Abstract
Primary care physicians should encourage their patients to engage in adequate physical activity. Current recommendations for physical activity in adults are as follows: at least 150–300 minutes per week of moderate-intensity, 75–150 minutes per week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Adults should also perform muscle-strengthening activities of moderate intensity or higher that involve all major muscle groups for 2 or more days per week. The elderly should perform additional balance training and fall prevention exercises more than 3 times a week. Children and adolescents should perform at least 1 hour of moderate-to-vigorous physical activity daily, which includes vigorous aerobic activity at least 3 days per week. As part of their 60 minutes or more of daily physical activity, resistance training and bone strengthening exercise should be done at least 3 days per week. According to new evidence, one bout of any exercises can be shorter than 10 minutes. Previously, physical activities were recommended for more than 10 minutes. For patients with diabetes, it is advisable to perform resistance exercise or short-distance running before aerobic exercise to prevent hypoglycemia. New evidence shows that dynamic resistance training is safe and effective in patients with hypertension provided the load is not too heavy. Exercise reduces pain and improves quality of life and physical function in patients with osteoarthritis,. Therefore, the treatment guidelines for osteoarthritis have been changed recently from not recommending exercise to highly recommending it.
Keywords: Exercise, Guideline, Diabetes Mellitus, Hypertension, Osteoarthritis
INTRODUCTION
Research about the effects of exercise and physical activity on health began in the 1950s with cardiovascular disease. The positive effects of exercise has been verified in a variety of additional research areas including cancer, cerebrovascular disease, mental illness, and musculoskeletal disorders. Therefore, exercise and physical activity are an important topic in clinical practice, and ever increasing in the modern age where lifestyle-relate and chronic diseases have become more important than infectious and acute diseases.
It was suggested that exercise should be vigorous to have a positive effect on health, because it was believed that extensive exercise causes physiological changes such as improvement of cardiopulmonary endurance which is beneficial. However, many studies concluded that even without intensive exercise, there were health benefits as long as there was enough of physical activity. With that, moderate exercise was recommended to promote health after the mid 1990s. Moderate exercise produces enough health benefits without a high risk of injury. Exercise amount is defined by the equation intensity×frequency×duration and as it increases as does its positive impact on health, as long as it is not overdone.
It is also known that physical activity that can encompass standard daily activities are beneficial to health. In recent years, physical activity, which is a broader term than exercise, tends to be defined by its impact on health.
This article summarizes the recent advances in sports medicine and exercise-related research.
EFFECT OF PHYSICAL ACTIVITY ON HEALTH
Physical activity reduces mortality, prevents various cancers, musculoskeletal and cerebrovascular diseases, improves metabolism, and is beneficial for mental health.
There is a great deal of research showing that mortality declines when physical activity increases or body fitness improves. The Shanghai women study showed that general daily physical activity, without intentional exercise, is also beneficial to health [1].
Physical activity decreases the incidence of colorectal cancer, breast cancer, bladder cancer, endometrial cancer, esophageal cancer, kidney cancer, lung cancer, and stomach cancer. Physical activity also has a positive effect on rehabilitation of cancer patients.
Studies on the prevention and treatment of cardiovascular diseases using exercise have been ongoing for many years. Physical activity controls hypertension, diabetes, and dyslipidemia, thereby preventing cerebrovascular disease. It also improves obesity and insulin resistance, otherwise known as metabolic syndrome.
Positive effects of physical activity on the musculoskeletal system have been demonstrated as they prevent osteoporosis, reduce fractures, and improve the function of patients with rheumatoid and degenerative arthritis. Physical activity is also important in reducing musculoskeletal pain and aiding the rehabilitation of injured patients. Exercise therapy plays a major role in back pain, shoulder impingement syndrome, myopathy syndrome, fibromyalgia syndrome, plantar fasciitis, and ankle sprains.
The effect of exercise on mental health have been proven in depression, anxiety, stress, sleep, dementia, and psychological well-being. Physical activity lowers the risk of depression and improves depressive symptoms, regardless of whether they are diagnosed with depression. It reduces symptoms of anxiety regardless on whether the episode is acute or chronic. Improvement in sleep quality after exercise can be attributed to reduced length of time it takes to go to sleep, reduced awakening, increased deep sleep, and reduced daytime sleepiness. Improvement in cognitive function, memory, concentration, and learning ability were also demonstrated.
