Abstract
Importance
Complications that arise after treatment of mandible fractures can result in significant morbidity. Identifying modifiable risk factors associated with these complications is valuable in guiding clinical practice for improved patient outcomes.
Objective
To describe the risk factors associated with complications in patients undergoing treatment for mandible fracture.
Design, Setting, and Participants
A retrospective review was conducted of 137 patients presenting to a tertiary care, level 1 trauma center with mandible fractures between January 1, 2014, and January 1, 2017. Outcomes and demographic characteristics for patients with at least 3 weeks of follow-up were compared using multivariate logistic regression analysis.
Results
Of the 137 patients meeting inclusion criteria, there were 113 males (82.5%) and 24 females (17.5%), with a mean (SD) age at presentation of 32.3 (15.7) years. Median follow-up was 71 days (range, 22-1189 days). Postoperative complications were identified in 29 patients (21.2%); complications included wound dehiscence or surgical site infection (n = 17), bony nonunion (n = 5), and hardware exposure (n = 13). Complications were managed surgically in 19 patients and nonsurgically in 10 patients. On univariate analysis, the initial surgery was completed later (mean [SD], 5.9 [6.6] days after injury) in patients who developed complications than in those who did not (mean [SD], 3.8 [4.0] days). On multivariate analysis, complications were associated with increased time from injury to treatment (odds ratio [OR], 1.60; 95% CI, 1.02-2.53; P = .04), tobacco use (OR, 8.10; 95% CI, 1.26-52.00; P = .03), and dental extraction (OR, 93.00; 95% CI, 1.19 to >999.00; P = .04). Residence in the same city as the medical center was associated with fewer complications (OR, 0.08; 95% CI, 0.01-0.69; P = .02).
Conclusions and Relevance
In a 3-year review of mandible fractures managed at a single academic center, complications were associated with an increased time to treatment, tobacco use, dental extraction, and living farther from the treatment facility. On a systems level, the results of this study suggest that expediting intervention for mandible fractures may improve outcomes.
Level of Evidence
3.
This cohort study describes the risk factors associated with complications in patients undergoing treatment for mandible fracture.
Key Points
Question
What risk factors are associated with treatment complications in patients with traumatic mandible fractures?
Findings
In this cohort study, complications were associated with an increased time to treatment, tobacco use, dental extraction, and living farther from the treatment facility. These risk factors represent both patient-related and systems-level factors.
Meaning
Patient-related factors, such as tobacco use and need for dental extraction, negatively influence complication rates; on a systems level, the results of this study suggest that expediting intervention for mandible fractures may improve outcomes.
Introduction
Mandible fractures are one of the most common traumatic injuries of the head and neck, accounting for 36% to 70% of all facial fractures.1,2,3,4,5,6,7 Treatment for a mandible fracture ranges from nonoperative management (eg, soft diet) to closed reduction with maxillomandibular fixation to open reduction with internal fixation, depending on the characteristics of the fracture and the surgeon’s management preferences.8 Although the high prevalence of mandible fractures and the options for treatment are not new, we are now in an era in which evidence-based management algorithms are sought, casting a new focus on surgical outcomes and the patient and management factors that affect them.
Complications after mandible fracture treatment include quality-of-life issues such as numbness, malocclusion, pain with mastication, and poor wound healing. After surgical intervention, local wound complications can include wound dehiscence, surgical site infection, hardware extrusion or exposure, and bony malunion or nonunion. Prior studies have associated increased rates of complication with patient factors, such as smoking and delay in receiving medical care.9,10,11 The role of other factors, such as fracture characteristics (location, comminution, and number), antibiotic use and type, comorbid illness, and early surgical intervention, are controversial, particularly in studies in which lack of multivariate analysis creates difficulties in identifying independent and nonconfounded risk factors for complication.11,12,13,14,15 Furthermore, the wide variety in patient presentation, practice patterns, and poor follow-up and/or compliance have contributed additional challenges to studying the outcomes of mandible fracture management.16,17
The primary purpose of this study is to determine which factors (patient or systems-related) are associated with an increased risk of posttreatment complication in patients with a mandible fracture. We hypothesized that substance abuse, increased time from injury to surgical management, and more complex fracture patterns (eg, multiple and comminuted) would be associated with greater numbers of surgical site complications as measured by wound dehiscence or surgical site infection, hardware exposure, and bony nonunion. Our secondary aim is to determine the rate and type of intervention used to manage patients presenting with a complication from repair of a mandible fracture.
