Abstract
Background
The aim of this study was to assess the incidence, clinicopathologic characteristics, prognostic factors, and treatment outcomes in lung large cell neuroendocrine carcinoma (LCNEC).
Material/Methods
Patients diagnosed with lung LCNEC between 2000 and 2013 were identified using the Surveillance, Epidemiology, and End-Results database. Kaplan–Meier methods and univariate and multivariate analyses were used for statistical analysis.
Results
A total of 2097 patients were identified. The total age-adjusted incidence rate of lung LCNEC was 0.3/100 000, with a rise in incidence over the study period. The 5-year lung cancer-specific survival (LCSS) and overall survival (OS) were 20.7% and 16.7%, respectively. Multivariate analysis indicated that age ≥65 years, male sex, advanced tumor stage, advanced nodal stage, not undergoing surgery. and not undergoing chemotherapy were independent adverse indicators for survival outcomes. After stratification by tumor stage, undergoing surgery was associated with more favorable LCSS and OS compared with those without surgery, regardless of tumor stage.
Conclusions
LCNEC is a rare lung cancer subtype with a dismal prognosis. Primary surgical treatment has significant survival benefits, even for stage IV patients. The optimal treatment strategies for lung LCNEC require further investigation.
MeSH Keywords: Carcinoma, Non-Small-Cell Lung; Epidemiologic Study Characteristics as Topic; Survival Analysis
Background
Pulmonary large cell neuroendocrine carcinoma (LCNEC) is a rare, highly aggressive lung cancer subtype, accounting for about 3% of all lung cancers [1,2]. LCNEC was introduced as a lung cancer classification in 1991, and is characterised by large cells with a neuroendocrine appearance under light microscopy, a high mitotic rate, a low nuclear-to-cytoplasmic ratio, abundant necrosis, and frequent nucleoli. These pathologic characteristics were used as standards for classification for lung LCNEC diagnosis by the World Health Organization (WHO) in 1999 [3]. The 2015 WHO standards have classified lung LCNEC, small cell lung carcinoma (SCLC), atypical carcinoids, and typical carcinoids together as neuroendocrine neoplasms [4].
Lung LCNEC has a poor survival outcome. Local recurrence and distant metastasis are the main failure modes [5,6], and previous studies have shown a 5-year survival of 15–57% [5–8]; the large difference in survival rates may be due to sample size in these studies. Age, tumor size, cumulative tobacco consumption, neuroendocrine marker, tumor stage, and nodal stage have been found to be prognostic factors for lung LCNEC [5,7,9,10]. Surgical treatment is the primary treatment for stage I–III LCNEC patients [6,7,11]; however, the LCNEC subtype has a higher risk of tumor recurrence after surgery, even in stage I patients, and prevention of tumor recurrence by adjuvant chemotherapy after surgery is important [12–15]. The optimal chemotherapy regimen remains unclear in this population, as does the effect of local treatment, including thoracic radiotherapy and prophylactic cranial irradiation (PCI) [16–18].
Due to its low incidence and a lack of large randomized clinical studies, prognostic factors and survival in lung LCNEC remain controversial. The purpose of this study was to investigate the clinicopathologic characteristics, prognostic factors, and treatment outcomes in patients with lung LCNEC using data from the Surveillance, Epidemiology, and End-Results (SEER) dataset.
Material and Methods
Patients
The National Cancer Institute SEER program is a cancer registry that records data on cancer incidence, patient demographics, clinicopathologic details, first course of treatment, and outcomes, covering approximately 28% of the United States population. We obtained permission to access the dataset (authorization code: 13425-Nov2017). We searched the SEER database for patients diagnosed with lung LCNEC between 2000 and 2013 [19]. The histology of lung LCNEC is coded as 8013/3 in SEER, according to the International Classification of Disease for Oncology, 3rd edition. Our study did not require approval from our institutional review board, as patient information from the SEER dataset is anonymous.
Variables
The following variables were identified from the dataset: age at diagnosis, race/ethnicity, grade, tumor stage, nodal stage, surgical procedures, chemotherapy, radiotherapy, and marital status. The primary outcomes were lung cancer-specific survival (LCSS) and overall survival (OS).
Statistical analysis
Age-specific incidence rates were evaluated using the US standard population for the year 2000, and were presented as per 100 000 person-years. The chi-square test or Fisher’s exact probability tests were used to compare patients’ demographic, clinicopathologic, and treatment variables between treatment arms. Survival curves and rates were estimated using the Kaplan-Meier method and compared using log-rank test. Univariate and multivariate analyses were performed using the Cox proportional hazards model. Multivariate Cox regression models were performed using the backward Wald method. Statistical analyses were performed using SPSS, version 22 (IBM Corporation, NY, USA) and SEER*Stat software (version 8.3.5; http://seer.cancer.gov/seerstat/). All P values were 2-sided, with P values less than 0.05 considered statistically significant.
