Abstract
Introduction: Metabolic disorders are common amongst HIV-infected patients. Data from real-life setting on the impact of DTG/ABC/3TC in virologically suppressed HIV-infected patients are scarce.
Methods: We investigated the modification of metabolic profile including fasting glucose, lipid profile and markers of insulin resistance (IR) in experienced patients switching from a boosted protease inhibitors (bPI) or a non-nucleoside reverse transcriptase inhibitor (NNRTI)-based regimen to DTG/ABC/3TC in a prospective, observational, multicenter study.
Results: We enrolled 131 HIV-infected patients, of whom 91 (69.5%) males, mean age was 50.5±10.6 years. CDC stage was A in 66 (50.4%) patients, of whom 91 (69.5%) had acquired HIV through sexual contacts. The previous regimen was bPI-based in 79 patients (60.3%) and NNRTI-based in 52 (39.7%). Patients switching from NNRTI showed a significant reduction at week 24 in total cholesterol (TC) and low-density lipoprotein cholesterol (LDL). Triglycerides/high-density lipoprotein cholesterol (TG/HDL) ratio, HDL, median TG and TG/HDL ratio did not show significant modification during follow-up times. Among patients switching from a bPI, we observed a significant reduction in TC and LDL at both follow-up times and a slight increase in HDL. Triglycerides/HDL ratio, median TG and TG/HDL ratio showed a decrease over time that became significant at weeks 24 and 48. Blood glucose levels did not significantly vary during the observation period in patients switching from both bPI and NNRTI-based regimens.
Conclusion: Our data suggest an improvement in lipid profile and TG/HDL ratio in pretreated HIV-1-infected patients who switched to DTG/ABC/3TC over 48 weeks, especially in those previously receiving a bPI-based regimen.
Keywords: HIV-1 infection, dolutegravir/abacavir/lamivudine, lipid profile
Introduction
Metabolic disorders are common amongst HIV-infected patients and show a higher prevalence in respect to healthy controls.1,2 The proportion of HIV-infected adults over the age of 50 is also growing, thus increasing the number of HIV-infected people at particular risk for metabolic perturbations and cardiovascular disease.3 Considering long-term use of antiretroviral therapy, the impact on the lipid profile of antiretroviral agents is critical when choosing from among different options for a treatment regimen.
Dolutegravir (DTG), a second-generation unboosted integrase inhibitor with a high barrier to resistance, proved efficacious and safe in naïve and experienced patients in clinical trials and is currently recommended by guidelines both for initial therapy and for optimization strategy.4
In the STRIVING study, switching to the combination of DTG with abacavir/lamivudine (ABC/3TC) as single tablet regimen versus continuing current combination antiretroviral therapy (cART) demonstrated noninferiority,5 good tolerability and improvements in inflammatory biomarker profiles.6 More recently, the study NEAT 022 showed that switching to DTG +2 nucleoside reverse transcriptase inhibitors (NRTI) compared to staying on a boosted protease inhibitor (bPI)-based regimen in HIV patients with high cardiovascular risk and/or age >50 years was associated with a significant improvement in lipid profile.7
To date, real-life data on the impact of DTG/ABC/3TC in virologically suppressed HIV-infected patients are limited.
We aimed at evaluating the modification of metabolic profile including fasting glucose, lipid profile and markers of insulin resistance (IR) in experienced patients switching from a bPI or a non-nucleoside reverse transcriptase inhibitor (NNRTI)-based regimen.
