Abstract
The objective of this study was to evaluate the relationship between insurance status and access to physical therapy (PT). Masked telephone interviews with PT facilities in a major metropolitan area were conducted with researchers posing as parents of children. Each facility was called twice: once with a private insurer and once with a government insurer. Earliest available appointment, if the facility accepted insurance, and amount of time required to return a call were recorded. Fifty-four PT clinics responded. Clinics that accepted private insurance were significantly greater than the proportion that accepted government insurance (85.2% vs 14.8%, P < .001). There was no significant difference in time between initial call and first offered appointment, in the 2 insurance conditions (private: 8.09 days, government: 8.67 days, P = .33). There were no significant differences in appointment delays between both insurance conditions. Our study found there was a significantly lower rate of children with government-funded insurance that had access to postsurgical rehabilitation.
Keywords: physical therapy, barriers, insurance, rehabilitation, orthopedics
Background
Recent health care reform in the United States has brought national attention to the difficulties of receiving medical care. Patients who come from lower socioeconomic classes, often minorities and children, are the majority of those who have the most difficulty obtaining insurance authorization and coverage of care.1-7 Following initial intervention, delay to physical and occupational therapy can often extend care needs and prolong recovery.
Little has been written on the association between insurance status and access to physical therapy (PT). Trauma research on PT utilization shows that publicly insured and uninsured patients are less likely to receive rehabilitation following hospital admission.8,9 Englum et al showed that while patients insured through public programs were discharged to rehabilitation facilities more often than uninsured patients, minorities with public insurance are significantly less likely to receive post-hospitalization rehabilitation.10 This finding may contribute to the disparities seen in post-trauma mortality rates for these populations.11
These studies underscore the importance of determining the impact of insurance status in the orthopedic field. The detrimental effects of prolonged postoperative immobilization have been well described in the literature.12-15 Importantly, physical rehabilitation has been shown to effectively prevent these complications and decrease the time needed to return to full activity following orthopedic surgery.16-21 As a result, recognizing and addressing risk factors associated with delays in rehabilitation are crucial for successful return to pre-injury activities. The purpose of this study was to investigate the impact of insurance status on access to PT in pediatric patients in orthopedics.
Methods
Institutional review board approval was obtained prior to initiating this study. PT facilities within a 27-mile radius were identified through an extensive online search and licensure was verified through the Physical Therapy Board of California Registry. Previous literature has shown that immobilization strongly affects knee and ankle joints,18,19,22 as well as weight-bearing and paraspinal muscles.12,23,24 Based on this, orthopedic conditions involving the knee, ankle, and back were selected. From August to November 2017, a series of telephone interviews were conducted by trained researchers, with private PT facilities in a major metropolitan area in Southern California. Researchers verified that the facilities cared specifically for pediatric patients prior to calling. In order to minimize reporting bias, calls were masked and researchers posed as parents of children with one of the following randomly assigned diagnoses: anterior cruciate ligament tear, ankle injury, or postoperative back pain. These diagnoses are among the most common to be referred to PT at our clinic. A standard script was used for the different clinical scenarios. Each facility was called twice by the same researcher with the same clinical scenario—once with a private insurer, Blue Cross Blue Shield, and once with a government insurer, Medi-Cal. Calls were made to the same facility 2 weeks after the initial correspondence. The following variables were recorded: if the facility accepted the insurance, soonest available appointment (counted in days), and, if applicable, amount of time required to return a call (counted in hours). If a facility did not accept the type of insurance, they were asked if an appointment could be scheduled with cash payment. If this was an option, the soonest available appointment was recorded. If a call went to voicemail, a brief message was left describing the clinical situation, insurance status, and a call back number. Analysis was performed using STATA (StataCorp LP, College Station, TX). For clinics that scheduled appointments for both insurance conditions, a one-sided paired t test analyzing days of appointments was performed. The P value was set at .05 as the significance cutoff.
Ethics and Informed Consent
This study was reviewed by the Committee of Clinical Investigations (Institutional Review Board) at the authors’ institution. Waiver of informed consent was granted per 45 CFR 46.116(d).