Methods
This single-center retrospective cohort study was conducted with patient data from January 1, 2014, through January 1, 2017. The study was performed at the University of California (UC) Davis Medical Center, a public, academic, tertiary care, level 1 trauma center situated between multiple rural, suburban, and urban communities in the Northern California region. University of California, Davis is 1 of 3 trauma centers in the greater Sacramento area, with a catchment area of more than 2 million people. This study was approved by the UC Davis Institutional Review Board. Patient consent was waived because the data were deidentified.
Patients in the UC Davis electronic health record were identified by queried search for all diagnoses of and procedural codes for mandible fracture (eTable in the Supplement). Patients were excluded if they had been treated elsewhere, had fewer than 3 weeks of follow-up, or had pathologic fractures (eg, caused by a tumor). For each encounter, data were abstracted from the electronic health record. Data collection included patient social and clinical demographic characteristics, insurance type, substance use (tobacco, alcohol, or other drug), mandible fracture characteristics, mechanism and date and time of injury, date and time of presentation to UC Davis, treatment date, time to treatment, treatment types, complication types, management of complications, and duration of follow-up. Data were extracted from the primary encounter narrative and all subsequent follow-up visits. Complications were grouped into the following 3 categories: wound dehiscence or surgical site infection, bony nonunion, and surgical hardware exposure.
Statistical Analysis
Deidentified data were tabulated in a Microsoft Excel (Microsoft Corp) spreadsheet, with demographic variables reported using mean, median, SD, range, and percentages for descriptive characteristics. Univariate comparisons between the groups with and without complications were performed using the Fisher exact test for categorical variables and Wilcoxon rank sum test for nonparametric continuous variables. The multivariate logistic regression model was fit incorporating variables that were significant on univariate analysis and of clinical relevance based on a priori knowledge. Categorical variables in which multiple responses were possible were simplified to binary responses for the multivariate model (eg, white race, private insurance, or Sacramento resident). All P values were from 2-sided tests, and results were deemed statistically significant at P < .05 for the purposes of this study. All statistical analyses were performed using SAS, version 9.4 (SAS Institute Inc).
Results
The queried search identified 224 potential patients, of which 137 met inclusion criteria. Patient characteristics are summarized in Table 1. More male patients (113 [82.5%]) were identified than female patients (24 [17.5%]). Mean (SD) patient age at presentation was 32.3 (15.7) years. Tobacco (60 of 129 [46.5%]), alcohol (60 of 126 [47.6%]), and other substance use (67 of 129 [51.9%]) were common among all patients. The median follow-up time after treatment was 71 days (range, 22-1189 days). The most common mechanisms of injury were assault (69 of 136 [50.7%]), falls (27 of 136 [19.9%]), and motor vehicle accidents (21 of 136 [15.4%]).
Table 1. Univariate Analysis of Patient Characteristics by Complications.
| Characteristic | Patients, No. (%)a | P Valueb | ||
