Abstract
Prostate cancer ranks second among male cancers in the United States in terms of death rate. Robot-assisted surgery (RAS) is now offered as the standard surgical procedure performed for radical prostatectomy. Urinary incontinence and erectile dysfunction were common complications after RAS prostatectomy. Patients felt ill-prepared after surgery, resulting in negative impacts on their quality of life. Pelvic floor muscle exercise is prioritized for patients with mild-to-moderate incontinence. The purpose of this study was to examine the effects of using resistance band pelvic floor muscle exercise for patients after RAS prostatectomy. A preexperimental single-group study was conducted for this study. A total of 43 patients completed the program. Urinary incontinence scale, Incontinence Impact Questionnaire, and Hospital Anxiety and Depression Scale were assessed at 0.5 months, 1 month, 2 months, and 3 months after urinary catheter removal. The results revealed that urinary incontinence, life impact, and depression and anxiety improved significantly as time went on. This study suggests that using simple and easy-to-learn resistance band pelvic floor muscle exercise program at home can benefit patients financially and reduce travel time.
Keywords: men’s health programs, health-care issues, prostate cancer, oncology/cancer, prostatectomy
Prostate cancer is the second deadliest cancer among men in the United States (American Cancer Society, 2018) and ranks sixth in Taiwan.
Robot-assisted surgery (RAS) is the standard surgical method for performing radical prostatectomy. Advantages of using RAS are reduced morbidity, less blood loss, and reduced length of hospital stay (Pal & Koupparis, 2018). Yet many patients experience moderate-to-severe urinary incontinence right after RAS prostatectomy; the percentage is as high as 74.3%, dropping to 46.8% after 1 month, 21.4% after 3 months, 13.6% after 6 months, and 9% after 12 months (Glazener et al., 2011; Ko et al., 2012). Incontinence seriously undermines quality of life. In addition to creating difficulties for patients in terms of socializing and hygiene, it is associated with negative self-awareness of health condition, reduced ability to perform daily activities, social isolation, and increased burden for caregivers, and thus the personal impact may be severe (Haylen et al., 2010).
Carrier, Edwards, and Harden (2018) documented that urinary incontinence and erectile dysfunction are common complications of radical prostatectomy; they found that patients felt ill-prepared for such changes after surgery, which negatively impacted their quality of life. A study conducted by Sallami (2017) revealed that risk factors affecting postoperative urinary incontinence include patients’ age, body mass index (BMI), sphincter defects, unstable bladder, surgical preservation of neurovacsular strips, and the extent of bleeding.
Research has shown that pelvic floor muscle exercises (Kegel exercises) can improve urinary incontinence and erectile dysfunction after prostatectomy (Fernández et al., 2015; Goonewardene, Gillatt, & Persad, 2018; Sayılan & Özbaş’s, 2018) and are a high priority for nonsurgical treatment (Yani et al, 2018). Furthermore, Park et al. (2018) observed that a change in hip extensor muscle strength was the only significant parameter predicting achievement of continence. Hung, Hsiao, Chih, Lin, and Tsauo (2011) emphasized that pelvic floor muscle contraction exercises should begin as soon as possible after surgery. But they found no significant difference between exercise under the guidance of a physical therapist and exercise at home performed by the patient alone, as long as patients received oral and written instructions from health-care professionals (Cavkaytar, Kokanali, Topcu, Aksakal, & Doğanay, 2015).
Urinary continence can be achieved through contraction training of the pelvic floor muscles. In the clinical setting, oral guidance is the most common approach to instructing patients on pelvic floor exercises. Patients are directed to try to hold urine or to reach a finger through the anus into the rectum to feel the muscles surrounding the anus squeeze the finger. In clinical practice, many older post-RAS patients complain about the difficulty of using “imagination” to practice pelvic floor muscle exercises. Resistance bands are a common training tool for reinforcing muscle strength. Resistance band exercises are designed to induce contraction of the muscle group of the pelvic floor, taking advantage of the strength applied by the abductor of the hip joint plus the rectus. The bands are easy to carry, low cost, very safe, multifunctional, and well suited to training at home. They are a good muscle strength–training option for older people with relatively poor muscle fitness.
Pelvic floor muscle exercises are a priority for patients with mild-to-moderate incontinence after RAS. Resistance bands have become a widely used tool for training muscle strength, as it may be difficult for patients to travel to and from the hospital on a weekly basis. Few studies, however, have investigated the use of resistance bands for pelvic floor muscle contraction exercises to ameliorate urinary incontinence after prostatectomy. Therefore, the objective of this study was to evaluate the efficacy of resistance band exercises for improving urinary incontinence, quality of life, and anxiety and depression after radical prostatectomy.
