Abstract
Hailed by supporters as the answer to many challenges facing medical schools and the wider health care system, longitudinal integrated clerkships (LICs) offer a practical and sustainable alternative to more traditional block rotational models. Given this, their popularity as a curricular measure is increasing, although such clerkships remain relatively novel within the United Kingdom. This narrative literature review of international work provides a comprehensive introduction to developing and implementing LICs within medical education. This review generates a practical guide for medical educators with a focus on the development and implementation of LICs within the United Kingdom, on which there is little work. Using illustrated examples and with reference to contemporary literature, it outlines the rationale for considering an LIC within a curriculum, the different types of LIC, barriers and enabling factors to LIC implementation and considers the contemporary application of LIC models within the United Kingdom. The practical guide details key questions educators must consider when developing and implementing an LIC, particularly within the landscape of UK medical education.
Keywords: longitudinal integrated clerkships, general practice, clinical clerkships
Introduction
Longitudinal integrated clerkships (LICs) are a relatively new type of medical student placement that aim to facilitate continuity of relationships between students, patients, and physicians to enhance learning.1 Longitudinal integrated clerkships have existed in some form for over 40 years, although the term was only defined in 2007.2
Longitudinal integrated clerkships are placements where
students participate in the comprehensive care of patients over time . . . participate in continuing learning relationships with these patients’ clinicians and . . . meet the majority of the year’s core clinical competencies, across multiple disciplines simultaneously through these experiences.3
In essence, longitudinal programmes offer continued exposure to the same clinical setting, with continuity of supervision, patient, and peer bases. Such exposure provides curricula integration, combining traditionally discipline-specific learning across the period of the LIC.4 There are many recognised types of LICs – which will be outlined in this review – yet the key principle of all LICs remains that students placed in one clinical location gain longitudinal experience of patient care and benefit from mentor continuity.5,6 Some authors suggest LICs represent a return to apprenticeship-based training4 and, in many programmes, LICs are part of ‘community-based medical education’ – education that takes place outside large-scale teaching hospitals, often in general practice, community, or district hospitals.7–9 However, this is not always the case as LICs operating within academic health centres and large-scale hospitals have been successfully implemented,4,10,11 with placements in underserved areas offering particularly memorable insights to students.12
Longitudinal integrated clerkships currently make up a very small minority of medical student clinical placements across the world, around 1000 placements in total in 2013 to 2014.2 There is contemporary discourse regarding the definition of LICs within the United Kingdom, giving rise to uncertainty surrounding the current number of medical schools delivering or developing LIC programmes. Despite this uncertainty, few LICs are currently advertised by UK medical schools, likely representing the relative scarcity of established programmes.13,14 Worldwide, the quantity of LICs on offer is known to be expanding, with the number of LICs offered globally doubling in the last 9 years.2 Several UK medical schools are invested in this new wave of development, including (but not necessarily limited to) the following: Imperial College London, Kings College London, the University of Dundee, the Hull York Medical School, Cardiff University, Newcastle University, and the University of Sheffield. It is likely that increasing LIC popularity is multifactorial, yet the recruitment and retention advantages LICs offer, an area or speciality, are often cited as a key factor for LIC development.15,16 Within the United Kingdom, well-documented shortages in the medical workforce15 – particularly in general practice17,14 – mean that recruitment and retention of doctors is of major interest to health care leaders and politicians. There is also a desire to educate medical students as generalists who are able to provide complex community care for the UK’s increasingly comorbid and elderly population.18–20 The evidence suggests that medical schools are increasingly looking to LICs to assist with this national crisis.20
Given the growing number of LICs in development, there is significant interest in ascertaining the most robust way to develop and implement one. Addressing this question forms the basis of this article. Although UK-based LIC research is now underway,21 there are still few publications specific to UK LICs – henceforth, international literature will be examined within this review, with a focus on how international LIC guidance and research may be practically applied.
Methods
The authors of this article conducted a narrative overview literature review, drawing from international LIC literature. Narrative overview was selected to fulfil the aims of this work by providing a contemporary synthesis of knowledge relating to the development and implementation of LICs. Narrative review can prove particularly useful when there is ‘one or more questions’22 offering a ‘broad perspective’23 on a contemporary topic and ‘often discussing . . . context’22 – as this work aims to develop recommendations on both developing and implementing LICs within a UK context, this review method is most appropriate.
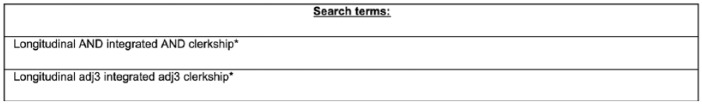
Four databases were searched (PubMed, EMBASE, MEDLINE, and ERIC) using keywords pertinent to our research question. The keywords used to search the above databases are listed in Figure 1. Filters were applied to each search to ensure retrieved articles were from within the last 15 years and were, therefore, most likely to represent contemporary discourse.
Figure 1.
Keywords used to search listed databases.
The inclusion criteria were as follows: all types of articles, articles published within the last 15 years, and articles related only to medical students. The exclusion criteria were as follows: articles for which full text was not available, articles not available in English, and grey literature. In addition to the articles retrieved in our database search, additional references were identified by a manual search among the cited references. Figure 2 details the literature selection process.
Figure 2.
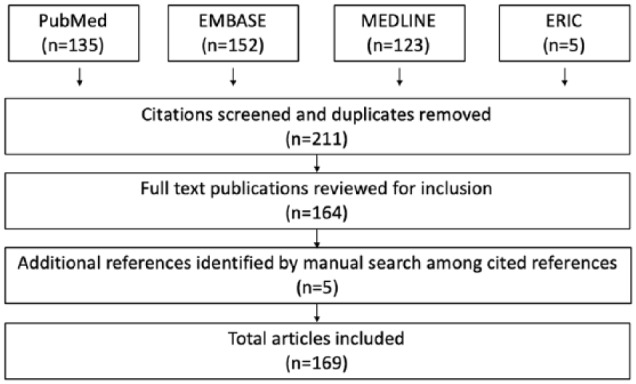
Flow chart detailing literature selection process.
Two authors preliminarily reviewed all retrieved abstracts against the review inclusion criteria. All three authors then undertook independent review of study full texts matching the inclusion criteria to extract data from the included works. All authors involved are medical educationalists and two (MELB and KA) are qualified clinicians. All extracted data were then reviewed by all authors for comprehensiveness and consistency, with any discrepancies resolved by review of the study full text and subsequent discussion between all authors until a consensus was reached. Extracted data were organised thematically and used to generate written discussion relevant to our review aims.
