Abstract
Background
During the last decades, social and life-style changes in Greenland have led to an increase in the incidence of several non-communicable diseases. Our aim is to present the cancer incidence and mortality in Greenland and compare the results with the other Nordic countries.
Methods
The data stems from The Danish Cancer Registry and The Danish Register of Causes of Death. Comparable data on cancer incidence and mortality in Denmark, Finland, Iceland, Norway, Sweden, and Greenland are available through collaboration between Nordic Cancer Registries (NORDCAN). We included all individuals residing in Greenland and diagnosed with or died of a cancer from 1983 to 2014.
Findings
The total number of cancer cases in Greenland for the study period was 4716 and there were 3231 cancer deaths. Respiratory and gastrointestinal cancers had the highest incidence as well as mortality in Greenland for the entire time period and for both sexes. Compared to the other Nordic countries, Greenland had significantly higher incidence and mortality rates for several cancers. Cancer of the lip, oral cavity, and pharynx, respiratory cancer, and cancer of unknown sites had the highest incidence rate ratios (2.3–3.9) and mortality rate ratios (2.7–9.9) for both sexes. The time trend from 1983 to 2014 showed a significant increase in cancer incidence in Greenland with nearly the same incidence level as the other Nordic countries. While the cancer mortality decreased in the other Nordic countries during the time period studied, there was no change in the cancer-specific mortality in Greenland.
Interpretations
The trends in cancer incidence and mortality in Greenland compared to the other Nordic countries have not been reported earlier. These data underline a need to focus on cancer-specific mortality in Greenland and prevention of high-incidence cancers related to well-established risk factors.
Keywords: Cancer incidence, Cancer mortality, Greenland, Inuit, Arctic, Cancer, Carcinoma, Nordic countries, Epidemiology
Research in context
Evidence before this study
We searched MEDLINE for studies on cancer in Greenland, using search terms “Greenland” “cancer” “Inuit” in October 2017, without language or publication date restrictions. We found publications on the incidence of cancer in Greenland for the periods 1950–1974, 1953–1985, 1969–1988, 1973–1997, 1973–2003, 1989–2003, none of these studies included information on cancer mortality. There were also publications on specific cancer sites in Greenland. There were no publications comparing the incidence and mortality from all cancers with the other Nordic countries.
Added value of this study
Our study provides cancer incidence and mortality data for the population of Greenland for the years 1983–2014, for both sexes, and all ages, including a comparison with the other Nordic countries (Denmark, Finland, Iceland, Norway, and Sweden). We calculated the number of cases and deaths, age-standardized incidence and mortality rates using World standard (ASR (W)) as well as the incidence rate ratios (IRR) and mortality rate ratios (MRR) compared to the other Nordic countries as one group with 95% confidence intervals. The time trend from 1983 to 2014 showed a significant increase in cancer incidence rates proportionally for Greenland and the other Nordic countries. Cancer mortality decreased over time in the other Nordic countries while there was no improvement in cancer mortality in Greenland. The differences between the incidence and mortality rates indicate a poorer cancer survival in Greenland compared to the other Nordic countries. We have given a comprehensive and updated overview of cancer incidence and mortality according to diagnosis groups and sex, with the time period divided into six calendar periods for all cancer sites except non-melanoma skin cancer.
Implication of all available evidence
The data reported in our study gives the current status of cancer incidence and mortality in Greenland with focus on high cancer mortality and high incidence of specific cancer sites in Greenland. The high mortality in Greenland compared to the other Nordic countries provides baseline data that can be used for future research in to finding the causes behind the high mortality. Focus on the challenges pointed out in our report can help form guidelines for the betterment of cancer treatment in Greenland. Furthermore, the data can be useful for comparison with other Inuit communities and indigenous people in general.
Alt-text: Unlabelled Box
1. Background
1.1. The Greenlandic Population
Greenland is the world's biggest island with a total population just below 56,000 (2018). Apart from a large number of small settlements, the population lives in a few urban centers. More than one fourth of the population lives in the capital city of Nuuk. The remaining live in smaller cities and settlements dispersed along primarily the western coastline. The majority of the population in Greenland is of Greenlandic Inuit descent (85–90%) and the remaining part of the population is mainly Caucasians of Danish origin (10–15%). Greenland became a Danish colony in 1721, fully integrated in the Danish Kingdom in 1953, and gained self-rule in 2009 [1], [2], [3], [4].
Since Greenland has a history of colonization, Greenlanders are often defined as indigenous people. Today, only a minority of the population pursues a subsistence based living consisting primarily of fishing and hunting. However, for many Greenlanders, hunting and fishing are considered important activities in pursuing what is perceived to be the good life. A much greater part of the population has jobs within commercial fishery, construction, and public service [3].
The unique living conditions in Greenland attracted much interest in describing the cancer pattern during the mid-1980's through the 1990's [2], [5]. The most recent publications presented the cancer incidence up to 2003 [5], [6], [7]. There has been a major change in life-style in Greenland, including urbanization, change of diet from locally hunted food to a more Western diet, smoking and a high intake of alcohol. This has led to an increasing incidence of life-style related conditions and diseases, such as obesity, diabetes, cardiovascular disease, and cancer [5], [8], [9]. The age-distribution of the Greenlandic population is also changing with an increasing number of individuals aged 60 years and above [10].
The average life expectancy of the Greenlandic population is 74 years for women and 70 years for men [1]. This is lower than Denmark, which has an average life expectancy of 83 years among women and 79 years among men [11].
1.2. Diagnostics and Treatment of Cancer in Greenland
All medical treatment, including medication, is free of charge. Due to a small population distributed over a large country, only the major specialties are represented in the capital Nuuk. There are five health regions in Greenland. Each region has a smaller hospital or clinics. The main hospital, Queen Ingrid's Hospital, is located in Nuuk together with clinics of general practitioners. The smaller hospitals in other bigger cities have four to five doctors, primarily general practitioners. The general practitioners also have some surgical skills and are able to perform emergency caesarean section, appendectomy, and uterine evacuation, in addition to treating minor internal medical conditions. In smaller cities, there are clinics with one to two general practitioners. If local doctors are unable to diagnose or treat a given patient, then the patient is referred to either Nuuk, Denmark or, in a few cases, Iceland.
At Queen Ingrid's Hospital, diagnostic procedures are carried out for cancers if a biopsy is possible, unless a biopsy is contraindicated in cases of curative treatment for some cancers. Cancer surgery is also performed for some diagnoses. Since there are no pathologists in Greenland, all biopsy samples and postoperative specimens are sent to Denmark for pathological evaluation. There were no facilities to carry out mammography or ultrasound of the breast during the years under study. If breast cancer was suspected, an open biopsy was performed. If breast cancer was ascertained, it resulted in mastectomy performed in Nuuk. Breast conserving surgery was not an option. Adjuvant and palliative chemotherapy can be given in Nuuk for selected diagnoses. More specialized diagnostics and complex treatments are therefore carried out at Rigshospitalet in Denmark. Radiation therapy can only be given at Rigshospitalet. The decision regarding referral to Denmark is based on a detailed assessment of each patient case in collaboration with the regularly visiting specialists in Denmark, in some cases including evaluation by telemedicine [12], [13], [14].
2. Aim of the Study
Our aim is to investigate the cancer incidence and cancer-specific mortality in Greenland for the period 1983–2014 and to compare the cancer incidence and cancer specific mortality for Greenland with the other Nordic countries.