Results
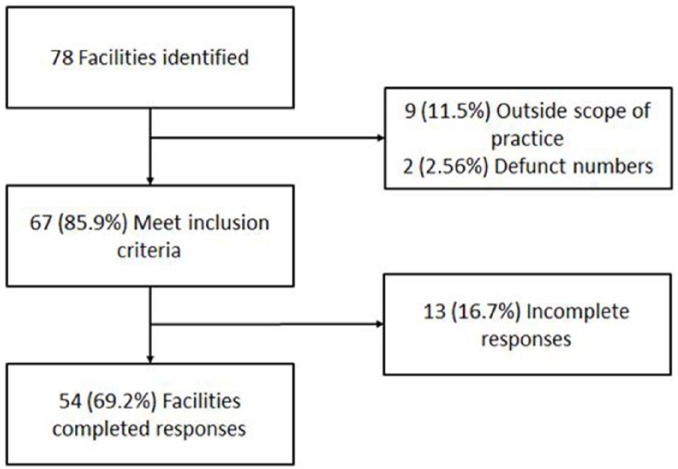
During the study period, 78 PT clinics were identified. There were 24 (30.7%) that were excluded due incomplete responses, defunct numbers, or the clinical scenario was outside of their scope of practice (Figure 1).
Figure 1.
Facility selection. Local physical therapy clinics were identified and contacted to determine if they were suitable for study inclusion. Reproduced with permission from the Children’s Orthopaedic Center, Los Angeles.
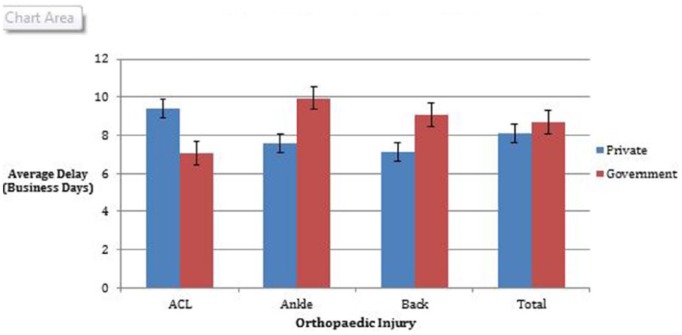
Of the remaining 54 centers, 8 (10.3%) accepted both insurance types. Seventy percent (38/54) of facilities accepted private insurance, but rejected government insurance. Eight insurance facilities did not accept Medi-Cal or Blue Cross. These facilities may have accepted insurance outside of the 2 insurance types that were offered by the research team. On average, patients with private insurance waited 8.09 days for their first PT appointment, and patients with government insurance waited 8.67 days for their first PT appointment (P = .33). Patients were also stratified into condition groups. When looking at the anterior cruciate ligament reconstruction, patients with private insurance had a delay of 9.42 days to first appointment, while patients with government insurance had a delay of 7.05 days to first appointment. Patients with an ankle condition had a delay of 7.58 days (private) and 9.95 days (government), and patients with a back condition had a delay of 7.13 days (private) and 9.06 days (government; Figure 2).
Figure 2.
Scheduling delay by injury type. Reproduced with permission from the Children’s Orthoapaedic Center, Los Angeles.
During the course of calling the 78 facilities, there were 22 voicemails left for missed calls (15 under the private condition and 7 under government). Only 9 calls (41%) were returned within 5 business days (1 week) with an average of call back time of 8.54 hours for private insurance (n = 7) and 12.68 hours for government insurance (n = 2).
The number of centers that accepted private insurance was significantly greater than the number that accepted government insurance (85.2% vs 14.8%, P < .001).