|---|---|---|---|---|
| No Complications (n = 108) | Complications (n = 29) | All (N = 137) | ||
| Age, y | .049 | |||
| Mean (SD) | 31.3 (16.0) | 36.2 (13.8) | 32.3 (15.7) | |
| Median (range) | 28 (4-79) | 36 (7-62) | 30 (4-79) | |
| Sex | 108 | 29 | 137 | .78 |
| Male | 88 (81.5) | 25 (86.2) | 113 (82.5) | |
| Female | 20 (18.5) | 4 (13.8) | 24 (17.5) | |
| Ethnicity | (n = 106) | (n = 29) | (n = 135) | .65 |
| White | 54 (50.9) | 16 (55.2) | 70 (51.9) | |
| Black | 20 (18.9) | 4 (13.8) | 24 (17.8) | |
| Hispanic | 22 (20.8) | 5 (17.2) | 27 (20.0) | |
| Asian | 3 (2.8) | 0 | 3 (2.2) | |
| Other | 7 (6.6) | 4 (13.8) | 11 (8.2) | |
| Insurance | (n = 106) | (n = 28) | (n = 134) | >.99 |
| No | 3 (2.8) | 0 | 3 (2.2) | |
| Yes | 103 (97.2) | 28 (100) | 131 (97.8) | |
| City of residence | (n = 108) | (n = 29) | (N = 137) | .09 |
| Sacramento | 45 (41.7) | 8 (27.6) | 53 (38.7) | |
| Elk Grove | 2 (1.5) | 0 | 2 (1.5) | |
| Redding | 8 (7.4) | 0 | 8 (5.8) | |
| Davis | 5 (4.6) | 0 | 5 (3.7) | |
| Yuba City | 2 (1.9) | 2 (6.9) | 4 (2.9) | |
| Stockton | 2 (1.9) | 0 | 2 (1.5) | |
| Vacaville | 1 (0.9) | 0 | 1 (0.7) | |
| Folsom | 0 | 1 (3.5) | 1 (0.7) | |
| Other | 43 (39.8) | 18 (62.1) | 61 (44.5) | |
| Tobacco use | (n = 102) | (n = 27) | (n = 129) | .19 |
| No | 58 (56.9) | 11 (40.7) | 69 (53.5) | |
| Yes | 44 (43.1) | 16 (59.3) | 60 (46.5) | |
| Alcohol use | (n = 101) | (n = 25) | (n = 126) | .50 |
| No | 51 (50.5) | 15 (60.0) | 66 (52.4) | |
| Yes | 50 (49.5) | 10 (40.0) | 60 (47.6) | |
| Other substance use | (n = 101) | (n = 28) | (n = 129) | .83 |
| No | 48 (47.5) | 14 (50.0) | 62 (48.1) | |
| Yes | 53 (52.5) | 14 (50.0) | 67 (51.9) | |
| Employed | (n = 45) | (n = 12) | (n = 57) | .76 |
| No | 20 (44.4) | 6 (50.0) | 26 (45.6) | |
| Yes | 25 (55.6) | 6 (50.0) | 31 (54.4) | |
| Other known injuries | (n = 108) | (n = 29) | (N = 137) | .06 |
| No | 66 (61.1) | 12 (41.4) | 78 (56.9) | |
| Yes | 42 (38.9) | 17 (58.6) | 59 (43.1) | |
| Medical history | (n = 108) | (n = 29) | (N = 137) | .50 |
| No | 74 (68.5) | 22 (75.9) | 96 (70.1) | |
| Yes | 34 (31.5) | 7 (24.1) | 41 (29.9) | |
| Previous mandible fractures | (n = 108) | (n = 29) | (N = 137) | >.99 |
| No | 103 (95.4) | 28 (96.6) | 131 (95.6) | |
| Yes | 5 (4.6) | 1 (3.5) | 6 (4.4) | |
| Mechanism of mandible fracture | (n = 108) | (n = 28) | (n = 136) | .68 |
| Assault | 56 (51.9) | 13 (46.4) | 69 (50.7) | |
| MVC | 15 (13.9) | 6 (21.4) | 21 (15.4) | |
| GSW | 7 (6.5) | 2 (7.1) | 9 (6.6) | |
| Fall | 23 (21.3) | 4 (14.3) | 27 (19.9) | |
| Other | 7 (6.5) | 3 (10.7) | 10 (7.4) | |
| Fractures in the mandible, No. | (n = 108) | (n = 9) | (N = 137) | .82 |
| Single | 30 (27.8) | 7 (24.1) | 37 (27.0) | |
| Multiple | 78 (72.2) | 22 (75.9) | 100 (73.0) | |
| Comminution | (n = 103) | (n = 24) | (n = 127) | .82 |
| Simple | 43 (41.8) | 11 (45.8) | 54 (42.5) | |
| Comminuted | 60 (58.3) | 13 (54.2) | 73 (57.5) | |
| Displacement of segments | (n = 105) | (n = 26) | (n = 131) | .33 |
| None | 18 (17.1) | 4 (15.4) | 22 (16.8) | |
| Mild | 65 (61.9) | 13 (50.0) | 78 (59.5) | |
| Moderate | 16 (15.2) | 5 (19.2) | 21 (16.0) | |
| Severe | 6 (5.7) | 4 (15.4) | 10 (7.6) | |
| Location of fracture | (n = 108) | (n = 29) | (N = 137) | .30 |
| Symphyseal, body, or angle | 95 (88.0) | 28 (96.6) | 123 (89.8) | |
| Ramus, subcondylar, or condyle | 13 (12.0) | 1 (3.5) | 14 (10.2) | |
| Condition of dentition prior to injury | (n = 59) | (n = 17) | (n = 76) | .37 |
| Good | 35 (59.3) | 7 (41.2) | 42 (55.3) | |