3. Materials and Methods
3.1. Data Sources
All cases of cancer in Denmark and Greenland are registered in The Danish Cancer Registry. All causes of death are registered in The Danish Register of Causes of Death with separate statistical reports for Greenland and Denmark [15]. The cancer registration in Greenland is based on paper forms for each case that is coded in The Greenlandic National Board of Health and included in and validated by The Danish Cancer Registry. In 2002, Association of Nordic Cancer Registries (ANCR) initiated a collaboration project, NORDCAN (http://ancr.nu), a Nordic cancer statistics database. Since December 2014, Greenland has been included in NORDCAN with incidence data from 1968 and cancer mortality data from 1983. The other included countries are Denmark, Faroe Islands, Finland, Iceland, Norway, and Sweden. More than 50 cancer entities are included in the NORDCAN database. Conversions of the original national data are carried out according to international rules to ensure comparability [16]. Aggregated data obtained from NORDCAN have been used for this article both for Greenland and for the comparison between Greenland and the other Nordic countries.
3.2. Inclusion Criteria and Data Selection
We included cancer incidence and cancer mortality data for the years 1983–2014 for all individuals residing in Greenland at the time of diagnosis. We present the number of cancer cases and deaths, age-standardized incidence and mortality rates using the World standard (ASR(W)), and calculated incidence rate ratios (IRR) and mortality rate ratios (MRR) relative to the other Nordic countries as one group (Denmark, Finland, Iceland, Norway, and Sweden) with 95% confidence intervals.
3.3. Methods
Since the Greenlandic population is small, there is a pronounced random variation in annual data, especially for less common cancer diagnoses. The diagnoses are therefore presented in 11 summary groups. Diagnosis groups are defined in Table 1 and shown according to ICD-10 codes and NORDCAN entities. To identify diagnosis groups with differing incidence or mortality rates in Greenland compared to the other Nordic countries, the respective IRR and MRR have been calculated for the 11 diagnosis groups for the period 1983–2014. If the incidence or mortality differ between Greenland and the other Nordic countries, the cancer sites (NORDCAN entities) contributing to the difference in the respective diagnosis groups are shown as trend graphs for ASR(W) with five-year smoothing to evaluate if the patterns are constant over the entire 32-year period.
Table 1.
Definition of the diagnosis groups.
| ICD-10 | NORDCAN entities | |
|---|---|---|
| Lip, oral cavity and pharynx | C00–14 (except C10.1) | Lip, oral cavity and pharynx |
| Respiratory organs | C30–34 + C10.1 + C38.4 + C45.0 | Nose, larynx, lung, pleura |
| Gastrointestinal organs | C15–25 | Oesophagus, stomach, small intestine, colon, rectum and anus, liver, gallbladder, pancreas |
| Urinary tract | C64–68 + D09.1 + D30.1–9 + D41.1–9 | Kidney, bladder |
| Female genital | C51–58 | Cervix uteri, corpus uteri, uterus other, ovary, other female genital organs |
| Male genital | C60–63 | Penis, prostate, testis |
| Breast | C50 | Breast |
| Melanoma of skin | C43 | Melanoma of skin |
| Lymphoma and leukaemia | C81–85 + C90–96 | Hodgkin and non-Hodgkin lymphoma, multiple myeloma, leukaemia |
| Other specified sites | C37 + C38.0–3 + C38.8 + C45.1–9 + C46.2–9 + C47–48 + C74 + C75.0 + C75.4–9 + C88 + D46 | Other specified, bone, soft tissue, eye, brain and central nervous system, thyroid |
| Unknown | C26 + C39 + C76–80 + C97 + D47 | Unknown and unspecified |
Survival is not evaluated directly but indicated by the difference between the age-standardized incidence and mortality rates (ASR(W)) and between the rate ratios, IRR and MRR.
We have illustrated the trend over time for six calendar periods for all cancers except non-melanoma skin cancer by sex and for six calendar periods. The estimated annual percent change (EAPC) is the average annual percentage of change in the ASR(W) over the time period selected. It is calculated by fitting a simple regression model to the log of the ASR(W).
4. Results
4.1. Incidence and Mortality
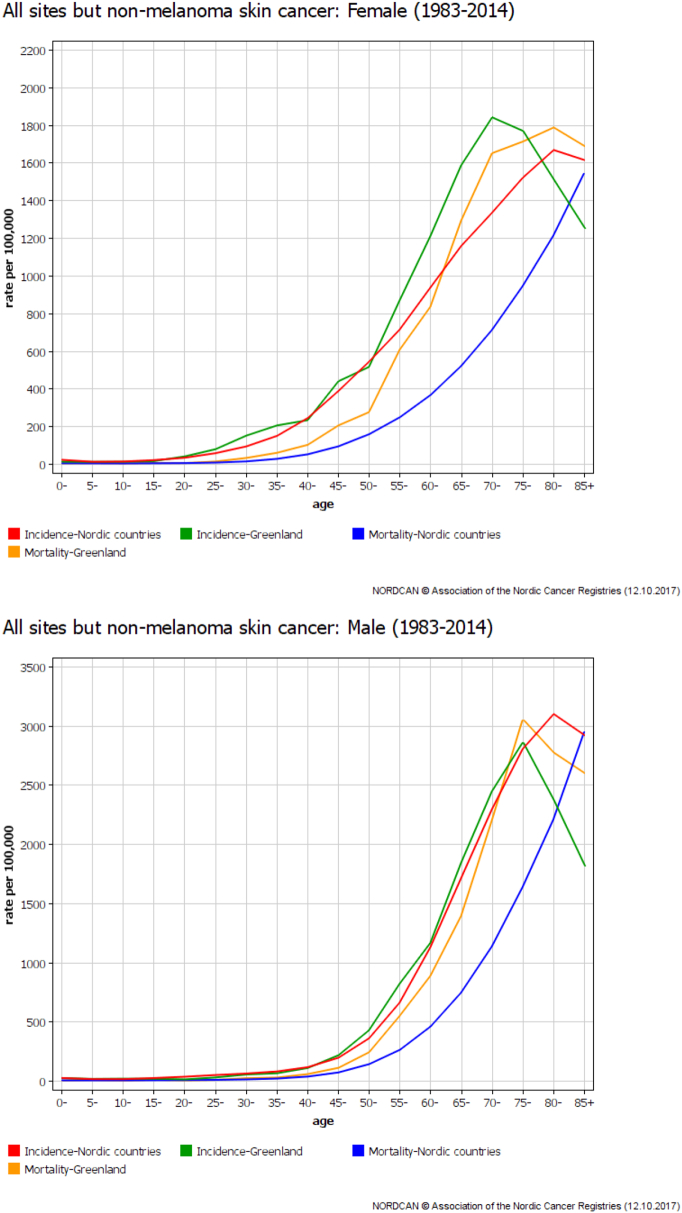
In the 32-year period, 4716 cases of cancer (2362 among women and 2354 among men), excluding non-melanoma skin cancer, were diagnosed in Greenland. There were 3231 cancer deaths (1532 among women and 1699 among men) (Table 2a, Table 2b). The age-specific cancer incidence and mortality rates for the time period are shown in Fig. 1.
Table 2a.
Cancer incidence and mortality among women by diagnosis groups, Greenland, 1983–2014.
| Incidence |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis groups | N | N (%) | ASR (W) | IRR (95% CI) | N | % | ASR (W) | MRR (95% CI) |
| Lip, oral cavity and pharynx | 116 | 4.9 | 15 | 3.9 (2.8–5.5) | 81 | 5.3 | 10 | 9.9 (5.6–17.4) |
| Respiratory organs | 447 | 18.9 | 61 | 3.2 (2.7–3.8) | 438 | 28.6 | 61 | 4.0 (3.3–4.7) |
| Gastrointestinal organs | 540 | 22.9 | 73 | 1.7 (1.5–1.9) | 404 | 26.4 | 54 | 2.0 (1.9–2.4) |
| Urinary tract | 62 | 2.6 | 8 | 0.8 (0.6–1.0) | 42 | 2.7 | 6 | 1.5 (1.0–2.1) |
| Female genital organs | 431 | 18.2 | 49 | 1.3 (1.2–1.5) | 198 | 12.9 | 25 | 1.9 (1.6–2.3) |
| Breast | 354 | 15.0 | 42 | 0.6 (0.5–0.6) | 127 | 8.3 | 16 | 0.9 (0.8–1.1) |
| Melanoma of skin | 16 | 0.7 | 2 | 0.1 (0.1–0.2) | 2 | 0.1 | 0 | 0.2 (0.1–0.2) |
| Lymphoma and leukaemia | 73 | 3.1 | 9 | 0.4 (0.4–0.5) | 34 | 2.2 | 4 | 0.6 (0.4–0.7) |
| Other specified sites | 144 | 6.1 | 18 | 0.8 (0.7–0.9) | 46 | 3.0 | 6 | 0.9 (0.7–1.2) |
| Unknown | 179 | 7.6 | 24 | 3.3 (2.5–4.2) | 160 | 10.4 | 22 | 3.8 (2.9–5.1) |
| Total | 2362 | 100.0 | 301 | 1.2 (1.1–1.2) | 1532 | 100.0 | 204 | 2.1 (1.9–2.2) |
N = Numbers of cancer incidence and mortality.