Methods
The SCOLTA Project (Surveillance Cohort Long-Term Toxicity of Antiretrovirals) is a prospective, observational, multicenter study created to assess the incidence of adverse events in patients receiving new antiretroviral drugs in clinical practice. This on-line pharmacovigilance program currently involves 21 Italian infectious disease departments. The Project has an internet site (http://www.cisai.info) where grade III and IV adverse events according to DAIDS table are recorded (http://rcc.tech-res-intl.com/tox_tables.htm). The SCOLTA Project currently includes 4 cohorts: dolutegravir, darunavir/cobicistat, atazanavir/cobicistat and tenofovir alafenamide/emtricitabine/elvitegravir/cobicistat. All patients starting one of the drugs included in the surveillance program in participating centers are consecutively asked to participate in the study after signing a written informed consent. Patients undergo follow-up at 6-month intervals and adverse events are notified when they are clinically observed. Complete data collection and follow-up procedures for the cohorts are described elsewhere.8
For the present study, we included all patients who switched to DTG/ABC/3TC from a triple cART based on a bPI or a NNRTI, had HIV RNA <50 copies/mL at enrolment and had at least 1 follow-up visit or reported reasons for interruption before the first follow-up visit. We aimed at evaluating the potential benefit of switching to DTG/ABC/3TC from different regimens on cardiovascular risk.
Specifically, we describe the changes in fasting glucose, lipid profile and insulin resistance, evaluated as triglycerides/high-density lipoprotein cholesterol (TG/HDL) ratio over 48 weeks after initiating DTG/ABC/3TC in HIV-infected individuals switching from bPI and NNRTI. Triglycerides/HDL ratio has been demonstrated to be a strong predictor of IR and cardiovascular events in several studies.9–11 Lipid profile included total cholesterol (TC), HDL and TG.
Statistical analysis
Categorical and discrete variables were described as frequency and percentage (%). Continuous variables were described using mean and SD if normally distributed, and median and interquartile range (IQR) if not normally distributed. At univariate analysis, groups were compared using chi-square for categorical variables and analysis of variance for continuous variables, or via a nonparametric test (Mann–Withney U test) for non-normally distributed continuous variables. Repeated measures were analyzed as change from baseline; to evaluate if means were significantly different from zero, within groups, AND we used the Student's t-test for normally distributed and the signed rank test for not normally distributed differences from baseline (ie TG/HDL).
Ethical approval
The study has been approved by the Ethics committee of the coordinator (Luigi Sacco Hospital Ethics Committee, June 13, 2013, registry number 352) and of the participating centers.
Results
Out of 611 patients enrolled from July 2014 to July 2017, 131 HIV-infected patients met the criteria of inclusion for this analysis.
The median follow-up time was 11 (IQR 7-19) months; 91 (69.5%) were males and 91 (69.5%) had acquired HIV through sexual contacts. CDC stage was A in 66 (50.4%) patients. Mean age at enrolment was 50.5±10.6 years and mean CD4-T cell count 640±357 cell/μL. Thirty (29.1%) patients had detectable HCV antibodies (17 of whom were HCV-RNA positive) and 8 (6.2%) were diabetic. The previous regimen was bPI-based in 79 patients (60.3%) and NNRTI-based in 52 (39.7%). Thirteen patients were on statins at study entry (8 in NNRTI and 5 in bPI group), which were continued in all cases, and no patient started such a treatment during follow-up. Out of the 131 patients, 5 (3.8%) did not report any lipid variables at study entry and were excluded from the analysis of lipids, but included in the analysis of blood glucose. Out of the 126 remaining subjects, 120 had the complete lipid profile but 6 lacked at least 1 variable. Overall, lipid analysis was based on 126, 106 and 72 patients at baseline, week 24 and week 48, respectively.
The patients who switched from a NNRTI-based regimen showed lower baseline TC and TG and higher HDL levels than those who switched from bPI. Furthermore, TG/HDL ratio was higher in patients who switched from a bPI regimen (median 3.6, IQR 1.6-6.2 vs 1.9, 1.2-2.6, p<0.0001). The baseline characteristics of the study population are further described in Table 1.
Table 1.
