Abstract
Background:
The glenohumeral joint is characterized by its large degree of movement and consequently is the most susceptible joint to dislocations. There are few studies on the first episode of a shoulder dislocation in younger athletes.
Purpose:
To report the results of arthroscopic treatment for the first episode of a glenohumeral dislocation in younger athletes.
Study Design:
Case series; Level of evidence, 4.
Methods:
In this retrospective study, 53 patients younger than 40 years (N = 54 shoulders) sustained their first anterior shoulder dislocation and underwent arthroscopic surgery. Surgery was undertaken in the lateral decubitus position. Standard posterior, anteroinferior, and anterosuperior portals were used, and the number of anchors and the degree of capsular plication were individualized and based on the arthroscopic findings of each patient. The minimum follow-up was 2 years (mean, 2.31 years), and patients were evaluated with the Rowe functional score, Athletic Shoulder Outcome Rating Scale (EROE; acronym in Portuguese), and visual analog scale (VAS) for pain.
Results:
The mean EROE score was 93.8, with 98% of results being good or excellent, and the mean Rowe score was 95.0, with 98% good or excellent results. The mean VAS pain score was <1.0. The rate of recurrence of dislocations was 2%. The return-to-sports rate was 83%; patients with associated superior labral anterior-posterior (SLAP) lesions had a lower return-to-sports rate (P = .001) and lower EROE (P = .017) and Rowe (P = .019) scores.
Conclusion:
The present study showed favorable results for arthroscopic surgical treatment after the first dislocation episode in young athletes. It was an effective and safe treatment option in this population.
Keywords: shoulder dislocation, shoulder, arthroscopic surgery, athletic injuries, Bankart lesions
The glenohumeral joint is characterized by a large degree of motion and therefore is the most susceptible joint to dislocations. The incidence of glenohumeral instability is approximately 1.7 injuries for each 1000 people in the American and European population, and a traumatic cause is responsible for the vast majority of cases.20,21
More than 40% of dislocations occur in the young and active population. Several studies have shown functional deficits and dislocation recurrence after a first episode, particularly in the young population.13,15,28 Considering the high recurrence rate, need to return to sports, and development of instability arthropathy, several authors have advocated surgical treatment after the first shoulder dislocation, thus making the repair procedure more anatomic with a lower risk of recurrence.22,26,27 There is a paucity of studies with younger athletes and first-time shoulder dislocations.16,17,23,25,31
This study aimed to report the results of arthroscopic surgical treatment after a first-time shoulder dislocation in younger athletes (aged <40 years).
Methods
This was a retrospective study with data collected prospectively. It was carried out with the approval of the ethics committee of our institution, and it met the ethical standards in sports and exercise science research according to Harriss and Atkinson.10
Between July 2012 and July 2014, a total of 53 patients (54 shoulders) sustained their first anterior shoulder dislocation and underwent surgery. Of these shoulders, 47 (87%) belonged to male patients, and 7 (13%) belonged to female patients. The mean time between the first episode of a dislocation and surgery was 59 days (range, 2-360 days). The minimum follow-up was 2 years (mean, 2.31 years).
The study inclusion criteria were professional and amateur athletes, aged between 18 and 40 years, with a symptomatic, single-time anterior traumatic shoulder dislocation and imaging (magnetic resonance arthrogram) showing either an anteroinferior capsulolabral lesion or an anteroinferior capsulolabral with superior labral anterior-posterior (SLAP) 5 lesion. The physical examination consisted of a range of motion assessment and evaluation of the apprehension signal, observed in both the supine and the decubitus positions. All patients presented with a positive apprehension test finding and felt discomfort and/or an unpleasant feeling indicating the presence of a dislocation.
Exclusion criteria included patients who did not provide consent, presence of associated injuries such as a rotator cuff injury observed during surgery (not visualized on imaging), previous surgery in the same shoulder, glenoid bone loss greater than 25%, and humeral avulsion of the glenohumeral ligament.
