and automated segmentation protocols. We have partly overcome this obstacle by making composite subfields that are more in line with other automated segmentation protocols, such as ASHS; (Yushkevich et al., 2015) as suggested by Mueller et al. (Mueller et al., 2018). Although more studies comparing the different automated methods are needed, Sone et al. (2016) reported similar results from ASHS and FreeSurfer version 6.0 in a group of epilepsy patients (Sone et al., 2016). Also, the subfield segmentation approach in Freesurfer has not been developed or validated for children. More studies for validation of the subfield segmentation methods in typically developing children as well as children with neurodevelopmental disorders are needed.
5. Conclusions
Our results indicate that hippocampal subfield volumes are differently affected by preterm birth and that the DG may be particularly susceptible to pathophysiological events associated with the preterm brain. The children born preterm with VLBW had reduced verbal and visual working memory function compared to term-born controls, and visual working memory deficits were correlated with reduced volume of the left DG. Both findings indicate an altered brain structure-function relationship in the preterm born. However, larger studies are needed before generalizing our results because of the limited study sample.
Acknowledgement
We are grateful for the participation and cooperation of the children and families in this study. We want to thank radiographer Bjarte Dagfinn Snekvik for coordinating the imaging, and research assistants Irén Aina Bastholm and Elisabeth Mellemstrand Stavnes, and psychologist Heidi Furre Østgård PhD for clinical testing of the children, Tor Ivar Hansen PhD for help calculating intracranial volumes and associate professor Lars Morten Rimol for help with statistical questions. We appreciate the collaboration with Professors Kristine B. Walhovd and Anders M. Fjell of the Lifespan Changes in Brain and Cognition group, Department of Psychology, University of Oslo, Norway. The Abel Cluster owned by the University of Oslo and the Norwegian Metacenter for Computational Science and operated by the Department for Research Computing at the University of Oslo, Center for Information Technology (http://www.hpc.uio.no) was used for image processing. The project received funding from the Research Council of Norway's FRIMED program (project number 204935/F20) and the Liaison Committee for Education, Research and Innovation in Central Norway (project number 46056907).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nicl.2019.101857.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
References
- Aanes S., Bjuland K.J., Skranes J., Løhaugen G.C.C. Memory function and hippocampal volumes in preterm born very-low-birth-weight (VLBW) young adults. NeuroImage. 2015;105 doi: 10.1016/j.neuroimage.2014.10.023. [DOI] [PubMed] [Google Scholar]
- Aggleton J.P., Christiansen K. The subiculum. Prog. Brain Res. 2015;219:65–82. doi: 10.1016/bs.pbr.2015.03.003. [DOI] [PubMed] [Google Scholar]
- Amaral D.G., Scharfman H.E., Lavenex P. The dentate gyrus: fundamental neuroanatomical organization (dentate gyrus for dummies) Prog. Brain Res. 2007;163:3–22. doi: 10.1016/S0079-6123(07)63001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P.J. Neuropsychological outcomes of children born very preterm. Semin. Fetal Neonatal Med. 2014;19(2):90–96. doi: 10.1016/j.siny.2013.11.012. [DOI] [PubMed] [Google Scholar]
- Aslaksen P.M., Bystad M.K., Ørbo M.C., Vangberg T.R. The relation of hippocampal subfield volumes to verbal episodic memory measured by the California Verbal Learning Test II in healthy adults. Behav. Brain Res. 2018;351:131–137. doi: 10.1016/j.bbr.2018.06.008. [DOI] [PubMed] [Google Scholar]
- Auer R.N. Progress Review: Hypoglycemic Brain Damage 699. Stroke. 1986;17 doi: 10.1161/01.str.17.4.699. http://ahajournals.org Retrieved from. [DOI] [PubMed] [Google Scholar]
- Auer R.N. Acute Neuronal Injury: The Role of Excitotoxic Programmed Cell Death Mechanisms. Vol. 146. 2010. Hypoglycemic brain damage; pp. 203–210. [Google Scholar]
