Abstract
Objective
To examine the association between lipid levels and hemorrhagic stroke risk among women.
Methods
We performed a prospective cohort study among 27,937 women enrolled in the Women's Health Study with measured total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C), as well as triglycerides. Strokes were confirmed by medical record review. We used Cox proportional hazards models to analyze associations between lipid categories and hemorrhagic stroke risk.
Results
During a mean of 19.3 years of follow-up, 137 hemorrhagic strokes occurred. Compared to those with LDL-C levels 100–129.9 mg/dL, after multivariable adjustment, those with LDL-C levels <70 mg/dL had 2.17 times the risk (95% confidence interval [CI] 1.05, 4.48) of experiencing a hemorrhagic stroke. No significant increase in risk was seen for those with LDL-C levels 130–159.9 mg/dL (relative risk [RR] 1.14; 95% CI 0.72, 1.80) or 70–99.9 mg/dL (RR 1.25; 95% CI 0.76, 2.04). There was a suggestion, although not significant, of increased risk for those with LDL-C levels ≥160 mg/dL (RR 1.53; 95% CI 0.92, 2.52). Women in the lowest quartile of triglycerides had a significantly increased risk of hemorrhagic stroke compared to women in the top quartile after multivariable adjustment (RR 2.00; 95% CI 1.18, 3.39). We observed no significant associations between total cholesterol or HDL-C levels and hemorrhagic stroke risk.
Conclusion
LDL-C levels <70 mg/dL and low triglyceride levels were associated with increased risk of hemorrhagic stroke among women.
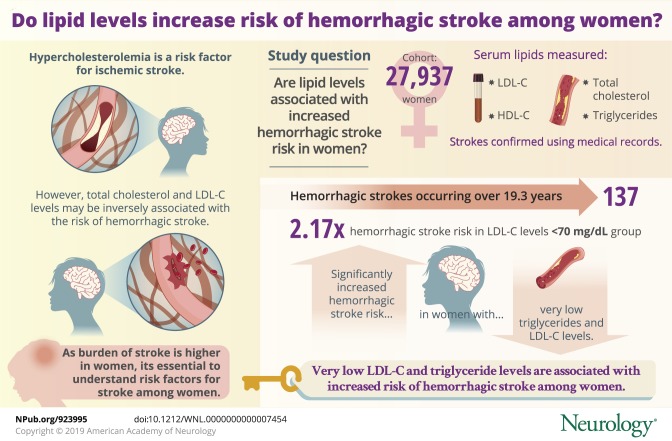 Hypercholesterolemia is a risk factor for ischemic stroke.1,2 However, a meta-analysis observed that total and low-density lipoprotein cholesterol (LDL-C) levels are inversely associated with the risk of hemorrhagic stroke, while no association was seen for high-density lipoprotein cholesterol (HDL-C).3 In addition, a meta-analysis of statin trials observed that a 1 mmol/L (or 38.67 mg/dL) reduction in LDL-C was associated with a 15% increased risk of hemorrhagic stroke.4 Results of other studies have also suggested that low triglyceride levels may increase hemorrhagic stroke risk.5–7 Because lipid-lowering strategies are widely used for prevention of cardiovascular disease, there is interest in whether low lipid levels, particularly total cholesterol, LDL-C, and triglycerides, increase risk of hemorrhagic stroke.
Hypercholesterolemia is a risk factor for ischemic stroke.1,2 However, a meta-analysis observed that total and low-density lipoprotein cholesterol (LDL-C) levels are inversely associated with the risk of hemorrhagic stroke, while no association was seen for high-density lipoprotein cholesterol (HDL-C).3 In addition, a meta-analysis of statin trials observed that a 1 mmol/L (or 38.67 mg/dL) reduction in LDL-C was associated with a 15% increased risk of hemorrhagic stroke.4 Results of other studies have also suggested that low triglyceride levels may increase hemorrhagic stroke risk.5–7 Because lipid-lowering strategies are widely used for prevention of cardiovascular disease, there is interest in whether low lipid levels, particularly total cholesterol, LDL-C, and triglycerides, increase risk of hemorrhagic stroke.
