Abstract
Background:
Variables affecting return to sport after anterior cruciate ligament reconstruction (ACLR) are multifactorial. The nonphysical factors germane to successful return to play (RTP) are being increasingly recognized.
Purpose:
To (1) evaluate the available evidence base for psychological factors relating to RTP after ACLR, (2) identify psychological factors affecting RTP after ACLR, and (3) understand currently available metrics used to assess psychological RTP readiness.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A review of the MEDLINE database was performed for studies reporting RTP after ACLR. Studies reporting on the psychological determinants of RTP were included. Demographic, methodological, and psychometric properties of the included studies were extracted. Weighted analysis was performed after patients were pooled across included studies.
Results:
Of 999 studies identified in the initial search, 28 (2.8%) studies, comprising 2918 patients, were included; 19 studies (n = 2175 patients) reported RTP rates. The mean time for RTP was 17.2 months. There was a 63.4% rate of RTP, and 36.6% of patients returning to sport were not able to perform at their prior level of play. Of the 795 patients who did not achieve RTP, 514 (64.7%) cited a psychological reason for not returning. Fear of reinjury was the most common reason (n = 394; 76.7%); other psychological factors included lack of confidence in the treated knee (n = 76; 14.8%), depression (n = 29; 5.6%), and lack of interest/motivation (n = 13; 2.5%). The Tampa Scale for Kinesiophobia, the Hospital Anxiety and Depression Scale, the ACL–Return to Sport after Injury scale, and the Knee Self-Efficacy Scale were reported measures for assessing the influence of psychology on RTP.
Conclusion:
Psychological factors play an important role in RTP after ACLR. Among studies evaluating the impact of psychology on RTP, there was a delay in returning as well as lower RTP rates compared with the previously reported normative literature. Fear of reinjury was the most commonly reported impediment to RTP. The psychosocial measures identified in this review may have a role in RTP protocols for assessing mental resiliency; however, their roles need to be further investigated and validated in patients who have undergone ACLR.
Keywords: anterior cruciate ligament, anterior cruciate ligament reconstruction, return to sport, sport psychology
Anterior cruciate ligament reconstruction (ACLR) is commonly performed in active patients with the goal of returning to preinjury sport participation.7,16,26 The currently available evidence base demonstrates variable rates of return to sport, with the reported incidence within 1 year of surgery between 33% and 92%.2,3,7,15 A meta-analysis looking at articles citing return to sport after ACLR demonstrated that, on average, 81% of people returned to any sport, 65% returned to their preinjury level of sport, and 55% returned to competitive-level sport after surgery.2 Known factors affecting return to play (RTP) include graft type, patient age, baseline activity level, sport type, and athletic experience within the sport.
Studies have found that objective measures of physical impairment may not relate to patient-reported knee function. As such, it has now been established that return to sport cannot be solely predicted by objective physical improvement after surgery.20 Variables affecting return to sport after ACLR are multifactorial, and specifically, psychological factors influencing RTP after ACLR are not as well described.
Psychological factors are being increasingly recognized as an important determinant of the ability for return to sport after ACLR. Ardern et al4 reported fear of reinjury as the most commonly cited reason for not returning to preinjury levels of activity after ACLR. Nwachukwu et al25 found that the 12-Item Short Form Health Survey Mental Composite Scale (SF-12 MCS) was a significant predictor of clinically significant outcomes and RTP after ACLR. Thus, while there has been increased attention to the role of psychology on RTP after ACLR, there has yet to be a comprehensive review of the state of evidence on the topic.
The purpose of this study was therefore to (1) evaluate the available evidence base for psychological factors relating to return to sport after ACLR, (2) identify psychological factors and their impact on the ability to RTP after ACLR, and (3) understand currently available metrics used to assess psychological return-to-sport readiness.
Methods
A systematic review of the MEDLINE database using the PubMed interface was performed in January 2018. Results were limited to articles published in PubMed between January 1, 1998, and December 1, 2017. The following search term was constructed: (((acl return play) OR acl return sport) OR anterior cruciate ligament return sport) OR anterior cruciate ligament return play. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines with the PRISMA checklist were appropriately applied.