For all study patients, the demographic and epidemiological data as well as arthroscopic findings were collected. The results were evaluated by the Rowe functional score, Athletic Shoulder Outcome Rating Scale (EROE; acronym in Portuguese),20 and visual analog scale (VAS) for pain.19,24,25,30 The EROE consists of objective criteria (range of motion; maximum, 10 points) and subjective criteria (pain, strength, stability, intensity, and sports performance; maximum, 90 points); scores are categorized as excellent (90-100), good (70-89), regular (51-69), or poor (≤50). The Rowe score consists of 3 criteria (stability, motion, and function) in which scores are categorized as excellent (90-100), good (75-89), fair (51-74), or poor (≤50). The VAS for pain was scored from 0 to 10, categorized as none (0-3), moderate/uncomfortable (4-8), and worst (9-10).
Surgical Technique
Surgery was undertaken in the lateral decubitus position under regional interscalene block and general anesthesia. All patients were examined under anesthesia according to the description of Ejnisman et al,8 observing inferior, anterior, and posterior translation.1,29 We did not close the rotator interval in any patient.
The forearm of the affected side was strapped by simple adhesive traction tape that was connected to a traction device. A weight of approximately 3 to 6 kg was applied to the traction device, depending on the size of the patient.
Standard posterior, anteroinferior (just proximal to the upper superior border of the subscapularis muscle), and anterosuperior portals were used. A small-diameter threaded cannula (5.0 mm) was inserted into the anterosuperior portal, and a large-diameter threaded cannula (8.0 mm) was placed into the anteroinferior portal. With the scope in the anterosuperior portal, the surgeon mobilized the anterior capsulolabral tissue from the anterior glenoid surface using a soft tissue mobilizer. Mobilization was conducted beyond the 6-o’clock position. Light decortication by abrading the medial wall of the glenoid was performed with an arthroscopic rasp and high-speed bur, which was inserted through the anteroinferior portal (Figures 1 and 2). Double-loaded bioabsorbable anchors (Osteoraptor with high-strength Ultrabraid suture; Smith & Nephew) were placed in the 5:30 position (at 4 and 3 o’clock considering the right side of the shoulder), and the knots were tied in a simple configuration. The number of anchors (3-4 anchors per patient) and the degree of capsular plication were individualized and based on the arthroscopic findings of each patient. Associated SLAP lesions were fixed after anteroinferior labral repair with a single double-loaded bioabsorbable anchor posterior to the biceps tendon and utilizing mattress sutures.
Figure 1.
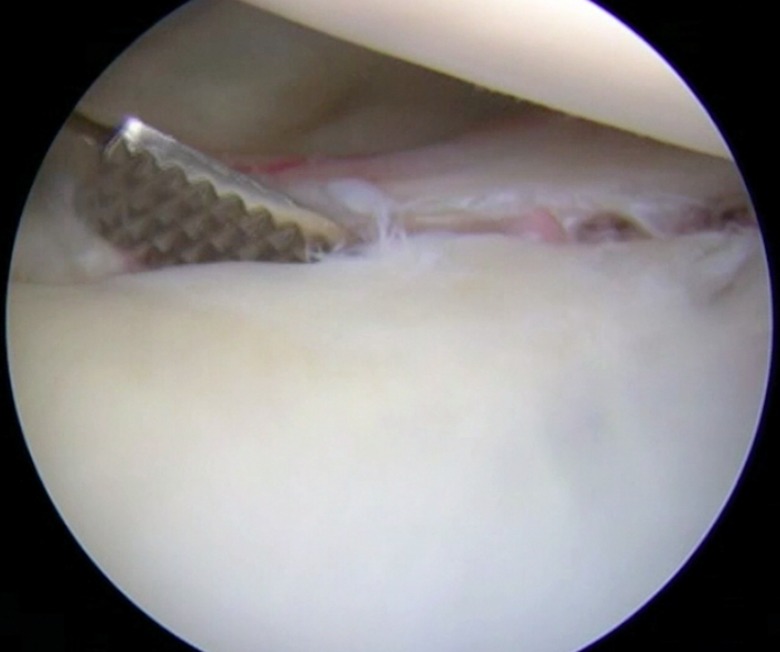
View of the posterior portal showing an anterior labral lesion.
