Abstract
Objectives:
Gender differences in neurocognition, social skills, and negative symptoms, favoring women, have been documented among young/middle-aged adults with schizophrenia. However, gender differences have rarely been examined among older adults with schizophrenia, when decreases in circulating estrogens may impact outcomes among women.
Methods:
Community-dwelling adults (N=242, ages 40–85) with schizophrenia/schizoaffective disorder completed assessments of negative symptoms (expressive and experiential deficits), neurocognition, and social skills. Mann-Whitney U tests examined gender differences; a regression-based bootstrapped approach to moderation examined gender by age interactions.
Results:
Female participants had better neurocognition (U= 6814.00, p=.011) and less severe experiential deficits (U=4130.50, p=.022). There was no gender difference on social skills (U=5,920.50, p=0.150). Older age was associated with greater expressive deficits among men but not women (b= −.04; 95% CI [−.0780, −.0114]; bootstrap p=.009).
Conclusions:
Gender differences among adults with schizophrenia may vary depending on age; gender differences on negative symptoms may vary by symptom subgroup.
Keywords: schizophrenia, negative symptoms, older adults, age differences, gender differences
Gender differences in outcomes among people with schizophrenia have rarely been examined in older adulthood. Studies of young/middle-aged individuals with schizophrenia have found that women exhibit later age of onset, better social functioning, and, more equivocally, better neurocognition and decreased negative symptom severity, than their male counterparts (1); it is unclear whether these differences persist with age. Decreases in circulating estrogens during menopause may be associated with greater symptom severity, poorer antipsychotic response, and worsening neurocognition among women (2).
In the few studies on gender differences with older adults with schizophrenia, findings have been mixed. Studies of institutionalized older adults with schizophrenia have found no gender differences in neurocognition but more severe negative symptoms among males compared to same-age females (e.g., 3). In contrast, two studies of community-dwelling middle- aged and older adults found no gender differences in negative symptoms, neurocognition, and/or social skills performance (4–5).
Negative symptoms may need to be measured with greater specificity, as they are not a monolithic entity. Research supports a two-factor model, in which expressive deficits, such as flat affect and poverty of speech, are distinct from experiential deficits, such as avolition, apathy, and social withdrawal (6). Gender differences on these symptom subgroups have not been examined among older adults with schizophrenia.
The present study aimed to examine gender differences in negative symptoms, neurocognition, and social skills among community-dwelling middle-aged and older individuals with schizophrenia. Specifically, we were interested in whether differences in negative symptoms previously reported for global scales were also present with more detailed analyses examining experiential and expressive negative symptoms. We additionally examined gender by age interactions.
Method
Participants and Procedures
The present analyses used baseline data from a longitudinal study examining cognitive and functional outcomes among community-dwelling adults with schizophrenia and schizoaffective disorder (7). The dataset for the present study included participants who were ages 40 and older with a recorded gender (N=242; see Table 1 for gender differences on demographic variables).
Table 1.
Demographics and Descriptives by Gender.
| Variable | Male | Female |
|---|---|---|
| n=178 | n= 64 | |
| Age (years) | 55.6 ± 9.3 | 57.4 ± 8.5 |
| Race | ||
| White | 93 (52.2%) | 35 (54.7%) |
| African-American/Black | 51 (28.7%) | 20 (31.3%) |
| American Indian/Alaska Native | 2 (1.1%) | 1 (1.6%) |
| More than one race | 12 (6.7%) | 1 (1.6%) |
| Not reported/missing | 19 (11.3%) | 7 (10.9%) |
| Years of Education | 12.4 ± 3.3 | 12.7 ± 3.1 |
| Never married | 94 (52.8%) | 30 (46.9%) |
| Age at First Psych Hosp.* | 25.3 ± 10.0 | 30.0 ± 10.9 |
| Total Number of Psych Hosp. | 8.3 ± 10.0 | 6.1 ± 5.6 |
| PANSS – Positive Symptoms | 13.9 ± 0.4 | 13.1 ± 0.6 |
| PANSS – Negative Symptoms | 14.1 ± 0.4 | 13.0 ± 0.6 |
| PANSS – Expression | 7.2 ± 0.3 | 7.2 ± 0.5 |
| PANSS – Experience* | 6.3 ± 0.2 | 5.3 ± 0.4 |
| Cognitive Composite* | −1.6 ± 0.1 | −1.2 ± 0.1 |
| SSPA-Mean | 3.8 ± 0.1 | 3.9 ± 0.1 |
Significant gender differenceper Mann-Whitney U test, p<.05
Notes: Psych Hosp.= psychiatric hospitalization; PANSS= Positive and Negative Syndrome Scale; SSPA= Social Skills Performance Assessment. PANSS Positive and Negative Symptom subscales can range from 7 to 49 with higher scores reflecting more severity. For PANSS Expression and Experience, item totals are displayed, with higher scores reflecting more severity; however, factor scores were used for all analyses. PANSS Expression scores can range from 4 to 28. PANSS Experience scores can range from 3 to 21. Cognitive Composite is a composite standard score calculated using age-based norms. SSPA ranges from 1 to 5, with higher scores reflecting better social skill
Participants were recruited through outpatient treatment programs located at academic, state, and VA medical centers. Inclusion criteria were a primary DSM-IV diagnosis of schizophrenia or schizoaffective disorder per structured clinical interview and evidence of current active illness. Exclusion criteria were medical illnesses that impact cognitive functioning and a Mini-Mental Status Examination score below 18.
