Abstract
Background: Patient gender and race, and physician–patient communication are associated with clinical outcomes.
Aim: To understand the role of these factors in the diagnosis of colorectal cancer (CRC) during primary care visits as measured by appropriate outcome.
Materials and Methods: Caucasian and African American unannounced standardized patients (USPs) of both genders presented to 207 primary care physicians (PCPs) from community and academic practices in Ohio and Virginia as new patients with CRC symptoms. PCPs were blinded to the diagnosis. Physician subjects consented to audiotaping the encounter. Medical records were obtained. Communication elements were coded by trained observers and appropriate visit outcomes were coded from the medical record and audiofiles, defined as (1) recommendation for colonoscopy/sigmoidoscopy/fecal occult blood test (FOBT) or (2) referral to gastroenterologist.
Results: A total of 141 of 367 USP visits (38%) resulted in appropriate clinical outcomes. Patient race was not associated with outcome, but being a male USP was (χ2 = 4.12, p = 0.04). Relational communication was represented as a latent variable with seven indicators (alpha = 0.84) and was independently associated with outcome (beta = 0.15; p = 0.025). After controlling for clustered sampling, relational communication, and race, structural equational modeling indicated that female USPs were less likely to have an appropriate clinical visit outcome (beta = −0.13; p = 0.033).
Conclusions: Using a novel and innovative methodology capturing PCP behaviors during real-time clinician–patient interaction, appropriate clinical outcome was independently associated with being male and PCP relational communication factors such as encouraging patient communication, being engaged and expressive in the physician–patient conversation, and appearing friendly and sincere. There are persistent biases in the delivery of health care to female patients and further research into targeted communication skills programs may be warranted.
Keywords: physician–patient communication, unannounced standardized patient, relational communication, primary health care, colorectal cancer, patient gender
Introduction
Colorectal cancer (CRC) is the third most common cancer and third leading cause of cancer death in both men and women in the United States.1 In 2017, 95,520 cases of colon cancer and 39,910 cases of rectal cancer will have been diagnosed; African American men and women had the highest CRC rates in the United States.1 Early detection is especially important as 5-year survival rates are above 90% for localized CRC and about 70% for regional CRC.2 Unfortunately, only 40% of all CRCs are diagnosed at localized stages.3 In 2014, a large number of the 50,310 deaths from CRC could have been prevented through early detection.3
Some sociodemographic characteristics of patients have been found to play a role in later diagnosis. Women experience more delay than men in diagnosis of CRC,4,5 lung cancer, and non-Hodgkin's lymphoma.4 Men are more likely to report sigmoidoscopy screenings than women.6 Cancer in African Americans is more likely to be diagnosed at later stages than Caucasians,7 including CRC.8 Moreover, African Americans' CRC mortality rates are almost 50% higher than Caucasians.3
One potential factor that may mediate the diagnostic process is the quality of communication between patient and primary care physician (PCP) during the clinical consultation. Collaborative communication styles have been shown to impact diagnostic efficiency and patient health outcomes, including use of empathy, respect, and less verbal dominanace.9–11 Delivery of information and effective engagement of patients are shown to be influenced by the demographic characteristics of the patient. Patients who are younger, white, and better-educated frequently receive more information from their physicians.12 Physicians may view these individuals as more proactive or more able to understand medical information and, therefore, are likely to provide more information. Studies have shown that African Americans perceive their communications with their physician as poorer than Caucasians,13,14 whereas being female is often associated with less time spent on physical examinations15 and lower likelihood of appropriate care for treatments and illnesses.16 Although communication issues between patients and PCPs may exist for all patients, race and gender may exacerbate communication challenges.
This study sought to examine how communication elements were associated with the recommendations of PCPs who met with an unannounced standardized patient (USP) presenting with symptoms of CRC. The USP methodology allowed us to capture reliable detailed real-time communication between standardized patients and real physicians who were unaware that the simulated patient was an actor.17–19 We hypothesized that USP race, gender, and communication would be significantly associated with appropriate clinical visit outcomes using a standardized CRC case scenario. We further hypothesized that physician–patient communication would mediate the relationship between appropriate outcomes and USP race and USP gender.
Materials and Methods
General study implementation procedures have been documented in detail elsewhere18 and detailed information regarding the methods and procedures can be found in Appendix A1. Key aspects of the study methodology are briefly described here.
Trained USPs of four types (Caucasian or African American and men or women) presented to primary care practices as new patients with symptoms of CRC. The USP case was designed to convey a reasonable suspicion of CRC if all symptoms were revealed upon physician questioning. The USP scenario was purposefully crafted of that of a 47-year-old bookkeeper so that the physician would have to respond to the illness experience of the USP and not the need for general screening because the patient was <50 years of age.