Figure 2.
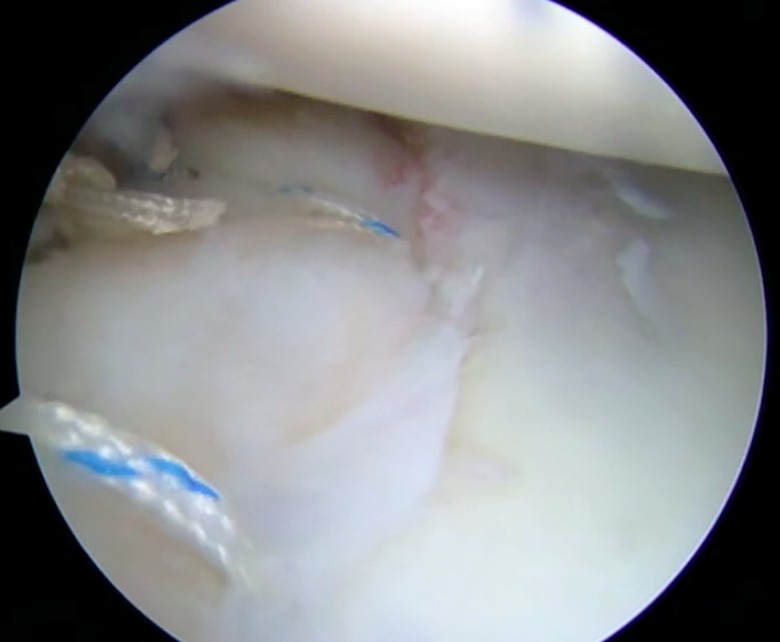
View of the anterosuperior portal showing an anteroinferior labral lesion repaired with 3 anchors.
Postoperative Protocol
Patients wore a sling full-time for 3 weeks and partially for 3 weeks. After the first 3 weeks, controlled passive movements were initiated as well as exercises of scapular control. After week 8, patients began active exercises, and after week 12, they initiated exercises of strengthening and stretching.1,27 Sporting gesture training and prelesion conditioning programs were initiated within 3 months. Athletes were permitted to return to regular practice after 5 to 6 months.
Statistical Analysis
Initially, a descriptive analysis of all variables studied was conducted. We opted for nonparametric tests because the data analyzed did not present a normal distribution, even after a transformation attempt. To identify the association between diagnoses and surgical outcomes (scores), the Fisher exact test was utilized. To make the analysis with the Fisher exact test possible, we combined the “poor” and “regular” results of the EROE as well as the “poor” and “fair” results of the Rowe score. We considered “no return to sports” a score of ≤30 on the sports performance section of the EROE.
The relationship between surgical outcomes (scores) and diagnoses, return to sports, overhead sport, and contact sport was evaluated by the nonparametric Mann-Whitney test. To verify the correlation between surgical outcomes with age and time between injury and surgery, we opted for the Spearman correlation test.
Statistical analysis was performed with SPSS (v 2.0; IBM). The level of significance utilized was alpha <.05.
Results
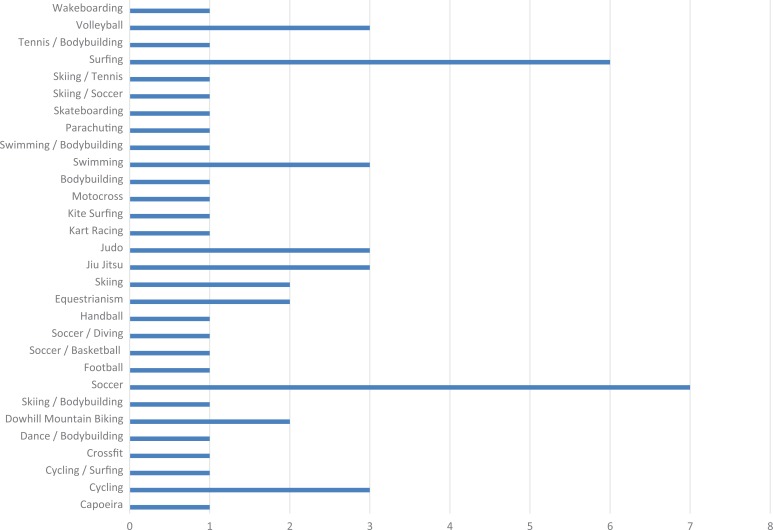
A total of 54 shoulders (53 patients), with a mean age of 30.9 years (range, 18-40 years), underwent arthroscopic labral repair with a mean follow-up of 27 months. Figure 3 presents the sports activities of the study patients.
