Abstract
BACKGROUND
Right hemicolectomy or ileocecal resection are used to treat benign conditions like Crohn’s disease (CD) and malignant ones like colon cancer (CC).
AIM
To investigate differences in pre- and peri-operative factors and their impact on post-operative outcome in patients with CC and CD.
METHODS
This is a sub-group analysis of the European Society of Coloproctology’s prospective, multi-centre snapshot audit. Adult patients with CC and CD undergoing right hemicolectomy or ileocecal resection were included. Primary outcome measure was 30-d post-operative complications. Secondary outcome measures were post-operative length of stay (LOS) at and readmission.
RESULTS
Three hundred and seventy-five patients with CD and 2,515 patients with CC were included. Patients with CD were younger (median = 37 years for CD and 71 years for CC (P < 0.01), had lower American Society of Anesthesiology score (ASA) grade (P < 0.01) and less comorbidity (P < 0.01), but were more likely to be current smokers (P < 0.01). Patients with CD were more frequently operated on by colorectal surgeons (P < 0.01) and frequently underwent ileocecal resection (P < 0.01) with higher rate of de-functioning/primary stoma construction (P < 0.01). Thirty-day post-operative mortality occurred exclusively in the CC group (66/2515, 2.3%). In multivariate analyses, the risk of post-operative complications was similar in the two groups (OR 0.80, 95%CI: 0.54-1.17; P = 0.25). Patients with CD had a significantly longer LOS (Geometric mean 0.87, 95%CI: 0.79-0.95; P < 0.01). There was no difference in re-admission rates. The audit did not collect data on post-operative enhanced recovery protocols that are implemented in the different participating centers.
CONCLUSION
Patients with CD were younger, with lower ASA grade, less comorbidity, operated on by experienced surgeons and underwent less radical resection but had a longer LOS than patients with CC although complications' rate was not different between the two groups.
Keywords: Crohn’s disease, Colon cancer, Complications, Length of stay, Bowel resection, Right hemicolectomy
Core tip: This paper shows that patients with Crohn’s disease (CD) have longer post-operative stay at the hospital although they were younger than those with colon cancer (CC), had a lower American Society of Anesthesiology score grade and had less comorbidity. They were also operated on by experienced surgeons and had undergone less radical resection than those with CC. This may stimulate further researches to investigate the factors influencing post-operative length of stay at hospital in patients with CD.
INTRODUCTION
Surgery is definitive treatment for patients with colon cancer (CC) and an option for patients with Crohn’s disease (CD) in case of complications or non-response to medical treatment.
CC and CD have some common features like geographical distribution where both diseases have high incidence in western countries. Incidences are rising in countries adopting western lifestyles[1,2], and among immigrants from low-incidence countries that move to western countries, suggesting that lifestyle is a risk factor[3,4]. Inexpedient diet and smoking are well known risk factors for both CC and CD[5-8]. Moreover, there is an evidence of genetic components in the pathogenesis of both diseases[2,9].
The two diseases differ in incidence. CD incidence is higher among women and the average age at diagnosis is approximately 30 years[10]. In contrast, the incidence of CC is slightly higher among men[11,12], with 90% of patients over 50 years when diagnosed[13]. Although bowel resection is performed for both diseases, the techniques implemented may differ. The extent of resection in CC is based on vascular supply and lymphatic drainage of the tumour. Therefore, central ligation of tumour draining blood vessels, lymph nodes harvest and free resection margin are important[11]. In contrast, central ligation of blood vessels and lymph nodes harvest are less important for patients with CD. The disease-free resection margin might influence recurrence rate[14,15].
Literature search showed no large prospective study investigating the effect of pre- and peri-operative risk factors in CD and CC on post-operative outcome. Retrospective and small series prospective studies showed divergent results[16-21]. There is a need for a large prospective study investigating post-operative outcome in patients with CC and CD to identify areas warranting further research like allocation of resources, pre-operative optimization and surgical techniques in the two patient groups respectively.
The aim of this study is to investigate differences in pre- and peri-operative factors and their impact on post-operative outcome in patients with CC and CD undergoing Right hemicolectomy or ileocecal resection. The two groups have previously been investigated separately within the ESCP snapshot audit, but this analysis presents the two in the same paper to demonstrate how the same surgical procedure have different post-operative outcome depending on the underlying disease.
MATERIALS AND METHODS
Patients
The ESCP snapshot audit included adult patients undergoing right hemicolectomy or ileocecal resection, regardless of the operative approach, in both elective and emergency settings. The inclusion period extended over a 2-mo period from January 15th to March 15th, 2015. Thirty-day post-operative outcome was reported. Details of centre inclusion, data entry and collection, follow up, approvals and patient recruit-ment as well as inclusion and exclusion criteria were based on a prespecified protocol[22] and have been explained in the main study of this audit[23]. No details about enhanced recovery after surgery program were registered in the snapshot audit however, ERAS is now standard in most of the world. Criteria for admission to critical care unit was decided by routine guidelines in the participating centers. Details on pre-operative characteristics, surgery for CD and post-operative outcome in patients with CD is explained in the recently published paper on this cohort24 while details about the CC cohort are reported in another paper (in press). ESCP study on CD reported pre-operative characteristics and indication for surgical interventions in CD. It investigated and adjusted for risk factors which are specific to CD[24] for example steroid, biological treatment and pre-operative sepsis while the other cohort studied factors specific for CC like chemotherapy, details of resection and anastomosis.
Outcome measures
Primary outcome measure was 30-d overall post-operative complication. Secondary outcome measures were post-operative length of stay (LOS) in hospital measured in days after operation and re-admission rates. Clinically suspected anastomosis leak, intraabdominal pelvic collection, surgical site infection (SSI) and reoperation were investigated as specific complications.
Statistical analysIs
For univariate analyses, Mann-Whitney U test was used to test continuous variables while categorical variables were tested using Pearson’s Chi-Square or Fisher’s exact test when relevant. Continuous variables were reported by median and interquartile range (IQR) while categorical variables were reported as frequencies. Variables that showed a significant association with the outcome in the univariate analyses (P < 0.05) and variables deemed clinically important were included as covariates in the multivariate analysis model. We used logistic regression models for binary outcome variables (e.g., complication yes/no) and linear regression models for the continuous variables. Results of the logistic regression analyses are presented as odds ratios (OR) with corresponding 95% confidence intervals (CI). The LOS variable was log-transformed, and results of the linear regression models are presented as the geometric mean with corresponding 95%CI. P-value < 0.05 was considered statis-tically significant. Statistician (RN) chose geometric mean due to the type of data from the audit. A multivariate model was constructed for each of the outcome variables that the study investigated. Analyses were performed with SPSS (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.2010) and the R statistical software version 3.2.2.
RESULTS
The ESCP snapshot audit included 3208 patients from 284 centres in 39 countries. The included patients underwent ileo-ceal resection or right hemi-coloectomy due to CC, CD or other reasons. Overall data completeness record in this audit was 97.4%. This is a sub group analysis of the original data from the audit. This subgroup includes 375 patients with CD and 2,515 patients with CC.