Each PCP saw two USPs—one of each race and gender—with assignment counterbalanced. Visit consultations were audio recorded using a concealed recorder, which were transcribed verbatim. The practice was reimbursed for the cost of the self-pay new patient visit and participating physicians received $50 honorariums. After all PCPs participating in the study in a given practice had seen both USPs, medical records were obtained. The study protocol was approved by institutional review boards at all participating institutions. The final sample includes 367 USP visits with 207 individual PCPs who did not ascertain the USP's identity.
Coding procedures
Speech and affect characteristics indicative of relational communication
Visit recordings and transcriptions were coded for content, behavior, and affect using the Siminoff Communication Content and Affect Program (SCCAP), a reliable and accepted coding approach to health care consultations.20 Coders were trained to rate physician nonverbal vocalic cues likely to indicate affective qualities of the physician–patient interaction. Speech ratings included those cues associated with the immediacy construct, such as speech rate and timber. Affect ratings included emotional tone (e.g., friendly and sincere) and more composite affect (e.g., expressive and engaged). Coders rated the physician on various aspects of speech and affect based on their overall impression after listening to the physician–patient interaction using a Likert scale from 1 (not at all present) to 7 (very present). The relational communication domains and definitions used in this analysis are described in Table 1.
Table 1.
Relational Communication Domains and Definitions
| Relational communication domains | Definitions |
|---|---|
| Sincere | Speech is genuine, straightforward, and honest. |
| Animated | Speech delivery is lively and vigorous. |
| Encourages talk | Physician prompts patient for more information after a patient's statement and/or allows the patient to elaborate on details without interruption; invites patients to “tell their story.” |
| Expressive | Speech delivery conveys feelings or ideas successfully, eloquently, and/or meaningfully. |
| Friendly | Physician expresses liking, congeniality, and amiability as exhibited by engaging in social and nonmedical conversation where the physician attempts to make a personal connection, inclusive of exhibiting an affect of approval, understanding, helpfulness, and kindliness. |
| Speaks clearly | Speech delivery is easy to understand as in physician did not mumble or slur words; spoke distinctly. (Note: This is not an indicator of whether the meaning of their communication was easy to understand). |
| Engaged | Physician is connected and involved with the patient; exhibiting a desire to speak with the patient. |
Medical record review procedures
Trained coders reviewed all medical records for the USP visits and extracted information regarding documentation of complaints; symptoms (e.g., frequency and severity); medical, family, social, and behavioral history; physical examination results; differential diagnoses; final diagnosis; testing and treatment recommendations; referrals made and recommended; and recommended follow-up. A coding manual was developed that included operational definitions of each construct coded. An appropriate visit outcome was defined as documentation in the medical record of, and/or verbal recommendation for, colonoscopy, sigmoidoscopy, fecal occult blood test (FOBT), or referral to a gastrointestinal (GI) specialist.
Statistical analyses
Independent variables were tested for association with the outcome using the chi-square, Student's t-test, or Pearson's correlation. Structural equation modeling (SEM) was used to test the effect of relational communication on appropriate visit outcome controlling for the effect of patient gender and patient race (African American vs. Caucasian). Relational communication was defined as a latent variable accounting for the associations among seven items taken from the SCCAP physician speech and affect characteristics. To take into account clustered sampling (USPs nested within physicians), TYPE = COMPLEX statement in Mplus was used to obtain the correct test statistics and standard errors of parameter estimates. The average cluster size was 1.77 (range 1–3). In addition to a nonsignificant chi-square test of exact model fit, the root mean-square error of approximation (RMSEA) <0.05, comparative fit index (CFI) >0.90, and Tucker–Lewis index (TLI) >0.90 were used to declare a good model fit.
Results
The final sample of 367 USP visits consisted of 94 Caucasian men (25.6%), 92 Caucasian women (25.1%), 87 African American men (23.7%), and 94 African American women (25.6%). Table 2 describes the demographic characteristics of the physician sample (n = 207). The majority were men with an MD degree working full-time in family medicine or general practice and seeing 93 patients/week. They had graduated, on average, 22 years before the visit.
Table 2.