- Baddeley A., Jarrold C., Vargha-khadem F. 2011. Working Memory and the Hippocampus, (2007) pp. 3855–3861. [DOI] [PubMed] [Google Scholar]
- Bjuland K.J., Rimol L.M., Løhaugen G.C.C., Skranes J. Brain volumes and cognitive function in very-low-birth-weight (VLBW) young adults. Eur. J. Paediatr. Neurol. 2014;18(5):578–590. doi: 10.1016/j.ejpn.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Bohbot V.D., Allen J.J.B., Nadel L. Memory deficits characterized by patterns of lesions to the hippocampus and parahippocampal cortex. Ann. New York Acad. Sci. 2006;911(1):355–368. doi: 10.1111/j.1749-6632.2000.tb06737.x. [DOI] [PubMed] [Google Scholar]
- Brunnemann N., Kipp K.H., Gortner L., Meng-Hentschel J., Papanagiotou P., Reith W., Shamdeen M.G. Alterations in the relationship between hippocampal volume and episodic memory performance in preterm children. Dev. Neuropsychol. 2013;38(4):226–235. doi: 10.1080/87565641.2013.773003. [DOI] [PubMed] [Google Scholar]
- Burgess N., Maguire E.A., O’Keefe J. Review The Human Hippocampus and Spatial and Episodic Memory. Neuron. 2002;35 doi: 10.1016/s0896-6273(02)00830-9. https://ac.els-cdn.com/S0896627302008309/1-s2.0-S0896627302008309-main.pdf?_tid=c89b6219-d72b-496b-9953-e998aa12aa0e&acdnat=1543688247_445d6e58f4c21c675e950630482a8d10 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Busl K.M., Greer D.M. Hypoxic-ischemic brain injury: Pathophysiology, neuropathology and mechanisms. NeuroRehabilitation. 2010;26:5–13. doi: 10.3233/NRE-2010-0531. [DOI] [PubMed] [Google Scholar]
- Cao B., Passos I.C., Mwangi B., Amaral-Silva H., Tannous J., Wu M.-J.…Soares J.C. Hippocampal subfield volumes in mood disorders. Mol. Psychiatry. 2017;22(9):1352–1358. doi: 10.1038/mp.2016.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L.W., Sun D., Davis S.L., Haswell C.C., Dennis E.L., Swanson C.A.…Morey R.A. Smaller hippocampal CA1 subfield volume in posttraumatic stress disorder. Depress. Anxiety. 2018;35(11):1018–1029. doi: 10.1002/da.22833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale A., Fischl B., Sereno M.I. Cortical surface-based analysis: I. Segmentation and surface reconstruction. NeuroImage. 1999;9(2):179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- de Flores R., La Joie R., Landeau B., Perrotin A., Mézenge F., de La Sayette V.…Chételat G. Effects of age and Alzheimer’s disease on hippocampal subfields. Hum. Brain Mapp. 2015;36(2):463–474. doi: 10.1002/hbm.22640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker A.L., Szulc K.U., Bouffet E., Laughlin S., Chakravarty M.M., Skocic J.…Mabbott D.J. Smaller hippocampal subfield volumes predict verbal associative memory in pediatric brain tumor survivors. Hippocampus. 2017;27(11):1140–1154. doi: 10.1002/hipo.22758. [DOI] [PubMed] [Google Scholar]
- Duvernoy H.M., Cattin F., Risold P.Y., Vannson J.L., Gaudron M. 4th ed. Springer Berlin Heidelberg; Berlin, Heidelberg: 2013. The human hippocampus: Functional anatomy, vascularization and serial sections with MRI, fourth edition. The Human Hippocampus: Functional Anatomy, Vascularization and Serial Sections with MRI, Fourth Edition. [Google Scholar]
- Eldridge L.L., Engel S.A., Zeineh M.M., Bookheimer S.Y., Knowlton B.J. 2005. Behavioral/Systems/Cognitive A Dissociation of Encoding and Retrieval Processes in the Human Hippocampus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn A.S., Sheridan M.A., Kam C.L.H., Hinshaw S., D’Esposito M. Longitudinal evidence for functional specialization of the neural circuit supporting working memory in the human brain. J. Neurosci. 2010;30(33):11062–11067. doi: 10.1523/JNEUROSCI.6266-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischl B., Salat D.~.H., Busa E., Albert M., Dieterich M., Haselgrove C.…Dale A.M. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33:341–355. doi: 10.1016/s0896-6273(02)00569-x. [DOI] [PubMed] [Google Scholar]
