Key Points
Question
What are the visual outcomes and rate of complications 1 year after pediatric cataract surgery?
Findings
In this cohort study of 880 children who underwent cataract surgery, amblyopia was diagnosed in half of children who underwent lensectomy, which was performed with intraocular lens implantation in 60.2% of eyes, resulting in normal visual acuity in about 1 in 3 eyes. The rate of unexpected complications was low, but nearly 1 in 5 eyes required a subsequent surgery, most often for visual axis obscuration.
Meaning
These findings suggest that frequent monitoring and management of refractive error, amblyopia, and visual axis clouding should be anticipated during the first year after surgery.
Abstract
Importance
Cataract is an important cause of visual impairment in children. Outcomes reported from a large clinical disease-specific registry can provide real-world estimates of visual outcomes and rates of adverse events in clinical practice.
Objective
To describe visual acuity and refractive error outcomes, as well as rates of amblyopia, glaucoma, and additional eye surgery, during the first year after lensectomy in children.
Design, Setting, and Participants
A prospective observational study was conducted from June 18, 2012, to July 8, 2015, at 61 pediatric eye care practices among 880 children younger than 13 years at the time of lensectomy in at least 1 eye with follow-up within 15 months after surgery. Statistical analysis was performed from December 12, 2016, to December 14, 2018.
Exposures
Lensectomy with or without implantation of an intraocular lens.
Main Outcomes and Measures
Visual acuity as well as rates of amblyopia, glaucoma, suspected glaucoma, and other intraocular surgery.
Results
Among the 880 children (432 girls and 448 boys; mean [SD] age at annual follow-up, 4.9 [3.8] years) in the study, lens surgery was bilateral in 362 (41.1%; 95% CI, 37.9%-44.4%) children and unilateral in 518 (58.9%; 95% CI, 55.6%-62.1%). An intraocular lens was implanted in 654 of 1132 eyes (60.2%; 95% CI, 57.0%-63.4% [proportions reported for eye-level outcomes account for the potential correlation induced by enrolling both eyes of some individuals; for participants who received bilateral surgery, these numbers will differ from the quotient of the number of cases divided by the total sample size]). Amblyopia was identified in 449 children (51.0%; 95% CI, 47.7%-54.3%). In children age 3 years or older, mean visual acuity was 0.30 logMAR (about 20/40) in 153 bilateral pseudophakic eyes, 0.49 logMAR (about 20/63) in 141 unilateral pseudophakic eyes, 0.47 logMAR (about 20/63) in 21 bilateral aphakic eyes, and 0.61 logMAR (about 20/80) in 17 unilateral aphakic eyes. Mean visual acuity improved with older age at surgery in eyes with bilateral pseudophakia by 0.2 logMAR line (99% CI, 0.02-0.4; P = .005) and by 0.3 logMAR line (99% CI, 0.04-0.60; P = .004) in eyes with unilateral pseudophakia. A new diagnosis of glaucoma or suspected glaucoma was made in 67 of 1064 eyes that did not have glaucoma prior to lensectomy (5.9%; 95% CI, 4.6%-7.7%); 36 of 273 eyes with bilateral aphakia (13.2%; 95% CI, 9.0%-19.0%), 5 of 308 eyes with bilateral pseudophakia (1.5%; 95% CI, 0.6%-4.2%), 14 of 178 eyes with unilateral aphakia (7.9%; 95% CI, 4.7%-12.8%), and 12 of 305 eyes with unilateral pseudophakia (3.9%; 95% CI, 2.2%-6.8%). Additional intraocular surgery, most commonly vitrectomy or membranectomy to clear the visual axis, was performed in 189 of 1132 eyes (17.0%; 95% CI, 14.8%-19.6%).
Conclusions and Relevance
Amblyopia was frequently observed during the first year after lensectomy in this cohort of children younger than 13 years. For children age 2 years or older at surgery visual acuity was typically less than normal for age and was worse with unilateral cataract. Management of visual axis obscuration was the most common complication requiring surgical intervention during the first year after surgery.
This cohort study describes visual acuity and refractive error outcomes, as well as rates of amblyopia, glaucoma, and additional eye surgery, during the first year after lensectomy in children younger than 13 years.
Introduction
Childhood cataract is uncommon in the developed world, but it is an important cause of visual impairment. Eyes that have undergone cataract surgery may develop amblyopia, secondary opacification of the visual axis, glaucoma, ametropia, anisometropia, strabismus, and retinal detachment; in addition, individuals who have undergone cataract surgery may need additional ocular surgery. Visual acuity (VA) outcomes and incidence of adverse events after cataract surgery have not, to our knowledge, been prospectively studied in a large cohort of children.
To understand current management and outcomes of cataract surgery in children, the Pediatric Eye Disease Investigator Group (PEDIG) developed a prospective registry to collect data on children from birth to less than 13 years of age undergoing lensectomy. A 2016 study reported the baseline findings and surgical approaches for 994 children who had lens surgery in 1266 eyes.1 In this report we describe outcomes and complications reported during the first year after surgery.