Discussion
Developing an LIC
Rationale
The original rationale for the development of LICs was multifactorial and links strongly to their perceived benefits. One such benefit that has proven a particularly strong drive in the will to develop LICs is the opportunity to address often significant staffing and workforce shortages evident in, most typically, rural areas.24–26 Since their inception, LICs have been shown as an effective tool in increasing recruitment of practitioners to rural areas, with those placed within rural LICs more likely to return to work in such an area, as opposed to their urban LIC counterparts.15 Worley et al2 postulate a reason for this – a combination of ‘extended immersion’ in rural, low resource settings, and ‘enabling . . . students [to make] meaningful contributions to care’ inspires students to choose careers with rural applications and henceforth practice in such areas in the future.25
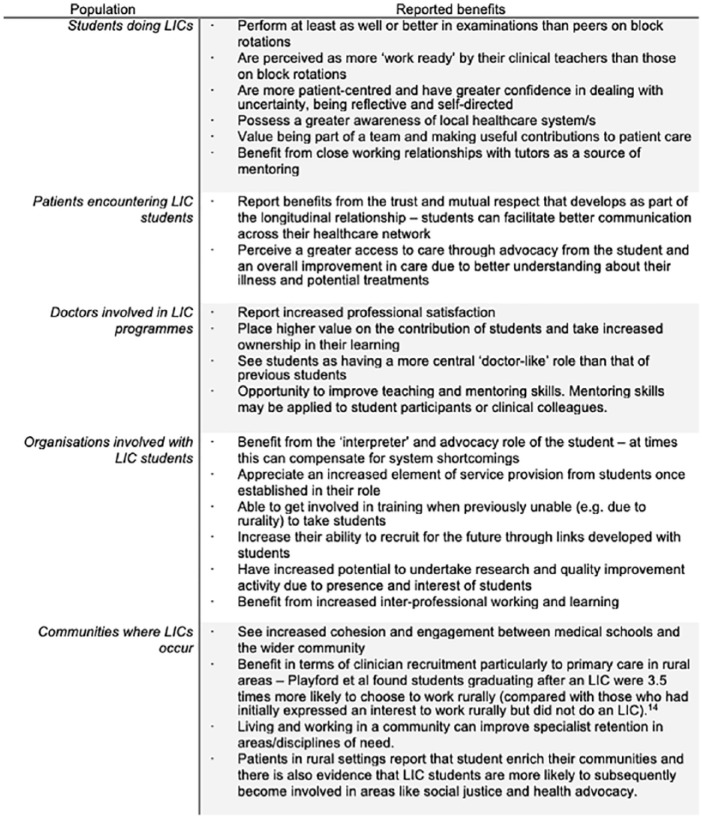
Longitudinal integrated clerkship development is often practically motivated and cited as a way of ‘manag[ing] logistical student placement pressures’.3 Despite this, the reported benefits of LIC programmes ‘present a strong argument for the consideration of the LIC as a pedagogical evolution in clinical education’.27 There is contemporary debate as to where the true value of LICs is derived from. Many suggestions have been made as to possible sources of value within an LIC and benefits have been reported for participating students,3,11,26–39 tutors,3,31,39–44 organisations,31,41,45,46 patients,4,31,34,47–49 and the communities3,9,15,16,21,31,50,51 in which LICs operate (summarised in Figure 3). These benefits may be a motivating factor in an institution deciding to develop an LIC.
Figure 3.
Summary of LIC benefits.
LIC indicates longitudinal integrated clerkships.
Selecting an appropriate model: what are the different types of LICs?
Within the development of an LIC, selecting an appropriate model to suit local context is crucial. To do this, one must understand the variety of LIC types in operation. Consideration will be given to determining model choice and considerations for curricular development within the practical application guide of this review.
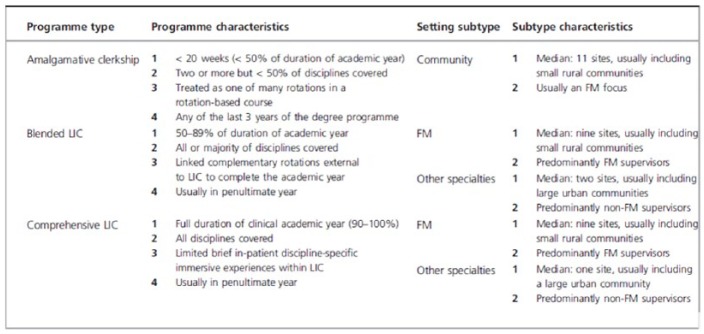
The international Consortium of Longitudinal Integrated Clerkships (CLIC) has been at the forefront of the discussion, classification, and development of LICs and a significant amount of LIC literature has arisen from CLIC-affiliated organisations.32 In 2016, Worley et al2 produced a seminal paper (on behalf of CLIC) suggesting a system for the classification of LICs. A summary of this typology is displayed in Figure 4. Worley et al argued such a system could not only facilitate better analysis of the benefits and challenges of LICs but also allow educationalists to reach conclusions regarding which elements of LICs infer the most value. Worley et al’s2 typology may also allow identification of, and collaboration between, similar LIC programmes, facilitating evidence generation on a wider scale.
Figure 4.
Longitudinal integrated clerkship typology (adapted from Worley et al2).
FM indicates family medicine.
Worley et al’s classification system suggests differentiation based on the following: placement duration, setting, proportion of disciplines covered, and the identity of the clinical supervisor. Perhaps, not surprisingly, LICs based in a rural location are more likely to have a clinical supervisor specialising in family medicine (equivalent to general practice within the United Kingdom), while those in more urban settings (often based in large teaching hospitals) tend to have a hospital specialist as clinical supervisor.2,5 These two distinct models are described as either ‘dispersed immersed’ (such as in Northern Ontario and several schools serving rural Australia and South Africa) or ‘multi-speciality streams’(such as the Cambridge Integrated Clerkship at Harvard Medical School).2
Implementing an LIC
Enabling factors for LIC implementation
Given the increasing popularity of LIC programmes, it is important to consider the factors that enable programme success. These enabling factors take the form of participating students, tutor engagement, medical school leadership, and the LIC environment. There is no one reason that permits complete enablement of LIC success, instead it is the dynamic interaction between enabling factors that determines student experience and, ultimately, programme success (Figure 5).
Figure 5.
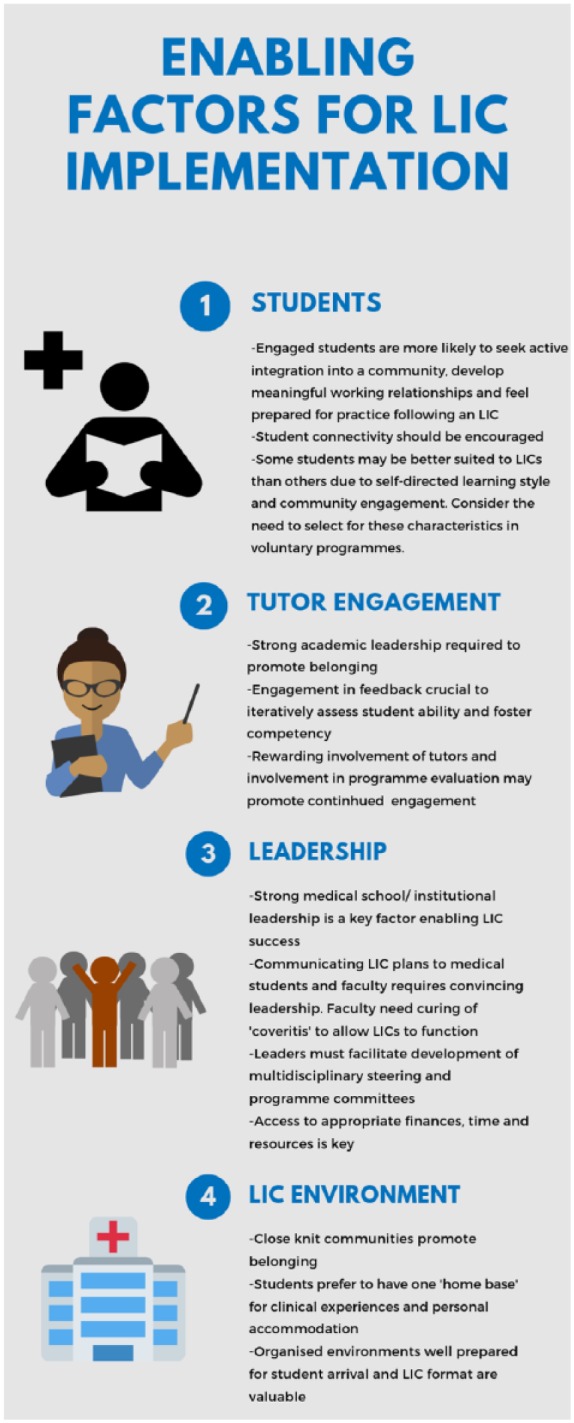
Infographic demonstrating summarised enabling factors to LIC implementation.