Physician Sample Demographic Characteristics (n = 207)
| Characteristic | n (%) or mean [SD] |
|---|---|
| Age | 51.1 [10.4] |
| Gender—male | 116 (56.0) |
| Spanish/Hispanic/Latino | 7 (3.4) |
| Race | |
| White | 153 (73.9) |
| Black/African American | 20 (9.7) |
| Other | 29 (14.0) |
| Not reported | 5 (2.4) |
| Degree | |
| MD/MD+other | 184 (88.9) |
| DO/DO+other | 20 (9.7) |
| Not reported | 3 (1.4) |
| Primary care discipline | |
| Family medicine or general practice | 150 (72.5) |
| General internal medicine or Med/Peds | 52 (25.1) |
| Not reported | 5 (2.4) |
| Board certified | 197 (95.2) |
| Completed fellowship | 19 (9.2) |
| Years since medical school graduation | 22.3 [10.3] |
| Work status—full-time | 163 (78.7) |
| Patients seen per week on average | 92.9 [52.5] |
| Physician's typical patient population | |
| % Male | 40.7 [10.4] |
| % Female | 59.3 [10.4] |
| % White, non-Hispanic | 63.9 [21.9] |
| % African American | 24.0 [19.4] |
| % Hispanic | 5.9 [7.3] |
| % Asian | 4.7 [7.0] |
| % Other | 3.4 [7.2] |
SD, standard deviation.
Of the 367 USP visits, 141 (38%) resulted in an appropriate clinical outcome. Caucasians and African Americans had similar appropriate outcomes (39% vs. 38%; χ2 = 0.11, p = 0.74); however, significant differences by gender were found (χ2 = 4.12, p = 0.04) with 44% for men versus 33% for women (Table 3). Physician age, gender, years since graduating medical school, patients seen per week on average, and percentage of typical patient population that is women were not associated with appropriate outcomes.
Table 3.
Distribution of Appropriate Clinical Visit Outcomes by Patient Race or Gender
| Appropriate clinical outcome | Nonappropriate clinical outcome | Total | |
|---|---|---|---|
| USP race | |||
| Caucasian | 73 (39% of Caucasians) | 113 (61% of Caucasians) | 186 |
| African American | 68 (38% of African Americans) | 113 (61% of Caucasians) | 181 |
| Total | 141 | 226 | 367 |
| USP gendera | |||
| Male | 79 (44% of males) | 102 (56% of males) | 181 |
| Female | 62 (33% of females) | 124 (67% of females) | 186 |
| Total | 141 | 226 | 367 |
p < 0.05; USP race χ2 = 0.11, p = 0.74; USP gender χ2 = 4.12, p = 0.04.
USP, unannounced standardized patient.
The following seven physician speech and affect characteristics were examined: speaks clearly, encourages talking, engaged, friendly, sincere, animated, and expressive. Visits with appropriate outcomes had significantly higher ratings on sincere speech than visits with nonappropriate outcomes (5.4 [1.1] vs. 5.2 [1.1], t = 1.82, p = 0.03) (Table 4).
Table 4.
Relationship Between Communication Characteristics and Appropriate Clinical Visit Outcomes
| Communication characteristic | Overallmean (SD) | Appropriate outcome (n = 141) Mean (SD) | Nonappropriate outcome (n = 226) Mean (SD) | t Value | One-tailed p-value |
|---|---|---|---|---|---|
| Speaks clearly | 4.2 (1.2) | 4.3 (1.2) | 4.2 (1.2) | 1.23 | 0.11 |
| Encourages talking | 4.0 (1.2) | 4.1 (1.1) | 4.0 (1.2) | 1.44 | 0.07 |
| Engaged | 4.4 (1.5) | 4.5 (1.0) | 4.3 (1.1) | 1.41 | 0.08 |
| Friendly | 4.3 (1.2) | 4.3 (1.1) | 4.2 (1.2) | 1.00 | 0.16 |
| Sincerea | 5.3 (1.2) | 5.4 (1.1) | 5.2 (1.2) | 1.82 | 0.03 |
| Animated | 3.9 (1.0) | 4.0 (1.3) | 3.8 (1.3) | 1.23 | 0.11 |
| Expressive | 4.4 (1.1) | 4.4 (1.1) | 4.2 (1.1) | 1.57 | 0.06 |
p < 0.05.
