Abstract
Background:
Double-row transosseous-equivalent (TOE) rotator cuff repair techniques have been widely accepted because of their superior biomechanical properties when compared with arthroscopic single-row repair. Concerns regarding repair overtensioning with medial-row knot tying have led to increased interest in knotless repair techniques; however, there is a paucity of clinical data to guide the choice of technique.
Hypothesis:
Arthroscopic TOE repair techniques using knotless medial-row fixation will demonstrate lower retear rates and greater improvements in the Constant score relative to conventional knot-tying TOE techniques.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of 3 databases (PubMed, Cochrane, and Embase) was performed using PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines. Inclusion criteria were English-language studies that examined repair integrity or Constant scores after arthroscopic rotator cuff repair with TOE techniques. Two investigators independently screened results for relevant articles. Data regarding the study design, surgical technique, retear rate, and Constant shoulder score were extracted from eligible studies. A quality assessment of all articles was performed using the Methodological Index for Non-Randomized Studies (MINORS) criteria.
Results:
The systematic review identified a total of 32 studies (level of evidence, 1-4) that met inclusion and exclusion criteria. Of the 32 studies, 5 reported on knotless TOE techniques, 25 reported on knot-tying TOE techniques, and 2 reported on both. In the knotless group, retear rates ranged from 6% to 36%, and Constant scores ranged from 38-65 (preoperative) to 73-83 (postoperative). In the knot-tying group, retear rates ranged from 0% to 48%, and Constant scores ranged from 42-64 (preoperative) to 55-96 (postoperative).
Conclusion:
Despite several theoretical advantages of knotless TOE repair, both knotless and knot-tying techniques reported considerable improvement in functional outcomes after rotator cuff repair. Although tendon failure rates showed a downward trend in knotless studies, additional prospective studies are warranted to better understand the role of medial-row fixation on tendon repair integrity and postoperative clinical outcomes.
Keywords: knot, knotless, arthroscopic, shoulder, surgical techniques, systematic review, meta-analysis
Despite significant advances and numerous improvements in arthroscopic rotator cuff repair techniques, a tendon retear remains a very common postoperative complication.3,19,21,42 Many factors, including a patient’s overall health and tendon quality, have been implicated in rotator cuff healing.4,38,65 Additionally, nonbiological factors such as suture repair technique have also been shown to affect the biomechanical properties of the repair construct and eventual clinical outcomes.16,31 Regardless of the method, current techniques aim to restore the anatomic configuration and provide an optimal environment for tendon-to-bone healing. While several techniques, including single-row and double-row anchor-based repair, have been described with good clinical outcomes, recent studies have demonstrated that transosseous-equivalent (TOE) techniques optimize footprint contact while maintaining high initial fixation and minimizing gap formation.16,31,34,35,39,51 TOE repair has also been shown to be superior to other methods in achieving tendon compression for healing and a higher ultimate load to failure.13,20,59
TOE repair can be performed using various configurations but generally can be divided into all-knotless repair or repair in which the medial or lateral row is tied.13,59 A recent systematic review noted that biomechanical properties, including ultimate load, stiffness, gap formation, and contact area, are significantly improved when medial knots are tied compared with knotless TOE constructs.41 Despite the biomechanical advantages of medial knots in TOE repair, controversy still remains regarding the clinical significance of tying the medial row. Recent investigations have reported medial-row failure with knot-tying TOE repair as a result of tension overload or decreased tendon perfusion due to medial stress.8,9,14,23,67,74 Blood supply to the rotator cuff tendon is critical to the healing process, and tendon perfusion is an important variable to consider when evaluating a suture technique.12,28,37,75 All-knotless repair has gained interest because of its improved vascularity and decreased risk of tissue strangulation and overtensioning.9,37 By eliminating the burden of a subacromial knot, knotless techniques also decrease irritation and the risk of impingement on the repair site. The advantages of this technique allow surgeons to achieve anatomic footprint restoration without compromising tissue circulation and decreasing the risk of tissue cut-through.18 Additionally, a recent study showed superior biomechanics of knotless TOE repair over knotted TOE repair via an improved self-reinforcement mechanism.50
Although the superior biomechanical characteristics of TOE constructs have been recognized, fewer studies have evaluated clinical healing rates and functional outcomes of these techniques. Studies have reported inconsistent results of repair site integrity with knot-tying TOE repair, with retear rates ranging from 12% to 30% in some reports.18,70 An even fewer number of published studies have reported outcomes after knotless repair, but small case series have reported failure rates as low as 6%.56 Given such limited existing clinical data, the purpose of this systematic review was to compare the outcomes of knot-tying with knotless medial-row anchors in TOE constructs to provide better guidance regarding the use of both techniques. We hypothesized that tying the medial row in TOE constructs would lead to higher failure rates and less clinical improvement as measured by the Constant score.
Methods
Search Strategy
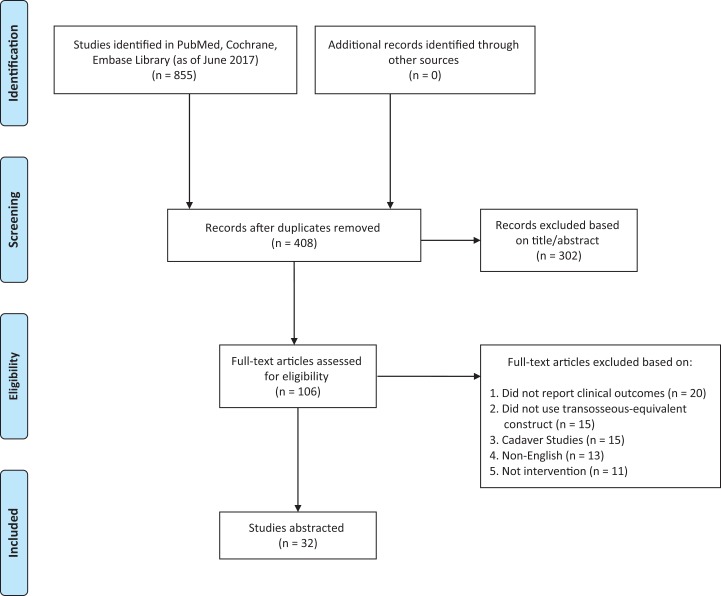
A systematic literature search was performed in accordance with the 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement (Figure 1). Two reviewers (A.M.E., N.L.R.) independently searched 3 online databases (PubMed, Cochrane, Embase) to identify all relevant articles published before June 2017. Reference lists of included studies and relevant reviews were examined for supplementary eligible studies. The search terms and inclusion/exclusion criteria were established a priori (Appendix Table A1). Key terms used in the search were “rotator cuff,” “repair,” “double row,” “suture bridge,” “speedbridge,” “knot tying,” “knotless,” and “transosseous equivalent.” Eligible studies were included based on the following criteria: (1) level of evidence 1 to 4, (2) articles published in the English language, (3) human studies, (4) arthroscopic rotator cuff repair, (5) studies reporting repair failure rates or Constant scores, and (6) full-text availability. Exclusion criteria were (1) basic science articles, (2) studies on rotator cuff repair associated with shoulder arthroplasty or trauma, and (3) potential overlap of patient populations when the study was conducted by the same authors or institutions.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart of systematic search strategy.