Methods
This study was conducted by PEDIG and was supported through a cooperative agreement with the National Eye Institute. An investigational device exemption (#G110149) was obtained from the US Food and Drug Administration because of the use of an intraocular lens (IOL) for an unapproved indication. The protocol and Health Insurance Portability and Accountability Act–compliant informed consent forms were approved by each site’s institutional review board. Children’s parent or guardian provided written consent.
Registry Data Collection
Between June 18, 2012, and July 8, 2015, 61 centers (57 in the United States, 3 in Canada, and 1 in the United Kingdom) prospectively enrolled children from birth to less than 13 years of age who had undergone lensectomy during the preceding 45 days. Surgery had been performed prior to consent and enrollment. There was no standardization of surgical approach. At enrollment, ophthalmic, systemic, and historical data were collected. Each year thereafter, data regarding medical history including optical correction, treatment, optotype VA (when available), refractive error, intraocular pressure, IOL centration, complications, and surgical procedures were collected from medical record reviews. Data for fellow eyes were included if they underwent surgery and follow-up data were available within 15 months after surgery. Adverse events and surgical procedures were included if they were reported within 15 months after eye surgery. Visual acuity and refractive error were included if they were reported between 9 and 15 months after eye surgery, hereafter referred to as the 1-year outcome.
Study-Specified Definitions
Participants were classified as having unilateral or bilateral lens surgery. Bilateral surgery was defined as surgery in both eyes within 15 months after enrollment or by history of a lensectomy in the fellow eye prior to study enrollment.
An eye was considered to have glaucoma if the investigator indicated that glaucoma was present, the eye received glaucoma medication after surgery, or additional surgery was performed for glaucoma. Eyes were considered to have suspected glaucoma if the investigator indicated this diagnosis on the case report form. Eyes were classified as amblyopic if the investigator indicated that amblyopia was present in the eye or treatment other than refractive correction was prescribed for amblyopia. Eyes were classified as having normal VA if VA was 20/50 or better at age 3 years, 20/40 or better at age 4 years, 20/32 or better at age 5 or 6 years, and 20/25 or better at age 7 years or older.2,3
Statistical Analysis
Statistical analysis was performed from December 12, 2016, to December 14, 2018. To account for correlation between eyes of participants who contributed both eyes, logistic regression models were used to compute the log odds (and CIs) of having ocular characteristics. The inverse logit function was used to calculate the proportion of eyes with the ocular characteristic and the corresponding CIs. Linear mixed models controlling for correlation between eyes were used to evaluate associations between age at initial lensectomy and VA at 1 year, and age 1 year after initial lensectomy and change in spherical equivalent refractive error (SER) from the first postoperative visit (within 45 days after lensectomy) to 1 year, controlling for SER at the first postoperative visit.
Analyses were performed separately for participants with unilateral aphakia, bilateral aphakia, unilateral pseudophakia, and bilateral pseudophakia. Snellen VA measurements were converted to logMAR lines for analysis; VA worse than 20/800 was assigned 1.70 logMAR (1 line worse than 20/800).
All statistical tests were 2-sided. When evaluating differences, P ≤ .01 was considered statistically significant, and corresponding 99% CIs were calculated. When estimating parameters, 95% CIs were calculated. Analyses were performed in SAS, version 9.4 (SAS Institute Inc).
Results
Of 1266 eyes of 994 children enrolled in the registry, 1132 eyes of 880 children had outcomes data reported within the year after surgery; 362 children (41.1%; 95% CI, 37.9%-44.4%) had bilateral surgery, 518 children (58.9%; 95% CI, 55.6%-62.1%) had unilateral surgery, and 448 (50.9%) were male (Table 1). An IOL was implanted in 654 of 1132 eyes (60.2%; 95% CI, 57.0%-63.4% [proportions reported for eye-level outcomes account for the potential correlation induced by enrolling both eyes of some individuals; for participants who received bilateral surgery, these numbers will differ from the quotient of the number of cases divided by the total sample size]). Median follow-up was 10.4 months (range, 1-15 months; interquartile range, 8.1-11.7 months) and median age at the time of the outcome examination was 4.2 years (range, 0.2-14.0 years). Of 347 children with aphakia, 169 (48.7%; 95% CI, 43.4%-54.0%) were managed with contact lenses alone, 82 (23.6%; 95% CI, 19.2%-28.1%) with glasses alone, and 85 (24.5%; 95% CI, 20.0%-29.0%) with both glasses and contact lenses.