N (%) = the percentage of the numbers of cancer incidence and mortality.
ASR (W) = Age standardized rates for the world, per 100,000 person years.
IRR: Incidence rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
MRR: Mortality rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
95% CI: 95% confidence intervals.
Table 2b.
Cancer incidence and mortality among men by diagnosis groups, Greenland, 1983–2014.
| Incidence |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis groups | N | N (%) | ASR (W) | IRR (95% CI) | N | % | ASR (W) | MRR (95% CI) |
| Lip, oral cavity and pharynx | 224 | 9.5 | 25 | 3.0 (2.4–3.8) | 141 | 8.3 | 17 | 6.0 (4.1–8.6) |
| Respiratory organs | 683 | 29.0 | 89 | 2.3 (2.0–2.6) | 637 | 37.5 | 86 | 2.7 (2.3–3.1) |
| Gastrointestinal organs | 730 | 31.0 | 93 | 1.5 (1.4–1.7) | 520 | 30.6 | 70 | 1.8 (1.6–2.0) |
| Urinary tract | 137 | 5.8 | 17 | 0.6 (0.5–0.7) | 73 | 4.3 | 10 | 1.0 (0.8–1.3) |
| Male genital organs | 136 | 5.8 | 17 | 0.2 (0.2–0.2) | 42 | 2.5 | 7 | 0.3 (0.3–0.4) |
| Breast | 0 | 0.0 | 0 | 0.0 (0.0–0.0) | 0 | 0.0 | 0 | 0.0 (0.0–0.0) |
| Melanoma of skin | 15 | 0.6 | 2 | 0.1 (0.1–0.2) | 6 | 0.4 | 1 | 0.3 (0.2–0.4) |
| Lymphoma and leukaemia | 128 | 5.4 | 14 | 0.5 (0.4–0.6) | 59 | 3.5 | 7 | 0.6 (0.5–0.7) |
| Other specified sites | 134 | 5.7 | 15 | 0.8 (0.7–0.9) | 49 | 2.9 | 6 | 0.7 (0.5–0.9) |
| Unknown | 167 | 7.1 | 22 | 2.7 (2.1–3.5) | 172 | 10.1 | 26 | 3.9 (2.8–5.4) |
| Total | 2354 | 100.0 | 292 | 1.0 (1.0–1.1) | 1699 | 100.0 | 229 | 1.7 (1.6–1.8) |
N = Numbers of cancer incidence and mortality.
N (%) = the percentage of the numbers of cancer incidence and mortality.
ASR (W) = Age standardized rates for the world, per 100,000 person years.
IRR: Incidence rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
MRR: Mortality rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
95% CI: 95% confidence intervals.
Fig. 1.
Cancer incidence and mortality for all cancers but non-melanoma skin cancer, 1983–2014, Greenland and the other Nordic countries, according to age.
ASR (W) = Age standardized rates for the world, per 100,00 person years.
4.1.1. Incidence
For women, the groups with the higher incident numbers for the entire time period were gastrointestinal, respiratory, female genital, and breast, accounting for about 75% of all cancers (Table 2a). For men, the incidence of the two groups, gastrointestinal and respiratory, dominated, accounting for 60% of all cancers (Table 2b). For both women and men, a low incidence was observed for melanoma of skin, urinary tract, and lymphoma and leukaemia (Table 2a, Table 2b).
4.1.2. Mortality
Respiratory and gastrointestinal cancers had the highest mortality for the entire time period, accounting for about 55% of all cancer deaths among women and almost 70% for men. The four groups with lowest number of cancer deaths were urinary tract, melanoma of skin, lymphoma and leukaemia, and other specified sites (Table 2a, Table 2b).
4.2. Changes in Trends in Age-Standardized Rates for Greenland
The age-standardized incidence rates (ASR (W)) for 1983–2014 were 301 and 291 per 100,000 person-years, for women and men, respectively. The incidence rates were slightly increasing (statistically significant for women) over the 32-year period with an estimated annual change per year (EAPC) for the age-standardized rates of 0.7% (95% CI: 0.1–1.4), while the increase among men did not reach statistical significance (EAPC = 0.4%; 95% CI: − 0.1–0.9). No significant changes were found for cancer mortality rates over the 32-year period; EAPCs were − 0.0 (95% CI: − 0.7; 0.6) for women and − 0.6 (95% CI: − 1.3; 0.1) for men (Table 3a, Table 3b). It should be mentioned that there was a tendency towards decline in cancer-specific mortality during the last 10–15 years (not shown in tables).
Table 3a.
Trend over time among women for all but non-melanoma skin cancer, Greenland, 1983–2014.
| Incidence |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Year | N | N (%) | ASR (W) | IRR (95% CI) | N | % | ASR (W) | MRR (95% CI) |
| 1983–1989 | 364 | 15.4 | 270 | 1.2 (1.1–1.3) | 239 | 15.6 | 190 | 1.8 (1.5–2.1) |
| 1990–1994 | 302 | 12.8 | 278 | 1.2 (1.0–1.3) | 217 | 14.2 | 216 | 2.0 (1.7–2.5) |
| 1995–1999 | 374 | 15.8 | 314 | 1.3 (1.1–1.4) | 255 | 16.6 | 231 | 2.2 (1.9–2.7) |
| 2000–2004 | 400 | 16.9 | 314 | 1.2 (1.1–1.4) | 256 | 16.7 | 208 | 2.1 (1.8–2.5) |
| 2005–2009 | 428 | 18.1 | 309 | 1.1 (1.0–1.3) | 285 | 18.6 | 211 | 2.3 (1.9–2.7) |
| 2010–2014 | 494 | 20.9 | 320 | 1.1 (1.0–1.3) | 280 | 18.3 | 182 | 2.1 (1.8–2.5) |
| Total | 2362 | 100.0 | 301 | 1.2 (1.1–1.2) | 1532 | 100.0 | 204 | 2.1 (1.9–2.2) |
| EAPC % | 0.7% (95% CI: 0.1–1.4) | − 0.0 (95% CI: − 0.7; 0.6) | ||||||
N = Numbers of cancer incidence and mortality.
N (%) = the percentage of the numbers of cancer incidence and mortality.
ASR (W) = Age standardized rates for the world, per 100,000 person years.
IRR: Incidence rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
MRR: Mortality rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
EAPC = Estimated annual percentage change in the age-standardized rates.
95% CI: 95% confidence intervals.
Table 3b.