Baseline characteristics of patients starting dolutegravir/abacavir/lamivudine after switching from a boosted protease inhibitor (bPI) or a non-nucleoside reverse transcriptase inhibitor (NNRTI)
| Previous NNRTI, N=52 (39.7%) | Previous bPI, N=79 (60.3%) | |||
|---|---|---|---|---|
| N or mean or median | % or SD or IQR | N or mean or median | % or SD or IQR | |
| Female gender * | 14 | 26.9 | 26 | 32.9 |
| Age (years) (mean, SD)** | 51.3 | 12.1 | 49.9 | 9.7 |
| Ethnicity Caucasian* | 50 | 96.2 | 75 | 94.9 |
|
HIV transmission category* IVDU Homo/heterosexual Other or unknown |
3 41 8 |
5.8 78.8 15.4 |
13 50 16 |
16.5 53.3 20.2 |
|
CDC stage* A B C |
29 17 6 |
55.8 32.7 11.5 |
37 21 21 |
46.8 26.6 26.6 |
|
CD4 count (cells/μL)* <200 200–349 ≥350 |
0 12 40 |
0 23.1 76.9 |
13 24 42 |
16.5 30.4 53.2 |
|
Previous regimen (NNRTI)* EFV RPV ETV NVP |
34 9 4 5 |
65.4 17.3 7.7 9.6 |
– – – – |
– – – – |
|
Previous regimen (bPI)* ATV DRV LPV FAMP SQV |
– – – – – |
35 33 7 3 1 |
44.3 41.8 8.9 3.8 1.27 |
|
|
Anti- HCV antibodies positive* Detectable HCV-RNA* |
5 4 |
9.8 7.7 |
25 13 |
32.5 16.5 |
| Median time in follow-up***(months) | 9 | 6–12 | 13 | 7–24 |
| Statins therapy* | 8 | 15.4 | 5 | 6.3 |
| Diabetes* | 4 | 7.7 | 4 | 5.1 |
| Total cholesterol (TC, mg/dL)** | 198 | 43 | 212 | 46 |
| High-density lipoprotein (HDL, mg/dL)- C** | 58 | 22 | 48 | 16 |
| Low-density lipoprotein (LDL, mg/dL)-C** | 118 | 39 | 144 | 46 |
| Triglycerides (TG, mg/dL)*** | 104 | 76–121 | 149 | 95–215 |
| TG/HDL ratio*** | 1.9 | 1.2–2.6 | 3.6 | 1.6–6.2 |
| TC/HDL ratio*** | 3.5 | 2.8–4.4 | 4.5 | 3.5–5.7 |
Notes: *Data expressed as number and percentage (%). **Data expressed as mean and standard deviation (SD). ***Data expressed as median and interquartile range (IQR).
Abbreviations: EFV, Efavirenz; RPV, Rilpivirine; ETV, Etravirine; NVP, Nevirapine; ATV, Atazanavir, DRV, Darunavir; LPV, Lopinavir; FAMP, Fosamprenavir; SQV, Saquinavir; TG, triglycerides; bPI, Boosted Protease Inhibitors.