| Poor | 18 (30.5) | 8 (47.1) | 26 (34.2) | |
| Edentulous | 6 (10.2) | 2 (11.8) | 8 (10.5) | |
| Teeth in fracture line | (n = 108) | (n = 29) | (N = 137) | >.99 |
| No | 43 (39.8) | 11 (37.9) | 54 (39.4) | |
| Yes | 65 (60.2) | 18 (62.1) | 83 (60.6) | |
| Fractured teeth | (n = 108) | (n = 29) | (N = 137) | .49 |
| No | 79 (73.2) | 19 (65.5) | 98 (71.5) | |
| Yes | 29 (26.9) | 10 (21.2) | 39 (28.5) | |
| Started antibiotics on admission | (n = 107) | (n = 29) | (n = 136) | >.99 |
| No | 29 (27.1) | 8 (27.6) | 37 (37.2) | |
| Yes | 78 (72.9) | 21 (72.4) | 99 (72.8) | |
| Started chlorhexidine on admission | (n = 106) | (n = 29) | (n = 135) | .48 |
| No | 30 (28.3) | 6 (20.7) | 36 (26.7) | |
| Yes | 76 (71.7) | 23 (79.3) | 99 (73.3) | |
| Soft diet | (n = 108) | (n = 29) | (N = 137) | .69 |
| No | 99 (91.7) | 28 (96.6) | 127 (92.7) | |
| Yes | 9 (8.3) | 1 (3.5) | 10 (7.3) | |
| Closed reduction | (n = 106) | (n = 29) | (n = 135) | .20 |
| No | 83 (78.3) | 26 (89.7) | 109 (80.7) | |
| Yes | 23 (21.7) | 3 (10.3) | 26 (19.3) | |
| ORIF | (n = 106) | (n = 29) | (n = 135) | .10 |
| No | 33 (31.1) | 4 (13.8) | 37 (27.4) | |
| Yes | 73 (68.9) | 25 (86.2) | 98 (72.6) | |
| Dental extraction | (n = 107) | (n = 29) | (n = 136) | .03 |
| No | 106 (99.1) | 26 (89.7) | 132 (97.1) | |
| Yes | 1 (0.9) | 3 (10.3) | 4 (2.9) | |
| Hours of injury prior to presentation | (n = 103) | (n = 26) | (n = 103) | .27 |
| Mean (SD) | 32.9 (76.2) | 50.2 (80.8) | 36.9 (78.0) | |
| Median (range) | 8 (1-600) | 11.5 (0.5-360) | 8 (0.5-600) | |
| Time between injury and surgery, d | (n = 98) | (n = 27) | (n = 125) | .04 |
| Mean (SD) | 3.8 (4.0) | 5.9 (6.6) | 4.2 (4.8) | |
| Median (range) | 2.1 (0.4-20) | 3.4 (0.8-30) | 64.0 (0.4-30) | |
| Postoperative antibiotics | (n = 82) | (n = 26) | (n = 106) | .59 |
| No | 19 (23.2) | 7 (29.2) | 26 (24.5) | |
| Yes | 63 (76.8) | 17 (70.8) | 80 (75.5) | |
| Duration of postoperative antibiotics, h | (n = 108) | (n = 28) | (n = 136) | .54 |
| Mean (SD) | 127.7 (197.9) | 120.3 (95.1) | 126.2 (181.2) | |
| Median (range) | 96 (0-1440) | 120 (0-336) | 120 (0-1440) | |
| Duration of follow-up, d | (n = 108) | (n = 29) | (N = 137) | .02 |
| Mean (SD) | 141.3 (160.5) | 260.3 (323.6) | 166.5 (210.2) | |
| Median (range) | 63.5 (22-704) | 110.0 (22-1189) | 71.0 (22-1189) | |
Abbreviations: GSW, gunshot wound; MVC, motor vehicle collision; ORIF, open reduction with internal fixation.
Data are presented as number (percentage) of patients unless otherwise indicated.
P values for continuous variables are from Wilcoxon rank sum tests and for categorical variables are from Fisher exact test.
Characteristics of Mandible Fractures
Fractures were dichotomized into 2 groups, with most occurring in the symphysis, body, and angle (123 [89.8%]) compared with the ramus, subcondylar, and condyle regions (14 [10.2%]) (Table 1). Most cases (100 [73.0%]) involved multiple concomitant fractures. There were more comminuted fractures (73 of 127 [57.5%]) than simple fractures (54 of 127 [42.5%]).
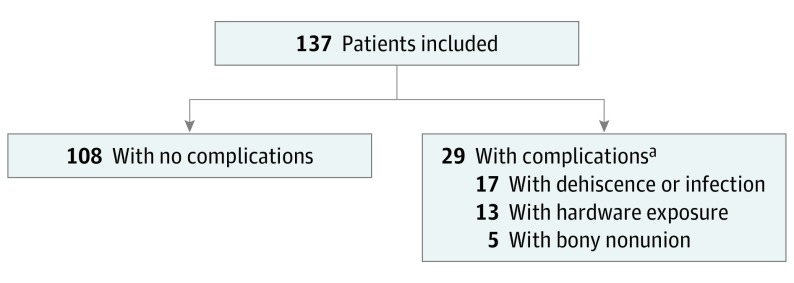
Characteristics of Complications
Posttreatment complications were identified in 29 patients (21.2%); complications included wound dehiscence or surgical site infection (17), bony nonunion (5), and hardware exposure (13) (Figure). Complications were managed surgically for 19 patients and nonsurgically for 10 patients. Nonsurgical treatment included oral antibiotics, wound care, and observation.
