Abstract
Objective
Hospitalisation rates for many chronic conditions are higher in socioeconomically disadvantaged and less accessible areas. We aimed to map diabetes hospitalisation rates by local government area (LGA) across Western Victoria, Australia, and investigate their association with socioeconomic status (SES) and accessibility/remoteness.
Design
Cross-sectional study
Methods
Data were acquired from the Victorian Admitted Episodes Dataset for all hospitalisations (public and private) with a diagnosis of type 1 or type 2 diabetes mellitus during 2011–2014. Crude and age-standardised hospitalisation rates (per 1000 population per year) were calculated by LGA for men, women and combined data. Associations between accessibility (Accessibility/Remoteness Index of Australia, ARIA), SES (Index of Relative Socioeconomic Advantage and Disadvantage, IRSAD) and diabetes hospitalisation were investigated using Poisson regression analyses.
Results
Higher LGA-level accessibility and SES were associated with higher rates of type 1 and type 2 diabetes hospitalisation, overall and for each sex. For type 1 diabetes, higher accessibility (ARIA category) was associated with higher hospitalisation rates (men incidence rate ratio [IRR]=2.14, 95% CI 1.64 to 2.80; women IRR=2.45, 95% CI 1.87 to 3.19; combined IRR=2.30, 95% CI 1.69 to 3.13; all p<0.05). Higher socioeconomic advantage (IRSAD decile) was also associated with higher hospitalisation rates (men IRR=1.25, 95% CI 1.09 to 1.43; women IRR=1.32, 95% CI 1.16 to 1.51; combined IRR=1.23, 95% CI 1.07 to 1.42; all p<0.05). Similarly, for type 2 diabetes, higher accessibility (ARIA category) was associated with higher hospitalisation rates (men IRR=2.49, 95% CI 1.81 to 3.43; women IRR=2.34, 95% CI 1.69 to 3.25; combined IRR=2.32, 95% CI 1.66 to 3.25; all p<0.05) and higher socioeconomic advantage (IRSAD decile) was also associated with higher hospitalisation rates (men IRR=1.15, 95% CI 1.02 to 1.30; women IRR=1.14, 95% CI 1.01 to 1.28; combined IRR=1.13, 95% CI 1.00 to 1.27; all p<0.05).
Conclusion
Our observations could indicate self-motivated treatment seeking, and better specialist and hospital services availability in the advantaged and accessible areas in the study region. The determinants for such variations in hospitalisation rates, however, are multifaceted and warrant further research.
Keywords: diabetes mellitus, hospitalisation, socioeconomic status, remoteness, accessibility
Strengths and limitations of this study.
Hospitalisation data were acquired from a comprehensive register of admissions to all hospitals in the state, both public and private.
Large study area spanning a wide range of socioeconomic status (SES).
Diabetes hospitalisation data included all admission records with diabetes, which could have resulted in overestimation of diabetes hospitalisation due to multiple admissions.
SES and accessibility indices represent geographical areas rather than individuals.
