Abstract
Free medical fairs have emerged to compensate for the lack of access to affordable healthcare in rural areas of the U.S. Mental health services are offered less frequently than other medical services, in spite of a documented need, perhaps due to a belief that mental health interventions could not be effective in a single session. We examined the types of problems presented at three rural medical fairs, and whether single session mental health interventions affected participants’ health confidence, distress, or progress toward health-related goals. Problems presented included mental health, legal, financial, tobacco cessation, and relationship problems. Findings indicated that, on average, participants gained health confidence and reduced distress, and found the service very helpful. The majority of those able to be reached for phone follow-up reported progress on one or more health goals. Goals that involved manageable steps within the participants’ own control, such as gratitude practices or progressive muscle relaxation, were the most likely to be completed. Patients who presented with at least one mental health problem were more likely to have taken steps toward a health goal. Implementation lessons included the importance learning the fairs’ cultures, advertising the services, location of services, being proactive in connecting with patients, and preparing resources for community referrals. Overall, findings suggest that mental health interventions can have a positive impact on some people at free medical fairs. Given that tens of thousands of people attend each year, the fairs offer a fruitful opportunity to reach some of our most underserved citizens.
Introduction
Free medical fairs have emerged in recent years to compensate for the lack of access to affordable healthcare in some rural areas of the U.S. [1] The fairs usually offer vision, dental and medical care, and often lab and pharmacy services, but less typically mental health care,[2] despite the striking need for these services in rural areas.[3] While the reasoning behind this exclusion is not discussed extensively in the literature, it may be driven by the belief that brief mental health interventions would not meaningfully affect persons struggling with the harsh daily living conditions of these underserved environments.[4]
To date, no published studies have examined the efficacy of mental health interventions at free rural medical fairs. There is also a scarcity of research on the efficacy of single-session mental health interventions at humanitarian medical sites after natural disasters and in war zones, and there has been a recent call for this research.[5, 6] However, single session mental health interventions have been offered in other contexts and, to a limited degree, examined for efficacy. The limited extant research on the efficacy of single session mental health interventions is mixed. Investigators at walk-in community mental health clinics have found that patients benefited from as little as one session,[7] and that many patients only wanted one session.[8] Single session interventions have also been found to be effective in reducing phobias, [9] [10] panic disorder severity, [11] anxiety in trauma-exposed adults, [12] an anxious mindset in adolescents, [13] acute insomnia[14] and consumption of alcohol in moderate to heavy drinking college students.[15] Because of the almost universally high rate of patients not returning after an initial session, some commentators have noted that the modal number of mental health sessions is, in fact, one.[16] Not all studies have found significant treatment effects, however. A single session motivational interviewing intervention was not found to decrease alcohol used in pregnant women[17] and a single session consultation was not found to achieve weight reduction in overweight children.[18] Overall, the limited research on single session therapy suggests efficacy in at least some settings, but in contexts somewhat different from free rural medical fairs.
Single session mental health interventions at rural health fairs can be seen as a type of integrated mental health care. Mental health providers are increasingly offering point-of-care treatment in primary care and other medical contexts. These “integrated behavioral health interventions” are often delivered in only one contact, because many patients in these contexts do not need, want, or have resources for further treatment. While recent research indicates the efficacy of integrated interventions,[19] it has not specifically investigated single session contacts.
Given the substantial and well-documented unmet mental health needs of rural residents, [3, 20, 21] we wanted to investigate whether single session mental health services could usefully be delivered at rural medical fairs that reach tens of thousands of underserved people. We hypothesized that the single session behavioral health interventions used in our primary care clinic might be a suitable model. While not remote, our primary care clinic serves many rural patients who present with issues also prevalent in the more remote rural areas where medical fairs take place, such as chronic pain, tobacco addiction, chronic medical conditions, anxiety, depression, psychosocial stressors, and low resources. Because these integrated services are designed precisely to reach people whose mental health problems would otherwise be untreated, we wanted to investigate their efficacy with the extremely underserved populations at the remote area medical fairs sponsored by RAM of Virginia. [22]
Our study aimed to investigate three questions: 1) If we offered very broadly defined mental health services, with what problems would patients most commonly present? 2) Would our services have any measureable impact on patients’ distress, health confidence, or coping behaviors at the time of service or at phone follow-up? 3) What lessons would we learn about how best to implement our services at the fair to maximize their scope and usefulness?