Methods
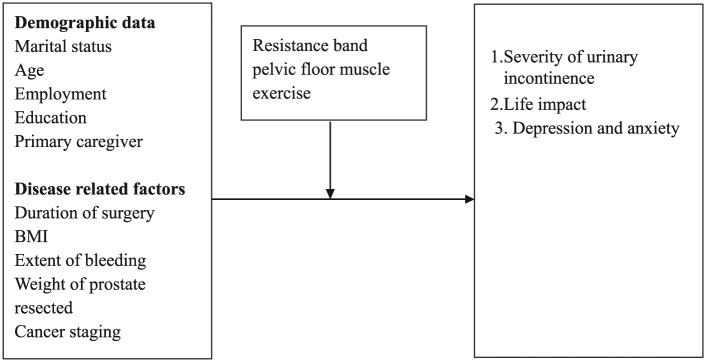
This is a preexperimental single-group study with the resistance band pelvic floor muscle exercise program as the intervention. The research design is presented in Figure 1. The researcher taught patients and their families during hospitalization to use the resistance band at home after discharge to facilitate pelvic floor muscle contraction exercises.
Figure 1.
Research design. BMI = body mass index.
This study was carried out in the urology unit of a teaching hospital in northern Taiwan. The inclusion criteria were (a) age 40 years or above, (b) capable of verbal communication, (c) capable of getting out of bed and moving around without assistance from others after surgery, (d) no urinary incontinence before surgery, and (e) no urinary tract infection after surgery. Patients who were not able to lie in a supine position for the resistance band exercises were excluded from this study.
Participants who fulfilled the inclusion criteria had their rights explained to them by the researcher and they provided written consent before they were enrolled in the study.
Method of Guidance
The researcher provided guidance on a one-on-one basis. The patient and family members watched a resistance band exercise video. Then a DVD and one resistance band were given to the patient (a TheraBand five-foot resistance band, red, with medium resistance). The patient was asked to demonstrate the exercise in bed to make sure that both the patient and the family members understood the instructions and were able to use the resistance band.
Exercise at home began after the urinary catheter was removed (around 7 to 10 days after surgery).
Exercise
Step 1: Align both ends of the resistance band and tie a knot to produce a loop (Figure 2, Picture 1).
Step 2: Lie down and bend the knees to place both legs inside the loop, with the resistance band beneath the knees (Figure 2, Picture 2).
Step 3: Apply force to keep the knees apart and raise the buttocks, then hold the position and count from 1 to 10, and then slowly lower the buttocks (Figure 2, Picture 3). This is one repetition.
Step 4: Do 20 repetitions each time, 3 times a day for a total of 60 repetitions a day (Figure 2, Picture 4).
Figure 2.
Resistance band exercise.
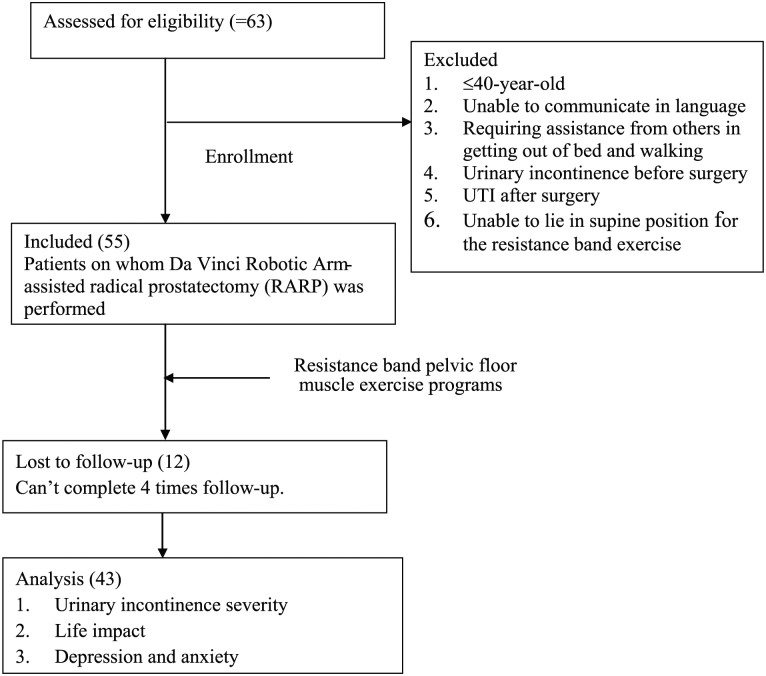
Also, the researcher worked with the doctor by arranging a visit to the hospital at 2 weeks, 1 month, 2 months, and 3 months after removal of the urinary catheter. During these visits, the researcher conducted a one-on-one interview with the patient at the clinic. Patients were asked to complete a structured questionnaire independently or under the guidance of the researcher. Data were collected through four questionnaires (each consisted of three forms and required 20 min; every time the patient completed a questionnaire, the study nurse gave the patient a gift certificate worth $3–4 as a gesture of thanks for doing so). A total of 55 patients were interviewed in the longitudinal follow-up survey. Of these, 12 were unable to complete the four follow-up interviews. As a result, a total of 43 patients completed the study, a completion rate of 78.2%. The flow chart showing the study design is presented in Figure 3.