Conversely, intensive physical activity pressure on the cardiopulmonary and musculoskeletal systems negatively. Undiagnosed ischemic heart disease can cause a myocardial infarction triggered by exercise. However, it can be prevented by appropriate physical activity, and the overall risk of a heart attack from exercise is relatively low compared its public health benefit.
PHYSICAL ACTIVITY RECOMMENDATIONS AND STATUS IN KOREA
1. Guidelines for Physical Activity
The department of health and human services of the United States has published guidelines for physical activity for Americans in 2018. It is the modified from one from the 2008 US Physical Activity Guidelines and the World Health Organization (WHO) Physical Activity Guidelines in 2010 [2]. The Ministry of Health and Welfare of Korea issued guidelines of physical activity for Koreans in 2013. The Korean and US guidelines are similar, and the revised guidelines have the same basic principles, although some guidelines have been revised and supplemented.
In all the physical activity guidelines, adults are encouraged to practice moderate aerobic physical activity for at least 150 minutes per week, or alternatively 75 minutes of high intensity exercise. High intensity exercise means vigorous intensity exercise. In this article, both words have been used as the same meaning. We can assume 1 minute of high intensity activity is equal to 2 minutes of moderate intensity activity. When combining high and moderate intensity activities, the guidelines of 150 minutes or more per week should be based on moderate intensity activity. For example, if you have 50 minutes of high intensity activity per week (100 minutes as moderate intensity) and 60 minutes of moderate intensity activity, it will be calculated as 160 minutes of moderate physical activity.
The latest US guidelines state that the moderate aerobic physical activity should be at least 150–300 minutes. This suggests that it is a minimum goal to increase to 300 minutes as much as possible, rather than just 150 minutes per week. It also stated that more than 300 minutes of moderate physical activity is linked to more health benefits.
Moderate physical intensity refers to the exercise intensity corresponding to 3 to 5.9 metabolic equivalents (METs), while high intensity refers to 6 METs and more. One MET is an oxygen uptake of 3.5 mL/kg/min when an adult is resting and corresponds to an energy consumption of 1 kcal/kg per hour. Moderate (3 to 5.9 METs) and high intensity (over 6 METs) physical activities are broad, but the high intensity is roughly double the intensity of moderate intensity.
During light-intensity activities most people are able to sing, during moderate-intensity they can talk but not sing, and during vigorous activities, even talking is difficult.
In the past, physical activity for more than 10 minutes at a time was recommended because evidence was based on the research that studied physical activities for longer than 10 minutes. But it is now known that exercising for as little as 10 minutes is effective, so exercise duration is no longer emphasized [3].
Since sparse exercise, defined as between 1–2 times per week, increases the risk of injury, it is recommended to exercise three or more days a week, for as many days as possible. Particularly, some papers showed that chronic disease patients should perform exercises for more than 3 days a week. Because increased insulin sensitivity by acute bout of exercise dissipate in 48–72 hours [4].
Many data sets define the intensity of exercise by the type of physical activity. The most extensive and accurate list is the compendium of physical activities from the University of South Carolina [5]. Intensities of daily activities, such as gardening, house chores, as well as sports activities, are clearly defined.
It is inappropriate to express intensity of exercise by the amount of sweat. Sweating ability varies from person to person and is affected by temperature and humidity. To be more precise, the intensity can be expressed as heart rate or maximum oxygen uptake, but this is too complicated to use in practice.
Muscle strengthening exercises or resistance exercises reduce the risk of injury, and help maintain weight. It is better to space muscle strengthening exercises to 2 to 3 times a week by each muscle groups rather than on consecutive days. This is because micro-tears in muscle fibers caused by muscle strengthening exercises need time to recover. Moreover, if exercise is performed frequently, the risk of injury may increase.
Muscle strengthening exercises include dumbbells, weight-lifting, push-ups, sit-ups, knee-flexion and extension, and moving objects. Most of the exercises using instruments at a gym are muscle strengthening exercises.
A typical method of determining the appropriate weight for an individual is as follows:
First, there is a way to express the load as a percentage of the maximum weight, or 1 repetition maximum (RM). Approximately 60%–70% of 1 RM (moderate to hard intensity) is for novice to intermediate exercisers to improve their strength. At 80% or higher of 1 RM (hard to very hard intensity) is when experienced strength trainers to improve strength. With 40%–50% of 1 RM (very light to light intensity), older persons and sedentary people initially beginning to exercise can start to improve strength.