Table 1. Characteristics of Children With Outcomes Data 1 Year After Surgery Stratified by Laterality of Surgery.
| Characteristic | Children, No. (%) | ||||
|---|---|---|---|---|---|
| Bilateral Surgery | Unilateral Surgery | All Participants (N = 880) | |||
| Aphakic Eyes (n = 157) | Pseudophakic Eyes (n = 205) | Aphakic Eyes (n = 190) | Pseudophakic Eyes (n = 328) | ||
| Male sex | 79 (50.3) | 103 (50.2) | 80 (42.1) | 186 (56.7) | 448 (50.9) |
| Race/ethnicity | |||||
| American Indian or Alaskan native | 0 | 1 (0.5) | 2 (1.1) | 2 (0.6) | 5 (0.6) |
| Asian | 7 (4.5) | 9 (4.4) | 3 (1.6) | 13 (4.0) | 32 (3.6) |
| Black or African American | 21 (13.4) | 28 (13.7) | 17 (8.9) | 49 (14.9) | 115 (13.1) |
| Hispanic | 22 (14.0) | 35 (17.1) | 37 (19.5) | 56 (17.1) | 150 (17.0) |
| White | 99 (63.1) | 120 (58.5) | 117 (61.6) | 187 (57.0) | 523 (59.4) |
| >1 Race | 5 (3.2) | 6 (2.9) | 11 (5.8) | 12 (3.7) | 34 (3.9) |
| Unknown or not reported | 3 (1.9) | 6 (2.9) | 3 (1.6) | 9 (2.7) | 21 (2.4) |
| Age at annual visit | |||||
| <6 mo | 1 (0.6) | 0 | 5 (2.6) | 0 | 6 (0.7) |
| 6 mo to <1 y | 41 (26.1) | 0 | 43 (22.6) | 0 | 84 (9.5) |
| 1 to <4 y | 99 (63.1) | 52 (25.4) | 114 (60.0) | 72 (22.0) | 337 (38.3) |
| 4 to <7 y | 8 (5.1) | 71 (34.6) | 9 (4.7) | 104 (31.7) | 192 (21.8) |
| 7-14 y | 8 (5.1) | 82 (40.0) | 19 (10.0) | 152 (46.3) | 261 (29.7) |
| Age, mean (SD), y | 1.9 (2.2) | 6.5 (3.2) | 2.3 (2.8) | 6.8 (3.4) | 4.9 (3.8) |
| Age, median (range), y | 1.1 (0.4-12.8) | 6.0 (1.1-13.9) | 1.2 (0.2-14.0) | 6.5 (1.0-14.0) | 4.2 (0.2-14.0) |
| Optical correction in participants with aphakia (n = 347) | |||||
| Contact lenses only | 58 (36.9) | NA | 111 (58.4) | NA | 169/347 (48.7) |
| Glasses only | 56 (35.7) | NA | 26 (13.7) | NA | 82/347 (23.6) |
| Both glasses and contact lenses | 40 (25.5) | NA | 45 (23.7) | NA | 85/347 (24.5) |
| None or unknown | 3 (1.9) | NA | 8 (4.2) | NA | 11/347 (3.2) |
Abbreviation: NA, not applicable.
Visual Acuity
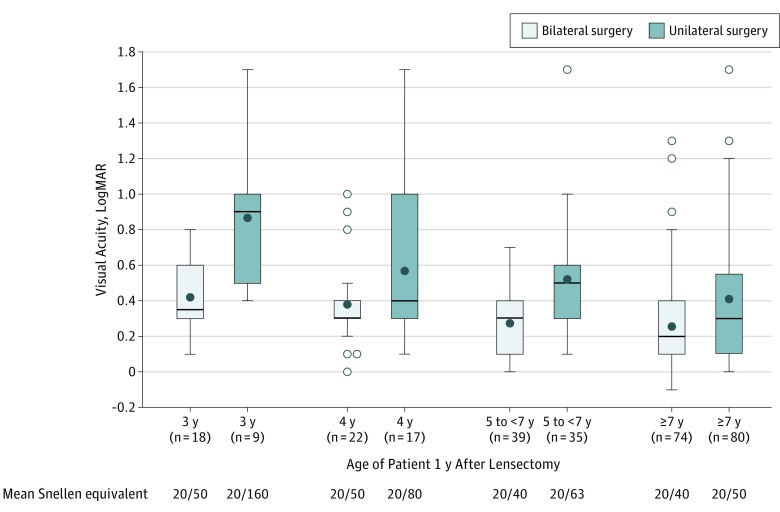
Quantitative VA data were available for 332 of 619 eyes (53.6%) of children age 3 years or older at follow-up. Mean age at VA test was 7.6 years. An IOL was implanted in 294 eyes (88.6%; 95% CI, 84.8%-91.8%). Visual acuity in pseudophakic eyes ranged from 20/16 to worse than 20/800, with 107 of 294 eyes (35.5%; 95% CI 30.0%-41.5%) achieving age-normal values (Figure 1). Visual acuity of 20/50 or better was reported in 125 of 153 (81.8%; 95% CI, 74.0%-87.7%) bilateral pseudophakic eyes and 73 of 141 (51.8%; 95% CI, 43.6%-59.9%) unilateral pseudophakic eyes. Visual acuity worse than 20/800 was reported in 4 eyes. In children age 3 years or older, mean VA was 0.30 logMAR (about 20/40) in 153 bilateral pseudophakic eyes and 0.49 logMAR (about 20/63) in 141 unilateral pseudophakic eyes. Mean VA was better with older age at surgery in bilateral pseudophakic eyes by 0.2 logMAR line (99% CI, 0.02-0.4; P = .005) and unilateral pseudophakic eyes by 0.3 logMAR line (99% CI, 0.04-0.60; P = .004) per additional year of age.
