Abstract
Background
Contrast-induced acute kidney injury (CI-AKI) contributes toward unfavorable clinical outcomes. Oral hydration with water is inexpensive and it may be effective in the prevention of CI-AKI, but its efficacy among patients undergoing primary percutaneous coronary intervention (PCI) remains unknown.
Methods/design
Our study is a secondary analysis on the database from the ATTEMPT study. We enrolled ST-elevation myocardial infarction (STEMI) patients undergoing primary PCI. Eligible patients received peri-procedural aggressive (left ventricular end-diastolic pressure-guided) or routine (≤ 500 mL) intravenous hydration with an isotonic solution (0.9% NaCl) with randomization. The primary endpoint was CI-AKI, defined as a > 25% or 0.5 mg/dL increase in serum creatinine from baseline during the first 48–72 h post-procedurally. All patients drank unrestricted amounts of fluids freely, the volume of which was recorded until 24 h following primary PCI. Oral hydration volume/weight (OHV/W) ratios were calculated. The association between post-procedural oral hydration (quartiles) and CI-AKI was assessed using multivariable analysis controlling for confounders, including intravenous hydration strategies.
Discussion
Our study determined the effects of post-procedural oral hydration on CI-AKI following primary PCI, which is a potential strategy for CI-AKI prevention among patients with STEMI at very high risk.
Trial registration
ClinicalTrials.gov, NCT02067195. Registered on 21 February 2014.
Electronic supplementary material
The online version of this article (10.1186/s13063-019-3413-5) contains supplementary material, which is available to authorized users.
Keywords: Primary percutaneous coronary intervention, Contrast-induced acute kidney injury, Oral hydration, ST-elevation myocardial infarction, Contrast media
Background
Patients with ST-elevation myocardial infarction (STEMI) have a higher risk of contrast-induced acute kidney injury (CI-AKI) [1, 2]. CI-AKI is a potentially serious complication of angiographic procedures and can constitute up to 10% of hospital-acquired acute kidney injury [3]. Severe acute kidney injury requires renal replacement therapy and results in increased morbidity and mortality, prolonged hospitalization, and overall increased healthcare costs [4–6]. Of concern, 14.5% of the patients undergoing cardiac catheterization develop CI-AKI; reports have shown a 50% incidence in high-risk patients [7, 8]. CI-AKI is associated with poorer outcomes, even in STEMI patients without impaired left ventricular ejection fraction (LVEF) and with normal renal function [9, 10].
According to the 2018 ESC/EACTS guidelines on myocardial revascularization, prophylactic hydration is recommended in high-risk patients [11]. Previous meta-analyses focusing on different types of procedures (cardiac catheterization, enhanced computed tomography scans, angiography for peripheral vascular disease, and so on) have suggested that oral hydration may be as effective as intravenous hydration in preventing CI-AKI [12, 13]. Conflicting results have arisen regarding whether oral hydration prevents CI-AKI. Previous studies have been conducted on relatively low-risk patients, including those subjects undergoing intravenous radiographic procedures or elective percutaneous coronary intervention (PCI). Optimal evidence for an oral hydration strategy has not been well established in a high-risk population such as STEMI patients undergoing primary PCI.
Given the data, we designed this study to evaluate the efficacy of post-procedural oral hydration for CI-AKI prevention in high-risk patients with STEMI undergoing primary PCI.
Methods
Study design and population
This is a secondary analysis of the Aggressive Hydration in Patients with ST-Elevation Myocardial Infarction undergoing Primary Percutaneous Coronary Intervention to Prevent Contrast-induced Nephropathy, the First Study for Reduction of Contrast-induced Nephropathy following Cardiac Catheterization (ATTEMPT RESCIND-1) study. Patients aged ≥ 18 years with STEMI undergoing primary PCI who provided written informed consent are included from 15 academic medical centers in China. Patients are excluded for the following reasons: 1) contrast medium administration within the previous 7 days; 2) end-stage renal failure or renal transplantation; 3) inferior and/or right ventricle myocardial infarction combined with hypotension (defined as systolic pressure ≤ 90 mmHg) on admission; 4) pre-procedural renal insufficiency (history of chronic kidney disease or estimated glomerular filtration rate ≤ 60 mL/min/1.73 m2 calculated using the level-modified Modification of Diet in Renal Disease formula); 5) cardiogenic shock or New York Heart Association functional classification IV; 6) acute kidney injury defined as an absolute serum creatinine increase of 0.5 mg/dL from baseline obtained in the previous 24 h; 7) lactation; 8) pregnancy; 9) malignant tumor or life expectancy < 1 year; 10) allergy to contrast; 11) peri-procedural administration of nonsteroidal anti-inflammatory drugs, aminoglycosides, cyclosporine, or cisplatin in the previous 48 h or during the study period; 12) planned renal catheterization; or 13) heart valve surgery [14].