LIC indicates longitudinal integrated clerkships.
Participating students
Students participating in LICs play a role in determining the success of the programme. Engaged students are more likely to seek active integration into a community, work to develop meaningful relationships with tutors and colleagues, and ultimately feel prepared for practice as a clinician.29 One way of facilitating such student engagement is through encouraging connectivity, which encompasses ‘relationship building by students . . . interprofessional interactions . . . social interactions with colleagues [and] interaction with patients outside of the clinical setting’.29 This can be encouraged in several ways, but it is important that consideration is given to providing this opportunity for students within appropriate environments in the planning stage of LIC development. Some students may be naturally suited to developing such connectivity due to their personal characteristics and may therefore thrive within an LIC. It is crucial students have – or can rapidly develop – a self-directed learning style and it is beneficial if students identify as being engaged with their local community in some way.52 Further to this, comfort in dealing with uncertainty and the ability to be both a caregiver and advocate for patients is desirable.53 Indeed, students with higher levels of ‘tolerance for ambiguity’ are more likely to express a desire to work in an underserved area.54 Longitudinal integrated clerkship programmes that run as a voluntary component of a course may deliberately target their selection at students already possessing such characteristics, to maximise the likelihood of engaged and successful participating students.53
Tutor engagement
Involved tutors play a large role in enabling the success of LIC programmes. Tutors providing strong academic leadership are valued by students and aid in their sense of belonging within an LIC.52 Preceptor feedback is particularly valued by students and recognised as more ‘authentic’ than feedback students have previously received, due to the continuity of working relationships.55 Overall, students’ perception of their LIC placement and ultimate ability is heavily influenced by how actively engaged their assigned tutor is in their learning plans52 – working iteratively to assess student ability ‘fosters student development into competent professionals’.54,56
As previously mentioned, student engagement is achieved through connectivity. Tutors can actively assist in the development of student connectivity by making efforts to ‘connect students with patients who are enthusiastic to interact with students . . . and are likely to have substantial contact with the healthcare system over the course of the year’.57 Throughout the programme, tutors should be actively engaged in reviewing student connectivity and the relationships they have built with patients to better support student-patient continuity.
It is important, however, that organisations recognise the workload burden of involved tutors and take steps to both minimise this where possible and adequately acknowledge and reward involvement to promote continued engagement.26 Involving tutors in the continued evaluation of LIC programmes and responding to their feedback is recognised as one way of promoting engagement10 and ensuring continued programme success.
Medical school leadership
Not only do tutors providing strong academic leadership aid in medical student belonging within an LIC but strong leadership from institutional managers is also a key enabling factor to LIC success.52 Institutional leaders are likely to be very involved in the planning and development of an LIC and the strength of these considerations is likely to influence the success of LIC implementation. How these plans are promoted to medical students and faculty by leadership is also crucial. Faculty may be particularly difficult to convince that the full curriculum can be covered with so much time dedicated to self-directed learning and student-motivated organisation of teaching activities.58 Indeed, faculty often fall prey to ‘coveritis’,20 where they believe they must personally teach all key topics to students. Convincing leadership, belief in the LIC model, and robust institutional planning will likely be necessary to cure clinicians of their ‘coveritis’ and enable LICs to function in a way that is true to their original design.
Medical school leaders must also ensure the development of multidisciplinary steering and programme committees. Longitudinal integrated clerkship structure necessitates ‘cross disciplinary collaboration’ which may give rise to timetabling, faculty and mentoring queries.58 The use of multidisciplinary steering committees may help navigate this collaboration and ensure the prompt resolution of any concerns.
The implementation of an LIC within a new environment is likely to incur financial, time, and resource costs, as will be detailed later.31,59 Adequate planning and provision of appropriate means by medical school leadership is crucial in enabling programme success.8
The LIC environment
The environment in which an LIC takes place has a large impact on participating students. Small, rural communities with a ‘close knit’ community spirit promote a greater sense of belonging, with students reporting LICs in such settings as more ‘rewarding’ than LICs run in more urban, regional settings.52 Students prefer to have a ‘home base’ located in one centre (that centre may be rural or urban and the students’ home base refers both to their clinical and living environment), offering academic, clinical, and social benefits through the continuity this provides.59 Operating within one clinical environment removes the struggle students can experience in adapting to new systems and cultures when moving between clinical settings.60 Furthermore, when clinical teams are well prepared for LIC student arrival, have ensured staff awareness of the students’ role, and provide comprehensive inductions, students perceive a greater sense of belonging within their LIC.52 Careful planning prior to LIC student arrival can ensure this sense of belonging is fostered early within the placement.
Longitudinal follow-up of patients can prove difficult in poorly organised or disjointed care settings. The provision of an electronic care programme notifying students of any assigned patients registering within adjacent clinical settings can greatly simplify this longitudinal process.61 However, this is not always financially or practically viable. If provision of such a notification system is not possible, careful consideration must be given as to how students will logistically follow the journey of their patients and adequate resources and support provided to maximise the likelihood of this occurring.
Despite the above-identified enabling factors for LIC programme success, there is a relative dearth of recent literature regarding this area. Further research into factors enabling LIC success is warranted.
Barriers to LIC implementation
Despite strong emerging evidence indicating the benefits of LICs, some authors have identified challenges to LIC implementation. These potential barriers take the form of geography, challenging relationships, time and funding implications, new faculty and new organisations, and student and patient discomfort. These challenges are detailed below and summarised in Figure 6. It is prudent to note that several factors which may be enabling when optimised can prove a barrier if not correctly addressed.
Figure 6.

Infographic demonstrating summarised barriers to LIC implementation.
LIC indicates longitudinal integrated clerkships.
Geography
As previously mentioned, LICs are most widely implemented in underserved areas.24–26 Such areas are most often rural in nature,15 although longitudinal clerkships within urban underserved areas are also well established.10,62 Each LIC setting offers unique challenges. Rural clerkships may necessitate placing students in remote areas, risking social network isolation and student anxiety.21,63 Urban, underserved areas may suffer a higher turnover of health care staff leading to decreased staff engagement and fragmented student-tutor relationships within clerkships.64 Further to this, the immersion experienced within rural and urban clerkships by students differs, with rural placements offering the opportunity for students to forge stronger community connections.2,65 It is possible such fragmentation and immersion difficulties within urban LICs are reasons urban placements do not currently improve later recruitment of qualified participants to their underserved areas, whereas rural LICs do.15
Consideration must be given as to the impact of LIC environments upon students, and adequate student support, acknowledging a placement’s limitations, should be provided.