Data Extraction
Two reviewers (A.M.E., N.L.R.) independently screened all titles, abstracts, and full texts of retrieved studies to determine eligibility. Disagreements were resolved by a discussion between the 2 authors, and if a consensus could not be reached, the senior reviewer (K.J.J.) resolved the discrepancy. The final decision on inclusion was made on the basis of the full-text article. Included studies were used to extract relevant data, including author, year of publication, sample size, study design, level of evidence, mean follow-up, surgical procedure (ie, knotless vs knot tying), initial tear size, preoperative fatty infiltration, repair integrity via the Sugaya classification,64 failure rate, location of rotator cuff failure according to Cho et al,9 and preoperative and postoperative Constant scores.
Literature Quality Evaluation
The MINORS (Methodological Index for Non-Randomized Studies) criteria were used for grading the methodological quality of selected studies. The MINORS is a validated scoring tool to assess internal and external validity for nonrandomized studies.63 Studies are assigned 0, 1, or 2, with a maximum of 24 for comparative studies and 16 for noncomparative studies. Although each included constituent study was scored, studies were not excluded from the systematic review on the basis of their MINORS score.
Qualitative Analysis
Because of the overall variation in study design (evidence levels 1-4) and outcome heterogeneity, a quantitative meta-analysis was deemed inappropriate. Therefore, a qualitative analysis was performed.
Results
Studies Included
Our initial search strategy yielded 855 studies. After the removal of 447 duplicates, the individual titles and abstracts of the remaining 408 articles were reviewed and resulted in the exclusion of 302 articles that were not relevant to our study. The full text of the remaining 106 articles was thoroughly reviewed for eligibility, and 74 were eliminated on the basis of inclusion and exclusion criteria. No other studies were extracted from the reference lists of these studies (Figure 1). The reasons for exclusion were as follows: study did not report failure rates or clinical outcome scores (31%), study did not use a TOE construct (22%), cadaveric or biomechanical studies (21%), non-English language (18%), and case reports (8%). The 32 included articles identified by the 2 independent reviewers were then evaluated by the senior reviewers to ensure that the strict eligibility criteria had been met.
Study Quality
Of the 32 studies that were included, 1 study represented level 1 evidence, 5 studies represented level 2 evidence, 17 studies represented level 3 evidence, and 9 studies represented level 4 evidence. Noncomparative studies had a mean MINORS score of 13.3, and comparative studies had a mean MINORS score of 20.9, indicating moderate quality of evidence (Appendix Table A2). A summary of the included studies is shown in Table 1.
TABLE 1.
Included Studiesa
| Author (Year) | Study Design | LOE | Follow-up, Mean ± SD, mo | No. of Patients | Initial Rotator Cuff Tear Size,b cm | Degree of Fatty Infiltrationc | Repair Integrity via Sugaya Classification | Retears, n (%) | Location of Rotator Cuff Failure, Type 1/Type 2 | Imaging Modalityd | Time From Surgery to Imaging, mo |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Knotless TOE | |||||||||||
| Boyer et al5 (2015) | Pro | 3 | 21 | 35 | 13 B1, 17 B2, 5 B3 | ≤G1 | Y | 6 (17) | 6/0 | MRI, CT | 13 |
| Ide et al26 (2015) | Retro | 3 | 81 | 36 | 2.1 ± 0.9 (1.0-3.5) | ≤G2 | — | 5 (14) | — | MRI | 12.8 |
| Hug et al25 (2015) | Retro | 3 | 24.4 ± 4.7 | 22 | 1-5 | 1.40 ± 0.34 | Y | 5 (23) | 3/2 | MRI | 24.4 |
| Kim et al30 (2014) | Retro | 3 | 6.21 | 61 | 1-4 | — | Y | 22 (36) | 12/9e | MRI | 6.2 |
| Werthel et al73 (2014) | Retro | 3 | 19.0 ± 4.2 | 32 | 14 B1, 17 B2, 1 B3 | ≤G2 | Y | 2 (6) | — | MRI | 19 |
| Rhee et al57 (2012) | Pro | 2 | 21.2 | 51 | 1-3 | G0-G4 | — | 3 (6) | — | MRI | 6.8 |
| El-Azab et al17 (2010) | Pro | 2 | 14 | 20 | — | G1-G3 | — | 4 (20) | — | MRI | 14 |
| Knot-tying TOE | |||||||||||
| Boyer et al5 (2015) | Pro | 3 | 29 | 38 | 12 B1, 22 B2, 4 B3 | ≤G1 | Y | 9 (24) | 7/2 | MRI, CT | 13 |
| Shin et al61 (2015) | Retro | 3 | 34.1 ± 8.9 | 37 | 1.67 ± 0.42 | — | — | 3 (8) | — | MRI | 6 |
| Wang et al72 (2015) | RCT | 1 | 4 | 30 | 13.70 ± 3.27 | — | Y | 9 (30) | — | MRI | 4 |
| Choi et al11 (2014) | Retro | 3 | 31.2 | 147 | 94 (63.9%) D2, 38 (25.9%) D3, 15 (10.2%) D4 | G0-G4 | Y | 25 (17) | 5/20 | MRI | 23.4 |