Results
Incidence rate
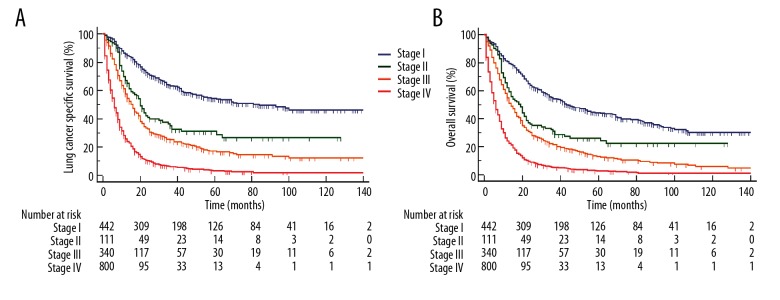
The total age-adjusted incidence rate for lung LCNEC was 0.3/100 000 for the period 2000–2013, and incidence in males and females was 0.4/100 000 and 0.3/100 000, respectively. Incidence increased during the study period (Figure 1), and only 2 patients were diagnosed in 2000. A total of 105 and 232 patients were diagnosed in 2001 and 2013, respectively.
Figure 1.
Age-adjusted morbidity of lung large cell neuroendocrine carcinoma from the surveillance, epidemiology, and end-results database, 2000–2013.
Patient characteristics
A total of 2097 patients were identified. The median age was 65 years (range, 18–94 years). Most patients were male (n=1155, 55.1%), white (n=1747, 83.3%), married (n=1130, 53.9%), poorly/undifferentiated tumors (n=1004, 47.9%), and stage III–IV disease (n=1140, 54.3%) (Table 1).
Table 1.
Patient characteristics.
| Variable | n (%) | No surgery (%) | Surgery (%) | P* |
|---|---|---|---|---|
| Age (years) | ||||
| <65 | 1045 (49.8) | 617 (48.8) | 428 (51.4) | 0.246 |
| ≥65 | 1052 (50.2) | 648 (51.2) | 404 (48.6) | |
| Sex | ||||
| Male | 1155 (55.1) | 710 (56.2) | 445 (53.5) | 0.243 |
| Female | 942 (44.9) | 555 (43.9) | 387 (46.5) | |
| Race/ethnicity | ||||
| White | 1747 (83.3) | 1040 (82.2) | 707 (85.0) | 0.226 |
| Black | 260 (12.4) | 169 (13.4) | 91 (10.9) | |
| Other | 90 (4.3) | 56 (4.4) | 34 (4.1) | |
| Marital status | ||||
| Married | 1130 (53.9) | 650 (51.4) | 480 (57.7) | 0.016 |
| Single | 898 (42.8) | 573 (45.3) | 325 (39.1) | |
| Unknown | 69 (3.3) | 42 (3.3) | 27 (3.2) | |
| T stage | ||||
| T1 | 416 (19.8) | 145 (11.5) | 271 (32.6) | <0.001 |
| T2 | 573 (27.3) | 276 (21.8) | 297 (35.7) | |
| T3 | 94 (4.5) | 52 (4.1) | 42 (5.0) | |
| T4 | 476 (22.7) | 419 (33.1) | 57 (6.9) | |
| Tx | 538 (25.7) | 373 (29.5) | 165 (19.8) | |
| N stage | ||||
| N0 | 715 (34.1) | 241 (19.1) | 474 (57.0) | <0.001 |
| N1 | 164 (7.8) | 66 (5.2) | 98 (11.8) | |
| N2 | 560 (26.7) | 468 (37.0) | 92 (11.1) | |
| N3 | 229 (10.9) | 220 (17.4) | 9 (1.1) | |
| Nx | 429 (20.5) | 270 (21.3) | 159 (19.1) | |
| Stage | ||||
| I | 442 (21.1) | 392(47.1) | 50 (4.0) | <0.001 |
| II | 111 (5.3) | 98 (11.8) | 13 (1.0) | |
| III | 340 (16.2) | 111 (13.3) | 229 (18.1) | |
| IV | 800 (38.1) | 67 (8.1) | 733 (57.9) | |
| Unknown | 404 (19.3) | 164 (19.7) | 240 (19.0) | |
| Grade | ||||
| Well differentiated | 7 (0.3) | 5 (0.4) | 2 (0.2) | <0.001 |
| Moderately differentiated | 32 (1.5) | 10 (0.8) | 22 (2.6) | |
| Poorly differentiated | 756 (36.1) | 323 (25.5) | 433 (52.0) | |
| Undifferentiated | 248 (11.8) | 119 (9.4) | 129 (15.5) | |
| Unknown | 1054 (50.3) | 808 (63.9) | 246 (29.6) | |
| Chemotherapy | ||||
| No | 1140 (54.4) | 438 (34.6) | 519 (62.4) | <0.001 |
| Yes | 957 (45.6) | 827 (65.4) | 313 (37.6) | |
| Radiotherapy | ||||
| No | 1240 (59.1) | 574 (45.4) | 666 (80.0) | <0.001 |
| Yes | 857(40.9) | 691 (54.6) | 166 (20.0) | |
N – nodal; T – tumor.