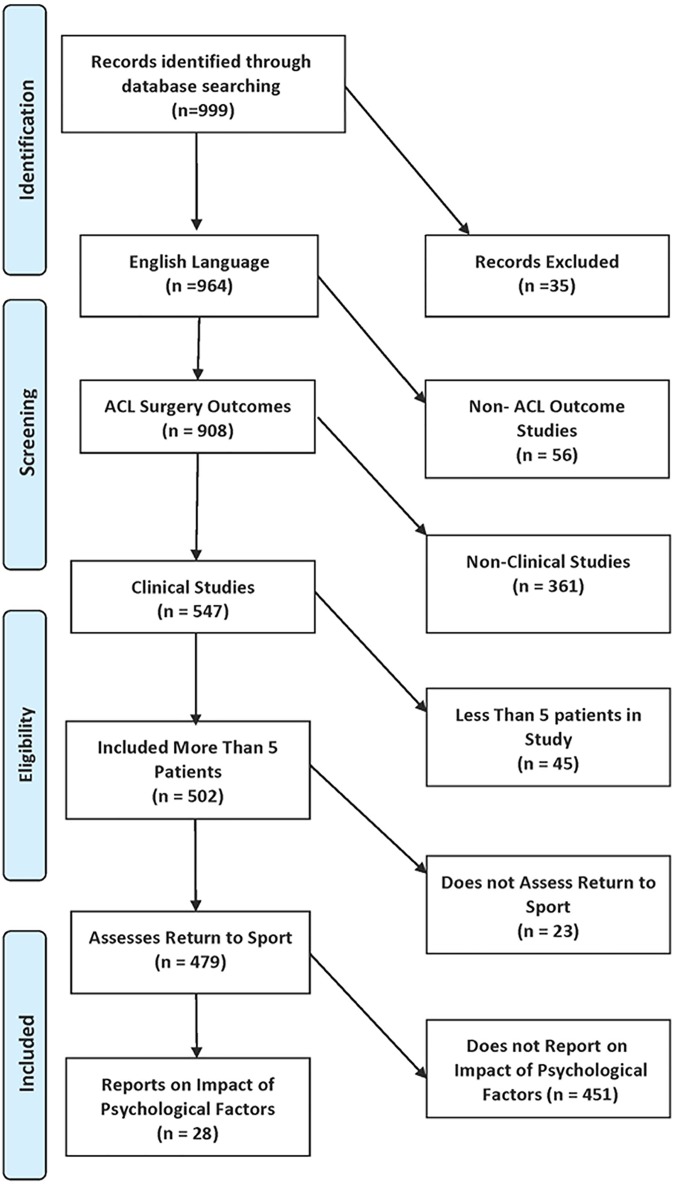
The primary search resulted in 999 articles. Each article was reviewed for inclusion with the following criteria: English language, studies related to clinical outcomes of ACLR, more than 5 patients included, and assessment of return to sport and reports on the impact of psychological factors on RTP (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart of inclusion and exclusion criteria. ACL, anterior cruciate ligament.
Extracted data from each study included the following: journal and author name, time of publication, level of evidence, number of patients, patient sex, patient age, ACLR graft type, mean follow-up time, and whether patients returned to play and the time until return to sport. Psychological measures utilized by the studies, psychological reasons cited by patients who did not return to sport, and proportion of patients who cited these reasons were also recorded. Studies were evaluated to determine preoperative and postoperative psychological factors that could be used to predict RTP. Finally, the quality of each study was evaluated using the Methodological Index for Non-Randomized Studies (MINORS) criteria. The MINORS is a validated scoring tool for nonrandomized studies that includes a 24-point scale for comparative studies and a 16-point scale for noncomparative studies.30
The heterogeneity of reported outcome data precluded a formal meta-analysis. Thus, statistics were primarily descriptive, and each study was analyzed qualitatively. Weighted analysis was performed after patients were pooled across included studies.
Results
Characteristics of Included Studies and Patients
Of 999 studies identified in the initial search, 28 (2.8%) met the inclusion criteria. Of these studies, 7 were level 2 evidence, 11 were level 3 evidence, and 10 were level 4 evidence. The studies were evaluated using the MINORS criteria; the included studies had a mean score of 12 (range, 8-20).30 Included studies came from a total of 16 different journals and were published between 1999 and 2017. The most common journals of publication for the included studies were Knee Surgery, Sports Traumatology, Arthroscopy and The American Journal of Sports Medicine (Table 1).
TABLE 1.