Pre- and peri-operative characterization
Patients with CD were significantly different from those with CC in most of the pre-operative characteristics as shown in Table 1. Patients with CD were predominantly female, more likely to be smokers and had more previous surgeries. In contrast patients with CC were older, had higher body mass index (BMI), more comorbidities, higher serum creatinine and lower haemoglobin. Patients with CD were more likely to be operated on by colorectal surgeons 83.5% (313/375) compared to patients with CC 71.5% (1798/2515, P < 0.01). Two thirds of patients with CD had ileocecal resection while almost all patients with CC had right hemicolectomy. Details of anastomosis explained in the main study[23]. Patients with CD were at higher risk of de-functioning/primary stoma construction compared to patients with CC (P < 0.01). The rate of unplanned intraoperative adverse events (UIAE) was higher in CD (14.9%) compared to CC (9.15%).
Table 1.
Patients’ demographics, pre- and peri-operative patient characterization n (%)
| Variables | CC n = 2515 | CD n = 375 | P value |
| Age (yr)1 | 71 (15) | 37 (23) | < 0.01 |
| Haemoglobin (g/dL)1 | 11.9 (3) | 12.8 (2) | < 0.01 |
| Gender Male Female | 1310 (52.1) 1205 (48.9) | 161 (42.9) 214 (57.1) | 0.01 |
| History of diabetes | 463 (18.4) | 7 (1.9) | < 0.01 |
| History of IHD | 548 (21.8) | 10 (2.7) | < 0.01 |
| BMI ≤ 18.5 18.6-25 25.1-30 > 30 Missing | 57 (2.5) 926 (39.9) 867 (37.4) 468 (20.2) 197 (7.8) | 43 (12.4) 209 (60.4) 72 (20.8) 22 (6.4) 29 (7.7) | < 0.01 |
| ASA grade I II III IV V | 250 (9.9) 1261 (50.1) 903 (35.9) 98 (3.9) 3 (0.01) | 88 (23.5) 239 (63.7) 45 (12.0) 3 (0.8) 0 (0) | < 0.01 |
| Abnormal s. creatinine | 294 (11.6) | 13 (3.5) | < 0.01 |
| Smoking status Non-smoker Current smoker Ex-smoker Missing | 1587 (63.1) 268 (10.7) 486 (19.3) 174 (6.9) | 219 (58.4.1) 81 (23.1) 52 (14.8) 23 (6.1) | < 0.01 |
| Previous surgery in the area | 607 (24.1) | 122 (32.5) | < 0.01 |
| Urgency of surgery Elective/expedited Emergency | 2216 (88.1) 299 (11.9) | 321 (85.6) 54 (14.4) | 0.130 |
| Surgeon in charge Colorectal surgeon General surgeon | 1798 (71.5) 717 (28.5) | 313 (83.5) 62 (16.5) | < 0.01 |
| Operative approach Laparoscopy Converted to open Open | 1221 (48.5) 219 (8.7) 1075 (42.7) | 177 (47.2) 42 (11.2) 156 (41.6) | 0.317 |
| Type of resection Ileocecal resection Right hemicolectomy | 125 (5.0) 2390 (95.0) | 266 (70.9) 109 (29.1) | < 0.01 |
| De-functioning stoma | 78 (3.1) | 46 (12.3) | < 0.01 |
| Skin closure technique Suture closure Stapled Others | 842 (33.5) 1450 (57.7) 223 (8.9) | 196 (52.2) 145 (38.7) 34 (9.1) | < 0.01 |
| Unplanned Intra-operative events2 | 230 (9.15) | 56 (14.9) | < 0.01 |
| Duration of operation (minutes)1 | 130 (65) | 128 (59) | 0.831 |
Patients with Crohn’s disease were younger, with lower American Society of Anesthesiology score grade, less comorbidity, operated on by experienced surgeons and underwent less extensive surgery. Pre- and peri-operative patient characterization (n/%). Missing data were observed in the following variables: “Age”, “BMI”, “Smoking status”, “Haemoglobin” and “Duration of operation”.
Median (IQR);
Some patients may have more than one unplanned intra-operative event. IHD: Ischemic heart diseases; CRP: C-reactive protein; BMI: Body mass index; CD: Crohn’s disease; CC: Colon cancer; UIAEs: Unplanned intraoperative adverse events; ASA: American Society of Anesthesiology score.
Univariate analysis of post-operative outcomes
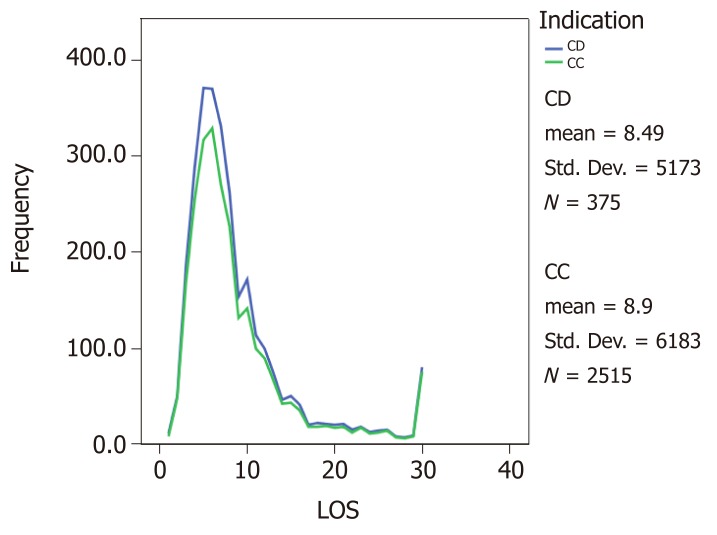
In unadjusted analysis, both groups had a median LOS in hospital of 7.0 d (IQR 5.0) as shown in Figure 1. There was no significant difference in risk of post-operative complications (33.6% in CD vs 38% in CC, P = 0.099). A closer look at anastomotic leak, SSI and reoperation did not show a significant difference between the two groups. Nevertheless, CC patients were more likely to be admitted to a critical care unit (773/2515, 30.7%) compared to patients with CD (70/375, 18.7%, P < 0.01). Sixty-six patients with CC died within the follow up period (2.3%) while no mortality was reported in patients with CD [details about causes of death are explained in the study of CC cohort (in press)]. Post-operative CRP levels (within first 3 d) were significantly higher in patients with CD [median (IQR) 133 (162)] compared to patients with CC [108 (134), P < 0.01].
Figure 1.
Post-operative length of stay at hospital in patients with Crohn’s disease compared to those with colon cancer. CD: Crohn’s disease; CC: Colon cancer; LOS: Length of stay.
Multivariate analyses
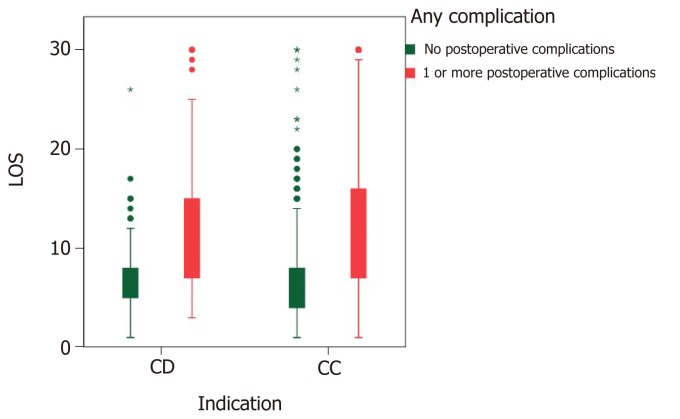
After adjustment for confounding factors the risk of post-operative complications and the risk of admission to critical care unit were not significantly different between the two cohorts (OR 0.80, 95%CI: 0.54-1.17 and OR 1.43, 95%CI: 0.94-2.18, respectively), as shown in Table 2. However, patients with CC had a significantly shorter stay in hospital compared to patients with CD (Geometric mean 0.87, 95%CI: 0.79-0.95). Factors associated with longer LOS are shown in Table 3.