Figure. Flowchart of Complications.
aSubgroups are not mutually exclusive.
Univariate Analysis
Univariate analysis was performed to compare 2 cohorts of patients: those with a posttreatment complication and those without a complication. An increased time between injury and treatment was associated with more wound complications: the initial surgery was completed at a mean (SD) of 5.9 (6.6) days after injury in patients who developed complications compared with 3.8 (4.0) days in those without complications (P = .02). Dental extraction was also associated with more wound complications.
The mean (SD) age of the patients without complications was 31.3 (16.0) years compared with 36.2 (13.8) years in the group with complications (P = .049). As expected, patients with complications had a longer mean (SD) follow-up for aftercare (260.3 [323.6] days) than did those without complications (141.3 [160.5] days; P = .02). The likelihood of complications was not different based on mechanism of injury or fracture characteristics such as location, number, or comminution.
Multivariate Analysis
A logistic regression model was fit to test the hypothesis that patient-specific and fracture-specific risk factors were associated with increased complications after treatment of mandible fractures. After controlling for the risk factors included in Table 2, complications were associated with the following: increased time from injury to treatment (odds ratio [OR], 1.60; 95% CI, 1.02-2.53; P = .04), tobacco use (OR, 8.10; 95% CI, 1.26-52.00; P = .03), and dental extraction (OR, 93.00; 95% CI, 1.19 to >999.00; P = .04). Residence in the same city as the medical center was associated with fewer complications (OR, 0.08; 95% CI, 0.01-0.69; P = .02).
Table 2. Multivariate Logistic Regression Analysis of the Likelihood of Postoperative Complication by Patient Characteristic.
| Variable | OR (95% CI) | P Value |
|---|---|---|
| Age | 1.04 (0.98 to 1.10) | .22 |
| Sex | 0.46 (0.06 to 3.71) | .46 |
| White race | 3.75 (0.61 to 23.19) | .16 |
| Private insurance | 1.82 (0.36 to 9.09) | .47 |
| Sacramento resident | 0.08 (0.01 to 0.69) | .02 |
| Substance use | ||
| Tobacco | 8.09 (1.26 to 51.78) | .03 |
| Alcohol | 0.30 (0.05 to 1.84) | .12 |
| Other | 0.77 (0.13 to 4.45) | .77 |
| Gunshot wound | 0.47 (0.01 to 20.89) | .70 |
| Fracture characteristics | ||
| Multiple | 1.14 (0.16 to 8.35) | .89 |
| Comminuted | 0.84 (0.16 to 4.41) | .84 |
| Displaced (moderate to severe) | 1.38 (0.55 to 3.45) | .50 |
| Dentate area (symphyseal, body, or angle) | <0.01 (<0.01 to >999.00) | .96 |
| Fractured tooth | 0.94 (0.17 to 5.14) | .95 |
| Tooth in fracture | 0.18 (0.01 to 2.36) | .19 |
| Other known injury | 0.37 (0.05 to 3.06) | .36 |
| Management on admission | ||
| Chlorhexidine mouthwash | 1.94 (0.32 to 11.82) | .47 |
| Systemic antibiotics | 5.28 (0.39 to 71.46) | .21 |
| Fracture management | ||
| Soft diet only | <0.01 (<0.01 to >999.00) | .99 |
| Maxillomandibular fixation only | 0.01 (<0.01 to 1.28) | .06 |
| ORIF | 0.09 (<0.01 to 3.64) | .21 |
| Dental extraction | 92.69 (1.19 to >999.00) | .04 |
| Time to presentation, h | 0.98 (0.96 to 1.00) | .10 |
| Time to surgery, d | 1.60 (1.02 to 2.53) | .04 |
Abbreviations: OR, odds ratio; ORIF, open reduction with internal fixation.
Discussion
In this review of outcomes of treatment of mandible fracture, we found that both patient-related and systems-level factors may be associated with an increase in wound complications. Tobacco use and dental extraction were patient-related risk factors associated with increased rates of wound dehiscence, nonunion, and hardware exposure. An increased time from injury to treatment and residency outside the city of treatment were systems-level factors associated with more complications. When adjusting for other factors, there was no association between risk of complications and fracture complexity, drug or alcohol use, insurance status, or antibiotic administration.
In this report, we sought to identify risk factors associated with undesirable outcomes for patients and surgeons, leading to reoperation or prolonged disability from mandible fractures. Complications after treatment for mandible fracture occurred in 21.2% of patients, which is consistent with prior reports.9,10,12,14,15 Wound dehiscence and/or surgical site infection, bony nonunion, and hardware exposure were 3 consistent, objective findings in our retrospective review that best represented undesirable outcomes. Nonsurgical treatment with oral antibiotics and wound care was effective in nearly one-third of the patients (10 of 29 [34.5%]), while the remaining 19 of 29 patients (65.5%) required a return to the operating room for incision and drainage, hardware removal, or revision open reduction with internal fixation of fractures.
