Abstract
Importance:
After a period of rapid growth, utilization of cardiac stress testing has recently decreased among Medicare beneficiaries and in a large integrated health system. However, it is not known whether declines in stress testing are universal, or are confined to certain populations.
Objective:
To determine trends in stress test utilization rates among a large and diverse cohort of commercially insured patients.
Design:
Serial cross-sectional study with time trends from 2005 to 2012.
Setting:
Comprehensive administrative claims from a large national managed care company.
Participants:
All members of the national managed care company aged 25–64 years.
Main Outcomes and Measures:
Age- and sex-adjusted rates of cardiac stress tests per calendar quarter. Linear trends in rates were determined using negative binomial regression models with procedure count as the dependent variable, calendar quarter as the key independent variable, and the size of the population as a logged offset term.
Results:
We identified 2,085,591 stress tests performed among 32,921,838 unique persons, of whom 51% were women and 23% were non-white. There was a small (2%) increase in stress testing rates from 2005 to 2012 (3486 [95% CI: 3458 to 3514] versus 3552 [95% CI: 3522 to 3582] tests per 100,000 person-years; p for linear trend=0.01). Declines in nuclear single photon emission computed tomography (a 15% relative decrease; p=0.03) were offset by increases in the use of stress echocardiography (a 24% relative increase; p<.001), exercise electrocardiography (a 10% relative increase; p<.001), and other stress testing modalities (a 66% relative increase; p<.001). Rates of stress testing increased most significantly among members aged 25–34 years (a 70% relative increase; p<.001), but declined among members aged 55–64 (a 9% relative decrease; p<.001).
Conclusions and Relevance:
In contrast to declines in stress test use in some health care systems, we observed a small increase in stress test utilization among a nationally representative cohort of commercially insured patients. Our findings suggest that observed trends in stress test utilization may have been driven more strongly by unique characteristics of populations and health systems than national efforts to reduce overuse of testing.
INTRODUCTION:
Due to rapid growth in the use of cardiac imaging from 1999 to 2006, cardiac stress tests have become a major focus of the debate on rising health care costs and inappropriate utilization1–3. Although recent studies conducted among Medicare beneficiaries and in Kaiser Permanente have shown reductions in stress testing rates since 20064–6, it is unknown if declining rates of testing are universal or confined to certain populations or payment models.
In this study, we examined whether the volume of stress tests and the modalities of testing have changed among a large and diverse cohort of commercially insured patients. If consistent declines in stress test use are observed in our population, national physician-led efforts to reduce overuse such as dissemination of appropriate use criteria may be responsible since such efforts are unlikely to have differential effects between health systems and insurers. On the other hand, if stress test use is stable or increasing in our cohort, organizational characteristics of health systems including payment models and/or population differences may be responsible for changes in stress test utilization. Therefore, we used a nationally representative sample of commercial insurance claims to estimate temporal trends in the annual volume of cardiac stress tests between 2005 and 2012.
METHODS:
Study Data
Data were obtained from the Clinformatics™ Data Mart (OptumInsight, Eden Prairie, MN), which is a database of administrative health claims for members of a large national managed care company. Administrative claims submitted for payment are verified, adjudicated, and de-identified prior to inclusion in Clinformatics™ Data Mart. The database consists of comprehensive medical claims for approximately 15 million annual covered lives spanning all 50 U.S. states, and includes member eligibility, demographic data, and socioeconomic data. For this study, we identified comprehensive administrative claims for all members from 2005–2012. We excluded patients under the age of 25 years due to the negligible expected likelihood of stress testing in this age group, and those over the age of 64 since Medicare coverage is nearly universal after that age. All other members were included.
Identification of Stress Tests
All cardiac stress tests performed among the eligible cohort from 2005–2012 were identified using Current Procedural Technology (CPT) codes for exercise electrocardiography, nuclear SPECT, stress echocardiography, cardiac computed tomography angiography, perfusion positron emission tomography, and stress cardiac magnetic resonance. CPT codes used are provided in an Online Supplemental File. Exercise electrocardiography tests performed within 48 hours of a SPECT or stress echocardiogram test were considered to be a single imaging stress event.
Calculation of Procedure Rates
We calculated the incidence of stress testing per 100,000 person-years for each calendar quarter. The denominator was defined as all members of the managed care company between the ages of 25 and 64 who had at least 30 days of membership in the health plan during that quarter. Rates of stress tests per person-quarter were determined by dividing the total number of stress tests performed by the denominator in each calendar quarter, and were adjusted for age and sex using direct standardization.