Table 2.
Risk factors of post-operative complications in multivariate analyses
| Variable | Units | OR | 95%CI | P value |
| Indication | CC vs CD | 0.80 | 0.54-1.17 | 0.25 |
| Gender | Male vs female | 1.53 | 1.28-1.83 | < 0.01a |
| Age | Years | 1.01 | 1.01-1.02 | < 0.01a |
| BMI | ≤ 18.5 vs 18.6-25 | 1.37 | 0.87-2.17 | 0.18 |
| 25.1-30 vs 18.6-25 > 30 vs 18.6-25 | 0.88 1.11 | 0.72-1.07 0.87-1.42 | 0.21 0.39 | |
| ASA grade | IV-V vs I-III | 1.63 | 1.04-2.56 | 0.03 |
| IHD | IHD vs no IHD | 1.17 | 0.94-1.46 | 0.16 |
| Diabetes | History of diabetes vs no history of diabetes | 1.05 | 0.84-1.32 | 0.66 |
| Smoking | Ex-smoker vs never smoker | 1.27 | [1.02-1.58 | 0.04a |
| Current smoker vs never smoker | 1.31 | 1.01-1.70 | 0.04a | |
| Haemoglobin | 0.99 | 0.95-1.03 | 0.62 | |
| Operating surgeon | General surgeon vs colorectal surgeon | 1.11 | 0.91-1.34 | 0.31 |
| Urgency | Emergency vs eLective/expedited | 1.55 | 1.18-2.05 | < 0.01a |
| De-functioning/primary stoma | De-functioning stoma vs no de-functioning stoma | 1.13 | 0.52-2.45 | 0.77 |
| Duration of operation | ≥ 120 min vs < 120 min | 1.34 | 1.13-1.59 | < 0.01a |
| Operative approach | Converted vs laparoscopy | 0.97 | 0.72-1.32 | 0.85 |
| Open vs laparoscopy | 1.52 | 1.24-1.85 | < 0.01a | |
| Unplanned intraoperative adverse events | Any UIAES vs no UIAEs | 1.54 | 1.21-1.95 | < 0.01a |
| CRP | 1.01 | 1.00-1.01 | < 0.01a | |
| Previous surgery | Any previous surgery vs no previous surgery | 1.26 | 1.04-1.52 | 0.02a |
| Resection type | Right hemicolectomy vs ileocecal resection | 0.86 | 0.63-1.19 | 0.37 |
| Skin closure | Stapled vs suture | 1.44 | 1.19-1.75 | < 0.01a |
Logistic regression. The model was adjusted for: Gender, age, BMI, ASA grade, ischemic heart disease, diabetes, smoking, haemoglobin, operating surgeon, urgency, defunctioning/primary stoma, duration of operation, operative approach, anastomosis type, unplanned intraoperative adverse events, CRP, previous surgery, resection type and skin closure.
Significant outcomes. IHD: Ischemic heart diseases; CRP: C-reactive protein; BMI: Body mass index; CD: Crohn’s disease; CC: Colon cancer; UIAEs: Unplanned intraoperative adverse events; ASA: American Society of Anesthesiology score.
Table 3.
Risk factors affecting the post-operative length of stay at hospital in multivariate analyses
| Variable | Units | Estimates | 95%CI | P value |
| Indication | CC vs CD | 0.87 | 0.79; 0.95 | < 0.01a |
| Gender | male vs female | 1.06 | 1.01; 1.10 | 0.01a |
| Age | 1.01 | 1.00; 1.01 | < 0.01a | |
| BMI | ≤18.5 vs 18.6-25 | 1.23 | 1.10; 1.38 | < 0.01a |
| 25.1-30 vs 18.6-25 >30 vs 18.6-25 | 0.98 1.04 | 0.92; 1.04 0.96; 1.12 | 0.54 0.35 | |
| ASA grade | IV-V vs I-III | 1.04 | 0.94; 1.16 | 0.45 |
| IHD | IHD vs no IHD | 1.07 | 1.01; 1.13 | 0.01a |
| Diabetes | History of diabetes vs no history of diabetes | 1.02 | 0.96; 1.08 | 0.50 |
| Smoking | Ex-smoker vs never smoker | 0.98 | 0.92; 1.04 | 0.43 |
| Current smoker vs never smoker | 1.05 | 0.98; 1.11 | 0.15 | |
| Haemoglobin | 0.99 | 0.98; 1.00 | 0.06 | |
| Operating surgeon | General surgeon vs colorectal surgeon | 1.10 | 1.05; 1.15 | < 0.01a |
| Urgency | Emergency vs elective/expedited | 1.06 | 0.99; 1.14 | 0.08 |
| De-functioning/primary stoma | De-functioning stoma vs no de-functioning stoma | 1.46 | 1.21; 1.77 | < 0.01a |
| Duration of operation | ≥ 120 vs < 120 | 1.08 | 1.04; 1.13 | < 0.01a |
| Operative approach | Converted vs laparoscopy | 1.10 | 1.02; 1.18 | 0.01a |
| Open vs laparoscopy | 1.35 | 1.29; 1.42 | < 0.01a | |
| Unplanned intraoperative adverse events | Any UIAES vs no UIAEs | 1.08 | 1.02; 1.15 | 0.01a |
| CRP | 1.00 | 1.00; 1.00 | < 0.01a | |
| Previous surgery | Any previous surgery vs no previous surgery | 1.03 | 0.98; 1.08 | 0.23 |
| Resection type | Right hemicolectomy vs ileocecal resection | 1.03 | 0.96; 1.11 | 0.42 |
| Skin closure | Stapled vs suture | 1.06 | 1.01; 1.11 | 0.02a |
Linear regression: The outcome is log-transformed. The model is adjusted for: Gender, age, BMI, ASA grade, ischemic heart disease, diabetes, smoking, haemoglobin, operating surgeon, urgency, defunctioning/primary stoma, duration of operation, operative approach, anastomosis type, unplanned intraoperative adverse events, CRP, previous surgery, resection type and skin closure.
Significant outcomes. IHD: Ischemic heart diseases; CRP: C-reactive protein; BMI: Body mass index; CD: Crohn’s disease; CC: Colon cancer; UIAEs: Unplanned intraoperative adverse events; ASA: American Society of Anesthesiology score.
Post-operative complications do not explain the longer LOS in patients with CD as Figure 2 illustrates. Emergency surgery increased the risk of complications (OR 1.55, 95%CI: 1.18-2.05, P = 0.002) and admission to critical care unit (OR 1.47, 95%CI: 1.12-1.93, P = 0.006) in the combined cohort data of CD and CD. There was, however, no significant difference between patients with CD and patients with CC who underwent emergency surgery.
Figure 2.
