Abstract
This study aimed to investigate the current contract rate and residents’ willingness to contract with general practitioner (GP) services in Guangzhou, China, during the policy trial phase, and also to explore the association of behavior contract and contract willingness with variables based on Andersen’s Behavioral Model of Health Services Use (ABM). In total, 160 residents from community health centers (CHCs) and 202 residents from hospitals were recruited in this study. The outcome variables were behavior contract and contract willingness. Based on the framework of ABM, independent variables were categorized as predisposing factors, enabling factors, need factors, and CHC service utilization experiences. Univariate and multivariate logistic regression analysis models were applied to explore the associated factors. Out of 362 participants, 14.4% had contracted with GP services. For those who had not contracted with GP services, only 16.4% (51 out of 310) claimed they were willing to do so. The contract rate for community-based participants was significantly higher than that for hospital-based participants. Major reasons for not choosing to contract were perceiving no benefit from the service and concerns about the quality of CHCs. Community health center experiences and satisfaction were significantly associated with contracting among hospital-based participants. A need factor (diagnosed with hypertension or diabetes) and CHC service utilization experiences (have gotten services from the same doctor in CHCs) were significantly associated with contract willingness among CHC-based participants. Intervention to improve awareness of GP services may help to promote this service. Different intervention strategies should be used for varying resident populations.
Keywords: general practitioner, contract willingness, primary health care, Andersen’s Behavioral Model of Health Services Use
What do we already know about this topic?
Since 2016, Chinese government has begun to promote contracts with general practitioner (GP) services in urban areas on a large scale to guide residents seeking health services in primary health care level; however, little is known about the willingness to contract GP services from the perspective of residents.
How does your research contribute to the field?
This is one of the first studies to investigate behavior contract and contact willingness to GP services and the associated factors based on Andersen’s Behavioral Model of Health Services Use, during the new GP services policy trial phase among residents in China.
What are your research’s implications toward theory, practice, or policy?
The prevalence of behavior contract and contract willingness were unfavorable during the trial phase in Guangzhou, especially among hospital-based participants. Unaware of the availability of GP services and primary health care qualities were the major reasons of uncontracting or unwilling to contract, and the associated factors vary among community health center (CHC)-based participants and hospital-based participants; therefore, different intervention strategies should be used for varying populations.
Introduction
Many developed countries have established the gatekeeper system in health care in which the primary care physician (PCP) plays a central role.1,2 In this system, PCPs are the patient’s first point of contact. Primary care physicians coordinate and manage patients’ overall care. Often internists and general practitioners (GPs), they diagnose and treat registered patients as well as provide health promotion and health management services. More importantly, they determine whether patients need to be referred to specialists, and in this sense are the gatekeepers to other sources in the health care system. Studies have shown that the gatekeeper system plays a key role in controlling health care cost; increasing the efficiency of the health care system; and providing convenient, continuous, comprehensive health care services to the public.3 In countries where they play an important role in the health care system, 90% of disease- or health-related problems can be solved by PCPs with only complex or rare conditions referred to specialists in secondary or tertiary hospitals.4
China has been in the process of establishing the gatekeeper system in health care since 2009. The most persistent obstacle to achieving this goal is patients’ underuse of primary health care and overuse of tertiary hospital-based health care.5,6 One reason for this imbalance is that patients are free to enter all types of medical institutions, including primary care facilities (community health centers [CHCs] in urban areas and township health centers in rural areas) and non-primary health institutions (secondary and tertiary hospitals), with no appointments or referrals necessary. Another reason is that the quality of care in tertiary hospitals is better than that in primary health care institutions. For these reasons, officials hope to improve the quality of primary health care and at the same time establish the gatekeeper system. One of the goals of the gatekeeper system is that patients with common or frequently occurring diseases and chronic diseases are to be treated at the primary health care level.7 With the quality of primary health care improving in China, the gatekeeper system will guide the public to make their first contact at primary level institutions with GPs as their PCPs. Therefore, contracting for GP services (also known as family doctor services) is under development as the chosen approach to guide the public into the system and take the first steps in establishing gatekeeper health care.8
General practitioner services in China are provided by a health care team in CHCs in urban areas. The team includes general physicians, nurses, and public health physicians.8 If residents contract with GP services, GP teams will provide them with primary health care services including health management, disease control, health assessment, and referral if it is needed. General practitioner services in China are mainly focused on generalist clinical care and basic public health services covered by the government’s public health program. Since 2009, many cities such as Beijing, Shanghai, and Shenzhen have initiated trials to establish the GP system. Since 2016, China has begun to promote contracts with GP services in urban areas on a large scale. New policy guidelines for promoting GP services were published which required that by the year 2017, 30% of the population should be contracted with GPs, and 60% of priority populations, such as the elderly, chronic disease patients, and mental health patients, should be covered for care.8 The hope has been that the GP system will attract more people into making their first contact at a primary health care institution and thus allow the GP to control and oversee their progress through the health care system. However, the prevalence of contracts with GP services among Chinese urban residents is currently not favorable.9-14
Despite news reports that the contract rate is increasing in China, little original local research has investigated the willingness to contract GP services from the perspective of residents. Previous Chinese studies focused mainly on evaluating the effects of GP services in improving health outcomes15,16 or discussing the optimal operating mechanism of the service.17-19 In pilot cities, some studies investigated residents’ contract rates and willingness to contract, but few of them examined residents’ reasons for refusing or failing to contract, especially during the new GP policy trial phase which was the critical phase for developing policy intervention.9-14 Furthermore, these studies did not include participants at hospital level, which may lead to selection bias. Finally, only limited research investigated the association factors with willingness to contract services based on a certain theoretical framework.