Study protocol
All eligible participants will receive peri-procedural intravenous hydration of different regimens. Oral hydration will begin at an unlimited rate until 24 h after the coronary procedure. By monitoring the fluid status, the rate and duration of oral intake, as well as the use of diuretics, are based on the clinical evaluation for heart function and at the discretion of the cardiologists.
Additionally, oral hydration volume/weight (OHV/W) ratios will be calculated. To determine the efficacy of oral hydration, we will collect data on the type of water taken, the volume per hour of water (mL), the duration in the 24 h after the procedure, and any use of diuretics. Additionally, the urine output per hour of the patients will be observed. Hemodynamic data will be obtained in various clinical settings to assess volume status and guide medical therapy, including the administration of intravenous fluids.
Follow-up events will be carefully monitored and recorded by trained investigators through office visits and telephone interviews at 3, 6, 12, 18, and 24 months after primary PCI. All data will be collected using standardized electronic case report forms. At the time of data entry, the data management team of Guangdong General Hospital will perform consistency checks and issue electronic data clarification forms to follow-up on discrepant data.
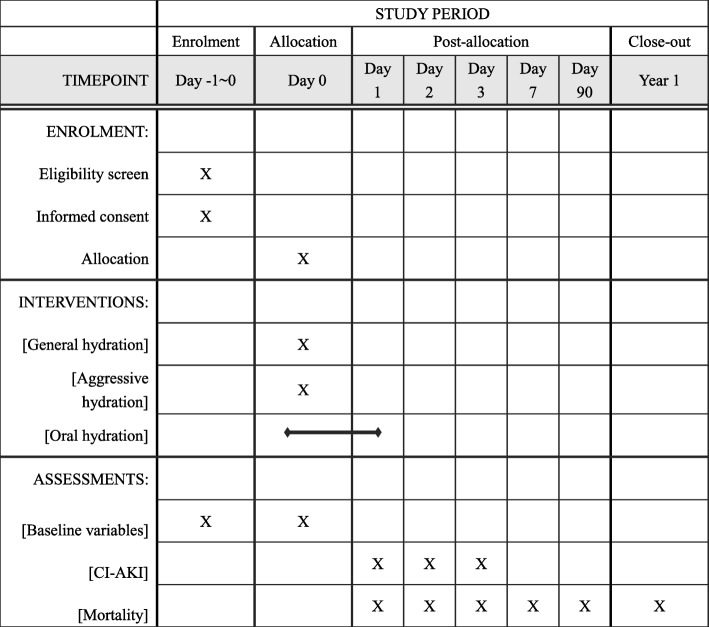
Data collected at enrolment will include baseline demographics, diagnosis, medical histories, clinical and laboratory parameters, concomitant drug treatment, and physical examination findings. Confounders such as age, sex, estimated glomerular filtration rate, LVEF, the use of an intra-aortic balloon pump, chronic heart failure, anemia, diabetes mellitus, and intravenous hydration will be measured to develop the logistic regression models. The primary outcome measure is CI-AKI, defined as a > 25% or 0.5 mg/dL increase in serum creatinine from baseline during the first 48–72 h post-procedure [15]. Secondary endpoints are the different definitions of CI-AKI, as well as persistent renal damage, major adverse cardiovascular events, major post-procedure in-hospital adverse clinical events, total hospitalization costs, and length of stay (Fig. 1).
Fig. 1.