Although prior studies have observed increased risk of hemorrhagic stroke with low lipid levels, several important questions remain. Most studies did not present sex-stratified results due to low numbers of events among women. Since the burden of stroke is considered to be higher in women than men,8 it is particularly important to understand risk factors for stroke among women. In addition, most studies have not explored whether the association with lipid levels varies by hemorrhagic stroke subtype. Finally, most prior studies had limited numbers of individuals with elevated lipid levels and did not specifically compare hemorrhagic stroke risk among those with elevated lipid levels to those with optimal or near optimal lipid levels.
We evaluated the association between lipid levels (total cholesterol, LDL-C, triglycerides, and HDL-C) and risk of hemorrhagic stroke in a large prospective cohort of women.
Methods
The design and main findings of the Women's Health Study (WHS) have been described in detail previously.9,10 In brief, the WHS was a randomized, double-blind, placebo-controlled trial of low-dose aspirin and vitamin E for the primary prevention of cardiovascular disease and cancer among 39,876 US female health professionals aged 45 years or older. The trial ended in March 2004, but observational follow-up of willing participants is ongoing.
Twice in the first year and yearly thereafter, women were asked to complete a questionnaire assessing disease endpoints, including stroke.
Biomarker measurements
Prior to randomization, women who agreed to provide a fasting venous blood sample were mailed a blood collection kit containing EDTA tubes. A core laboratory certified by the National Heart, Lung and Blood Institute/Centers for Disease Control and Prevention Lipid Standardization program measured levels of total cholesterol, HDL-C, LDL-C, and triglycerides in the plasma samples.11
Outcome ascertainment
Participants who reported a stroke on the annual follow-up questionnaires were asked for permission to review their medical records. An Endpoints Committee of physicians, including a board-certified vascular neurologist, reviewed the records to confirm events. A nonfatal stroke was defined as a focal neurologic deficit of sudden or rapid onset and vascular mechanism that lasted > 24 hours. In the event of a fatal stroke, all available sources, including death certificates and hospital records, were used to confirm the event. The committee recorded the date of each stroke event and also classified confirmed events into ischemic, hemorrhagic, and unknown types. Hemorrhagic strokes were further classified into intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), or intraventricular hemorrhage (IVH). Interobserver agreement for the 3 stroke subtypes is very high (kappa = 0.94).12 We counted only confirmed first hemorrhagic strokes for our analyses.
Statistical analysis
Of the 28,345 blood samples we received, 27,937 samples could be analyzed for levels of LDL-C, HDL-C, total cholesterol, and triglycerides. We created categories for LDL-C, HDL-C, and total cholesterol according to Adult Treatment Panel III guidelines.13,14 Triglycerides were categorized into quartiles by fasting status. We used Cox proportional hazards models to calculate the hazard ratio, a measure of the relative risk (RR), and 95% confidence intervals (CI) of incident hemorrhagic stroke events. Individuals contributed person-time from study entry until first stroke event, loss to follow-up, or end of study, whichever occurred first. We tested the proportional hazards assumption by including an interaction term between the log transformation time and lipid categories and found no significant violation.
We calculated age- and multivariable-adjusted RRs for the association between lipids levels and hemorrhagic stroke. Our multivariable model adjusted for covariates potentially leading to confounding based on prior literature including age; smoking status (current vs past/never); menopausal status and use (premenopausal, postmenopausal and no PMH use, postmenopausal and use PMH, uncertain menopausal status); body mass index (underweight [<18.5 kg/m2], normal weight [18.5−<24.9 kg/m2], overweight [25–29.9 kg/m2], obese [≥30 kg/m2]); alcohol consumption (none, 0.1–4.9 g/d, ≥5 g/d); history of diabetes (yes/no); history of hypertension (yes/no); treatment with cholesterol-lowering medication (yes/no); physical activity (quartiles); and randomized treatment assignment. Fewer than 100 participants were missing information on any covariate and those with missing information were imputed to the most common category.
We also assessed the association between LDL-C, HDL-C, total cholesterol, and triglycerides and hemorrhagic stroke subtypes, specifically ICH and SAH. We performed sensitivity analyses in which we excluded hemorrhagic strokes due to a procedure or that occurred while the participant was receiving anticoagulants. We also performed additional analyses in which we restricted our study to those women who did not report taking cholesterol-lowering medications at baseline. Finally, we performed an analysis in which we categorized non-HDL-C into quartiles and examined the association between non-HDL-C and risk of hemorrhagic stroke.