Method
Setting
Services were offered at three different Remote Area Medical fairs in far southwest Virginia. These fairs are typically held annually at central community locations and attract thousands of people, sometimes from hours away, who line up overnight and sleep in their cars in order to obtain free medical, vision and dental services.[23] One of the fairs we attended was located in Grundy, Virginia in an elementary school where behavioral health services were co-located with “Patient Education” in a classroom in the general medical area. Two fairs were located in Wise, Virginia at an outdoor fairground. At one of the Wise fairs, our services were offered in a free-standing tent near various auxiliary services; at the other Wise fair, we were located with Psychiatry near the medical tent.
Participants
Forty-seven patients (32 female, 15 male) at three fairs agreed to participate in the study. Some patients were referred by other providers at the fairs and some patients walked up for services themselves. The average age of participants was 42 (age range 18–69). All participants were English-speaking and Caucasian.
Interventions
All interventions were person-centered and proceeded in systematic steps. Clinicians began with an open-ended prompt to obtain the patient’s story in their own words. After expressing appropriate empathy, clinicians noted and reinforced any positive coping responses. Clinicians then assessed patients’ needs and implemented one or more behavioral interventions tailored to those needs. Each intervention concluded with the participant setting 1–3 health-related goals and specific action steps. Clinicians recorded the goals and action steps, plus any related referral information or instructions, in writing for the participants to refer to at home.
Measures
Types of Presenting Problems
During the intervention, investigating clinicians categorized participants’ presenting problems into 15 possible categories: depression, anxiety, grief, relationship difficulties, PTSD, stress, ADHD, substance abuse, diet, exercise, smoking, financial problems, pain, and other.
Types of Interventions
Investigating clinicians logged the type of interventions they delivered to each participant as one of the following: The BATHE Method,[24] Problem-solving, Motivational Interviewing for Behavior Change,[25] a Pain Management protocol, and an Anxiety Management protocol.
Subjective Distress and Health Confidence
Participants completed a single-item, Likert-scale measure of subjective distress immediately prior to the intervention, immediately post-intervention, and, if reached at phone follow-up, 2–5 weeks later: “On a scale of 0 to 10, with 0 being not distressed at all and 10 being the worst possible distress, how distressed are you right now?”[26] Participants also completed a single-item, Likert-scale measure of health confidence at these times: “How confident are you that you can control and manage most of your health problems?” [27]
Intervention helpfulness and goal progress
This study used a patient-report approach to therapeutic outcomes that has been established as a valid approach to assessing outcomes within therapy effectiveness trials, particularly in contexts under which control group approaches would be problematic.[28, 29] The approach asks patients to assess therapeutic helpfulness as well as progress in meeting specific goals. In this study, participants answered a single item, Likert-scale question regarding their perception of the helpfulness of the intervention immediately after the intervention and at phone follow-up: “On a scale of 1–5, how helpful do you feel this service has been?”
Goal Progress
At phone follow-up, a research assistant reminded participants of the one to three goals they had set during the intervention and queried them as to whether they had made progress on each goal. Participants’ responses were coded in a binary fashion (yes/no) as to whether they endorsed making progress. The research assistant also problem-solved solutions to any barriers during the call.
Implementation Lessons
The clinicians and trainees delivering services kept notes as to their observations about what facilitated or interfered with service implementation. Notes were reviewed and discussed by study authors and consensus themes were extracted.
Procedures
The institutional review board at the mid-Atlantic university that sponsored the research approved the study protocol. Organizers of each fair also approved the study. Patients were offered enrollment and signed a consent form at the onset of contact at the fairs. No identifying data except name and phone number were collected. Services were not contingent upon participation and a few patients accepted services but declined participation in the study. No compensation was offered for participation.
Investigating clinicians were licensed clinical psychologists experienced in Integrated Behavioral Healthcare and clinical psychology doctoral students and a Family Medicine resident under their supervision. To cast a wide net and avoid stigma, services were advertised as “Health Coaching” for chronic pain, smoking cessation, diet and exercise, and coping with any type of emotional issue or “stress.” Participants were informed that, with their permission, a staff member from the investigating clinicians’ clinic would phone in about two weeks to ask if they had made progress on their plan and offer further ideas if needed.