Post-operative length of stay at hospital in patients with Crohn’s disease compared to those with colon cancer showing length of stay in patients with and without post-operative complications. CD: Crohn’s disease; CC: Colon cancer; LOS: Length of stay.
DISCUSSION
This study showed that patients with CD had the same risk of post-operative complications but longer post-operative LOS at hospital compared to patients with CC. To the authors knowledge, this has not previously been investigated in a prospective study. A large retrospective database study, examining the cost of elective surgery for diverticulitis compared to other diseases, found that patients with inflammatory bowel diseases (IBD) were more likely to develop post-operative complications, compared to patients with CC[16]. An older retrospective study found higher morbidity and mortality rates for patients with CC compared to patients with IBD[17]. A recent retrospective observational study including 109 patients found no significant differences between patients with CC and CD regarding risk of post-operative complications, anastomotic leakage, SSI and death[18]. In other smaller series studies, SSI rates were higher in patients with CD compared to patients with CC[19,20]. However, no difference in readmission rates was shown[21].
Tables 2 and 3 show pre- and peri-operative risk factors and their effect on post-operative outcome. Patients with CC might have higher risk of post-operative complications and longer LOS due to their older age, higher pre-operative creatinine, higher American Society of Anesthesiology score (ASA) grade, comorbidities, higher BMI and having undergone more radical resections compared to patients with CD. Risk factors for longer LOS in patients with CD like smoking, de-functioning stoma, previous surgeries and emergency setting were adjusted in a multivariate model, indicating that there might be other explanations for the longer LOS in this group of patients, which are not accounted for in this paper. A BMI below 18.5 is another factor which significantly increases the LOS, but this is also adjusted for in the LOS model, which shows that a low BMI cannot explain the increased LOS in patients with CD either. This was not investigated in this study, thus further studies are needed to rule out that elements of malnutrition play a part in the LOS and post-operative status of patients with CD.
Timing of operation may be a modifiable risk factor for un-favourable post-operative outcome in patients with CD[24] but emergency surgery cannot explain the longer LOS because both groups of patients had the same rate of emergency operations. UIAEs increase the risk of post-operative complications as well as LOS. It is expected to have higher risks for UIAEs in patients with CD due to the inflammatory nature of the disease and previous surgeries in the area, but this was not the case after adjusting for other factors in the multivariate analyses.
Being a chronic disease not curable by surgery or medical treatment, patients with CD might have a higher inflammatory profile in response to surgery. This is supported by higher peak CRP when compared to patients with CC. Early surgical intervention after non-response to medical treatment as well as pre-operative optimization might therefore be beneficial in this group[25], especially when standard optimization schemes are implemented[26]. Patients with CD have higher risk for post-operative psychiatric morbidity[27] which might be a factor influencing LOS in this group of patients.
A similar paper was by Piessen et al[28] about prevalence of and risk factors for morbidity after left colectomy showed that disease entity can affect post-operative outcome for the same type of surgical intervention. A population-based study compared elective sigmoidectomy for diverticular disease with same intervention for cancer[29] showing different types of complications in the two groups. Our study on right side colectomy showed that same intervention can have different outcome according to underlying disease. This is important to plan pre-operative optimization in different diseases.
The strengths of this study include a prospective standardized approach, large geographical diversity (34 European countries, Argentina, Brazil, China, Japan and United States), and a large patient sample. The audit did not collect detailed data about nutritional status, disease severity in CD, pre-operative staging and neo-adjuvant chemo-radiotherapy in CC. These might influence the outcome and present a limitation. Another limitation might be reporting bias although it is unlikely given the method of data entry, where patient data is locked/saved pre- and peri-operatively, before any complications are registered. Comparison of LOS in patients with CD and CC might be tricky, as there are no standardized recovery pathways for either patient group in this study however, this study provides a valuable snapshot of reality.
Despite these limitations, this sub-group analysis of data from the ESCP snapshot audit can generate hypotheses and stimulate further studies. This study shows that patients with CD, despite their young age and relatively good health have a tendency for longer LOS in hospital, which cannot be fully explained by any of the investigated variables. This indicates that more can be done to improve the post-operative outcome in patients with CD. Further studies are needed to shed a light on the complexities of CD surgery and to examine whether certain approaches, such as standardized pre-operative optimization schemes or earlier surgical intervention, can improve the post-operative outcome for patients with CD. The power of this study is to be a brick in the design of a post-operative recovery program for patients with CD who seemed to be slow in recovering compared to patients with CC.
In conclusion, patients with CD were younger, with lower ASA grade, less comorbidity, operated on by experienced surgeons and underwent less radical resection, but had a longer post-operative stay in hospital compared to patients with CC. More studies are needed to investigate this association.
ARTICLE HIGHLIGHTS
Research background
Right hemicolectomy or ileocecal resection are used to treat benign conditions like Crohn’s disease (CD) and malignant ones like colon cancer (CC).
Research motivation
There is a need for a large prospective study investigating postoperative outcome in patients with CC and CD to identify areas warranting further research like allocation of resources, preoperative optimization and surgical techniques in the two patient groups respectively.
Research objectives
The objective of this study is to investigate differences in pre- and peri-operative factors and their impact on postoperative outcome in patients with CC and CD.
Research methods
This is a sub-group analysis of the European Society of Coloproctology’s prospective, multi-centre snapshot audit. Adult patients with CC and CD undergoing right hemicolectomy or ileocecal resection were included. Primary outcome measure was 30-d postoperative complica-tions. Secondary outcome measures were postoperative length of stay at and readmission.
Research results
375 patients with CD and 2,515 patients with CC were included. Patients with CD were younger, with a median of 37 years for CD and 71 years for CC (P < 0.01), had lower ASA grade (P < 0.01) and less comorbidity (P < 0.01), but were more likely to be current smokers (P < 0.01). Patients with CD were more frequently operated on by colorectal surgeons (P < 0.01) and frequently underwent ileocecal resection (P < 0.01) with higher rate of de-functioning/primary stoma construction (P < 0.01). Thirty-day postoperative mortality occurred exclusively in the CC group (66/2515, 2.3%). In multivariate analyses, the risk of postoperative complications was similar in the two groups (OR 0.80, 95%CI: 0.54-1.17; P = 0.25). Patients with CD had a significantly longer length of stay (Geometric mean 0.87, 95%CI: 0.79-0.95; P < 0.01). There was no difference in re-admission rates.
Research conclusions
Patients with CD were younger, with lower American Society of Anesthesiology score grade, less comorbidity, operated on by experienced surgeons and underwent less extensive surgery but had a longer length of stay than patients with CC although complications' rate was not different between the two groups.
Research perspectives
This study is hypothesis-generating study. It will stimulate further researches to explore the factors that affect the length of postoperative stay in the hospital.
ACKNOWLEDGEMENTS
The list of the full authors and their contributions are listed in the supplementary file.
Footnotes
Institutional review board statement: The study was reviewed and approved by the European Society of Coloproctology Institutional Review Board.
Informed consent statement: This is not applicable as this paper reports a prospective audit conducted bt European Society of Colo-Proctology in 2015.