Characteristics of Included Studies (N = 28)a
| Level of evidence, n (%) | |
| 1 | 0 (0.0) |
| 2 | 7 (25.0) |
| 3 | 11 (39.3) |
| 4 | 10 (35.7) |
| Mean MINORS score | 12 |
| Journals included, n | |
| Knee Surgery, Sports Traumatology, Arthroscopy | 6 |
| The American Journal of Sports Medicine | 5 |
| Journal of Bone and Joint Surgery | 1 |
| Orthopaedic Journal of Sports Medicine | 2 |
| Sports Health | 1 |
| Journal of Orthopaedic Surgery | 1 |
| Scandinavian Journal of Medicine & Science in Sports | 2 |
| Journal of Physiotherapy | 1 |
| BMC Sports Science, Medicine and Rehabilitation | 1 |
| Journal of Science and Medicine in Sport | 1 |
| Archives of Orthopaedic and Trauma Surgery | 1 |
| British Journal of Sports Medicine | 2 |
| Arthroscopy | 1 |
| Physical Therapy in Sport | 1 |
| Annals, Academy of Medicine, Singapore | 1 |
| Clinical Journal of Sport Medicine | 1 |
aMINORS, Methodological Index for Non-Randomized Studies.
A total of 2918 patients (2918 knees) were pooled from the included studies. Of the included patients, the mean age was 26.7 years, and 1559 (53.4%) were male. The graft type used during ACLR was reported in 10 studies. Of the 635 grafts used in total, 439 were hamstring autografts, 123 were bone–patellar tendon–bone autografts, and 73 were allografts (Table 2).
TABLE 2.
Clinical and Demographic Variables of Included Patients (N = 2918 Patients)
| Sex, n (%) | |
| Male | 1559 (53.4) |
| Female | 1234 (42.3) |
| Not reported | 125 (4.3) |
| Mean patient age, y | 26.7 |
| Graft type reported,a n (%) | |
| Hamstring autograft | 439 (69.1) |
| Bone–patellar tendon–bone autograft | 123 (19.4) |
| Quadriceps autograft | 0 (0.0) |
| Allograft | 73 (11.5) |
| Total | 635 (100.0) |
aOf the 28 studies included, 10 reported the graft type used.
RTP and Influence of Psychology
Of the included studies, 19 (n = 2175 patients) reported RTP proportions. Among these studies, the mean time until RTP was 17.2 months and ranged between 2.5 and 60.0 months. Of the 2175 patients, 1380 (63.4%) achieved RTP, and 795 were unable to return to play after ACLR. Fifteen of the included studies (n = 1494 patients) evaluated whether patients were able to return to prior levels of activity. It was noted that 547 (36.6%) patients did not return to prior levels of play (Table 3).
TABLE 3.
Psychological Factors and Return to Play
| Time to return to play, mean (range), mo | 17.2 (2.5-60.0) |
| Studies reporting return-to-play rate, n | 19 |
| Total No. of patients | 2175 |
| Patients returning to sport, n (%) | 1380 (63.4) |
| Patients not returning to sport, n (%) | 795 (36.6) |
| Studies assessing return to prior level, n | 15 |
| Total No. of patients | 1494 |
| Patients not returning to prior level, n (%) | 547 (36.6) |
| Patients with psychological reasons for not returning to play, n (%) | 514 (64.7) |
Among the 795 patients who were not able to return to play, 514 (64.7%) cited a psychological reason for not returning. Fear of reinjury was cited as the reason for not returning to sport in 394 (76.7%) patients who did not return to play. Other psychological factors cited for failure to return included lack of confidence in the treated knee (n = 76; 14.8%), depression (n = 29; 5.6%), lack of interest/motivation (n = 13; 2.5%), and psychosocial factors (n = 2; 0.4%) (Table 4).
TABLE 4.
Patient-Cited Psychological Factors Affecting RTPa
| Patients (n = 514) | Studies (n = 20) | |
|---|---|---|
| Factors affecting RTP, n (%) | ||
| Fear of reinjury | 394 (76.7) | 13 (65.0) |
| Lack of confidence in knee | 76 (14.8) | 3 (15.0) |
| Depression | 29 (5.6) | 1 (5.0) |
| Lack of interest/motivation | 13 (2.5) | 3 (15.0) |
| Psychosocial | 2 (0.4) | 1 (5.0) |
| Factors predicting RTP | ||
| Preoperative | Motivation for RTP Importance of RTP Possibility of RTP SF-12 MCS |
|
| Postoperative | Motivation during rehabilitation Self-esteem MHLC ACL-RSI ISP |
|
aACL-RSI, Anterior Cruciate Ligament–Return to Sport after Injury scale; ISP, Incredibly Short Profile of Mood States; MHLC, Multidimensional Health Locus of Control scale; RTP, return to play; SF-12 MCS, 12-Item Short Form Health Survey Mental Composite Scale.