Data availability statement
The dataset analyzed in this study is not publicly available because of restricted access but further information about the dataset is available from the corresponding author on reasonable request.
Standard protocol approvals, registrations, and patient consents
All participants provided written informed consent and the institutional review board of Brigham and Women's Hospital approved the WHS (registered at clinicaltrials.gov NCT00000479).
Results
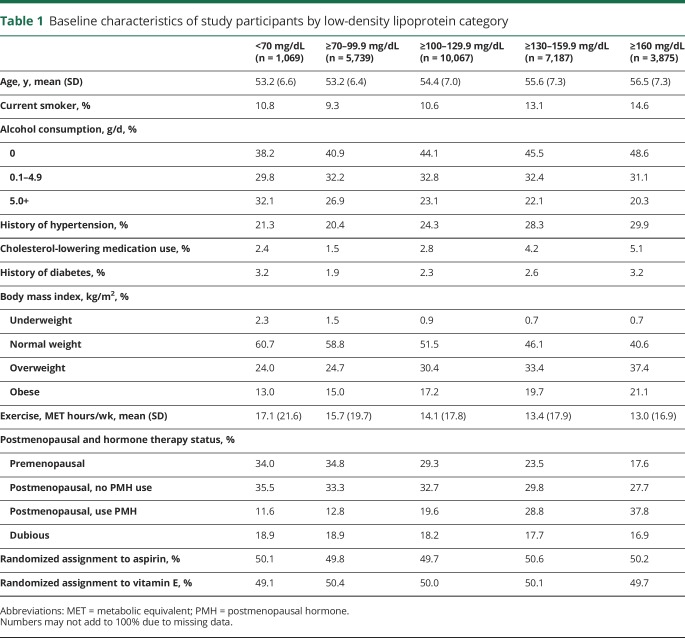
Table 1 displays the baseline characteristics of the study participants by LDL-C category. Those in the lowest LDL-C category (<70 mg/dL) were younger, less likely to have a history of hypertension, and to use cholesterol-lowering medications, and more likely to consume alcohol, be normal weight, be physically active, and to be premenopausal than those with cholesterol levels of 100–129.9 mg/dL (referent). Those in the highest LDL-C category (≥160 mg/dL) were older, more likely to smoke, to use cholesterol-lowering medications and postmenopausal hormones, to have a history of hypertension or diabetes, and to be obese, and less likely to consume alcohol or be physically active than those with cholesterol levels of 100–129.9 mg/dL.
Table 1.
Baseline characteristics of study participants by low-density lipoprotein category
During a mean of 19.3 years of follow-up, 137 incident hemorrhagic stroke events were confirmed (85 ICH, 43 SAH, 3 IVH, 3 combination ICH/SAH, and 3 hemorrhagic strokes due to a procedure).
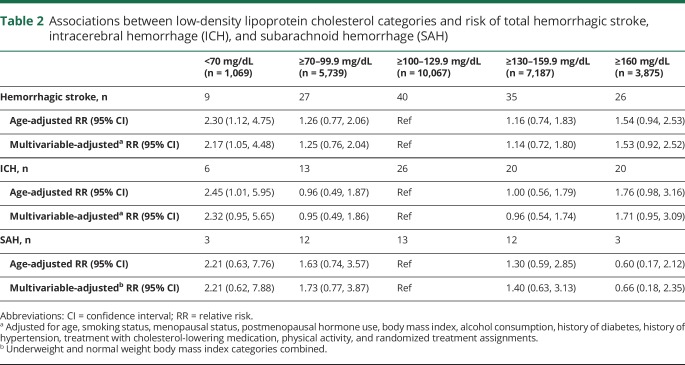
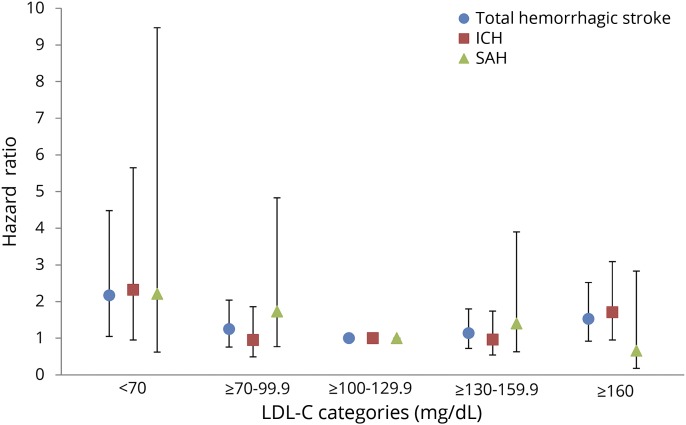
There was a U-shaped relationship between LDL-C and hemorrhagic stroke risk (table 2 and figure). After multivariable adjustment, compared to those with LDL-C levels 100–129.9 mg/dL, those with LDL-C level <70 mg/dL had 2.17 times the risk (95% CI 1.05, 4.48) of experiencing a hemorrhagic stroke. There was a suggestion of elevated risk among those with LDL-C level ≥160 mg/dL (RR 1.53; 95% CI 0.92, 2.52), but this increase was not statistically significant. Those with LDL-C levels 70–99.9 mg/dL or with LDL-C levels 130–159.9 mg/dL did not have a significantly increased risk of hemorrhagic stroke (RR 1.25; 95% CI 0.76, 2.04 and RR 1.14; 95% CI 0.72, 1.80, respectively).