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Manuscript source: Unsolicited manuscript
Peer-review started: March 7, 2019
First decision: May 9, 2019
Article in press: May 23, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: Denmark
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Abdolghaffari AH, Zhou W S-Editor: Ji FF L-Editor: A E-Editor: Wang J
Contributor Information
2015 European Society of Coloproctology (ESCP) collaborating group:
S Dich Grandt, A El-Hussuna, M Frasson, B Singh, G Gallo, F Pata, I Negoi, T Pinkney, O Zmora, A Bhangu, N Battersby, S Chaudhri, D Nepogodiev, S Vennix, J Glasbey, A Minaya, L Basso, M Pukuotukai, ME Kelly, L Sánchez Guillén, G Pellino, N Buchs, D Morton, T Pinkney, W Bemelman, P Christensen, A D’Hoore, S Laurberg, M Rubbini, C Vaizey, L Magill, R Perry, N Sheward, RN Mortensen, M Cillo, D Estefania, J Patron Uriburu, H Ruiz, M Salomon, A Makhmudov, L Selnyahina, A Varabei, Y Vizhynis, D Claeys, B Defoort, F Muysoms, P Pletinckx, V Vergucht, I Debergh, T Feryn, H Reusens, D Francart, C Jehaes, S Markiewicz, B Monami, J Weerts, W Bouckaert, B Houben, J Knol, G Sergeant, G Vangertruyden, L Haeck, C Lange, C Sommeling, K Vindevoghel, S Castro, H De Bruyn, M Huyghe, E De Wolf, D Reynders, A D’Hoore, A de Buck van Overstraeten, A Wolthuis, S Delibegovic, A Christiani, M Marchiori Jr, C Rocha de Moraes, V Tercioti Jr, E Arabadjieva, D Bulanov, D Dardanov, V Stoyanov, A Yonkov, K Angelov, S Maslyankov, M Sokolov, G Todorov, S Toshev, Y Georgiev, A Karashmalakov, G Zafirov, X Wang, D Condic, D Kraljik, H Mrkovic, V Pavkovic, K Raguž, V Bencurik, E Holášková, M Skrovina, M Farkašová, T Grolich, Z Kala, F Antos, V Pruchova, O Sotona, M Chobola, T Dusek, A Ferko, J Örhalmi, J Hoch, P Kocian, L Martinek, I Bernstein, K Gotschalck Sunesen, J Leunbach, O Thorlacius-Ussing, A Uth Oveson, P Christensen, S Dahl Chirstensen, V Gamez, M Oeting, U Schou Loeve, A Ugianskis, M Jessen, PM Krarup, K Linde, Q Mirza, J Overgaard Stovring, L Erritzøe, H Loft Jakobsen, J Lykke, E Palmgren Colov, A Husted Madsen, T Linde Friis, J Amstrup Funder, R Dich, S Kjær, S Rasmussen, N Schlesinger, M Dilling Kjaer, N Qvist, A Khalid, G Ali, A El-Hussuna, S Hadi, L Rosell Walker, A Kivelä, T Lehtonen, A Lepistö, T Scheinin, P Siironen, J Kössi, P Kuusanmäki, T Tomminen, A Turunen, T Rautio, M Vierimaa, H Huhtinen, J Karvonen, M Lavonius, A Rantala, P Varpe, E Cotte, Y Francois, O Glehen, V Kepenekian, G Passot, L Maggiori, G Manceau, Y Panis, M Gout, E Rullier, B van Geluwe, N Chafai, JH Lefevre, Y Parc, E Tiret, C Couette, E Duchalais, A Agha, M Hornberger, A Hungbauer, I Iesalnieks, I Weindl, F Crescenti, M Keller, N Kolodziejski, R Scherer, D Sterzing, B Bock, G Boehm, M El-Magd, C Krones, M Niewiera, J Buhr, S Cordesmeyer, M Hoffmann, K Krückemeier, T Vogel, M Schön, J Baral, T Lukoschek, S Münch, F Pullig, K Horisberger, P Kienle, J Magdeburg, S Post, K Batzalexis, S Germanos, C Agalianos, C Dervenis, N Gouvas, P Kanavidis, A Kottikias, IE Katsoulis, D Korkolis, G Plataniotis, G Sakorafas, I Akrida, M Argentou, C Kollatos, C Lampropoulos, S Tsochatzis, I Besznyák, A Bursics, T Egyed, G Papp, I Svastics, J Atladottir, P Möller, H Sigurdsson, T Stefánsson, E Valsdottir, E Andrews, N Foley, D Hechtl, M Majeed, M McCourt, A Hanly, J Hyland, S Martin, PR O'Connell, D Winter, T Connelly, W Joyce, P Wrafter, R Berkovitz, S Avital, I Haj Yahia, N Hermann, B Shpitz, I White, Y Lishtzinsky, A Tsherniak, N Wasserberg, N Horesh, U Keler, R Pery, R Shapiro, O Zmora, H Tulchinsky, B Badran, K Dayan, A Iskhakov, J Lecaros, N Nabih, I Angrima, R Bardini, E Pizzolato, M Tonello, F Arces, R Balestri, C Ceccarelli, V Prosperi, E Rossi, I Giannini, L Vincenti, F Di Candido, M Di Iena, A Guglielmi, O Caputi-Iambrenghi, P Marsanic, A Mellano, A Muratore, M Annecchiarico, L Bencini, S Amore Bonapasta, A Coratti, F Guerra, CR Asteria, L Boccia, L Gerard, A Pascariello, G Manca, F Marino, A Casaril, M Inama, G Moretto, C Bacchelli, M Carvello, N Mariani, M Montorsi, A Spinelli, E Romairone, S Scabini, A Belli, F Bianco, S De Franciscis, G Maria Romano, P Delrio, U Pace, D Rega, C Sassaroli, D Scala, R De Luca, E Ruggieri, C Elbetti, A Garzi, L Romoli, M Scatizzi, A Vannucchi, G Curletti, V Durante, R Galleano, F Mariani, L Reggiani, R Bellomo, A Infantino, L Franceschilli, P Sileri, I Clementi, D Coletta, F La Torre, A Mingoli, F Velluti, A Di Giacomo, A Fiorot, M Massani, L Padoan, C Ruffolo, S Caruso, F Franceschini, R Laessig, I Monaci, M Rontini, P De Nardi, U Elmore, M Lemma, R Rosati, A Tamburini, M De Luca, A Sartori, A Benevento, C Bottini, CC Ferrari, F Pata, G Tessera, G Pellino, F Selvaggi, A Lanzani, F Romano, G Sgroi, F Steccanella, L Turati, T Yamamoto, G Ancans, S Gerkis, M Leja, A Pcolkins, A Sivins, T Latkauskas, P Lizdenis, Ž Saladžinskas, S Švagždys, A Tamelis, A Razbadauskas, M Sokolovas, A Dulskas, N Samalavicius, V Jotautas, S Mikalauskas, E Poskus, T Poskus, K Strupas, C Camenzuli, C Cini, A Predrag, J Psaila, N Spiteri, W Bemelman, C Buskens, EJ de Groof, J Gooszen, P Tanis, E Belgers, P Davids, E Furnee, E Postma, A Pronk, N Smakman, S Clermonts, D Zimmerman, J Omloo, E van der Zaag, P van Duijvendijk, E Wassenaar, M Bruijninckx, E de Graff, P Doornebosch, G Tetteroo, M Vermaas, G Iordens, S Knops, B Toorenvliet, HL van Westereenen, E Boerma, P Coene, E van der Harst, A Van Der Pool, M