Indicates chi-square test or Fisher’s exact probability tests to compare the patient characteristics by treatment arms.
Treatment
Across the entire cohort, most patients received surgical treatment (n=832, 60.3%). The percentages of patients receiving surgery at stage I, II, III, and IV disease were 88.7%, 88.3%, 32.6%, and 8.4%, respectively. Married patients and those at early tumor and nodal stage were more likely to receive surgical treatment (Table 1). A total of 1140 (54.4%) patients received chemotherapy, with the percentages receiving chemotherapy at stages I, II, III, and IV disease 23.8%, 62.2%, 71.5%, and 65.4%, respectively. In addition, 40.9% of patients received radiotherapy, with 11.3%, 26.1%, 54.7%, and 52.5% receiving radiotherapy at stages I, II, III, and IV disease, respectively.
Prognostic analysis
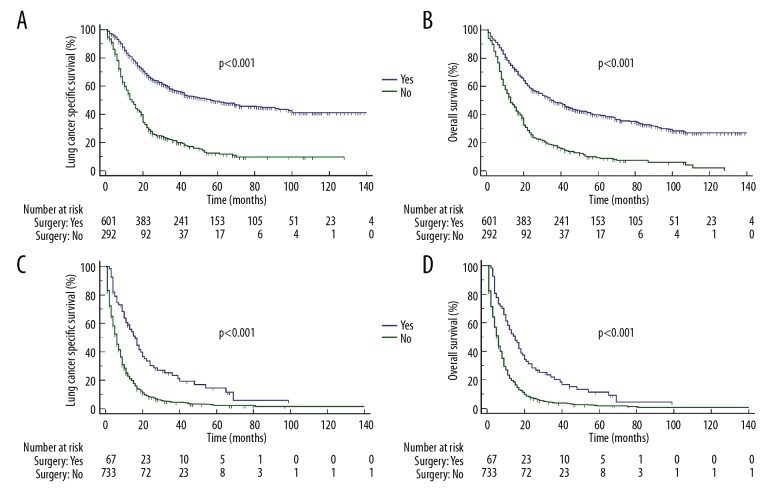
The median follow-up time of these patients was 24.4 months (range, 1–179 months). Five-year LCSS and OS were 20.7% and 16.7%, respectively, with a median LCSS and OS of 12 months and 11 months, respectively. Five-year LCSS was 53.8%, 28.8%, 16.6%, and 3.2% (P<0.001; Figure 2A) and 5-year OS was 43.9%, 24.1%, 12.7%, and 2.6% (P<0.001; Figure 2B) in stages I, II, III, and IV disease, respectively. The median LCSS was 84, 20, 16, and 6 months in patients with stages I, II, III, and IV disease, respectively. In addition, the median OS was 44, 19, 14, and 6 months in stages I, II, III, and IV disease, respectively.
Figure 2.
Survival outcomes of patients with lung large cell neuroendocrine carcinoma by tumor stage (A – lung cancer-specific survival; B – overall survival).
In univariate analysis, aged ≥65 years, male sex, advanced tumor and nodal stage, not undergoing surgery, not undergoing radiotherapy, and not undergoing chemotherapy were associated with poor LCSS and OS (Tables 2, 3). The results of multivariate analysis indicated that advanced tumor stage, advanced nodal stage, not undergoing surgery, and not undergoing chemotherapy were independent adverse indicators of LCSS and OS (Tables 2, 3). In addition, patients aged ≥65 years and male sex were also the independent adverse indicators related to OS.
Table 2.
Univariate and multivariate Cox proportional hazard regression analyses of prognostic analyses for lung cancer-specific survival of lung large cell neuroendocrine carcinoma patients.