Psychological measures commonly used to evaluate return to sport included the Tampa Scale for Kinesiophobia (TSK),22,37 the Hospital Anxiety and Depression Scale (HADS),37 the Incredibly Short Profile of Mood States (ISP),9,35 the ACL–Return to Sport after Injury scale (ACL-RSI),35 the Knee Self-Efficacy Scale (K-SES),31,35 and the Multidimensional Health Locus of Control scale (MHLC).34 Preoperative factors included patient-perceived importance of returning and motivation for RTP. Postoperative factors influencing RTP included motivation during rehabilitation as well as certain measures of psychological hardiness (Table 5).
TABLE 5.
Included Studies, Psychological Factors Considered, and Psychological Measures Useda
| Author (Year) | Factors Considered | Psychological Measures Used (Preoperative vs Postoperative) |
|---|---|---|
| Webster et al36 (2017) | Fear | N/A |
| Nwachukwu et al26 (2017) | Fear | N/A |
| Faltstrom et al10 (2016) | Lack of confidence, fear of reinjury, motivation for return, possibility of return | N/A |
| Filbay et al11 (2017) | Depression | HADS (postoperative) |
| Christino et al8 (2016) | Self-esteem | MHLC, RSES, POMS-B (postoperative) |
| Filbay et al12 (2016) | Fear of reinjury, adaptation and acceptance | N/A |
| Rodriguez-Roiz et al29 (2015) | Fear of reinjury | N/A |
| Ardern et al5 (2015) | Motivation for return | ACL-RSI, TSK, SRLC, ERAIQ, ISP (postoperative) |
| Lentz et al20 (2015) | Fear/confidence | TSK-11 (postoperative) |
| Ardern et al1 (2014) | Fear of a new injury | K-SES, MHLC, ACL-RSI, TSK-11 (postoperative) |
| Muller et al23 (2015) | Fear of reinjury | TSK-11, ACL-RSI (postoperative) |
| Tjong et al33 (2014) | Innate personality traits | N/A (postoperative) |
| Flanigan et al13 (2013) | Lack of interest | ACL-RSI, TSK-11, SRLC (postoperative) |
| Ardern et al2 (2014) | Psychological readiness, fear of reinjury | ACL-RSI, TSK-11, ERAIQ, ISP (postoperative) |
| McCullough et al21 (2012) | Fear of reinjury | N/A |
| Webster et al35 (2008) | Emotions, confidence in performance, risk appraisal | N/A |
| Langford et al18 (2009) | N/A | ACL-RSI, ERAIQ (postoperative) |
| Lee et al19 (2008) | Fear of reinjury | N/A |
| Gobbi and Francisco14 (2006) | Fear of reinjury, personal reasons | “Psychovitality” (preoperative) |
| Kvist et al17 (2005) | Fear of reinjury, motivation for return | TSK-11 |
aACL-RSI, ACL–Return to Sport after Injury scale; ERAIQ, Emotional Responses of Athletes to Injury Questionnaire; HADS, Hospital Anxiety and Depression Scale; ISP, Incredibly Short Profile of Mood States; K-SES, Knee Self-Efficacy Scale; MHLC, Multidimensional Health Locus of Control scale; N/A, not available; POMS-B, Profile of Mood States–Brief; RSES, Rosenberg Self-Esteem Scale; SRLC, Sport Rehabilitation Locus of Control scale; TSK, Tampa Scale for Kinesiophobia.