Results
Data collected at the three fairs were combined. Gender was examined as a potential predictor of all outcome measures. The only gender effects found were that males were significantly less likely to participate in phone follow-up (20% participation for males vs. 56% for females; χ2 (1, 46) = 5.43, p = .02).
The most common problem presented was smoking cessation, followed (in order of frequency) by financial stress, anxiety, relationship problems, depression, pain, grief, substance abuse, post-traumatic stress, exercise, diet, ADHD, and other. For purposes of data analysis, these categories were collapsed into five groups: Mental Health (depression, anxiety, grief, relationship difficulties, PTSD, stress, ADHD, substance abuse); Lifestyle (diet, exercise, smoking); Financial, Pain and Other (medical, learning and legal problems). Twenty-six patients presented problems in the Mental Health category; 15 in the Lifestyle category, 8 in the Financial category, 8 in Other, and 5 in Pain (Figure 1).
Figure 1. Frequency of Problems presented.
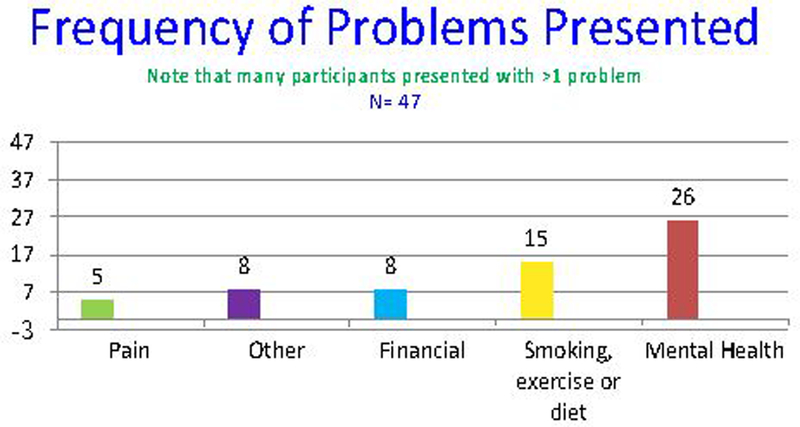
Mental Health Problems included depression, anxiety, substance abuse, grief, realationship problems, ADHD, schizophrenia, PTSD.
Other included legal, medical, and learning problems.
Compared to their pre-intervention baseline, paired t-tests indicated that participants reported significantly increased health confidence immediately after the intervention (t (44) = 5.41, p < .001) and at phone follow-up (t (20) = 4.09, p < .001) (Figure 2). Health confidence increased slightly further between the post-intervention rating and phone follow-up. Participants also reported significantly decreased levels of subjective distress immediately after the intervention (t (44) = −2.19, p = .03) (Figure 2). Subjective distress rebounded somewhat between post-intervention and phone follow-up and the change from pre-intervention to post-intervention was not significant (t (20) = −1.55, p = .14).
Figure 2.