| Hug et al25 (2015) | Retro | 3 | 24.4 ± 4.7 | 20 | 1-5 | — | Y | 5 (25) | 1/4 | MRI | 24.4 |
| Kim et al31 (2014)f | Retro | 3 | 36 | 21 | — | — | — | 2 (10) | — | US, MRI | 32.4 |
| Kim et al31 (2014)f | Retro | 3 | 35.3 | 16 | — | — | — | 0 (0) | — | US, MRI | 21.9 |
| McCormick et al44 (2014) | Retro | 3 | 48 | 19 | 3.30 ± 0.74 | ≤G2 | Y | 2 (11) | — | MRI | 48.8 |
| Park et al47 (2014)g | Retro | 3 | 24 | 42 | 3.87 ± 0.64 | 1.6 ± 0.7 | — | 8 (19) | 4/4 | US | 24 |
| Park et al47 (2014)g | Retro | 3 | 24 | 53 | 3.44 ± 0.52 | 0.8 ± 0.7 | — | 9 (17) | 2/7 | US | 24 |
| Park et al53 (2014) | Retro | 3 | 5.7 | 103 | 1-5 | — | — | 7 (7) | — | MRI | 6 |
| Ryu et al58 (2015) | Pro | 2 | 58 | 34 | 2.91 ± 1.46 | 0.69 ± 0.40 | Y | 8 (24) | — | MRI | 8.2 |
| Anakwenze et al1 (2013) | Retro | 3 | 13.3 | 69 | 3-5 | ≤G2 | — | 4 (6) | — | — | N/A |
| Haneveld et al24 (2013) | Retro | 3 | 28.4 ± 8.9 | 36 | 1-5 | — | Y | 13 (36) | — | MRI | 28.4 |
| Kim et al29 (2013) | Pro | 2 | 31 | 26 | 2.15 (1.2-4.0) | — | Y | 3 (12) | 2/1 | US, MRI | 27.9 |
| Kim et al33 (2013) | Pro | 2 | 26.6 | 32 | >3 | 0.97 ± 0.48 | Y | 2 (6) | — | MRI | 26.6 |
| Lee et al36 (2013) | Retro | 3 | 27.4 | 62 | 11 D1, 47 D2, 4 D3 | 0.73 ± 0.57 | Y | 30 (48) | — | MRI | 27.4 |
| Neyton et al46 (2013) | CS | 4 | 16.1 | 107 | <3 | ≤G2 | Y | 11 (10) | 10/1 | MRI | 16.1 |
| Park et al48 (2013) | Retro | 3 | 25.1 | 119 | 68 D2, 51 D3 | — | — | — | — | — | N/A |
| Park et al49 (2013) | CS | 4 | 37.6 ± 8.9 | 36 | >5 | 1.3 ± 0.6 (0.3-2.7) | — | 9 (25) | — | US | 24 |
| Tudisco et al68 (2013) | Retro | 3 | 38.9 ± 2.3 | 20 | 1-3 | — | — | 5 (25) | 0/5 | MRI | 38.9 |
| Choi et al10 (2012) | CS | 4 | 28 | 41 | 3 D1, 23 D2, 11 D3, 4 D4 | 33 G1-G2, 6 G3-G4 | — | 8 (20) | 5/3 | US | 28 |
| Gerhardt et al23 (2012) | Retro | 3 | 23.4 ± 2.9 | 20 | 16 (80%) B2, 4 (20%) B3 | 1.15 ± 0.50 | Y | 5 (25) | — | MRI | 23.4 |
| Cho et al8 (2011) | CS | 4 | 25.2 | 87 | 7 (8%) D1, 41 (47%) D2, 32 (37%) D3, 7 (8%) D4 | G0-G4 | — | 29 (33) | 12/17 | MRI | 8.5 |
| Mihata et al45 (2011) | Retro | 3 | 38.5 | 107 | 67 D1-D2 (1.8 ± 0.5), 40 D3-D4 (4.2 ± 1.2) | G0-G4 | Y | 5 (5) | — | MRI | 32.9 |
| Toussaint et al66 (2011) | CS | 4 | 15 | 154 | 47 (30.3%) P1, 88 (57.4%) P2, 19 (12.3%) P3 | ≤G2 | — | 22 (14) | — | MRI, CT | 15 |
| Park et al50 (2010) | CS | 4 | 12 | 78 | 11 D1, 32 D2, 18 D3, 17 D4 | G0-G4 | — | 7 (9) | — | US | 12 |
| Pennington et al55 (2010) | Retro | 3 | 24 | 37 | 3.40 ± 0.95 | — | Y | 12 (32) | — | MRI | 21 |
| Sethi et al60 (2010) | CS | 4 | 16.1 | 40 | 2.9 (2.5-5.1) | 0.45 ± 0.66 | — | 7 (18) | — | MRI | 16.1 |
| Voigt et al70 (2010) | CS | 4 | 24 | 45 | — | G0-G4 | Y | 13 (29) | 7/6 | MRI | 12 |
| Frank et al18 (2008) | CS | 4 | 14.6 | 25 | — | G0-G4 | — | 3 (12) | — | MRI | 14.6 |
aDashes indicate data not reported. CS, case series; CT, computed tomography; LOE, level of evidence; MRI, magnetic resonance imaging; N/A, not applicable; Pro, prospective study; RCT, randomized controlled trial; Retro, retrospective study; TOE, transosseous-equivalent; US, ultrasound; Y, yes.
bInitial rotator cuff tear size in the anteroposterior dimension, reported as No., mean ± SD (range), range, mean ± SD, n (%), mean (range), or mean. B, Bateman classification2 (grade 1 [B1]: <1 cm; grade 2 [B2]: 1-3 cm; grade 3 [B3]: 3-5 cm); D, DeOrio and Cofield classification15 (small [D1]: <1 cm; medium [D2]: 1-3 cm; large [D3]: 3-5 cm; massive [D4]: >5 cm); P, Patte classification54 (type 1 [P1]: “small tears” or retraction of the tendon to the articular surface margin on the humerus; type 2 [P2]: “large tears” or retraction of the tendon between the articular margin of the humerus to the glenoid; type 3 [P3]: “massive tears” or retraction of the tendon to the glenoid or more medial).
c Degree of fatty infiltration, as defined by the 5-stage Goutallier Classification49 (G0, no fatty deposits; G1, some fatty streaks; G2, more muscle than fat; G3, as much muscle as fat; and G4, muscle < fat), or reported as global fatty degeneration index mean ±SD, which is the mean value of 3 muscles’ (supraspinatus, infraspinatus, and subscapularis) degree of fatty infiltration.49
dWhen 2 imaging modalities were indicated, the primary modality is listed first.
e1/22 was unable to be classified.
fKim et al31 (2014) listed twice to differentiate between 21 patients with bursal-side lesions and 16 patients with articular-side lesions.
gPark et al47 (2014) listed twice to differentiate between 42 patients with U-shaped tears and 53 patients with L-shaped tears.