Discussion
In this study, we found that psychological factors play an important role in RTP after ACLR. Among studies evaluating the impact of psychology on RTP, there was a 63.4% (1380/2175 patients in 19 sampled studies) rate of RTP. Furthermore, 36.6% (547/1494 patients in 15 studies) were not able to return to the same level of play. Among included studies, the mean time for RTP was 17.2 months, which is longer than in the previously reported normative literature. In a study considering RTP in 187 patients, 124 of whom were competitive athletes, Ardern et al4 found that worse ACL-RSI and TSK scores were associated with slower rates of RTP after ACLR, a finding that may play a role in the longer time for RTP in our systematic review. These findings suggest that when psychological factors are present in study cohorts, there is a decline in the RTP rate as well as a prolongation of the time for RTP. Fear of reinjury was the most commonly reported psychological factor. Preoperative measures of motivation and postoperative psychosocial measures such as the MHLC may have a role in identifying postoperative patients at risk for psychologically based impairment of RTP.
There is an increasing body of evidence demonstrating excellent RTP outcomes after ACLR.15,24,26,28 Despite advances in surgical technique and rehabilitation, there is a persistent subset of patients that is not able to achieve RTP after ACLR. Some authors have suggested that psychological factors are a significant impediment to maximizing postoperative outcomes after ACLR.1,4 Ardern et al4 found that psychological responses before surgery and in early recovery were associated with returning to preinjury levels of sport at 12-month follow-up. Similarly, Lentz et al20 found that elevated fear of reinjury/lack of confidence in the postoperative knee were predictive of an inability to return to preinjury sport status. In 2017, Nwachukwu et al25 found that the SF-12 MCS can be used preoperatively to identify patients who are likely to achieve RTP and a minimal clinically important difference after ACLR. The authors posited that the SF-12 MCS could be used as a proxy for mental resiliency and similar psychological traits. Brewer et al6 prospectively examined the relationship between psychological factors and rehabilitation outcomes after ACLR in 95 patients. Self-motivation, athletic identity, and psychological distress were significant preoperative predictors of objective outcomes such as knee laxity. However, postoperative rehabilitation adherence did not affect rehabilitation outcomes.6 Additionally, our study identified a skew in the proportion of psychological measures developed to identify failure to return to sport postoperatively relative to preoperative predictors of return to sport. Although the current literature shows that psychological factors identified preoperatively and postoperatively may affect RTP, there are no established guidelines on how to best approach patients at risk for not returning to play. A major strength of this review is that we compiled and analyzed the aforementioned studies as well as other relevant studies to create summative data for the impact of psychology on return to sport after ACLR.
As part of this review, we identified a number of preoperative and postoperative psychological proxies and variables that can be used to identify patients at potential risk for diminished RTP outcomes. In addition, we provided a survey of the currently utilized psychological assessments in ACLR rehabilitation as well as specific measures utilized in the studies sampled. Currently utilized psychological instruments include the TSK, HADS, ISP, ACL-RSI, K-SES, and MHLC.
Kinesiophobia is defined as a fear of pain or reinjury that may lead to the avoidance of particular movements. The TSK is a survey consisting of 17 items on the patient’s subjective experience of injury and physical activity with the goal of quantifying the fear of pain or reinjury due to physical activity.22 While not specifically validated for return to sport, there is an association between higher TSK scores (more fear of pain or reinjury) and not returning to preinjury activity levels after ACLR.17 The HADS is a self-assessment scale that is reliable in detecting states of anxiety and depression in general outpatient clinics,37 and the ISP asks respondents to rate their mood by measuring their levels of anxiety, sadness/depression, confusion, anger, energy, and fatigue.9 The ACL-RSI is a scale that measures the psychological impact of returning to sport after ACLR by assessing emotions, confidence in performance, and risk appraisal.35 The ACL-RSI has been shown to be reliable and valid after ACLR, with patients who did not return to sport scoring lower on the scale than those who returned to sport.4,35 The K-SES was developed to measure perceived self-efficacy in patients with an ACL injury.31 There are sections evaluating daily activities, sport activities, and knee functional tasks. Patients are asked to fill out the survey at the time of injury and assess their current ability to perform these tasks as well as how certain they feel about their future capabilities. Better scores on the K-SES predicted better function in physical activities 1 year after ACLR.32 The K-SES demonstrates good reliability and validity for outcomes but has not been specifically validated for return to sport after ACLR. The MHLC evaluates how patients perceive their ability to control life events. Patients who feel that they have control over their own health are more likely to comply with precautions and participate diligently in physical therapy. Subsequently, patients with MHLC scores consistent with believing events are the consequences of their own actions demonstrated better outcomes, including returning to sport, after ACLR.27