Figure 3.
Flow chart. RARP = robotic arm–assisted radical prostatectomy; UTI = urinary tract infection.
Instruments
Demographic Data
The participants’ baseline characteristics were recorded, including age, BMI, marital status, primary caregivers, occupation, prostate weight, and cancer stage. In addition, several risk factors for incontinence, such as advanced age, obesity, comorbidity index, and prostate volume, were also included in this study.
Urinary Incontinence Scale After Radical Prostatectomy
The Urinary Incontinence Scale after Radical Prostatectomy (UISRP) was developed by Lin and Yang (2010)
who investigated prostate cancer patients who underwent radical prostatectomy. The Cronbach’s α coefficient was 0·90. Two-week test–retest reliability (intraclass correlation coefficient [ICC] = 0·56; 95% CI [0·26, 0·72]) and criterion-related validity was r = 0·74, p < ·001. The scale contained 14 questions to be answered on a 5-point Likert scale (1–5 points indicating never, rarely, sometimes, often, always). Higher scores indicate greater severity of incontinence.
Incontinence Impact Questionnaire
This study also used the Chinese version of the Incontinence Impact Questionnaire (IIQ) created by Lin and Dougherty (2003). It employs a 4-point Likert Scale (1–4 points: not at all, slightly, moderately, and greatly). The scale contains 30 questions that cover four domains: emotional health (8 questions), physical activity (6 questions), travel (6 questions), and social relationships (10 questions). Higher scores indicate greater impact on the patient’s daily life. The Cronbach’s α for the Chinese version of the IIQ is 0.97, and the Cronbach’s α for the subscales of physical activity, travel, social relationships, and emotional health are 0.88, 0.89, 0.93, and 0.97, respectively.
Hospital Anxiety and Depression Scale
The study also used the Hospital Anxiety and Depression Scale (HADS) for physical disorders developed by Zigmond and Snaith (1983). HADS contains 14 questions, with 7 questions each in the anxiety and depression subscales. Each question has a 4-point response scale (0–3 points) and each subscale is scored separately. A higher score indicates a greater degree of anxiety or depression. The developers of the HADS have recommended the following cutoff points to identify mild (8–10), moderate (11–14), and severe (15–21) anxiety or depression. Cronbach’s α for HADS in HADS-A (anxiety) varied from .68 to .93 (mean .83) and for HADS-D (depression) from .67 to .90 (mean .82), indicating a good tool.
After receiving permission from the human research ethics committee of the Chang Gung Medical Foundation (IRB No.101-4459C), the researchers obtained written consent from each participant and started carrying out the research program.
Data Analysis
The patient’s baseline characteristics, including age, BMI, marital status, primary caregiver, occupation, surgery type, prostate weight, and prostate cancer stage, were collected and analyzed descriptively. Generalized estimating equation (GEE) was used to analyze the differences in degree and impact of urinary incontinence, impact of urinary incontinence, and hospital anxiety and depression at 2 weeks, 1 month, 2 months, and 3 months after catheter removal in patients who underwent radical prostatectomy.
Results
Patients’ Baseline Characteristics
A total of 55 patients were initially included in this study, but 12 patients were lost to follow-up, with the result that 43 patients completed the program. The mean age of participants was 65 ± 6 years. The great majority of participants (93%) were married. More than two thirds (72.1%) had graduated from high school or above. The duration of surgery, blood loss volume, BMI, preoperative prostate-specific antigen (PSA) index, and resected prostate weights are presented in Table 1.
Table 1.