Raber, J Melenhorst, S de Castro, M Gerhards, M Arron, A Bremers, H de Wilt, F Ferenschild, S Yauw, H Cense, A Demirkiran, M Hunfeld, I Mulder, J Nonner, H Swank, B van Wagensveld, M Bolmers, J Briel, A van Geloven, E Echazarreta-Gallego, M Elia-Guedea, J Ramirez, C van Rossem, V Klemann, J Konsten, B Leenders, T Schok, W Bleeker, A Gidwani, R Lawther, P Loughlin, B Skelly, R Spence, M Brun, M Helgeland, D Ignjatovic, T Øresland, P Yousefi, I Flåten Backe, O Helmer Sjo, A Nesbakken, M Tandberg Eriksen, A Cais, J Hallvard Træland, R Herikstad, H Kørner, N Lauvland, D Jajtner, W Kabiesz, M Rak, L Gmerek, K Horbacka, N Horst, P Krokowicz, A Kwiatkowski, K Pasnik, P Karcz, M Romaniszyn, T Rusek, P Walega, R Czarencki, Z Obuszko, M Sitarska, W Wojciech, M Zawadzki, S Amado, P Clara, A Couceiro, R Malaquias, N Rama, A Almeida, E Barbosa, E Cernadas, A Duarte, P Silva, S Costa, C Martinez Insua, J Pereira, C Pereira, M Sacchetti, B Carvalho Pinto, P Jorge Vieira Sousa, R Marques, A Oliveira, R Cardoso, S Carlos, J Corte-Real, P Moniz Pereira, R Souto, C Carneiro, R Marinho, V Nunes, R Rocha, M Sousa, J Leite, F Melo, J Pimentel, L Ventura, C Vila Nova, C Copăescu, V Bintintan, C Ciuce, G Dindelegan, R Scurtu, R Seicean, N Domansky, A Karachun, A Moiseenko, Y Pelipas, A Petrov, I Pravosudov, R Aiupov, Y Akmalov, A Parfenov, N Suleymanov, N Tarasov, H Jumabaev, Z Mamedli, A Rasulov, I Aliev, I Chernikovskiy, V Kochnev, K Komyak, I Pravosudov, A Smirnov, S Achkasov, K Bolikhov, Y Shelygin, O Sushkov, A Zapolskiy, M Gvozdenovic, D Jovanovic, Z Lausevic, D Cvetković, M Maravić, B Milovanovic, N Stojakovic, I Tripković, D Mihajlovic, M Nestorovic, V Pecic, D Petrovic, G Stanojevic, G Barisic, I Dimitrijevic, Z Krivokapic, V Markovic, M Popovic, A Aleksic, D Dabic, I Kostic, A Milojkovic, V Perunicic, D Lukic, T Petrovic, D Radovanovic, Z Radovanovic, VM Cuk, VV Cuk, M Kenic, B Kovacevic, I Krdzic, J Korcek, M Rems, J Toplak, J Escarrâ, M Gil Barrionuevo, T Golda, E Kreisler Moreno, C Zerpa Martin, C Álvarez Laso, P Cumplido, H Padin, J Baixauli Fons, J Hernández Lizoain, P Martinez Ortega, M Molina Fernández, C Sánchez Justicia, J Antonio Gracia Solanas, E Córdoba Díaz de Laspra, E Echazarreta-Gallego, M Elia-Guedea, J Ramirez, J Arredondo Chaves, P Diez González, T Elosua, J Sahagún, A Turienzo Frade, J Álvarez Conde, E Castrillo, R Diaz Maag, V Maderuelo, L Saldarriaga, I Aldrey Cao, X Fernández Varela, S Núñez Fernández, A Parajó Calvo, S Villar Álvarez, I Blesa Sierra, A Duarte, R Lozano, M Márquez, O Porcel, P Menendez, M Fernández Hevia, L Flores Sigüenza, M Jimenez Toscano, A Lacy Fortuny, J Ordoñez, A Espi, S Garcia Botello, J Martín Arévalo, D Moro Valdezate, MartíV Pla, F Blanco Antona, J Abrisqueta, N Ibañez Canovas, J Lujan Mompean, D Escolá Ripoll, S Martinez Gonzalez, J Parodi, A Fernández López, M Ramos Fernández, J Castellvi Valls, L Ortiz de Zarate, R Ribas, D Sabia, L Viso, S Alonso Gonçalves, M José Gil, M Pascual Damieta, M Pera, S Salvans Ruiz, J Bernal, F Landete, G Ais, J Etreros, J Aguiló Lucia, A Boscá, S Deusa, J García del Caño, V Viciano, J García Armengol, J Roig, J Blas, J Escartin, J Fatás, J Fernando, R Ferrer, R Arias Pacheco, L García Flórez, M Moreno Gijón, J Otero Díez, L Solar Garcia, F Aguilar Teixido, C Balaguer Ojo, J Bargallo Berzosa, S Lamas Moure, J Enrique Sierra, A Fermiñán, F Herrerias, M Rufas, J Viñas, A Codina Cazador, R Farrés, N Gómez, D Julià, P Planellas, J López, A Luna, C Maristany, A Muñoz Duyos, N Puértolas, M Alcantara Moral, X Serra Aracil, P Concheiro Coello, D Gómez, C Carton, A Miguel, F Reoyo Pascual, X Valero Cerrato, R Zambrano Muñoz, J Cervera Aldama, J García González, J Ramos Prada, M Santamaría Olabarrieta, A Urigüen Echeverría, R Coves Alcover, J Espinosa Soria, E Fernandez Rodriguez, J Hernandis Villalba, V Maturana Ibañez, F De la Torre Gonzalez, D Huerga, E Pérez Viejo, A Rivera, E Ruiz Ucar, J Garcia Septiem, V Jiménez, J Jiménez Miramón, J Ramons Rodriquez, V Rodriguez Alvarez, A Garcea, L Ponchietti, N Borda, J Enriquez Navascues, Y Saralegui, G Febles Molina, E Nogues, M Rodríguez, C Roque Castellano, Y Sosa Quesada, M Alvarez Gallego, I Pascual, I Rubio Perez, B Diaz San Andrés, F Tone Villanueva, J Alonso, C Cagigas, J Castillo, M Gómez, J Martín Parra, M Mengual Ballester, E Pellicer Franco, V Soria Aledo, G Valero Navarro, E Caballero Rodríguez, P Gonzalez De Chaves, G Hernandez, A Perez Alvarez, A Soto Sanchez, F Cesar Becerra Garcia, J Guillermo Alonso Roque, Rodríguez López, F Arias, SR Del Valle Ruiz, G Sánchez De La Villa, A Compañ, A García Marín, C Nofuentes, MicóF Orts, V Pérez Auladell, M Carrasco, C Duque Perez, S Gálvez Pastor, I Navarro Garcia, A Sanchez Perez, D Enjuto, F Manuel Bujalance, N Marcelin, M Pérez, R Serrano García, A Cabrera, F de la Portilla, J Diaz Pavon, R Jimenez Rodriguez, J Vazquez Monchul, J Martínez Alegre, I Ortega, A Picardo Nieto Antonio, A Caro, J Escuder, F Feliu, M Millan, R Alos Company, A Frangi Caregnato, R Lozoya Trujillo, R Rodríguez Carrillo, M Ruiz Carmona, N Alonso, D Ambrona Zafra, B Amilka Ayala, CJ Bonnin Pascual, C Pineño Flores, J Alcazar Montero, M Angoso Clavijo, J Garcia, J Sanchez Tocino, C Gómez Alcazar, D Costa Navarro, J Ferri Romero, M Rey Riveiro, M Romero Simó, B Arencibia, P Esclapez, M Frasson, E García Granero, P Granero, FJ Medina Fernández, AB Gallardo Herrera, C