Introduction
Diabetes mellitus is a major risk factor for hospitalisation, repeated admissions and longer hospital stays.1–4 The incidence of both planned and unplanned hospital admissions in individuals with diabetes is substantially higher than those without.5 6 Hospital care is the largest component of the expenditure attributable to diabetes mellitus.7 8 The American Diabetes Association reported that during 2011–2012, inpatient care accounted for 43% of the direct medical costs for diabetes in the USA.7 Similarly, diabetes accounted for 14% of hospital admissions for chronic disease in Australia during 2013–2014.2 3 Furthermore, in Australia, hospital care contributed nearly half of the annual direct costs for type 1 diabetes mellitus (T1DM) and one-third for type 2 diabetes mellitus (T2DM).8 According to a national inpatient audit report for 2016, one in six hospital beds in the UK were occupied by a person with diabetes.9 An audit of 11 hospitals across Melbourne, Australia, reported an overall diabetes prevalence of 24.7% among hospitalised patients.10
The global prevalence of diabetes is rising rapidly, with one in ten adults expected to have the condition by 2040.11 Population ageing, increasing rates of obesity and unhealthy lifestyle are some of the factors contributing to this global pandemic.3 12 Consequently, health systems in developing and developed countries will have to cope with an increased demand for diabetes-related acute health services.13 Some of the known determinants of diabetes-related hospitalisations are advancing age,6 suboptimal glycaemic management,14 comorbidities,6 15 16 previous admission,14 physical inactivity17 as well as minimal and excessive contact with primary care.18
Globally, residents of regional and remote areas experience adverse health outcomes, including higher hospitalisation rates for chronic diseases, as compared with those living in metropolitan areas.19 20 Various factors are implicated in this disparate healthcare experience including lower socioeconomic status (SES),19 higher prevalence of lifestyle risk factors,21 lower access to primary care services20 and shortage of healthcare professionals.22 In Australia, those living in ‘rural and remote areas’ tend to have lower life expectancy, higher rates of disease and injury, and poorer access to and use of health services than people living in ‘major cities’.23 Diabetes hospitalisation rates also vary by place of residence, which could be explained by differences in area-level SES and accessibility.24–26 There are limited data on the relationship between SES, accessibility and diabetes hospitalisation in regional populations. Such information could aid in planning future diabetes-related service delivery, identifying discrepancies between the need for and uptake of health services, and to devise strategies to reduce service demand by addressing its community-level determinants.
These analyses were undertaken as part of the Ageing, Chronic Disease and Injury (ACDI) study,27 launched in 2015 with the overarching aim to describe chronic disease and injury patterns in the western region of the state of Victoria, Australia. There are no previous reports on diabetes hospitalisation for the region; we aimed to map the geographical variations in diabetes hospitalisation rates and investigated their relationship with area-level SES and accessibility indicators.
Methods
Study region
The ACDI study region comprises 21 of the 79 local government areas (LGAs), which are administrative boundaries that cover legally designated parts of the state of Victoria (Australia) over which incorporated local governing bodies have responsibility. As of 2011, the estimated resident population of the ACDI study region was 617 794, representing almost one-tenth of the state’s population.27 The median LGA population was 16 145 and ranged from 3058 (Queenscliffe) to 221 515 (Greater Geelong). A profile of the study region describing its key sociodemographic characteristics has been published previously.27 This region is often described as a microcosm, ideally placed for epidemiological research due to its close resemblance with the overall national demographic structure.28 There is a major urban centre (Geelong) and areas of varying SES and remoteness levels.27 The study region also includes large agriculture areas with farming communities, involved in dairy production and broad acre farming (cropping, wool and meat production).27
SES and accessibility/remoteness
We cross-referenced residential addresses to the Australian Bureau of Statistics (ABS) census data, and also ascertained the region of residence according to LGAs. We defined deciles of area-level SES using the composite Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD), which is one of the four Socio-Economic Indexes For Areas, developed by the ABS, using the 2011 Census data.29 The IRSAD accounts for high and low area-based income and occupation types including unskilled employment to professional positions, among other variables. The IRSAD values of the LGA of usual residence were mapped for the study region.29 The IRSAD scores are equivalised for both advantage and disadvantage, therefore, providing values that span the continuum from the most socially disadvantaged decile (lowest 10%=decile 1) to the most socially advantaged decile. Deciles cut-points for IRSAD values were based on the Victorian population.29 Our study region included LGAs that spanned the range of SES deciles, ranging from the most disadvantaged (Central Goldfields, Northern Grampians, Hindmarsh and Pyrenees) to the most advantaged (Surf Coast).27 Importantly, Central Goldfields is also the lowest ranking LGA in the state of Victoria in terms of SES while Surf Coast is the seventh most socioeconomically advantaged.27
Accessibility/Remoteness Index of Australia (ARIA) was used as the measure of LGA-level accessibility.27 The ARIA was developed by the Australian Government’s Department of Health and Aged Care and uses a geographical approach to defining remoteness.30 The scores are determined by distance from towns and cities, access to goods and services, and opportunities for social interaction.30 A low ARIA score indicates high accessibility and there are five categories ranging from highly accessible (≤1.84), accessible (1.84–3.51), moderately accessible (3.51–5.80), remote (5.80–9.08) and very remote (≥9.08).30 In our study region, the LGAs of Hindmarsh, West Wimmera and Yarriambiack were classified as ‘moderately accessible’, which is the lowest accessible category in the state of Victoria as there are no LGAs in the ‘remote’ or ‘very remote’ categories.27 The remaining LGAs were either in the ‘accessible’ or ‘highly accessible’ categories.