The schedule of enrolment, interventions, and assessments. CI-AKI contrast-induced acute kidney injury
All data from the study will be collected following approval by the corresponding ethics committees of the participating centers. An independent data monitoring committee will be responsible for the review of the ongoing safety of patients enrolled in the study (Additional file 1).
Statistical analysis
Baseline patient characteristics and information will be described as means ± standard deviation or medians and interquartile ranges of descriptive statistics. Categorical variables will be presented as frequencies and percentages. OHV/W ratios will be calculated and grouped according to the interquartile range. For continuous variables, one-way analysis of variance (ANOVA) will be conducted for normally distributed data, and the Kruskal–Wallis test used for non-normal distributions (presented as the median and interquartile range). Pearson’s chi-square test or Fisher’s exact test will be used, as appropriate, for categorical data.
The odds ratios of CI-AKI for quartiles with different OHV/W ratios (cut-off values determined by the quartiles) will be estimated using univariate and multivariate logistic regression analyses. Multivariable logistic regression models have been developed to adjust for clinical characteristics (e.g., age, sex, estimated glomerular filtration rate, LVEF, the use of an intra-aortic balloon pump, chronic heart failure, anemia, diabetes mellitus, intravenous hydration), and the Mehran risk score will be calculated [16]. All variables that are univariately associated with this outcome measure will be entered as possible predictors in a multivariable logistic regression analysis. A two-tailed p value < 0.05 will be considered as statistically significant. The power calculation was based on our previous findings [17], and a CI-AKI incidence of 23% was estimated for the inadequate oral hydration group, while 11.5% was assumed for the adequate oral hydration group (50% relative reduction). Using a two-sided chi-square test, a significance level of 0.05, and a sample size of 280 each group, the power of the tests is 95.44%.
All statistical analyses will be performed using SAS version 9.4 or later (SAS Institute, Cary, NC, USA) and R software (version 3.1.2; R Foundation for Statistical Computing, Vienna, Austria).
Discussion
Patients with STEMI are likely to present with hypotension or even shock, and it is often impossible to start renal prophylactic therapy, which is associated with an increased risk of CI-AKI [18]. Despite a considerable number of risk factors, including reduced LVEF, renal dysfunction, and diabetes mellitus in patients needing adequate hydration [19, 20], cardiologists in previous studies were primarily concerned with rapid revascularization for occluded culprit arteries instead of adequate pre-procedural hydration to prevent CI-AKI; this was related to a lack of information regarding baseline renal function and related medical history. Therefore, post-procedural oral hydration might be more suitable for CI-AKI prevention in patients with STEMI.
The first study, published in 1998, reported that oral hydration was as effective as intravenous hydration [21]. Two other studies applied oral hydration to the entire group with the aim of determining the incidence of CI-AKI [22] and comparing the efficacy of different oral volumes [23] where the incidence of CI-AKI could be reduced by oral hydration. The latest three studies reported similar results [24–26]. Four meta-analyses have been published so far, which included between four and eight randomized controlled trials (RCTs) [13, 27–29]. These studies also demonstrated no significant difference between oral fluid hydration and intravenous fluid hydration regimens in the prevention of CI-AKI, nor that the oral route was inferior. There have been heterogeneities in the reported incidence of CI-AKI among studies, due to differences in CI-AKI definition, study population, and imaging procedure (Table 1).
Table 1.