Challenging relationships
The closer and, at times, more intense working relationships that occur in LICs can cause difficulties for some students, despite imparting benefits to others. If relationship tensions or difficulties arise, intervention such as a change in tutor, location, or even withdrawal from an LIC may be necessary to negate any harmful effects upon student learning or experience.31
Time and funding implications
LICs can require increased tutor and administrative input compared with more traditional rotations, particularly in the early stages. This needs to be acknowledged and planned for in the design phase of an LIC8 as this provision carries financial, organisation, and service delivery implications. There is some debate concerning whether LICs are costlier to implement than ‘traditional’ block rotations.66 One concern within this debate is that LIC implementation may require a shift in funding from secondary to primary care providers, which may bring challenges.10 Additional costs may also be incurred due to the increased need for video-conferencing facilities, added travel, and accommodation requirements.31
New faculty and new organisations
There may also be challenges in developing a suitable local faculty for LIC implementation in areas not accustomed to training students.10 Indeed, even in areas with existing and concurrent block rotations, LIC implementation can bring difficulties in terms of tutor availability and in accessing wards and clinics, for example, when an LIC student accompanies a patient to a hospital appointment where students on block rotations are also in attendance.4 This issue requires scrutiny in the planning phase of a new LIC. New and existing faculty require appropriate training, and consideration must be given to how resource sharing among students will be fairly managed.
Organisations not accustomed to accommodating students may also prove a barrier or challenge to LIC implementation. Staff within new organisations may demonstrate poor understanding of what an LIC is and student purpose within such a clerkship.21 This is most troublesome when students follow their patient into an unfamiliar environment where staff do not have regular contact with students undertaking LICs.21 It is crucial that education regarding the nature and purpose of LICs, as well as raising the awareness of the potential presence of LIC students, is undertaken with all staff at involved institutions and not just directly involved faculty.
Student and patient discomfort
Students undertaking an LIC can experience stress and uncertainty when faced by, what can first appear as, unpredictable clinical opportunities and engagement simultaneously in multiple disciplines.26,67,68 Students may be faced with logistical difficulties in organising and gaining access to secondary care services and, due to the length of waiting times for non-urgent NHS care, students may be unable to follow the same patient’s journey through to secondary care,21 giving rise to further uncertainty. Given this, learner disorientation within LICs is relatively common and may give rise to student anxiety. To avoid such distress, active work by both tutors and the coordinating medical school is required.3 Greenhill and colleagues26,68 suggest clinical supervisors are instrumental in helping students navigate their ‘transformative learning journey’, ultimately allowing students to become agentic learners. Blitz et al69 found that even very senior medical students tend to adopt a learning style dependent on ‘being recipients of teaching, rather than becoming directors of their own learning’. Given the independence that LICs afford students, transitioning to a self-directed, adult approach to learning is crucial in optimising student learning experience.21,53,68 Directly addressing this need for transition with students and tutors, highlighting the possibility of difficulty, and signposting that students may experience ‘conscious incompetence’ may help to mitigate against the risk of extreme student unease during this transition.68 Resource provision may also enable students to develop a self-directed learning style – in some work, this has taken the form of electronic tablet provision to students, facilitating resource access and encouraging independent management of learning opportunities.70 Further to this, ‘near-peer’ LIC graduate support once LICs are established may help with the transition into seemingly disorientating LIC learning.64 Ensuring an adequate structure within LICs is also important to avoid an LIC being labelled as ‘disorganised’ –measures to achieve this upon implementation are discussed in the next section of this work.
The needs of students and those of patients exist in constant equilibrium – this balance may be tested during an LIC, with the potential for harm to occur if due heed is not paid to maintaining the scales. Longitudinal integrated clerkship organisers must make active efforts to manage the consent and confidentiality issues than can arise with such close living and working – this can be particularly complex in some of the smaller communities in which LICs occur.4,9,49 Managing such key issues should leave organisations able to reassure any concerned patients of the measures they are taking to prevent problems arising.
Assessment
Appropriately aligned summative assessment within LICs may prove challenging. Often, LICs run alongside more traditional block rotations as a voluntary programme for interested students. This is the case particularly within the United Kingdom, where LIC programmes are not yet widely well established. Given this, LIC student summative assessment often takes the form of the summative assessment undertaken by students on block rotations to maintain standardisation and consistency.21 However, this gives rise to significant issues in that the assessment used to evaluate LIC students is often not well aligned to their experience. It is well acknowledged that the desire to pass summative examinations influences learning55 – if summative examinations are not well aligned to LIC placements, one could reasonably deduce students may not fully engage with their LIC experience. More authentic measures of assessment designed specifically for LIC participants and including the integration of tutor and patient feedback would be preferable71 yet is not always practically feasible. One way of improving learner engagement with seemingly unaligned clerkships could be through direct discussion between tutors and students, aiming to contextualise learner needs within the provided clinical experience.72 In addition to this, the constructive alignment of LICs and assessment may be more directly improved through the addition of community engagement projects and review of current mandatory assessments to ascertain whether any can be adapted to ‘align better with LIC principles’.21
UK perspective on barriers to LIC implementation
Given that LIC implementation within the United Kingdom is still in its relative infancy, it is important to consider any context-specific barriers institutions may encounter. Dundee medical school was the first institution within the United Kingdom to introduce a comprehensive LIC and, during their pilot programme, recognised issues concerning the practicality of following patients into secondary care.20 National Health Service (NHS) waiting lists for referral to secondary care clinics means students may miss out on following their patient’s journey, increasing fragmentation within LIC placements. Careful consideration must be given as to how students will follow their patients into secondary care, with adequate planning and provision for situations when this cannot practically happen.
With LICs operating as relatively new innovations within UK medical degrees, a lack of familiarity of their structure and functions means that obtaining widespread institutional commitment for implementation of comprehensive LIC programmes may be difficult. Several UK programmes have tried to avoid this difficulty by gradually introducing longitudinality as a concept to their pre-existing curricula.20,73,74 This may represent a desire to implement more formal LIC models in the future. The introduction of longitudinality as a concept within UK programmes already demonstrates significant interinstitutional variation. As discussed within the introduction, there is contemporary discourse surrounding what should be classed as an LIC within the UK – such debate has also been evident internationally. Ellaway et al’s75 review of Canadian clinical clerkships suggests that LICs do not need to adhere to such ‘binary model[s]’ – instead, attending to the ‘ebb and flow of longitudinality, integration and continuity in the design of clerkships’ is more important. Casting doubt on this, Varpio et al76 question whether the transference of an educational innovation to a new context is actually a process of transformation that may threaten and distort the fundamental principles of a curricula measure. It is probable consideration regarding the definition of LICs will continue within the United Kingdom. A broader definition, beyond that of traditional models, may well be adopted, suiting the reality of the UK’s context and acting in line with Ellaway et al’s findings. Despite this, caution should be exercised and work undertaken to analyse whether each institution’s context-dependent modifications continue to uphold the underlying philosophy of LICs.
Analysis of further context-specific barriers within the United Kingdom is troublesome due to a lack of published work on the matter. Further research offering insight into the implementation of LICs and, more broadly, longitudinal curricula elements within the United Kingdom would add to understanding regarding any UK-specific barriers or enabling factors.
Practical application guide: what are the steps involved in developing and implementing an LIC?
This narrative review generates 10 key questions to ask when introducing an LIC into a medical curriculum.
Question 1: which typology?
As previously detailed, variation exists within the types of LICs available. The most appropriate model will depend on a variety of factors relevant to the individual school. These factors may include, but are not limited to, student, tutor, and patient availability as well as workforce and service needs.2,62,75 For example, an ‘immersed dispersed’ model using family medicine clinical supervisors based in community clinics (eg, general practice) may be the most appropriate choice for an area with an identified shortage of primary care clinicians. Once the most appropriate typology has been identified theoretically, this should also be considered in practice – with the previous example in primary care, the medical school would have to ensure there was sufficient capacity among the current workforce to support delivery of an LIC.