Eligible participants completed informed consent. Demographic and clinical information was collected via questionnaire, interview, and chart review. Symptom ratings, neurocognition, and social skills were assessed by trained raters. The appropriate institutional review boards approved all study procedures.
Measures
Positive and Negative Syndrome Scale (PANSS).
The PANSS is an interview-based measure containing 30 common symptoms of schizophrenia-spectrum disorders. Items were scored on Likert scales from 1 (absent) to 7 (extreme) based on structured participant interviews and chart review. Recent factor analyses of the PANSS have reliably produced two distinct negative symptom clusters: PANSS Reduced Emotional Expression [Blunted Affect (N1), Poor Rapport (N3), Lack of Spontaneity (N6), and Motor Retardation (G7)], and PANSS Reduced Emotional Experience [Emotional Withdrawal (N2), Passive Social Withdrawal (N4), and Active Social Avoidance (G16)]. A single principle component was created for each factor, hereafter referred to as PANSS-Expression and PANNS-Experience, respectively, using unrotated principal components analysis with the items in that factor (6).
Global Cognition.
Participants completed a comprehensive neuropsychological battery. Age-based norms were used to create Z-scores of individual cognitive tests, which were combined to create a composite standard score representing global cognition (Cog-Comp; 7).
Social Skills Performance Assessment (SSPA).
Participants completed role plays of common social situations with unscripted communication between the participant and an interviewer. Trained raters coded participants on interest, fluency, clarity, focus, affect, grooming, overall conversation, and social appropriateness to produce a global estimate of social skill level for each participant (SSPA-Mean). The SSPA has good test-retest and interrater reliability (8).
Data Analysis
Missing data was less than 10% for all variables. Mann-Whitney U tests were used to compare males and females on PANSS-Expression, PANSS-Experience, Cog-Comp, and SSPA- Mean. A regression-based bootstrapped approach to linear moderation (9) was used to examine gender as a moderator of age differences on these outcomes. This approach produces a confidence interval for the coefficient of the product of the predictor variable and the moderator in a regression equation; if this value is significantly different from zero, there is a significant effect of the moderator. Number of bootstrap samples was set to 5,000. All analyses were conducted using IBM SPSS Version 22.0. We corrected for multiple comparisons using the Benjamini-Hochberg false discovery rate (FDR) procedure (10); FDR was set at 0.10.
Results
See Table 1 for participant demographics and descriptive statistics. Participants were taking the following antipsychotic medications: olanzapine (n=43), risperidone (n=43). haloperidol (n=30), other typical antipsychotics (n=32), clozapine (n=21), quetiapine (n=17), aripiprazole (n=11), and ziprasidone (n=5). Female participants had better cognitive performance and less severe PANSS-Experience symptoms (U= 6814.00, p=.011 and U=4130.50, p=.022, respectively). There were no significant gender differences for SSPA-Mean (U=5,920.50, p=0.150) or PANSS-Expression (U=5125.50, p=.520).
Moderator analyses revealed a significant gender by age interaction for PANSS-Expression (b= −.04; 95% CI [−.0780, −.0114]; bootstrap p=.009). Among men, age was associated with more severe expressive deficits, while among women, there was a trend indicating that age was associated with less severe expressive deficits. (See Figure 1 in supplemental materials for visual representation of this interaction.) Gender was not a significant moderator in any other analyses (all t<1.5, all p>0.15).
Figure 1. Negative Symptoms by Age in Men and Women.