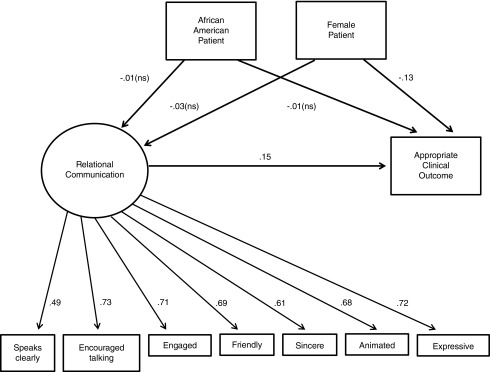
We examined USP gender, race, and communication features of the clinical encounter using SEM to fully explore their associations with appropriate outcome. The interested reader can refer to the correlations and covariances for the variables in the model provided in Appendix Table A1. Graphical representation of the SEM appears in Figure 1. Overall model fit was good: χ2 = 80.14, df = 32, p < 0.001; RMSEA (90% CI) = 0.064 (0.047–0.082); CFI = 0.940; TLI = 0.918. Within the SEM analysis, relational communication is represented as a latent variable with the seven physician speech and affect characteristics examined as indicators (alpha = 0.84). Relational communication was not associated with patient gender. PCP relational communication was significantly associated with appropriate clinical outcome (beta = 0.15; p = 0.025) after controlling for the clustered sampling, USP gender, and USP race. In other words, the better the physician relational communication with the USP during the visit (e.g., the higher the ratings on speaking clearly, encouraging talking, being engaged, friendliness, sincerity, animated, and expressiveness), the more likely is an appropriate clinical outcome (recommendation for, colonoscopy, sigmoidoscopy, FOBT, or referral to a GI specialist) was generated for that USP, regardless of his/her gender and race. USP race was not associated with appropriate clinical visit outcomes, whereas USP gender was. Female USPs were less likely to receive an appropriate clinical outcome than their male counterparts (beta = −0.13; p = 0.033) after controlling for the clustered sampling, USP race, and physican–patient relationship communication.
FIG. 1.
Structural equational model examining relationships among patient gender, patient race, communication, and appropriate clinical visit outcome. ns, nonsignificant.
Discussion
In a sample of USPs, 44% of men but only 33% of women, irrespective of race, received an appropriate clinical outcome that could have led to a timely diagnosis of CRC. It is noteworthy that, for more than half of the entire sample, the clinical consultation did not result in an appropriate outcome. Besides being a male patient, the other significant variable associated with appropriate outcome was relational communication, as characterized by physician–patient interactions in which the physician was engaging, friendly, animated, sincere, and expressive, and also spoke clearly and encouraged the patient to talk.
Prior research indicates gender and race play a role in recommendations for screenings or timely diagnoses of CRC. Men are more likely to receive screening recommendations or experience timely diagnoses of CRC than their women counterparts.4–6,21 Our findings support these previous findings. Physician–patient relational communication did not mediate this relationship. One factor that might explain our findings may be potential physician stereotypes that CRC is a “man's disease,”22 even though the incidence of CRC among men is only slightly higher than women. Another factor may be related to the CRC symptom of stomach pain presented by USPs in this study. Vague symptoms have been found to be more likely to produce quality deviations in cancer diagnosis and increase diagnostic delay.23,24 It is possible that physicians might find stomach pain to be vague more often in female versus male patients. Another possibility is that clinical presentation becomes more complex when the symptom is presented by a woman, for instance, because the physician must discern the need for gynecological follow-up as well. It is interesting to note that, in contrast to recent studies,25 the percentage of women typically seen by an individual physician was not related to the clinical outcome.
Contrary to the initial hypothesis, our study did not find a significant association between patient race and appropriate clinical outcomes, whereas other research suggests African Americans experience lower quality care. For example, African Americans are less likely to receive recommendations for appropriate tests and screenings for CRC,26 especially African American women.21 In follow-on analyses (not reported), the patient race by gender interaction term was also not associated with clinical visit outcomes. One explanation is that education and linguistic patterns may have a heavy influence. In this study, USPs were standardized such that all presented using similar language and speech patterns and all were well educated. Another explanation is that lower socioeconomic status, and income in particular, may account for racial disparities in care between Africian Americans and Caucasians.21 In this study, all USPs were middle class with the same income levels.
Finally, visits leading to this appropriate clinical outcome were associated with physician use of relational communication, regardless of patient gender. Previous work in this area demonstrates that patients are more satisfied or prefer when their physicians use a more collaborative style of communication27–29 and place value on relational communication.30 Furthermore, studies also indicate that the use of a collaborative style is related to beneficial clinical outcomes.9,31,32 This study provides direct confirmation of these findings.
This study is novel in the use of USP methodology that controls for symptom presentation and class differences. In this study, actors were instructed to follow the physician's lead and divulge information according to the physican's communication style. Results suggest that PCPs who engaged in more relational communication obtained more information that subsequently led (including the revelation of more symptoms) to appropriate referral and/or follow-up. In particular, it appears that a crucial component of relational communication's association with appropriate clinical outcomes involves engaging with patients in such a way as to elicit meaning as conveyed through their communication and how their experiences influence their interpretation of symptoms and chosen coping strategies.5,12,33 Those physicians who were less engaged or did not sufficiently encourage relevant communication may have lacked the ability to fully understand the illness experience of the patient and gain knowledge of key symptoms, thus leading to their ability to conclude that testing or referral was needed. Of note is that it was not enough to be friendly. Rather, it was important to communicate about health-related issues rather than spend time on social chit-chat. However, being male was still associated with appropriate outcomes, regardless of physician–patient relational communication during the consultation, further research into mediators of this relationship is warranted.