An LIC must provide an environment in which students can meet their objectives, as well as an environment that fits the local landscape. Given this, the type and site of an LIC must be selected and developed accordingly, with student attainment in mind.31
Question 2: pilot or whole programme?
Historically LICs have developed rather organically, often as part of a pilot, with a model bespoke to the individual institution,10 although there are some examples of initial larger scale implementation.77 Some argue, given the increasing evidence of benefit, that initial larger scale introduction is now more appropriate.31 Success with whole cohort implementation has been evidenced within the Northern Ontario School of Medicine (NOSM), the first medical school worldwide in which all students complete a rural LIC placement.78 The LIC within NOSM is overwhelmingly positively received by students, even by those who initially had reservations about the mandatory placement.4 This must be interpreted, however, in the context of NOSM’s socially accountable admission criteria, which aims to select medical students who have lived in underserved areas.79 There is evidence that use of such criteria means upon graduation, students are more likely to practice in underserved areas.79,80 Selecting for such a demographic may increase the likelihood participating students will enjoy a compulsory LIC within such an underserved area.
Question 3: existing or new curriculum?
Hudson et al6 highlight the importance of continuity in curriculum for LICs and suggest that a case-based spiral curriculum can lend itself well to the opportunities that arise during an LIC. The same core outcomes and objectives as those created for more traditional block rotations should be achievable throughout an LIC, although there may be additional LIC-specific outcomes, particularly regarding communication skills, professionalism, and teamwork.
Following the usual principles of curriculum design,81 those implementing a new LIC should examine existing curriculum arrangements and the associated learning outcomes to see what changes may need to be made. Ultimately, curricula implementation within an LIC depends on the projected outcomes of the placement. Given this, it is important to establish which of the disciplines usually covered during that placement period would be anticipated to be encountered during an LIC and consequently what additional educational resources and activities may need to be provided during the course of the placement period to ensure that all academic aims for the year are achieved. For example, those on a 1-year LIC may require a short period of time attached to a surgical ward, acute assessment unit, or emergency department.4,10
Ensuring that a planned LIC continues to meet regulatory standards (eg, GMC requirements in the United Kingdom) is another key step in the process.
Question 4: when should an LIC occur and how long should it be?
While an LIC may occur any time during the traditional ‘clinical phase’ of a medical degree, the majority of LICs occur in the penultimate year of the medical programme.2 It is argued that having further block rotations still to come following an LIC (in a final year) can allay the anxiety that some students experience during an LIC about gaps in their experience.77
There has been much debate about the ideal length of an LIC.2 Ellaway33 argues it needs to be of sufficient length for continuity to be established and provide opportunities to encounter the stipulated disciplines. If an LIC is too short, it may lead to increased student anxiety about the model, without realisation of the programme benefits. Brown et al9 believe that for the placement provider to see the potential shift from ‘net drain’ to ‘net contributor’ in terms of student service delivery, between 2 and 5 months of an LIC are required.33,66 The generally held consensus is that an LIC does not need to be longer than 12 months.34
Question 5: how will a typical week work?
To be successful, an LIC needs sufficient structure to facilitate the key aspects of continuity previously discussed.33 This structure can take a variety of forms. Students may follow a ‘patient panel’ (selected by their tutor to provide the agreed case mix linked to relevant learning outcomes) which the student will need to plan their own time to achieve. Students may also follow a more formally planned timetable, with no stipulated patient panel and less organisational burden upon students. A combination of these options is also possible.
A student’s typical week is likely to include a proportion of supervised clinic or ward time and time with their clinical tutor. Additional, planned learning sessions which link back to the core curriculum may also be utilised as another means to allay student fears about potential gaps during their time studying as part of an LIC.10,33 Students should have opportunity within their week for self-directed learning/unstructured time to follow-up and attend appointments with relevant patients, as well as to pursue areas of particular clinical interest. Unstructured time may also involve the completion of mandatory curricula elements, such as a student selected project.
The logistics and technology required to facilitate different aspects of an LIC week need consideration, for example, access to video-conferencing for core curriculum learning activities or sessions. So-called ‘flipped classroom’ teaching methods can lend themselves well to an LIC model.82
Question 6: how will students and tutors be recruited?
As LICs have tended to start on a small scale as part of an existing medical course, the majority are still an elective choice for students. As more schools deliver LICs (and on a larger scale), there are now examples of them being an integral part of the course for all students.78 For those that remain elective, the key question is how applying students are selected. As of yet, there are no consensus principles for selection and selection is either random or based on locally agreed criteria.33
The nature of the recruitment of tutors will very much depend on the local landscape, the type of LIC being developed, and what existing educational activity local clinicians are delivering. Mentor and organisational capacity require careful analysis as overburdening tutors could lead to mentor burnout and negatively impact student experience.33 In areas of workforce shortage, development of clinical teaching fellows in a joint arrangement between clinical providers and a school (to provide additional clinical and educational capacity) could be one way to address this challenge.
Key to the recruitment of both students and tutors is the provision of a clear vision and purpose about what the LIC is and what it will entail for the involved parties.79 Explanation regarding potential benefits is also important – for students, this could be evidence an LIC will not negatively affect examination performance, whereas for placement providers, the element of service delivery an LIC student can bring compared with students on shorter placements (after the first few months) may be a key point to highlight.33
Question 7: how will the LIC run alongside existing rotations?
With adequate planning, it should be possible to introduce an LIC to an existing course that runs in parallel to existing placements although, as suggested above, tutor capacity may affect the number of LIC places that can be accommodated. Consideration should be given about potential cross-over points between LICs and other rotations (eg, when an LIC student accompanies one of their patient panel to a hospital clinic or ward) and how this will be managed so that individual students and trainees are not disadvantaged.15
Question 8: how will assessment work?
As well as continuity of patient journey, support, and supervision, LICs also offer potential continuity in assessment. Despite this proposed benefit, some schools implementing LICs have encountered challenges aligning the placement with existing assessment arrangements,4 often deemed necessary for consistency when LICs operate alongside more traditional block rotations as a voluntary programme.21 Given this, summative assessments may not be constructively aligned to LIC student experience. As previously mentioned, this may decrease student engagement within an LIC as summative examinations approach and student focus shifts to passing poorly aligned examinations.55
Such challenges may be reduced by ensuring an LIC curriculum (particularly the curriculum’s learning outcomes) is aligned as closely as possible with the course assessment. However, this may prove difficult if institutions mandate assessment for voluntary LIC programmes must remain identical to the assessment of ‘block rotation’ students. In such situations, encouraging direct tutor discussion with students regarding their learning needs and eventual exams may prove beneficial to contextualise their LIC experience.72
While summative assessment arrangements may have to remain identical for all students, it may be possible to use different (although ideally comparable) tools for formative student assessment throughout an LIC. The supervisor continuity that develops during an LIC can make formative assessment particularly valuable. Bates et al71 found that students valued the informality and authenticity of the feedback they received during their LIC. Rather than simply assessing against a specific competency, LIC supervisors are perhaps more likely to be in a position to judge the subtly different competence.56
Question 9: how do you support students and mentors?
Depending on the type and location of an LIC, there is potential for LIC students to experience feelings of isolation from peers, friends, family, and the main body of the course.33 It is, therefore, important that the school takes steps to mitigate against this. This can include measures such as placing students in groups of two or more to ensure some peer support. In very rural areas, accessing health care for students themselves outside the setting of their own placement can also be a challenge.4
As discussed in the barriers to LIC implementation section of this work, there should be contingency planning for relationship failures and more widely regarding arrangements when, for whatever reason, a placement is not functioning as planned or a student needs additional support.33 Suitable arrangements to facilitate communication between LIC location and the wider medical school need to be in place for access to central learning resources and activities but also to reduce the risk of disconnect forming between the two. This applies to both learners and tutors – both should be made to feel part of the wider learning community of the school.