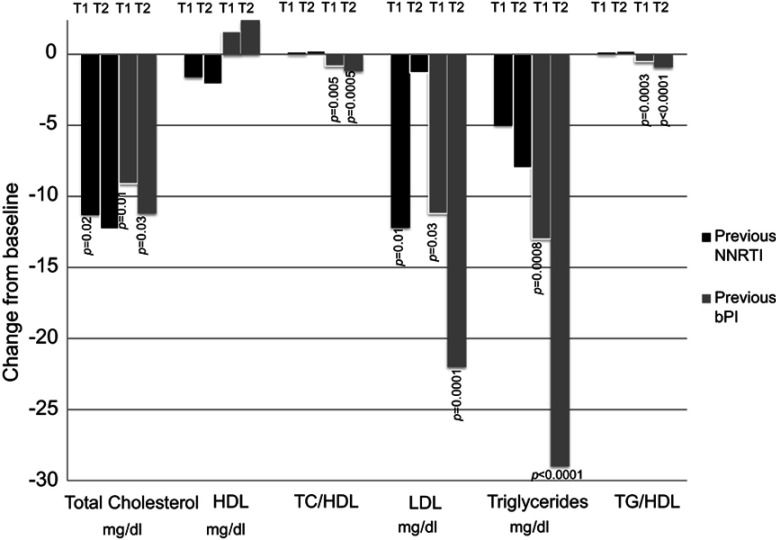
During follow-up, patients switching from NNRTI showed a reduction in TC that was significant at week 24 (−11.3±29.6 mg/dL, p=0.02 at 24 and −2.3±26.0 mg/dL at 48 weeks, p=0.65); LDL showed the same trend (−12.2±28.3 mg/dl at week 24, p=0.01 and −1.3±34.6 mg/dL at week 48, p=0.85). A slight nonsignificant reduction in HDL at week 24 and 48 (−1.6±9.4 mg/dL, p=0.31 and −2.1±9.5, p=0.30, respectively) was also observed. No significant changes were observed in TC/HDL ratio during follow-up (0.01±0.91, p=0.92, 0.12±0.61, p=0.33). Median TG levels remained stable during observation: 104 mg/dL at baseline (IQR 76-121) and 24 weeks (IQR 65-139) and 106 mg/dL at 48 weeks (IQR 78 −168). Mean changes from baseline were not significantly different from 0 at both follow-up visits (p=0.65 and 0.83, respectively). TG/HDL ratio did not show significant modification during follow-up times: 0.00 (IQR −0.47-0.51), p=0.51, at week 24 and 0.11 (IQR −0.19-0.74), p=0.33, at week 48 (Figure 1).
Figure 1.
Changes from baseline to 24 (T1) and 48 (T2) weeks in total cholesterol (TC), high-density lipoprotein (HDL), TC/HDL ratio, low-density lipoprotein (LDL), triglycerides (TG) and TG/HDL ratio. Data are shown as a mean change from baseline for TC, HDL, TC/HDL, LDL, TG and median change from baseline for TG/HDL.
Abbreviations: bPI, boosted protease Inhibitors; NNRTI, non-nucleoside reverse transcriptase inhibitors.
Among patients switching from a bPI, we observed a significant reduction in TC and LDL at both weeks 24 (−9.1±29.8 mg/dL, p=0.015 and −18.7±31.6 mg/dL, p<0.0001, respectively) and 48 (−11.2±33.5 mg/dL, p=0.026 and −22.0±35.1 mg/dL, p=0.0001, respectively) and a slight increase in HDL (1.6±8.9 mg/dL, p=0.15, 2.4±9.8 mg/dL, p=0.10). TC/HDL ratio decreased significantly at weeks 24 and 48 (−0.41±1.34, p=0.02, −0.59±1.21 p=0.002). Median TG significantly declined over time as follows: 149 (IQR 95-215) mg/dL at baseline, 122 mg/dL (IQR 75-178) at 24 (p=0.0006) and 118 mg/dL (IQR 83-141) at 48 weeks (p=0.015). TG/HDL ratio showed a decrease over time that became significant at weeks 24 and 48 (−0.49, IQR −1.97-0.11, p=0.0003 and −0.89 IQR −1.75-0.00, p<0.0001, respectively) (Figure 1).
In both groups, the decrease was more marked in patients who started with higher levels of blood lipids. Despite the small sample size, in subjects with TC>240 mg/dL at baseline and not on statins, we found that TC levels significantly decreased at T1: −26.0±4.7 (p<0.0001) and −35.0±10.5 (p=0.008) mg/dL in those switching from bPI and NNRTI, respectively.
Blood glucose levels did not significantly vary during the observation period in patients switching from both bPI and NNRTI-based regimens: excluding 8 diabetic subjects (4 in each group), at weeks 24 and 48, variations were 1.2±1.6 and 1.2±62.1 mg/dL for bPI patients, and 0.8±5.7 and −2.0±7.0 mg/dL for NNRTI.
Two cases in each group that were undetectable at week 24 and had a detectable viral load at week 48.