Diabetes hospitalisation data
Data on hospital admissions were acquired from the Victorian Admitted Episodes Dataset, which maintains a comprehensive record of hospitalisations in the state. All state hospitals, public and private, are required to submit data for each admitted episode. The ‘primary’ and ‘additional’ diagnoses are classified using the Australian Modification of International Classification of Disease, 10th revision.31 For each episode of admission, one primary and up to 40 additional diagnoses can be recorded.31
As we intended to capture all admission episodes in individuals ‘with’ diabetes, not limited to those specifically ‘for’ diabetes or its complications, we included all instances with a T1DM (code E10) or T2DM (code E11) diagnosis, during 2011–2014, inclusive. Admissions for other forms of diabetes, including gestational diabetes were excluded (codes E13, E14 and O24). Repeated admissions in the same individuals were also included in the aggregated hospitalisation data.
Patient and public involvement
There was no direct patient or public involvement.
Statistical analysis
We used aggregated data for our analysis over 2011–2014, inclusive. Initially, crude T1DM-hospitalisation and T2DM-hospitalisation rates were calculated by age group (<40 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years and 80+ years), sex and LGA of residence. Age-standardisation was performed using the Australian population (2011) as the standard. Population estimates were obtained from the ABS.32 All hospitalisation rates were expressed as ‘per 1000 population per year’ and presented separately for men and women, as well as combined for both sexes.
To investigate the associations between sociodemographic indicators and diabetes-hospitalisations, Poisson regression analysis was performed and incidence rate ratios (IRRs) were calculated by age group, SES (SES decile) and accessibility (ARIA category) for men, women and combined data. Due to high level of correlation between SES and ARIA, separate regression models were used considering both individually. All models were weighted according to LGAs’ population to account for heterogeneity in population size. Statistical analyses were performed using Stata (V.14).
Results
Table 1 provides an overview of diabetes hospitalisations in the ACDI region during 2011–2014, inclusive. In total, there were 104 126 T1DM-hospitalisations or T2DM-hospitalisations in the region, of which, 57 077 (54.8%) were in men. Overall, only 5.0% of diabetes-related admissions had diabetes as a ‘primary’ diagnosis, whereas in most cases, diabetes was recorded as an ‘additional’ diagnosis. This differed between T1DM-hospitalisation and T2DM-hospitalisation, with 22.0% of T1DM-hospitalisations recorded as primary diagnosis, compared with 2.7% of T2DM-hospitalisations. Type 2 diabetes accounted for almost 90.0% of all diabetes hospitalisations overall, as well as for men (91.5%) and women (90.0%) separately (table 1).
Table 1.