Characteristics of randomized controlled trials with intervention of oral hydration among patients undergoing coronary angiography/percutaneous coronary intervention
| Study | Year | Sample size | Procedure | Contrast agent | Kidney function of participants | Contrast-induced nephropathy definition | Intervention protocols | |
|---|---|---|---|---|---|---|---|---|
| Regimen one | Regimen two | |||||||
| Wrobel et al. [24] | 2010 | 102 | Elective CAG/PCI | Low osmolality, non-ionic (isoverol) | CKD and diabetes mellitus | > 44.2 μmol/L (> 0.5 mg/dL) absolute increase or a > 25% relative increase in serum creatinine within 72 h of contrast exposure | Oral mineral water 1 mL/kg/h for 6–12 h before and 12 h after contrast exposure | Isotonic saline, IV, 1 mL/kg/h for 6 h before and 12 h after contrast exposure (reduced to 50% in patients with CHF) |
| Kong et al. [26] | 2012 | 120 | Elective CAG | Low osmolality,ionic (iopromide) | Normal renal function | > 44.2 μmol/L (> 0.5 mg/dL) absolute increase or a > 25% relative increase in serum creatinine within 48–72 h of contrast exposure | Oral 2000 mL neutral water within 24 h after and/or 500 mL water before contrast exposure | Isotonic saline, IV, 1 mL/kg/h for 12 h before and 24 h after contrast exposure |
| Akyuz et al. [12] | 2014 | 225 | Elective CAG | Non-ionic low osmolar iopromide, Ultravist | At least one of the high-risk factors for developing CI-AKI (advanced age, type 2 diabetes mellitus, anemia, hyperuricemia, a history of cardiac failure or systolic dysfunction), eGFR ≥ 60 mL/min) | > 44.2 μmol/L (> 0.5 mg/dL) absolute increase or a > 25% relative increase in serum creatinine within 48 h of contrast exposure | Drink neutral water as much as possible for 12 h before and 2 h after contrast exposure | Isotonic saline, IV, 1 mL/kg/h for 12 h before and 12 h after contrast exposure |
| Cho et al. [25] | 2010 | 91 | Elective CAG | Low osmolality, non-ionic (isoverol) | CKD (baseline creatinine at least 1.1 md/dL or eGFR < 60 mL/min) | > 44.2 μmol/L (> 0.5 mg/dL) absolute increase or a > 25% relative increase in serum creatinine within 72 h of contrast exposure | Water; 500 mL started 4 h prior and stopped 2 h prior to procedure followed by oral hydration with 600 mL of water post-procedure | Isotonic saline or sodium bicarbonate solution, IV, 3 mL/kg/h for 1 h before and 6 h after contrast exposure (for patients greater than 110 kg, infusion rates will be based on that for a 110 kg person |
| Angoulvant et al. [30] | 2009 | 201 | Elective CAG | Ionic low osmolar (Hexabrix) | Serum creatinine < 140 μmol/L | The change in calculated creatinine clearance in 24 h and 3 days | 1000 mL isotonic saline, IV, during and oral 2000 mL tap water within 24 h after contrast exposure | Oral 2000 mL tap water within 24 h after contrast exposure |
| Taylor et al. [21] | 1998 | 36 | Elective cardiac catheterization | Ionic contrast media in most cases | Renal dysfunction (serum creatinine ≥ 1.4 mg/dL) | An increase in creatinine of ≥ 0.5 mg/dL within 48 h of contrast exposure | Oral 1000 mL water over 10 h before then 0.45% saline, IV, 300 mL/h during and 6 h after contrast exposure | 0.45% saline, IV, 75 mL/h for 12 h before and 12 h after contrast exposure |
CAG coronary angiography, CHF congestive heart failure, CI-AKI contrast-induced acute kidney injury, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, IV intravenous, PCI percutaneous coronary intervention
The above-mentioned studies were conducted on relatively low-risk patients, including those subjects undergoing intravenous radiographic procedures. The frequencies of risk factors were merely reported, and some RCTs excluded patients with chronic kidney disease, congestive heart failure, or systolic dysfunction, with a lower proportion of diabetic patients. Moreover, the oral hydration protocol varied greatly, with no two trials having a similar oral regimen.
It is reported that the incidence is < 2% in the general population but is up to 20–30% in high-risk populations with congestive heart failure, chronic kidney disease, diabetes mellitus, and anemia [3].
For in-patient settings or individuals who require emergent coronary angiography or radiological procedures with contrast exposures, intravenous hydration has been studied and used as first-line treatment for the prevention of CI-AKI [11]. However, there is no consensus regarding the mode of administration. In modern medicine, with an evolving number of diagnostic studies that depend on iodinated contrast along with an increasing number of complex high-risk patients, the costs of hospitalizations and nursing care are growing. Previous hydration strategies have not been investigated in STEMI patients. Therefore, oral hydration, which is considered safe and effective in low-risk patients, should be investigated in patients with STEMI undergoing primary PCI.