Study Characteristics
The 32 studies included in the systematic review were published between 2008 and 2015 (Table 1). Of those studies, 7 utilized a knotless TOE construct in a total of 257 patients, and 27 studies utilized a knot-tying TOE construct in a total of 1701 patients. A total of 29 studies documented initial tear size, either with mean tear size, range of tear sizes, or DeOrio and Cofield classification15 or Bateman classification,2 and 1 study classified size according to Patte.54 A total of 24 studies evaluated patients’ preoperative rotator cuff fatty infiltration, and 33 studies (n = 1839 patients) evaluated patients for full-thickness retears at or before final follow-up. The mean follow-up was 26.7 and 27.6 months in the knotless and knot-tying groups, respectively. Overall, 17 studies evaluated repair integrity via magnetic resonance imaging (MRI) according to the Sugaya classification, in which Sugaya types 1 and 2 (intact repair) and Sugaya types 4 and 5 (not intact repair) were interpreted universally across all studies.64 The interpretation of Sugaya type 3, however, was not uniform across studies regarding the integrity of rotator cuff repair. A total of 11 studies specified the location of retears according to Cho et al,9 with type 1 retears located at the tendon-bone interface (original repair site) and type 2 retears located medially with the original repair intact. We found 24 studies (n = 1432 patients) that reported preoperative and postoperative Constant scores (Table 2).
TABLE 2.
Constant Scoresa
| Author (Year) | Preoperative | Postoperative |
|---|---|---|
| Knotless TOE | ||
| Boyer et al5 (2015) | 49.7 ± 13.2 | 82.6 ± 8.3 |
| Ide et al26 (2015) | — | — |
| Hug et al25 (2015) | — | 78.2 ± 13.2 |
| Kim et al30 (2014) | — | — |
| Werthel et al73 (2014) | 38 ± 11 | 73 ± 11 |
| Rhee et al57 (2012) | 65.2 | 79.1 |
| El-Azab et al17 (2010) | 46 ± 26 | 80 ± 16 |
| Knot-tying TOE | ||
| Boyer et al5 (2015) | 48.2 ± 13.9 | 81.3 ± 9.9 |
| Shin et al61 (2015) | 62.8 ± 2.4 | 89.4 ± 1.8 |
| Wang et al72 (2015) | — | — |
| Choi et al11 (2014) | 53.3 | 84.3 |
| Hug et al25 (2015) | — | 77.0 ± 8.6 |
| Kim et al31 (2014)b | 51.0 ± 20.5 | 75.9 ± 10.6 |
| Kim et al31 (2014)b | 57.4 ± 18.0 | 83.0 ± 11.8 |
| McCormick et al44 (2014) | — | 76.0 ± 16.9 |
| Park et al47 (2014)c | 50.9 ± 12.2 | 75.8 ± 12.2 |
| Park et al47 (2014)c | 52.4 ± 11.5 | 77.6 ± 10.8 |
| Park et al53 (2014) | 50.5 ± 14.0 | 55.3 ± 11.4 |
| Ryu et al58 (2015) | 53.8 ± 15.9 | 73.4 ± 10.3 |
| Anakwenze et al1 (2013) | — | — |
| Haneveld et al24 (2013) | — | — |
| Kim et al29 (2013) | 58.6 ± 17.7 | 75.4 ± 10.9 |
| Kim et al33 (2013) | — | — |
| Lee et al36 (2013) | 63.6 | 74.9 |
| Neyton et al46 (2013) | 54.5 ± 12.5 | 80.0 ± 12.1 |
| Park et al48 (2013) | 48.8 ± 12.3 | 76.9 ± 7.0 |
| Park et al49 (2013) | 44.8 ± 12.3 | 75.3 ± 9.9 |
| Tudisco et al68 (2013) | 42 ± 12 | 67 ± 15 |
| Choi et al10 (2012) | 58 | 91 |
| Gerhardt et al23 (2012) | — | 77.0 ± 8.6 |
| Cho et al8 (2011) | 48.0 | 80.3 |
| Mihata et al45 (2011) | — | — |
| Toussaint et al66 (2011) | 44.4 ± 8.9 | 80.5 ± 9.3 |
| Park et al50 (2010) | — | — |
| Pennington et al55 (2010) | — | — |
| Sethi et al60 (2010) | — | — |
| Voigt et al70 (2010) | 64 | 96 |
| Frank et al18 (2008) | — | 84.3 |
aData are reported as mean or mean ± SD. Dashes indicate data not reported. TOE, transosseous-equivalent.
bKim et al31 (2014) listed twice to differentiate between 21 patients with bursal-side lesions and 16 patients with articular-side lesions.
cPark et al47 (2014) listed twice to differentiate between 42 patients with U-shaped tears and 53 patients with L-shaped tears.
Failure Rates and Clinical Outcomes
Rotator cuff healing and repair integrity can be assessed using various imaging modalities, including ultrasound, MRI, or computed tomography (CT) arthrography. Imaging modalities used among the studies were as follows: MRI (78%), ultrasound (17%), and CT arthrography (5%). Several studies used both ultrasound and MRI depending on patient preference and ability to pay. When 2 imaging modalities were used in a study, the one that was used primarily is listed first in Table 1. Time from surgery to imaging varied among studies, with some performing imaging at mean final follow-up and others at shorter intervals (Table 1). When analyzed by surgical technique, the knotless studies reported a retear rate ranging from 6% to 36%. In comparison, the retear rate in the knot-tying group ranged from 0% to 48% (Table 1).
The preoperative and postoperative Constant scores for both repair techniques were used to determine functional improvement at final follow-up. All included studies reported an increase in the mean preoperative to postoperative Constant score. The knotless studies reported a preoperative Constant score ranging from 38 to 65 and a postoperative range from 73 to 83. The preoperative Constant score range in the knot-tying group was from 42 to 64, and postoperative scores ranged from 55 to 96 (Table 2).
Discussion
Although prior evidence has shown improved biomechanics and a lower risk for medial retears in all-knotless repair, the results of this study do not support our initial hypothesis that clinical results of knotless repair demonstrate superiority over knot-tying repair. Our study found that both TOE techniques demonstrated a considerable increase in the Constant score from baseline to 2 years postoperatively. Prior studies, however, have shown that postoperative clinical outcomes do not necessarily correlate with rotator cuff retears. Our study did support a narrower range of retear rates in knotless studies (6%-36%) compared with knot-tying studies (0%-48%). As studies with evidence levels 3 to 4 were primarily analyzed in this systematic review, we were unable to provide any direct quantitative comparison of technique outcomes.