Similar to previous studies, patients in this cohort were predominately male, involved in an assault or motor vehicle collision, and experienced multiple concomitant mandible fractures, most commonly of the symphysis, body, and angle.9,18,19,20 After controlling for other variables, these risk factors were not associated with an increased risk of complications. Additional patient-related risk factors that failed to demonstrate an increased risk of complications in our study included alcohol and substance use (eg, methamphetamines), medical comorbidities (eg, diabetes or coronary artery disease), and employment status. The high prevalence of these risk factors contributes to poorer outcomes than the general population might experience. However, the pervasiveness of these medical conditions and social determinants of health in this study are generally representative of the population with mandible fractures.
Systems-Level Factors
In our study, we demonstrated an increased time to treatment as an independent risk factor for complications based on multivariate analysis. The mean (SD) time between injury and surgery was 3.8 (4.0) days in those without complications compared with 5.9 (6.6) days in those with complications (Table 1). This interval may represent a clinically important time difference to mitigate posttreatment complications.
There is a paucity of evidence to support a specific time during which a surgeon should aim to take a patient with a mandible fracture to surgery. In the maxillofacial trauma literature, time to surgery has been commonly examined, with mixed outcomes. In a retrospective review of more than 700 cases in Ukraine, Malanchuk and Kopchak11 found that an increased time to treatment was one of the risk factors associated with infection after repair of mandible fracture.
On the contrary, other studies found that time to treatment was not a risk factor for complications.9,10,12,21,22,23,24 The authors of these studies chose different time points to examine. Biller et al,21 Czerwinski et al,22 and Webb et al23 did not find an increase in complication rates when repair was delayed beyond 72 hours. Similarly, Lucca et al24 compared rates of complication when repair was performed within 48 hours and when it was performed after 48 hours and found no statistical significance between these groups. In these studies, however, no multivariate analysis was performed, allowing for potential confounding factors.
Increased time to treatment can encompass a number of different factors, including comorbid injuries taking precedence, surgeon or operating room availability (particularly for complex and time-consuming cases), and transfer from a community hospital. In our experience, the time to surgical repair is affected by operating room availability and necessary triage of the patient’s other possibly life-threatening traumatic injuries and overall clinical stability. However, in incorporating patient-related factors, such as fracture complexity and comorbid injuries, in our multivariate analysis, the potential for confounding effects of these individual characteristics was minimized, while time to treatment persisted as a factor significantly associated with posttreatment complication. One systems-level change that we are therefore seeking is to improve access to the operating room, with the goal of reducing time from injury to fracture fixation.
In our study, the proximity to our facility, which is a level 1 trauma center, was an independent risk factor for complications. Patients residing closer to the medical center had lower rates of complications. This finding could be attributed to several factors, including access to more prompt intervention at a high-level trauma center, proximity to specialized care, and easier access for close follow-up. In the public health literature, Dodson et al25 found reduced trauma-related mortality associated with proximity and access to trauma centers.
Patient-Related Factors
Tobacco use was prevalent among subjects in our study (46.5%). Our multivariate analysis determined smoking to be an independent risk factor for increased complications, in line with most prior studies showing a high incidence of smoking and its association with poorer outcomes.9,10,20 Smoking is a known risk factor for impaired wound healing due to degeneration of mesenchymal tissues and decreased collagen production and oxygen delivery and has been demonstrated to cause an estimated 6-fold increase in infections in smokers compared with nonsmokers after repair of fractures.26 Smoking cessation efforts should therefore be undertaken, when feasible, to improve outcomes.
Dental extractions may be necessary in some patients with mandible fractures, which include the following factors that guide the heuristic currently used by one of us (T.T.T.): severe decay, impediment to fracture reduction, or root fracture. The findings of this study are consistent with those of Christensen et al,27 who found that extraction of a tooth in the line of fracture increased postoperative complications as defined by hospital readmission, reoperation rate, or prolonged postoperative hospitalization. Other studies have found that tooth extraction did not affect postoperative complications.9,11,28 A tooth with significant decay may lead to a weaker point in the mandible, predisposing that area to fracture. One could surmise that if tooth extraction was necessary, then more severe dental and periodontal disease may have been present, which would predispose the patient to a poorer outcome. This area warrants more rigorous examination in a series in which a greater number of dental extractions occurred.