Patient’s Baseline Characteristics.
| (n =
43) |
|||
|---|---|---|---|
| Category | n (%) | M | SD |
| Mean age | 65 | 6.0 | |
| <60 | 11 (25.6) | ||
| 60–70 | 25 (58.1) | ||
| >70 | 7 (16.3) | ||
| Marital status | |||
| Married | 40 (93.0) | ||
| Single | 3 (7.0) | ||
| Education | |||
| Primary school | 7 (16.3) | ||
| Junior high school | 5 (11.6) | ||
| Senior high school | 7 (16.3) | ||
| College or above | 24 (55.8) | ||
| Employment status | |||
| No | 26 (60.5) | ||
| Yes | 17 (39.5) | ||
| Mean duration of surgery | 294 | 38 | |
| 300 min or longer | 19 (44.2) | ||
| Less than 300 min | 24 (55.8) | ||
| Mean extent of bleeding | 151 | 122 | |
| 100 cc or less | 12 (27.9) | ||
| 100–199 cc | 19 (44.2) | ||
| 200 cc or more | 12 (27.9) | ||
| Mean BMI | 25.0 | 2.8 | |
| 25 or less | 22 (51.2) | ||
| Over 25 | 21 (48.8) | ||
| Mean preoperative PSA | 9.7 | 6.6 | |
| Less than 4 | 4 (9.3) | ||
| 4–10, inclusive | 24 (55.8) | ||
| More than 10 | 15 (34.9) | ||
| Mean weight of prostate | 47 | 17.0 | |
| 50 g or less | 30 (69.8) | ||
| Over 50 g | 13 (30.2) | ||
Note. BMI = body mass index; PSA = prostate-specific antigen.
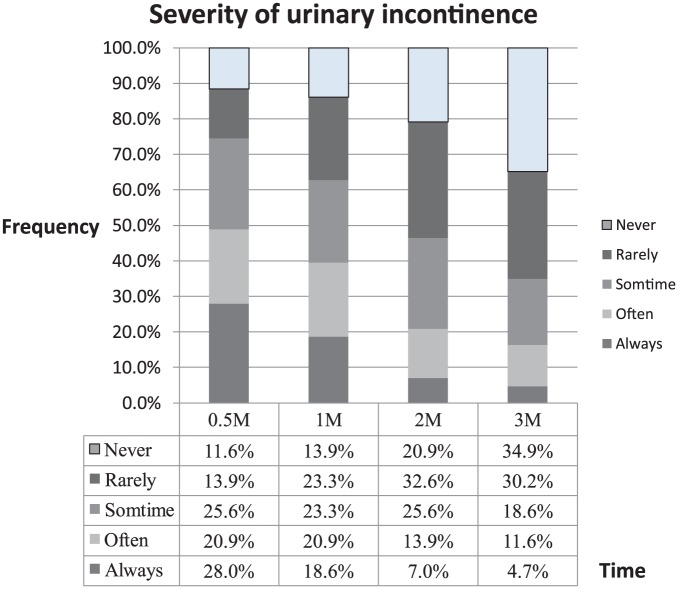
Urinary Incontinence Severity
The mean scores for urinary incontinence severity at four different evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 47.6 ± 19.3, 43.4 ± 14.4, 36.4 ± 12.6, and 29.4 ± 7.0 points, respectively. Significant statistical differences were found at these different time points (2 weeks vs. 1 month after catheter removal, B = −0.4, p = .001 and 2 weeks vs. 2 months after catheter removal, B = −0.9, p = .018; Table 1). Results indicated that the degree of urinary incontinence was most severe at 2 weeks after catheter removal, with more than three fourths (88.4%, n = 38) of patients having varying degrees of urinary incontinence and nearly half of those (48.9%, n = 21) suffering from severe urinary incontinence. However, 11.6% (n = 5) patients never had incontinence and only 16% always or frequently had incontinence in the third month after catheter removal (Table 2; Figure 4).
Table 2.
Urinary Incontinence Severity, the Impact of Urinary Incontinence on Daily Life, and Severity of Anxiety and Depression After Intervention.