Figure 3.
Sports activities of the study patients. Kart is a car racing mode, similar to Formula 1.
Table 1 contains a descriptive analysis of quantitative variables, and Table 2 contains descriptive information on qualitative/categorical variables. The mean EROE score was 93.8, with 98% of the results considered good or excellent. The mean Rowe score was 95.0, with a good or excellent result in 98% of patients. The mean VAS pain score was <1.0. There was no significant loss of lateral rotation in the operated patients. The mean shoulder elevation was 178°, and the mean external rotation was 82°. There was 1 case of recurrence at the final follow-up (2%). This patient developed a recurrence but refused further surgery. Four patients presented a positive apprehension sign, and 1 patient had subluxation during the examination.
TABLE 1.
Descriptive Analysis of Quantitative Variablesa
| Mean ± SD | Median (Range) | |
|---|---|---|
| Age, y | 30.89 ± 8.20 | 29 (18-40) |
| EROE score | ||
| Pain | 9.40 ± 1.19 | 10 (4-10) |
| Strength/endurance | 9.92 ± 0.35 | 10 (8-10) |
| Stability | 9.81 ± 0.59 | 10 (8-10) |
| Intensity | 9.58 ± 1.06 | 10 (6-10) |
| Sports performance | 44.53 ± 8.22 | 50 (20-50) |
| Objective (range of motion) | 9.76 ± 0.64 | 10 (8-10) |
| Total | 93.77 ± 9.01 | 99 (66-100) |
| Rowe score | ||
| Stability | 47.59 ± 7.50 | 50 (10-50) |
| Motion | 19.17 ± 2.87 | 20 (5-20) |
| Function | 28.43 ± 2.34 | 30 (25-30) |
| Total | 95.00 ± 8.18 | 100 (60-100) |
| VAS pain score | 0.74 ± 1.20 | 0 (0-6) |
| Time from injury to surgery, d | 59.56 ± 62.20 | 40 (2-360) |
aN = 54 shoulders (53 patients). EROE, Athletic Shoulder Outcome Rating Scale; VAS, visual analog scale.
TABLE 2.
Descriptive Analysis of Categorical Variablesa
| n (%) | |
|---|---|
| Sex | |
| Male | 47 (87.0) |
| Female | 7 (13.0) |
| Affected shoulder | |
| Right | 28 (51.9) |
| Left | 26 (48.1) |
| Dominant limb | |
| Right | 48 (88.9) |
| Left | 6 (11.1) |
| Activity level | |
| Amateur | 40 (74.1) |
| Competitive | 13 (25.9) |
| Contact sport | |
| No | 35 (64.8) |
| Yes | 19 (35.2) |
| Overhead sport | |
| No | 38 (70.4) |
| Yes | 16 (29.6) |
| Diagnosis | |
| Instability | 49 (90.7) |
| SLAP 5 lesion | 5 (9.3) |
| Return to sportsb | |
| No return | 9 (16.7) |
| Return | 45 (83.3) |
| EROE score | |
| Poor (≤50) | 0 (0.0) |
| Regular (51-69) | 1 (1.9) |
| Good (70-89) | 14 (25.9) |
| Excellent (90-100) | 39 (72.2) |
| Rowe score | |
| Poor (≤50) | 0 (0.0) |
| Fair (51-74) | 1 (1.9) |
| Good (75-89) | 7 (13.0) |
| Excellent (90-100) | 46 (85.2) |
| VAS pain score | |
| No pain (0-3) | 52 (96.3) |
| Moderate/uncomfortable (4-8) | 2 (3.7) |
| Worst (9-10) | 0 (0.0) |
aEROE, Athletic Shoulder Outcome Rating Scale; SLAP, superior labral anterior-posterior; VAS, visual analog scale.
bNo return to sports was considered a score of ≤30 on the sports performance section of the EROE.