Table 2.
Associations between low-density lipoprotein cholesterol categories and risk of total hemorrhagic stroke, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH)
Figure. Multivariate adjusted associations between low-density lipoprotein cholesterol (LDL-C) categories and risk of total hemorrhagic stroke, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH).
Results for the ICH subtype were similar to those seen for total hemorrhagic stroke with the highest risks of events occurring among those with LDL-C <70 mg/dL followed by those with LDL-C ≥160 mg/dL (table 2). For SAH, the highest risk was observed for those with LDL-C <70 mg/dL (RR 2.21; 95% CI 0.62, 7.88) but this increase in risk was not statistically significant.
Those with LDL-C ≥ 160 mg/dL did not have an increased risk of SAH (RR 0.66; 95% CI 0.18, 2.35). The low number of SAH events in this cohort resulted in unstable estimates of the association between LDL-C levels and the risk of SAH.
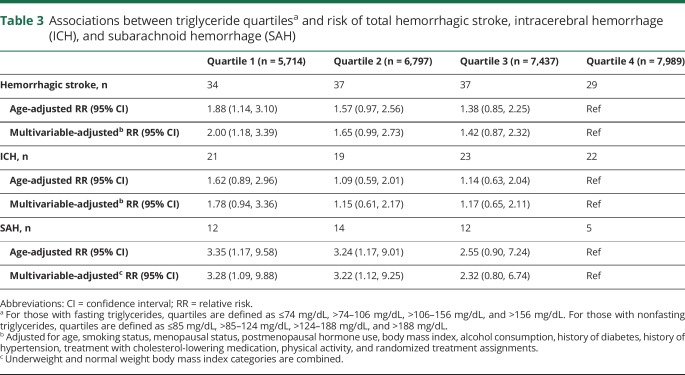
Women in the lowest quartile of triglycerides (≤74 mg/dL for fasting and ≤85 mg/dL for nonfasting) had a significantly increased risk of hemorrhagic stroke compared to those in the top quartile after multivariable adjustment (RR 2.00; 95% CI 1.18, 3.39) (table 3). Other quartiles were not associated with significant increases in risk. When examining hemorrhagic stroke subtypes, low triglyceride levels were associated with a significant risk of SAH but not with a significantly increased risk of ICH.
Table 3.
Associations between triglyceride quartilesa and risk of total hemorrhagic stroke, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH)
Finally, we constructed a model including both LDL-C categories (<70, 70–99.9, 100–129.9, 130–159.9, ≥160 mg/dL) and triglyceride quartiles. Those in the lowest triglyceride quartile had an increased risk of hemorrhagic stroke (RR 2.14; 95% CI 1.24, 3.70) compared to those in the highest quartile after controlling for LDL-C. In addition, those with LDL-C <70 mg/dL (RR 2.04; 95% CI 0.98, 4.23) and those with LDL-C ≥160 mg/dL (RR 1.75; 95% CI 1.05, 2.92) had an increased risk of hemorrhagic stroke compared to those with LDL-C 100–129.9 mg/dL after controlling for triglycerides.