The second is a method that estimates appropriate starting weight by what can be lifted. It is used largely because it is easy to measure. Generally, the weight recommended for resistance exercise is the one that can be lifted 8 to 15 times at a time.
Muscle strength is usually increased by the weighted exercise with eight repetitions, while muscular endurance is improved by the one 15 repetitions. Therefore, at the beginning, using a weight that can be lifted only 8 times at a time is recommended. If the designated weight can be lifted 15 times at a time, then it can be increased.
The easiest way is to breathe while doing muscle strengthening exercises is slowly without a pause while lifting a weight for 3 seconds, resting for 1 second, then lowering it for 3 seconds. This is repeated 8–15 times, which is called a set. It is appropriate to perform three sets of muscle strengthening exercise.
Guidelines recommend the elderly or 65 years of age or older should do same physical activities as adults. Especially for the elderly, prevention of falls is important, so balance, leg strength, and flexibility should be improved.
Physical activities for fall prevention should be performed more than 3 times a week, which can include the following: standing on one leg, moving the upper body while standing on one leg, standing or moving on a heel, standing with closed eyes, and standing on a soft, bumpy, or inclined floor. Physical activity should be modified according to the physical fitness and situation to prevent injury.
Children and adolescents should perform 60 minutes or more of physical activity daily which includes aerobic, muscle and bone strengthening activities.
Most of the 60 minutes or more per day should be either moderateor vigorous-intensity aerobic physical activity and should include vigorous-intensity physical activity for at least 3 days a week. They should also include muscle and bone-strengthening physical activity on at least 3 days a week. Jumping, hopping, skipping, and dancing are activities that are good examples of these.
Warming up and cooling down should be done pre- and post-exercise period. These are physical activities with an intensity of about 50% of the originally planned exercise and may include stretching [6]. For example, you can walk and stretch before and after jogging.
Although the evidence of warming up for prevention of injuries is weak, it is recommended to be carried out to prevent musculoskeletal injuries and heart attacks. Cooling down is also recommended to promote recovery from minute injuries and to prevent dizziness after exercise.
Physical activity should also be performed for chronic patients because regular physical activity is very important for general health maintenance and prevention of cerebrovascular disease. Primary care physicians should encourage the patients with chronic diseases to perform physical activity, educate them on how to exercise safely in accordance with their physical strength, and give them precautions for exercise [7].
Table 1 summarizes the recommendations of primary care physicians recommend physical activity for the patients based on the WHO, US, and Korea Physical Activity Guidelines.
Table 1.
Recommendations for physical activities for the patients in primary care
| Recommendations | |||
|---|---|---|---|
| 1. | Primary care physicians should frequently check on the amount of physical activity performed by the patients and encourage physical activities. | ||
| 2. | Educate patients to perform the following physical activities: | ||
| 1) | Move as much as possible and avoid sedentary activities. | ||
| 2) | For substantial health benefits, adults should perform at least 150–300 min/wk of moderate-intensity, 75–150 min/wk of vigorous-intensity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week. Additional health benefits are gained by engaging in physical activity beyond the equivalent of 300 minutes (5 hours) of moderate-intensity physical activity per week. | ||
| 3) | Adults should also perform muscle-strengthening exercises of moderate or greater intensity that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits. | ||
| 4) | Guidelines for the elderly (aged 65 years or older) are as follows: | ||
| (1) | The key guidelines for adults also apply to the elderly patients depending on their condition. | ||
| (2) | Balance training and fall prevention exercises should be performed more than 3 times a week | ||
| (3) | Older adults should determine their level of effort for physical activity relative to their level of fitness. | ||
| 5) | Guidelines for children and adolescents | ||
| Patients should perform 60 minutes or more of moderate-to-vigorous physical activity daily with the following distribution: | |||
| (1) | Aerobic: Most of the daily activity should be either moderate-or vigorous-intensity aerobic physical activity and should also include vigorous-intensity physical activity on at least 3 d/wk. | ||
| (2) | Muscle-strengthening: Children and adolescents should include muscle-strengthening physical activity as part of their 60 minutes or more of daily activity on at least 3 days a week. | ||
| (3) | Bone-strengthening: Children and adolescents should include bone-strengthening physical activity on at least 3 days a week. | ||
| 3. | Warming up and cooling down exercises are recommended in the pre- and post-exercise period, respectively. | ||
| 4. | If patients have chronic diseases, they must engage in physical activity, as outlined above; however, the following considerations should be kept in mind: | ||
| 1) | Regular physical activity is crucial to maintaining health and preventing cardiovascular disease complications. | ||
| 2) | Patients must consult their physician and work out safely according to their fitness level. | ||
2. Status of Physical Activity in the Korean Population
According to the Korea National Health and Nutrition Examination Survey about 50% of Korean adults met the guidelines for aerobic physical activity. Unfortunately this percentage has been decreasing yearly from 2014 to 2017 (Figure 1) [8]. About 20% of Korean adults who met the guidelines of muscle strengthening physical activity (Figure 2) [8]. Muscle strengthening activities should be encouraged more, especially for women.