The ideal rotator cuff repair should allow for easy and quick arthroscopic application while still achieving adequate biomechanical stability to facilitate tendon-to-bone contact and eventual healing.22,43 The development of knot-tying TOE repair has provided a more anatomic configuration of the rotator cuff footprint, but recent evidence has suggested concerns of overtensioning of tissue and potential strangulation with medial knots, which has been shown to impede blood flow and long-term healing.12,32,37 The importance of structurally healed rotator cuffs has also been shown to affect clinical outcomes, which can affect patient satisfaction after the procedure.62 Despite the technical improvements and mechanical advantages of knot-tying TOE repair, it must be weighed against the importance of optimizing the healing environment and long-term tissue quality. In turn, arthroscopic rotator cuff repair utilizing knotless suture anchor fixation has become increasingly popular. Knotless repair allows for a technically facile and reliable operative procedure. In addition to the theoretical benefits of efficient suture limb management and the monetary and patient-derived benefits from reduced operative time, knotless repair allows surgeons to achieve compression and mechanical stability without reducing perfusion to the tendon.32 A biomechanical study by Burkhart et al7 found that knotless repair had yield load, ultimate load, and cyclic displacement that were statistically equivalent to classic double-row repair.
Given the potential decrease in tendon perfusion with knot-tying TOE repair, we hypothesized that eliminating medial knot impingements with knotless techniques could reduce medial strangulation and perforation, thereby leading to fewer repair failures. Studies have associated blood flow with healing and structural integrity of the rotator cuff, which has been shown to affect postoperative clinical results.62 Although knot tying the medial row increases the biomechanical properties of the TOE construct, Park et al52 revealed that medial knots inhibit self-reinforcement and adversely affect rotator cuff biomechanics, potentially leading to increased rotator cuff failure; however, their study did not specifically investigate clinical outcomes. Furthermore, an in vivo human study using laser Doppler flowmetry found a nearly 50% reduction in tendon blood flow after lateral anchor fixation.12 Considering the relative impact of blood supply on tendon healing, the Christoforetti et al12 study indicated that a decrease in intratendinous blood flow from this construct could result in worse outcomes for tissue repair. A recent study by Kim et al32 used indocyanine green fluorescence to assess the perfusion status of the compressed tendon with the knot-tying TOE construct compared with parallel-type transosseous repair in rabbits. Their study showed that knot tying hindered blood supply to the tendon in the compressed region near the tuberosity. The authors reported that medial-row failure of the construct may be related to interruption in the blood supply caused by overcompression in the closed-circuit configuration.
Biomechanical studies have also examined the mechanical integrity of anchor fixation on the rotator cuff. A study by Mazzocca et al43 reported that cyclic loading of double-row repair resulted in failure of the medial row first, with tension overload causing mattress sutures to pull through the tendon medial to the repair site. Although medial knots increase initial fixation strength, studies have shown that repeated loading over time can lead to loosening or slippage of the knot and eventual gap formation.13,40 Rhee et al57 reported no retears with the knotless technique, but nearly 75% of retears for the knot-tying TOE group occurred at the medial row. Furthermore, although limited by their number of patients, Hug et al25 reported that the pattern of retears was medial rotator cuff failure in 4 of 5 cases for knot-tying repair and only 2 of 5 cases for knotless TOE repair. Therefore, medial rotator cuff failure has been shown to have a higher tendency after knot-tying TOE repair. Each of these studies raises the concern of medial strangulation and ultimate failure as a result of knot tying the medial row. However, even with similar failure rates among TOE techniques, the knotless application still allows for a relatively easier and more efficient procedure, resulting in a decreased length of surgery.6,56,69,71
Our study also analyzed clinical differences using the Constant score, a measure of function of the shoulder. Studies have shown that functional assessment scores can often be correlated with postoperative repair integrity, in which superior results have been reported in patients with intact repair.27 Given these findings, we hypothesized lower Constant scores for knot-tying TOE repair based on the effect of strangulation and overtensioning on rotator cuff integrity. However, we found that both groups showed considerable improvement from preoperative to 2-year postoperative Constant scores. These results were also supported by Hug et al,25 who evaluated the clinical and radiological results of the knotless anchor technique in 22 patients. Despite finding a reduction in the frequency of medial rotator cuff failure compared with knot-tying TOE repair, they reported no significant difference in the Constant score, subjective shoulder value (SSV), or Western Ontario Rotator Cuff Index (WORC) between the groups.25 This highlights the possibility that postoperative clinical outcomes do not necessarily correlate with rotator cuff retears. In the study by Rhee et al,57 the authors found a statistically significant improvement in clinical assessments within the knotless group using the Constant and University of California, Los Angeles (UCLA) scores. However, the difference between the knotless and knot-tying groups was nonsignificant. After a minimum follow-up of 12 months, Boyer et al5 showed that the Constant score significantly improved in the postoperative period in both groups, but there was no statistical difference between groups. Their study reported no significant difference in retear rates between the knot-tying (24%) and knotless groups (17%).5
A review of the literature supports our findings that both TOE repair techniques achieve successful functional outcomes, but longer follow-up studies are needed to confirm these results and the role of knot tying in medial rotator cuff failure. The main strength of this study was our ability to identify a substantial number of overall patients by using an extensive search strategy with broad inclusion criteria to capture all related literature. However, there are several limitations in our study. First, our analysis is limited by the paucity of clinical outcome data regarding the newer knotless technique. Second, the majority of studies included in our analysis were observational, which further reduces the quality of evidence provided by our conclusions. Third, our analysis could not control for potentially confounding variables such as tear size and tissue quality, which could have affected both the choice of surgical technique and the postoperative outcomes. Last, the lack of a standardized imaging protocol to evaluate repair integrity in the constituent studies could possibly have led to variations in the reporting of rotator cuff failure.
Conclusion
This study supports previous literature that both knotless and knot-tying TOE techniques improve functional outcomes after rotator cuff repair. Although medial fixation has been shown as a mechanism of tendon failure, there is not sufficient evidence to support that knot-tying techniques contribute to medial-row failure of rotator cuff repair. Future studies should focus on conducting more robust comparative studies to improve our understanding of the medial row as a mode of rotator cuff failure. Further clinical and biomechanical research is needed to determine the optimal suture technique for long-term repair integrity.