We observed similar associations for all analyses after excluding hemorrhagic stroke cases due to an infarct or procedure (n = 3) and after excluding cases on anticoagulant treatment (warfarin, heparin) at the time of the event (n = 17) (results not shown). Our analyses restricted to women who were not on cholesterol-lowering medications at baseline (n = 27,044) showed similar results as our main analyses although the increased risk among those with LDL-C <70 mg/dL was no longer statistically significant. We observed no significant associations between non-HDL-C quartiles and risk of hemorrhagic stroke (results not shown).
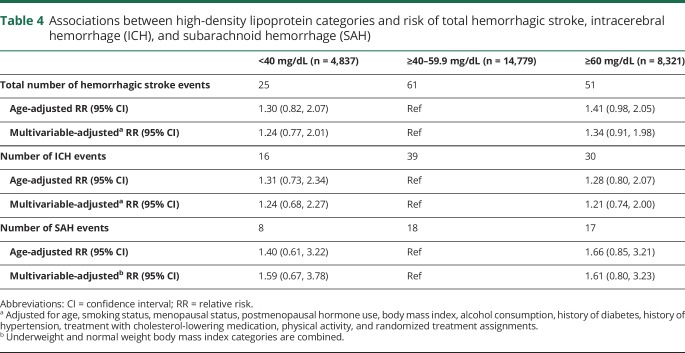
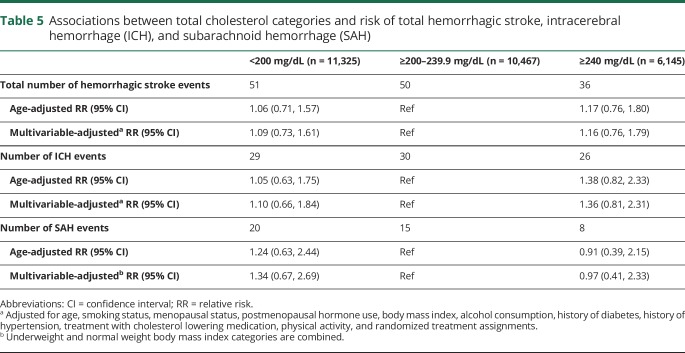
We observed no significant associations between HDL-C or total cholesterol and risk of hemorrhagic stroke (tables 4 and 5). After multivariate adjustment, compared to those with HDL-C levels 40–59.9 mg/dL, those with <40 mg/dL had 1.24 times the risk (95% CI 0.77, 2.01) and those with ≥60 mg/dL had 1.34 times the risk (95% CI 0.91, 1.98) of hemorrhagic stroke. After multivariate adjustment, compared to those with total cholesterol levels 200–239.9 mg/dL, those with <200 mg/dL had 1.09 times the risk (95% CI 0.73, 1.61) and those with ≥240 mg/dL had 1.16 times the risk (95% CI 0.76, 1.79) of hemorrhagic stroke.
Table 4.
Associations between high-density lipoprotein categories and risk of total hemorrhagic stroke, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH)
Table 5.
Associations between total cholesterol categories and risk of total hemorrhagic stroke, intracerebral hemorrhage (ICH), and subarachnoid hemorrhage (SAH)
Discussion
In this large prospective cohort of middle-aged to elderly women, we found increased risk of hemorrhagic stroke among those with LDL-C <70 mg/dL and a potential increase in risk among those with LDL-C ≥160 mg/dL. We also observed an increased risk of hemorrhagic stroke, specifically SAH, among those with low triglyceride levels. We did not observe associations between total cholesterol or HDL-C and risk of hemorrhagic stroke. Few prior studies have examined the association between LDL-C levels and the risk of hemorrhagic stroke and the populations enrolled in each study have varied. Two studies enrolled elderly men and women and observed no association between LDL-C levels and the risk of ICH.6,7 Another study of 116 ICH events among US men and women enrolled in the Atherosclerosis Risk in Communities Study and the Cardiovascular Health Study observed that those in the top quartile of LDL-C levels (>158.8 mg/dL) had a lower risk of hemorrhagic stroke (RR 0.52; 95% CI 0.31, 0.88) compared to those in the bottom 3 quartiles (≤159 mg/dL).5 Two other studies were performed in Japanese populations where hemorrhagic strokes are a larger proportion of the total stroke burden. One study observed no significant association between LDL-C levels and risk of hemorrhagic stroke (80 events),15 and the other observed that those with higher levels of LDL-C (≥80 mg/dL) had a significantly decreased risk of death due to intraparenchymal hemorrhage (264 deaths) compared to those with low levels of LDL-C (<80 mg/dL).16
In contrast to some of the prior studies, our study enrolled only women who were primarily white, making this the one of the largest studies of lipid levels and hemorrhagic stroke risk among women to date. Similar to some studies, we observed an increased risk of hemorrhagic stroke among those with low triglyceride levels and among those with very low levels of LDL-C (<70 mg/dL). The mechanisms by which low triglyceride and LDL-C levels increase risk of hemorrhagic stroke are not fully known but it is thought that low cholesterol may result in arterial medial layer smooth muscle cell necrosis17 and that the impaired endothelium may be more susceptible to microaneursyms,3 which are often found in ICH patients.18 Our results also suggest that there may be an increased risk of hemorrhagic