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (years) | ||||
| <65 | 1 | 1 | ||
| ≥65 | 1.170 (1.060–1.292) | 0.002 | 1.098 (0.993–1.214) | 0.069 |
| Sex | ||||
| Male | 1 | 1 | ||
| Female | 0.854 (0.773–0.943) | 0.002 | 0.906 (0.819–1.001) | 0.053 |
| Race/ethnicity | ||||
| White | 1 | – | ||
| Black | 1.084 (0.935–1.258) | 0.284 | – | – |
| Other | 1.037 (0.814–1.321) | 0.769 | – | – |
| Marital status | ||||
| Married | 1 | – | ||
| Singles | 1.063 (0.961–1.175) | 0.237 | – | – |
| Unknown | 0.870 (0.647–1.171) | 0.358 | – | – |
| T stage | ||||
| T1 | 1 | 1 | ||
| T2 | 1.276 (1.103–1.476) | 0.001 | 1.404 (1.193–1.652) | <0.001 |
| T3 | 1.751 (1.373–2.233) | <0.001 | 1.807 (1.397–2.338) | <0.001 |
| T4 | 2.677 (2.311–3.100) | <0.001 | 1.697 (1.428–2.016) | <0.001 |
| Tx | 1.732 (1.501–1.999) | <0.001 | 1.146 (0.922–1.424) | 0.220 |
| N stage | ||||
| N0 | 1 | 1 | ||
| N1 | 1.612 (1.335–1.946) | <0.001 | 1.743 (1.423–2.136) | <0.001 |
| N2 | 2.254 (1.992–2.551) | <0.001 | 1.561 (1.343–1.815) | <0.001 |
| N3 | 3.242 (2.759–3.811) | <0.001 | 2.004 (1.659–2.420) | <0.001 |
| Nx | 1.725 (1.511–1.969) | <0.001 | 1.683 (1.354–2.092) | <0.001 |
| Stage | ||||
| I | 1 | 1 | ||
| II | 2.023(1.539–2.661) | <0.001 | 1.875(1.336–2.630) | <0.001 |
| III | 2.837(2.350–3.426) | <0.001 | 1.429(1.099–1.857) | 0.080 |
| IV | 6.181(5.239–7.293) | <0.001 | 2.916(2.304–3.689) | <0.001 |
| Unknown | 2.987(2.492–3.581) | <0.001 | 1.790(1.277–2.508) | 0.001 |
| Grade | ||||
| Well differentiated | 1 | – | ||
| Moderately differentiated | 0.639 (0.258–1.583) | 0.333 | – | – |
| Poorly differentiated | 0.727 (0.325–1.627) | 0.438 | – | – |
| Undifferentiated | 0.785 (0.348–1.772) | 0.56 | – | – |
| Unknown | 1.217 (0.545–2.717) | 0.631 | – | – |
| Surgery | ||||
| No | 1 | 1 | ||
| Yes | 0.266 (0.237–0.298) | <0.001 | 0.286 (0.249–0.329) | <0.001 |
| Chemotherapy | ||||
| No | 1 | 1 | ||
| Yes | 0.820 (0.741–0.907) | <0.001 | 0.630 (0.561–0.708) | <0.001 |
| Radiotherapy | ||||
| No | 1 | 1 | ||
| Yes | 0.662 (0.599–0.732) | <0.001 | 0.946 (0.847–1.057) | 0.326 |
CI – confidence interval; HR – hazard ratio; N – nodal; T – tumor.
Table 3.
Univariate and multivariate Cox proportional hazard regression analyses of prognostic analyses for overall survival of lung large-cell neuroendocrine carcinoma patients.
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (years) | ||||
| <65 | 1 | 1 | ||
| ≥65 | 1.245 (1.134–1.366) | <0.001 | 1.162 (1.057–1.278) | 0.002 |
| Sex | ||||
| Male | 1 | 1 | ||
| Female | 0.842 (0.767–0.925) | <0.001 | 0.879 (0.800–0.966) | 0.008 |
| Race/ethnicity | ||||
| White | 1 | – | ||
| Black | 1.067 (0.927–1.229) | 0.366 | – | – |
| Other | 1.068 (0.853–1.337) | 0.568 | – | – |
| Marital status | ||||
| Married | 1 | – | ||
| Singles | 1.071 (0.974–1.177) | 0.157 | – | – |
| Unknown | 0.919 (0.699–1.209) | 0.547 | – | – |
| T stage | ||||
| T1 | 1 | 1 | ||
| T2 | 1.276 (1.103–1.476) | 0.001 | 1.244 (1.074–1.442) | 0.004 |
| T3 | 1.751 (1.373–2.233) | <0.001 | 1.521 (1.188–1.946) | 0.001 |
| T4 | 2.677 (2.311–3.100) | <0.001 | 1.544 (1.317–1.810) | <0.001 |
| Tx | 1.732 (1.501–1.999) | <0.001 | 1.027 (0.837–1.260) | 0.801 |
| N stage | ||||
| N0 | 1 | 1 | ||
| N1 | 1.612 (1.335–1.946) | <0.001 | 1.635 (1.350–1.980) | <0.001 |
| N2 | 2.254 (1.992–2.551) | <0.001 | 1.511 (1.312–1.741) | <0.001 |
| N3 | 3.242 (2.759–3.811) | <0.001 | 1.915 (1.598–2.294) | <0.001 |
| Nx | 1.725 (1.511–1.969) | <0.001 | 1.612 (1.310–1.983) | <0.001 |
| Stage | ||||
| I | 1 | 1 | ||
| II | 1.708 (1.332–2.191) | <0.001 | 1.706 (1.244–2.339) | 0.001 |
| III | 2.368 (2.004–2.799) | <0.001 | 1.355 (1.066–1.722) | 0.013 |
| IV | 4.821 (4.167–5.577) | <0.001 | 2.602 (2.099–3.225) | <0.001 |
| Unknown | 2.411 (2.054–2.829) | <0.001 | 1.580 (1.149–2.171) | 0.005 |
| Grade | ||||
| Well di fferentiated | 1 | – | ||
| Moderately differentiated | 0.624 (0.269–1.447) | 0.272 | – | – |
| Poorly differentiated | 0.728 (0.346–1.535) | 0.405 | – | – |
| Undifferentiated | 0.797 (0.375–1.693) | 0.555 | – | – |
| Unknown | 1.165 (0.554–2.450) | 0.688 | – | – |
| Surgery | ||||
| No | 1 | 1 | ||
| Yes | 0.312 (0.282–0.347) | <0.001 | 0.328 (0.289–0.374) | <0.001 |
| Chemotherapy | ||||
| No | 1 | 1 | ||
| Yes | 0.898 (0.817–0.987) | 0.025 | 0.615 (0.552–0.687) | <0.001 |
| Radiotherapy | ||||
| No | 1 | 1 | ||
| Yes | 0.696 (0.634–0.765) | <0.001 | 0.965 (0.868–1.073) | 0.506 |
CI – confidence interval; HR – hazard ratio; N – nodal; T – tumor.