Statistical Analysis
Differences in characteristics of the overall cohort over time were compared using Chi-square tests for categorical variables and Student t-tests for continuous variables. Linear trends in the annual rates of stress tests were assessed using negative binomial regression models with procedure count as the dependent variable and calendar quarter as the key independent variable. Models were adjusted for age and sex, and included the size of the population as a logged offset term. All statistical tests were two-sided, with p<0.05 indicating statistical significance. Analyses were performed using Stata version 13.1 (Stata Corp, College Station, TX). The study protocol was deemed exempt by the Institutional Review Board at the University of Pennsylvania.
RESULTS:
Our study cohort consisted of 32,921,838 unique members representing 224.6 million member-quarters of membership from 2005–2012. Over the study period, we identified 2,085,591 stress tests. In 2011–2012, 50% of the cohort were women and 23% were non-white (Table 1).
TABLE 1:
Demographics of Commercially Insured Patients, 2005–2012
| 2005–2006 n=11,578,087a |
2007–2008 n=11,599,670a |
2009–2010 n=10,465,398a |
2011–2012 n=9,595,615a |
P value | |
|---|---|---|---|---|---|
| Age Category | <.001 | ||||
| 25–34 y | 26 | 28 | 27 | 28 | |
| 35–44 y | 28 | 27 | 28 | 28 | |
| 45–54 y | 27 | 27 | 27 | 27 | |
| 55–64 y | 19 | 18 | 18 | 17 | |
| Women | 51 | 51 | 51 | 50 | <.001 |
| Race | <.001 | ||||
| White | 74 | 72 | 72 | 73 | |
| Black | 9 | 10 | 10 | 10 | |
| Hispanic | 9 | 10 | 10 | 9 | |
| Asian | 3 | 4 | 4 | 4 | |
| Unknown | 5 | 4 | 4 | 4 | |
| Region | <.001 | ||||
| Northeast | 11 | 10 | 10 | 9 | |
| South | 45 | 48 | 48 | 47 | |
| Midwest | 29 | 26 | 25 | 26 | |
| West | 15 | 16 | 17 | 18 |
Data are expressed as percentages.
Unique members eligible for at least one calendar quarter during the two-year period.
The overall age- and sex-adjusted use of stress tests increased by a relative rate of 2% over the study period (p=0.01; Table 2). Stress test use increased from 2005 (3486 [95% CI: 3458 to 3514] tests per 100,000 person-years) to a peak in 2009 (3933 [95% CI 3905 to 3961] tests per 100,000 person-years) and then slowly declined to 2012 (3552 tests [95% CI: 3522 to 3582] per 100,000 person-years).
TABLE 2:
Annual Incidence of Stress Testing, 2005–2012
| 2005–2006 n=11,578,087a |
2007–2008 n=11,599,670a |
2009–2010 n=10,465,398a |
2011–2012 n=9,595,615a |
P for trendb | |
|---|---|---|---|---|---|
| Stress Tests | |||||
| SPECT | 298,390 (2.6) | 310,935 (2.7) | 272,026 (2.6) | 210,277 (2.2) | 0.03 |
| SE | 107,548 (0.9) | 113,458 (1.0) | 118,786 (1.1) | 112,692 (1.2) | <.001 |
| EECG | 126,798 (1.1) | 124,497 (1.1) | 127,325 (1.2) | 122,504 (1.3) | <.001 |
| PET/CCTA/CMR | 4,423 (0.0) | 13,094 (0.1) | 11,638 (0.1) | 11,200 (0.1) | <.001 |
| Total | 537,159 (4.6) | 561,984 (4.8) | 529,775 (5.1) | 456,673 (4.8) | 0.01 |
Unique members eligible for at least one calendar quarter during the two-year period
Trends tested using negative binomial regressions on quarterly count data from 2005–2012, adjusted for age and sex, and offset by population size.
Data are expressed as: n (%)
SPECT denotes nuclear single photon emission computed tomography, SE denotes stress echocardiography, EECG denotes exercise electrocardiography, PET denotes nuclear positron emission tomography, CCTA denotes coronary computed tomography angiography, CMR denotes stress cardiac magnetic resonance.