Use of Antibiotics
In this current era of antibiotic stewardship, we included use of antibiotics in the preoperative, perioperative, and postoperative periods as a possible protective factor to prevent complications. Our study agrees with previous reports that found no association between use of antibiotics and postoperative surgical site complications.9,10 The patients in our study were predominantly given systemic antibiotics (99 of 136 [72.8%]) and chlorhexidine mouthwash (99 of 135 [73.3%]), while the current practice is to limit antibiotics to the immediate perioperative period. Given the lack of high-quality evidence, postoperative antibiotics should be used judiciously in patients with mandibular fractures. Further studies to determine the best practice of prophylactic use of antibiotics in patients with mandible fractures are needed.
Strengths and Limitations
The data should be interpreted in the context of the study design. We sought to strengthen the retrospective nature of the study by abstracting extensive objective data rather than relying on subjective narrative. Patient medical records were queried for an expansive number of variables that could affect outcomes (eg, traumatic concomitant injuries, medical comorbidities, drug and tobacco use, or status of dental health). Prospective studies of care of mandible fractures are rare owing to a variety of factors, including variations in treatment planning, lack of data on equivalency of treatment protocols, and unpredictable follow-up. Some patients with mandible fractures are transferred to our higher-level trauma facility but are unable to continue follow-up secondary to insurance restrictions. Patient adherence to returning for care can also be limited by geography, cost of care, lack of health care coverage, or being out of network. Planned expansion of the electronic health record with integrated capabilities across health systems will greatly benefit this type of retrospective work in future studies.
Conclusions
Patients treated for mandible fractures at a single academic level 1 trauma center during a 3-year period had a complication rate of 21.2%, which included wound dehiscence or surgical site infection, bony nonunion, and hardware exposure. Risk factors associated with these complications were an increased time to surgery, tobacco use, dental extraction, and living farther from the treatment facility. Future studies are needed to evaluate the combined effects of patient-related and systems-level factors that affect outcomes. Surgical systems may consider prioritizing mandible fracture repair to within the first 3 to 6 days after injury, implementing smoking cessation programs, and promoting dental care in this patient population.
eTable. Diagnostic and Procedure Codes for Mandible Fractures
References
- 1.Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg. 2003;61(6):713-718. doi: 10.1053/joms.2003.50118 [DOI] [PubMed] [Google Scholar]
- 2.Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48(9):926-932. doi: 10.1016/0278-2391(90)90004-L [DOI] [PubMed] [Google Scholar]
- 3.Ellis E III, Moos KF, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59(2):120-129. doi: 10.1016/0030-4220(85)90002-7 [DOI] [PubMed] [Google Scholar]
- 4.Brook IM, Wood N. Aetiology and incidence of facial fractures in adults. Int J Oral Surg. 1983;12(5):293-298. doi: 10.1016/S0300-9785(83)80016-7 [DOI] [PubMed] [Google Scholar]
- 5.van Hoof RF, Merkx CA, Stekelenburg EC. The different patterns of fractures of the facial skeleton in four European countries. Int J Oral Surg. 1977;6(1):3-11. doi: 10.1016/S0300-9785(77)80066-5 [DOI] [PubMed] [Google Scholar]
- 6.Sojot AJ, Meisami T, Sandor GK, Clokie CM. The epidemiology of mandibular fractures treated at the Toronto General Hospital: A review of 246 cases. J Can Dent Assoc. 2001;67(11):640-644. [PubMed] [Google Scholar]
- 7.Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Pollock RE. Schwartz’s Principles of Surgery. 8th ed New York, NY: McGraw-Hill Professional; 2004. [Google Scholar]
- 8.Nasser M, Pandis N, Fleming PS, Fedorowicz Z, Ellis E, Ali K. Interventions for the management of mandibular fractures. Cochrane Database Syst Rev. 2013;8(7):CD006087. doi: 10.1002/14651858.CD006087.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gutta R, Tracy K, Johnson C, James LE, Krishnan DG, Marciani RD. Outcomes of mandible fracture treatment at an academic tertiary hospital: a 5-year analysis. J Oral Maxillofac Surg. 2014;72(3):550-558. doi: 10.1016/j.joms.2013.09.005 [DOI] [PubMed] [Google Scholar]
- 10.Furr AM, Schweinfurth JM, May WL. Factors associated with long-term complications after repair of mandibular fractures. Laryngoscope. 2006;116(3):427-430. doi: 10.1097/01.MLG.0000194844.87268.ED [DOI] [PubMed] [Google Scholar]