Appendix
TABLE A1.
Search Criteriaa
| 1. Double-row rotator cuff repair 2. Rotator cuff suture bridge 3. Rotator cuff speed bridge 4. Rotator cuff knot tying 5. Rotator cuff knotless 6. Transosseous-equivalent |
aSearch engines used: PubMed, Cochrane, and Embase.
TABLE A2.
MINORS Scoresa
| Author (Year) | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Data Collection | Endpoints Appropriate to Study Aim | Unbiased Assessment of Study Endpoint | Follow-up Period Appropriate to Study Aim | % Lost to Follow-up | Prospective Calculation of Study Size | Adequate Control Group | Contemporary Groups | Baseline Equivalence of Groups | Adequate Statistical Analyses | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anakwenze et al1 (2013) | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20/24 |
| Boyer et al5 (2015) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Cho et al8 (2011) | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 19/24 |
| Choi et al10 (2012) | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | N/A | N/A | N/A | N/A | 13/16 |
| Choi et al11 (2014) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| El-Azab et al17 (2010) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| Frank et al18 (2008) | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 0 | N/A | N/A | N/A | N/A | 11/16 |
| Gerhardt et al23 (2012) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Haneveld et al24 (2013) | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20/24 |
| Hug et al25 (2015) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 21/24 |
| Ide et al26 (2015) | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 20/24 |
| Kim et al30 (2014) | 2 | 1 | 1 | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 19/24 |
| Kim et al29 (2013) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Kim et al31 (2014) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Kim et al33 (2013) | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 0 | 2 | 2 | 1 | 2 | 18/24 |
| Lee et al36 (2013) | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 13/16 |
| McCormick et al44 (2014) | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 23/24 |
| Mihata et al45 (2011) | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 21/24 |
| Neyton et al46 (2013) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| Park et al47 (2014) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 1 | 2 | 2 | 20/24 |
| Park et al48 (2013) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Park et al49 (2013) | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 0 | N/A | N/A | N/A | N/A | 12/16 |
| Park et al50 (2010) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| Park et al53 (2014) | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 0 | 1 | 2 | 2 | 2 | 19/24 |
| Pennington et al55 (2010) | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 21/24 |
| Rhee et al57 (2012) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Ryu et al58 (2015) | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 20/24 |
| Sethi et al60 (2010) | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | N/A | N/A | N/A | N/A | 13/16 |
| Shin et al61 (2015) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22/24 |
| Toussaint et al66 (2011) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| Tudisco et al68 (2013) | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 20/24 |
| Voigt et al70 (2010) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 14/16 |
| Wang et al72 (2015) | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 24/24 |
| Werthel et al73 (2014) | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | N/A | N/A | N/A | N/A | 13/16 |
aMINORS, Methodological Index for Non-Randomized Studies; N/A, not applicable.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: P.D.F. has received educational support from Smith & Nephew and hospitality payments from Medical Device Business Services. M.J.A. has received educational support and speaking fees from Arthrex and has received hospitality payments from DePuy and Gotham Surgical. K.J.J. has received educational support from Arthrex, honoraria from the Musculoskeletal Transplant Foundation, and hospitality payments from Aesculap and Micromed. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Anakwenze OA, Baldwin K, Milby AH, Warrender W, Shulman B, Abboud JA. Arthroscopic repair of large rotator cuff tears using the double-row technique: an analysis of surgeon experience on efficiency and outcomes. J Shoulder Elbow Surg. 2013;22(1):26–31. [DOI] [PubMed] [Google Scholar]
- 2. Bayne O, Bateman J. Long-term results of surgical repair of full-thickness rotator cuff tears In: Bateman JE, Welsh R, eds. Surgery of the Shoulder. Philadelphia: CV Mosby; 1984:167–171. [Google Scholar]
- 3. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15(3):290–299. [DOI] [PubMed] [Google Scholar]
- 4. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. [DOI] [PubMed] [Google Scholar]
- 5. Boyer P, Bouthors C, Delcourt T, et al. Arthroscopic double-row cuff repair with suture-bridging: a structural and functional comparison of two techniques. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):478–486. [DOI] [PubMed] [Google Scholar]
- 6. Brown BS, Cooper AD, McIff TE, Key VH, Toby EB. Initial fixation and cyclic loading stability of knotless suture anchors for rotator cuff repair. J Shoulder Elbow Surg. 2008;17(2):313–318. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS, Adams CR, Burkhart SS, Schoolfield JD. A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthroscopy. 2009;25(3):274–281. [DOI] [PubMed] [Google Scholar]
- 8. Cho NS, Lee BG, Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011;39(10):2108–2116. [DOI] [PubMed] [Google Scholar]
- 9. Cho NS, Yi JW, Lee BG, Rhee YG. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38(4):664–671. [DOI] [PubMed] [Google Scholar]
- 10. Choi CH, Kim SK, Cho MR, et al. Functional outcomes and structural integrity after double-pulley suture bridge rotator cuff repair using serial ultrasonographic examination. J Shoulder Elbow Surg. 2012;21(12):1753–1763. [DOI] [PubMed] [Google Scholar]
- 11. Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. 2014;23(11):1675–1681. [DOI] [PubMed] [Google Scholar]
- 12. Christoforetti JJ, Krupp RJ, Singleton SB, Kissenberth MJ, Cook C, Hawkins RJ. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21(4):523–530. [DOI] [PubMed] [Google Scholar]