| (n =
3) |
||||||
|---|---|---|---|---|---|---|
| After postoperative urinary catheter removal | GEE models |
|||||
| Mean | SD | B | p | 95% CI |
||
| Lower | Upper | |||||
| Urinary incontinence severity | ||||||
| 0.5 months | 47.6 | ±19.3 | 0.0 | |||
| 1 month | 43.4 | ±14.4 | −0.4 | .001** | −0.5 | −0.2 |
| 2 months | 36.4 | ±12.6 | −0.9 | .018* | −1.6 | −0.2 |
| 3 months | 29.4 | ± 7.0 | −1.3 | .546 | −5.3 | 2.8 |
| The impact on daily life | ||||||
| Impact on physical activities | ||||||
| 0.5 months | 14.4 | ±6.0 | 0.0 | |||
| 1 month | 13.2 | ±5.4 | −0.3 | .003** | −0.5 | −0.1 |
| 2 months | 11.4 | ±4.2 | −0.5 | .000*** | −0.7 | −0.4 |
| 3 months | 9.6 | ±4.2 | −0.8 | .000*** | −1.2 | −0.5 |
| Impact on social relationships | ||||||
| 0.5 months | 24 | ±10 | 0.0 | |||
| 1 month | 22 | ±8 | −0.2 | .002** | −0.4 | −0.1 |
| 2 months | 19 | ±7 | −0.5 | .000*** | −0.8 | −0.3 |
| 3 months | 17 | ±7 | −0.7 | .000*** | −1.0 | −0.4 |
| Impact on emotional health | ||||||
| 0.5 months | 18.3 | ±6.4 | 0.0 | |||
| 1 month | 16.8 | ±6.4 | −0.2 | .065 | −0.4 | 0.01 |
| 2 months | 15.2 | ±5.6 | −0.4 | .000*** | −0.6 | −0.2 |
| 3 months | 12.8 | ±4.8 | −0.6 | .000*** | −0.9 | −0.4 |
| Impact on travel | ||||||
| 0.5 months | 15.0 | ±6.0, | 0.0 | |||
| 1 month | 13.2 | ±5.4 | −0.3 | .003** | −0.5 | −0.1 |
| 2 months | 11.4 | ±4.8 | −0.6 | .000*** | −0.8 | −0.3 |
| 3 months | 9.6 | ±4.8 | −0.9 | .029* | −1.7 | −0.1 |
| Severity of anxiety and depression | ||||||
| 0.5 months | 12.5 | ±7.8 | 0.0 | |||
| 1 month | 11.7 | ±8.2 | −0.8 | .325 | −2.4 | 0.8 |
| 2 months | 9.7 | ±7.6 | −2.5 | .008** | −4.3 | −0.7 |
| 3 months | 7.0 | ±7.0 | −5.2 | .000*** | −7.3 | −3.1 |
Note. GEE = generalized estimating equation.
p < .05. **p < .01. ***p < .001.
Figure 4.
Incidence of urinary incontinence after intervention.
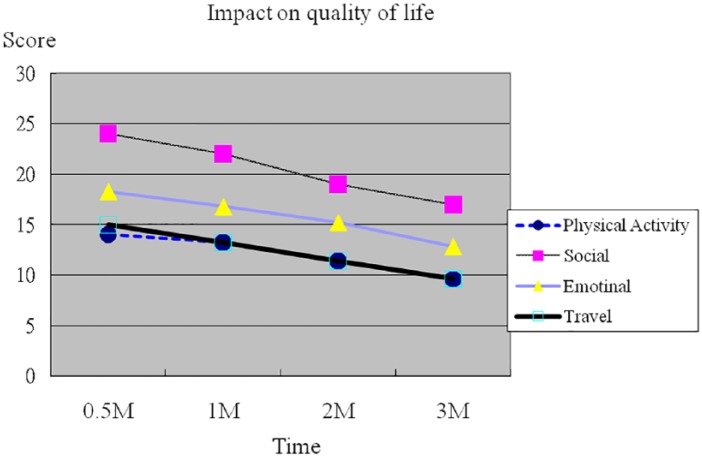
Impact on Daily Life
The impact of urinary incontinence on daily life included four domains: emotional health, physical activity, travel, and social relationships (Figure 5). The results are as follows:
Figure 5.
Graphs of the impact on the four domains of quality of life after intervention.
(1) Impact on physical activities.
Results from the four evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 14.4 ± 6.0, 13.2 ± 5.4, 11.4 ± 4.2, and 9.6 ± 4.2 points, respectively. Significant statistical differences were found between measurements at different time points (2 weeks vs. 1 month after catheter removal, B = −0.3, p = .003; 2 weeks vs. 2 months after catheter removal, B = −0.5, p < .001; and 2 weeks vs. 3 months after catheter removal, B = −0.8, p < .001). The degree of impact on patients’ physical activity was greatest at 2 weeks after catheter removal and the impact decreased gradually thereafter (Table 2; Figure 3).
(2) Impact on social relationships.