Subgroup analysis
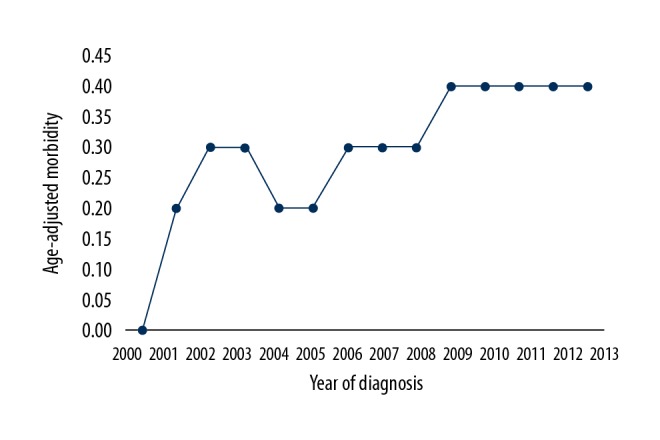
We further analyzed the effect of surgery at different cancer stages, adjusted by age at diagnosis, race/ethnicity, grade, tumor stage, nodal stage, chemotherapy radiotherapy, and marital status. We found that undergoing surgery was independently related to longer LCSS and OS, compared with not undergoing surgery, regardless of tumor stage. Patients with stage IV disease who had surgery also had longer LCSS (hazard ratio [HR] 0.440, 95% confidence interval [CI] 0.331–0.587, P<0.001) and OS (HR 0.456, 95% CI 0.346–0.600, P<0.001) than those not treated with surgery (Table 4) (Figure 3A–3D).
Table 4.
Adjusted hazard ratio for the effect of surgery on lung cancer-specific survival and overall survival of lung large cell neuroendocrine carcinoma patients by tumor stage.
| Variables | LCSS | OS | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Stage I | ||||
| No-surgery | 1 | 1 | ||
| Surgery | 0.245 (0.144–0.418) | <0.001 | 0.280 (0.174–0.448) | <0.001 |
| Stage II | ||||
| No-surgery | 1 | 1 | ||
| Surgery | 0.670 (0.296–1.514) | <0.336 | 0.738 (0.347–1.572) | 0.432 |
| Stage III | ||||
| No-surgery | 1 | 1 | ||
| Surgery | 0.500 (0.355–0.702) | <0.001 | 0.590 (0.431–0.808) | <0.001 |
| Stage IV | ||||
| No-surgery | 1 | 1 | ||
| Surgery | 0.440 (0.331–0.587) | <0.001 | 0.456 (0.346–0.600) | <0.001 |
CI – confidence interval; HR – hazard ratio; LCSS – lung cancer-specific survival; OS – overall survival.
Figure 3.
Survival outcomes of patients with surgery and without surgery in lung large cell neuroendocrine carcinoma patients (lung cancer-specific survival: A – stage I–III; C – stage IV. Overall survival: B – stage I–III; D – stage IV).
Discussion
For this study, we used a population-based approach to assess the clinicopathologic characteristics and prognosis of lung LCNEC patients and investigate their survival outcomes according to stage and treatment strategy. Our study indicates that although lung LCNEC subtype is related to a dismal prognosis, surgery can improve outcomes, even in patients with stage IV disease. However, the effect of radiotherapy in this population remains unclear.
The incidence rate of lung LCNEC increased during the study period, a similar finding to those of Derks et al. [20] and Varlotto et al. [21]. In our study, only 2 patients were diagnosed in 2000, and the incidence of lung LCNEC was significantly increased in 2001 and gradually increased over subsequent years. The reason for this increasing incidence of lung LCNEC is unknown, although a growing awareness of lung LCNEC may be the main reason for the perceived increase in incidence. In addition, the fact that pathologists began using the histologic diagnostic designation for lung LCNEC more often than before may be another potential reason for the increasing incidence of lung LCNEC after 2001.
Similar to results for non-small cell lung carcinoma (NSCLC), the optimal local treatment for stage I–III operable lung LCNEC was surgery. However, survival of lung LCNEC was significantly poorer than for NSCLC [5–9]. Patients treated with surgery had better survival outcomes than those who did not receive surgical treatment, regardless of tumor stage. Our findings raise the question of whether surgical treatment is necessary for this subtype at advanced stage.