Limitations
Our current secondary analysis is subject to the following limitations. First, it was less sensitive than defined as a > 0.5 mg/dL increase in serum creatinine, because it recognized less selectively those patients with a higher risk of mortality and morbidity. Second, according to the ATTEMPT study, participants received either aggressive or routine intravenous hydration. Hemodilution can reduce serum creatinine, and cumulative daily fluid balance (input/output) directly affects the concentration (i.e., dilution) of serum creatinine. In our study, post-procedural daily fluid balance (input/output) was recorded to estimate the change in renal function to reduce the influence of hemodilution. Third, there were the inherent limitations of an observational study, including differences in oral hydration administration protocols regarding hydration rate, time, and total volume. Fourth, the fact that post-procedure serum creatinine measurements were not random but standardized at 48 h might suggest that delayed-onset elevation of serum creatinine (> 48 h) could be overlooked. Finally, this was a secondary analysis, which is not able to conclude a causal relationship. On the basis of the above limitations, future large-sample, well-designed RCTs are required to confirm and update the findings of this secondary analysis. However, to the best of our knowledge, this is the first prospective, subanalysis to investigate the effect of oral hydration on the prevention of CI-AKI in high-risk patients undergoing primary PCI.
Oral hydration has a practical value in daily life. It is easy to administer, allows better use of hospital resources due to shorter hospital stays, does not require intravascular cannulation, is less expensive, and is more comfortable for the patient. Our study will determine the association between post-procedural oral hydration and the decreasing incidence of CI-AKI following primary PCI, as well as the risk factors among quartiles of OHV.
Additional file
SPIRIT 2013 checklist: recommended items to address in a clinical trial protocol and related documents. (DOC 121 kb)
Acknowledgments
The authors are solely responsible for the design and conduct of this study, all study analyses, and the drafting and editing of the paper and its final contents. Special thanks go to the project managers Mr. Yongquan Yang and Ms. Lingfen Chen for their considerable time and effort in the ATTEMPT study.
Funding
This study was supported by grants from the Science and Technology Planning Project of Guangdong Province (no. 2014B070706010), the National Natural Science Foundation of China (no. 81670339), and the Guangdong General Hospital Clinical Research Fund and Guangdong Society of Interventional Cardiology Research Fund (no. 2014dzx02).
Trial status
The RESCIND-1 ATTEMPT trial (protocol version 2.0, 11 June 2014) enrolled the first participant on 1 July 2014 and expected to complete recruitment in December 2018. As of 24 October 2018, recruitment is ongoing with 555 patients randomized at 15 centers in China.
Abbreviations
- CI-AKI
Contrast-induced acute kidney injury
- LVEF
Left ventricular ejection fraction
- OHV/W
Oral hydration volume/weight
- PCI
Percutaneous coronary intervention
- RCT
Randomized controlled trial
- STEMI
ST-elevation myocardial infarction
Authors’ contributions
Conceptualization: FS. Project administration: JL, YL. Resources: YL, JC. Writing—original draft: FS. Writing—review and editing: FS, JL, GS, YH, LL. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All participants provided written informed consent before enrolment. All data in the study will be collected following approval by the corresponding ethics committees of the participating centers. An independent data monitoring committee will be responsible for the review of the ongoing safety of patients enrolled in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Feier Song, Email: feiersong@126.com.
Guoli Sun, Email: sunguoli2016@qq.com.
Jin Liu, Email: ljaw397017568@163.com.
Ji-yan Chen, Email: chenji_yandr@126.com.
Yibo He, Email: heyibo2011@163.com.
Liwei Liu, Email: liuliwei1001@126.com.
Yong Liu, Email: liuyong2099@126.com.