Figure. 1.
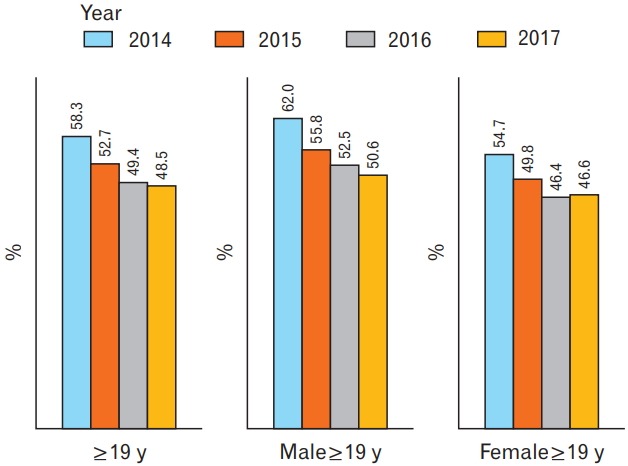
Proportion of Korean adults who met the aerobic physical activity guidelines, 2014–2017. From Korea Center for Disease Control and Prevention. Korean National Health and Nutrition Examination Survey reports [Internet]. Cheongju: Korea Center for Disease Control and Prevention [cited 2019 May 4]. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.[8]
Figure. 2.
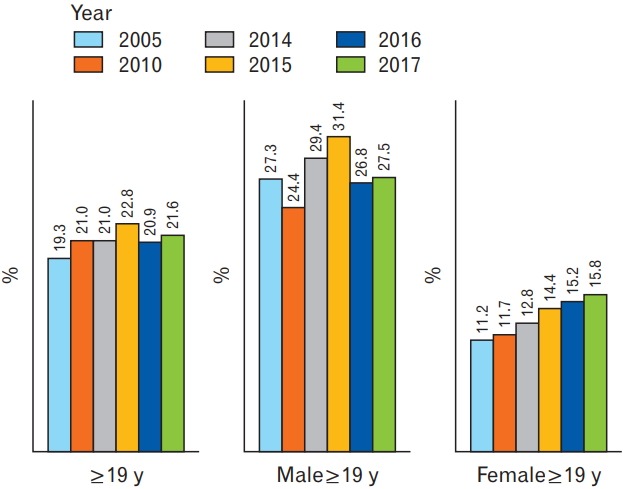
Proportion of Korean adults who met the muscle-strengthening activity guidelines, 2005–2017. From Korea Center for Disease Control and Prevention. Korean National Health and Nutrition Examination Survey reports [Internet]. Cheongju: Korea Center for Disease Control and Prevention [cited 2019 May 4]. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.[8]
Korean adults who met the physical activity guidelines in 2014 were 15.6% of the total population, comprising of 22% of total men, 9.4% of total women (Figure 3) [8]. As age increased, fewer physical activities were performed. In the United States, about 26% of men, 19% of women, and 20% of adolescents met the guidelines in 2016 [9].
Figure. 3.