To support LIC tutors, faculty development arrangements must be robust, particularly in the early stages.77 The logistics of how this training will be delivered across the relevant geography needs consideration although, in many cases, tutors may already be within the existing medical school catchment.
Question 10: how can you best evaluate, and quality assure, an LIC?
At a school level, there is a variety of ways that an LIC and its implementation can be evaluated and quality assured. How this will be achieved should be considered during the LIC planning phase. It is important that any evaluation policy considers the effects on all the relevant stakeholders: patients, students, tutors, organisations, and communities.83 In terms of quality assurance, decisions need to be made as to whether data gathered will be against absolute or relative standards.84 Ellaway33 suggests that ‘longitudinality’ should also be a factor in the evaluation of LICs; the longer nature of placements mean they may take longer to assess and analyse fully. Necessary changes following feedback and highlighting such actions back to relevant stakeholders will be key steps as an LIC develops.
As discussed in the previous section on potential LIC challenges, the current diversity of the type and geography of LICs across the world has made comparison and analysis of the key contributing factors for the observed benefits difficult.2 As the number of LICs continues to increase across the globe, gathering evidence through collaboratives of similar models should help give meaningful scale and increase the significance of results.
Limitations to this narrative review
There are several limitations to this narrative overview. As established previously, there is a relative lack of UK literature regarding the development and implementation of LICs. This review has synthesised international literature in a format that considers UK context, yet further details of this context and specific enabling factors and barriers are likely to emerge as the body of UK-based LIC literature expands. This review offers a contemporary snapshot of the current LIC climate within the United Kingdom, which is subjected to further change. As a narrative overview of international literature, this work encounters limitations due to the chosen review format. It is held that unsystematic narrative reviews risk introducing bias from the author’s potential to omit, often inadvertently, relevant literature that may add to the review’s discussion or contradict the key points made.85 Despite this, a narrative review best serves the research aims of this work. Selection bias is a concern, yet the inclusion of an explicit methods section and structured literature search aims to address this issue.86 Narrative review use has facilitated the production of a contemporary overview of LIC development and implementation that considers context, ultimately generating recommendations for LIC application within a UK setting.22
Conclusions
This article has provided a narrative overview of international literature concerning the development and implementation of LICs. Particular focus has been given as to how this literature may be applied within a UK context. It is hoped that by summarising what an LIC is, along with potential benefits, enabling factors, and barriers to programme success, this review will assist medical educators considering the development of such a model. A practical application guide with 10 questions developers need to consider has been generated which summarises the key practical points of this review in a more easily digestible format.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All the authors made substantial contributions to drafting, revising, and approving the final version of the manuscript.
ORCID iD: Megan EL Brown  https://orcid.org/0000-0002-9334-0922
https://orcid.org/0000-0002-9334-0922
References
- 1. McKeown I, Parekh R. Longitudinal integrated clerkships in the community. Educ Prim Care. 2017;28:185–187. [DOI] [PubMed] [Google Scholar]
- 2. Worley P, Couper I, Strasser R, et al. A typology of longitudinal integrated clerkships. Med Educ. 2016;50:922–932. [DOI] [PubMed] [Google Scholar]
- 3. Walters L, Greenhill J, Richards J, et al. Outcomes of longitudinal integrated clinical placements for students, clinicians and society. Med Educ. 2012;46:1028–1041. [DOI] [PubMed] [Google Scholar]
- 4. Couper I, Worley P, Strasser R. Rural longitudinal integrated clerkships: lessons from two programs on different continents. Rural Remote Health. 2011;11:1665 https://www.rrh.org.au/journal/article/1665. Accessed January 2, 2019. [PubMed] [Google Scholar]
- 5. Hirsh D, Ogur B, Thibault GE, et al. New models of clinical clerkships: ‘continuity’ as an organizing principle for clinical education reform. N Engl J Med. 2007;356:858–866. [DOI] [PubMed] [Google Scholar]
- 6. Hudson J, Poncelet A, Weston M, et al. Longitudinal integrated clerkships. Med Teach. 2016;39:7–13. [DOI] [PubMed] [Google Scholar]
- 7. Von Pressentin KB, Waggie F, Conradie H. Towards tailored teaching: using participatory action research to enhance the learning experience of longitudinal integrated clerkship students in a South African rural district hospital. BMC Med Educ. 2016;16:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mennin S, Mennin R. Community based medical education. Clinical Teach. 2006;392:90–96. [Google Scholar]
- 9. Hudson JN, Thomson B, Weston KM, Knight-Billington PJ. When a LIC came to town: the impact of longitudinal integrated clerkships on a rural community of healthcare practice. Rural Remote Health. 2015;15:3333. [PubMed] [Google Scholar]
- 10. Poncelet A, Bokser S, Calton B, et al. Development of a longitudinal integrated clerkship at an academic medical center. Med Educ Online. 2011;16:5939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hirsh D, Gaufberg E, Ogur B, et al. Educational outcomes of the Harvard Medical School-Cambridge integrated clerkship: a way forward for medical education. Acad Med. 2012;87:643–650. [DOI] [PubMed] [Google Scholar]
- 12. Crampton P, McLachlan JC, Illing JC. A systematic literature review of undergraduate clinical placements in underserved areas. Med Educ. 2013;47:969–978. [DOI] [PubMed] [Google Scholar]
- 13. The British Medical Association (BMA). News: BMA report warns that doctors under pressure and patients at risk due to gaps in hospital rotas. https://www.bma.org.uk/news/media-centre/press-releases/2018/july/bma-report-warns-that-doctors-under-pressure-and-patients-at-risk-due-to-gaps-in-hospital-rotas. Up-dated 2018. Accessed March 17, 2019.
- 14. The British Medical Association (BMA). News: England will lose more than 600 GP practices by 2022 without urgent investment, BMA analysis reveals, 2018. https://www.bma.org.uk/news/media-centre/press-releases/2018/may/england-will-lose-more-than-600-gp-practices-by-2022-without-urgent-investment-bma-analysis-reveals. Up-dated 2018. Accessed March 17, 2019.
- 15. Myhre DL, Bajaj S, Woloschuk W. Practice locations of longitudinal integrated clerkship graduates: a matched-cohort study. Can J Rural Med. 2016;21:13–16. [PubMed] [Google Scholar]
- 16. Playford D, Ng W, Burkitt T. Creation of a mobile rural workforce following undergraduate longitudinal rural immersion. Med Teach. 2016;38:498–503. [DOI] [PubMed] [Google Scholar]
- 17. Majeed A. Shortage of general practitioners in the NHS. BMJ. 2017;358:j3191. [DOI] [PubMed] [Google Scholar]
- 18. NHS Year of Care partnerships. Care and support planning: the process. NHS. https://www.yearofcare.co.uk/process. Up-dated 2017. Accessed March 22, 2019.