Discussion
The results of our study obtained in a “real-world” scenario are in part original and in part confirmatory.
Our data confirm in clinical practice that switching from a bPI to DTG/ABC/3TC in experienced HIV-infected patients with undetectable viral load is associated with an overall improvement of lipid profile. We also found beneficial effects on TG/HDL ratio, a marker of insulin resistance, glucose homeostasis and cardiovascular risk.
Both patients switching from bPI and NNRTI to DTG/ABC/3TC showed a decrease over time in TC levels, a primary target of lipid-lowering therapies. However, levels of HDL did not markedly change during follow-up time. Furthermore, patients switched from bPI showed a significant reduction in TC/HDL ratio, thus suggesting a potential reduction in the risk of cardiovascular disease.
With respect to hypertriglyceridemia, which is also considered an independent risk factor for cardiovascular disease,12 individuals treated with DTG/ABC/3TC showed an overall decrease, that resulted statistically significant in patients switching from bPI at every follow-up evaluation.
DTG/ABC/3TC demonstrated a neutral effect on glycemia in both treatment groups.
One of the most interesting findings of our study was the beneficial effect on the TG/HDL ratio recognized as a strong predictor of insulin resistance and cardiovascular disease in patients switching from bPI.1,2
Boosted PIs (Darunavir) and Efavirenz have been associated with a worse impact on lipids compared to Dolutegravir (Single and Flamingo) in antiretroviral naïve patients.13,14 Furthermore, switching to DTG from a boosted PI in the NEAT 022 study compared to staying on a bPI-based regimen was associated with a significant improvement in lipid profile. Therefore, our data confirm in an observational “real-life” study that switching to DTG/ABC/3TC could be associated with an improvement of lipids and markers of insulin resistance such as TG/HDL ratio. In our opinion, the discontinuation of the previous “third drug” (NNRTI or bPI) could explain these results since Dolutegravir has proved neutral on metabolic parameters.15
According to our data, patients switching from bPI showed a high TG/HDL ratio suggestive of insulin resistance at baseline.9,16,17 However, it is well known that there is variability in the threshold to define insulin resistance using TG/HDL ratio based on age, gender and ethnicity.18 The significant and persistent TG/HDL ratio decrease registered in our study at both follow-up times suggests that patients at increased risk of developing abnormal glucose tolerance and cardiovascular disease could benefit, in term of TG/HDL ratio, by the switch to DTG/ABC/3TC.
However, patients switching from NNRTI, who presented a normal mean TG/HDL ratio at baseline, did not show significant modifications during follow-up. Therefore, the benefit with regard to TG/HDL ratio seems lower in these patients.
The present study has some limitations. Firstly, the sample size was small, with only 131 patients enrolled with a limited observation period. Secondly, despite the prospective data collection, the study was purely observational. We do not have a randomized control group and cannot demonstrate the causality between ART switch and the measured outcomes. Thirdly, lifestyle interventions during follow-up have not been registered, and thus we cannot estimate their impact on the study outcomes. Thus, it is possible that the choice to switch regimens was guided by different patients’ characteristics that may have influenced the results of the analysis, and this may introduce a confounder in the analysis.
However, as far as we know, this is the first observational study to evaluate the impact on metabolic profile of switching patients with an undetectable viral load to DTG/ABC/3TC in an unselected “real-life” population. Therefore, our study adds new and more generalizable evidence to the existing knowledge deriving only from randomized clinical trials.
Taken together, our data suggest an improvement in lipid and metabolic profile in cART-treated patients switched to DTG/ABC/3TC over 48 weeks, especially in those previously receiving a bPI-based regimen.