- 13. Cole BJ, ElAttrache NS, Anbari A. Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy. 2007;23:662–669. [DOI] [PubMed] [Google Scholar]
- 14. Cummins CA, Murrell GA. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J Shoulder Elbow Surg. 2003;12(2):128–133. [DOI] [PubMed] [Google Scholar]
- 15. DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial. J Bone Joint Surg Am. 1984;66:563–567. [PubMed] [Google Scholar]
- 16. Dines JS, Bedi A, ElAttrache NS, Dines DM. Single-row versus double-row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg. 2010;18:83–93. [DOI] [PubMed] [Google Scholar]
- 17. El-Azab H, Buchmann S, Beitzel K, Waldt S, Imhoff AB. Clinical and structural evaluation of arthroscopic double-row suture-bridge rotator cuff repair: early results of a novel technique. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1730–1737. [DOI] [PubMed] [Google Scholar]
- 18. Frank JB, ElAttrache NS, Dines JS, Blackburn A, Crues J, Tibone JE. Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med. 2008;36(8):1496–1503. [DOI] [PubMed] [Google Scholar]
- 19. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. [DOI] [PubMed] [Google Scholar]
- 20. Gartsman GM, Drake G, Edwards TB. Ultrasound evaluation of arthroscopic full-thickness supraspinatus rotator cuff repair: single-row versus double-row suture bridge (transosseous equivalent) fixation. Results of a prospective, randomized study. J Shoulder Elbow Surg. 2013;22:1480–1487. [DOI] [PubMed] [Google Scholar]
- 21. Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed] [Google Scholar]
- 22. Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br. 1994;76:371–380. [PubMed] [Google Scholar]
- 23. Gerhardt C, Hug K, Pauly S, Marnitz T, Scheibel M. Arthroscopic single-row modified Mason-Allen repair versus double-row suture bridge reconstruction for supraspinatus tendon tears: a matched-pair analysis. Am J Sports Med. 2012;40(12):2777–2785. [DOI] [PubMed] [Google Scholar]
- 24. Haneveld H, Hug K, Diederichs G, Scheibel M, Gerhardt C. Arthroscopic double-row repair of the rotator cuff: a comparison of bio-absorbable and non-resorbable anchors regarding osseous reaction. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1647–1654. [DOI] [PubMed] [Google Scholar]
- 25. Hug K, Gerhardt C, Haneveld H, Scheibel M. Arthroscopic knotless-anchor rotator cuff repair: a clinical and radiological evaluation. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2628–2634. [DOI] [PubMed] [Google Scholar]
- 26. Ide J, Karasugi T, Okamoto N, Taniwaki T, Oka K, Mizuta H. Functional and structural comparisons of the arthroscopic knotless double-row suture bridge and single-row repair for anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2015;24(10):1544–1554. [DOI] [PubMed] [Google Scholar]
- 27. Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88(3):472–479. [DOI] [PubMed] [Google Scholar]
- 28. Kannus P, Jozsa L. Histopathological changes preceding spontaneous rupture of a tendon: a controlled study of 891 patients. J Bone Joint Surg Am. 1991;73(10):1507–1525. [PubMed] [Google Scholar]
- 29. Kim KC, Shin HD, Cha SM, Lee WY. Comparison of repair integrity and functional outcomes for 3 arthroscopic suture bridge rotator cuff repair techniques. Am J Sports Med. 2013;41(2):271–277. [DOI] [PubMed] [Google Scholar]
- 30. Kim KC, Shin HD, Cha SM, Park JY. Comparisons of retear patterns for 3 arthroscopic rotator cuff repair methods. Am J Sports Med. 2014;42(3):558–565. [DOI] [PubMed] [Google Scholar]
- 31. Kim KC, Shin HD, Cha SM, Park JY. Repair integrity and functional outcome after arthroscopic conversion to a full-thickness rotator cuff tear: articular- versus bursal-side partial tears. Am J Sports Med. 2014;42(2):451–456. [DOI] [PubMed] [Google Scholar]
- 32. Kim SH, Cho WS, Joung HY, Choi YE, Jung M. Perfusion of the rotator cuff tendon according to the repair configuration using an indocyanine green fluorescence arthroscope: a preliminary report. Am J Sports Med. 2017;45(3):659–665. [DOI] [PubMed] [Google Scholar]
- 33. Kim YK, Moon SH, Cho SH. Treatment outcomes of single-versus double-row repair for larger than medium-sized rotator cuff tears: the effect of preoperative remnant tendon length. Am J Sports Med. 2013;41(10):2270–2277. [DOI] [PubMed] [Google Scholar]
- 34. Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. [DOI] [PubMed] [Google Scholar]
- 35. Lapner PL, Sabri E, Rakhra K, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012;94:1249–1257. [DOI] [PubMed] [Google Scholar]
- 36. Lee KW, Seo DW, Bae KW, Choy WS. Clinical and radiological evaluation after arthroscopic rotator cuff repair using suture bridge technique. Clin Orthop Surg. 2013;5(4):306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Liem D, Dedy NJ, Hauschild G, et al. In vivo blood flow after rotator cuff reconstruction in a sheep model: comparison of single versus double row. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):470–477. [DOI] [PubMed] [Google Scholar]
- 38. Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007;89:1770–1776. [DOI] [PubMed] [Google Scholar]
- 39. Lo IK, Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035–1042. [DOI] [PubMed] [Google Scholar]
- 40. Lorbach O, Bachelier F, Vees J, Kohn D, Pape D. Cyclic loading of rotator cuff reconstructions: single-row repair with modified suture configurations versus double-row repair. Am J Sports Med. 2008;36:1504–1510. [DOI] [PubMed] [Google Scholar]
- 41. Mall NA, Lee AS, Chahal J, et al. Transosseous-equivalent rotator cuff repair: a systematic review on the biomechanical importance of tying the medial row. Arthroscopy. 2013;29(2):377–386. [DOI] [PubMed] [Google Scholar]
- 42. Mansat P, Cofield RH, Kersten TE, Rowland CM. Complications of rotator cuff repair. Orthop Clin North Am. 1997;28:205–213. [DOI] [PubMed] [Google Scholar]
- 43. Mazzocca AD, Bollier MD, Ciminiello AM. Biomechanical evaluation of arthroscopic rotator cuff repairs over time. Arthroscopy. 2010;26:592–599. [DOI] [PubMed] [Google Scholar]
- 44. McCormick F, Gupta A, Bruce B, et al. Single-row, double-row, and transosseous equivalent techniques for isolated supraspinatus tendon tears with minimal atrophy: a retrospective comparative outcome and radiographic analysis at minimum 2-year followup. Int J Shoulder Surg. 2014;8(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mihata T, Watanabe C, Fukunishi K, et al. Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med. 2011;39(10):2091–2098. [DOI] [PubMed] [Google Scholar]