We believe that there is a role for psychological screening before ACLR. Based on the included studies, understanding motivation levels in patients with ACL injuries may be helpful for preoperatively identifying those who may be at an increased risk for poor postoperative outcomes. Specifically, the motivation for RTP, importance of RTP, and possibility of RTP were identified as preoperative factors that predict RTP outcomes after ACLR. Gobbi and Francisco14 studied return to sport in 100 patients who underwent ACLR via numerous preoperative and postoperative measures. Preoperative measures included a “psychovitality” questionnaire in which patients who returned to sport scored significantly better than patients who failed to return.14 Other measures, including the SF-12 MCS, may also be useful preoperatively in determining RTP in select patients. From our perspective, the ideal psychological measure of RTP should consider factors including willingness, motivation, and fear of returning both preoperatively and postoperatively. More studies are necessary to establish the validity and general usability of such questionnaires in patient populations of different sporting activity levels. In addition to employing preoperative screening measures, our data suggest that psychological assessments should be considered in postoperative rehabilitation and return-to-sport guidelines. We believe that screening assessments may have a role postoperatively to best tailor a graduated return-to-sport program that addresses kinesiophobia and issues of psychological unpreparedness. Psychological assessments can also be administered postoperatively on an interval basis to track progress. There is a significant opportunity for continued research in the area of psychological readiness for return to sport. More work can be done to further validate the psychological assessments identified in this review as well as to evaluate for the clinical applicability and optimal-use time frames of psychological measures.
This study is subject to certain limitations. The quality of our review is limited by the data available in the included studies. The methodological quality of the included studies was variable and may have limited the quality of the data that we were able to extract. We did not limit our included studies to recently published articles because of the expected paucity of included studies; as such, studies included in this review spanned several decades. This wide inclusion may have resulted in a heterogeneity of surgical techniques, rehabilitation protocols, and RTP criteria. Although surgical techniques, rehabilitation protocols, and RTP criteria have evolved over the past several decades, the psychological determinants of outcomes have most likely remained constant. Additionally, studies included a variety of psychological outcome measures, resulting in difficulty comparing these various measures reliably. However, the current review works to understand the breadth and scope of the literature on the topic. Future studies are needed to effectively compare the efficacy and usefulness of the various measures in different patient populations and various time frames. Similarly, because of the expected paucity of evidence, we did not apply robust qualitative exclusion criteria. We did, however, exclude studies with fewer than 5 patients to screen out low-quality studies and case reports. Additionally, while RTP is one metric of success after ACLR, this study did not assess the role of psychology on knee function or other patient-reported outcome scores that are also important for a successful outcome. Despite these limitations, our review has a number of strengths. Specifically, this study evaluated an underexplored area of ACLR outcome research with significant potential for improving outcomes and identifying patients at risk for diminished RTP outcomes.
Conclusion
Psychological factors play an important role in RTP after ACLR. Among studies evaluating the impact of psychology on RTP, there was a delay in RTP as well as lower RTP rates for patients compared with the previously reported normative literature. Fear of reinjury was the most commonly reported impediment to RTP.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: N.N.V. receives royalties from Smith & Nephew and has received consulting fees from Medacta and Smith & Nephew, educational support from Medwest, nonconsulting fees from Pacira Pharmaceuticals, and hospitality payments from Arthrex. A.A.A. has received consulting fees from Arthrex and DePuy and hospitality payments from SpineFrontier. R.J.W. has received consulting fees from Arthrex and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ardern CL, Osterberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613–1619. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40:41–48. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41:1549–1558. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43:848–856. [DOI] [PubMed] [Google Scholar]