The return-to-sports rate was 83%. Patients with an associated SLAP 5 lesion had a lower return-to-sports rate (P = .001), EROE score (P = .017), and Rowe score (P = .019) (Tables 3 and 4). There was no correlation between the timing of surgery and the surgical outcome: EROE score (P = .16), Rowe score (P = .13), or VAS pain score (P = .68) (Table 5).
TABLE 3.
Relationship Between Diagnoses and Categorical Variablesa
| Instability | SLAP 5 Lesion | Total | P Value | |
|---|---|---|---|---|
| EROE score | .017b | |||
| Poor | 0 (0.0) | 1 (20.0) | 1 (1.9) | |
| Good | 11 (22.4) | 3 (60.0) | 14 (25.9) | |
| Excellent | 38 (77.6) | 1 (20.0) | 39 (72.2) | |
| Rowe score | .019b | |||
| Poor | 1 (2.0) | 0 (0.0) | 1 (1.9) | |
| Good | 4 (8.2) | 3 (60.0) | 7 (13.0) | |
| Excellent | 44 (89.8) | 2 (40.0) | 46 (85.2) | |
| Return to sportsc | .001b | |||
| No return | 5 (10.2) | 4 (80.0) | 9 (16.6) | |
| Return | 44 (89.9) | 1 (20.0) | 45 (83.3) |
aData are reported as n (%). EROE, Athletic Shoulder Outcome Rating Scale; SLAP, superior labral anterior-posterior.
bP < .05 (Fisher exact test).
cNo return to sports was considered a score of ≤30 on the sports performance section of the EROE.
TABLE 4.
Relationship Between Diagnoses and Surgical Outcomesa
| Instability | SLAP 5 Lesion | P Value | |
|---|---|---|---|
| EROE score | 95.47 ± 6.90 | 78.00 ± 11.90 | ≤.001b |
| Rowe score | 95.82 ± 7.70 | 87.00 ± 9.00 | .031c |
aData are reported as mean ± SD. EROE, Athletic Shoulder Outcome Rating Scale; SLAP, superior labral anterior-posterior.
bP ≤ .001 (Mann-Whitney test).
cP ≤ .05 (Mann-Whitney test).
TABLE 5.
Relationship Between Time From Injury to Surgery and Quantitative Variablesa
| Correlation Coefficient | P Value | |
|---|---|---|
| EROE score | –0.19 | .16 |
| Rowe score | –0.20 | .13 |
| VAS pain score | 0.56 | .68 |
aEROE, Athletic Shoulder Outcome Rating Scale; VAS, visual analog scale.
The mean EROE and Rowe scores of the patients who returned to sports were significantly higher than for those who did not return to sports (Table 6). The Rowe score of patients who did not practice a contact sport was significantly higher than in the ones who did (Table 7), however this difference was not observed in patients who participated/did not participate in overhead sports. The return-to-sports rate did not show an association with the type of sport (contact: P = .704; overhead: P = .709). There was no statistically significant relationship between surgical outcomes and either age or level of sports activity.
TABLE 6.
Relationship Between Return to Sports and Surgical Outcomesa
| No Return | Return | P Value | |
|---|---|---|---|
| EROE score | 81.10 ± 11.40 | 96.60 ± 5.70 | .001b |
| Rowe score | 87.20 ± 13.00 | 96.50 ± 5.90 | .008b |
aData are reported as mean ± SD. EROE, Athletic Shoulder Outcome Rating Scale.
bP ≤ .05 (Mann-Whitney test).
TABLE 7.