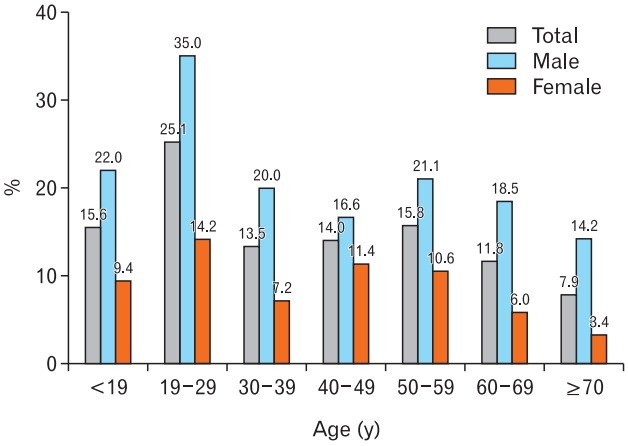
Proportion of Korean adults who met the aerobic and musclestrengthening guidelines, 2014. From Korea Center for Disease Control and Prevention. Korean National Health and Nutrition Examination Survey reports [Internet]. Cheongju: Korea Center for Disease Control and Prevention [cited 2019 May 4]. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.[8]
3. Exercises for Musculoskeletal Health
Exercise is one of the main treatment methods for some musculoskeletal disorders [10]. Chronic pain leads to muscle atrophy and joint contracture, fatigue and even depression, which exercise can then alleviate.
Muscle strengthening exercises and flexibility and balance training are the cornerstones for the treatment of musculoskeletal diseases.
Muscle strengthening exercise is recommended to be performed 2–3 times a week. It is necessary to leave more than one day of rest in between to relax and strengthen muscles.
Stretching is required for whole body muscles. Larger muscles such as the calves, thighs, hamstrings, lumbosacral spine, and anterior shoulder muscles particularly should be stretched to be flexible. For those with back pain, it is essential to stretch the muscles behind the waist and femur. Range of motion exercises are helpful for the arthritic joints.
A sense of balance prevents injuries caused by falls. Although balance improves to some extent with muscle strengthening or stretching exercises, it is preferable to have active balance training.
Exercise therapy is effective in the treatment of some musculoskeletal problems such as shoulder instability and/or impingement syndrome, myofascial pain syndromes (upper trapezius, sternocleidomastoid muscle, levator scapulae, and other such muscles), adhesive capsulitis, tennis and golf elbows, osteoarthritis, patellofemoral pain syndrome, and chronic low back pain.
In order to treat musculoskeletal pain of the shoulder, exercises for shoulder stability and rotator cuff strengthening are important. Muscle strengthening and stretching of the wrist are needed for tennis and/or golf elbow. To prevent and treat knee osteoarthritis, walking, cycling and swimming are recommended. Aerobic exercise and muscle strengthening training around the joints are needed for the treatment of osteoarthritis. Weight reduction of 5% of total body weight improves osteoarthritis if the patient is overweight. Overall, exercise reduces musculoskeletal pain and improve function, quality of life as well as mental health.
Exercise is not recommended for acute lower back pain although it is effective for chronic lower back pain (LBP). Core stabilization exercises are recommended for chronic LBP. Aerobic exercise is also good for chronic LBP.
Exercise should be modified according to the individual’s response. For example, if the patient feels pain during the musculoskeletal exercise, it is recommended to hold the exercise. If the patient feels pain next day as well, the amount of exercise should be reduced 50%. From there, they can gradually increase the amount.
PRECAUTIONS WHEN EXERCISING
Exercise should be done safely and effectively. Primary care physicians should have four basic principles in mind for the recommendation of physical activities.
First, exercise should not impair or damage patients’ health. Second, exercise should be effective; it should improve illnesses and promote health. Third, overloading is needed since it is effective when the patient applies a load greater than what is usually experienced in normal routine. Fourth, slow progression is needed. Depending on the patient’s fitness level, the patient should increase their load from low to high, gradually.
Exercise prescription should include five elements of exercise: type, intensity, duration, frequency, and speed of movement. Primary care physicians should inform the patient of the risks and provide them with precautions for that particular exercise.
1. Exercise-Induced Heart Attack or Musculoskeletal Injuries
People with chronic diseases who have cardiovascular risk factors may not have any problems even if they are active. However, since there may be a component of underlying cerebrovascular disease, it is recommended to determine if the patients have any abnormal symptoms or signs before they start their activity. If they are planning for higher intensity physical activity, a more thorough check-up is needed. If the risk of cardiovascular disease is high, it is important to exclude the possibility of ischemic heart disease. Recent myocardial infarction, unstable angina, acute heart failure, and complete heart block are contraindications to exercise.