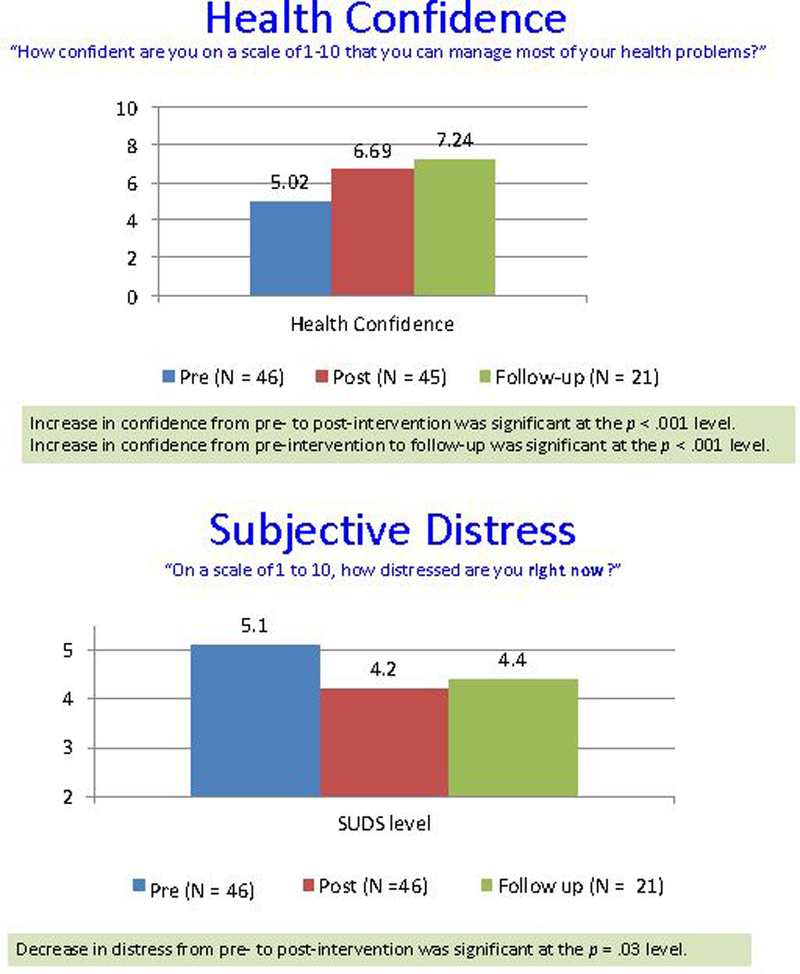
Changes in Health Confidence and subjective distress
Post-intervention, 86% of participants rated the service as “very helpful” or “extremely helpful,” and of those reached at phone follow-up, 100% did.
Seventy-two percent (n = 15) of participants reached by phone follow-up reported that they had made progress on at least one of the goals set during the intervention (Figure 3). Having made progress on a goal was not found to be correlated with initial levels of health confidence or distress, with changes in those, or with ratings of intervention helpfulness. Goals were categorized into three groups for analysis: 1) Goals to make lifestyle change (n = 5) (tobacco cessation, diet, spending habits); 2) Goals to contact community resources (n = 8) (i.e., legal aid, mental health counselor); and 3) Goals involving self-care (n = 39) (i.e. calm breathing exercises, gratitude exercises, progressive muscle relaxation). Five percent of participants (n = 1) reported progress toward goals involving lifestyle change, 10% of participants (n = 2) reported success toward goals related to contacting outside organizations, and 56% of participants (n = 15) reported progress toward goals categorized as self-care. A t-test indicated that participants who initially presented with a mental health problem (even if they also presented with a situational or lifestyle problem) were significantly more likely to report having taken steps toward a goal than those who did not (t (5, 15) = −3.44, p = .003).
Figure 3.
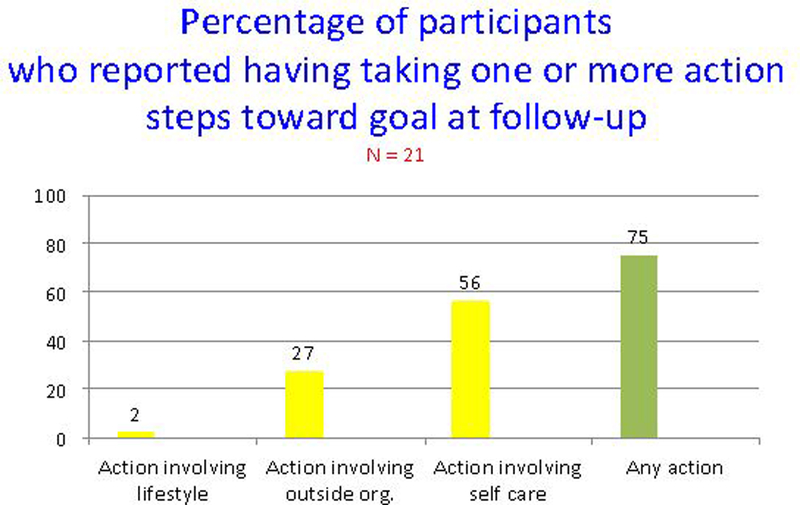
Percentage of participants who reported having taking one or more action steps toward goal at follow-up.