Andersen’s Behavioral Model of Health Services Use (ABM) is widely used in studies on health service utilization.20-30 It provides a framework for describing and understanding individuals’ decision to use health care services. We consider the dependent variables in this study, contracted with GP services and willingness to contract, as health care utilization, which is similar to other published studies.26,31-33 Therefore, we applied ABM as a conceptual framework to guide the investigation. According to this model, an individual’s willingness to contract GP services is influenced by 3 factors: predisposing, enabling, and need factors. Predisposing factors such as sociodemographic characteristics may influence use indirectly: for example, age and gender are related to illness and health which may in some way influence the individual’s health utilization. Enabling factors such as types of health insurance at both personal and community level may facilitate or impede the use of health services. Need factors include a perceived need or evaluated need. Perceived need refers to how people view their health status and the severity of their symptoms or disease while evaluated need refers to a professional assessment of people’s need for certain health services.34 In addition to these 3 factors in ABM, according to a previous study in China, the experience or satisfaction of CHCs were significantly associated with willingness to contract.12 Experiences in CHCs and satisfaction with CHCs are not under the ABM framework, but the experience of using CHCs where GP services are provided influences the willingness to contract/contract with GP services. Therefore, it is a significant variable to be measured, and we developed variables related to experiences in CHCs in the study.
The purpose of this study was to investigate the current contract rate of GP services and willingness to contract among residents in Guangzhou and also to examine the association of behavior contract and contract willingness with variables based on ABM.
Methods
This study was conducted in the Haizhu District of Guangzhou from September to November in 2015. Guangzhou is the capital of Guangdong Province in southern China and has a population of 14 million; it is one of the first cities to promote GPs contract services in China. Haizhu is the first district in Guangzhou to pilot the GP services contract since 2015.
Sampling
Stratified random sampling was applied to recruit participants. First, CHCs were divided into 2 levels according to whether there were more than one secondary or tertiary hospital within a radius of 1 km. At each level, a CHC was selected by simple random sampling and then the nearest secondary and tertiary hospitals were selected. According to the sample size calculation, we needed at least 340 samples in total or 170 samples at each stratification. Finally, we reached 397 potential participants and a total of 362 respondents completed the questionnaires. The overall response rate was 91%. Participants were Guangzhou registered permanent residents aged 18 years or older who agreed to sign the informed consent form and were recruited in the waiting area of an outpatient department for chronic diseases. Next, we conducted a face-to-face questionnaire interviews in a quiet place while participants were waiting for their consultations. It took 10 to 15 minutes to complete the questionnaire. Those who had difficulty understanding the interview questions were excluded. The study protocol was approved by the ethics review committee of the School of Public Health at Sun Yat-sen University.
Measures
A questionnaire was designed based on literature review and under the framework of ABM.
Behavior contract and contract willingness
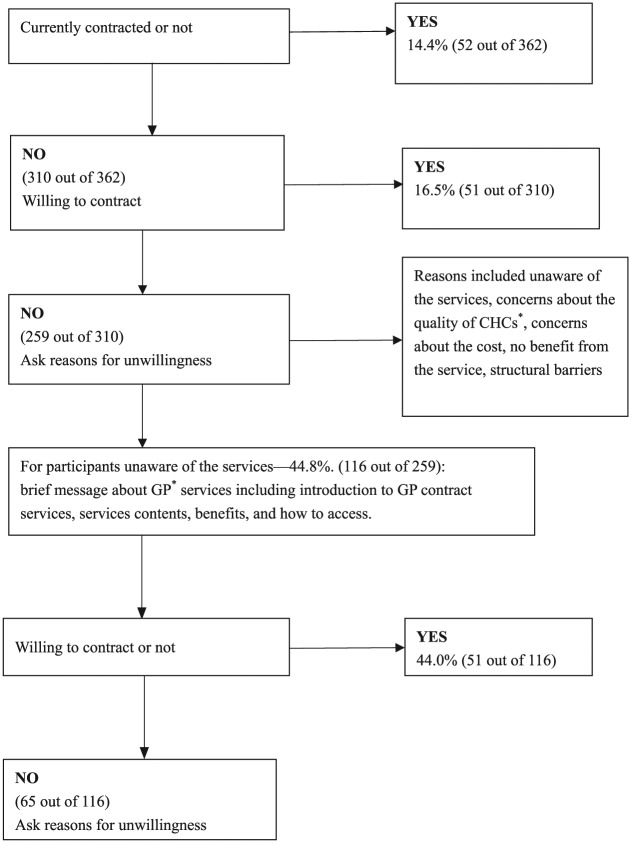
The dependent variables of this study were residents’ behavior contract (contracted with GP services) and contract willingness (willingness to contract with GP services). Behavior contract was defined specifically as participants currently contracted with GP services. All participants were first asked whether they were currently contracted with GP services. Contract willingness was defined specifically targeting participants not contracted with GP services, who were asked about their willingness to contract. Participants not willing to contract were asked their reasons for not doing so. Afterward, those who reported being unaware of the services were introduced to them. A brief message identified the types of services, benefits of the services, and how to access the services. Finally, after message delivery, these participants were asked again about their willingness to contract with GP services and reasons for unwillingness (see Figure 1).