stroke among those with substantially elevated LDL-C (≥160 mg/dL) compared to those with LDL-C levels from 100 to 129.9 mg/dL although this increase in risk was not statistically significant. Some prior studies had lower distributions of LDL-C levels than our study, preventing them being able to examine risk of hemorrhagic stroke among those with substantially elevated LDL-C. The low number of cases among those with elevated LDL-C levels in prior studies may have also limited their ability to detect an increased risk of hemorrhagic stroke. In addition, most studies used the lowest quartile of LDL-C levels as their reference group and did not specifically compare those participants with substantially elevated LDL-C levels to those participants with LDL-C levels between 100 and 129.9 mg/dL. Concordant with our findings, a recent Mendelian randomization analysis suggested that elevated LDL-C levels may be associated with an increased risk of ICH.19 Other studies have suggested links between arterial stiffness20 or carotid atherosclerosis21 and the risk of cerebral microbleeds, a potential risk factor for ICH.22 It is possible that elevated LDL-C levels may increase the risk of hemorrhagic stroke through their atherosclerotic effects.
Three prospective studies have observed a decreased risk of hemorrhagic stroke with increasing levels of triglycerides.5–7 One of these studies also suggested that the association between triglyceride levels and hemorrhagic stroke may be stronger in men.7 One nested case–control study observed a higher risk of ICH among those with elevated triglyceride levels but this study only observed 27 events in women.23
Similar to a previous meta-analysis,3 we observed no association between HDL-C levels and the risk of hemorrhagic stroke. Although we observed no association between total cholesterol levels and the risk of hemorrhagic stroke, a recent meta-analysis observed that women in the highest category of total cholesterol may have a decreased risk of hemorrhagic stroke compared to women in the lowest category.3 However, many of the individual studies did not find significant associations.24–27 A study among middle-aged Finnish women observed a significant inverse association between total cholesterol and risk of ICH but not SAH.28 One study among Japanese women observed an increased risk of death due to hemorrhagic stroke among those with total cholesterol levels <4.14 mmol/L.29
The association between low LDL-C or triglyceride levels and an increased risk of hemorrhagic stroke seen in some studies led to concern that statins may increase the risk of hemorrhagic stroke events. Two large meta-analyses, one only of randomized controlled trials30 and one of both trials and observational studies,31 concluded that there was no association between statin use and the risk of ICH. In addition, risk of ICH was not associated with achieved LDL-C or reduction in LDL-C, suggesting that any effect of statins on ICH risk may be due to mechanisms independent of their cholesterol-lowering effects; for example, their antithrombotic properties.30 Another meta-analysis using individual patient-level data from statin trials observed a nonsignificant 15% increase in the risk of hemorrhagic stroke, but emphasized that any potential increase in risk of hemorrhagic stroke would be outweighed by the reduction in ischemic stroke and other cardiovascular events, even among individuals at low risk of cardiovascular disease.43 The differences between the statin trials and observational studies such as the one presented here may be due to the different questions the studies address. Statin trials are typically only a few years in duration and examine the effect of a pharmaceutical agent that lowers cholesterol on hemorrhagic stroke risk. In contrast, our observational study may reflect the effect of longer-term exposure to very low LDL-C levels (in the absence of cholesterol-lowering treatment) on vessel wall integrity.