Currently, systemic therapy remains the main treatment in stage IV disease. However, stage IV lung cancer is a group with highly heterogeneity. A study by Shin et al. [22] showed a significant difference in median survival time in patients with various metastatic (M) stages, with median survival times of 22.5 months, 17.8 months, and 13.6 months in patients with M1a, M1b, and M1c disease, respectively (P<0.001), indicating that treatment strategies may differ depending on M stage. Although the role of surgery in stage IV disease remains controversial, there have been several retrospective studies suggesting that the addition of surgery in selected NSCLC patients improves survival outcomes, especially for patients with small tumor burden and oligometastasis [23–28]. A prospective randomized clinical trial has shown that in stage IV disease, patients with less than 3 metastatic lesions who received first-line systemic therapy, surgical treatment, or local radiotherapy had significantly longer progression-free survival (PFS) compared with patients treated with maintenance therapy (11.9 months vs. 3.9 months, P=0.005) [29]. We also found in our study that surgical treatment is an important part of comprehensive treatment in stage IV lung LCNEC. However, which subgroups can benefit from local treatment needs further investigation [30].
Several previous studies have found a higher risk of tumor recurrence after surgery in lung LCNEC than in the NSCLC subtype, even in stage I patients [7–9,31], and that adjuvant chemotherapy is also associated with better survival outcomes in this disease [13–15]. Our study also demonstrated better outcomes for patients who received chemotherapy. However, the standard chemotherapy regimen in lung LCNEC remains controversial, and the use of different chemotherapy regimens can result in different outcomes. Whether the chemotherapy regimen for lung LCECC should refer to the regimens for NSCLC or SCLC is unclear. A prior study from Varlotto et al. [21] showed similarities in the clinical and pathologic features of lung LCNEC and large cell lung cancer, and they recommended a similar chemotherapy regimen for lung LCNEC to that of NSCLC. However, other studies have recommended that the chemotherapy regimens for SCLC are more appropriate to the lung LCNEC subtype [32–34]. A retrospective study by Sun et al. [35] compared the clinical effects of NSCLC and SCLC chemotherapy regimens used in advanced-stage lung LCNEC, finding that SCLC chemotherapy regimens are more suitable for lung LCNEC patients, although the difference was not statistically significant.
Due to a lack of prospective reports, the role of thoracic radiotherapy in lung LCNEC is also unclear. A study by Arsela et al. [16] of stage III–IV inoperable patients treated with cisplatin – etoposide-based chemotherapy with/without thoracic radiotherapy and PCI indicated that patients receiving thoracic radiotherapy had longer PFS (12.5 months vs. 5 months, P=0.02) and median OS time (28.3 months vs. 5 months, P=0.004) than those without thoracic radiotherapy. Metro et al. [36] found that prognosis was worse for patients with advanced inoperable lung LCNEC than that of SCLC patients, even after chemotherapy and thoracic radiotherapy. Our study showed that undergoing radiotherapy was not an independent prognostic factor in lung LCNEC patients, suggesting that the role of thoracic radiotherapy and PCI in lung LCNEC patients needs further investigation.
Several notable limitations in this study should be acknowledged. First, there is inherent bias in any retrospective study. Second, the reasons for the choice of different treatment strategies for patients were unknown. Therefore, several confounding factors cannot be ruled out. Third, the SEER program does not include detailed information about chemotherapy or radiotherapy, or the sequence of surgery and chemotherapy. Moreover, it has been shown that there are high rates of under-reporting for receipt of chemotherapy and radiotherapy in the SEER program. In addition, the decision-making regarding surgical treatment in stage IV patients was unclear. It was hypothesized that patients undergoing surgical treatment had a better starting point (by being operable) at time of diagnosis, and that patients who had not undergone surgery were inoperable in the first place, so their tumor characteristics were worse or their fitness and status did not permit surgery. Finally, patterns of tumor recurrence and treatment history after disease recurrence were not recorded in the SEER database. The primary strength of our study is that it involves one of the largest population-based cohorts of patients with lung LCNEC, spanning 18 US registries, which allowed us to minimize the selection and surveillance biases observed with single institutions.
Conclusions
LCNEC is a rare lung cancer subtype with a dismal prognosis and increased incidence in recent years. The primary surgery may be associated with better outcomes in stage IV disease. More studies are needed to investigate the optimal treatment strategy for LCNEC.
Footnotes
Source of support: Departmental sources
Conflicts of interest
None.