Patients with chronic diseases or disability can have health benefits even with low intensity activities. Physical activity should be modified on an individual basis. Patients who have not exercised before should begin with mild activity for less than 10 minutes. Activity time is increased gradually, and if there are no problems, the number of days of activity per week are increased. It is safe to increase exercise intensity after an increase in exercise time. If periodic physical activity is temporarily suspended due to illness or injury, it is safe to start again with lower activity intensity and gradually increase it to previous activity levels.
A heart attack may occur when the patients exercise violently due to undiagnosed arteriosclerosis. However, the risk of a heart attack due to exercise is relatively small compared to the risk reduction of myocardial infarction by exercise. The sudden death risk of an active person is about 30% of inactive people.
If the patient is a novice who undergoes sudden, strenuous exercise, overuse syndromes such as sprains, tendinopathies, shin splints, fasciitis, bursitis, and stress fractures may occur. In order to prevent overuse syndromes, it is necessary to use adequate footwear with arch support, obtain proper nutrition and hydration, perform adequate warming up, gradually increase exercise time and intensity, have a good posture during exercise, and engage in cross training [11]. Cross training alternates the type of exercises engaged, which reduces boredom and prevents overuse syndrome.
Once a patient is injured or sprained, resting of the joints and muscles are recommended. For example, if a knee problem occurs with jogging or aerobics, free style swimming or aquatic exercise may be applied to rest the injured knee.
Overtraining syndrome refers to myalgia, chronic fatigue, and overuse syndrome caused by excessive exercise. When the exercise ability is reduced, reduction of the amount of exercise or rest is recommended to rule out overtraining syndrome.
2. General Exercise Precautions
When exercising outdoors, patients should be mindful about temperature, humidity, and air pollution. Generally, exercising for more than 30 minutes at 27℃–29℃ and above 70% relative humidity is harmful to the body and is a contraindication to exercise, especially for heart disease patients. In hot weather it is better to exercise early in the morning or evening or indoors.
When pollen-sensitive asthmatic patients exercise outdoors, preventive measures are needed, such as bronchodilator inhalation. In cold weather, asthma is easily induced by exercise because of dry air, thus, indoor activities are recommended.
When prescribing exercise, the primary care physician needs to identify the patients’ current medication and respond appropriately. For example, if a patient is taking nitroglycerin, intervals as needed between medication and exercise because exercising immediately after taking nitroglycerin may cause hypotension. Insulin-dependent patients with diabetes should reduce the amount of insulin to prevent hypoglycemia, and administration should be on the abdomen instead of extremities to prevent quick absorption. Beta blockers may slow the heart rate; therefore, the primary care physician should not use heart rate as an index of exercise intensity in these patients. Subjective exercise intensity is a more appropriate and realistic indicator. Beta blockers may also reduce exercise capacity by reducing cardiac contractility. Potassium sparing diuretics may cause hyperkalemia, while other diuretics may cause potassium deficiency, resulting in arrhythmias during exercise. It should also be noted that anticholinergic drugs such as antispasmodics and antihistamines may inhibit sweating and can easily increase body temperature.
3. Precautions in Chronic Diseases
1) Diabetes mellitus
To date, there is no consensus on whether pre-exercise health screening should be performed for patients with diabetes. Patients with diabetes who are asymptomatic and inactive may not be required to undergo screening if they perform low or moderate intensity exercise; if the intensity is equivalent to brisk walking or less, screening is not necessary. However, if they are going to engage in more intense activity than usual, if they are at high risk for cardiovascular disease (high blood pressure, smoking, family history, and other such factors) and if they are suspected to have other exercise-related health problems, pre-exercise screening is needed [12].
Patients with diabetes are also encouraged to exercise per standard guidelines but with additional emphasis on exercising more than three days a week. Rest for more than 2 days is avoided due to the temporary positive effect of exercise on insulin sensitivity.
Exercise-induced hypoglycemia should be considered as insulin sensitivity increases for about 24–48 hours after active exercise. Hypoglycemia can occur due to exercise particularly when insulin secretagogues or insulin injections are used. Fortunately, there are many types of diabetes medications that rarely cause hypoglycemia. To determine effect of exercise on blood glucose, measurements of blood glucose before and after exercise are recommended. If the patient has a high risk of hypoglycemia, reduction of pre-exercise medication dose or having a pre-exercise meal is required. If the pre-exercise blood glucose is less than 90 mL/dL, carbohydrate intake is necessary. Insulindependent patients with diabetes should reduce their insulin dose to prevent development of exercise-induced hypoglycemia and should consume carbohydrates once hypoglycemic symptoms occur. In addition, on the day of exercise, injection into the arms and the legs which muscles that are mostly exercising should be avoided, injection into the abdomen is recommended to prevent too rapid insulin absorption.