- Fischl Bruce, van der Kouwe A., Destrieux C., Halgren E., Ségonne F., Salat D.H.…Dale A.M. Automatically parcellating the human cerebral cortex. Cerebral Cortex. 2004;14(1):11–22. doi: 10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- Gadian D.G., Aicardi J., Watkins K.E., Porter D.A., Mishkin M., Vargha-Khadem F. 2000. Developmental amnesia associated with early hypoxic-ischaemic injury. Brain, 123 Pt 3; pp. 499–507.http://brain.oxfordjournals.org/content/123/3/499.full.pdf Retrieved from. [DOI] [PubMed] [Google Scholar]
- Hansen T.I., Brezova V., Eikenes L., Håberg A., Vangberg T.R. How does the accuracy of intracranial volume measurements affect normalized brain volumes? sample size estimates based on 966 subjects from the HUNT MRI cohort. Am. J. Neuroradiol. 2015;36(8):1450–1456. doi: 10.3174/ajnr.A4299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes J.P., Hayes S., Miller D.R., Lafleche G., Logue M.W., Verfaellie M. Automated measurement of hippocampal subfields in PTSD: Evidence for smaller dentate gyrus volume. J. Psychiatr. Res. 2017;95:247–252. doi: 10.1016/j.jpsychires.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J.P., Mueller N.K. Role of the ventral subiculum in stress integration. Behav. Brain Res. 2006;174(2):215–224. doi: 10.1016/j.bbr.2006.05.035. [DOI] [PubMed] [Google Scholar]
- Herten A., Konrad K., Krinzinger H., Seitz J., von Polier G.G. Accuracy and bias of automatic hippocampal segmentation in children and adolescents. Brain Struct. Funct. 2018:1–16. doi: 10.1007/s00429-018-1802-2. [DOI] [PubMed] [Google Scholar]
- Hollinghead A. 1957. Two factor index of social position. [Google Scholar]
- Huang Y., Coupland N.J., Lebel R.M., Carter R., Seres P., Wilman A.H., Malykhin N.V. Structural changes in hippocampal subfields in major depressive disorder: a high-field magnetic resonance imaging study. Biol. Psychiatry. 2013;74(1):62–68. doi: 10.1016/j.biopsych.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Iglesias J.E., Augustinack J.C., Nguyen K., Player C.M., Player A., Wright M., Leemput …., Van K. A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: Application to adaptive segmentation of in vivo MRI, for the Alzheimer’s Disease Neuroimaging Initiative 1. NeuroImage. 2015;115:117–137. doi: 10.1016/j.neuroimage.2015.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob F.D., Habas P.A., Kim K., Corbett-Detig J., Xu D., Studholme C., Glenn O.A. Fetal hippocampal development: analysis by magnetic resonance imaging volumetry. Pediatr. Res. 2011;69(5 Pt 1):425–429. doi: 10.1203/PDR.0b013e318211dd7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkman M., Kemp S. Hogrefe Psykologiförlaget AB; 2002. A Developmental NEuroPSYchological Assessment (NEPSY) (Norwegian version) [Google Scholar]
- Krogsrud S.K., Tamnes C.K., Fjell A.M., Amlien I., Grydeland H., Sulutvedt U.…Walhovd K.B. Development of hippocampal subfield volumes from 4 to 22 years. Hum. Brain Mapp. 2014;35(11):5646–5657. doi: 10.1002/hbm.22576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnus P., Irgens L.M., Haug K., Nystad W., Skjaerven R., Stoltenberg C., MoBa Study Group Cohort profile: the Norwegian Mother and Child Cohort Study (MoBa) Int. J. Epidemiol. 2006;35(5):1146–1150. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- Mammarella I.C., Cornoldi C. Sequence and space: The critical role of a backward spatial span in the working memory deficit of visuospatial learning disabled children. Cognitive Neuropsychol. 2005;22(8):1055–1068. doi: 10.1080/02643290442000509. [DOI] [PubMed] [Google Scholar]
- Matsumoto N., Kitanishi T., Mizuseki K. The subiculum: Unique hippocampal hub and more. Neurosci. Res. 2018 doi: 10.1016/j.neures.2018.08.002. [DOI] [PubMed] [Google Scholar]
- McHugo M., Talati P., Woodward N.D., Armstrong K., Blackford J.U., Heckers S. 2018. Regionally specific volume deficits along the hippocampal long axis in early and chronic psychosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers J.E., Meyers K.R. Assesio Norge AS; Oslo: 2004. Rey complex figure test and recognition trial manual (norwegian version 2004) ISBN: 9174183060. [Google Scholar]
- Morris R. Stress and the hippocampus. In: Anderson T., Morris R., Amaral D., O'Keefe J., Bliss T., editors. The Hippocampus Book. 1st ed. Oxford University Press; 2007. pp. 751–768. [Google Scholar]