Trend over time among men for all but non-melanoma skin cancer, Greenland, 1983–2014.
| Incidence |
Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Year | N | N (%) | ASR (W) | IRR (95% CI) | N | % | ASR (W) | MRR (95% CI) |
| 1983–1989 | 355 | 15.1 | 276 | 1.1 (1.0–1.2) | 265 | 15.6 | 229 | 1.5 (1.3–1.8) |
| 1990–1994 | 271 | 11.5 | 262 | 1.0 (0.9–1.1) | 221 | 13.0 | 252 | 1.7 (1.4–2.1) |
| 1995–1999 | 314 | 13.3 | 275 | 1.0 (0.9–1.1) | 255 | 15.0 | 254 | 1.8 (1.5–2.1) |
| 2000–2004 | 467 | 19.8 | 343 | 1.2 (1.0–1.3) | 332 | 19.5 | 263 | 2.0 (1.7–2.4) |
| 2005–2009 | 453 | 19.2 | 308 | 1.0 (0.9–1.1) | 308 | 18.1 | 232 | 1.9 (1.6–2.3) |
| 2010–2014 | 494 | 21.0 | 279 | 0.9 (0.8–1.0) | 318 | 18.7 | 184 | 1.6 (1.4–1.9) |
| Total | 2354 | 100.0 | 292 | 1.0 (1.0–1.1) | 1699 | 100.0 | 229 | 1.7 (1.6–1.8) |
| EAPC % | 0.4% (95% CI: − 0.1–0.9) | − 0.6 (95% CI: − 1.3; 0.1) | ||||||
N = Numbers of cancer incidence and mortality.
N (%) = the percentage of the total incidence and mortality.
ASR (W) = Age standardized rates for the world, per 100,000 person years.
IRR: Incidence rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
MRR: Mortality rate-ratios, with 95% confidence intervals, relative to the rates in the other Nordic countries.
EAPC = Estimated annual percentage change in the age-standardized rates.
95% CI: 95% confidence intervals.
4.3. Comparison With the Other Nordic Countries
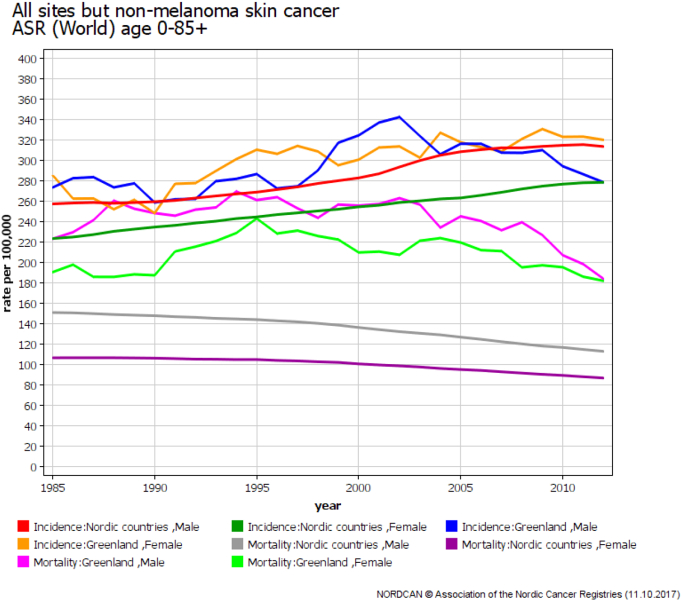
Compared to the other Nordic countries, the cancer incidence rate ratios (IRR) for all cancer sites were constant over time and only slightly higher than one, thus showing nearly the same incidence level, IRR = 1.2 (95% CI: 1.1–1.2) for women and IRR = 1.0 (95% CI: 1.0–1.1) for men. The cancer mortality rate ratios (MRR) increased slightly over time and rates were much higher in Greenland than in the other Nordic countries (Table 3a, Table 3b and Fig. 2). For the Nordic countries, the cancer mortality rates decreased during the time period studied, EAPCs were − 0.8 (95% CI: − 0.9; − 0.7) for women and − 1.1 (95% CI: − 1.2; − 1.0) for men (not shown in tables).
Fig. 2.
Cancer incidence and mortality for all cancers but non-melanoma skin cancer, 1983–2014, Greenland and the other Nordic countries.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
4.3.1. IRR for the Diagnosis Groups
Compared to the other Nordic countries, women and men in Greenland had significantly higher incidence rates for lip, oral cavity and pharynx, respiratory, gastrointestinal, and unknown sites. The IRRs for the entire calendar period were 3.9, 3.2, 1.7, and 3.3 among women, and 3.0, 2.3, 1.5, and 2.7 among men, respectively. Greenlandic women had a much lower risk of breast cancer while men had lower risk of cancer of the urinary tract and of the male genital organs compared to the other Nordic countries (Table 2a, Table 2b).
4.3.2. MRR for the Diagnosis Groups
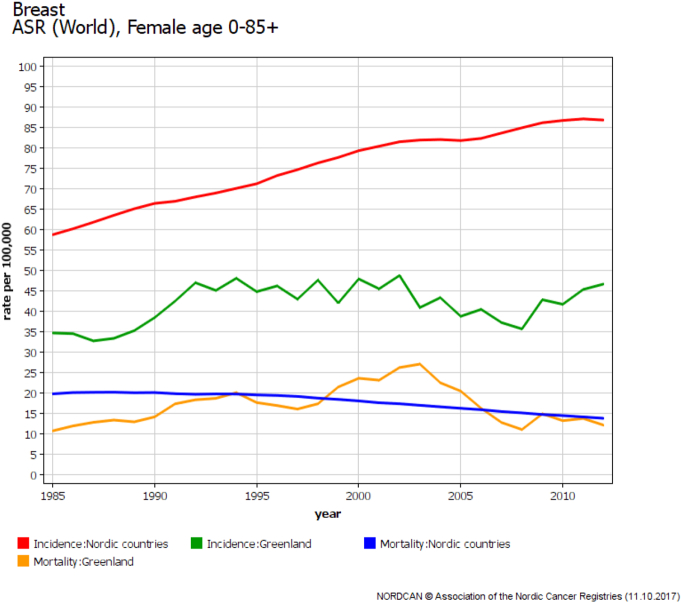
Mortality rates for both Greenlandic women and men compared to the other Nordic countries were much higher for lip, oral cavity and pharynx, respiratory, and unknown sites, with MRRs 9.9, 4.0, and 3.8 for women, and 6.0, 2.7, and 3.9 for men, respectively. The MRRs were much higher than the corresponding IRRs. Furthermore, the incidence rates for cancer of the urinary tract were lower among the Greenlandic women and men, while mortality rates were higher than the other Nordic countries, with IRRs 0.8 and 0.6 and MRRs 1.5 and 1.0, respectively (Table 2a, Table 2b). Breast cancer incidence in Greenland was much lower than in the other Nordic countries while the mortality of breast cancer was approximately the same (Fig. 3).
Fig. 3.