- 46. Neyton L, Godenèche A, Nové-Josserand L, Carrillon Y, Cléchet J, Hardy MB. Arthroscopic suture-bridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy. 2013;29(1):10–17. [DOI] [PubMed] [Google Scholar]
- 47. Park JY, Jung SW, Jeon SH, Cho HW, Choi JH, Oh KS. Arthroscopic repair of large U-shaped rotator cuff tears without margin convergence versus repair of crescent- or L-shaped tears. Am J Sports Med. 2014;42(1):103–111. [DOI] [PubMed] [Google Scholar]
- 48. Park JY, Lee SY, Chung SW, Zulkifli H, Cho JH, Oh KS. Clinical comparison between double-row and transosseous-equivalent repairs for medium to large size rotator cuff tears. Arch Orthop Trauma Surg. 2013;133(12):1727–1734. [DOI] [PubMed] [Google Scholar]
- 49. Park JY, Lhee SH, Oh KS, Moon SG, Hwang JT. Clinical and ultrasonographic outcomes of arthroscopic suture bridge repair for massive rotator cuff tear. Arthroscopy. 2013;29(2):280–289. [DOI] [PubMed] [Google Scholar]
- 50. Park JY, Siti HT, Keum JS, Moon SG, Oh KS. Does an arthroscopic suture bridge technique maintain repair integrity? A serial evaluation by ultrasonography. Clin Orthop Relat Res. 2010;468(6):1578–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Park MC, ElAttrache NS, Ahmad CS, Tibone JE. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22(12):1360. [DOI] [PubMed] [Google Scholar]
- 52. Park MC, Peterson AB, McGarry MH, Park CJ, Lee TQ. Knotless transosseous-equivalent rotator cuff repair improves biomechanical self-reinforcement without diminishing footprint contact compared with medial knotted repair. Arthroscopy. 2017;33(8):1473–1481. [DOI] [PubMed] [Google Scholar]
- 53. Park YE, Shon MS, Lim TK, Koh KH, Jung SW, Yoo JC. Knot impingement after rotator cuff repair: is it real? Arthroscopy. 2014;30(9):1055–1060. [DOI] [PubMed] [Google Scholar]
- 54. Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 55. Pennington WT, Gibbons DJ, Bartz BA, et al. Comparative analysis of single-row versus double-row repair of rotator cuff tears. Arthroscopy. 2010;26(11):1419–1426. [DOI] [PubMed] [Google Scholar]
- 56. Redziniak DE, Hart J, Turman K, et al. Arthroscopic rotator cuff repair using the Opus knotless suture anchor fixation system. Am J Sports Med. 2009;37(6):1106–1110. [DOI] [PubMed] [Google Scholar]
- 57. Rhee YG, Cho NS, Parke CS. Arthroscopic rotator cuff repair using modified Mason-Allen medial row stitch: knotless versus knot-tying suture bridge technique. Am J Sports Med. 2012;40(11):2440–2447. [DOI] [PubMed] [Google Scholar]
- 58. Ryu KJ, Kim BH, Lee Y, Lee YS, Kim JH. Modified suture-bridge technique to prevent a marginal dog-ear deformity improves structural integrity after rotator cuff repair. Am J Sports Med. 2015;43(3):597–605. [DOI] [PubMed] [Google Scholar]
- 59. Salata MJ, Sherman SL, Li EC. Biomechanical evaluation of transosseous rotator cuff repair: do anchors really matter? Am J Sports Med. 2013;41:283–290. [DOI] [PubMed] [Google Scholar]
- 60. Sethi PM, Noonan BC, Cunningham J, Shreck E, Miller S. Repair results of 2-tendon rotator cuff tears utilizing the transosseous equivalent technique. J Shoulder Elbow Surg. 2010;19(8):1210–1217. [DOI] [PubMed] [Google Scholar]
- 61. Shin SJ, Kook SH, Rao N, Seo MJ. Clinical outcomes of modified Mason-Allen single-row repair for bursal-sided partial-thickness rotator cuff tears: comparison with the double-row suture-bridge technique. Am J Sports Med. 2015;43(8):1976–1982. [DOI] [PubMed] [Google Scholar]
- 62. Slabaugh MA, Nho SJ, Grumet RC, et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26(3):393–403. [DOI] [PubMed] [Google Scholar]
- 63. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 64. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. [DOI] [PubMed] [Google Scholar]
- 65. Tashjian RZ, Hollins AM, Kim HM, et al. Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med. 2010;38:2435–2442. [DOI] [PubMed] [Google Scholar]
- 66. Toussaint B, Schnaser E, Bosley J, Lefebvre Y, Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med. 2011;39(6):1217–1225. [DOI] [PubMed] [Google Scholar]
- 67. Trantalis JN, Boorman RS, Pletsch K, Lo IK. Medial rotator cuff failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2008;24(6):727–731. [DOI] [PubMed] [Google Scholar]
- 68. Tudisco C, Bisicchia S, Savarese E, et al. Single-row vs. double-row arthroscopic rotator cuff repair: clinical and 3 Tesla MR arthrography results. BMC Musculoskelet Disord. 2013;14(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Vaishnav S, Millett PJ. Arthroscopic rotator cuff repair: scientific rationale, surgical technique, and early clinical and functional results of a knotless self-reinforcing double-row rotator cuff repair system. J Shoulder Elbow Surg. 2010;19(suppl 2):83–90. [DOI] [PubMed] [Google Scholar]
- 70. Voigt C, Bosse C, Vosshenrich R, Schulz AP, Lill H. Arthroscopic supraspinatus tendon repair with suture-bridging technique: functional outcome and magnetic resonance imaging. Am J Sports Med. 2010;38(5):983–991. [DOI] [PubMed] [Google Scholar]
- 71. Walton J, Murrell G. Effects of operative time on outcomes of rotator cuff repair. Tech Shoulder Elbow Surg. 2012;13:23–27. [Google Scholar]
- 72. Wang A, McCann P, Colliver J, et al. Do postoperative platelet-rich plasma injections accelerate early tendon healing and functional recovery after arthroscopic supraspinatus repair? A randomized controlled trial. Am J Sports Med. 2015;43(6):1430–1437. [DOI] [PubMed] [Google Scholar]
- 73. Werthel JD, Pelissier A, Massin P, Boyer P, Valenti P. Arthroscopic double row cuff repair with suture-bridging and autologous conditioned plasma injection: functional and structural results. Int J Shoulder Surg. 2014;8(4):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Yamakado K, Katsuo S, Mizuno K, Arakawa H, Hayashi S. Medial-row failure after arthroscopic double-row rotator cuff repair. Arthroscopy. 2010;26(3):430–435. [DOI] [PubMed] [Google Scholar]
- 75. Yepes H, Tang M, Morris SF, Stanish WD. Relationship between hypovascular zones and patterns of ruptures of the quadriceps tendon. J Bone Joint Surg Am. 2008;90(10):2135–2141. [DOI] [PubMed] [Google Scholar]