Overview of T1DM-hospitalisations and T2DM-hospitalisations in the ACDI region during 2011–2014 inclusive, by age group, sex, socioeconomic status and accessibility, presented as n (%)
| T1DM-hospitalisation | T2DM-hospitalisation | |||||
| Total n=10 617 | Men n=5431 (51.1%) | Women n=5276 (49.6%) | Total n=93 508 | Men n=51 736 (55.3%) | Women n=47 048 (50.3%) | |
| Age (years) | ||||||
| <40 | 3886 (36.6%) | 1596 (29.3%) | 2290 (43.4%) | 1137 (1.2%) | 409 (0.7%) | 728 (1.5%) |
| 40–49 | 1348 (12.6%) | 648 (11.9%) | 700 (13.2%) | 3589 (3.8%) | 1692 (3.2%) | 1894 (4.0%) |
| 50–59 | 1902 (17.9%) | 1046 (19.2%) | 856 (16.2%) | 11 848 (12.6%) | 6860 (13.2%) | 4988 (10.6%) |
| 60–69 | 1858 (17.5%) | 1105 (20.3%) | 753 (14.2%) | 23 791 (25.4%) | 14 529 (28.0%) | 9262 (19.6%) |
| 70–79 | 991 (9.3%) | 627 (11.5%) | 364 (6.8%) | 29 248 (31.2%) | 16 400 (31.6%) | 12 848 (27.3%) |
| ≥80 | 632 (5.9%) | 319 (5.8%) | 313 (5.9%) | 23 898 (25.5%) | 11 846 (22.8%) | 12 052 (25.6%) |
| Socioeconomic status (IRSAD) of local government area | ||||||
| Decile 1 (most disadvantaged) | 775 (7.2%) | – | – | 7595 (8.1%) | – | – |
| Decile 2 | 381 (3.5%) | – | – | 3714 (3.9%) | – | – |
| Decile 3 | 441 (4.1%) | – | – | 6298 (6.7%) | – | – |
| Decile 4 | 3046 (28.6%) | – | – | 21 351 (22.8%) | – | – |
| Decile 5 | 4832 (45.5%) | – | – | 43 805 (46.8%) | – | – |
| Decile 6 | – | – | – | – | ||
| Decile 7 | 614 (5.7%) | – | – | 5936 (6.3%) | – | – |
| Decile 8 | 266 (2.5%) | – | – | 1930 (2.0%) | – | – |
| Decile 9 | 31 (0.2%) | – | – | 651 (0.6%) | – | – |
| Decile 10 (most advantaged) | 231 (2.1%) | – | – | 2229 (2.3%) | – | – |
| Accessibility/remoteness (ARIA) of local government area | ||||||
| Moderately accessible (lowest accessibility) | 287 (2.7%) | – | – | 3806 (4.0%) | – | – |
| Accessible | 1835 (17.2%) | – | – | 21 015 (22.4%) | – | – |
| Highly accessible (highest accessibility) | 8495 (80.0%) | – | – | 68 688 (73.4%) | – | – |
ACDI, Ageing, Chronic Disease and Injury; ARIA, Accessibility/Remoteness Index of Australia; IRSAD, Index of Relative Socioeconomic Advantage and Disadvantage; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Of the 10 617 total T1DM-hospitalisations, 3886 (~36%) were <40 years of age (29.3% men and 43.3% women), whereas just under 11% were in the 80+ years group (table 1). A significantly higher proportion of T2DM-hospitalisations were in the older age groups (table 1). On the basis of the ARIA scores, 74.1% of diabetes hospitalisations represented residents of ‘highly accessible’ LGAs (table 1)
The rate of T1DM-hospitalisations in men was 2.6 per 1000 population per year in the <40 years age group (95% CI 2.5 to 2.7), increasing to 7.8 per 1000 population per year in the 60–69 years age group (95% CI 7.3 to 8.3) and declining afterwards in the 70–79 years and >80 years age groups (figure 1A). A similar pattern was evident in women with the highest rate of T1DM-hospitalisations in the 60–69 years age group, that is, 5.3 per 1000 population per year (95% CI 4.9 to 5.6) (figure 1A).
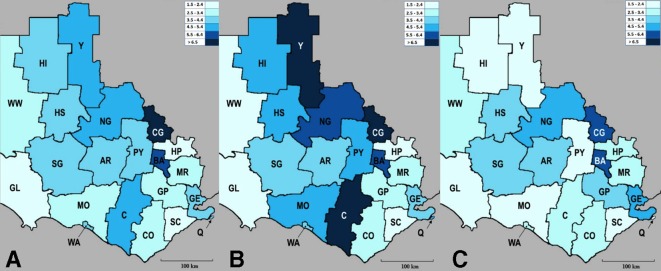
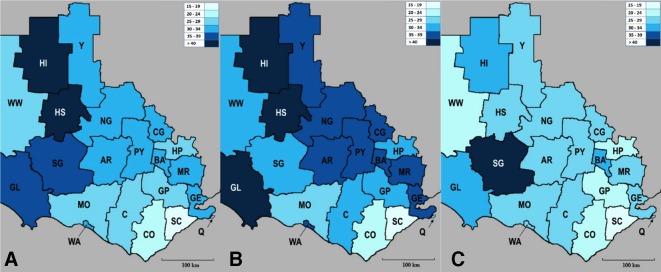
Figure 1.