Breast cancer incidence and mortality among women, 1983–2014, Greenland and the other Nordic countries.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
4.3.3. Specific Cancer Sites
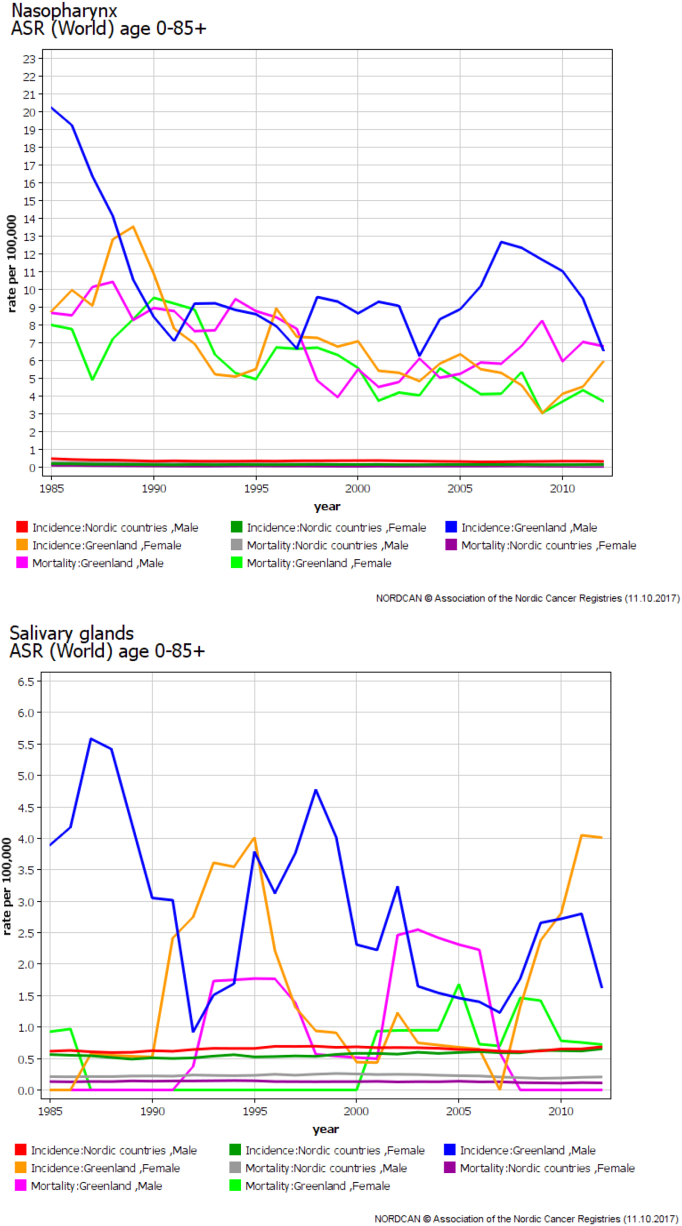
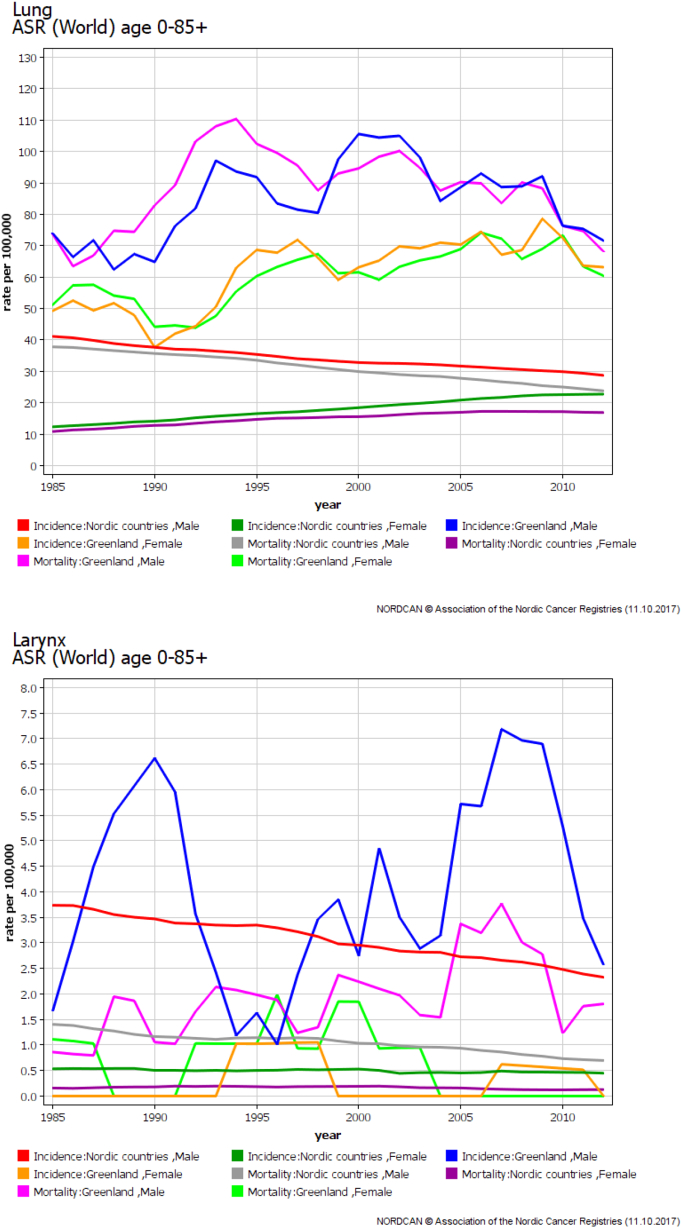
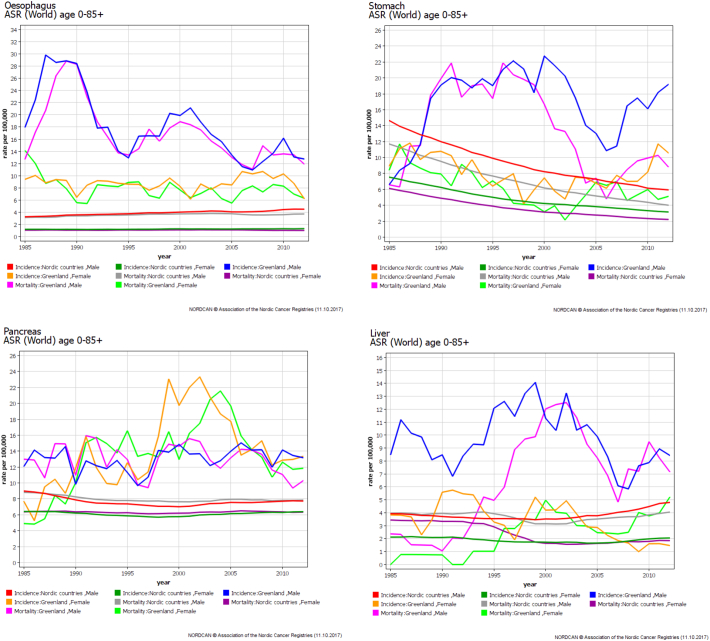
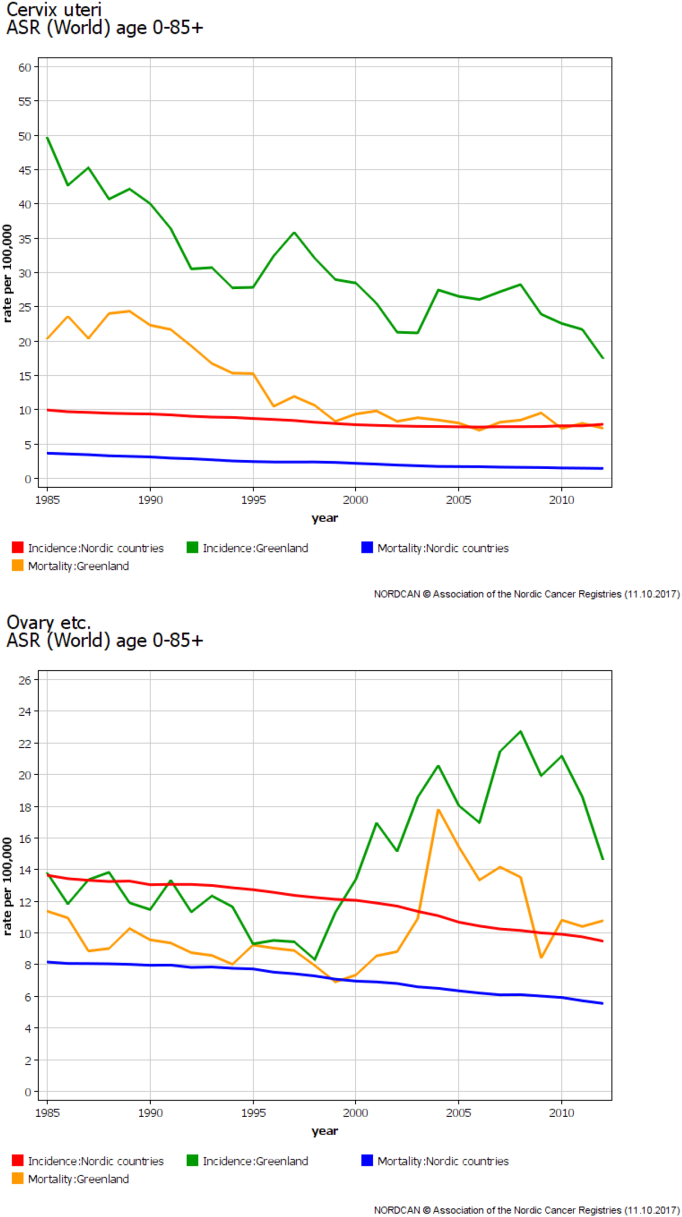
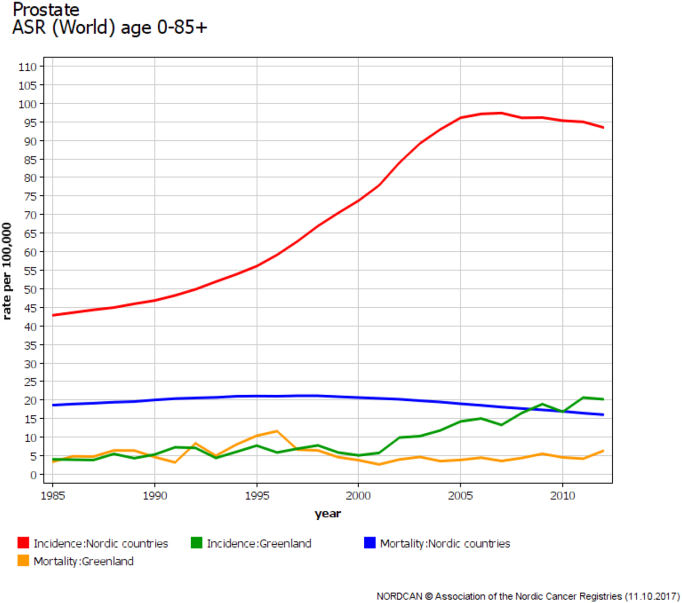
While the total cancer incidence rate was similar to the other Nordic countries, the distribution between cancer sites differed. The specific cancer sites contributing to the elevated incidence rate for lip, oral cavity, and pharynx were nasopharynx and salivary glands (Fig. 4). For respiratory cancer, it was lung for both sexes, as well as larynx among men (Fig. 5). In the group gastrointestinal organs, oesophagus, stomach, liver, and pancreas were the sites with elevated incidence rate (Fig. 6). In the group female genital organs, cervical cancer had the main influence even though decreasing over time, and an elevated incidence rate for ovarian cancer was seen from the year 2000 and on (Fig. 7). In the group male genital organs, it was especially the incidence rate of prostate cancer that was low among the Greenlandic men compared to the other Nordic countries (Fig. 8).
Fig. 4.
Cancer entities contributing to differences in incidence and mortality between Greenland and the other Nordic countries, nasopharynx and salivary glands, 1983–2014.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
Fig. 5.
Cancer entities contributing to differences in incidence and mortality between Greenland and the other Nordic countries, lung and larynx, 1983–2014.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
Fig. 6.
Cancer entities contributing to differences in incidence and mortality between Greenland and the other Nordic countries, oesophagus, stomach, pancreas, and liver, 1983–2014.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
Fig. 7.
Cancer entities contributing to differences in incidence and mortality between Greenland and the other Nordic countries, cervix of the uterus and ovaries, 1983–2014.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
Fig. 8.
Cancer entities contributing to differences in incidence and mortality between Greenland and the other Nordic countries, prostate, 1983–2014.
ASR (W) = Age standardized rates for the world, per 100,00 person years, with 5-years smoothing.
5. Discussion
NORDCAN receives data from Cancer Registries and Registers of Cause of Death from all the Nordic countries and allows for easily comparable data between the countries [17]. Nordic Cancer Registries are some of the most complete registries in the world [18]. There is a good concordance between cancer incidence data and the cancer-specific mortality derived from the Registers of Cause of Death, the registration is complete but the proportion of ill-defined cancer sites was considered high for data before 2002 [19], [20]. The cancer sites unknown and ill-defined have both higher incidence and mortality in Greenland compared to the other Nordic countries and the respective incidence and mortality follow the same trend. The government of Greenland only publishes brief data on cancer incidence and mortality in Greenland, but no data has been published regarding cancer survival [12], [21]. By using ASR (W) as well as numbers, the reported data are internationally comparable with the majority of earlier studies describing incidence and mortality from cancer.