Relationship Between Contact Sport and Surgical Outcomesa
| No Contact Sport | Contact Sport | P Value | |
|---|---|---|---|
| EROE score | 95.03 ± 7.80 | 91.68 ± 10.63 | .329 |
| Rowe score | 97.43 ± 4.70 | 90.53 ± 11.04 | .011b |
aData are reported as mean ± SD. EROE, Athletic Shoulder Outcome Rating Scale.
bP ≤ .05 (Mann-Whitney test).
None of the study patients had complications related to a neurological injury or deep infection. Only 1 case of a superficial infection was noted, and this patient was treated with first-generation cephalosporin for 7 days.
Discussion
We evaluated the minimum 2-year follow-up outcomes of 53 patients who underwent capsulolabral repair after a single-time shoulder dislocation. Our final Rowe and EROE scores showed good results, and we had a low recurrence rate of 2%.
Arthroscopic repair of a Bankart lesion is associated with high rates of success, with failure related to more than 5 episodes in the preoperative stage and the presence of associated bone and capsular lesions.6,7,29 Habermeyer et al9 evaluated the evolution of intra-articular lesions in 91 patients with traumatic glenohumeral instability and suggested that successive dislocation episodes progressively lead to damaged anatomic structures.32 The most frequently associated injury is periosteal detachment of the anteroinferior labrum. Detachment of the glenohumeral ligament complex occurs in the second stage. Progressive instability alters tissue structures, and in the fourth stage, degenerative processes occur with cartilage lesions and destruction of the structures of the capsulolabral complex. Burkhart and De Beer,6 in a retrospective study, showed excellent and good results in contact athletes (93.5%) after a meticulous selection of patients who underwent arthroscopic surgical procedures. They described the importance of inverted-pear glenoid lesions and engaging Hill-Sachs lesions as exclusion criteria for an arthroscopic procedure, showing that the correct identification of the type of injury and the tissue quality are keys for the success of arthroscopic treatment. In our study, we did not have patients who presented complex capsular injuries or humeral avulsion of the glenohumeral ligament, which contraindicated performing an arthroscopic procedure. We believe that good tissue quality of both the capsulolabral complex and glenohumeral ligament, as well as the absence of significant bone injuries, are some of the main contributors to the success of arthroscopic treatment.
Bacilla et al,3 in their study involving 32 athletes with recurring dislocations, demonstrated a 91% rate of return to sports, 81% of whom returned to the same or higher preinjury level. Bigliani et al4,5 reported a 92% return-to-sports rate, with 75% returning to the same level after open repair with capsular plication. The results of our study are similar to these reports, with an 83% return-to-sports rate and an EROE sports performance score of >30 (ie, at or slightly lower than performance level compared with preoperatively).
Arliani et al,2 in a literature review comparing surgical and nonsurgical treatment after the first episode of a shoulder dislocation in athletes, reported better results with surgical treatment. The same group of authors in another study, in which a literature review was conducted with conservative treatment of this injury, showed that less than 60% of the patients returned to sports and that those who were immobilized in the lateral position of the involved upper limb had better rates.28
We believe that for this specific population, the best time to treat capsulolabral lesions is after the first episode because, in this way, we will be able to achieve a more anatomic repair in a tissue that is still of good quality. The return-to-sports rate in our study was 83%, and it was lower in patients who had an associated SLAP lesion. Despite the small group of these patients (n = 5), we believe that patients with a SLAP 5 lesion had the worst functional scores and a lower return-to-sports rate because of the severity of the injury. This result was probably because a SLAP 5 is a more extensive labral lesion, involving the insertion of the long head of the biceps tendon.