In order to prevent hypoglycemia, it is advisable to perform resistance exercises or short-distance running before aerobic exercise. This is because strenuous activity can signal counter-regulatory hormones which can prevent a decrease in the blood glucose.
Exercise-induced nocturnal hypoglycemia should also be noted. Blood glucose levels can be reduced up to 48 hours after exercise. This can be prevented by a reduction in evening insulin dose, incorporating midnight snacks, and engaging in continuous glucose monitoring.
Exercise-induced hyperglycemia is also possible, especially when high pre-exercise blood glucose is elevated. It can be caused by high intensity exercise such as short-distance running, strong aerobic exercise, and heavy weight-lifting exercises. If patients are going to perform these exercises, insulin dose control and interval training (alternating between high intensity and moderate intensity exercises) are recommended.
If uncontrolled blood pressure, severe autonomic or peripheral neuropathy, history of diabetic foot disease, and/or unstable proliferative retinopathy are present, it is advisable to avoid high intensity exercise and to perform moderate and lower intensity exercise.
If autonomic neuropathy is present, sudden vertical positional changes should be avoided to prevent orthostatic hypotension. Adequate hydration is required for prevention of dehydration and hyperthermia. Because of the possibility of diabetic foot ulcers, the patient should have well-fitting shoes and conduct a careful inspection for wounds before and after their workout.
If there is severe non-proliferative retinopathy or unstable proliferative retinopathy, high intensity aerobic exercise and resistance exercise should be avoided. In particular, jumping, exercises with a lowered head, and breath holding exercises should be avoided. Breath holding during isometric exercise that does not change in distance can increase intraocular pressure via the Valsalva effect.
Unlike the previous guidelines, there is no limitation of exercise when albuminuria or kidney disease is present. Physical activity can be performed even during dialysis.
High-intensity exercise should be avoided if there is concern of ketoacidosis. However, if there is no ketoacidosis and the patient’s overall systemic condition is good, it is not necessary to delay exercise even if hyperglycemia is present. Unlike previous guidelines, hyperglycemia itself is not a contraindication to exercise. High-intensity exercise is safe when pre-exercise blood glucose is less than 250 mg/dL [13]. In addition, if type 1 diabetes patients do not get insulin injections for a long time, hyperglycemia may occur, so it is desirable to prohibit vigorous activities.
2) Hypertension
The importance of physical activity has become even greater as the levels designating of hypertension have decreased. In the case of systolic blood pressure 130–140 mm Hg, lifestyle modification is recommended before taking medication. Physical activity lowers blood pressure by 5–8 mm Hg. Regardless of exercise intensity, duration, or type, blood pressure lowering effects are demonstrated.
Previously resistance exercises were prohibited in hypertensive patients because it was hypothesized to cause a Valsalva effect and decrease blood circulation, which then would result in a compensatory elevation in heart rate and subsequent elevation in blood pressure. However, this has been disproven by many studies and ultimately have shown that there are blood pressure lowering effects in the long term. As a result, patients with hypertension are now encouraged to perform resistance exercises. Dynamic resistance exercise is safe and effective in hypertension if the load is not too heavy [14]. Generally, the weight that can be lifted 8 times or more is not a problem. While isometric exercise is safe and effective, there is not enough evidence to support it, so it cannot be formally recommended.
However, hypertensive patients may have problems if the weight is too heavy, thus should be encouraged to exercise with proper weights and to avoid breath holding.
3) Osteoarthritis
In patients with osteoarthritis, exercise reduces pain, improves quality of life, and improves physical function. Therefore, the guidelines have been changed from not recommending exercise to highly recommending it. Recommendations for non-pharmacological treatment include weight loss (5% decrease in total body weight when overweight), aerobic physical activity, range of motion exercises, resistance exercises, and proper footwear [15].