Our report presents the best available data on the recent trend of cancer incidence and mortality for the population of Greenland for the time period 1983–2014. The summary groups and a five-year smoothing in graphs for the entire period of time 1983–2014 provide a better overview of the data without too many fluctuations. The population in Greenland is much smaller than the population in the other Nordic countries and this results in some fluctuations for the Greenlandic rates, whereas the Nordic countries have smooth trend lines.
Compared to the other Nordic countries, the overall incidence was similar with IRRs close to one while the overall MRRs were much higher. The time trend from 1983 to 2014 showed a significant increase in cancer incidence rates proportionally for Greenland and the other Nordic countries. Cancer mortality has decreased in the other Nordic countries while it has not changed much for the Greenlandic population, only with a slight decrease since 2000. NORDCAN has survival data for most of the Nordic countries. Survival calculations for the Faroe Islands and Greenland are not included, awaiting validation of complete follow-up for death and emigration. We can, based on the differences between the incidence and mortality rates, get an indication that the survival after cancer in Greenland is lower than in the other Nordic countries.
The cancer pattern in Greenland was different from the other Nordic countries and similar to the pattern among Inuit populations described in earlier studies [2], [4], [5], [6], [7], [22], [23]. Higher incidence rates were observed for cancer of nasopharynx, salivary glands, larynx, lung, oesophagus, stomach, liver, pancreas, uterine cervix, and ovaries. A high, but decreasing incidence of cervical cancer was observed throughout the observation period, although the incidence for the last five-year time period was still higher than the other Nordic countries. Lower incidence rates were seen for prostate, bladder, other specified sites, lymphoma and leukaemia, and melanoma of skin.
Friborg and colleagues stated a 12–14 percentage points lower histological verification of cancers in Greenland compared to Denmark based on a report from 1997 and around 4% of all cancers in Greenland were in the group unknown and unspecified sites in reports from 1993 to 1997 [5]. In our study, the proportion of histologically verified cancers for the entire time period was 82% in Greenland compared to 87% in the other Nordic countries. 76% and 85% were histology from the primary tumor, in Greenland and the other Nordic countries, respectively. A larger proportion of biopsies were from metastases in Greenland compared to the other Nordic countries (around 4 percentage points more). This is probably due to cancers being more advanced when diagnosed in remote areas in Greenland where diagnostic tools and specialized competence do not exist, resulting in a delay due to referral to a hospital in a larger city. The proportion of unknown and unspecified cancers constituted 8% (2–14%) during the observation period for Greenland compared to 4% (2–5%) for the other Nordic countries. This likely represents patients clinically diagnosed in an advanced stage where further diagnostics where unreasonable based on the patients' condition, especially where the specialized diagnostics where unavailable locally and the travel to another city was not considered an option. We found that the proportion of cancers known from death certificate only constituted 1.8% of all cancers in Greenland, compared to 0.2%, 0.5%, and 1.2%, for Iceland, Denmark, and Norway, respectively. The Greenlandic population lives dispersed along the coastline, and not all have easy access to the health care system, but still we consider the cancer registration comparable with the other Nordic countries.