Figure 1.
Flow chart for measuring residents’ behavior contract and contract willingness in Guangzhou, China.
Note. CHC = community health centers; GP = general practitioner.
Predisposing factors
According to the ABM, predisposing factors are defined as individual characteristics that exist prior to an individual’s illness or the onset of their need for health care services, which may affect their utilization of health services indirectly.34 Predisposing factors include demographic and social structural characteristics (age and gender, education, marital status, family size). Family size was measured by the number of family members.
Enabling factors
Enabling factors refer to external condition factors which permit individuals to satisfy their needs for health services.34 In this study, family income, types of health insurance (Urban Employee Basic Medical Insurance [UEBMI], Urban Residents’ Basic Medical Insurance [URBMI], New Rural Cooperative Medical System [NRCMS], others), social support (measured by Oslo 3-item Social Support Scale),31 and whether participants have paid attention to health-related information were measured as enabling factors.
China now has 3 main types of health insurance. UEBMI covers all employees from state-owned enterprises, private enterprises, public institutions, social organizations, and non-government organizations in urban areas. Those who are not employed in urban areas (eg, students) are covered by URBMI; rural populations are covered by the NRCMS. Medical Assistance for Poverty, Civil Servant Medical Insurance for national civil servants, and other kinds of commercial health insurance were grouped as other types of health insurance in this study.
Need factors
Need factors are defined as direct causes of health services use. That is to say, people will first perceive an illness or probability of illness and then seek health services or treatments.34 Need factors were divided into perceived health and evaluated health. In this study, measures of perceived health include perceived health status (categorized as very good, good, ordinary, bad, very bad) and perceived severity of hypertension or diabetes (categorized as slight, moderate, severe, no idea). Objective health status measured by hypertension or diabetes condition (whether diagnosed with hypertension or diabetes) and length of disease history.
Experiences in CHCs
A previous study in China noted that experiences with and attitudes toward CHCs might influence the willingness to contract GP services.12 Experience of utilization of CHCs, where GP services are provided, would in turn influence the willingness to contract/contract with GP services. Therefore, we included measures for experience using CHC health care (Do you have any medical care experience in CHCs?); referral experience (Have you been referred to specialists in CHCs?); satisfaction with CHCs (categorized as strongly dissatisfied, dissatisfied, neutral, satisfied, strongly satisfied); having gotten services from the same physician in CHCs (Do you consult the same doctor every time you need medical treatment?).
Statistical Analysis
To differentiate between the factors’ influence on community-based residents and on hospital-based residents, stratified analysis was applied. We first used univariate analysis to investigate the association between variables mentioned above and dependent variables. Then, age, gender, marital status, and education level were treated as confounders in the multivariate regression model to evaluate the association. Two multivariate regression models were separately built among community-based residents and hospital-based residents. Statistical significance was defined by P value <.05. Data of this study were analyzed with SPSS20.0.
Results
Sociodemographic Characteristics, Behavior Contract, and Willingness to Contract With GP Services Among Guangzhou Residents
In total, 362 participants were aged from 40 to 91 years, and the mean age was 65. 77.9% were married. 12.8% had a post-secondary education level or above, and 41.1% had completed high school. 54.4% participants had 3 or more family members.
Out of 362 participants, 44.2% (160/362) of participants were recruited from CHCs and 55.8% (202/362) from a secondary or tertiary hospital. Gender, marital status, and education variables were comparable between these 2 groups. Only age and number of family members were significantly different. 44.4% (71 out of 160) of participants from CHCs were ≥65 years old while 60.9% (123 out of 202) from hospitals were that age. Participants from CHCs had a larger family size with 63.8% (102 out of 160), having more than 3 family members compared to 47.0% (95 out of 202) of hospital-based participants (see Table 1).
Table 2.
Reasons for Unwillingness to Contract With GPs Before and After Message Delivery of the GP Contract Service Information Among Residents in Guangzhou, China.
| Col % (n) | ||
|---|---|---|
| Before briefing (n1 = 259) |
After briefing (n2 = 65) |
|
| Unaware of the service | 44.8 (116) | — |
| Benefits and necessity of contract service | 38.6 (100) | 90.8 (59) |
| No significant benefits of contract services | 21.2 (55) | 55.4 (36) |
| Do not need the service now | 17.4 (45) | 35.4 (23) |
| Concerns about quality of services in CHCs | 36.6 (95) | 38.5 (25) |
| Doctors’ quality of services in CHCs | 26.2 (68) | 15.4 (10) |
| Variety and quality of medicine and medical devices in CHCs | 10.4 (27) | 23.1 (15) |
| Concerns about the cost | 10.8 (28) | 13.8 (9) |
| Structural barriers | 6.9 (18) | 15.4 (10) |
| Inconvenience of CHCs | 6.2 (16) | 15.4 (10) |
| Inaccessibility of contracts/services | 0.7 (2) | 0 (0) |
Note. GP = general practitioner; CHC = community health center. The bolded values indicated the sum of proportion of the subdomains.