References
- 1.Sadeghi HM, Stone GW, Grines CL, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. 2003;108(22):2769–2775. doi: 10.1161/01.CIR.0000103623.63687.21. [DOI] [PubMed] [Google Scholar]
- 2.Narula A, Mehran R, Weisz G, et al. Contrast-induced acute kidney injury after primary percutaneous coronary intervention: results from the HORIZONS-AMI substudy. Eur Heart J. 2014;35(23):1533–1540. doi: 10.1093/eurheartj/ehu063. [DOI] [PubMed] [Google Scholar]
- 3.Singri N, Ahya SN, Levin ML. Acute renal failure. JAMA. 2003;289(6):747–751. doi: 10.1001/jama.289.6.747. [DOI] [PubMed] [Google Scholar]
- 4.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103(5):368–375. doi: 10.1016/S0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 5.Tepel M, Aspelin P, Lameire N. Contrast-induced nephropathy: a clinical and evidence-based approach. Circulation. 2006;113(14):1799–1806. doi: 10.1161/CIRCULATIONAHA.105.595090. [DOI] [PubMed] [Google Scholar]
- 6.James MT, Ghali WA, Knudtson ML, et al. Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation. 2011;123(4):409–416. doi: 10.1161/CIRCULATIONAHA.110.970160. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R, Birnbaum Y, Uretsky BF. The renal patient with coronary artery disease: current concepts and dilemmas. J Am Coll Cardiol. 2004;44(7):1343–1353. doi: 10.1016/j.jacc.2004.06.058. [DOI] [PubMed] [Google Scholar]
- 8.Levy EM, Viscoli CM, Horwitz RI. The effect of acute renal failure on mortality. A cohort analysis. JAMA. 1996;275(19):1489–1494. doi: 10.1001/jama.1996.03530430033035. [DOI] [PubMed] [Google Scholar]
- 9.Marenzi G, Lauri G, Assanelli E, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004;44(9):1780–1785. doi: 10.1016/j.jacc.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 10.Pyxaras SA, Sinagra G, Mangiacapra F, et al. Contrast-induced nephropathy in patients undergoing primary percutaneous coronary intervention without acute left ventricular ejection fraction impairment. Am J Cardiol. 2013;111(5):684–688. doi: 10.1016/j.amjcard.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 11.Neumann Franz-Josef,Sousa-Uva Miguel,Ahlsson Anders et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. [J] Eur. Heart J. 2019;40:87-165. [DOI] [PubMed]
- 12.Akyuz S, Karaca M, Kemaloglu OT, et al. Efficacy of oral hydration in the prevention of contrast-induced acute kidney injury in patients undergoing coronary angiography or intervention. Nephron Clin Pract. 2014;128(1–2):95–100. doi: 10.1159/000365090. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal SK, Mohareb S, Patel A, et al. Systematic oral hydration with water is similar to parenteral hydration for prevention of contrast-induced nephropathy: an updated meta-analysis of randomised clinical data. Open Heart. 2015;2(1):e000317. doi: 10.1136/openhrt-2015-000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Chen JY, Huo Y, et al. Aggressive hydration in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention to prevent contrast-induced nephropathy (ATTEMPT): study design and protocol for the randomized, controlled trial, the ATTEMPT, RESCIND 1 (first study for reduction of contrast-induced nephropathy following cardiac catheterization) trial. Am Heart J. 2016;172:88–95. doi: 10.1016/j.ahj.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Briguori C, Visconti G, Rivera NV, et al. Cystatin C and contrast-induced acute kidney injury. Circulation. 2010;121(19):2117–2122. doi: 10.1161/CIRCULATIONAHA.109.919639. [DOI] [PubMed] [Google Scholar]
- 16.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–1399. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 17.Tan N, Liu Y, Chen JY, et al. Use of the contrast volume or grams of iodine-to-creatinine clearance ratio to predict mortality after percutaneous coronary intervention. Am Heart J. 2013;165(4):600–608. doi: 10.1016/j.ahj.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Zoungas S, Ninomiya T, Huxley R, et al. Systematic review: sodium bicarbonate treatment regimens for the prevention of contrast-induced nephropathy. Ann Intern Med. 2009;151(9):631–638. doi: 10.7326/0003-4819-151-9-200911030-00008. [DOI] [PubMed] [Google Scholar]