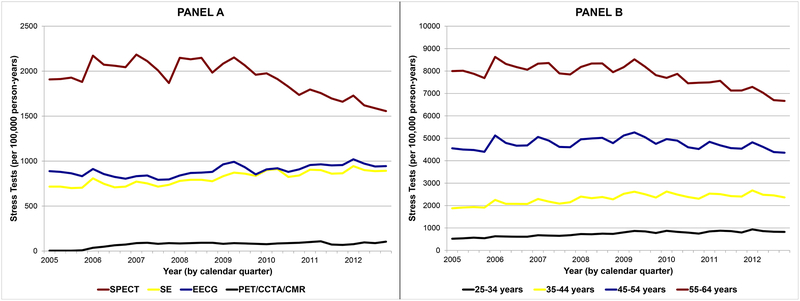
Use of SPECT decreased by 14.9% over the study period (p=0.03), peaking in 2008 (2103 [95% CI 2083 to 2123] tests per 100,000 person-years) and then steadily declining until 2012 (1623 [95% CI 1603 to 1643] tests per 100,000 person-years; Figure 1A). Use of stress echocardiography steadily increased by 23.9% (p<.001), from 709 [95% CI 697 to 721] tests per 100,000 person-years in 2005 to 906 [95% CI 894 to 920] tests per 100,000 person-years in 2012. Use of exercise electrocardiography steadily increased by 10.2% (p<.001), from 861 [95% CI 847 to 873] tests per 100,000 person-years in 2005 to 969 [95% CI 953 to 985] tests per 100,000 person-years in 2012. Use of alternative imaging modalities increased by 65.5% from 2006 (the first year CPT codes for coronary computed tomography angiography were used) to 2012 (p<.001).
FIGURE 1:
Adjusted Quarterly Rates of Stress Testing by Modality (Panel A) and Age Group (Panel B) From 2005–2012. Relative rates of nuclear single photon emission computed tomography decreased by 15% (p=0.03) but were offset by increases in the use of all other stress testing modalities (Panel A). Relative rates of stress testing increased by 70% among members aged 25–34 (p<.001), and decreased by 9% among members aged 55–64 (p<.001; Panel B).
Stress test use increased steadily among members aged 25–34 (a 70% relative increase from 2005 to 2012; p<.001; Figure 1B) and members aged 35–44 (a 36% relative increase; p<.001). There was no change in stress test use among members aged 45–54 (p=0.51), and there was a decline in stress test use among members aged 55–64 (a 9% relative decrease; p<.001).
DISCUSSION:
Contrary to recent findings among Medicare beneficiaries and in Kaiser Permanente, our data from a large cohort of commercially insured patients show a small increase in the overall use of stress tests from 2005 to 2012. Stress testing rates increased substantially among patients aged 25–44 years, and for all modalities except nuclear SPECT. These findings suggest that trends in stress test use may be driven more strongly by unique characteristics of health systems and populations than national efforts to reduce overuse of testing by physician groups.
Differences in Health Systems and Populations
Recent studies have revealed that from 2005 to 2012 there was a nearly 50% relative decline in use of stress tests in Kaiser Permanente, and a 25% relative decline in use of stress tests among Medicare fee-for-service beneficiaries4–6. Divergent trends in stress test use between these populations and our cohort may be explained by differences in health system organizational characteristics. Integrated health systems such as Kaiser Permanente use capitated payment models without direct financial incentives to perform testing, which often leads to lower procedure use compared to traditional fee-for-service payment models7–9. These health systems often emphasize quality measurement and accountability, which could further contribute to declines in procedure use.
Recent studies have also shown that health care utilization may be different between Medicare beneficiaries and privately insured patients who are located in the same geographic regions10,11. This may be due to hospital consolidation leading to preferential reductions in testing among Medicare beneficiaries, since they tend to use more healthcare resources in general12,13.
Patients under the age of 64 years have not been well-represented in previous studies of national stress test trends. However, age alone is unlikely to explain the divergent trends in stress testing over time since the age groups in our cohort and those previously studied remained largely stable over the study period. More research is needed to understand whether the striking increase in stress test utilization among younger patients in our cohort is due to evolving trends in the detection and surveillance of coronary artery disease, or a need for improvement in patient selection for testing14,15.
Policy Implications
Healthcare policies are often based on data from Medicare beneficiaries. Our study shows that utilization patterns of diagnostic cardiac imaging may be different among commercially insured patients. Furthermore, the disparate trends in use of stress testing between our population and previously studied cohorts suggests that organizational characteristics of health systems had a greater effect on stress test trends than physician-led efforts to reduce overuse such as appropriate use criteria. This finding is consistent with a recent meta-analysis that found that reported rates of appropriate use of stress imaging tests have not significantly changed since publication of appropriate use criteria14.