Strengths of this study include the prospective design and the large number of participants. Although hemorrhagic strokes are much less common than ischemic strokes, 137 hemorrhagic strokes occurred in this large cohort, making it one of the larger studies to date on lipid levels and the risk of hemorrhagic stroke. However, some important limitations should be noted. We had limited power for our hemorrhagic stroke subtype analyses. The low number of women who were premenopausal at baseline also prevented us from exploring whether factors like menopausal status may modify the association between lipid levels and risk of hemorrhagic stroke. Lipid levels were only measured at baseline and we were unable to explore how changes in lipid levels over time may modify the risk of hemorrhagic stroke, and rates of usage of statin medications were low (<5%) in this cohort at baseline. Our results may be specific to women, and the cohort was predominantly white. Finally, there is the potential for residual confounding, especially for the analyses where we only adjusted for age due to low numbers of cases.
We observed an association between very low LDL-C levels and low triglycerides levels and an increased risk of hemorrhagic stroke. Women with very low LDL-C or low triglycerides should be monitored for other modifiable risk factors for hemorrhagic stroke, for example, hypertension and smoking, to help reduce their overall risk of experiencing a hemorrhagic stroke event. Additional targeted research is needed to determine if our finding of elevated LDL-C levels (≥160 mg/dL) being associated with an increased risk of hemorrhagic stroke can be replicated in other cohorts and to provide insights on how to reduce hemorrhagic stroke risk in these individuals.
Glossary
- CI
confidence interval
- HDL-C
high-density lipoprotein cholesterol
- ICH
intracerebral hemorrhage
- IVH
intraventricular hemorrhage
- LDL-C
low-density lipoprotein cholesterol
- PMH
postmenopausal hormone
- RR
relative risk
- SAH
subarachnoid hemorrhage
- WHS
Women's Health Study
Footnotes
CME Course: NPub.org/cmelist
Authors contributions
Pamela M. Rist: drafting and revising the manuscript for content, including medical writing for content; study concept or design; analysis and interpretation of data. J.E. Buring: obtaining funding; interpretation of data; revising the manuscript for content. Paul M. Ridker: interpretation of data and revising the manuscript for content. C.S. Kase: interpretation of data and revising the manuscript for content. T. Kurth: interpretation of data; study concept or design; revising the manuscript for content; supervision. Kathryn M. Rexrode: interpretation of data; study concept or design; revising the manuscript for content; supervision.
Study funding
The Women's Health Study is funded by CA047988, HL043851, HL080467, HL099355, and UM1 CA182913. Dr. Rist is funded by K01 HL128791.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Meschia JF, Bushnell C, Boden-Albala B, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:3754–3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology 2007;68:556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke 2013;44:1833–1839. [DOI] [PubMed] [Google Scholar]
- 4.Cholesterol Treatment Trialists' (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 2012;380:581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sturgeon JD, Folsom AR, Longstreth WT Jr, Shahar E, Rosamond WD, Cushman M. Risk factors for intracerebral hemorrhage in a pooled prospective study. Stroke 2007;38:2718–2725. [DOI] [PubMed] [Google Scholar]
- 6.Wieberdink RG, Poels MMF, Vernooij MW, et al. Serum lipid levels and the risk of intracerebral hemorrhage: the Rotterdam Study. Arterioscler Thromb Vasc Biol 2011;31:2982–2989. [DOI] [PubMed] [Google Scholar]
- 7.Bonaventure A, Kurth T, Pico F, et al. Triglycerides and risk of hemorrhagic stroke vs. ischemic vascular events: the Three-City Study. Atherosclerosis 2010;210:243–248. [DOI] [PubMed] [Google Scholar]
- 8.Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol 2008;7:915–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293–1304. [DOI] [PubMed] [Google Scholar]
- 10.Lee IM, Cook NR, Gaziano JM, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women's Health Study: a randomized controlled trial. JAMA 2005;294:56–65. [DOI] [PubMed] [Google Scholar]