Implementation Lessons
1. Learn and join the culture. Each medical fair has its own culture. Spend time talking with the event organizers and previous volunteers well in advance. Travel, eat, and share lodging with the medical providers to strengthen trust and increase knowledge about what you can contribute. They will help you connect with appropriate patients and collaborate in their care. 2. Location, location, location. Arrange with the fair organizers well in advance about where you will be located and how patient flow will work. Close proximity to the general medical providers (as opposed to dental, vision, or ancillary services) increased referrals and decreased the likelihood of referred patients getting “lost” on their way to our area. Having a stand-alone tent among other ancillary services was much less effective. At one fair, we were located with Psychiatry in a Behavioral Health tent, which had the advantages of good flow from the medical tent and easy coordination with Psychiatry, but the associated stigma appeared to have deterred some types of patients. At another fair, we were located with “Patient Education” in a room that most patients came through after seeing a medical provider. This arrangement worked well in that it reduced the stigma barrier and facilitated a “warm hand-off” of patients. However, we did not yet feel that we had discovered the optimal way to access patients and felt that we were missing many people who might benefit. 3. Be active in connecting with potential patients. Create an information sheet for providers with a summary of who you are and the services you will offer written in patient-friendly language. Make sure that a list of your services and where you are located is prominent at the registration desk. If it fits the culture, provide PSA-type group instruction to patients waiting for vision or dental around stress management and behavior change. Signage is important, as many patients walk around the fair and simply choose services that interest them. The term “Health Coaching” seemed acceptable to patients, but we found that signs with more specific messages such as “Feeling stressed? Let’s talk!” may have been better attractors. 4. Prepare resources for referrals. Arrive at the fair with a list of low-cost community resources (mental health, exercise and recreation, adult education, social services, legal aid, food and housing assistance, eldercare services) in the geographic region of the fairs. As patients often come to these fairs from a distance, researching the resources in communities up to a couple of hours away was worthwhile. Providing patients with ideas about and up-to-date contact information for those resources was valued. 5. Mindset of flexibility and adaptability. Be prepared to be flexible, both in terms of working conditions and intervention approaches, as the range of patients who presented was very broad in terms of problem, acuity, health literacy, and needs. 6. Bring trainees. Most disciplines at the health fair brought trainees, and the trainees who accompanied us found it a rich learning experience both in terms of developing behavioral health skills and learning about the culture and needs of a drastically underserved rural population.
Discussion
Types of Problems Presented
Participants at these fairs presented with a wide variety of serious problems, including situational challenges such as financial or legal stressors, lifestyle factors such as tobacco use or poor diet, and mental health concerns ranging from adjustment issues to psychosis. Many participants presented with multiple problems or with complex problems affected by more than one category. Some participants were already in contact with relevant professional services, while many had never previously talked with a professional about their problem. The range of problems was very similar to those found in our primary care clinic, which serves both urban and rural poor.
Efficacy of Services
Participants overwhelmingly rated the intervention as helpful, a finding consistent with their reports of reduced distress, increased health confidence, and progress toward health goals, on average. Progress was most often reported on action steps not requiring extra resources and within participants’ own control, such as engaging in calm breathing, gratitude exercises, or positive self-talk that had been practiced with the clinician. Progress toward a goal of connecting with a specific community resource was smaller, perhaps reflecting some reluctance to share private concerns or get involved in an outside system. The fact that only one participant reported progress toward lifestyle goals such as quitting smoking, improving diet or better managing finances may illustrate the intractability of lifestyle habits in the setting of scarce resources and few supports.
Apart from type of goal, patients who presented with any mental health problem were more likely to report steps toward a goal than persons who only presented with a lifestyle (smoking, diet, exercise) or situational (housing, financial, legal) problem. It is likely that presenting with a mental health problem led to choosing the types of goals that were more successful, such as self-care and contacting community organizations. This finding may also reflect that the persons delivering the services were mental health clinicians and thus more skilled at addressing those types of problems.
Limitations and areas for future research
One limitation of the study is its relatively small sample size, especially with regard to the number of participants who were able to be followed up by phone. Other limitations were lack of a control group and possible response bias due to the fact that the clinicians providing the services also collected the post-intervention ratings (although the research assistants who collected phone follow-up ratings had not been involved in the intervention.) The study is also limited by the relatively narrow scope and depth of measures collected.