Limitations
We did not have details on the indications for stress tests, and therefore were unable to directly assess rates of appropriateness or the percentage of tests performed for detection of coronary artery disease. Also, differential enrollment of sicker persons or disenrollment of healthier persons could lead to increases in the use of stress testing, but these effects could not be accurately determined.
Conclusions
We observed a small increase in the overall use of stress tests among a large cohort of commercially insured patients. Divergent trends in stress test use between populations suggest that organizational characteristics of health systems including payment models may strongly influence utilization of cardiovascular testing. Trends in use of cardiac imaging derived from single health systems or insurers may not reflect larger practice patterns.
Acknowledgements:
Dr. Kini had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding/Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. At the time the study was conducted, Dr. Kini was supported by grants 5T32HL007843–18 and L30HL129283–01 by the National Institutes of Health. Dr. Groeneveld was supported by grants IIR14–077 by the Veterans Health Administration and 1R01-HS023615 by the National Institutes of Health.
Footnotes
Conflict of Interest Disclosures: All authors report no conflicts of interest.
REFERENCES:
- 1).Mark DB, Anderson JL, Brinker JA et al. ACC/AHA/ASE/ASNC/HRS/IAC/Mended Hearts/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SNMMI 2014 health policy statement on use of noninvasive cardiovascular imaging: a report of the American College of Cardiology Clinical Quality Committee. J Am Coll Cardiol. 2014;63:698–721. [DOI] [PubMed] [Google Scholar]
- 2).Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circ Cardiovasc Qual Outcomes. 2012;5(1):31–6. [DOI] [PubMed] [Google Scholar]
- 3).Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med. 2014;161(7):482–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).McNulty EJ, Hung YY, Almers LM, Go AS, Yeh RW. Population trends from 2000–2011 in nuclear myocardial perfusion imaging use. JAMA. 2014;311(12):1248–9. [DOI] [PubMed] [Google Scholar]
- 5).Levin DC, Parker L, Halpern EJ, Rao VM. Recent Trends in Imaging for Suspected Coronary Artery Disease: What Is the Best Approach? J Am Coll Radiol. 2016;13(4):381–6. [DOI] [PubMed] [Google Scholar]
- 6).Levin DC, Parker L, Intenzo CM, Rao VM. Recent reimbursement changes and their effect on hospital and private office use of myocardial perfusion imaging. J Am Coll Radiol. 2013;10:198–201. [DOI] [PubMed] [Google Scholar]
- 7).Matlock DD, Groeneveld PW, Sidney S et al. Geographic variation in cardiovascular procedure use among Medicare fee-for-service vs Medicare Advantage beneficiaries. JAMA. 2013;310(2):155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).McWilliams JM, Dalton JB, Landrum MB et al. Geographic variation in cancer-related imaging: Veterans Affairs health care system versus Medicare. Ann Intern Med. 2014;161(11):794–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Kini V, McCarthy FH, Rajaei S, Epstein AJ, Heidenreich PA, Groeneveld PW. Variation in use of echocardiography among veterans who use the Veterans Health Administration vs Medicare. Am Heart J. 2015;170(4):805–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Cooper Z, Craig SV, Gaynor M, Van Reenen J. The price ain’t right? Hospital prices and health spending on the privately insured. National Bureau of Economic Research: NBER Working Paper No. 21815 2015. Available at: http://www.healthcarepricingproject.org/sites/default/files/pricing_variation_manuscript_0.pdf. Accessed March 23, 2016. [Google Scholar]
- 11).Newhouse JP, Garber AM. Geographic variation in health care spending in the United States: insights from an Institute of Medicine report. JAMA. 2013;310(12):1227–8. [DOI] [PubMed] [Google Scholar]
- 12).Dafny L Hospital industry consolidation--still more to come? N Engl J Med. 2014;370(3):198–9. [DOI] [PubMed] [Google Scholar]
- 13).Welch HG, Hayes KJ, Frost C. Repeat testing among Medicare beneficiaries. Arch Intern Med. 2012;172(22):1745–51. [DOI] [PubMed] [Google Scholar]
- 14).Fonseca R, Negishi K, Otahal P, Marwick TH. Temporal changes in appropriateness of cardiac imaging. J Am Coll Cardiol. 2015;65(8):763–73. [DOI] [PubMed] [Google Scholar]
- 15).Patel MR, Peterson ED, Dai D et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–95. [DOI] [PMC free article] [PubMed] [Google Scholar]