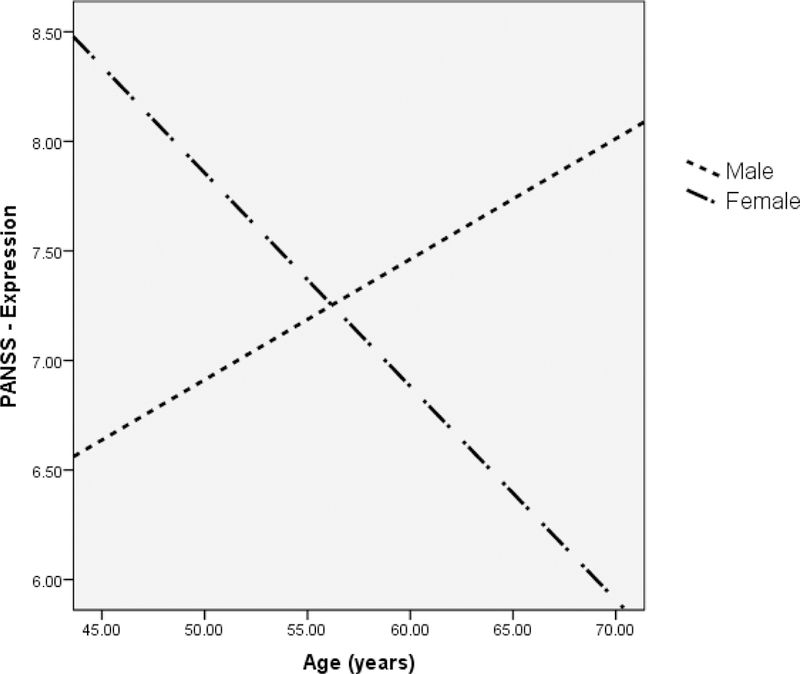
Notes. PANSS= Positive and Negative Syndrome Scale. PANSS Expression scores can range from 4 to 28. Item totals are displayed, with higher scores reflecting more severity; however, factor scores were used for all analyses.
Discussion
The present study examined gender differences in negative symptoms, neurocognition, and social skills in community-dwelling middle-aged and older adults with schizophrenia. Previous studies on gender differences in negative symptoms have yielded mixed results; our study is the first to examine two empirically-validated negative symptom factors. We found a significant gender difference on experiential, but not expressive, negative symptoms. Women with schizophrenia in the sample were less likely to exhibit active socioemotional withdrawal and avoidance; this is consistent with comparisons of older men and women in the general population (11).
Women in the sample exhibited better cognitive functioning than men. There was no significant gender by age interaction, indicating that both middle-aged and older women exhibited, on average, better cognitive function than their same-age male counterparts. This contrasts with a previous study comparing institutionalized older men and women with schizophrenia, which found no gender differences in cognition (3), though individuals with schizophrenia who live in institutions generally have very poor cognitive function, which might produce a floor effect that makes detection of group differences less likely. Importantly, institutionalized patients live in a restrictive environment and experience an associated lack of cognitive stimulation. These findings may speak to the importance of cognitive reserve capacity for women with schizophrenia: better cognitive function through youth and early middle-age, putatively mediated by the neuroprotective effects of estrogen and opportunities for cognitive stimulation, could provide a buffer against the effects of age-associated declines in estrogen in older adulthood.
Male and female participants did not significantly differ on social skills performance, consistent with what has been found in previous studies of middle-aged and older adults (4–5) and in contrast with what has been found with young adults with schizophrenia where women exhibit better social functioning than men (1). Thus, gender differences in social skills may attenuate between young adulthood and middle age among individuals with schizophrenia. With later age of onset, women with schizophrenia have more time than males, on average, for skills development in adolescence, contributing to better social functioning in young adulthood. This social advantage may diminish over time as women with schizophrenia live for longer with the illness and experience associated isolation and cumulative declines in social status and functioning.
Regarding expressive deficits such as flat affect and alogia, older age was associated with more severe expressive deficits for men but not women. Longitudinal evidence is needed to investigate whether women with schizophrenia experience a decrease in expressive negative symptoms in older age. Given that this was the only significant age by gender interaction, and that it indicated potentially better outcomes for women than men with age, the present study does not provide evidence to support the hypothesis that decreases in circulating estrogens with age is associated with worsening outcomes among women. Longitudinal evidence with more precise measurement of menopausal status is required to draw firm conclusions about the effects of the transition through menopause.