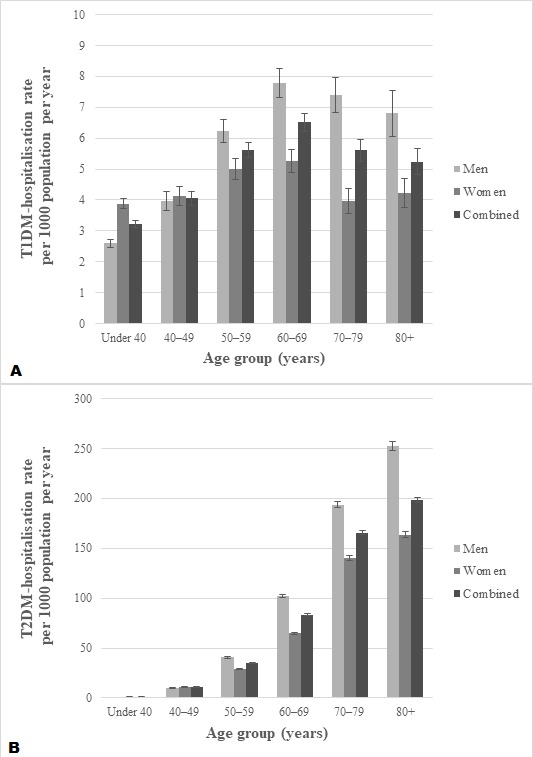
Age group stratified hospitalisation rate for (A) T1DM and (B) T2DM per 1000 population per year during 2011–2014 inclusive, across ACDI study region presented for men, women and combined data, with error bars showing 95% CIs. ACDI, Ageing, Chronic Disease and Injury; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
A linear increase in T2DM-hospitalisation rates was observed with increasing age (figure 1B). In men, T2DM-hospitalisation rate was 0.6 per 1000 population per year in the <40 years age group (95% CI 0.6 to 0.7) to 252.9 per 1000 population per year in the 80+ years age group (95% CI 248.4 to 257.5). For women, the rate was 1.2 per 1000 population per year in the <40 years age group (95% CI 1.1 to 1.3), increasing to 163.6 in the >80 years age group (95% CI 160.6 to 166.5)
For the whole study region, both T1DM-hospitalisation and T2DM-hospitalisation rates were higher in men compared with women. Unadjusted T1DM-hospitalisation rate was 6.1 per 1000 population per year in men (95% CI 5.9 to 6.5) versus 3.5 per 1000 population per year in women (95% CI 3.4 to 3.9) and T2DM-hospitalisation rate was 85.6 per 1000 population per year in men (95% CI 84.0 to 88.2) versus 64.3 per 1000 population per year in women (95% CI 63.2 to 67.1).
Figures 2 and 3 show the geographical variation in T1DM-hospitalisation and T2DM-hospitalisation rates across the study region, for men and women combined (figures 2A and 3A), men only (figures 2B and 3B) and women only (figures 2C and 3C), respectively. Overall, the LGA of Central Goldfields, which has the lowest SES in the study region (decile 1), had the highest T1DM-hospitalisation rate, whereas Surf Coast (decile 10), Glenelg (decile 3) and Hepburn (decile 4) had the lowest (figure 2A). The LGA of Hindmarsh (decile 1) had the highest T2DM-hospitalisation rate and Surf Coast (decile 10) had the lowest (figure 3A).
Figure 2.
Density map showing T1DM-hospitalisation rate for (A) men and women combined (B) men only and (C) women only for the ACDI study region during 2011–2014 inclusive (age-standardised rates per 1000 population per year). LGAs are shaded according to the legend from the lowest to highest hospitalisation rates. ACDI, Ageing, Chronic Disease and Injury; AR, Ararat; BA, Ballarat; C, Corangamite; CG, Central Goldfields; CO, Colac Otway; GE, Greater Geelong; GL, Glenelg; GP, Golden Plains; HI, Hindmarsh; HP, Hepburn; HS, Horsham; LGAs, local government areas; MO, Moyne; MR, Moorabool; NG, Northern Grampians; PY, Pyrenees; Q, Queenscliffe; SC, Surf Coast; SG, Southern Grampians; T1DM, type 1 diabetes mellitus; WA, Warrnambool; WW, West Wimmera; Y, Yarriambiack.