- Mueller S.G., Chao L.L., Berman B., Weiner M.W. Evidence for functional specialization of hippocampal subfields detected by MR subfield volumetry on high resolution images at 4 T. NeuroImage. 2011;56(3):851–857. doi: 10.1016/j.neuroimage.2011.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller Susanne G., Yushkevich P.A., Das S., Wang L., Van Leemput K., Iglesias J.E.…Alzheimer’s Disease Neuroimaging Initiative, for the A. D. N Systematic comparison of different techniques to measure hippocampal subfield volumes in ADNI2. NeuroImage. Clinical. 2018;17:1006–1018. doi: 10.1016/j.nicl.2017.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahara S., Matsumoto M., van Erp T.G.M. Hippocampal subregion abnormalities in schizophrenia: A systematic review of structural and physiological imaging studies. Neuropsychopharmacol. Rep. 2018 doi: 10.1002/npr2.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura Y., Nakashima T., Fukuda S., Nakashima H., Hashimoto T. Hypoxic-ischemic brain lesions found in asphyxiating neonates. Acta Pathologica Japonica. 1986;36(4):551–563. doi: 10.1111/j.1440-1827.1986.tb01044.x. http://www.ncbi.nlm.nih.gov/pubmed/3728012 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Newnham C.A., Inder T.E., Milgrom J. Measuring preterm cumulative stressors within the NICU: The neonatal infant stressor scale. Early Hum. Dev. 2009;85:549–555. doi: 10.1016/j.earlhumdev.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Nosarti C., Al-Asady M.H., Frangou S., Stewart A.L., Rifkin L., Murray R.M. Adolescents who were born very preterm have decreased brain volumes. Brain. 2002;125:1616–1623. doi: 10.1093/brain/awf157. http://brain.oxfordjournals.org/content/125/7/1616.full.pdf Pt 7. Retrieved from. [DOI] [PubMed] [Google Scholar]
- Nosarti C., Froudist-Walsh S. Alterations in development of hippocampal and cortical memory mechanisms following very preterm birth. Dev. Med. Child Neurol. 2016;58:35–45. doi: 10.1111/dmcn.13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mara S.M., Sanchez-Vives M.V., Brotons-Mas J.R., O’Hare E. Roles for the subiculum in spatial information processing, memory, motivation and the temporal control of behaviour. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2009;33:782–790. doi: 10.1016/j.pnpbp.2009.03.040. [DOI] [PubMed] [Google Scholar]
- Omizzolo C., Scratch S.E., Stargatt R., Kidokoro H., Thompson D.K., Lee K.J.…Anderson P.J. 2013. Neonatal brain abnormalities and memory and learning outcomes at 7 years in children born very preterm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ørbo M.C., Vangberg T.R., Tande P.M., Anke A., Aslaksen P.M. Memory performance, global cerebral volumes and hippocampal subfield volumes in long-term survivors of Out-of-Hospital Cardiac Arrest. Resuscitation. 2018;126:21–28. doi: 10.1016/j.resuscitation.2018.02.011. [DOI] [PubMed] [Google Scholar]
- Perneger T.V. What’s wrong with Bonferroni adjustments. BMJ (Clinical Research Ed.) 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. http://www.ncbi.nlm.nih.gov/pubmed/9553006 Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter M., Rosas H.D., Fischl B. Highly Accurate Inverse Consistent Registration: A Robust Approach. NeuroImage. 2010;53(4):1181–1196. doi: 10.1016/j.neuroimage.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt-Kastner R., Freund T.F. Selective vulnerability of the hippocampus in brain ischemia. Neuroscience. 1991;40(3):599–636. doi: 10.1016/0306-4522(91)90001-5. [DOI] [PubMed] [Google Scholar]
- Schmidt M.F., Storrs J.M., Freeman K.B., Jack C.R., Turner S.T., Griswold M.E., Mosley T.H. A comparison of manual tracing and FreeSurfer for estimating hippocampal volume over the adult lifespan. Hum. Brain Mapp. 2018;39(6):2500–2513. doi: 10.1002/hbm.24017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scoville W., Milner B. Scoville&Milner, Loss of Recent Memory After Bilateral Hippocampal Lesions, 2000.pdf. J. Neuropsychiatry Clin. Neurosci. 2000;12(1):103–113. doi: 10.1176/jnp.12.1.103. [DOI] [PubMed] [Google Scholar]