The study had other important limitations. First it was a cross-sectional study; longitudinal evidence is needed to clarify the impact of age and gender on outcomes over time. In addition the study was a post-hoc analysis with multiple comparisons, increasing risk for Type I error, though we corrected for this using the Benjamini-Hochberg procedure. Additionally we did not have data on lifetime antipsychotic exposure or current antipsychotic dose, which may have influenced group differences.
Nonetheless, together with previous literature, the present study indicates that gender differences on symptom and functional outcomes in schizophrenia may vary by age group and residential status (institutionalized versus community-dwelling). Gender differences on negative symptoms vary by symptom subgroup; future research examining gender differences on negative symptoms requires use of specific and empirically validated symptom factors.
Supplementary Material
Sources of support:
This research was funded by NIMH grant MH 63116 to Dr. Harvey and by the U.S. Department of Veterans Affairs VISN 3 MIRECC. This manuscript is result of work supported by the U.S. Departments of Veterans Affairs Rehabilitation Research and Development Career Development Award IK2RX002339 and with resources and the use of facilities at the U.S. Department of Veterans Affairs VISN 5 MIRECC. This work reflects the authors’ personal views and in no way represents the official view of the Department of Veterans Affairs or the U.S. Government.
Footnotes
Conflict of interest:
Dr. Muralidharan has no conflicts of interest to report with regard to this work. Dr. Harvey has received consulting fees or travel reimbursements from Allergan, Boehringer Ingelheim, Lundbeck Pharma, Minerva Pharma, Otsuka Digital Health, Sanofi Pharma, Sunovion Pharma, and Takeda Pharma during the past year. He has a research grant from Takeda and from the Stanley Medical Research Foundation. Dr. Bowie has received consulting fees from Boehringer Ingelheim, Lundbeck Pharma, Otsuka Digital Health, and Takeda Pharma. He has received grant support from Lundbeck, Pfizer, and Takeda.
Previous presentation:
This data was partially previously presented at the 2018 Annual Meeting for the American Association for Geriatric Psychiatry, Honolulu, HI, March 15–18, 2018.
References
- 1.Ochoa S, Usall J, Cobo J, et al. : Gender differences in schizophrenia and first-episode psychosis: a comprehensive literature review. Schizophrenia Research and Treatment 2012; doi: 10.1155/2012/916198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Searles S, Makarewicz JA, Dumas JA: The role of estradiol in schizophrenia diagnosis and symptoms in postmenopausal women. Schizophrenia Research 2017; June 3 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Moriarty PJ, Lieber D, Bennett A, et al. : Gender differences in poor outcome schizophrenia. Schizophrenia Bulletin 2001; 27:103–113 [DOI] [PubMed] [Google Scholar]
- 4.Sitzer DI, Twamley EW, Patterson TL, et al. : Multivariate predictors of social skills performance in middle-aged and older out-patients with schizophrenia spectrum disorders. Psychological Medicine 2008; 38(5):755–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mueser KT, Pratt SI, Bartels SJ, et al. : Neurocognition and social skill in older persons with schizophrenia and major mood disorders: an analysis of gender and diagnosis effects. Journal of Neurolinguistics; 2010; 23(3):297–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey PD, Khan A, Keefe RS: Using the PANSS to define different domains of negative symptoms: prediction of everyday functioning by impairments in emotional expression and emotional experience. Innov Clin Neurosci 2017; 14(11–12):18–22 [PMC free article] [PubMed] [Google Scholar]
- 7.Bowie CR, Reichenberg A, Patterson TL, et al. : Determinants of real-world functional performance in schizophrenia subjects: correlations with cognition, functional capacity, and symptoms. American Journal of Psychiatry 2006; 163(3):418–25 [DOI] [PubMed] [Google Scholar]
- 8.Patterson TL, Moscona S, McKibbin CL, et al. : Social skills performance assessment among older patients with schizophrenia. Schizophrenia Research 2001; 48(2):351–60 [DOI] [PubMed] [Google Scholar]
- 9.Hayes AF: Introduction to Mediation, Moderation, And Conditional Process Analysis: A Regression-Based Approach. New York, NY, Guilford Press, 2013 [Google Scholar]
- 10.Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, Series B (Methodological), 57, 289–300. doi: 10.2307/2346101 [DOI] [Google Scholar]
- 11.Antonucci TC, Ajrouch KJ, Birditt KS: The convoy model: explaining social relations from a multidisciplinary perspective. The Gerontologist 2014; 54(1):82–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