References
- 1.Fasano M, Della Corte CM, Papaccio F, et al. Pulmonary large-cell neuroendocrine carcinoma: From epidemiology to therapy. J Thorac Oncol. 2015;10:1133–41. doi: 10.1097/JTO.0000000000000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Battafarano RJ, Fernandez FG, Ritter J, et al. Large cell neuroendocrine carcinoma: An aggressive form of non-small cell lung cancer. J Thorac Cardiovasc Surg. 2005;130:166–72. doi: 10.1016/j.jtcvs.2005.02.064. [DOI] [PubMed] [Google Scholar]
- 3.Brambilla E. [Classification of broncho-pulmonary cancers (WHO 1999)]. Rev Mal Respir. 2002;19:455–66. [in French] [PubMed] [Google Scholar]
- 4.Travis WD, Brambilla E, Nicholson AG, et al. WHO Panel. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol. 2015;10:1243–60. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 5.Travis WD, Linnoila RI, Tsokos MG, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15:529–53. doi: 10.1097/00000478-199106000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Eichhorn F, Dienemann H, Muley T, et al. Predictors of survival after operation among patients with large cell neuroendocrine carcinoma of the lung. Ann Thorac Surg. 2015;99:983–89. doi: 10.1016/j.athoracsur.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Sakurai H, Asamura H. Large-cell neuroendocrine carcinoma of the lung: Surgical management. Thorac Surg Clin. 2014;24:305–11. doi: 10.1016/j.thorsurg.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Fournel L, Falcoz PE, Alifano M, et al. Surgical management of pulmonary large cell neuroendocrine carcinomas: A 10-year experience. Eur J Cardiothorac Surg. 2013;43:111–14. doi: 10.1093/ejcts/ezs174. [DOI] [PubMed] [Google Scholar]
- 9.Matsuura N, Nakashima N, Igai H, et al. [Prognosis of surgically treated large cell neuroendocrine carcinoma]. Kyobu Geka. 2011;64:187–90. [in Japanese] [PubMed] [Google Scholar]
- 10.Tanaka Y, Ogawa H, Uchino K, et al. Immunohistochemical studies of pulmonary large cell neuroendocrine carcinoma: A possible association between staining patterns with neuroendocrine markers and tumor response to chemotherapy. J Thorac Cardiovasc Surg. 2013;145:839–46. doi: 10.1016/j.jtcvs.2012.03.036. [DOI] [PubMed] [Google Scholar]
- 11.Kinoshita T, Yoshida J, Ishii G, et al. The differences of biological behavior based on the clinicopathological data between resectable large-cell neuroendocrine carcinoma and small-cell lung carcinoma. Clin Lung Cancer. 2013;14:535–40. doi: 10.1016/j.cllc.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Paci M, Cavazza A, Annessi V, et al. Large cell neuroendocrine carcinoma of the lung: A 10-year clinicopathologic retrospective study. Ann Thorac Surg. 2004;77:1163–71. doi: 10.1016/j.athoracsur.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 13.Filosso PL, Rena O, Guerrera F, et al. ESTS NETs-WG Steering Committee. Clinical management of atypical carcinoid and large-cell neuroendocrine carcinoma: A multicentre study on behalf of the European Association of Thoracic Surgeons (ESTS) Neuroendocrine Tumours of the Lung Working Groupdagger. Eur J Cardiothorac Surg. 2015;48:55–64. doi: 10.1093/ejcts/ezu404. [DOI] [PubMed] [Google Scholar]
- 14.Abedallaa N, Tremblay L, Baey C, et al. Effect of chemotherapy in patients with resected small-cell or large-cell neuroendocrine carcinoma. J Thorac Oncol. 2012;7:1179–83. doi: 10.1097/JTO.0b013e3182572ead. [DOI] [PubMed] [Google Scholar]
- 15.Saji H, Tsuboi M, Matsubayashi J, et al. Clinical response of large cell neuroendocrine carcinoma of the lung to perioperative adjuvant chemotherapy. Anticancer Drugs. 2010;21:89–93. doi: 10.1097/CAD.0b013e328330fd79. [DOI] [PubMed] [Google Scholar]
- 16.Prelaj A, Rebuzzi SE, Del Bene G, et al. Evaluation of the efficacy of cisplatin-etoposide and the role of thoracic radiotherapy and prophylactic cranial irradiation in LCNEC. ERJ Open Res. 2017;3 doi: 10.1183/23120541.00128-2016. pii: 00128-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rieber J, Schmitt J, Warth A, et al. Outcome and prognostic factors of multimodal therapy for pulmonary large-cell neuroendocrine carcinomas. Eur J Med Res. 2015;20:64. doi: 10.1186/s40001-015-0158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naidoo J, Santos-Zabala ML, Iyriboz T, et al. Large cell neuroendocrine carcinoma of the lung: clinico-pathologic features, treatment, and outcomes. Clin Lung Cancer. 2016;17:e121–29. doi: 10.1016/j.cllc.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Surveillance, Epidemiology, and End-Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence – SEER 18 Regs Custom Data (with additional treatment fields), Nov 2017 Sub (1973–2015 varying) – Linked To County Attributes – Total U.S., 1969–2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2018, based on the November 2017 submission