Although our study has many strengths, including objectively rated communication, a large sufficiency powered sample size to detect differences in relational communication, and the reduction of variability in case presentation by using trained USPs instead of real patients, it is not without limitations. Although using trained USPs who responded to the physician based on the communication style of the physician (e.g., answering a close-ended question with a close-ended response) provided more internal validity to our findings, it may not necessarily represent actual communication between real patients and providers because we flattened out the differences between patients and their communication styles. In doing so, we may have also diminished the real communication differences employed by actual patients of different genders and ethnic backgrounds. It is also possible that different sociodemographic patient profiles could impact the communication style of the physician and the resulting outcome; however, this variable was held constant in our study. It is important to note that the USP was a 47-year-old middle class bookkeeper, thus the study's findings cannot be generalized beyond educated patients in their late 40's. In addition, although it is possible that the physicians we sampled are not representative of those across the entire United States or in other countries, physicians were recruited from two areas in the United States, across rural, suburban, and urban locations, and across varying physician practice types with a range of sizes and types (academic and community). Lastly, the design of the study does not permit inference of causality. However, the strong correlations found suggest that additional research is warranted regarding the clinical implications of the findings.
Conclusions
Taken together, the study finds that there are persistent biases in the delivery of health care to female patients. Physician–patient relational communication did not mediate relationship between patient gender and clinical visit outcome. Similarly, patient gender did not mediate the relationship between increased relational communication and improved clinical visit outcome. Although medical schools now provide a modicum of communication training to its students, a greater emphasis and continued education, especially through residency, could prove valuable to increasing the quality of physician–patient interactions and lead to improved health outcomes. Communication skills interventions have identified some clear benefits, such as lowering overall medical costs and frequency of admissions and surgeries,33 providing more patient-centered care,34 and increasing well-being of patients,35 but there is a lack of standardized programs that have been evaluated across settings, specialties, and locations. Given the paucity of standardized programs, research in this area would benefit from improved clarity of which communication skills are key and how best to address issues of translation into clinical practice and skills maintenance.36 The findings from this study suggest that specific speech and affect characteristics that define relational communication are independently associated with better visit outcomes. Video recording of actual patient visits, with appropriate patient-informed consent, could be used to demonstrate to physicians the impact of their own communication on patient behaviors and potentially linked to visit outcomes.
In this study, only one out of three USP visits to a PCP with symptoms of CRC resulted in a recommendation for further diagnostic testing (colonoscopy and sigmoidoscopy) or evaluation by a GI specialist, and being male was independently associated with appropriate visit outcomes. Further examination into mediators and moderators of this relationship is warranted, given that physician–patient communication does not explain it. Females are at higher risk of not receiving a timely diagnosis of CRC, therefore, more education about the women's risk for CRC would be useful. Additional research into the causes of such delay is warranted. Study of critical aspects of relational communication and communication skills programs that are associated with appropriate visit outcomes may be warranted to ensure all individuals have a stronger chance to receive a timely diagnosis.
Acknowledgment
This study was funded by the NIH/NCI grant #R01 CA134280. The funding source had no influence on the following: study design; data collection, analysis, and interpretation; writing of the article; and decision to submit it for publication.
Appendix A1: Detailed Description of Study Methods and Procedures
Unannounced Standardized Patient Case
The 47-year-old middle class bookkeeper unannounced standardized patient (USP)'s opening line was “I've been having pains in my stomach that won't completely go away and I've been more tired than usual.” This and constipation and diarrhea were the required symptoms to be communicated to the physician during the visit. Physician questioning and physical examination revealed upper left quadrant dull aching pain, decreased energy level, and difficulty with bowel movements. The USP reported experiencing alternation of constipation and diarrhea for many years as a result of irritable bowel syndrome (IBS), but that these symptoms were now worse with increased difficulty with constipation. He/she had had a colonoscopy 5 years prior with negative results that supported the IBS diagnosis. The USP also recently observed a few spots of blood on the toilet tissue. Throughout the visit, the emotionally stable patient initially described being “annoyed” by his/her symptoms, but later stated “concern,” and finally “worry.”