- Segonne F., Dale A.M., Busa E., Glessner M., Salat D., Hahn H.K., Fischl B. A hybrid approach to the skull stripping problem in MRI. NeuroImage. 2004;22(3):1060–1075. doi: 10.1016/j.neuroimage.2004.03.032. [DOI] [PubMed] [Google Scholar]
- Sharma A., Davis A., Shekhawat P.S. Hypoglycemia in the preterm neonate: etiopathogenesis, diagnosis, management and long-term outcomes. Translational Pediatrics. 2017;6(4):335–348. doi: 10.21037/tp.2017.10.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sizonenko S.V., Borradori-Tolsa C., Vauthay D.M., Lodygensky G., Lazeyras F., Hüppi P.S. Impact of intrauterine growth restriction and glucocorticoids on brain development: Insights using advanced magnetic resonance imaging. Mol. Cell. Endocrinol. 2006;254(255):163–171. doi: 10.1016/j.mce.2006.04.035. [DOI] [PubMed] [Google Scholar]
- Small S.A. Age-Related Memory Decline. Arch. Neurol. 2001;58(3):360–364. doi: 10.1001/archneur.58.3.360. [DOI] [PubMed] [Google Scholar]
- Smith G.C., Gutovich J., Smyser C., Pineda R., Newnham C., Tjoeng T.H.…Inder T. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann. Neurol. 2011 doi: 10.1002/ana.22545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sølsnes A.E., Grunewaldt K.H., Bjuland K.J., Stavnes E.M., Bastholm I.A., Aanes S.…Rimol L.M. Cortical morphometry and IQ in VLBW children without cerebral palsy born in 2003-2007. NeuroImage: Clinical. 2015;8 doi: 10.1016/j.nicl.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sølsnes A.E., Sripada K., Yendiki A., Bjuland K.J., Østgård H.F., Aanes S.…Skranes J. Limited microstructural and connectivity deficits despite subcortical volume reductions in school-aged children born preterm with very low birth weight. NeuroImage. 2016;130 doi: 10.1016/j.neuroimage.2015.12.029. [DOI] [PubMed] [Google Scholar]
- Sone D., Sato N., Maikusa N., Ota M., Sumida K., Yokoyama K.…Matsuda H. Automated subfield volumetric analysis of hippocampus in temporal lobe epilepsy using high-resolution T2-weighed MR imaging. NeuroImage. Clinical. 2016;12:57–64. doi: 10.1016/j.nicl.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sripada K., Bjuland K.J., Sølsnes A.E., Håberg A.K., Grunewaldt K.H., Løhaugen G.C., Skranes J. Trajectories of brain development in school-age children born preterm with very low birth weight. Sci. Rep. 2018;8(1) doi: 10.1038/s41598-018-33530-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark C. Functional role of the human hippocampus. In: Andersen J., Morris R., Amaral D., Bliss T., O'Keefe, editors. The Hippocampus Book. 1st ed. Oxford University Press; 2007. pp. 549–580. [Google Scholar]
- Stretton J., Winston G., Sidhu M., Centeno M., Vollmar C., Bonelli S.…Thompson P.J. Neural correlates of working memory in Temporal Lobe Epilepsy — An fMRI study. NeuroImage. 2012;60:1696–1703. doi: 10.1016/j.neuroimage.2012.01.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suthana N., Ekstrom A., Moshirvaziri S., Knowlton B., Bookheimer S. Dissociations within human hippocampal subregions during encoding and retrieval of spatial information. Hippocampus. 2011;21(7):694–701. doi: 10.1002/hipo.20833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamnes C.K., Walhovd K.B., Engvig A., Grydeland H., Krogsrud S.K., Østby Y.…Fjell A.M. Regional hippocampal volumes and development predict learning and memory. Dev. Neurosci. 2014;36(3–4):161–174. doi: 10.1159/000362445. [DOI] [PubMed] [Google Scholar]
- Tamnes C.K., Walhovd K.B., Grydeland H., Holland D., Østby Y., Dale A.M., Fjell A.M. Longitudinal Working Memory Development Is Related to Structural Maturation of Frontal and Parietal Cortices. J. Cogn. Neurosci. 2013;25(10):1611–1623. doi: 10.1162/jocn_a_00434. [DOI] [PubMed] [Google Scholar]