Figure 3.
Density map showing T2DM-hospitalisation rate for (A) men and women combined (B) men only and (C) women only for the ACDI study region during 2011–2014 inclusive (age-standardised rates per 1000 population per year). LGAs are shaded according to the legend from the lowest to highest hospitalisation rates. ACDI, Ageing, Chronic Disease and Injury; AR, Ararat; BA, Ballarat; C, Corangamite; CG, Central Goldfields; CO, Colac Otway; GE, Greater Geelong; GL, Glenelg; GP, Golden Plains; HI, Hindmarsh; HP, Hepburn; HS, Horsham; LGAs, local government areas; MO, Moyne; MR, Moorabool; NG, Northern Grampians; PY, Pyrenees; Q, Queenscliffe; SC, Surf Coast; SG, Southern Grampians; T2DM, type 2 diabetes mellitus; WA, Warrnambool; WW, West Wimmera; Y, Yarriambiack.
In univariate analysis, compared with <40 years age group, T1DM-hospitalisation rate was three times higher in the 50–59 years and 60–69 years groups, but not significantly different in the 40–49 years, 70–79 years and 80+ years age groups. Rate of T2DM-hospitalisation was significantly higher in older age groups as compared with <40 years group. Furthermore, being male was associated with higher rates of both T1DM-hospitalisation and T2DM-hospitalisation.
After adjusting for age, rates of both T1DM-hospitalisation and T2DM-hospitalisation were associated with accessibility (residence in more accessible LGA) and SES (socioeconomic advantage) (table 2). These associations were observed for the overall data, as well as for men and women separately.
Table 2.
Regression analysis showing associations of diabetes-hospitalisation with socioeconomic status and accessibility/remoteness for men, women and combined data, adjusted for age
| T1DM-hospitalisation | T2DM-hospitalisation | |||
| IRR (95% CI) | P value | IRR (95% CI) | P value | |
| Men | ||||
| Model: age and ARIA | ||||
| Age (years) | 0.85 (0.78 to 0.92) | <0.001 | 1.63 (1.51 to 1.75) | <0.001 |
| ARIA category of LGA | 2.14 (1.64 to 2.80) | <0.001 | 2.49 (1.81 to 3.43) | <0.001 |
| Model: age and SES | ||||
| Age (years) | 1.07 (0.95 to 1.20) | 0.22 | 2.39 (2.15 to 2.65) | <0.001 |
| SES decile of LGA | 1.25 (1.09 to 1.43) | 0.001 | 1.15 (1.02 to 1.30) | 0.020 |
| Women | ||||
| Model: age and ARIA | ||||
| Age (years) | 0.69 (0.64 to 0.74) | <0.001 | 1.61 (1.49 to 1.73) | <0.001 |
| ARIA category of LGA | 2.45 (1.87 to 3.19) | <0.001 | 2.34 (1.69 to 3.25) | <0.001 |
| Model: age and SES | ||||
| Age (years) | 0.88 (0.77 to 1.00) | <0.060 | 2.30 (2.07 to 2.56) | <0.001 |
| SES decile of LGA | 1.32 (1.16 to 1.51) | <0.001 | 1.14 (1.01 to 1.28) | 0.027 |
| Combined | ||||
| Model: age, sex and ARIA | ||||
| Age (years) | 0.77 (0.73 to 0.80) | <0.001 | 1.61 (1.50 to 1.72) | <0.001 |
| Sex (female) | 0.98 (0.76 to 1.28) | 0.930 | 1.30 (1.11 to 1.53) | 0.001 |
| ARIA category of LGA | 2.30 (1.69 to 3.13) | <0.001 | 2.32 (1.66 to 3.25) | <0.001 |
| Model: age, sex and SES | ||||
| Age (years) | 0.94 (0.86 to 1.03) | 0.190 | 2.20 (2.00 to 2.43) | <0.001 |
| Sex (female) | 1.93 (1.50 to 2.49) | <0.001 | 1.85 (1.63 to 2.10) | <0.001 |
| SES decile of LGA | 1.23 (1.07 to 1.42) | 0.003 | 1.13 (1.00 to 1.27) | 0.035 |
P values <0.05 are shown in bold.