14.4% of participants (52 out of 362) had contracted with GP services. For those who had not contracted with GPs before, 16.4% (51 out of 310) claimed they were willing to contract. The contract rate in community-based participants was 23.8% (38 out of 160), which was significantly higher than that in hospital-based participants (6.9%, 14 out of 202). 13.1% (16 out of 122) of uncontracted participants from CHCs were willing to contract, which was comparable with hospital-based participants (18.6%, 35 out of 188) (see Table 1).
Table 1.
Behavior Contract/Willingness and Factors Based on Andersen’s Behavioral Model of Health Services Use Among Residents in Guangzhou, China.
| All N = 362 |
Community n = 160 |
Hospital n = 202 |
χ2 (P) | |
|---|---|---|---|---|
| Contract with GPs | ||||
| Currently contracted with general practitioners | 18.56 (<.001) | |||
| No | 85.6 (310) | 76.3 (122) | 93.1 (188) | |
| Yes | 14.4 (52) | 23.8 (38) | 6.9 (14) | |
| Willing to contract with general practitioners (N′= among 310 who did not have contract with GPs) | n = 122 | n = 188 | 0.94 (.333) | |
| No | 83.5 (259) | 86.9 (106) | 81.4 (153) | |
| Yes | 16.5 (51) | 13.1 (16) | 18.6 (35) | |
| Predisposing factors | ||||
| Age | 7.27 (.007) | |||
| <65 | 46.4 (168) | 55.6 (89) | 39.1 (79) | |
| ≥65 | 53.6 (194) | 44.4 (71) | 60.9 (123) | |
| Gender | 0.80 (.372) | |||
| Male | 38.4 (139) | 33.8 (54) | 42.1 (85) | |
| Female | 61.6 (223) | 66.3 (106) | 57.9 (117) | |
| Marital status | 1.68 (.195) | |||
| Married | 77.9 (282) | 81.3 (130) | 75.2 (152) | |
| Co-habitant/divorced/widow | 22.1 (80) | 18.8 (30) | 24.8 (50) | |
| Education | 0.37 (.544) | |||
| High school or below | 46.1 (167) | 48.8 (78) | 44.1 (89) | |
| College or above | 53.9 (195) | 51.3 (82) | 55.9 (113) | |
| Family member | 6.87 (.009) | |||
| <3 people | 45.6 (165) | 36.3 (58) | 53.0 (107) | |
| ≥3 people | 54.4 (197) | 63.8 (102) | 47.0 (95) | |
| Enabling factors | ||||
| Family per capita income monthly | 5.75 (.016) | |||
| <$450 | 38.1 (138) | 45.0 (72) | 32.7 (66) | |
| ≥$450 | 61.9 (224) | 55.0 (88) | 67.3 (136) | |
| Health insurance | 7.15 (.307) | |||
| UEBMI | 67.7 (245) | 69.4 (111) | 66.3 (134) | |
| URBMI | 18.5 (67) | 16.9 (27) | 19.8 (40) | |
| NRCMS | 2.2 (8) | 1.9 (3) | 2.5 (5) | |
| Other types | 3.3 (12) | 2. 5 (4) | 4.0 (8) | |
| None | 8.3 (30) | 9.4 (15) | 7.4 (15) | |
| Pay attention to health-related information | 0.91 (.341) | |||
| No | 11.0 (40) | 8.8 (14) | 12.9 (26) | |
| Yes | 89.0 (322) | 91.3 (146) | 87.1 (176) | |
| Social support* | 6.08 (.048) | |||
| Weak | 17.4 (63) | 11.3 (18) | 22.3 (45) | |
| Moderate | 30.9 (112) | 33.1 (53) | 29.2 (59) | |
| Strong | 51.6 (187) | 55.6 (89) | 48.5 (98) | |
| Need factors | ||||
| Perceived health status in the last month | 0.88 (0.347) | |||
| Very bad/bad | 24.0 (87) | 25.6 (41) | 22.8 (46) | |
| Very good/good/ordinary | 76.0 (275) | 74.4 (119) | 77.2 (156) | |
| Diagnosed with hypertension or diabetes | 3.39 (.066) | |||
| No | 22.4 (81) | 27.5 (44) | 18.3 (37) | |
| Yes | 77.6 (281) | 72.5 (116) | 81.7 (165) | |
| Length of hypertension or diabetes history, y | 1.48 (0.223) | |||
| <8 | 42.0 (118) | 46.6 (54) | 38.8 (64) | |
| ≥8 | 58.0 (163) | 53.4 (62) | 61.2 (101) | |
| Perceived severity of hypertension or diabetes | 3.41 (.065) | |||
| Slight/unknown | 35.2 (99) | 26.7 (31) | 41.2 (68) | |
| Severe/moderate | 64.8 (182) | 73.3 (85) | 58.8 (97) | |
| Experience with CHCs | ||||
| Have experience in consulting in CHCs | 21.32 (<.001) | |||
| No | 29.8 (108) | 5.0 (8) | 49.5 (100) | |
| Yes | 70.2 (254) | 95.0 (152) | 50.5 (102) | |
| Have referral experience in CHCs | 81.21 (<.001) | |||
| No | 83.4 (302) | 73.8 (118) | 91.1 (184) | |
| Yes | 16.6 (60) | 26.3 (42) | 8.9 (18) | |
| Have gotten services from the same doctor in CHCs | 15.74 (<.001) | |||
| No/never visited CHCs before | 71.5 (259) | 60.6 (97) | 80.2 (162) | |
| Yes | 28.5 (103) | 39.4 (63) | 19.8 (40) | |
| Satisfaction with the services in CHCs | 88.21 (<.001) | |||
| Never visited CHCs before | 29.8 (108) | 5.0 (8) | 49.5 (100) | |
| Strongly dissatisfied/Dissatisfied/Neutral | 15.7 (57) | 15.6 (25) | 15.8 (32) | |
| Satisfied/Strongly satisfied | 54.4 (197) | 79.4 (127) | 34.7 (70) | |
Note. Other types: any type of medical assistant, Civil Servant Medical Insurance and commercial health insurance. Social support is measured by Oslo 3-item Social Support Scale. GP = general practitioner; UEBMI = Urban Employee Basic Medical Insurance; URBMI = Urban Residents Basic Medical Insurance; NRCMS = New Rural Cooperative Medical System; CHC = community health center.