- 19. Royal College of General Practice (RCGP). The 2022 GP. RCGP; https://www.rcgp.org.uk/policy/rcgp-policy-areas/general-practice-2022.aspx. Up-dated 2016. [Google Scholar]
- 20. Bartlett M, Muir F. A new model of undergraduate clinical education. Br J Gen Pract. 2018;68:216–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bartlett M, Dowell J, Graham F, et al. Dundee’s longitudinal integrated clerkship: drivers, implementation and early evaluation. Educ Prim Care. 2019;30:72–79. [DOI] [PubMed] [Google Scholar]
- 22. Ferrari R. Writing narrative style literature reviews. Medical Writing. 2015;24:230–235. [Google Scholar]
- 23. Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5:101–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Strasser R, Hirsh D. Longitudinal integrated clerkships: transforming medical education worldwide. Med Educ. 2011;45:436–437. [DOI] [PubMed] [Google Scholar]
- 25. Hirsh D, Worley P. Better learning, better doctors, better community: how transforming education can help repair society. Med Educ. 2013;47:942–949. [DOI] [PubMed] [Google Scholar]
- 26. Greenhill J, Poncelet AN. Transformative learning through longitudinal integrated clerkships. Med Educ. 2013;47:336–339. [DOI] [PubMed] [Google Scholar]
- 27. Takamura A, Ie K, Takemura Y. Overcoming challenges in primary care education: a trial of a longitudinal integrated clerkship in a rural community hospital setting in Japan. Educ Prim Care. 2015;26:122–126. [DOI] [PubMed] [Google Scholar]
- 28. Mundell L. Being an agent of change: a student’s view of the UK’s first yearlong longitudinal integrated clerkship (LIC). Educ Prim Care. 2018;29:121. [DOI] [PubMed] [Google Scholar]
- 29. Roberts C, Daly M, Held F, Lyle D. Social learning in a longitudinal integrated clinical placement. Adv Health Sci Educ Theory Pract. 2017;22:1011–1029. [DOI] [PubMed] [Google Scholar]
- 30. Konkin J, Suddards C. Students’ experiences of role, relationships and learning in two clerkship models. Med Educ. 2017;51:490–497. [DOI] [PubMed] [Google Scholar]
- 31. Ellaway R, Graves L, Berry S, Myhre D, Cummings BA, Konkin J. Twelve tips for designing and running longitudinal integrated clerkships. Med Teach. 2013;35:989–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Denz-Penhey H, Murdoch JC. Is small beautiful? Student performance and perceptions of their experience at larger and smaller sites in rural and remote longitudinal integrated clerkships in the Rural Clinical School of Western Australia. Rural Remote Health. 2010;10:1470. [PubMed] [Google Scholar]
- 33. Ellaway R. Commentary: what’s not to LIC? Adv Health Sci Educ Theory Pract. 2012;18:135–138. [DOI] [PubMed] [Google Scholar]
- 34. Hauer KE, O’Brien B, Poncelet AN. Longitudinal, integrated clerkship education: better for learners and patients. Acad Med. 2009;84:821. [DOI] [PubMed] [Google Scholar]
- 35. Birden H, Barker J, Wilson I. Effectiveness of a rural integrated clerkship in preparing medical students for internship. Med Teach. 2016;38:946–956. [DOI] [PubMed] [Google Scholar]
- 36. O’Brien BC, Poncelet AN, Hansen L, et al. Students’ workplace learning in two clerkship models: a multi-site observational study. Med Educ. 2012;46:613–624. [DOI] [PubMed] [Google Scholar]
- 37. Latessa R, Beaty N, Royal K, Colvin G, Pathman DE, Heck J. Academic outcomes of a community-based longitudinal integrated clerkships program. Med Teach. 2015;37:862–867. [DOI] [PubMed] [Google Scholar]
- 38. Poncelet AN, Hauer KE, O’Brien B. The longitudinal integrated clerkship. Virtual Mentor: AMA J Ethics. 2009;11:864–869. [DOI] [PubMed] [Google Scholar]
- 39. Teherani A, O’Brien BC, Masters DE, Poncelet AN, Robertson PA, Hauer KE. Burden, responsibility and reward: preceptor experiences with the continuity of teaching in a longitudinal integrated clerkship. Acad Med. 2009;84:S50–S53. [DOI] [PubMed] [Google Scholar]
- 40. Blitz J, de Villiers M, Van Schalkwyk S. Implications for faculty development for emerging clinical teachers at distributed sites: a qualitative interpretivist study. Rural Remote Health. 2018;18:4482. [DOI] [PubMed] [Google Scholar]
- 41. Connolly M, Sweet L, Campbell D. What is the impact of longitudinal rural medical student clerkships on clinical supervisors and hospitals. Aust J Rural Health. 2014;22:179–188. [DOI] [PubMed] [Google Scholar]
- 42. Couper I, Worley P. Meeting the challenges of training more medical students: lessons from Flinders University’s distributed medical education programme. Med J Aust. 2010;193:34–36. [DOI] [PubMed] [Google Scholar]
- 43. Walters L, Prideaux D, Worley P, et al. Demonstrating the value of longitudinal integrated placements for general practice preceptors. Med Educ. 2011;45:455–463. [DOI] [PubMed] [Google Scholar]
- 44. Snow SC, Gong J, Adams JE. Faculty experience and engagement in a longitudinal integrated clerkship. Med Teach. 2017;39:527–534. [DOI] [PubMed] [Google Scholar]
- 45. Cristobal F, Worley P. Can medical education in poor rural areas be cost-effective and sustainable: the case of the Ateneo de Zamboanga University School of Medicine. Rural Remote Health. 2012;12:1835. [PubMed] [Google Scholar]
- 46. Smith J, Jones P, Fink J, et al. Peer mentoring: evaluation of a new model of clinical placement in the Solomon Islands undertaken by an Australian Medical School. Rural Remote Health. 2015;15:3410. [Google Scholar]
- 47. Poncelet AN, Wamsley M, Hauer KE, Lai C, Becker T, O’Brien B. Patient views of continuity relationships with medical students. Med Teach. 2013;35:465–471. [DOI] [PubMed] [Google Scholar]
- 48. Hudson J, Weston K, Farmer E, et al. Are patients willing participants in the new wave of community-based medical education in regional and rural Australia? Med J Aust. 2010;192:150–153. [DOI] [PubMed] [Google Scholar]
- 49. Hudson JN, Knight PJ, Weston KM. Patient perceptions of innovative longitudinal integrated clerkships based in regional, rural and remote primary care: a qualitative study. BMC Fam Pract. 2012;13:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Somporn P, Ash J, Walters L. Stakeholder views of rural community-based medical education: a narrative review of the international literature. Med Educ. 2018;52:791–802. [DOI] [PubMed] [Google Scholar]
- 51. Omotara BA, Padonu MO, Yahya SJ. Assessment of the impact of community-based medical education of the University of Maiduguri on communities in three local government areas of Borno State, Nigeria: community leaders’ perspectives. Educ Health (Abingdon). 2004;17:6–16. [DOI] [PubMed] [Google Scholar]
- 52. Bonney A, Albert G, Hudson JN, et al. Factors affecting medical students’ sense of belonging a longitudinal integrated clerkship. AFP. 2014;43:53–57. [PubMed] [Google Scholar]
- 53. Epstein-Lubow G, Cineas S, Yess J, Anthony D, Fagan M, George P. Development of a longitudinal integrated clerkship at The Warren Alpert Medical School of Brown University. R I Med J (2013). 2015;98:27–31. [PubMed] [Google Scholar]
- 54. Caulfield M, Andolsek K, Grbic D, Roskovensky L. Ambiguity tolerance of students matriculating to U.S. Medical School. Acad Med. 2014;89:1526–1532. [DOI] [PubMed] [Google Scholar]