For patients with hip and knee osteoarthritis, it is recommended to engage in low-impact exercises with low weight-bearing. Additionally, swimming and stationary bicycle exercises are preferable. However, it is important to consider that the breast-stroke can be a challenge for patients with knee osteoarthritis, because it requires wide knee flexion. If knee pain occurs, it is advised to swim using free style, back stroke or participate in an aquatic sport. Even when riding a stationary bicycle, knee pain worsen due to continuous knee flexion. Raising the saddle height of the stationary bicycle to straighten the leg may relieve knee pain. Knee flexion and extension exercises in addition to cycling would be helpful in decreasing knee loads. For example, a semi-squat exercise is effective.
Muscle strengthening exercises around the knee, especially the quadriceps, are essential in treating lower extremity osteoarthritis and also in alleviating patellofemoral pain syndrome.
CONCLUSION
Exercise or physical activity should be done at least moderately. Adult physical activity guidelines are for moderate intensity aerobic physical activity for 150–300 minutes per week and muscle strengthening exercise 2–3 times a week. The elderly have the same physical activity guidelines as adults, but additionally need balance training to prevent falls. Children and adolescents need at least one hour of physical activity each day, including high intensity aerobic activity, resistance training, and bone strengthening exercises for at least three days per week. Previously, physical activities for more than 10 minutes were recommended, but now shorter activities are being encouraged because evidence demonstrates that shorter activities are also effective. However, since the aerobic physical activity of Korean people is decreasing, various efforts are needed to promote physical activity.
Living a sedentary lifestyle is also an independent risk factor for disease, and even a little physical activity has a positive impact on our health.
The risk of injuries or negative outcomes from physical activities should be identified and eliminated by pre-participation testing, for patients who are at risk. It is also necessary to provide exercise instructions and exercise precautions to prevent injuries.
In reality, it is not easy to carry out detailed exercise counseling during busy outpatient clinic hours. However, during primary care appointments, physicians have an opportunity to assess and encourage physical activity for their patients. It is necessary to caution patients with hypertension, diabetes and osteoarthritis on appropriate physical activity.
Footnotes
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Matthews CE, Jurj AL, Shu XO, Li HL, Yang G, Li Q, et al. Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women. Am J Epidemiol. 2007;165:1343–50. doi: 10.1093/aje/kwm088. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization; 2010. Global recommendations on physical activity for health [Internet] [cited 2019 Apr 29]. Available from: http://whqlibdoc.who.int/publications/2010/9789241599979_eng.pdf. [PubMed] [Google Scholar]
- 3.Rockville (MD): U.S. Department of Health and Human Services; 2018. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee scientific report [Internet] [cited 2019 Apr 29]. Available from: https://health.gov/paguidelines/second-edition/report/ [Google Scholar]
- 4.King DS, Baldus PJ, Sharp RL, Kesl LD, Feltmeyer TL, Riddle MS. Time course for exercise-induced alterations in insulin action and glucose tolerance in middle-aged people. J Appl Physiol (1985) 1995;78:17–22. doi: 10.1152/jappl.1995.78.1.17. [DOI] [PubMed] [Google Scholar]
- 5.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Jr, Tudor-Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 6.Horia-Daniel I, Georges J. Comparison of two warm-up models for obese and normal-weight adults performing supramaximal cycling exercise. Biol Sport. 2018;35:93–8. doi: 10.5114/biolsport.2018.71487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang YJ. Physical activity. In: Korean Academy of Family Medicine, editor. Family medicine. 4th ed. Seoul: IJPNC; 2013. pp. 232–41. [Google Scholar]
- 8.Korea Center for Disease Control and Prevention . Cheongju: Korea Center for Disease Control and Prevention; Korean National Health and Nutrition Examination Survey reports [Internet] [cited 2019 May 4]. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7. [Google Scholar]
- 9.Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320:2020–8. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang YJ. Exercise therapy for musculoskeletal pain. Korean J Fam Pract. 2014;4:186–93. [Google Scholar]
- 11.Brukner P, Khan K. Clinical sports medicine. 4th ed. Sydney: McGrow Hill; 2012. [Google Scholar]
- 12.Colberg SR. Key points from the updated guidelines on exercise and diabetes. Front Endocrinol (Lausanne) 2017;8:33. doi: 10.3389/fendo.2017.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–79. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for hypertension: a prescription update integrating existing recommendations with emerging research. Curr Hypertens Rep. 2015;17:87. doi: 10.1007/s11906-015-0600-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000;43:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]