- 11.Kurth T, Ridker PM, Buring JE. Migraine and biomarkers of cardiovascular disease in women. Cephalalgia 2008;28:49–56. [DOI] [PubMed] [Google Scholar]
- 12.Atiya M, Kurth T, Berger K, Buring JE, Kase CS; Women's Health Study. Interobserver agreement in the classification of stroke in the Women's Health Study. Stroke 2003;34:565–567. [DOI] [PubMed] [Google Scholar]
- 13.National Cholesterol Education Program. ATP III Guidelines At-a-glance: Quick Desk Reference. Bethesda: National Heart, Lung, and Blood Institute; 2001. [Google Scholar]
- 14.Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. J Am Coll Cardiol 2004;44:720–732. [DOI] [PubMed] [Google Scholar]
- 15.Imamura T, Doi Y, Arima H, et al. LDL cholesterol and the development of stroke subtypes and coronary heart disease in a general Japanese population. Stroke 2009;40:382–388. [DOI] [PubMed] [Google Scholar]
- 16.Noda H, Iso H, Irie F, et al. Low-density lipoprotein cholesterol concentrations and death due to intraparenchymal hemorrhage. Circulation 2009;119:2136–2145. [DOI] [PubMed] [Google Scholar]
- 17.Ooneda G, Yoshida Y, Suzuki K, et al. Smooth muscle cells in the development of plasmatic arterionecrosis, arteriosclerosis, and arterial contraction. Blood Vessels 1978;15:148–156. [DOI] [PubMed] [Google Scholar]
- 18.Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT Jr, Psaty BM. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology 2004;63:1868–1875. [DOI] [PubMed] [Google Scholar]
- 19.Akoudad S, Ikram MA, Portegies MLP, et al. Genetic loci for serum lipid fractions and intracerebral hemorrhage. Atherosclerosis 2016;246:287–292. [DOI] [PubMed] [Google Scholar]
- 20.Ochi N, Tabara Y, Igase M, et al. Silent cerebral microbleeds associated with arterial stiffness in an apparently healthy subject. Hypertens Res 2009;32:255–260. [DOI] [PubMed] [Google Scholar]
- 21.Romero JR, Preis SR, Beiser A, et al. Carotid atherosclerosis and cerebral microbleeds: the Framingham heart study. J Am Heart Assoc 2016;5:e002377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akoudad S, Portegies ML, Koudstaal PJ, et al. Cerebral microbleeds are associated with an increased risk of stroke: the Rotterdam study. Circulation 2015;132:509–516. [DOI] [PubMed] [Google Scholar]
- 23.Zia E, Pessah-Rasmussen H, Khan FA, et al. Risk factors for primary intracerebral hemorrhage: a population-based nested case-control study. Cerebrovasc Dis 2006;21:18–25. [DOI] [PubMed] [Google Scholar]
- 24.Knekt P, Reunanen A, Aho K, et al. Risk factors for subarachnoid hemorrhage in a longitudinal population study. J Clin Epidemiol 1991;44:933–939. [DOI] [PubMed] [Google Scholar]
- 25.Gatchev O, Råstam L, Lindberg G, Gullberg B, Eklund GA, Isacsson SO. Subarachnoid hemorrhage, cerebral hemorrhage, and serum cholesterol concentration in men and women. Ann Epidemiol 1993;3:403–409. [DOI] [PubMed] [Google Scholar]
- 26.Iribarren C, Jacobs DR, Sadler M, Claxton AJ, Sidney S. Low total serum cholesterol and intracerebral hemorrhagic stroke: is the association confined to elderly men? The Kaiser Permanente Medical Care Program. Stroke 1996;27:1993–1998. [DOI] [PubMed] [Google Scholar]
- 27.Okumura K, Iseki K, Wakugami K, et al. Low serum cholesterol as a risk factor for hemorrhagic stroke in men: a community-based mass screening in Okinawa, Japan. Jpn Circ J 1999;63:53–58. [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Total and high-density lipoprotein cholesterol and stroke risk. Stroke 2012;43:1768–1774. [DOI] [PubMed] [Google Scholar]
- 29.Nago N, Ishikawa S, Goto T, Kayaba K. Low cholesterol is associated with mortality from stroke, heart disease, and cancer: the Jichi Medical School Cohort Study. J Epidemiol 2011;21:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McKinney JS, Kostis WJ. Statin therapy and the risk of intracerebral hemorrhage: a meta-analysis of 31 randomized controlled trials. Stroke 2012;43:2149–2156. [DOI] [PubMed] [Google Scholar]
- 31.Hackam DG, Woodward M, Newby LK, et al. Statins and intracerebral hemorrhage: collaborative systematic review and meta-analysis. Circulation 2011;124:2233–2242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed in this study is not publicly available because of restricted access but further information about the dataset is available from the corresponding author on reasonable request.