USP Role Adherence Procedures and Measurement
Trained coders listened to the audio recordings from the visit and rated the accuracy of the USP's role portrayal. For instance, in addition to role adherence using specific text phrases, six applicable items from the Maastricht Assessment of Simulated PatientsA1 were used to rate authenticity on a Likert scale from 0 to 4, with higher scores indicating better performance. The average score on the sum of these six items was 23.5 (1.3) out of 24 possible points, suggesting high levels of authenticity.
Appendix Table A1.
Correlation and Covariances Among the Variables in the Structural Equation Modeling
| Speaks clearly | Encourages talking | Engaged | Friendly | Sincere | Animated | Expressive | Race (African American) | Gender (female) | Appropriate outcome | |
|---|---|---|---|---|---|---|---|---|---|---|
| Speaks clearly | 1 | 0.35a | 0.35a | 0.29a | 0.24a | 0.22a | 0.46a | 0.01 | 0.02 | 0.08 |
| Encourages talking | 0.48a | 1 | 0.55a | 0.52a | 0.53a | 0.43a | 0.46a | 0 | 0.03 | 0.10 |
| Engaged | 0.43a | 0.69a | 1 | 0.51a | 0.46a | 0.50a | 0.53a | −0.07 | −0.08 | 0.10 |
| Friendly | 0.38a | 0.70a | 0.62a | 1 | 0.40a | 0.50a | 0.47a | 0.01 | 0.05 | 0.07 |
| Sincere | 0.33a | 0.73a | 0.58a | 0.54a | 1 | 0.41a | 0.35a | 0.03 | −0.09 | 0.12 |
| Animated | 0.33a | 0.65a | 0.68a | 0.73a | 0.63a | 1 | 0.55a | −0.09 | −0.11 | 0.08 |
| Expressive | 0.59a | 0.59a | 0.61a | 0.59a | 0.45a | 0.78a | 1 | −0.11 | 0.06 | 0.11 |
| Race (African American) | 0.01 | 0 | −0.08 | 0.01 | 0.04 | −0.12 | −0.13 | 1 | 0.04 | −0.03 |
| Gender (female) | 0.03 | 0.03 | −0.08 | 0.06 | −0.11 | −0.14 | 0.07 | 0.04 | 1 | −0.17b |
| Appropriate outcome | 0.10 | 0.11 | 0.10 | 0.08 | 0.15 | 0.11 | 0.12 | −0.03 | −0.17b | 1 |
| Mean (or %) | 4.23 | 4.02 | 4.39 | 4.24 | 5.28 | 3.90 | 4.27 | 49.32% | 50.58% | 38.42% |
| SD | 1.16 | 1.16 | 1.06 | 1.15 | 1.18 | 1.29 | 1.10 | 0.50 | 0.50 | 0.44 |
Correlations are above the diagonal and covariances below the diagonal.
p < 0.001.
p < 0.05.
SD, standard deviation.
General Study Procedures
Each primary care physician (PCP) saw two USPs—one of each race and gender. If the first assigned visit was a white male, the second visit was an African American female. Assignment of USPs was counter-balanced so that approximately equal number of each type of USP was seen in the first visit. To reduce reactivity, the first visit did not occur until at least 3 months after consent with a median interval between consent and the first visit of ∼7 months (median = 203 days [mean = 250 days, standard deviation (SD) = 176]). The second visit occurred a minimum of 3 weeks (21 days) after the first visit, with a median interval between the first and second visits of ∼5 months (median = 141 days [mean = 174 days, SD = 107]).
Research staff often enlisted practice managers as confederates to help make medical appointments for the USPs and assist with any issues regarding the self-pay fee. Immediately after the visit, USPs verified the audio recording and completed the postvisit Set the stage, Elicit information, Give information, Understand the patient's perspective, and End the encounter evaluation form.A2
After all PCPs participating in the study in a given practice had seen both USPs, medical records for those USPs were obtained and PCPs were faxed a poststudy detection survey asking for details of any suspected USP. Once the completed poststudy form was received, the physician was sent a debriefing letter explaining the purpose of the study with the identities and visit dates of the USPs. Physicians who were not randomized to participate were sent a follow-up letter upon termination of the study.
Physician Recruitment Strategy
Physicians were first identified through practice-based research networks in Richmond, VA, and northeast OH and further through a list of all PCP practices located in the target regions obtained from county medical societies. All were contacted via mail and/or fax with telephone follow-up and in-person presentations to explain the study and obtain PCP consent. Finally, a snowball technique was used, in which physicians who had completed the study recommended colleagues who might be interested in participating. Physicians were told that the study would involve possibly seeing two USPs several months apart, with the purpose to “better understand physician–patient communication factors” and “responses to patient symptom communication.”