- 6. Brewer BW, Cornelius AE, Van Raalte JL, Tennen H, Armeli S. Predictors of adherence to home rehabilitation exercises following anterior cruciate ligament reconstruction. Rehabil Psychol. 2013;58:64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40:2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christino MA, Fleming BC, Machan JT, Shalvoy RM. Psychological factors associated with anterior cruciate ligament reconstruction recovery. Orthop J Sports Med. 2016;4:2325967116638341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dean JE, Whelan JP, Meyers AW. An Incredibly Quick Way to Assess Mood States: The Incredibly Short POMS. San Antonio, Texas: Association for the Advancement of Applied Sport Psychology; 1990. [Google Scholar]
- 10. Faltstrom A, Hagglund M, Kvist J. Factors associated with playing football after anterior cruciate ligament reconstruction in female football players. Scand J Med Sci Sports. 2016;26:1343–1352. [DOI] [PubMed] [Google Scholar]
- 11. Filbay SR, Ackerman IN, Russell TG, Crossley KM. Return to sport matters: longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sports. 2017;27:514–524. [DOI] [PubMed] [Google Scholar]
- 12. Filbay SR, Crossley KM, Ackerman IN. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: a qualitative study. J Physiother. 2016;62:103–110. [DOI] [PubMed] [Google Scholar]
- 13. Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1322–1329. [DOI] [PubMed] [Google Scholar]
- 14. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14:1021–1028. [DOI] [PubMed] [Google Scholar]
- 15. Howard JS, Lembach ML, Metzler AV, Johnson DL. Rates and determinants of return to play after anterior cruciate ligament reconstruction in National Collegiate Athletic Association Division I soccer athletes: a study of the Southeastern Conference. Am J Sports Med. 2016;44:433–439. [DOI] [PubMed] [Google Scholar]
- 16. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84:1560–1572. [DOI] [PubMed] [Google Scholar]
- 17. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393–397. [DOI] [PubMed] [Google Scholar]
- 18. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377–381. [DOI] [PubMed] [Google Scholar]
- 19. Lee DY, Karim SA, Chang HC. Return to sports after anterior cruciate ligament reconstruction: a review of patients with minimum 5-year follow-up. Ann Acad Med Singapore. 2008;37:273–278. [PubMed] [Google Scholar]
- 20. Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345–353. [DOI] [PubMed] [Google Scholar]
- 21. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40:2523–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Miller RP, Kori SH, Todd DD. The Tampa Scale: a measure of kinesiophobia. Clin J Pain. 1991;7:51–52. [Google Scholar]
- 23. Muller U, Kruger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23:3623–3631. [DOI] [PubMed] [Google Scholar]
- 24. Nwachukwu BU, Anthony SG, Lin KM, Wang T, Altchek DW, Allen AA. Return to play and performance after anterior cruciate ligament reconstruction in the National Basketball Association: surgeon case series and literature review. Phys Sportsmed. 2017;45:303–308. [DOI] [PubMed] [Google Scholar]
- 25. Nwachukwu BU, Chang B, Voleti PB, et al. Preoperative Short Form Health Survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2784–2790. [DOI] [PubMed] [Google Scholar]
- 26. Nwachukwu BU, Voleti PB, Berkanish P, et al. Return to play and patient satisfaction after ACL reconstruction: study with minimum 2-year follow-up. J Bone Joint Surg Am. 2017;99:720–725. [DOI] [PubMed] [Google Scholar]
- 27. Nyland J, Cottrell B, Harreld K, Caborn DN. Self-reported outcomes after anterior cruciate ligament reconstruction: an internal health locus of control score comparison. Arthroscopy. 2006;22:1225–1232. [DOI] [PubMed] [Google Scholar]
- 28. Okoroha KR, Kadri O, Keller RA, Marshall N, Cizmic Z, Moutzouros V. Return to play after revision anterior cruciate ligament reconstruction in National Football League players. Orthop J Sports Med. 2017;5:2325967117698788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rodriguez-Roiz JM, Caballero M, Ares O, Sastre S, Lozano L, Popescu D. Return to recreational sports activity after anterior cruciate ligament reconstruction: a one- to six-year follow-up study. Arch Orthop Trauma Surg. 2015;135:1117–1122. [DOI] [PubMed] [Google Scholar]
- 30. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 31. Thomeé P, Wahrborg P, Borjesson M, Thomeé R, Eriksson BI, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports. 2006;16:181–187. [DOI] [PubMed] [Google Scholar]
- 32. Thomeé P, Wahrborg P, Borjesson M, Thomeé R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:118–127. [DOI] [PubMed] [Google Scholar]
- 33. Tjong VK, Murnaghan ML, Nyhof-Young JM, Ogilvie-Harris DJ. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. Am J Sports Med. 2014;42:336–342. [DOI] [PubMed] [Google Scholar]
- 34. Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Educ Monogr. 1978;6:160–170. [DOI] [PubMed] [Google Scholar]
- 35. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9–15. [DOI] [PubMed] [Google Scholar]
- 36. Webster KE, Feller JA, Whitehead TS, Myer GD, Merory PB. Return to sport in the younger patient with anterior cruciate ligament reconstruction. Orthop J Sports Med. 2017;5:2325967117703399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]