In terms of the impact of post-prostatectomy incontinence on social relationships, results from the four evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 24 ± 10, 22 ± 8, 19 ± 7, and17 ± 7 points, respectively. Significant statistical differences were found between measurements from different points in time (2 weeks vs. 1 month after catheter removal, B = −0.2, p = .002; 2 weeks vs. 2 months after catheter removal, B = −0.5, p < .001; and 2 weeks vs. 3 months after catheter removal, B = −0.7, p < .001). The degree of impact on patients’ social relationships was the greatest at 2 weeks after catheter removal and the impact decreased gradually thereafter (Table 2; Figure 3).
(3) Impact on emotional health.
Results on the emotional health subscale at four evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 18.3 ± 6.4, 16.8 ± 6.4, 15.2 ± 5.6, and 12.8±4.8 points, respectively. Significant statistical differences were found among measurements from different points in time (2 weeks vs. 1 month after catheter removal, B = −0.2, p = .065; 2 weeks vs. 2 months after catheter removal, B = −0.4, p < .001; and 2 weeks vs. 3 months after catheter removal, B = −0.6, p < .001). The impact on patients’ emotional health was the greatest at 2 weeks after catheter removal and the impact decreased gradually thereafter (Table 2; Figure 3).
(4) Impact on travel.
Regarding the impact of urinary incontinence on travel, results from the four evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 15.0 ± 6.0, 13.2 ± 5.4, 11.4 ± 4.8, and 9.6 ± 4.8 points, respectively. Significant statistical differences were found among these data (2 weeks vs. 1 month after catheter removal, B = −0.3, p = .003; 2 weeks vs. 2 months after catheter removal, B = −0.6, p < .001; 2 weeks vs. 3 months after catheter removal, B = −0.9, p < .029). The degree of impact on patients’ travel was the highest at 2 weeks after catheter removal and decreased gradually after that (Table 2; Figure 3).
Severity of Anxiety and Depression
Results on anxiety and depression at the four evaluation time points (2 weeks, 1 month, 2 months, and 3 months after urinary catheter removal) were 12.5 ± 7.8, 11.7 ± 8.2, 9.7 ± 7.6, and 7.0 ± 7.0 points, respectively. Statistically significant differences were noted among the measurements (at 2 weeks vs. 1 month after catheter removal, B = −0.8, p = .325; 2 weeks vs. 2 months after catheter removal, B = −2.5, p = .008; 2 weeks vs. 3 months after catheter removal, B = −5.2, p < .001; Table 2).
The Influence of Urinary Incontinence on Patients’ Baseline Characteristics, Overall Daily Life, and Anxiety and Depression
Results showed no significant differences in basic attributes, such as age, marital status, education, duration of surgery, extent of bleeding, BMI, PSA, or resected prostate weight, among others.
Table 3 reveals that greater severity of urinary incontinence corresponded to greater impact on patients’ overall daily quality of life. Urinary incontinence had a significant influence on patients’ physical activity (β = .74, p < .001), social relationships (β = .70, p < .001), emotional health (β = .75, p < .001), and travel (β = .73, p < .001). Furthermore, greater severity of urinary incontinence also corresponded to higher anxiety (β = .10, p < .001) and depression (β = .12, p < .001) scores.
Table 3.
Influence of Urinary Incontinence on the Overall Daily Life, and Anxiety and Depression After Intervention.
| Item | Beta | Lower | Upper | p value |
|---|---|---|---|---|
| Overall impact on daily life | 0.81 | 0.55 | 1.08 | .000*** |
| Impact on physical activity | 0.74 | 0.52 | 0.96 | .000*** |
| Impact on social relationships | 0.70 | 0.49 | 0.91 | .000*** |
| Impact on emotional health | 0.75 | 0.49 | 1.02 | .000*** |
| Impact on travel | 0.73 | 0.47 | 0.98 | .000*** |
| Overall Impact on anxiety and depression | 0.07 | 0.04 | 0.09 | .000*** |
| Impact on anxiety | 0.10 | 0.07 | 0.14 | .000*** |
| Impact on depression | 0.12 | 0.07 | 0.17 | .000*** |
Note. *p < .05. **p < .01. ***p < .001.