Figure 1. Visual Acuity in Pseudophakic Eyes 1 Year After Lensectomy Stratified by Age 1 Year After Lensectomy and by Laterality.
Data are for 294 pseudophakic eyes of participants aged 3 years or older who could undergo quantitative visual acuity testing. Visual acuity was not reported for or could not be performed for 263 eyes. Visual acuity was better with increasing age at surgery for both unilateral and bilateral cases. The top of each box represents the 75th percentile of the data and the bottom of each box represents the 25th percentile of the data. Group medians are represented by the horizontal line in each box and group means by filled circles. The bars extending above and below each box represent 1.5 times the interquartile range (difference between the 75th and 25th percentiles), or the maximum (or minimum) observed value within the range if not as extreme as the calculated value. Open circles represent statistical outliers.
Thirty-eight aphakic eyes had VA reported, ranging from 20/20 to worse than 20/800, with 16 eyes (42.2%; 95% CI, 27.5%-58.5%) achieving age-normal values. Mean VA was 0.47 logMAR (about 20/63) in 21 bilateral aphakic eyes and 0.61 logMAR (about 20/80) in 17 unilateral aphakic eyes. The association between mean VA and age at surgery was not statistically significant in bilateral or unilateral aphakic eyes. (This analysis 1 year after surgery does not include children younger than 2 years at the time of surgery).
Amblyopia
Amblyopia was identified in 449 (51.0%; 95% CI, 47.7%-54.3%) of 880 participants: 44 of 157 children with bilateral aphakia (28.0%; 95% CI, 21.0%-35.1%), 45 of 205 children with bilateral pseudophakia (22.0%; 95% CI, 16.3%-27.6%), 159 of 190 children with unilateral aphakia (83.7%; 95% CI, 78.4%-88.9%), and 201 of 328 children with unilateral pseudophakia (61.3%; 95% CI, 56.0%-66.6%). Median age at time of lensectomy among children with amblyopia was 1.7 years (mean, 2.8 years; range, 0.04-12.5 years), compared with 5.4 years (mean, 5.4 years; range, 0.07-13.0 years) for those without amblyopia. Treatment for amblyopia was reported in 412 participants (46.8%; 95% CI, 43.5%-50.1%): 36 of 157 children with bilateral aphakia (22.9%; 95% CI, 16.4%-29.5%), 31 of 205 children with bilateral pseudophakia (15.1%; 95% CI, 10.2%-20.0%), 158 of 190 children with unilateral aphakia (83.2%; 95% CI, 77.8%-88.5%), and 187 of 328 children with unilateral pseudophakia (57.0%; 95% CI, 51.7%-62.4%).
Refractive Error
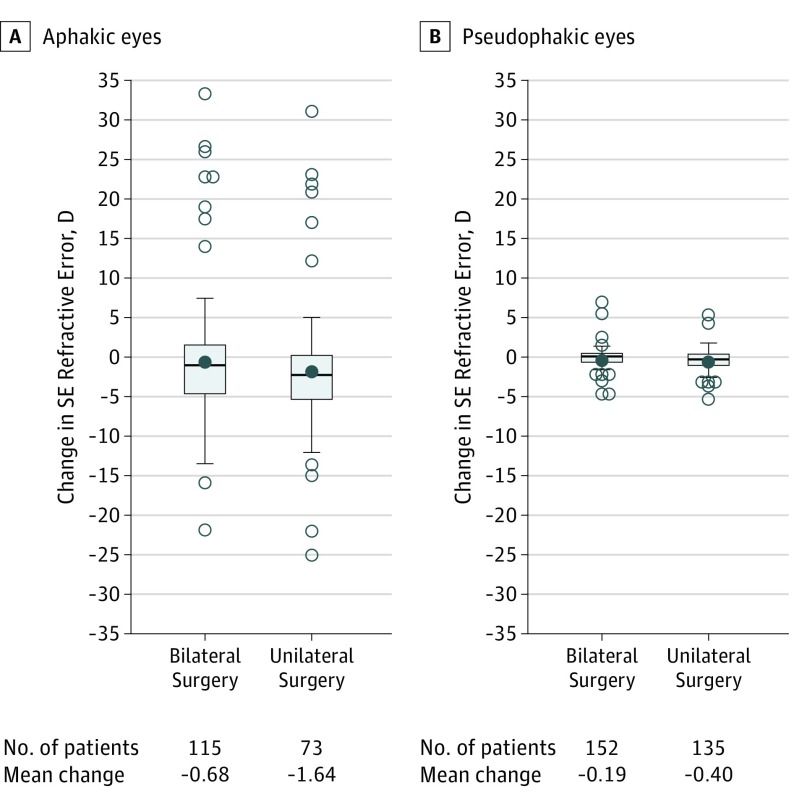
Data on refractive error were available for 522 eyes of 412 participants, after excluding 21 participants who received a secondary IOL. Change in SER from the first postoperative visit to 1 year was available for 475 eyes of 376 participants. Median SER at the 1-year outcome was 19.00 diopters (D) (n = 127; range, 1.25-35.00 D) in children with bilateral aphakia, 1.31 D (n = 166; range, −3.50 to 8.50 D) in children with bilateral pseudophakia, 16.88 D (n = 84; range, 0.00-32.00 D) in children with unilateral aphakia, and 0.88 D (n = 145; range, −10.25 to 16.00 D) in children with unilateral pseudophakia. A myopic shift in SER