Discussion
Physical therapy is often necessary following orthopedic surgery. Getting a patient into PT reduces postoperative disuse muscle atrophy, decreases utilization of other health care resources (magnetic resonance imaging or analgesic medications), and decreases the time needed to resume normal activities.16,25,26 At our institution, we have noticed that pediatric patients with orthopedic conditions have difficulty getting an appointment for PT if the insurance is Medi-Cal. Although our results showed no significant difference between the insurance types with regard to the number of days between the initial call and soonest available appointment, it found far fewer PT centers that accepted government insurance compared with private. We also found that centers that accept both insurances do not differentiate between types of insurance, and there was no significant difference in wait time for appointment. Our findings are consistent with similar studies examining children’s access to specialty health care including Bisgaier et al who also found a disparity in access to outpatient specialty care between children who had private and government insurances.4,6
This study highlights some of the challenges faced when seeking PT. The available literature suggests that low acceptance rates of government-funded insurance may act as a barrier to access PT. Two retrospective studies examining PT utilizations among trauma patients showed that, when controlling for severity, patients were significantly less likely to receive post-discharge PT if they had Medicaid or no insurance.8,9 This suggests that insurance status correlates with a real difference in access to rehabilitation services. Insurance barriers can have clinically important impacts, given that a number of studies have demonstrated that timely intervention with PT for acute orthopedic injuries leads to improved outcomes.25,26 Furthermore, with only 41% of calls returned within 1 week, the poor response rates make it increasingly difficult to schedule PT visits in a timely manner.
This study is limited by its inability to fully simulate the scheduling process (eg, time required to get insurance authorization) and inability to standardize practical restrictions on patients, such as physical distance, time constraints, or transportation issues. Since appointments cannot be completely scheduled until insurance has authorized the visit, a more accurate measure of delays would require prospective, standardized tracking of real patients through the entire process. Although this is a small sample size, it compares well with previously published studies.3,6,7 Future work should focus on how the insurance status may have an impact on validated clinical measures or subjective outcomes to better characterize the impact of delays in receiving health care.
The pediatric population is full of young, developing, and eager individuals who want to return to their everyday activities as soon as possible especially following surgery. PT is an essential and beneficial component toward recovery of any injury or surgery. Techniques in PT can help reduce and eliminate pain, and improve mobility. However, our study shows that even in the setting of a diverse, metropolitan area, many facilities will not take government insurance. Although the easiest solution would be for facilities to take all insurances, this is an unrealistic concept as there are many bureaucratic factors that are outside our scope of control. Although it is possible that change can be initiated with the help of hospital staff. Hospitals across the United States have resources that can help families combat the problem of not finding an appropriate PT center. Some solutions include helping patients schedule appointments prior to discharge or providing a list of facilities per zip code that will take the patients’ insurance. Social work can also be an important asset to use when helping families with transportation, follow-ups, and so on. Theoretically, there are solutions that can help patients get into PT in a timely fashion. However, without addressing the low number of providers who accept public insurance, the inequitable access to health care will likely persist.
Footnotes
Author Contributions: NS: Contributed to acquisition and interpretation of data, drafted manuscript, critically revised manuscript, gave final approval, agrees to be accountable for all aspects of work ensuring integrity and accuracy.
RS: Contributed to interpreration of data, drafted manuscript, critically revised manuscript, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
CV: Contributed to conception and design, critically revised manuscript, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
JLP: Contributed to conception and design, critically revised manuscript, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