Conclusion
The severe lack of mental health access in rural areas of the United States has been well documented. Numerous organizations are working hard to improve access through telemedicine, behavioral workforce development, training of primary care physicians, federal and state funding, and inter-agency collaboration. Much as with access to general medical care, however, progress is slower than optimal and tens of thousands of citizens remain untreated for mental health conditions that undermine their physical health, emotional well-being, relationships, and ability to work or care for family members. The thousands of rural citizens who come out every year for free medical fairs present a unique opportunity to deliver mental health care at a moment when people may be psychologically open to receiving help and where they have already invested the time and transportation costs to come to a central location. This small, exploratory study suggests that some people who attend rural medical fairs are hungry for the opportunity to talk about their problems and may, in doing so, experience reduced distress, increased confidence that they can manage their health, and progress towards adaptive coping. People who presented with mental health problems were more likely to have made progress toward a goal at follow-up than people with lifestyle or situational problems. Setting goals that involve very manageable steps that the person has control over may reap more benefits than goals requiring broader lifestyle change. Identifying and providing contact information for the community resources most appropriate for individual patients also appears to add value. Delivery of services was facilitated by building connections with fair organizers and medical providers, being physically located with medical providers, and proactively seeking participants at the fair. Our experience is that mental health providers and trainees whose skill set is fairly broad and who are able to be flexible find participating at rural medical fairs to be a unique and rewarding experience. Further research with a larger sample, including a control group, and more robust outcome measures will be helpful in refining what types of single sessions interventions have the most benefit for this underserved population.
Acknowledgements:
This study was supported by grants from the National Institute of Child Health and Human Development to J. P. Allen (R01-MH58066 & R37HD058305).
References
- 1.Werzen A, Joshi P, Teng S: Redefining Medical Care in Appalachia: Remote Area Medical. 2013. [Google Scholar]
- 2.[https://ramusa.org]
- 3.Roll JM, Kennedy J, Tran M, Howell D: Disparities in Unmet Need for Mental Health Services in the United States, 1997–2010. Psychiatric Services 2013, 16(1):80. [DOI] [PubMed] [Google Scholar]
- 4.Bass J, Poudyal B, Tol W, Murray L, Nadison M, Bolton P: A controlled trial of problem-solving counseling for war-affected adults in Aceh, Indonesia. Social psychiatry and psychiatric epidemiology 2012, 47(2):279–291. [DOI] [PubMed] [Google Scholar]
- 5.Jordans MJ, Tol WA: Mental health in humanitarian settings: shifting focus to care systems. International Health 2013, 5(1):9–10. [DOI] [PubMed] [Google Scholar]
- 6.Tol WA, Patel V, Tomlinson M, Baingana F, Galappatti A, Panter-Brick C, Silove D, Sondorp E, Wessells M, van Ommeren M: Research priorities for mental health and psychosocial support in humanitarian settings. PLoS medicine 2011, 8(9):e1001096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stalker CA, Horton S, Cait C-A: Single-session therapy in a walk-in counseling clinic: A pilot study. Journal of Systemic Therapies 2012, 31(1):38–52. [Google Scholar]
- 8.Harper-Jaques S, Foucault D: Walk-in single-session therapy: Client satisfaction and clinical outcomes. Journal of Systemic Therapies 2014, 33(3):29–49. [Google Scholar]
- 9.Ryan SM, Strege MV, Oar EL, Ollendick TH: One session treatment for specific phobias in children: Comorbid anxiety disorders and treatment outcome. Journal of Behavior Therapy and Experimental Psychiatry 2017, 54:128–134. [DOI] [PubMed] [Google Scholar]