Sample
Of approximately 500 PCPs from community and academic practices in the state of Virginia and northeast Ohio who were contacted, 265 consented to participate in the study. A random sample of recruited physicians received a USP visit, arousing less suspicion of a USP. Two hundred and twenty PCPs from 139 individual practices received at least one USP visit. The majority (70%) were family practice physicians. The practice was reimbursed for the cost of the self-pay new patient visit and participating physicians received $50 honorariums for completing a poststudy detection survey. In 11% of the 414 USP visits (n = 46), PCPs correctly ascertained the USP's identity before or during the visit. Because detection would be expected to influence relational communication and visit outcomes, those visits were removed from analysis. The final sample for this analysis includes 367 USP visits with 207 individual PCPs.
Coding Procedures for the Physician–Patient Interaction
The audio recordings of the visits were transcribed. The audio and transcription were both used by trained observers to code for content and affect using the Siminoff Communication Content and Affect Program (SCCAP),A3 a reliable and accepted coding approach to health care consultations. SCCAP uses relational communication theory to conceptualize the affiliative function of communication and includes measures of patient participation of the following speech dimensions: content (what was said), behavior (what was done), and affect (how it was said). SCCAP captures the dynamic nature of transactional communication by allowing specific content to be connected to verbal and nonverbal relational codes. Further details on the computerized SCCAP for coding health care conversations, and its high reliability (averages of 0.92, range 0.80–0.95, for conversations averaging 55 minutes each), can be found elsewhere.A3
A coding manual was developed that provided the operational definitions of each content theme, communication type, and speech and affect rating item. Ten percent of the interactions were double coded with discrepancies resolved via consensus. Correlations of the scores between coders were generally high (>0.80). Paired sample t-tests indicated a lack of statistically significant differences between the coders' means. Taken together, this indicates high reliability of SCCAP ratings for this study.
Medical Record Review Procedures
Written or computerized medical record documentation for each USP visit was obtained. Trained coders reviewed all medical records for the USP visits and extracted information regarding documentation of complaints and symptoms (e.g., frequency and severity); medical, family, social, and behavioral history; physical examination results; differential diagnoses; final diagnosis; testing and treatment recommendations; referrals made and recommended; and recommended follow-up. A coding manual was developed that included operational definitions of each construct coded. Ten percent of medical record reviews were double coded, with discrepancies resolved via consensus. Reliability of ratings was high, with correlations of scores between coders >0.80.
Appendix References
Wind L, Van Dalen J, Muijtjens AM, Rethans JJ. Assessing simulated patients in an educational setting: The MaSP (Maastricht Assessment of Simulated Patients). Med Educ 2004;38:39–44.
Makoul G. The SEGUE Framework for teaching and assessing communication skills. Patient Educ Couns 2001;45:23–34.
Siminoff LA, Step MM. A comprehensive observational coding scheme for analyzing instrumental, affective, and relational communication in health care contexts. J Health Commun 2011;16:178–197.
Author Disclosure Statement
No competing financial interests, real or perceived, exist for any authors of this article.
References
- 1. American Cancer Society. Cancer facts & figures 2017–2019. Atlanta, GA: American Cancer Society, 2017 [Google Scholar]
- 2. Siegel R, DeSantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin 2014;64:104–117 [DOI] [PubMed] [Google Scholar]
- 3. American Cancer Society. Colorectal cancer facts & figures 2014–2016. Atlanta, GA: American Cancer Society, 2014 [Google Scholar]
- 4. Neal RD, Allgar VL. Sociodemographic factors and delays in the diagnosis of six cancers: Analysis of data from the ‘National Survey of NHS Patients: Cancer’. Br J Cancer 2005;92:1971–1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Siminoff LA, Rogers HL, Harris-Haywood S. Missed opportunities for the diagnosis of colorectal cancer. Biomed Res Int 2015;2015:285096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Slattery ML, Kinney AY, Levin TR. Factors associated with colorectal cancer screening in a population-based study: The impact of gender, health care source, and time. Prev Med 2004;38:276–283 [DOI] [PubMed] [Google Scholar]
- 7. Virnig BA, Baxter NN, Habermann EB, Feldman RD, Bradley CJ. A matter of race: Early-versus late-stage cancer diagnosis. Health Aff 2009;28:160–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chien C, Morimoto LM, Tom J, Li CI. Differences in colorectal carcinoma stage and survival by race and ethnicity. Cancer 2005;104:629–639 [DOI] [PubMed] [Google Scholar]