was seen during the first year after surgery, with a mean change of −0.68 D in children with bilateral aphakia, −0.19 D in children with bilateral pseudophakia, −1.64 D in children with unilateral aphakia, and −0.40 D in children with unilateral pseudophakia (Figure 2). In bilateral aphakic eyes, the mean 1-year change in SER was smaller by 1.33 D (P = .003) with each additional year of age; however, no association was observed in bilateral pseudophakic, unilateral aphakic, or unilateral pseudophakic eyes. After 1 year, pseudophakic eyes on average remained slightly hyperopic (about 1.30 D), although 144 of 577 eyes (25.6%; 95% CI, 20.9%-31.0%) were already myopic.
Figure 2. Change in Refractive Error From First Postoperative Visit to 1 Year After Lensectomy Stratified by Laterality of Surgery and Intraocular Lens Implantation.
Negative values indicate a myopic shift. Little change was seen in bilateral pseudophakic eyes (−0.19 diopters [D]) and unilateral pseudophakic eyes (−0.40 D), while modest loss of hyperopia was seen in bilateral aphakic eyes (−0.68 D) and unilateral aphakic eyes (−1.64 D). The top of each box represents the 75th percentile of the data and the bottom of each box represents the 25th percentile of the data. Group medians are represented by the horizontal line in each box and group means by filled circles. The bars extending above and below each box represent 1.5 times the interquartile range (difference between the 75th and 25th percentiles), or the maximum (or minimum) observed value within the range if not as extreme as the calculated value. Open circles represent statistical outliers. SE indicates spherical equivalent.
Glaucoma and Other Ocular Complications
Intraocular pressure was reported for 889 of 1132 eyes (78.5%), with a mean (SD) of 15 (5) mm Hg (median, 15 mm Hg; range, 5-45 mm Hg). Elevated intraocular pressure (≥21 mm Hg) was found in 69 of 889 eyes (7.3%; 95% CI, 5.6%-9.4%): 32 of 231 bilateral aphakic eyes (14.5%; 95% CI, 9.7%-21.0%), 13 of 254 bilateral pseudophakic eyes (4.5%; 95% CI, 2.3%-8.6%), 8 of 139 unilateral aphakic eyes (5.8%; 95% CI, 2.9%-11.1%), and 16 of 265 unilateral pseudophakic eyes (6.0%; 95% CI, 3.7%-9.6%).
A new diagnosis of glaucoma or suspected glaucoma (hereafter termed glaucoma adverse event) was identified in 67 of 1064 eyes that did not have glaucoma prior to lensectomy (5.9%; 95% CI, 4.6%-7.7%): 36 of 273 bilateral aphakic eyes (13.2%; 95% CI, 9.0%-19.0%), 5 of 308 bilateral pseudophakic eyes (1.5%; 95% CI 0.6%-4.2%), 14 of 178 unilateral aphakic eyes (7.9%; 95% CI, 4.7%-12.8%), and 12 of 305 unilateral pseudophakic eyes (3.9%; 95% CI, 2.2%-6.8%) (Table 2). Glaucoma adverse events were reported for 9 of 115 eyes with abnormalities of the anterior segment (7.8%; 95% CI, 2.9%-12.7%), 4 of 78 eyes with abnormalities of the posterior segment (5.1%; 95% CI, 0.2%-10.0%), 7 of 39 eyes with abnormalities of both the anterior and posterior segments (18.0%; 95% CI, 5.9%-30.0%), and 47 of 832 eyes with no abnormalities (5.7%; 95% CI, 4.1%-7.2%). Glaucoma surgery was performed in 25 of 1132 eyes (2.0%; 95% CI, 1.3%-3.1%), most often in aphakic eyes (Table 3).