- 20.Derks JL, Hendriks LE, Buikhuisen WA, et al. Clinical features of large cell neuroendocrine carcinoma: A population-based overview. Eur Respir J. 2016;47:615–24. doi: 10.1183/13993003.00618-2015. [DOI] [PubMed] [Google Scholar]
- 21.Varlotto JM, Medford-Davis LN, Recht A, et al. Should large cell neuroendocrine lung carcinoma be classified and treated as a small cell lung cancer or with other large cell carcinomas? J Thorac Oncol. 2011;6:1050–58. doi: 10.1097/JTO.0b013e318217b6f8. [DOI] [PubMed] [Google Scholar]
- 22.Shin J, Keam B, Kim M, et al. Prognostic impact of newly proposed m descriptors in TNM classification of non-small cell lung cancer. J Thorac Oncol. 2017;12:520–528. doi: 10.1016/j.jtho.2016.11.2216. [DOI] [PubMed] [Google Scholar]
- 23.Abdel-Rahman O. Outcomes of surgery as part of the management of metastatic non-small-cell lung cancer: A surveillance, epidemiology and end results database analysis. Cancer Invest. 2018;36:238–45. doi: 10.1080/07357907.2018.1466895. [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi M, Edagawa M, Suzuki Y, et al. Pulmonary resection for synchronous M1b-c stage IV non-small cell lung cancer patients. Ann Thorac Surg. 2017;10:1594–1599. doi: 10.1016/j.athoracsur.2016.08.098. [DOI] [PubMed] [Google Scholar]
- 25.David EA, Clark JM, Cooke DT, et al. The role of thoracic surgery in the therapeutic management of metastatic non-small cell lung cancer. J Thorac Oncol. 2017;12:1636–45. doi: 10.1016/j.jtho.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shen H, Cao Y, Li X, et al. Surgical intervention improves survival for metastatic non-small cell lung cancer patients. Medicine (Baltimore) 2016;95:e3800. doi: 10.1097/MD.0000000000003800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.David EA, Canter RJ, Chen Y, et al. Surgical management of advanced non-small cell lung cancer is decreasing but is associated with improved survival. Ann Thorac Surg. 2016;102:1101–9. doi: 10.1016/j.athoracsur.2016.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu T, Liu H, Wang G, et al. Survival of M1a non-small cell lung cancer treated surgically: A retrospective single-center study. Thorac Cardiovasc Surg. 2015;63:577–82. doi: 10.1055/s-0034-1396666. [DOI] [PubMed] [Google Scholar]
- 29.Gomez DR, Blumenschein GR, Jr, Lee JJ, et al. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: A multicentre, randomised, controlled, phase 2 study. Lancet Oncol. 2016;17:1672–82. doi: 10.1016/S1470-2045(16)30532-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.David EA, Andersen SW, Beckett LA, et al. A model to predict the use of surgical resection for advanced-stage non-small cell lung cancer patients. Ann Thorac Surg. 2017;104:1665–72. doi: 10.1016/j.athoracsur.2017.05.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iyoda A, Hiroshima K, Moriya Y, et al. Prognostic impact of large cell neuroendocrine histology in patients with pathologic stage Ia pulmonary non-small cell carcinoma. J Thorac Cardiovasc Surg. 2006;132:312–15. doi: 10.1016/j.jtcvs.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 32.Le Treut J, Sault MC, Lena H, et al. Multicentre phase II study of cisplatin-etoposide chemotherapy for advanced large-cell neuroendocrine lung carcinoma: The GFPC 0302 study. Ann Oncol. 2013;24:1548–52. doi: 10.1093/annonc/mdt009. [DOI] [PubMed] [Google Scholar]
- 33.Kenmotsu H, Niho S, Ito T, et al. A pilot study of adjuvant chemotherapy with irinotecan and cisplatin for completely resected high-grade pulmonary neuroendocrine carcinoma (large cell neuroendocrine carcinoma and small cell lung cancer) Lung Cancer. 2014;84:254–58. doi: 10.1016/j.lungcan.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Eba J, Kenmotsu H, Tsuboi M, et al. Lung Cancer Surgical Study Group of the Japan Clinical Oncology Group; Lung Cancer Study Group of the Japan Clinical Oncology Group. A Phase III trial comparing irinotecan and cisplatin with etoposide and cisplatin in adjuvant chemotherapy for completely resected pulmonary high-grade neuroendocrine carcinoma (JCOG1205/1206) Jpn J Clin Oncol. 2014;44:379–82. doi: 10.1093/jjco/hyt233. [DOI] [PubMed] [Google Scholar]
- 35.Sun JM, Ahn MJ, Ahn JS, et al. Chemotherapy for pulmonary large cell neuroendocrine carcinoma: Similar to that for small cell lung cancer or non-small cell lung cancer? Lung Cancer. 2012;77:365–70. doi: 10.1016/j.lungcan.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 36.Metro G, Ricciuti B, Chiari R, et al. Survival outcomes and incidence of brain recurrence in high-grade neuroendocrine carcinomas of the lung: Implications for clinical practice. Lung Cancer. 2016;95:82–87. doi: 10.1016/j.lungcan.2016.03.006. [DOI] [PubMed] [Google Scholar]