Discussion
This study presents evidence of improvement in the severity of urinary incontinence, impact on daily life, and anxiety and depression among RARP patients after a resistance band pelvic floor muscle exercise program. Results showed that urinary incontinence, life impact, and depression and anxiety all improved significantly as time went on and patients continued the exercise program. Urinary incontinence was most severe at 2 weeks after catheter removal. This finding supported those of Ko et al. (2012) and Palisaar et al. (2014), which indicated a high incidence of incontinence in the early stages after catheter removal. Therefore, in this study, the resistance band pelvic floor muscle exercises began as soon as the urinary catheter was removed after surgery. The benefits could indeed be observed after patients began muscle strength training. Haylen et al. (2010) observed that urinary incontinence seriously undermines quality of life and is associated with self-perception of compromised health and social isolation. Haylen’s study also revealed that severe incontinence not only affects daily life but also increases patients’ anxiety and depression. By practicing simple and easy-to-learn band pelvic floor muscle exercises, slight improvements in the severity of patients’ urinary incontinence were evident over time. The impact of incontinence on daily life and on the extent of anxiety and depression also gradually ameliorated after surgery.
Sayılan and Özbaş’s study (2018) used the Kegel exercise program (three sessions daily) with 30 patients after prostatectomy; 10% of them had no urinary incontinence 10 days after the urinary catheter was removed; 20% of them at 1 month after surgery; and 23.3% at 3 months after surgery. Results of the current study showed that of the 43 patients who engaged in resistance band pelvic floor muscle contraction exercises, 11.6% had no urinary incontinence at 14 days; 13.9% at 1 month; and 34.9% at 3 months. Resistance band exercises appeared to yield superior results to those obtained by Sayılan and Özbaş using Kegel exercises.
Resistance band pelvic floor muscle exercise precisely induces contraction of the muscle group of the pelvic floor, taking advantage of the strength applied by the abductor of the hip joint plus the rectus. Park et al., 2018 and Hung et al. (2011) indicated in their study that as long as patients receive guidance from health-care professionals on how to perform pelvic floor muscle exercises, there is no significant difference in the benefits from exercise performed at home and at the hospital. Prostate cancer tends to occur among men ages 65 years and above. These patients are often retired. They no longer have salary income and their children are working and thus unable to accompany them often to the hospital to do pelvic floor muscle exercises. A resistance band costs only a few dollars and patients can practice the pelvic floor muscle contraction exercises themselves independently at home without assistance from family members. These are a simple, convenient, and cost-effective form of targeted exercise. In sum, the benefits of resistance bands are they are easy to use, easy to carry, easy to learn, and financially affordable; they save health-care costs and time traveling to the hospital for rehabilitation. Pelvic floor exercises performed using a resistance band are proven to reduce urinary incontinence and improve quality of life following radical prostatectomy.
This study has several limitations: The use of nonprobability sampling precludes generalizability of findings; this study was conducted at only one medical center; and there was no control group due to the limited number of surgical patients and longitudinal period. Future studies should use longitudinal designs, include more health-care institutions, as well as add a control group.
Conclusions and Clinical Implications
Postoperative urinary incontinence is a common clinical care issue for patients considering undergoing prostatectomy. In addition to informing patients of why urinary incontinence may occur, nurses are responsible for providing guidance, teaching them a simple and easy-to-learn pelvic floor muscle contraction exercise using a resistance band.
The resistance band pelvic floor exercise program should be used routinely with patients who undergo robotic arm–assisted radical prostatectomy. Resistance bands should be included in hospitals’ out-of-pocket, on-hand materials lists, with one resistance band provided to each patient during guidance. The patient can scan the QR code generated by the nurse to watch the training material demonstrating the pelvic floor exercise program and can move along with what is shown in the video to add fun to the exercise. In addition, it is advised that timings for exercise be set as alarms on a mobile phone to facilitate consistent exercise.