- 10.Ollendick TH, Halldorsdottir T, Fraire MG, Austin KE, Noguchi RJ, Lewis KM, Jarrett MA, Cunningham NR, Canavera K, Allen KB et al. : Specific phobias in youth: a randomized controlled trial comparing one-session treatment to a parent-augmented one-session treatment. Behavior therapy 2015, 46(2):141–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lessard M-J, Marchand A, Pelland M-È, Belleville G, Vadeboncoeur A, Chauny J-M, Poitras J, Dupuis G, Fleet R, Foldes-Busque G et al. : Comparing Two Brief Psychological Interventions to Usual Care in Panic Disorder Patients Presenting to the Emergency Department with Chest Pain. Behavioural and Cognitive Psychotherapy 2012, 40(02):129. [DOI] [PubMed] [Google Scholar]
- 12.Vujanovic AA, Bernstein A, Berenz EC, Zvolensky MJ: Single-Session Anxiety Sensitivity Reduction Program for Trauma-Exposed Adults: A Case Series Documenting Feasibility and Initial Efficacy. SPECIAL SERIES: Innovations in the Treatment of Anxiety Psychopathology 2012, 43(3):482–491. [DOI] [PubMed] [Google Scholar]
- 13.Schleider JL, Weisz JR: Reducing risk for anxiety and depression in adolescents: Effects of a single-session intervention teaching that personality can change. Behaviour research and therapy 2016, 87:170–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellis JG, Cushing T, Germain A: Treating Acute Insomnia: A Randomized Controlled Trial of a “Single-Shot” of Cognitive Behavioral Therapy for Insomnia. Sleep 2015, 38(6):971–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lau-Barraco C, Dunn ME: Evaluation of a single-session expectancy challenge intervention to reduce alcohol use among college students. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors 2008, 22(2):168–175. [DOI] [PubMed] [Google Scholar]
- 16.Budman SH, Hoyt MF, Friedman S: The First session in brief therapy. New York: Guilford Press; 1992. [Google Scholar]
- 17.Osterman RL, Carle AC, Ammerman RT, Gates D: Single-session motivational intervention to decrease alcohol use during pregnancy. Journal of substance abuse treatment 2014, 47(1):10–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinehr T, Kersting M, Alexy U, Andler W: Long-term follow-up of overweight children: after training, after a single consultation session, and without treatment. Journal of pediatric gastroenterology and nutrition 2003, 37(1):72–74. [DOI] [PubMed] [Google Scholar]
- 19.Asarnow JR, Rozenman M, Wiblin J, Zeltzer L: Integrated Medical-Behavioral Care Compared With Usual Primary Care for Child and Adolescent Behavioral Health: A Meta-analysis. JAMA Pediatr 2015, 169(10):929–937. [DOI] [PubMed] [Google Scholar]
- 20.Snyder A, Thatcher E: From the trunk of a Volkswagen beetle: a mobile nursing clinic in Appalachia. Family & community health 2014, 37(3):239–247. [DOI] [PubMed] [Google Scholar]
- 21.Mechanic D: More people than ever before are receiving behavioral health care in the United States, but gaps and challenges remain. Health affairs (Project Hope) 2014, 33(8):1416–1424. [DOI] [PubMed] [Google Scholar]
- 22.[https://ramusa.org/virginia/]
- 23.Huttlinger K: Research and collaboration in rural community health. Online Journal of Rural Nursing and Health Care 2012, 4(1):22–36. [Google Scholar]
- 24.Lieberman JA 3rd, Stuart MR: The BATHE Method: Incorporating Counseling and Psychotherapy Into the Everyday Management of Patients. Primary care companion to the Journal of clinical psychiatry 1999, 1(2):35–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller WR, Rollnick S: Motivational interviewing: Helping people change: Guilford press; 2012. [Google Scholar]
- 26.Wolpe J, Lazarus A: The Commonwealth and international library Mental health and social medicine division Behavior therapy techniques: A guide to the treatment of neuroses Elmsford, NY: Pergamon Press; 1966. [Google Scholar]
- 27.Wasson J, Coleman EA: Health confidence: A simple, essential measure for patient engagement and better practice. Family practice management 2014, 21(5):8–12. [PubMed] [Google Scholar]
- 28.Seligman ME: The effectiveness of psychotherapy: The Consumer Reports study. American psychologist 1995, 50(12):965. [DOI] [PubMed] [Google Scholar]
- 29.Strupp HH: The tripartite model and the Consumer Reports study. American Psychologist 1996, 51(10):1017. [DOI] [PubMed] [Google Scholar]