P < .05.
Reasons for Unwillingness to Contract With GPs
Out of the 259 participants who were unwilling to contract with GPs, 44.8% of respondents claimed they were not aware of the GP contract service. For example, most of them stated, “I didn’t know the CHC had this service.” 38.6% of respondents considered there was no significant benefit or necessity to contract with GPs. They claimed, “Contracts make no difference” or “I am healthy now and I do not need this service.” 36.6% of respondents were unwilling to contract GP services because of concerns about the quality of services in CHCs, including the quality of physicians (26.2%), shortage of medicine, and medical devices examination and readiness (10.4%), as indicated in the following statement: “I am a little worried about the quality of doctors in CHC.” Finally, 10.8% were concerned about the cost of such services and 6.9% met some structural barriers including inconvenience of distance to CHC: “CHC is quite far from my home” and inaccessibility of contracts/services with GPs: “I don’t know where to sign the contract” (see Table 2).
A total of 116 respondents who stated they were unaware of the GP services contract were introduced to its contents, benefits, and access information on the spot. The willingness to contract was assessed again for these participants, and 56.0% (65 out of 116) were still unwilling to contract GP services. Their related questions and reasons are shown in Figure 1 and Table 2.
Variables Related to ABM
All variables related to the ABM are shown in Table 1. Out of 362 participants, 77.6% were diagnosed with hypertension or diabetes with an average disease history of 8 years. 70.2% had been to CHCs for medical consultation and 16.6% had referral experience. 54.4% felt satisfied or strongly satisfied with CHCs. Variables were comparable between community-based participants and hospital-based participants except for family income (≥$450/mo 55.0% vs 67.3%, P = .016) and variables related to CHC experiences.
The Association Between Variables Related to Anderson’s Behavioral Model of Health Services Use and Behavior Contract and Contract Willingness
According to stratified analysis, experiences of medical-related consulting in CHCs (AORh = 4.17; 95% confidence interval (CI), 1.11-15.68; P < .05) and satisfaction with CHCs (satisfied vs never visited CHCs AORh = 4.24; 95% CI, 1.06-16.88; P < .05) were significantly associated with behavior contract among hospital-based participants but not community-based participants (see Table 3).
Table 3.
Associations Between Variables and Behavior Contract/Willingness With GPs Among Residents Recruited From Different Venues in Guangzhou, China.
| Community-based participants | Hospital-based participants | |||||
|---|---|---|---|---|---|---|
| Contracted/willing to contract Row% (n) | OR (95% CI) | AORc (95% CI) | Contracted/willing to contract Row% (n) | OR (95% CI) | AORh (95% CI) | |
| Associations between variables and contracts | ||||||
| Experience with CHCs | ||||||
| Have experience in consulting in CHCs | ||||||
| No | 12.5 (1) | 1 | 1 | 3.0 (3) | 1 | 1 |
| Yes | 24.3 (37) | 2.25 (0.27-18.91) | 2.30 (0.27-19.44) | 10.8 (11) | 3.91 (1.06-14.46)* | 4.17 (1.11-15.68)* |
| Satisfaction with the services in CHCs | ||||||
| Never visited CHCs before | 12.5 (1) | 1 | 1 | 3.0 (3) | 1 | 1 |
| Strongly dissatisfied/Dissatisfied/Neutral | 16.0 (4) | 1.33 (0.13-14.01) | 1.29 (0.12-13.70) | 9.4 (3) | 3.34 (0.64-17.47) | 4.01 (0.74-21.58) |
| Satisfied/Strongly satisfied | 26.0 (33) | 2.46 (0.29-20.73) | 2.55 (0.30-21.70) | 11.4 (8) | 4.17 (1.07-16.33)* | 4.24 (1.06-16.88)* |
| Associations between variables and contract willingness | ||||||
| Need factors | ||||||
| Diagnosed with hypertension or diabetes | ||||||
| No | 0.0 (0) | 1 | 1 | 13.9 (5) | 1 | 1 |
| Yes | 18.6 (16) | —a | —a | 19.7 (30) | 1.52 (0.55-4.25) | 1.40 (0.49-3.98) |
| Experience with CHCs | ||||||
| Have gotten services from the same doctor in CHCs | ||||||
| No/never visited CHCs before | 8.0 (6) | 1 | 1 | 18.5 (28) | 1 | 1 |
| Yes | 21.3 (10) | 3.11 (1.05-9.23)* | 5.29 (1.43-19.53)* | 18.9 (7) | 1.03 (0.41-2.57) | 1.03 (0.40-2.68) |
Note. All factors based on Andersen’s Behavior Model of Health Service Use in Table 2 were included in analysis; those statistically significant are shown here. AORh and AORc: adjusted for age, gender, marital status, and education. GP = general practitioner; OR = odds ratio; AORc=adjusted odds ratio for community-based participants; AORh=adjusted odds ratio for hopital-based participants; CI = confidence interval; CHC = community health center.