- 9. Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonella JS. Physicians' empathy and clinical outcomes for diabetic patients. Acad Med 2011;86:359–364 [DOI] [PubMed] [Google Scholar]
- 10. Baile WF, Aaron J. Patient-physician communication in oncology: Past, present, and future. Curr Opin Oncol 2005;17:331–335 [DOI] [PubMed] [Google Scholar]
- 11. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: A systematic review. Br J Gen Pract 2013;63:e76–e84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviors. Patient Educ Couns 2006;62:355–360 [DOI] [PubMed] [Google Scholar]
- 13. Cooper LA, Roter DL, Carson KA, et al. The association of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health 2012;102:979–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manfredi C, Kaiser K, Matthews AK, Johnson TP. Are racial differences in patient-physician cancer communication and information explained by background, predisposing, and enabling factors? J Health Commun 2010;15:272–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bertakis KD. The influence of gender on the doctor–patient interaction. Patient Educ Couns 2009;76:356–360 [DOI] [PubMed] [Google Scholar]
- 16. Borkhoff CM, Hawker GA, Wright JG. Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res 2011;469:1829–1837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: A prospective validation study of 3 methods for measuring quality. J Amer Med Assoc 2000;283:1715–1722 [DOI] [PubMed] [Google Scholar]
- 18. Siminoff LA, Rogers HL, Waller AC, Harris-Haywood S, Esptein RM, Carrio FB, Gliva-McConvey G, Longo DR. The advantages and challenges of unannounced standardized patient methodology to assess healthcare communication. Patient Educ Couns 2011;82:318–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fiscella K, Franks P, Srinivasan M, Kravitz RL, Epstein RM. Ratings of physician communication by real and standardized patients. Ann Fam Med 2007;5:151–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Siminoff LA, Step MM. A comprehensive observational coding scheme for analyzing instrumental, affective, and relational communication in health care contexts. J Health Commun 2011;16:178–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ahmed NU, Pelletier V, Winter K, Albatineh AN. Factors explaining racial/ethnic disparities in rates of physician recommendation for colorectal cancer screening. Am J Public Health 2013;103:e91–e99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Donovan JM, Syngal S. Colorectal cancer in women: An underappreciated but preventable risk. J Womens Health 1998;7:45–48 [DOI] [PubMed] [Google Scholar]
- 23. Jensen H, Nissen A, Vedsted P. Quality deviations in cancer diagnosis: Prevalance and time to diagnosis in general practice. Br J Gen Pract 2014;64:e92–e98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jensen H, Torring ML, Olesen F, Overgaard J, Vedsted P. Cancer suspicion in general practice, urgent referral and time to diagnosis: A population-based GP survey and registry study. BMC Cancer 2014;14:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A 2018;115:8569–8574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Coughlin SS, Thompson T. Physician recommendation for colorectal cancer screening by race, ethnicity, and health insurance among men and women in the United States, 2000. Health Promot Pract 2005;6:369–378 [DOI] [PubMed] [Google Scholar]
- 27. Siminoff LA, Gordon NH, Silverman P, Budd T, Ravdin PM. A decision aid to assist in adjuvant therapy choices for breast cancer. Psychooncology 2006;15:1001–1013 [DOI] [PubMed] [Google Scholar]
- 28. Dowsett SM, Saul JL, Butow PN, et al. Communication styles in the cancer consultation: Preferences for a patient-centred approach. Psychooncology 2000;9:147–156 [DOI] [PubMed] [Google Scholar]
- 29. Siminoff LA, Ravdin P, Colabianchi N, Sturm CMS. Doctor‐patient communication patterns in breast cancer adjuvant therapy discussions. Health Expect 2000;3:26–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cegala DJ, McGee DS, McNeilis KS. Components of patients' and doctors' perceptions of communication competence during a primary care medical interview. Health Commun 1996;:1–27 [Google Scholar]
- 31. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: A systematic review and meta-analysis of randomized controlled trials. PLoS One 2014;9:e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cooper LA, Roter DL, Carson KA, et al. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med 2011;26:1297–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rao JK AL, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: A systematic review of the evidence. Med Care 2007;45:340–349 [DOI] [PubMed] [Google Scholar]
- 34. Veroff D, Marr A, Wennberg DE. Enhanced support for shared decision making reduced costs of care for patients with preference-sensitive conditions. Health Affair 2013;32:285–293 [DOI] [PubMed] [Google Scholar]
- 35. Griffin SJ, Kinmonth AL, Veltman MWM, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: A systematic review of trials. Ann Fam Med 2004;2:595–608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gysels M, Richardson A, Higginson I. Communication training for health professionals who care for patients with cancer: A systematic review of effectiveness. Support Care Cancer 2004;12:692–700 [DOI] [PubMed] [Google Scholar]