- 19.Sgura FA, Bertelli L, Monopoli D, et al. Mehran contrast-induced nephropathy risk score predicts short- and long-term clinical outcomes in patients with ST-elevation-myocardial infarction. Circ Cardiovasc Interv. 2010;3(5):491–498. doi: 10.1161/CIRCINTERVENTIONS.110.955310. [DOI] [PubMed] [Google Scholar]
- 20.Oduncu V, Erkol A, Karabay CY, et al. Relation of the severity of contrast induced nephropathy to SYNTAX score and long-term prognosis in patients treated with primary percutaneous coronary intervention. Int J Cardiol. 2013;168(4):3480–3485. doi: 10.1016/j.ijcard.2013.04.166. [DOI] [PubMed] [Google Scholar]
- 21.Taylor AJ, Hotchkiss D, Morse RW, McCabe J. PREPARED: preparation for angiography in renal dysfunction: a randomized trial of inpatient vs outpatient hydration protocols for cardiac catheterization in mild-to-moderate renal dysfunction. Chest. 1998;114(6):1570–1574. doi: 10.1378/chest.114.6.1570. [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Ruiz C, Martinez-Vea A, Sempere T, et al. Low risk of contrast nephropathy in high-risk patients undergoing spiral computed tomography angiography with the contrast medium iopromide and prophylactic oral hydratation. Clin Nephrol. 2004;61(3):170–176. doi: 10.5414/CNP61170. [DOI] [PubMed] [Google Scholar]
- 23.Yoshikawa D, Isobe S, Sato K, et al. Importance of oral fluid intake after coronary computed tomography angiography: an observational study. Eur J Radiol. 2011;77(1):118–122. doi: 10.1016/j.ejrad.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 24.Wrobel W, Sinkiewicz W, Gordon M, Wozniak-Wisniewska A. Oral versus intravenous hydration and renal function in diabetic patients undergoing percutaneous coronary interventions. Kardiol Pol. 2010;68(9):1015–1020. [PubMed] [Google Scholar]
- 25.Cho R, Javed N, Traub D, et al. Oral hydration and alkalinization is noninferior to intravenous therapy for prevention of contrast-induced nephropathy in patients with chronic kidney disease. J Interv Cardiol. 2010;23(5):460–466. doi: 10.1111/j.1540-8183.2010.00585.x. [DOI] [PubMed] [Google Scholar]
- 26.Kong DG, Hou YF, Ma LL, Yao DK, Wang LX. Comparison of oral and intravenous hydration strategies for the prevention of contrast-induced nephropathy in patients undergoing coronary angiography or angioplasty: a randomized clinical trial. Acta Cardiol. 2012;67(5):565–569. doi: 10.1080/AC.67.5.2174131. [DOI] [PubMed] [Google Scholar]
- 27.Cheungpasitporn W, Thongprayoon C, Brabec BA, et al. Oral hydration for prevention of contrast-induced acute kidney injury in elective radiological procedures: a systematic review and meta-analysis of randomized controlled trials. N Am J Med Sci. 2014;6(12):618–624. doi: 10.4103/1947-2714.147977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiremath S, Akbari A, Shabana W, Fergusson DA, Knoll GA. Prevention of contrast-induced acute kidney injury: is simple oral hydration similar to intravenous? A systematic review of the evidence. PLoS One. 2013;8(3):e60009. doi: 10.1371/journal.pone.0060009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Weidai, Zhang Jiawei, Yang Baojun, Wu Kefei, Lin Hanfei, Wang Yanping, Zhou Lihong, Wang Huatao, Zeng Chujuan, Chen Xiao, Wang Zhixing, Zhu Junxing, Songming Chen. Effectiveness of oral hydration in preventing contrast-induced acute kidney injury in patients undergoing coronary angiography or intervention. Coronary Artery Disease. 2018;29(4):286–293. doi: 10.1097/MCA.0000000000000607. [DOI] [PubMed] [Google Scholar]
- 30.Angoulvant Denis, Cucherat Michel, Rioufol Gilles, Finet Gérard, Beaune Jacques, Revel Didier, Laville Maurice, Ovize Michel, André-Fouët Xavier. Preventing acute decrease in renal function induced by coronary angiography (PRECORD): a prospective randomized trial. Archives of Cardiovascular Diseases. 2009;102(11):761–767. doi: 10.1016/j.acvd.2009.07.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SPIRIT 2013 checklist: recommended items to address in a clinical trial protocol and related documents. (DOC 121 kb)