- 55. Wormald BW, Schoeman S, Somasunderam A, Penn M. Assessment drives learning: an unavoidable truth. Anat Sci Educ. 2009;2:199–204. [DOI] [PubMed] [Google Scholar]
- 56. Hirsh DA, Holmboe ES, ten Cate O. Time to trust: longitudinal integrated clerkships and entrustable professional activities. Acad Med. 2014;89:201–204. [DOI] [PubMed] [Google Scholar]
- 57. Bernstein J, Wood S, Latessa R, Hirsh DA. Teaching in longitudinal integrated clerkships: the seven ‘C’s. Clin Teach. 2019;16:101–107. [DOI] [PubMed] [Google Scholar]
- 58. Heddle W, Robertson G, Mahoney S, et al. Challenges in transformation of the ‘traditional block rotation’ medical student clinical education into a longitudinal clerkship model. Educ Health. 2014;27:138–142. [DOI] [PubMed] [Google Scholar]
- 59. Diuguid-Gerber J, Porter S, Quiah SC, et al. The Columbia-Bronx VA amalgamative clerkship: an effective, 12-week, integrated, longitudinal clinical experience. Med Educ Online. 2017;22:1301630. https://www.tandfonline.com/doi/full/10.1080/10872981.2017.1301630. Accessed March 22, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Teherani A, Irby DM, Loeser H. Outcomes of different clerkship models: longitudinal integrated, hybrid, and block. Acad Med. 2013;88:35–43. [DOI] [PubMed] [Google Scholar]
- 61. Ogur B, Hirsh D, Krupat E, Bor D. The Harvard Medical School–Cambridge integrated clerkship: an innovative model of clinical education. Acad Med. 2007;82:397–404. [DOI] [PubMed] [Google Scholar]
- 62. Poncelet AN, Mazotti LA, Blumberg B, Wamsley MA, Grennan T, Shore WB. Creating a longitudinal integrated clerkship with mutual benefits for an academic medical center and a community health system. Perm J. 2014;18:50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Deaville J, Grant A. Overcoming the pull factor of convenient urban living- Perceptions of rural general practice. Med Teach. 2011;33:e211–e217. [DOI] [PubMed] [Google Scholar]
- 64. Illing JC, Crampton PES. Collaborative relationships and learning in rural communities. Med Educ. 2015;49:852–854. [DOI] [PubMed] [Google Scholar]
- 65. Denz-Penhey H, Shannon S, Murdoch CJ, Newbury JW. Do benefits accrue from longer rotations for students in rural clinical schools? Rural Remote Health. 2005;5:414. [PubMed] [Google Scholar]
- 66. Hudson JN, Weston KM, Farmer EA. Medical students on long-term regional and rural placements: what is the financial cost to supervisors? Rural Remote Health. 2012;12:1951. [PubMed] [Google Scholar]
- 67. Mol SSL, Chen HC, Steerneman AHM, de Groot E, Zwart DLM. The feasibility of longitudinal patient contacts in a large Medical School. Teach Learn Med. 2018;26:1–8. [DOI] [PubMed] [Google Scholar]
- 68. Greenhill J, Fielke KR, Richards JN, et al. Towards an understanding of resilience in longitudinal integrated clerkships. BMC Med Educ. 2015;15:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Blitz J, de Villiers M, van Schalkwyk S. Designing faculty development: lessons learnt from a qualitative interpretivist study exploring students’ expectations and experiences of clinical teaching. BMC Med Educ. 2019;19:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Alegria DAH, Boscardin C, Poncelet A, Mayfield C, Wamsley M. Using tablets to support self-regulated learning in a longitudinal integrated clerkship. Med Educ Online. 2014;19:23638 https://www.tandfonline.com/doi/full/10.3402/meo.v19.23638. Accessed March 20, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bates J, Konkin J, Suddards C, Dobson S, Pratt D. Student perceptions of assessment and feedback in longitudinal integrated clerkships. Med Educ. 2013;47:362–374. [DOI] [PubMed] [Google Scholar]
- 72. Goldman S. Enhancing adult learning in clinical supervision. Acad Psychiatry. 2011;35:302–306. [DOI] [PubMed] [Google Scholar]
- 73. Sandhu P, Wylie A, Jakeways N, Kirtchuk L. Clinical humanities in primary care for year 2 medical students: a student perspective [published online ahead of print September 4, 2018]. MedEdPublish. doi: 10.15694/mep.2018.0000193.1 https://www.mededpublish.org/manuscripts/1890. Accessed March 22, 2019. [DOI] [PMC free article] [PubMed]
- 74. The University of Sheffield. Longitudinal placements – Resources for tutors – Teaching – AUPMC – Research – The Medical School – The University of Sheffield. https://www.sheffield.ac.uk/medicine/research/aupmc/teaching/resources. Accessed March 22, 2019.
- 75. Ellaway RH, Graves L, Cummings B. Dimensions of integration, continuity and longitudinality in clinical clerkships. Med Educ. 2016;50:912–921. [DOI] [PubMed] [Google Scholar]
- 76. Varpio L, Bell R, Hollingworth G, et al. Is transferring an educational innovation actually a process of transformation? Adv Health Sci Educ Theory Pract. 2012;17:357–367. [DOI] [PubMed] [Google Scholar]
- 77. Hudson J, Farmer E, Weston K, Bushnell JA. Using a framework to implement large-scale innovation in medical education with the intent of achieving sustainability. BMC Med Educ. 2015;15:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Hogenbirk JC, French MG, Timony PE, Strasser RP, Hunt D, Pong RW. Outcomes of the Northern Ontario School of Medicine’s distributed medical education programmes: protocol for a longitudinal comparative multicohort study. BMJ Open. 2015;5:e008246. https://bmjopen.bmj.com/content/5/7/e008246. Accessed March 22, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Grobler L, Marais BJ, Mabunda SA, et al. Interventions for increasing the proportion of health professionals practicing in rural and other underserved areas. Cochrane Database of Syst Rev. 2009;1:CD005314. [DOI] [PubMed] [Google Scholar]
- 80. Hogenbirk JC, Mian O, Pong RW. Postgraduate speciality training in northeastern Ontario and subsequent practice location. Rural Remote Health. 2011;11:1603. [PubMed] [Google Scholar]
- 81. Brodsky D, Newman L. Educational perspectives: a systematic approach to curriculum development. NeoReviews. 2010;12:e2–e7. https://neoreviews.aappublications.org/content/12/1/e2. Accessed April 4, 2019. [Google Scholar]
- 82. Bernstein J, Wood S. Clerkship Didactics: Re-Examining Our Pedagogical Approach Within Longitudinal Integrated Curricula. Society of Teachers of Family Medicine, Educational Column; 2014. https://www.stfm.org/publicationsresearch/publications/educationcolumns/2017/march/. Accessed March 22, 2019. [Google Scholar]
- 83. Fish D, Coles C. Medical Education: Developing a Curriculum for Practice. Maidenhead, UK: Open University Press; 2005. [Google Scholar]
- 84. Dolmans D, Stalmeijer RE, van Berkel HJM, Wolfhagen HAP. Quality assurance of teaching and learning: enhancing the quality culture. In: Dornan T, Mann KV, Scherpbier AJJA, Spenc4er J, eds. Medical Education: Theory and Practice. Amsterdam, The Netherlands: Elsevier Health Sciences; 2011:257–264. [Google Scholar]
- 85. Montori V, Swiontkowski M, Cook D. Methodologic issues in systematic reviews and meta-analyses. Clin Orthop Relat Res. 2003;413:43–54. [DOI] [PubMed] [Google Scholar]
- 86. Grant MJ, Booth A. A typology of review: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26:91–108. [DOI] [PubMed] [Google Scholar]