Table 2. Ocular Complications Stratified by Placement of Intraocular Lens.
| Complication | Eyes, No. (%)a | ||||
|---|---|---|---|---|---|
| Bilateral Surgery | Unilateral Surgery | All Eyes (N = 1132) | |||
| Aphakic Eyes (n = 286) | Pseudophakic Eyes (n = 328) | Aphakic Eyes (n = 192) | Pseudophakic Eyes (n = 326) | ||
| Amblyopia | 34 (11.5) | 27 (8.2) | 160 (83.3) | 200 (61.3) | 421 (42.8) |
| Corneal calcification | 0 | 0 | 4 (2.1) | 6 (1.8) | 10 (0.9) |
| Endophthalmitis | 1 (0.3) | 0 | 0 | 0 | 1 (0.1) |
| Preexisting glaucoma | 13 (4.4) | 20 (5.7) | 14 (7.3) | 21 (6.4) | 68 (5.9) |
| Glaucomab | 32 (11.7) | 3 (1.0) | 11 (5.7) | 8 (2.5) | 54 (4.7) |
| Suspected glaucomab | 4 (1.5) | 2 (0.5) | 3 (1.6) | 4 (1.2) | 13 (1.2) |
| Intraocular inflammation | 1 (0.3) | 1 (0.3) | 3 (1.6) | 8 (2.5) | 13 (1.1) |
| Iris abnormalities | 11 (3.9) | 4 (1.2) | 2 (1.0) | 3 (0.9) | 20 (1.6) |
| Iris capsular synechiae | 4 (1.4) | 4 (1.2) | 6 (3.1) | 4 (1.2) | 18 (1.6) |
| Peripheral anterior synechiae | 4 (1.5) | 2 (0.5) | 5 (2.6) | 2 (0.6) | 13 (1.1) |
| Retinal detachment | 0 | 3 (0.7) | 2 (1.0) | 3 (0.9) | 8 (0.7) |
| Visual axis opacification | 27 (9.3) | 53 (16.0) | 19 (9.9) | 69 (21.2) | 168 (15.1) |
| Other | 18 (6.2) | 16 (5.0) | 12 (6.3) | 10 (3.1) | 56 (4.9) |
| No complications reported | 179 (62.4) | 221 (67.7) | 19 (9.9) | 74 (22.7) | 493 (38.8) |
Proportions reported for eye-level outcomes are adjusted for correlation induced by enrolling both eyes of some individuals. For the bilateral surgery group, the proportions may differ from the number of cases divided by the total sample size.
New diagnosis of glaucoma or suspected glaucoma after lens surgery. Results for glaucoma and suspected glaucoma reported for the 1064 eyes for which glaucoma was not present at enrollment.
Table 3. Additional Intraocular Surgery Stratified by Implantation of Intraocular Lens.
| Surgery | Eyes, No. (%)a | ||||
|---|---|---|---|---|---|
| Bilateral Surgery | Unilateral Surgery | All Eyes (N = 1132) | |||
| Aphakic Eyes (n = 286) | Pseudophakic Eyes (n = 328) | Aphakic Eyes (n = 192) | Pseudophakic Eyes (n = 326) | ||
| Intraocular surgery | 48 (16.5) | 39 (12.1) | 40 (20.8) | 62 (19.0) | 189 (17.0) |
| Glaucoma surgery | 16 (5.6) | 1 (0.3) | 7 (3.6) | 1 (0.3) | 25 (2.0) |
| Secondary intraocular lens implantation | 7 (2.5) | 1 (0.3) | 14 (7.3) | 0 | 22 (2.0) |
| Retinal detachment repair | 0 | 2 (0.6) | 1 (0.5) | 2 (0.6) | 5 (0.4) |
| Clear visual axis opacification | 27 (9.3) | 37 (11.7) | 18 (9.4) | 55 (16.9) | 137 (12.4) |
| Other | 6 (2.1) | 2 (0.6) | 9 (4.7) | 8 (2.5) | 25 (2.2) |
Proportions reported for eye-level outcomes are adjusted for correlation induced by enrolling both eyes of some individuals. For the bilateral surgery group, the proportions may differ from the number of cases divided by the total sample size.
Other ocular complications developing within 1 year after lensectomy included retinal detachment in 8 of 1132 eyes (0.7%; 95% CI, 0.3%-1.5%), endophthalmitis in 1 of 1132 eyes (0.1%; 95% CI, 0.0%-0.6%) (which occurred 9 months after the lensectomy), and visual axis opacification in 168 of 1132 eyes (15.1%; 95% CI, 13.0%-17.5%) (Table 2). The IOL remained centered in 621 of 654 pseudophakic eyes (95.3% CI, 93.2%-96.8%), while mild subluxation (optic useable) was reported in 5 of 654 eyes (0.8%; 95% CI, 0.3%-1.8%). One IOL was sufficiently dislocated that an IOL exchange was performed. Intraocular centration was not reported for 28 eyes.