Larrain et al18 reported their surgical results with arthroscopic and open surgery in 198 rugby players with recurrent episodes of glenohumeral instability. Of the 158 recurrent instability cases, 77% underwent arthroscopic stabilization, with a recurrence rate of 8.3%. Arthroscopic repair was performed in 97.5% of the acute cases, with a recurrence rate of only 5%.18 Hovelius and Rahme14 reported an 88% rate of recurrence of dislocations in hockey players younger than 20 years. In our study, 100% of the patients underwent an arthroscopic procedure, with a recurrence rate of 2%; this patient was a soccer goalkeeper who suffered a new fall, which raises doubts as to whether it was a new trauma or failure of the surgical technique. There were 4 patients who had a positive apprehension test finding and 1 patient with painless episodes of subluxation, which contributed to a VAS pain score of <1.0. In this group of patients with apprehension and subluxation, only 2 patients had a satisfactory return to sports. If we also consider as treatment failure those patients with apprehension and subluxation, our study had a failure rate of 11%.
Hovelius et al11,12,15 reported on the evolution of instability arthropathy after 25 years of follow-up and related the worst results with the largest number of dislocations. Return to sports in the athletic population depends on many factors, such as joint stability and the absence of pain. In our study, we used the EROE, which is validated for the Brazilian population and takes into consideration objective and subjective criteria such as pain, strength, stability, and degree of return to sports activities. We also observed that the time between the initial trauma and the surgery date did not influence the functional scores or the pain score for these patients with a single shoulder dislocation.
The present study has several limitations. First, this was a retrospective study that did not include a control group. Second, the mean follow-up was short (27 months). However, Hovelius et al11,15 indicated that even if a recurrence occurs after surgery, approximately 70% of them occur in the first 2 years. Rowe et al24 reported that almost 90% of recurrences occur in the first 2 years, particularly in young patients. Our patients were highly involved in sports, so we applied a specific questionnaire for this population (EROE) and measured their rate of return to sports.
Conclusion
This study showed favorable results for arthroscopic surgical treatment after a single-time shoulder dislocation in younger athletes. The procedure was an effective and safe treatment for this population. It provided good functional outcomes, a low recurrence rate, and a low rate of complications. The elapsed time from dislocation to surgery and age at the time of dislocation had no influence on functional scores.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the ethics committee of the Federal University of São Paulo.
References
- 1. Abrams JS, Savoie FH, 3rd, Tauro JC, Bradley JP. Recent advances in the evaluation and treatment of shoulder instability: anterior, posterior, and multidirectional. Arthroscopy. 2002;18(9 suppl 2):1–13. [DOI] [PubMed] [Google Scholar]
- 2. Arliani GG, Astur Dda C, Cohen C, et al. Surgical versus nonsurgical treatment in first traumatic anterior dislocation of the shoulder in athletes. Open Access J Sports Med. 2011;2:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bacilla P, Field LD, Savoie FH., 3rd Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13(1):51–60. [DOI] [PubMed] [Google Scholar]
- 4. Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25(5):609–613. [DOI] [PubMed] [Google Scholar]
- 5. Bigliani LU, Kurzweil PR, Schwartzbach CC, Wolfe IN, Flatow EL. Inferior capsular shift procedure for anterior-inferior shoulder instability in athletes. Am J Sports Med. 1994;22(5):578–584. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. [DOI] [PubMed] [Google Scholar]
- 7. Di Giacomo G, Golijanin P, Sanchez G, Provencher MT. Radiographic analysis of the Hill-Sachs lesion in anteroinferior shoulder instability after first-time dislocations. Arthroscopy. 2016;32(8):1509–1514. [DOI] [PubMed] [Google Scholar]