OR and AOR are absent because of a zero in the table.
Bolded values indicated *: P < .05.
Diagnosed with hypertension or diabetes and have gotten services from the same doctor in CHCs (AORc = 5.29; 95% CI, 1.43-19.53; P < .05) were significantly associated with contract willingness among community-based participants, while none of these variables were significant among hospital groups (see Table 3).
Discussion
This is one of the first studies to investigate behavior contract and contact willingness to GP services during the new GP services policy trial phase among residents in China. Our results showed that the prevalence of behavior contract and contract willingness were unfavorable during the trial phase in Guangzhou, especially among hospital-based participants. Influence factors of behavior contract and contract willingness were different among hospital-based participants and community-based participants.
The contract rate in our study was 14.4%, which is relatively low compared to that of previous studies in other cities in China. One study reported that the contract rate was 70.08% among 1200 participants in the Pudong New Area in Shanghai in 2012.35 Another study conducted in 2014 in Shanghai reported that 30.2% of 1021 participants had contracted with GPs.9 The contract rate among 11 CHCs in Beijing in 2015 was around 30% to 80%.11 Possible reasons for these significant differences are as follows: first, all these studies were conducted among the general population. Second, participants in Shanghai’s and Beijing’s surveys were recruited from CHCs whereas participants in our study were recruited from CHCs and hospitals. This study showed that the contract rate among community-based participants was significantly higher than that among hospital-based participants. Furthermore, Shanghai and Beijing have established a more developed primary health care system than other cities in the country. Residents of Shanghai and Beijing might therefore have more positive experiences in CHCs, and in this case, there would be a higher prevalence of behavior contract with GP services.
It was interesting to find that behavior contract was associated with having health services experience with CHCs and satisfaction with CHC services, and these associations were observed only among hospital-based participants. Meanwhile, the association between contract willingness and having health services from the same physician in CHCs was only observed among community-based participants. The reason for CHC experiences associations not existing among community-based participants is possibly that these people were residents who usually used primary health care. Therefore, their regular experiences in CHCs might not be sufficient to affect their decision on contracting, except when they have a familiar doctor in CHCs with whom they would contract for GP services. In this case, the doctor has built trust with these patients and thus facilitates contracting or willingness to contract. This point is related to the quality of care in CHCs, especially regarding doctors’ quality. Residents’ focus on quality of care in CHCs was also reported in another finding in this study. One of the major reasons for participants’ failure to contract GP services was their concern about the quality of care in CHCs, including the quality of doctors, medicine, and medical devices. The quality of care a doctor provides plays a critical role in promoting GP services. A similar study on GP contract services found that lack of high-quality GPs was an obstacle in building patients’ trust.35 A study from Hong Kong reported that the main cause of a low community-based first contact rate was distrust of PCPs with lower education.5 Hence, several projects have been launched to improve the quality of primary care. At this stage, with limited human resources in primary health care in China, our finding suggests that intentionally introducing better doctors from CHCs to patients who never contracted before would facilitate the willingness to sign up for GP services. On the other hand, more research is warranted to estimate workloads and appropriate payment incentives for GP teams during the ongoing large-scale promotion of GP services. Finally, our finding suggests that, for people who usually use health services in hospitals, interventions to increase their access to and positive experiences with CHCs would facilitate behavior contract with GPs. For example, promotions of GP services should not only be conducted in communities but also in hospital waiting areas. In those waiting areas, patients may be more receptive to messages about the benefits of GP services and may more seriously consider visiting CHCs for future health problems.
Another finding from this study was that a large portion of participants felt that there was no significant benefit to contracts and no necessity for contracting GP services. In the policy, contract benefits include broader reimbursement from health insurance, a green channel for referrals, appointment register, and comprehensive medical and preventive health management.8 Even after briefing participants on these benefits in the survey, there were still many who believed there are no significant benefits for them to contract services. It is possible that the trade-off between the relatively lower quality of care and the deductible payments in primary health care is insufficient for residents. With the country’s economy improving, a higher quality of health care might become a priority while out-of-pocket expenses, especially those incurred due to common/frequent diseases, may be less so. An even greater priority for residents than primary health care is accessibility to facilities. For example, hospitals are open 24 hours a day, but most primary health care facilities are only open during working hours. In addition, making appointments with doctors in hospitals is sometimes easier than making appointments with GPs in primary health care facilities through phone apps and other devices in the mHealth platform (the mobile health platform). Chinese residents’ need for contracts with GPs thus involve not only economic leverage but also other important factors such as the accessibility of the primary health care facility and the time and effort required to get appointments. Improving the quality of care in primary health care is complex and requires an extended length of time, but the accessibility of CHCs can more quickly be improved. Interventions or policies to promote GP behavior contract should consider how to increase the accessibility of CHCs in local areas.