Of known risk factors for cancer, smoking prevalence has increased over the years, but recently decreased slightly. There is a decreasing level of physical activity, change of diet to western food habits, and high consumption of alcohol [24]. Smoking is a strong risk factor for cancer in general, especially respiratory and urinary tract cancer. Diet and physical activities especially play a role in the development of gastrointestinal cancers, and high alcohol consumption especially increases the risk of gastrointestinal and liver cancer [25]. The UV-exposure is low in Greenland and type of skin may also influence the low incidence of melanoma of skin. The Greenlandic women have their first child at a younger age than women in the other Nordic countries even though the childbearing age is higher now than it was a few decades ago [1]. The changes in diet resulting in a decrease in intake of sea food have been found to correlate with reduced vitamin D status among the Greenlandic population during the last decades [26]. An inverse relationship between vitamin D and cancer incidence has been shown [27]. Exposure to persistent organic pollutants has been found to increase the risk of breast cancer in Greenlandic women and a combination with BRCA1 founder mutations further contributes to the risk [22], [28].
Many changes in life-style have taken place over the last decades and it is reasonable to believe that these changes have contributed to the increase in cancer incidence during the time period studied. Part of the increase might be due to an improvement in the reporting of cancer incidence and mortality in Greenland and a more accurate cancer registration during the last decades compared to the 1980's and 1990's. Since the Greenlandic population is small and the numbers of cancers are low, variation from year to year is seen. Data might also be influenced by a lack of consistency in reporting of cancer, either due to varying reporting routines and experience or because the reporting is not done by a medical doctor. It is a challenge to maintain well-established routines with frequent replacement of health care personnel.
Our results underline a high mortality of cancer in Greenland compared to the other Nordic countries. In a report by Bjerregaard from 1991, the mortality in Greenland during 1968–1985 was compared to mortality in Denmark. A high infant and child mortality and high rates of suicide, homicide, and accidents were found. The mortality rates from acute infectious diseases, ischemic heart disease and certain accidents decreased significantly, while mortality rates for lung cancer, other heart diseases, suicides, and homicides increased [29]. Even though the life expectancy is lower in Greenland than in the other Nordic countries, it has increased during the last decades and so has the proportion of elderly above the age of 60 [1]. Future studies looking at mortality and life expectancy in Greenland might shed more light on this.
The disparities in cancer incidence and mortality are not only seen among the Greenlandic population where the majority is indigenous. A review on cancer patterns among circumpolar populations looked into three indigenous groups, the Inuit, Athabaskan Indians, and the Sami. The Inuit had an overall increase of cancer incidence of all sites combined, the sites contributing most were lung, colorectal, and female breast cancer, while cervical cancer declined. The Athabaskans had a higher risk of prostate and breast cancer relative to the world average in contrast to the Inuit. There was no significant difference between cancer incidence among the Sami compared to non-Sami [30]. The cancer mortality from oesophageal, lung and breast cancer among the indigenous population of coastal Chukotka was much higher than the rest of Russia [31], [32]. The cancer mortality among Aboriginal people living on reserves and Northern villages in Quebec did not show any increased overall cancer mortality during 1988–2004, even though the cancer pattern differed [33]. Enhanced attention to indigenous people is necessary for a better worldwide cancer control.
The high mortality from cancer in Greenland could partly be explained by inequality in health care based on geography. A recent publication found that the median time from first consultation to referral for colorectal cancer was four days in Nuuk versus 55 days for patients from other cities in Greenland, and they found a lack of standardized examination in primary care [34]. The referral from the main hospital in Nuuk to Denmark might further delay the process. A probable less aggressive treatment for cancer in Greenland compared to Denmark also needs to be assessed, including the reasons behind. A study by Augustussen and colleagues assessed the level of satisfaction among relatives to patients receiving advanced cancer care in Greenland, 70% of the relatives were dissatisfied with the length of time required to diagnose cancer, supporting that time delay is a problem [35].
There is a high incidence of potentially preventable cancers, especially the ones associated with smoking (lung and head and neck cancers) and oncogenic infections (stomach, liver, and cervical cancer). Decreasing the prevalence of smoking, especially the early onset of smoking among the youth, decreasing alcohol consumption as well as focus on physical activity and healthy eating habits are all reflected in ongoing programs initiated by the government of Greenland [36]. Nasopharyngeal carcinoma and carcinoma of the salivary gland are both associated with a prior Epstein–Barr virus (EBV) infection, which is seen more often and in an early age in Greenland [5]. There is a high prevalence of chronic Hepatitis B virus (HBV) infection in the Greenlandic population (around 10–15%), the incidence of liver cancer is high, although not as high as other countries with high prevalence of HBV infection [37]. The cervical cancer screening in Greenland, initiated in 1998, was assessed by Holst and colleagues, low screening coverage was observed with the highest level being 54% in 2011 [38]. Vaccination against HPV for girls (2008) and HBV (2010) is now a part of the nationwide vaccination program in Greenland [21].
Besides the initiatives regarding prevention, there is also a need to focus on cancer symptoms, early detection of cancer, and reduction of time delay. There is only a screening program for cervical cancer in Greenland. With the increasing incidence of cancer, such as breast, lung, and colorectal cancer, it is important to consider screening programs or more specialized diagnostics in Greenland, such as triple test for breast cancer implemented in Nuuk since April 2017 together with breast conserving surgery as an option. Screening with fecal-occult-blood test (FOBT), which is easily carried out, can help reduce the mortality from colorectal cancer. Also, recruiting pathologists to Nuuk could optimize surgical cancer treatment for certain cancer diagnoses by eliminating time delay associated with awaiting final histology from Denmark. Furthermore, it should be prioritized to get oncological expertise in Nuuk for diagnostics, treatment, and palliative care in order to improve the quality of cancer care and a better cancer control.
Our data point to a need to reduce cancer mortality in Greenland. The changing life-style and the increased aging of the population can be expected to further increase the cancer burden in Greenland, which advocates continued focus on cancer prevention. The data reported here might prove useful for planning of future studies as well as guidelines for cancer care in Greenland benchmarked against the political decisions. The data can also be used for improvement in Greenlandic cancer registration, more detailed studies of the differences within Greenland (including geographical inequality), and for comparison with other Inuit communities and indigenous groups. We aim to promote improved cancer care in Greenland and also to increase awareness of cancer among Inuit and indigenous people. We strongly believe that the data made available in this study is one step towards that goal.
Funding
No funding received.
Ethical Considerations
We have used tabulated data from the cancer statistics database NORDCAN. The data is anonymous and thus an approval from the Greenlandic or Danish Ethical Committee is not required.
Authors' Contributions
UY, GE, and HS contributed to the study conception and design. GE and NC contributed to data acquisition. UY, GE, and HS contributed to analysis and interpretation. UY drafted the manuscript. UY, GE, HS, NC, EZ, HT, FS, PB and LCT critically reviewed the manuscript.
Declaration of Interests
We declare no competing interests.