- 8. Ejnisman B, de Figueiredo EA, Terra BB, et al. Management of the treatment of glenohumeral instability in patients with extensive bone defect. BMJ Case Rep. 2012;2012;BCR1120115221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Habermeyer P, Gleyze P, Rickert M. Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: a prospective study. J Shoulder Elbow Surg. 1999;8(1):66–74. [DOI] [PubMed] [Google Scholar]
- 10. Harriss DJ, Atkinson G. Ethical standards in sports and exercise science research: 2016 update. Int J Sports Med. 2015;36:1121–1124. [DOI] [PubMed] [Google Scholar]
- 11. Hovelius L. The natural history of primary anterior dislocation of the shoulder in the young. J Orthop Sci. 1999;4(4):307–317. [DOI] [PubMed] [Google Scholar]
- 12. Hovelius L. Shoulder dislocation in Swedish ice hockey players. Am J Sports Med. 1978;6(6):373–377. [DOI] [PubMed] [Google Scholar]
- 13. Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am. 1996;78(11):1677–1684. [DOI] [PubMed] [Google Scholar]
- 14. Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):330–342. [DOI] [PubMed] [Google Scholar]
- 15. Hovelius L, Saeboe M. Neer Award 2008. Arthropathy after primary anterior shoulder dislocation: 223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg. 2009;18(3):339–347. [DOI] [PubMed] [Google Scholar]
- 16. Ide J, Maeda S, Takagi K. Arthroscopic Bankart repair using suture anchors in athletes: patient selection and postoperative sports activity. Am J Sports Med. 2004;32(8):1899–1905. [DOI] [PubMed] [Google Scholar]
- 17. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507–514. [DOI] [PubMed] [Google Scholar]
- 18. Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavon F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22(12):1283–1289. [DOI] [PubMed] [Google Scholar]
- 19. Leme L, Saccol M, Barbosa L, Ejnisman B, Faloppa F, Cohen M. Translation, cultural adaptation, and validation of the Athletic Shoulder Outcome Rating Scale into Portuguese [in Portuguese]. Rev Bras Med. 2010;67:29–38. [Google Scholar]
- 20. Miyazaki AN, Fregoneze M, Santos PD, et al. Evaluation of the results from arthroscopic surgical treatment for traumatic anterior shoulder instability using suturing of the lesion at the opened margin of the glenoid cavity. Rev Bras Ortop. 2012;47(3):318–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Provencher MT, Bhatia S, Ghodadra NS, et al. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92(suppl 2):133–151. [DOI] [PubMed] [Google Scholar]
- 22. Robinson CM, Jenkins PJ, White TO, Ker A, Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, double-blind trial. J Bone Joint Surg Am. 2008;90(4):708–721. [DOI] [PubMed] [Google Scholar]
- 23. Rowe CR. The surgical management of recurrent anterior dislocations of the shoulder using a modified Bankart procedure. Surg Clin North Am. 1963;43:1663–1666. [DOI] [PubMed] [Google Scholar]
- 24. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- 25. Rowe CR, Sakellarides HT. Factors related to recurrences of anterior dislocations of the shoulder. Clin Orthop Relat Res. 1961;20:40–48. [PubMed] [Google Scholar]
- 26. Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–460. [PubMed] [Google Scholar]
- 27. Savoie FH, 3rd, O’Brien MJ. Anterior instability in the throwing shoulder. Sports Med Arthrosc. 2014;22(2):117–179. [DOI] [PubMed] [Google Scholar]
- 28. Soliaman RR, Cunha RA, Pocchini Ade C, Andreoli CV, Ejnisman B, Cohen M. Less than 60% return to preinjury sports activities after primary anterior shoulder dislocation treated with immobilisation only. J ISAKOS. 2016;1:198–201. [Google Scholar]
- 29. Terra BB, Ejnisman B, Figueiredo EA, et al. Arthroscopic treatment of glenohumeral instability in soccer goalkeepers. Int J Sports Med. 2013;34(6):473–476. [DOI] [PubMed] [Google Scholar]
- 30. Tibone JE, Bradley JP. Evaluation of treatment outcomes for the athlete’s shoulder In: Matsen FA III, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, Illinois: American Academy of Orthopaedic Surgeons; 1993:519–529. [Google Scholar]
- 31. Uhring J, Rey PB, Rochet S, Obert L. Interest of emergency arthroscopic stabilization in primary shoulder dislocation in young athletes. Orthop Traumatol Surg Res. 2014;100:S401–S408. [DOI] [PubMed] [Google Scholar]
- 32. Werner AW, Lichtenberg S, Schmitz H, Nikolic A, Habermeyer P. Arthroscopic findings in atraumatic shoulder instability. Arthroscopy. 2004;20(3):268–272. [DOI] [PubMed] [Google Scholar]