Need factors are associated with the willingness to contract GP services in this study. Patients diagnosed with hypertension or diabetes were more willing to enter into contracts. This is consistent with previous studies’ findings. In Beijing, it was found that people with chronic diseases were more likely to sign contracts with GPs.36 In a study in a district in Shanghai, 99.07% of the family with members suffering from chronic diseases were willing to contract with GPs.12 In China, the GP contract services package includes cost-saving and convenience provisions, such as free annual physical examinations, consultations about medicine, diet, and life style; provisions for a green channel for referrals; and extension of single dosages as appropriate.8 The latter service should be particularly helpful for patients with chronic diseases. Again, interventions to promote GP services to these patients should not only be conducted in the community but should also consider targeting outpatients who visit hospitals.
This study has some limitations. Our study is a cross-sectional study. Many previous studies have used cross-sectional designs and reported significant findings9-13,18,35,37-41; however, as a cross-sectional study, only associations between factors could be observed, not causality. Second, a self-reporting bias may exist although we made efforts to minimize bias, including interviewing in a quiet room. Finally, only one district in Guangzhou was studied. To fully investigate contract rates and better understand contract willingness in Guangzhou, further studies need to be conducted on a larger scale.
Conclusions
The prevalence of behavior contract and contract willingness were relatively low during the GP services policy trial phase in Guangzhou, China, especially among the hospital-based participants of our study. In the short run, improving GP services awareness is necessary to promote GP behavior contract. Furthermore, we should pay attention to the types of intervention strategies employed for community-based residents and hospital-based residents. Intervention strategies should focus on increasing the opportunity to visit CHCs among hospital-based residents and on building trust with community-based residents.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Science and Technology Program of Guangzhou, China under Grant number 201607010332.
ORCID iD: Chun Hao  https://orcid.org/0000-0002-9881-6504
https://orcid.org/0000-0002-9881-6504
References
- 1. Öcek ZA, Çiçeklioğlu M, Yücel U, Özdemir R. Family medicine model in Turkey: a qualitative assessment from the perspectives of primary care workers. BMC Fam Pract. 2014;15:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(suppl 1):S34-S18. [DOI] [PubMed] [Google Scholar]
- 3. Reibling N, Wendt C. Gatekeeping and provider choice in OECD healthcare systems. Curr Sociol. 2012;60(4):489-505. [Google Scholar]
- 4. Zheng XM, Wang XL. Analysis of British national health service (NHS). Chin Health Serv Manage. 2011;28(12):919-921. (In Chinese) [Google Scholar]
- 5. Wu D, Lam TP, Lam KF, Zhou XD, Sun KS. Health reforms in china: the public’s choices for first-contact care in urban areas. Fam Pract. 2017:194-200. [DOI] [PubMed] [Google Scholar]
- 6. Wu D, Lam TP. Underuse of primary care in China: the scale, causes, and solutions. J Am Board Fam Med. 2016;29(2):240-247. [DOI] [PubMed] [Google Scholar]
- 7. The State Council of the People’s Republic of China. Guidance on establishing a hierarchical medical treatment system. http://www.gov.cn/zhengce/content/2015-09/11/content_10158.html.Published2015. (In Chinese)
- 8. The State Council of the People’s Republic of China. Guidance on promoting general practitioners’ contract service. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=e3e7d2670a8b4163b1fe8e409c7887af.Published2016. (In Chinese)
- 9. Qian W, Lin LP, Dai JM. Analysis on the relationship between patients’ demography and the prevalence of contract with family physician among patients at communities in Shanghai. Chin Primary Health Care. 2014;28(2):47-49. (In Chinese) [Google Scholar]
- 10. Wang NN, Gu YM, Liu LH, Chen DW, Shen Q, Zhong YH. Current status and strategies of family doctor contract services in Zhejiang province. Health Econ Res. 2015;32(3):15-17. (In Chinese) [Google Scholar]
- 11. Wang T, Zhao Y, Jin GH. Current status of family doctor service system undertaken in Beijing urban area. Chin Gen Pract. 2015;18(28):3413-3416. (In Chinese) [Google Scholar]
- 12. Wu J, Xu L, Lu M, et al. Demand of residents in Chengjiaqiao community for family physician services. Chin Gen Pract. 2012;15(16):1809-1811, 1814. (In Chinese) [Google Scholar]
- 13. Wang JM, Zhang T, Gai HM, Feng W, Ye S, Li YZ. Survey of signing, utilization and satisfaction of the family doctor service contract in the town of Huinan in the Shanghai Pudong new area. Chin Primary Health Care. 2015;29(6):32-33+36. (In Chinese) [Google Scholar]
- 14. Chen F, Xu X-L, Yang Z, Tan H-W, Zhang L. The willingness-to-pay for general practitioners in contractual service and influencing factors among empty nesters in Chongqing, China. Int J Environ Res Public Health. 2015;12(8):9330-9341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xiao X, Li Y, Zhou CM, et al. Influence of family physician contract services on utilization of community health services. Chin Health Resour. 2015;18(1):64-67. (In Chinese) [Google Scholar]