Acknowledgments
The authors thank all of the patients and physicians who were involved in this study. The Coordinamento Italiano Studio Allergie e Infezione da HIV (C.I.S.A.I.) comprises the following members: Napoli: Paolo Maggi; Bari: Chiara Bellacosa, Carmen Rita Santoro; Bologna: Leonardo Calza, Eleonora Magistrelli; Busto Arsizio: Tiziana Quirino, Barbara Menzaghi, Maddalena Farinazzo; Cagliari: Marzia Garau, Goffredo Angioni, Chiara Bolliri, Marta Motzo; Catania: Benedetto Maurizio Celesia, Maria Gussio, Mauro Maresca; Cesena: Carmela Grosso; Chieti: Jacopo Vecchiet, Katia Falasca, Claudio Ucciferri; Firenze (S.M. Annunziata): Francesca Vichi; Firenze (Careggi): Canio Martinelli, Elena Salomoni, Paola Corsi; Genova (Galliera): Giovanni Penco, Giovanni Cenderello, Alberto Venturini; Genova (S.Martino): Antonio Di Biagio, Lucia Taramasso, Laura Ambra Nicolini; Lecco: Paolo Bonfanti, Chiara Molteni; Messina: Giuseppe Nunnari, Giovanni Pellicanò; Milano (Sacco, I Divisione): Laura Carenzi, Simone Passerini, Carlo Magni; Milano (Sacco, II Divisione): Laura Valsecchi, Laura Cordier; Milano (Sacco, CMI): Stefano Rusconi, Valeria Colombo; Monza: Nicola Squillace, Valentina Ferroni, Valeria Pastore; Padova: Marzia Franzetti; Pavia: Roberto Gulminetti, Alberto Gatti Comini; Perugia: Giuseppe De Socio, Aria Patacca, Giorgia Angeli; Pescara: Giustino Parruti, Donatella Cibelli; Sanremo: Chiara Dentone; Sassari: Giordano Madeddu, Paola Bagella, Vito Fiore, Maria Sabrina Mameli; Torino: Giancarlo Orofino, Marta Guastavigna.
Disclosure
GM has acted as advisor for Gilead Sciences, Janssen and Merck Sharp and Dohme and ViiV Healthcare and has received speakers’ honoraria from Gilead Sciences, Merck Sharp and Dohme, Janssen and ViiV Healthcare. NS has received travel grants from Gilead Sciences, Janssen, and ViiV Healthcare. ER declares consultancy fees from ViiV Healthcare. GVDS has received speakers’ honoraria from Gilead Sciences, Merck Sharp and Dohme, Janssen and ViiV Healthcare. LT has received consultancy fees from Janssen and Abbvie. He also reports personal fees from ViiV and Janssen, outside the submitted work. BMC has received grants, travel grants and speakers’ honoraria from bbvie, Bristol-Myers Squibb, Gilead Sciences, Merck Sharp & Dohme, Janssen and ViiV Healthcare. PBo has received personal fees from Gilead Sciences, Merck Sharp and Dohme, Janssen and ViiV Healthcare.
The authors report no other conflicts of interest in this work.
References
- 1.Guaraldi G, Orlando G, Zona S, et al. Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis. 2011;53:1120–1126. doi: 10.1093/cid/cir522 [DOI] [PubMed] [Google Scholar]
- 2.d’Ettorre G, Ceccarelli G, Pavone P, et al. What happens to cardiovascular system behind the undetectable level of HIV viremia? AIDS Res Ther. 2016;13:21. doi: 10.1186/s12981-016-0105-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tavoschi L, Gomes Dias J, Pharris A; EU/EEA HIV Surveillance Network. New HIV diagnoses among adults aged 50 years or older in 31 European countries, 2004-15: an analysis of surveillance data. Lancet HIV. 2017:4(11):e514–e521. [DOI] [PubMed] [Google Scholar]
- 4.European AIDS clinical Society. Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Version 9.0 November 2017; 2017. [Google Scholar]
- 5.Trottier B, Lake JE, Logue K, et al. Dolutegravir/abacavir/lamivudine versus current ART in virally suppressed patients (STRIIVING): a 48-week, randomized, non-inferiority, open-label, phase IIIb study. Antivir Ther. 2017;22(4):295–305. [DOI] [PubMed] [Google Scholar]
- 6.Lake J, Currier JS, Koteff J, et al. Cardiovascular biomarkers after switch to ABC/DTG/3TC: the STRIIVING. [Abstract 660]- 24th Conference on Retroviruses and Opportunistic Infections (CROI), Seattle: February 13–16, 2017.