Additional intraocular surgery (including glaucoma surgery) was performed in 189 of 1132 eyes (17.0%; 95% CI, 14.8%-19.6%) eyes (Table 3). Surgery to clear the visual axis was the most common additional surgery, performed in 137 of 1132 eyes (12.4%; 95% CI, 10.4%-14.7%). Membranectomy was performed in 57 of 137 eyes (42.5%; 95% CI, 34.0%-51.5%), a laser capsulotomy in 76 of 137 eyes (54.2%; 95% CI, 45.2%-62.9%), and both procedures in 3 of 137 eyes (2.2%; 95% CI, 0.7%-6.6%). The procedure was not reported for 1 eye. The mean age for membranectomy was 1.8 years (range, 0.2-11.1 years), while the mean age for capsulotomy was 7.6 years (range, 0.2-13.7 years). Among children age 2 years or younger at the time of initial lens surgery, additional surgery to clear the visual axis was performed in 58 of 507 eyes (11.6%; 95% CI, 8.9%-15.0%): 26 of 255 bilateral aphakic eyes (10.2%; 95% CI, 6.6%-15.5%), 6 of 43 bilateral pseudophakic eyes (13.8%; 95% CI, 5.3%-31.5%), 16 of 161 unilateral aphakic eyes (9.9%; 95% CI, 6.2%-15.6%), and 10 of 48 unilateral pseudophakic eyes (20.8%; 95% CI, 11.6%-34.6%). For pseudophakic eyes that had anterior vitrectomy or capsulotomy during the primary cataract surgery, 35 of 441 eyes (8.2%; 95% CI, 5.9%-11.4%) required surgery to clear the visual axis.
Twenty-one aphakic eyes underwent secondary IOL implantation during this period. Twenty-six children (3.0%; 95% CI, 1.8%-4.1%) underwent surgery for strabismus.
Discussion
The PEDIG cataract surgery registry was designed to prospectively collect data for 5 years on outcomes and adverse events associated with cataract surgery in children in the developed world younger than 13 years. Although the interventions in this study were not randomized, a large prospective registry provides point estimates of outcomes and adverse events that can be used to inform clinical practice, to benchmark individual practitioner outcomes, and judge change in those outcomes over time, as well as provide pilot data for development of clinical trials. We included sites and investigators throughout the United States, Canada, and the United Kingdom in academic and private practice, so the outcomes should be representative of clinical outcomes for childhood cataract surgery in the developed world.
There were no unexpected adverse events. Significant complications within 1 year of pediatric lensectomy were unusual but included new glaucoma and glaucoma suspect (5.9%) and retinal detachment (0.7%). Additional intraocular surgery during the first year after pediatric lensectomy was performed in 17.0% of eyes, most often to clear the visual axis by laser capsulotomy or membranectomy.
Of pseudophakic eyes, slightly more than half had VA of 20/50 or better. Visual acuity outcomes in pseudophakic eyes were better with older age at surgery and with bilateral compared with unilateral surgery. Thirty-eight aphakic eyes had VA reported, ranging from 20/20 to worse than 20/800 with 16 eyes (42.2%; 95% CI, 27.5%-58.5%) achieving age-normal values. Mean VA was 0.47 logMAR (about 20/63) in 21 bilateral aphakic eyes and 0.61 logMAR (about 20/80) in 17 unilateral aphakic eyes. Analysis of VA outcomes for infants and toddlers who underwent surgery before age 2 years are planned when these participants become old enough to undergo quantitative VA testing.
Amblyopia was diagnosed in just over half of the children and amblyopia treatment was the most common postsurgical intervention after prescription of glasses and contact lenses. As expected, amblyopia was most common with unilateral cataract. The rate was highest with unilateral aphakia (83.7%) and lowest with bilateral pseudophakia (22.0%). The participants with unilateral aphakia were generally very young at surgery, while those with bilateral pseudophakia were generally older at surgery.
Accurately anticipating the change in SER from hyperopia toward emmetropia during childhood and adolescence is important when choosing an IOL for implantation. After 1 year, pseudophakic eyes on average remained slightly hyperopic (about 1.30 D), although 144 of 577 eyes (25.6%) were already myopic. The pseudophakic eyes, both unilateral and bilateral, showed essentially no loss of hyperopia during the first postoperative year. A low rate of myopic shift has been found to be characteristic of pseudophakic eyes in young humans and other primates.4,5 Aphakic eyes (generally the younger patients in this cohort) experienced moderate reductions in hyperopia (mean change of −0.68 D for bilateral aphakia and −1.64 D for unilateral aphakia) in the first year after surgery. Insufficient numbers of older children with aphakia were enrolled to explore the age effect in these eyes; however, longitudinal analyses are anticipated with future follow-up.
Glaucoma is a concern after pediatric lensectomy. A new diagnosis of a glaucoma adverse event was made in 5.9% of eyes in the registry, more often in aphakic eyes than in pseudophakic eyes. These findings should be interpreted in light of 2 selection biases making the IOL appear protective. First, young age is a key risk factor for glaucoma and younger children typically did not have an IOL implanted.6,7 Second, anterior segment abnormalities are a risk factor for postoperative glaucoma and would often cause the surgeon to avoid IOL implantation.