References
- 1.Greenland statistics. 2017. Greenland in figures.http://www.stat.gl/publ/en/GF/2017/pdf/GreenlandinFigures2017.pdf Available from. [Google Scholar]
- 2.Prener A., Nielsen N.H., Storm H.H., Hansen J.P., Jensen O.M. Cancer in Greenland 1953–1985. APMIS Suppl. 1991;20:1–79. [PubMed] [Google Scholar]
- 3.Rethinking Greenland and the Arctic in the era of climate change: new Northern Horizons. Routlegde; London & New York: 2015. [Google Scholar]
- 4.Storm H.H., Nielsen N.H., Prener A., Jensen O.M. A comparison of cancer in Greenland and Denmark. A study based on routinely collected incidence data 1973–1985, using the Danish population as baseline. Arctic Med Res. 1991;(Suppl:470–71) [PubMed] [Google Scholar]
- 5.Friborg J.T., Melbye M. Cancer patterns in Inuit populations. Lancet Oncol. 2008;9:892–900. doi: 10.1016/S1470-2045(08)70231-6. [DOI] [PubMed] [Google Scholar]
- 6.Kelly J., Lanier A., Santos M. Cancer among the circumpolar Inuit, 1989–2003. I. Background and methods. Int J Circumpolar Health. 2008;67:396–407. doi: 10.3402/ijch.v67i5.18348. [DOI] [PubMed] [Google Scholar]
- 7.Kelly J., Lanier A., Santos M. Cancer among the circumpolar Inuit, 1989–2003. II. Patterns and trends. Int J Circumpolar Health. 2008;67:408–420. [PubMed] [Google Scholar]
- 8.Bjerregaard P. Rapid socio-cultural change and health in the Arctic. Int J Circumpolar Health. 2001;60:102–111. [PubMed] [Google Scholar]
- 9.Jorgensen M.E., Bjerregaard P., Borch-Johnsen K. Diabetes and impaired glucose tolerance among the Inuit population of Greenland. Diabetes Care. 2002;25:1766–1771. doi: 10.2337/diacare.25.10.1766. [DOI] [PubMed] [Google Scholar]
- 10.Greenland statistics. 2017. Population by time and age.http://www.stat.gl/dialog/topmain.asp?lang=en&subject=Population&sc=BE Available from. [Google Scholar]
- 11.Statistics Denmark. 2016. Life expectancy in Denmark.http://www.dst.dk/Site/Dst/Udgivelser/GetPubFile.aspx?id=20715&sid=befudv2015 Available from. [Google Scholar]
- 12.Kræftredegørelsen 2011. [Cancer statement 2011]. Naalakkersuisut - Government of Greenland; 2011. http://naalakkersuisut.gl/~/media/Nanoq/Files/Publications/DepartementforSundhedogInfrastruktur/Sundhed/Kraeftredegoerelsen_DK_web.PDF Available from. [In Danish] [Google Scholar]
- 13.A comparative review of circumpolar health systemsInt J Circumpolar Health. 2012;71:1–116. doi: 10.1080/22423982.2012.11864611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chatwood S., Bytautas J., Darychuk A. Approaching a collaborative research agenda for health systems performance in circumpolar regions. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.21474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Storm H.H., Michelsen E.V., Clemmensen I.H., Pihl J. The Danish Cancer Registry–history, content, quality and use. Dan Med Bull. 1997;44:535–539. [PubMed] [Google Scholar]
- 16.Engholm G., Ferlay J., Christensen N. NORDCAN-a Nordic tool for cancer information, planning, quality control and research. Acta Oncol. 2010;49:725–736. doi: 10.3109/02841861003782017. [DOI] [PubMed] [Google Scholar]
- 17.Engholm G., Ferley J., Christensen N. Association of Nordic Cancer Registries. Danish Cancer Society; 08/07/2016. Cancer incidence, mortality, prevalence and survival in the Nordic countries, version 7.3.http://www.ancr.nu Available from. [Google Scholar]
- 18.Pukkala E., Engholm G., Hojsgaard Schmidt L.K. Nordic Cancer Registries - an overview of their procedures and data comparability. Acta Oncol. 2017;56:1–16. doi: 10.1080/0284186X.2017.1407039. [DOI] [PubMed] [Google Scholar]
- 19.Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39:26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 20.Mathers C.D., Fat D.M., Inoue M., Rao C., Lopez A.D. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–177. [PMC free article] [PubMed] [Google Scholar]
- 21.Årsberetning 2014/2015. [Annual reports 2014/2015]. The National Board of Health in Greenland; 2014. http://www.nun.gl/%C3%85rsberetning-2014-2015/59 Available from. [In Danish] [Google Scholar]
- 22.Fredslund S.O., Bonefeld-Jorgensen E.C. Breast cancer in the Arctic–changes over the past decades. Int J Circumpolar Health. 2012;71 doi: 10.3402/ijch.v71i0.19155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friborg J., Koch A., Wohlfarht J., Storm H.H., Melbye M. Cancer in Greenlandic Inuit 1973–1997. Int J Circumpolar Health. 2004;63:195–198. doi: 10.3402/ijch.v63i0.17900. [DOI] [PubMed] [Google Scholar]
- 24.Bjerregaard P., Aidt A. Greenland N-Go; Nuuk: 2010. Levevilkår, livsstil og helbred: Befolkningsundersøgelsen i Grønland 2005–2009. [Living conditions, lifestyle and health: Populationbased survey in Greenland 2005–2009. In Danish] [Google Scholar]
- 25.Food, nutrition, physical activity, and the prevention of cancer: a global perspective. World Cancer Research Fund/American Institute for Cancer Research; 2007. http://www.aicr.org/assets/docs/pdf/reports/Second_Expert_Report.pdf Available from. [Google Scholar]
- 26.Nielsen N.O., Jorgensen M.E., Friis H. Decrease in vitamin D status in the Greenlandic adult population from 1987–2010. PLoS One. 2014;9 doi: 10.1371/journal.pone.0112949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant W.B. A review of the evidence supporting the vitamin D-cancer prevention hypothesis in 2017. Anticancer Res. 2018;38:1121–1136. doi: 10.21873/anticanres.12331. [DOI] [PubMed] [Google Scholar]
- 28.Wielsoe M., Kern P., Bonefeld-Jorgensen E.C. Serum levels of environmental pollutants is a risk factor for breast cancer in Inuit: a case control study. Environ Health. 2017;16:56. doi: 10.1186/s12940-017-0269-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bjerregaard P. Disease pattern in Greenland: studies on morbidity in Upernavik 1979–1980 and mortality in Greenland 1968–1985. Arctic Med Res. 1991;50(Suppl. 4):1–62. [PubMed] [Google Scholar]
- 30.Young T.K., Kelly J.J., Friborg J., Soininen L., Wong K.O. Cancer among circumpolar populations: an emerging public health concern. Int J Circumpolar Health. 2016;75 doi: 10.3402/ijch.v75.29787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dudarev A.A., Chupakhin V.S., Odland J.O. Cancer mortality in the indigenous population of coastal Chukotka, 1961–1990. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.20471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dudarev A.A., Chupakhin V.S., Odland J.O. Cancer incidence and mortality in Chukotka, 1997–2010. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.20470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Louchini R., Beaupre M. Cancer incidence and mortality among Aboriginal people living on reserves and northern villages in Quebec, 1988–2004. Int J Circumpolar Health. 2008;67:445–451. doi: 10.3402/ijch.v67i5.18355. [DOI] [PubMed] [Google Scholar]
- 34.Tolstrup J., Madsen R.C., Sneftrup M.V., Niclasen B. Greenlandic patients with colorectal cancer: symptomatology, primary investigations and differences in diagnostic intervals between Nuuk and the rest of the country. Int J Circumpolar Health. 2017;76 doi: 10.1080/22423982.2017.1344086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Augustussen M., Hounsgaard L., Pedersen M.L., Sjogren P., Timm H. Relatives' level of satisfaction with advanced cancer care in Greenland - a mixed methods study. Int J Circumpolar Health. 2017;76 doi: 10.1080/22423982.2017.1335148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inuuneritta II . Naalakkersuisut - The Government of Greenland; 2012. Naalakersuisuts strategier og målsætninger for folkesundheden 2013–2019.http://peqqik.gl/Footerpages/Publikationer/Inuuneritta_2.aspx?sc_lang=da-DK [Strategies and goals for the public health 2013–2019. In Danish] Available from. [Google Scholar]
- 37.Rex K.F., Andersen S., Krarup H.B. Hepatitis B among Inuit: a review with focus on Greenland Inuit. World J Hepatol. 2015;7:1265–1271. doi: 10.4254/wjh.v7.i9.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holst S., Wohlfahrt J., Kjaer S.K. Cervical cancer screening in Greenland, 1997–2011: screening coverage and trends in the incidence of high-grade cervical lesions. Gynecol Oncol. 2016;143:307–312. doi: 10.1016/j.ygyno.2016.03.029. [DOI] [PubMed] [Google Scholar]