Diaz López, E Navarro Rodriguez, E Torres Tordera, J Arenal, M Citores, J Marcos, J Sánchez, C Tinoco, E Espin, A Garcia Granero, L Jimenez Gomez, J Sanchez Garcia, F Vallribera, J Folkesson, F Sköldberg, K Bergman, E Borgström, J Frey, A Silfverberg, M Söderholm, J Nygren, J Segelman, D Gustafsson, A Lagerqvist, A Papp, M Pelczar, M Abraham Nordling, M Ahlberg, A Sjovall, J Tengstrom, K Hagman, A Chabok, E Ezra, M Nikberg, K Smedh, C Tiselius, N Al Naimi, M Dao Duc, J Meyer, M Mormont, F Ris, G Prevost, P Villiger, H Hoffmann, C Kettelhack, P Kirchhoff, D Oertli, B Weixler, B Aytac, S Leventoglu, B Mentes, O Yuksel, S Demirbas, B Busra Ozkan, G Selçuk Özbalci, U Sungurtekin, B Gülcü, E Ozturk, T Yilmazlar, C Challand, N Fearnhead, R Hubbard, S Kumar, J Arthur, C Barben, P Skaife, S Slawik, M Williams, M Zammit, J Barker, J French, I Sarantitis, C Slawinski, R Clifford, N Eardley, M Johnson, C McFaul, D Vimalachandran, S Allan, A Bell, E Oates, V Shanmugam, A Brigic, M Halls, P Pucher, B Stubbs, T Agarwal, A Chopada, S Mallappa, M Pathmarajah, C Sugden, C Brown, E Macdonald, A Mckay, J Richards, A Robertson, M Kaushal, P Patel, S Tezas, N Touqan, S Ayaani, K Marimuthu, B Piramanayagam, M Vourvachis, N Iqbal, S Korsgen, C Seretis, U Shariff, S Arnold, N Battersby, H Chan, E Clark, R Fernandes, B Moran, A Bajwa, D McArthur, K Cao, P Cunha, H Pardoe, A Quddus, K Theodoropoulou, C Bolln, G Denys, M Gillespie, N Manimaran, J Reidy, AI Malik, A Malik, J Pitt, K Aryal, A El Hadi, R Lal, A Pal, V Velchuru, S Chaudhri, M Oliveira Cunha, B Singh, M Thomas, S Bains, K Boyle, A Miller, M Norwood, J Yeung, L Goian, S Gurjar, W Saghir, N Sengupta, E Stewart Parker, S Bailey, T Khalil, D Lawes, S Nikolaou, G Omar, R Church, B Muthiah, W Garrett, P Marsh, N Obeid, S Chandler, P Coyne, M Evans, L Hunt, J Lim, Z Oliphant, E Papworth, H Weaver, K Cuiñas Leon, G Williams, J Hernon, S Kapur, R Moosvi, I Shaikh, L Swafe, M Aslam, J Evans, U Ihedioha, P Kang, J Merchant, R Hompes, R Middleton, A Broomfield, D Crutten Wood, J Foster, G Nash, M Akhtar, M Boshnaq, S Eldesouky, S Mangam, M Rabie, J Ahmed, J Khan, N Ming Goh, A Shamali, S Stefan, D Nepogodiev, T Pinkney, C Thompson, A Amin, J Docherty, M Lim, K Walker, A Watson, M Hossack, N Mackenzie, M Paraoan, N Alam, I Daniels, S Narang, S Pathak, N Smart, A Al Qaddo, R Codd, O Rutka, G Williams, C Bronder, I Crighton, E Davies, T Raymond, L Bookless, B Griffiths, S Plusa, G Carlson, R Harrison, N Lees, C Mason, J Quayle, G Branagan, J Broadhurst, H Chave, S Sleight, F Awad, A Bhangu, N Cruickshank, H Joy, C Boereboom, P Daliya, A Dhillon, N Watson, R Watson, D Artioukh, K Gokul, M Javed, R Kong, J Sutton, O Faiz, I Jenkins, CA Leo, SF Samaranayake, J Warusavitarne, S Arya, C Bhan, H Mukhtar, A Oshowo, J Wilson, S Duff, T Fatayer, J Mbuvi, A Sharma, J Cornish, L Davies, R Harries, C Morris, J Torkington, J Knight, C Lai, O Shihab, A Tzivanakis, A Hussain, D Luke, R Padwick, A Torrance, A Tsiamis, P Dawson, A Balfour, R Brady, J Mander, H Paterson, N Chandratreya, H Chu, J Cutting, S Vernon, C Wai Ho, S Andreani, H Patel, M Warner, YQ Tan, A Iqbal, A Khan, K Perrin, A Raza, and S Tan
References
- 1.Center MM, Jemal A, Smith RA, Ward E. Worldwide variations in colorectal cancer. CA Cancer J Clin. 2009;59:366–378. doi: 10.3322/caac.20038. [DOI] [PubMed] [Google Scholar]
- 2.Baumgart DC, Sandborn WJ. Crohn's disease. Lancet. 2012;380:1590–1605. doi: 10.1016/S0140-6736(12)60026-9. [DOI] [PubMed] [Google Scholar]
- 3.Joossens M, Simoens M, Vermeire S, Bossuyt X, Geboes K, Rutgeerts P. Contribution of genetic and environmental factors in the pathogenesis of Crohn's disease in a large family with multiple cases. Inflamm Bowel Dis. 2007;13:580–584. doi: 10.1002/ibd.20086. [DOI] [PubMed] [Google Scholar]
- 4.Boyle P, Langman JS. ABC of colorectal cancer: Epidemiology. BMJ. 2000;321:805–808. doi: 10.1136/bmj.321.7264.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tuvlin JA, Raza SS, Bracamonte S, Julian C, Hanauer SB, Nicolae DL, King AC, Cho JH. Smoking and inflammatory bowel disease: trends in familial and sporadic cohorts. Inflamm Bowel Dis. 2007;13:573–579. doi: 10.1002/ibd.20043. [DOI] [PubMed] [Google Scholar]
- 6.Liang PS, Chen TY, Giovannucci E. Cigarette smoking and colorectal cancer incidence and mortality: systematic review and meta-analysis. Int J Cancer. 2009;124:2406–2415. doi: 10.1002/ijc.24191. [DOI] [PubMed] [Google Scholar]
- 7.Johnson IT, Lund EK. Review article: nutrition, obesity and colorectal cancer. Aliment Pharmacol Ther. 2007;26:161–181. doi: 10.1111/j.1365-2036.2007.03371.x. [DOI] [PubMed] [Google Scholar]
- 8.Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011;106:563–573. doi: 10.1038/ajg.2011.44. [DOI] [PubMed] [Google Scholar]
- 9.Jackson-Thompson J, Ahmed F, German RR, Lai SM, Friedman C. Descriptive epidemiology of colorectal cancer in the United States, 1998-2001. Cancer. 2006;107:1103–1111. doi: 10.1002/cncr.22007. [DOI] [PubMed] [Google Scholar]
- 10.Rogers BH, Clark LM, Kirsner JB. The epidemiologic and demographic characteristics of inflammatory bowel disease: an analysis of a computerized file of 1400 patients. J Chronic Dis. 1971;24:743–773. doi: 10.1016/0021-9681(71)90087-7. [DOI] [PubMed] [Google Scholar]