- 16. Mo RH, Zeng RY, Huang SH. Practice and effect evaluation of health care service mode by family physicians in Futian district. Chin J Gen Prac. 2015;13(3):428-429. (In Chinese) [Google Scholar]
- 17. Wu SD, Liu ZY, Hong Y, et al. Comparison study on the pilot service package of general practice contracted service in China. Chin Health Econ. 2014;33(11):5-7. (In Chinese) [Google Scholar]
- 18. He XL, Lou JQ, Liang H, et al. The implementation status and development strategies of the family doctor responsibility system in the Changning district. Chin Primary Health Care. 2013;27(12):17-19. (In Chinese) [Google Scholar]
- 19. Wu J, Shi Q. Thinking on reform of family doctors contract service and medical insurance payment mode. Chin Gen Pract. 2013;16(10A):3346-3350. (In Chinese) [Google Scholar]
- 20. Iecovich E, Carmel S. Differences between users and nonusers of day care centers among frail older persons in Israel. J Appl Gerontol. 2010;30(4):443-462. [Google Scholar]
- 21. Werner P, Segel-Karpas D. Factors associated with preferences for institutionalized care in elderly persons: comparing hypothetical conditions of permanent disability and Alzheimer’s disease. J Appl Gerontol. 2016;35(4):444-464. [DOI] [PubMed] [Google Scholar]
- 22. Baernholdt M, Hinton I, Yan G, Rose K, Mattos M. Factors associated with quality of life in older adults in the United States. Qual Life Res. 2012;21(3):527-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williams SW, Zimmerman S, Williams CS. Family caregiver involvement for long-term care residents at the end of life. J Gerontol B Psychol Sci Soc Sci. 2012;67(5):595-604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee HY, Lee J, Kim NK. Gender differences in health literacy among Korean adults: do women have a higher level of health literacy than men. Am J Mens Health. 2015;9(5):370-379. [DOI] [PubMed] [Google Scholar]
- 25. Kaskie B, Obrizan M, Jones MP, et al. Older adults who persistently present to the emergency department with severe, non-severe, and indeterminate episode patterns. BMC Geriatr. 2011;11:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Varga LM, Surratt HL. Predicting health care utilization in marginalized populations: black, female, street-based sex workers. Women Health Iss. 2014;24(3):e335-e343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baernholdt M, Yan G, Hinton I, Rose K, Mattos M. Quality of life in rural and urban adults 65 years and older: findings from the National Health and Nutrition Examination survey. J Rural Health. 2012;28(4):339-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhu HY. Unmet needs in long-term care and their associated factors among the oldest old in China. BMC Geriatr. 2015;15(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sreeramareddy CT, Sathyanarayana TN, Kumar HN. Utilization of health care services for childhood morbidity and associated factors in India: a national cross-sectional household survey. PLoS ONE. 2012;7(12):e51904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jang Y, Chiriboga DA, Allen JY, Kwak J, Haley WE. Willingness of older Korean-American adults to use hospice. J Am Geriatr Soc. 2010;58(2):352-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hoebel J, Starker A, Jordan S, Richter M, Lampert T. Determinants of health check attendance in adults: findings from the cross-sectional German Health Update (GEDA) study. BMC Public Health. 2014;14:913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Azuero C, Allen RS, Kvale E, Azuero A, Parmelee P. Determinants of psychology service utilization in a palliative care outpatient population. Psychooncology. 2014;23(6):650-657. [DOI] [PubMed] [Google Scholar]
- 33. Lowe SR, Kwok RK, Payne J, Engel LS, Galea S, Sandler DP. Mental health service use by cleanup workers in the aftermath of the Deepwater Horizon oil spill. Soc Sci Med. 2015;130:125-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95-124. [PubMed] [Google Scholar]
- 35. Jing L, Shu Z, Sun X, Chiu JF, Lou J, Xie C. Factors influencing patients’ contract choice with general practitioners in Shanghai. Asia Pac J Public Health. 2015;27(suppl 2):77S-85S. [DOI] [PubMed] [Google Scholar]
- 36. Zhang YH, Zhang TH, Wang ZF. Status of signing on family doctor service for residents in Desheng area of Beijing and its influencing factors. Chin Gen Pract. 2013;16(11A):3715-3718. (In Chinese) [Google Scholar]
- 37. Wang LY, Liu JH, Zhao J, et al. Analysis on chronic disease related Knowledge-Attitude-Practice (KAP) situation among patients in the Desheng community of Beijing. Chin J Health Educ. 2013;29(12):1071-1071-1073+1080. (In Chinese) [Google Scholar]
- 38. Wen XQ, Han CC, Lu Y, et al. Health behavior situation and influence factor of patients with chronic disease in the Beijing Desheng community. Chin Gen Pract. 2014;17(18):2123-2126. (In Chinese) [Google Scholar]
- 39. Huang KH, Song YT, He YH, Feng XL. Health system strengthening and hypertension management in China. Glob Health Res Policy. 2016;1:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang P, Luo D, Han C, Wang J, Yang WX. Implementation status of the contracted family doctor system in Tianjin and its influencing factors. Chin Gen Pract. 2015;18(10):1138-1141. (In Chinese) [Google Scholar]
- 41. Zhao JG, Zhang XD, Wang M, Zhao J, Han CC, Xu J. Residents’ willingness for renewing the contract of family doctor service in Xicheng district of Beijing and its influencing factors. Chin Gen Pract. 2015;18(28):3417-3422. (In Chinese) [Google Scholar]