- 11.Malanchuk VO, Kopchak AV. Risk factors for development of infection in patients with mandibular fractures located in the tooth-bearing area. J Craniomaxillofac Surg. 2007;35(1):57-62. doi: 10.1016/j.jcms.2006.07.865 [DOI] [PubMed] [Google Scholar]
- 12.Lee UK, Rojhani A, Herford AS, Thakker JS. Immediate versus delayed treatment of mandibular fractures: a stratified analysis of complications. J Oral Maxillofac Surg. 2016;74(6):1186-1196. doi: 10.1016/j.joms.2016.01.019 [DOI] [PubMed] [Google Scholar]
- 13.Schaller B, Soong PL, Zix J, Iizuka T, Lieger O. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomized, double-blind, placebo-controlled pilot clinical study, part 2: mandibular fractures in 59 patients. Br J Oral Maxillofac Surg. 2013;51(8):803-807. doi: 10.1016/j.bjoms.2013.08.008 [DOI] [PubMed] [Google Scholar]
- 14.Senel FC, Jessen GS, Melo MD, Obeid G. Infection following treatment of mandible fractures: the role of immunosuppression and polysubstance abuse. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(1):38-42. doi: 10.1016/j.tripleo.2006.02.013 [DOI] [PubMed] [Google Scholar]
- 15.Serena-Gómez E, Passeri LA. Complications of mandible fractures related to substance abuse. J Oral Maxillofac Surg. 2008;66(10):2028-2034. doi: 10.1016/j.joms.2008.06.022 [DOI] [PubMed] [Google Scholar]
- 16.Mundinger GS, Borsuk DE, Okhah Z, et al. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofac Trauma Reconstr. 2015;8(1):64-78. doi: 10.1055/s-0034-1378187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyzas PA. Use of antibiotics in the treatment of mandible fractures: a systematic review. J Oral Maxillofac Surg. 2011;69(4):1129-1145. doi: 10.1016/j.joms.2010.02.059 [DOI] [PubMed] [Google Scholar]
- 18.Vyas A, Mazumdar U, Khan F, Mehra M, Parihar L, Purohit C. A study of mandibular fractures over a 5-year period of time: a retrospective study. Contemp Clin Dent. 2014;5(4):452-455. doi: 10.4103/0976-237X.142808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellis E., III A prospective study of 3 treatment methods for isolated fractures of the mandibular angle. J Oral Maxillofac Surg. 2010;68(11):2743-2754. doi: 10.1016/j.joms.2010.05.080 [DOI] [PubMed] [Google Scholar]
- 20.Zavlin D, Jubbal KT, Echo A, Izaddoost SA, Friedman JD, Olorunnipa O. Multi-institutional analysis of surgical management and outcomes of mandibular fracture repair in adults. Craniomaxillofac Trauma Reconstr. 2018;11(1):41-48. doi: 10.1055/s-0037-1603460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biller JA, Pletcher SD, Goldberg AN, Murr AH. Complications and the time to repair of mandible fractures. Laryngoscope. 2005;115(5):769-772. doi: 10.1097/01.MLG.0000157328.10583.A7 [DOI] [PubMed] [Google Scholar]
- 22.Czerwinski M, Parker WL, Chehade A, Williams HB. Identification of mandibular fracture epidemiology in Canada: enhancing injury prevention and patient evaluation. Can J Plast Surg. 2008;16(1):36-40. doi: 10.1177/229255030801600107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webb LS, Makhijani S, Khanna M, et al. A comparison of outcomes between immediate and delayed repair of mandibular fractures. Can J Plast Surg. 2009;17(4):124-126. doi: 10.1177/229255030901700401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucca M, Shastri K, McKenzie W, Kraus J, Finkelman M, Wein R. Comparison of treatment outcomes associated with early versus late treatment of mandible fractures: a retrospective chart review and analysis. J Oral Maxillofac Surg. 2010;68(10):2484-2488. doi: 10.1016/j.joms.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 25.Dodson BK, Braswell M, David AP, et al. Adult and elderly population access to trauma centers: an ecological analysis evaluating the relationship between injury-related mortality and geographic proximity in the United States in 2010 [published online November 28, 2017]. J Public Health (Oxf). doi: 10.1093/pubmed/fdx156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams CI, Keating JF, Court-Brown CM. Cigarette smoking and open tibial fractures. Injury. 2001;32(1):61-65. doi: 10.1016/S0020-1383(00)00121-2 [DOI] [PubMed] [Google Scholar]
- 27.Christensen BJ, Mercante DE, Neary JP, King BJ. Risk factors for severe complications of operative mandibular fractures. J Oral Maxillofac Surg. 2017;75(4):787.e1-787.e8. doi: 10.1016/j.joms.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 28.Bobrowski AN, Sonego CL, Chagas Junior OL. Postoperative infection associated with mandibular angle fracture treatment in the presence of teeth on the fracture line: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2013;42(9):1041-1048. doi: 10.1016/j.ijom.2013.02.021 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Diagnostic and Procedure Codes for Mandible Fractures