- 7.Gatell JM, Assoumou L, Moyle G, et al. Switching from a ritonavir-boosted protease inhibitor to a dolutegravir-based regimen for maintenance of HIV viral suppression in patients with high cardiovascular risk. Aids. 2017;31(18):2503–2514. doi: 10.1097/QAD.0000000000001675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonfanti P, Martinelli C, Ricci E, et al. An Italian approach to postmarketing monitoring: preliminary results from the SCOLTA (Surveillance cohort long-term toxicity antiretrovirals) project on the safety of lopinavir/ritonavir. J Acquir Immune Defic Syndr. 2005;39:317–320. [DOI] [PubMed] [Google Scholar]
- 9.McLaughlin T, Reaven T, Abbasi F, et al. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease? Am J Cardiol. 2005;96:399–404. doi: 10.1016/j.amjcard.2005.03.085 [DOI] [PubMed] [Google Scholar]
- 10.Gaziano JM, Hennekens CH, O’Donnell CJ, Breslow JL, Buring JE. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation. 1997;96:2520–2525. [DOI] [PubMed] [Google Scholar]
- 11.Hanak V, Munoz J, Teague J, Stanley A Jr, Bittner V. Accuracy of the triglyceride to high-density lipoprotein cholesterol ratio for prediction of the low-density lipoprotein phenotype B. Am J Cardiol. 2004;94:219–222. doi: 10.1016/j.amjcard.2004.03.069 [DOI] [PubMed] [Google Scholar]
- 12.Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2011;123:2292–2333. doi: 10.1161/CIR.0b013e3182160726 [DOI] [PubMed] [Google Scholar]
- 13.Molina JM, Clotet B, van Lunzen J, et al. Once-daily dolutegravir is superior to once-daily darunavir/ritonavir in treatment-naïve HIV-1-positive individuals: 96 week results from FLAMINGO. J Int AIDS Soc. 2014;17(4 Suppl 3):19490. doi: 10.7448/IAS.17.4.19490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walmsley SL, Antela A, Clumeck N, et al.; SINGLE Investigators. Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection. N Engl J Med. 2013;369(19):1807–1818. doi: 10.1056/NEJMoa1215541 [DOI] [PubMed] [Google Scholar]
- 15.Quercia R, Roberts J, Martin-Carpenter L, Zala C. Comparative changes of lipid levels in treatment-naive, HIV-1-infected adults treated with dolutegravir vs. efavirenz, raltegravir, and ritonavir-boosted darunavir-based regimens over 48 weeks. Clin Drug Investig. 2015;35(3):211–219. doi: 10.1007/s40261-014-0266-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLaughlin T, Abbasi F, Cheal K, Chu J, Lamendola C, Reaven G. Use of metabolic markers to identify overweight individuals who are insulin resistant. Ann Intern Med. 2003;139(10):802–809. [DOI] [PubMed] [Google Scholar]
- 17.Salazar MR, Carbajal HA, Espeche WG, et al. Relation among the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio, insulin resistance, and associated cardio-metabolic risk factors in men and women. Am J Cardiol. 2012;109(12):1749–1753. doi: 10.1016/j.amjcard.2012.02.016 [DOI] [PubMed] [Google Scholar]
- 18.Li C, Ford ES, Meng YX, Mokdad AH, Reaven GM. Does the association of the triglyceride to high-density lipoprotein cholesterol ratio with fasting serum insulin differ by race/ethnicity? Cardiovasc Diabetol. 2008;7:4. doi: 10.1186/1475-2840-7-4 [DOI] [PMC free article] [PubMed] [Google Scholar]