Footnotes
Authors’ Note: All authors have participated sufficiently in the work to take public responsibility for appropriate portions of the content after receiving permission from the human research ethics committee of the Hospital (IRB No.101-4459C). Li-Hui Pan is also affiliated to School of Nursing, Chang Gung University of Science and Technology, Taoyuan City.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Chang Gung Memorial Hospital (grant number CMRPG3B0621).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Li-Hui Pan  https://orcid.org/0000-0001-5262-4163
https://orcid.org/0000-0001-5262-4163
References
- American Cancer Society. (2018). Cancer facts & figures 2018. Atlanta: American Cancer Society; Retrieved from https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2018.html [Google Scholar]
- Carrier J., Edwards D., Harden J. (2018). Men’s perceptions of the impact of the physical consequences of a radical prostatectomy on their quality of life: A qualitative systematic review. JBI Database of Systematic Reviews and Implementation Reports, 16(4), 892–972. doi: 10.11124/JBISRIR-2017-003566 [DOI] [PubMed] [Google Scholar]
- Cavkaytar S., Kokanali M. K., Topcu H. O., Aksakal O. S., Doğanay M. (2015). Effect of home-based Kegel exercises on quality of life in women with stress and mixed urinary incontinence. Journal of Obstetrics and Gynaecology, 35(4), 407–410. doi: 10.3109/01443615.2014.960831 [DOI] [PubMed] [Google Scholar]
- Fernández R. A., García-Hermoso A., Solera-Martínez M., Correa M. T. M., Morales A. F., Martínez-Vizcaíno V. (2015). Improvement of continence rate with pelvic floor muscle training post-prostatectomy: A meta-analysis of randomized controlled trials. Urology International, 94(2), 125–132. doi: 10.1159/000368618 [DOI] [PubMed] [Google Scholar]
- Glazener C., Boachie C., Buckley B., Cochran C., Dorey G., Grant A., … Vale L. (2011). Conservative treatment for urinary incontinence in Men after Prostate Surgery (MAPS): Two parallel randomised controlled trials. Health Technology Assessment, 15(24):1–290. doi: 10.3310/hta15240 [DOI] [PubMed] [Google Scholar]
- Goonewardene S. S., Gillatt D., Persad R. (2018). A systematic review of PFE pre-prostatectomy. Journal of Robotic Surgery, 12(3), 397–400. doi: 10.1007/s11701-018-0803-8 [DOI] [PubMed] [Google Scholar]
- Haylen B. T., de Ridder D., Freeman R. M., Swift S. E., Berghmans B., Lee J., … Schaer G. N. (2010). An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. International Urogynecology Journal, 21(1), 5–26. doi: 10.1007/s00192-009-0976-9 [DOI] [PubMed] [Google Scholar]
- Hung H.-C., Hsiao S.-M., Chih S.-Y., Lin H.-H., Tsauo J.-Y. (2011). An alternative intervention for urinary incontinence: Retraining diaphragmatic, deep abdominal and pelvic floor muscle coordinated function. Manual Therapy, 15(3), 273–279. doi: 10.1016/j.math.2010.01.008 [DOI] [PubMed] [Google Scholar]
- Ko Y. H., Coelho R. F., Chauhan S., Sivaraman A., Schatloff O., Cheon J., Patel V. R. (2012). Factors affecting return of continence three months after robot assisted radical prostatectomy: Analysis from a large, prospective data by a single surgeon. Journal of Urology, 187(1), 190–195. doi: 10.1016/j.juro.2011.09.037 [DOI] [PubMed] [Google Scholar]
- Lin Y. H., Yang M. S. (2010). Assessing the reliability and validity of a urinary incontinence scale after radical prostatectomy. International Journal of Urological Nursing, 4(3), 118-124. doi: 10.1111/j.1749-771X.2010.01103.x [DOI] [Google Scholar]
- Lin S.-Y., Dougherty M. C. (2003). Incontinence impact, symptom distress and treatment-seeking behavior in women with involuntary urine loss in Southern Taiwan. International Journal of Nursing Studies, 40(3), 227–234. doi: 10.1016/s0020-7489(02)00081-0 [DOI] [PubMed] [Google Scholar]
- Pal R. P., Koupparis A. J. (2018). Expanding the indications of robotic surgery in urology: A systematic review of the literature. Arab Journal of Urology, 16(3), 270–284. doi: 10.1016/j.aju.2018.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palisaar J. R., Roghmann F., Brock M., Löppenberg B., Noldus J., von Bodman C. (2014). Predictors of short-term recovery of urinary continence after radical prostatectomy. World Journal of Urology, 33(6), 771–779. doi: 10.1007/s00345-014-1340-3 [DOI] [PubMed] [Google Scholar]
- Park J., Yoon D. H., Yoo S., Cho S. Y., Cho M. C., Han G.-Y., … Jeong H. (2018). Effects of progressive resistance training on post-surgery incontinence in men with prostate cancer. Journal of Clinical Medicine, 7(9), pii: E292, 2–10. doi:10.3390/jcm7090292 7(9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallami S. (2017). Predictive factors of urinary incontinence after radical prostatectomy: Systematic review. La Tunisie Medicale, 95(4), 229–235. [PubMed] [Google Scholar]
- Sayılan A. A., Özbaş A. (2018). The effect of pelvic floor muscle training on incontinence problems after radical prostatectomy, American Journal of Men’s Health, 12(4).1007–1015. doi: 10.1177/1557988318757242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yani M. S., Wondolowski J. H., Eckel S. P., Kulig K., Fisher B. E., Gordon J. E., Kutch J. J. (2018). Distributed representation of pelvic floor muscles in human motor cortex. Scientific Reports, 8(1), 7213. doi: 10.1038/s41598-018-25705-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]