RYG: Contributed to conception and design, contributed to interpretation of data, critically revised manuscript, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Rachel Y. Goldstein  https://orcid.org/0000-0002-3691-7529
https://orcid.org/0000-0002-3691-7529
References
- 1. Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006;96:1300-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152:1119-1125. [DOI] [PubMed] [Google Scholar]
- 3. Newacheck PW, McManus M, Fox HB, Hung YY, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105(4 pt 1):760-766. [DOI] [PubMed] [Google Scholar]
- 4. Bisgaier J, Rhodes KV. Auditing access to specialty care for children with public insurance. N Engl J Med. 2011;364:2324-2333. [DOI] [PubMed] [Google Scholar]
- 5. Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357:1515-1523. [DOI] [PubMed] [Google Scholar]
- 6. Skaggs DL, Clemens SM, Vitale MG, Femino JD, Kay RM. Access to orthopedic care for children with Medicaid versus private insurance in California. Pediatrics. 2001;107:1405-1408. [DOI] [PubMed] [Google Scholar]
- 7. Iobst C, King W, Baitner A, Tidwell M, Swirsky S, Skaggs DL. Access to care for children with fractures. J Pediatr Orthop. 2010;30:244-247. [DOI] [PubMed] [Google Scholar]
- 8. Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84:1605-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nirula R, Nirula G, Gentilello LM. Inequity of rehabilitation services after traumatic injury. J Trauma. 2009;66:255-259. [DOI] [PubMed] [Google Scholar]
- 10. Englum BR, Villegas C, Bolorunduro O, et al. Racial, ethnic, and insurance status disparities in use of posthospitalization care after trauma. J Am Coll Surg. 2011;213:699-708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., 3rd Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945-949. [DOI] [PubMed] [Google Scholar]
- 12. Dittmer DK, Teasell R. Complications of immobilization and bed rest. Part 1: Musculoskeletal and cardiovascular complications. Can Fam Physician. 1993;39:1428-1437. [PMC free article] [PubMed] [Google Scholar]
- 13. Elmqvist LG, Lorentzon R, Johansson C, Långström M, Fagerlund M, Fugl-Meyer AR. Knee extensor muscle function before and after reconstruction of anterior cruciate ligament tear. Scand J Rehabil Med. 1989;21:131-139. [PubMed] [Google Scholar]
- 14. Snow BJ, Wilcox JJ, Burks RT, Greis PE. Evaluation of muscle size and fatty infiltration with MRI nine to eleven years following hamstring harvest for ACL reconstruction. J Bone Joint Surg Am. 2012;94:1274-1282. [DOI] [PubMed] [Google Scholar]
- 15. Burks RT, Crim J, Fink BP, Boylan DN, Greis PE. The effects of semitendinosus and gracilis harvest in anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1177-1185. [DOI] [PubMed] [Google Scholar]
- 16. Greenberg EM, Greenberg ET, Ganley TJ, Lawrence JT. Strength and functional performance recovery after anterior cruciate ligament reconstruction in preadolescent athletes. Sports Health. 2014;6:309-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wells L, Dyke JA, Albaugh J, Ganley T. Adolescent anterior cruciate ligament reconstruction: a retrospective analysis of quadriceps strength recovery and return to full activity after surgery. J Pediatr Orthop. 2009;29:486-489. [DOI] [PubMed] [Google Scholar]
- 18. Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33:1751-1767. [DOI] [PubMed] [Google Scholar]
- 19. Beynnon BD, Johnson RJ, Fleming BC. The science of anterior cruciate ligament rehabilitation. Clin Orthop Relat Res. 2002;(402):9-20. [DOI] [PubMed] [Google Scholar]
- 20. Kruse LM, Gray B, Wright RW. Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94:1737-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128-1144. [DOI] [PubMed] [Google Scholar]
- 22. Uh BS, Beynnon BD, Helie BV, Alosa DM, Renstrom PA. The benefit of a single-leg strength training program for the muscles around the untrained ankle. Am J Sports Med. 2000;28:568-573. [DOI] [PubMed] [Google Scholar]
- 23. Gille O, Jolivet E, Dousset V, et al. Erector spinae muscle changes on magnetic resonance imaging following lumbar surgery through a posterior approach. Spine (Phila Pa 1976). 2007;32:1236-1241. [DOI] [PubMed] [Google Scholar]
- 24. Hu ZJ, Fang XQ, Zhou ZJ, Wang JY, Zhao FD, Fan SW. Effect and possible mechanism of muscle-splitting approach on multifidus muscle injury and atrophy after posterior lumbar spine surgery. J Bone Joint Surg Am. 2013;95:e192. [DOI] [PubMed] [Google Scholar]
- 25. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStayo PC. Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2007;89:559-570. [DOI] [PubMed] [Google Scholar]
- 26. Fritz JM, Cleland JA, Speckman M, Brennan GP, Hunter SJ. Physical therapy for acute low back pain: associations with subsequent healthcare costs. Spine (Phila Pa 1976). 2008;33:1800-1805. [DOI] [PubMed] [Google Scholar]