- 11.van de Velde CJ, Boelens PG, Borras JM, Coebergh JW, Cervantes A, Blomqvist L, Beets-Tan RG, van den Broek CB, Brown G, Van Cutsem E, Espin E, Haustermans K, Glimelius B, Iversen LH, van Krieken JH, Marijnen CA, Henning G, Gore-Booth J, Meldolesi E, Mroczkowski P, Nagtegaal I, Naredi P, Ortiz H, Påhlman L, Quirke P, Rödel C, Roth A, Rutten H, Schmoll HJ, Smith JJ, Tanis PJ, Taylor C, Wibe A, Wiggers T, Gambacorta MA, Aristei C, Valentini V. EURECCA colorectal: multidisciplinary management: European consensus conference colon & rectum. Eur J Cancer. 2014;50:1.e1–1.e34. doi: 10.1016/j.ejca.2013.06.048. [DOI] [PubMed] [Google Scholar]
- 12.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 13.Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–197. doi: 10.1055/s-0029-1242458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Buck van Overstraeten A, Eshuis EJ, Vermeire S, Van Assche G, Ferrante M, D'Haens GR, Ponsioen CY, Belmans A, Buskens CJ, Wolthuis AM, Bemelman WA, D'Hoore A. Short- and medium-term outcomes following primary ileocaecal resection for Crohn's disease in two specialist centres. Br J Surg. 2017;104:1713–1722. doi: 10.1002/bjs.10595. [DOI] [PubMed] [Google Scholar]
- 15.Hendel K, Kjærgaard S, El-Hussuna A. A systematic review of pre, peri and post-operative factors and their implications for the lengths of resected bowel segments in patients with Crohn's disease. IJS Open. 2017;7:10–16. [Google Scholar]
- 16.Van Arendonk KJ, Tymitz KM, Gearhart SL, Stem M, Lidor AO. Outcomes and costs of elective surgery for diverticular disease: a comparison with other diseases requiring colectomy. JAMA Surg. 2013;148:316–321. doi: 10.1001/jamasurg.2013.1010. [DOI] [PubMed] [Google Scholar]
- 17.Slater G, Greenstein AJ, Aufses AH., Jr Postoperative complications after right colonic resections for inflammatory bowel disease and carcinoma. Am J Gastroenterol. 1980;74:516–518. [PubMed] [Google Scholar]
- 18.Boaron L, Facchin L, Bau M, Zacharias P, Ribeiro D, Miranda EF, de Barcelos IF, Ropelato RV, Filho AS, de Meira Junior JD, Sassaki L, Saad-Hossne R, Kotze PG. Post-operative complication rates between Crohn's disease and Colorectal cancer patients after ileocolic resections: a comparative study. J Coloproctol (Rio J) 2017;37:290–294. [Google Scholar]
- 19.Wideroff M, Xing Y, Liao J, Byrn JC. Crohn's disease but not diverticulitis is an independent risk factor for surgical site infections in colectomy. J Gastrointest Surg. 2014;18:1817–1823. doi: 10.1007/s11605-014-2602-5. [DOI] [PubMed] [Google Scholar]
- 20.Bhakta A, Tafen M, Glotzer O, Ata A, Chismark AD, Valerian BT, Stain SC, Lee EC. Increased Incidence of Surgical Site Infection in IBD Patients. Dis Colon Rectum. 2016;59:316–322. doi: 10.1097/DCR.0000000000000550. [DOI] [PubMed] [Google Scholar]
- 21.Kwaan MR, Vogler SA, Sun MY, Sirany AM, Melton GB, Madoff RD, Rothenberger DA. Readmission after colorectal surgery is related to preoperative clinical conditions and major complications. Dis Colon Rectum. 2013;56:1087–1092. doi: 10.1097/DCR.0b013e31829aa758. [DOI] [PubMed] [Google Scholar]
- 22.Pinkney T, Bhangu A, Battersby N, Chaudri S, El-Hussuna A, Frasson M, Singh B, Vennix S, Zmora O. Protocol. ESCP Pan-European snapshot audit. Right Hemicolectomy/Ileo-caecal resection. 2015. Available from: http://www.escp.eu.com/images/research/documents/ESCP_ Cohort_Study_right_hemicolectomy_protocol_2_6.pdf. [Google Scholar]
- 23.2015 European Society of Coloproctology collaborating group. The relationship between method of anastomosis and anastomotic failure after right hemicolectomy and ileo-caecal resection: an international snapshot audit. Colorectal Dis. 2017 doi: 10.1111/codi.13646. [DOI] [PubMed] [Google Scholar]
- 24.2015 European Society of Coloproctology collaborating group. Risk factors for unfavourable postoperative outcome in patients with Crohn's disease undergoing right hemicolectomy or ileocaecal resection An international audit by ESCP and S-ECCO. Colorectal Dis. 2017 doi: 10.1111/codi.13889. [DOI] [PubMed] [Google Scholar]
- 25.El-Hussuna A, Iesalnieks I, Horesh N, Hadi S, Dreznik Y, Zmora O. The effect of pre-operative optimization on post-operative outcome in Crohn's disease resections. Int J Colorectal Dis. 2017;32:49–56. doi: 10.1007/s00384-016-2655-x. [DOI] [PubMed] [Google Scholar]
- 26.Zangenberg MS, Horesh N, Kopylov U, El-Hussuna A. Preoperative optimization of patients with inflammatory bowel disease undergoing gastrointestinal surgery: a systematic review. Int J Colorectal Dis. 2017;32:1663–1676. doi: 10.1007/s00384-017-2915-4. [DOI] [PubMed] [Google Scholar]
- 27.Zangenberg MS, El-Hussuna A. Psychiatric morbidity after surgery for inflammatory bowel disease: A systematic review. World J Gastroenterol. 2017;23:8651–8659. doi: 10.3748/wjg.v23.i48.8651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piessen G, Muscari F, Rivkine E, Sbaï-Idrissi MS, Lorimier G, Fingerhut A, Dziri C, Hay JM FRENCH (Fédération de Recherche EN CHirurgie) Prevalence of and risk factors for morbidity after elective left colectomy: cancer vs noncomplicated diverticular disease. Arch Surg. 2011;146:1149–1155. doi: 10.1001/archsurg.2011.231. [DOI] [PubMed] [Google Scholar]
- 29.Ilyas MI, Zangbar B, Nfonsam VN, Maegawa FA, Joseph BA, Patel JA, Wexner SD. Are there differences in outcome after elective sigmoidectomy for diverticular disease and for cancer? A national inpatient study. Colorectal Dis. 2017;19:260–265. doi: 10.1111/codi.13461. [DOI] [PubMed] [Google Scholar]