When preparing for lens surgery, parents may ask if their child will need additional eye surgery. The most common intraocular surgery performed in the first year after lens surgery was to clear the visual axis in 12.4% of all enrolled eyes. The rate of additional surgery to clear the visual axis was also 11.6% for children age 2 years or younger at surgery. In contrast, the British Isles Congenital Cataract Interest Group investigators performed an operation in the first year after lens surgery to clear the visual axis in 94 of 350 eyes (26.9%), most often in eyes with an IOL.8 The Infant Aphakia Treatment Study investigators also reported a need to clear the visual axis in 40 of 114 participants (35.1%) who had undergone lensectomy between 1 and 6 months of age, most often in the IOL group.9 The lower rate found in this PEDIG registry may reflect the infrequent use of IOLs in the first year of life by PEDIG investigators, perhaps influenced by reports from these 2 research groups that cautioned about IOL implantation in the first year of life.
Strengths and Limitations
Strengths of our study include its large size, wide age range of children included, bilateral and unilateral cases of aphakia and pseudophakia, multiple ocular conditions, and prospective collection of data. Important limitations include loss to follow-up as families move and our lack of standardized VA measurement because of the wide age range included. Visual acuity outcome data are limited to older children who could undergo the testing. Visual acuity outcomes may change as younger children at surgery are able to complete VA testing. In addition, the rates of glaucoma and visual axis opacification are expected to increase with length of follow-up. An additional limitation is that surgical techniques and postoperative management was at investigator discretion, and thus represents real-world experience, rather than outcomes following a particular consensus protocol.
Conclusions
Lens surgery in children was often associated with good VA, although the mean VA was less than normal. Amblyopia occurred in 51.0% of children, but the rate of other adverse events was low. Management of visual axis obscuration was the most common reason for a second surgery. Myopic shift was minimal with the placement of an IOL in the first postoperative year. This finding, if it persists through longer follow-up, will affect the outcomes and could require adjustment of guidelines for IOL power selection. The frequency of these outcomes suggests the need for follow-up care. To explore longer-term outcomes for these children we are collecting outcomes data for 5 years after surgery.
References
- 1.Repka MX, Dean TW, Lazar EL, et al. ; Pediatric Eye Disease Investigator Group . Cataract surgery in children from birth to less than 13 years of age. Ophthalmology. 2016;123(12):2462-2473. doi: 10.1016/j.ophtha.2016.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pan Y, Tarczy-Hornoch K, Cotter SA, et al. ; Multi-Ethnic Pediatric Eye Disease Study Group . Visual acuity norms in pre-school children: the Multi-Ethnic Pediatric Eye Disease Study. Optom Vis Sci. 2009;86(6):607-612. doi: 10.1097/OPX.0b013e3181a76e55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS. 2008;12(2):145-149. doi: 10.1016/j.jaapos.2007.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert SR, Fernandes A, Drews-Botsch C, Tigges M. Pseudophakia retards axial elongation in neonatal monkey eyes. Invest Ophthalmol Vis Sci. 1996;37(2):451-458. [PubMed] [Google Scholar]
- 5.McClatchey SK, Hofmeister EM. The optics of aphakic and pseudophakic eyes in childhood. Surv Ophthalmol. 2010;55(2):174-182. doi: 10.1016/j.survophthal.2009.07.001 [DOI] [PubMed] [Google Scholar]
- 6.Beck AD, Freedman SF, Lynn MJ, Bothun E, Neely DE, Lambert SR; Infant Aphakia Treatment Study Group . Glaucoma-related adverse events in the Infant Aphakia Treatment Study: 1-year results. Arch Ophthalmol. 2012;130(3):300-305. doi: 10.1001/archophthalmol.2011.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mataftsi A, Haidich AB, Kokkali S, et al. Postoperative glaucoma following infantile cataract surgery: an individual patient data meta-analysis. JAMA Ophthalmol. 2014;132(9):1059-1067. doi: 10.1001/jamaophthalmol.2014.1042 [DOI] [PubMed] [Google Scholar]
- 8.Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS; British Isles Congenital Cataract Interest Group . Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol. 2015;99(11):1471-1476. doi: 10.1136/bjophthalmol-2014-306394 [DOI] [PubMed] [Google Scholar]
- 9.Lambert SR, Buckley EG, Drews-Botsch C, et al. ; Infant Aphakia Treatment Study Group . A randomized clinical trial comparing contact lens with intraocular lens correction of monocular aphakia during infancy: grating acuity and adverse events at age 1 year. Arch Ophthalmol. 2010;128(7):810-818. doi: 10.1001/archophthalmol.2010.101 [DOI] [PMC free article] [PubMed] [Google Scholar]