- Teicher M.H., Anderson C.M., Polcari A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc. Natl. Acad. Sci. U. S. A. 2012;109(9):E563–E572. doi: 10.1073/pnas.1115396109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson D.K., Adamson C., Roberts G., Faggian N., Wood S.J., Warfield S.K.…Inder T.E. Hippocampal shape variations at term equivalent age in very preterm infants compared with term controls: perinatal predictors and functional significance at age 7. NeuroImage. 2013;70:278–287. doi: 10.1016/j.neuroimage.2012.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson D.K., Omizzolo C., Adamson C., Lee K.J., Stargatt R., Egan G.F.…Anderson P.J. Longitudinal growth and morphology of the hippocampus through childhood: Impact of prematurity and implications for memory and learning. Hum. Brain Mapp. 2014;35(8):4129–4139. doi: 10.1002/hbm.22464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis S., Coupland N.J., Silversone P.H., Huang Y., Fujiwara E., Carter R.…Malykhin N.V. Dentate gyrus volume and memory performance in major depressive disorder. J. Affect. Disord. 2015;172:159–164. doi: 10.1016/j.jad.2014.09.048. [DOI] [PubMed] [Google Scholar]
- Tulving E., Markowitsch H.J. Episodic and declarative memory: Role of the hippocampus. Hippocampus. 1998;8(3):198–204. doi: 10.1002/(SICI)1098-1063(1998)8:3<198::AID-HIPO2>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- Volpe J.J. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe J.J. Neonatal encephalopathy: an inadequate term for hypoxic-ischemic encephalopathy. Ann. Neurol. 2012;72(2):156–166. doi: 10.1002/ana.23647. [DOI] [PubMed] [Google Scholar]
- Walker M., Chan D., Thom M., Andersen J., Morris R., Amaral D., Bliss T. Hippocampus and human disease. In: O'Keefe, editor. The Hippocampus Book. 1st ed. Oxford University Press; 2007. [Google Scholar]
- Wang G.-W., Cai J.-X. Disconnection of the hippocampal–prefrontal cortical circuits impairs spatial working memory performance in rats. Behav. Brain Res. 2006;175(2):329–336. doi: 10.1016/j.bbr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Wechsler D. The Psychological Corporation; 1997. Wechsler Memory Scale, third edition. [Google Scholar]
- Wechsler D. Pearson; 1999. Wechsler Abbreviated Scale of Intelligence. [Google Scholar]
- Wechsler D. 3rd edition. Pearson; 2002. Wechsler Preschool and Primary Scale of Intelligence. (Norwegian version 2008. [Google Scholar]
- Wechsler D. fourth edition. Pearson; 2003. Wechsler Intelligence Scale for Children. Norwegian version, 2009. [Google Scholar]
- Whelan C.D., Hibar D.P., Van Velzen L.S., Zannas A.S., Carrillo-Roa T., McMahon K.Z.…Thompson P.M. Heritability and reliability of automatically segmented human hippocampal formation subregions. NeuroImage. 2016 doi: 10.1016/j.neuroimage.2015.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winston Gavin P., Stretton Jason, Sidhu Meneka K., Symms R., Thompson J., Duncan S. 2013. Structural correlates of impaired working memory in hippocampal sclerosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisse L.E.M., Biessels G.J., Geerlings M.I. A critical appraisal of the hippocampal subfield segmentation package in FreeSurfer. Front. Aging Neurosci. 2014;6 doi: 10.3389/fnagi.2014.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisse L.E.M., Daugherty A.M., Olsen R.K., Berron D., Carr V.A., Stark C.E.L.…la Joie R. A harmonized segmentation protocol for hippocampal and parahippocampal subregions: Why do we need one and what are the key goals? Hippocampus. 2017;27(1):3–11. doi: 10.1002/hipo.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xavier G.F., Costa V.C.I. Dentate gyrus and spatial behaviour. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2009;33(5):762–773. doi: 10.1016/j.pnpbp.2009.03.036. [DOI] [PubMed] [Google Scholar]
- Yushkevich P.A., Pluta J.B., Wang H., Xie L., Ding S.-L., Gertje E.C.…Wolk D.A. Automated volumetry and regional thickness analysis of hippocampal subfields and medial temporal cortical structures in mild cognitive impairment. Hum. Brain Mapp. 2015;36(1):258–287. doi: 10.1002/hbm.22627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zammit A.R., Ezzati A., Zimmerman M.E., Lipton R.B., Lipton M.L., Katz M.J. Roles of hippocampal subfields in verbal and visual episodic memory. Behav. Brain Res. 2017;317:157–162. doi: 10.1016/j.bbr.2016.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2