ARIA, Accessibility/Remoteness Index of Australia; IRR, incidence rate ratio; LGA, local government area; SES, socioeconomic status; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Discussion
As part of the larger ACDI study, we have previously proposed a methodology for using routinely collected data to provide contemporary information on region-specific health outcomes for Western Victoria, Australia, which could be replicated in other settings.27 We also reported associations between socioeconomic position, place of residence and utilisation of primary total knee and hip joint replacements,33 and hospital admissions for hip fractures,34 for this region. In this paper, we examine rates of T1DM-hospitalisations and T2DM-hospitalisations by age, sex and place of residence across the ACDI region and their association with SES and accessibility. Increasing accessibility and higher SES were associated with higher rates of T1DM-hospitalisation and T2DM-hospitalisation overall, and for both men and women separately. The rate of T1DM-hospitalisation increased with age and was highest in those aged 60–69 years, followed by a decline in the 70–79 and >80 years age groups. In contrast, rates of T2DM-hospitalisation increased steadily with age, the highest being in the >80 years age group. Rates of both T1DM-hospitalisation and T2DM-hospitalisation were higher in men as compared with women.
We observed that better geographic accessibility was associated with higher rates of T1DM-hospitalisation and T2DM-hospitalisation. Although diabetes is an ambulatory care sensitive condition,35 meaning better access to primary care services helps to reduce hospitalisations, the evidence is mixed.36 The major reason for the variation is that primary care delivery structures differ among countries and regions. In Australia, for instance, general practitioners (GPs) are usually the first point of contact between individuals and health system. They provide referrals to specialists and may often facilitate hospital admissions, particularly in areas with limited specialist availability. A survey of 28 207 Australians aged 15 years and older showed that during 2016–2017, 83% of the responders had seen their GP.37 Hence, the proposition that frequent use of primary health services translates into fewer diabetes hospitalisations may be too simplistic. In a cross-sectional study of indigenous Australians, Zhao et al 18 reported an overall U-shaped relationship between the number of diabetes-related primary healthcare visits and hospitalisation. The lowest hospitalisation rates were observed in those with 20–30 primary care visits per year, increasing in those with <20 or>30 visits per year.18 A similar relationship was reported between avoidable hospitalisation rates and distance from hospital in a Canadian study.38 The study reported that living <35 km and >50 km from a hospital were associated with higher rates of avoidable hospitalisations38; thus, both availability and lack of hospital services close to places of residence may contribute to higher hospitalisation rates. As our data were aggregated by patients’ area of residence, rather than admitting hospital, we were unable to examine this possibility in our study. However, in our study, more than 70% of diabetes admissions represented residents of ‘highly accessible’ areas, which are more likely to live in close proximity of a hospital. Other studies have shown that availability of hospital beds or specialists could increase hospitalisation rates.39 Connell et al 40 argued that higher rates of diabetes hospitalisations do not necessarily indicate inadequate primary care but may just reflect availability of hospital services and variable thresholds of disease severity at which physicians recommend admissions. The study, conducted in the US state of Washington, showed that severity of diabetes in admitted patients (determined by blood glucose levels, admissions for coma, surgery, intensive care or terminal episodes) was considerably higher in counties with lower bed supply.40 Over-servicing may also play a role in areas where hospital beds and admitting physicians are in oversupply, although this needs further investigation.
We observed a direct association between socioeconomic advantage and diabetes-hospitalisation. This is not consistent with previously reported hospitalisation data from the Australian Institute of Health and Welfare that show higher hospital separations for diabetes complications in more disadvantaged and remote areas, compared with more affluent and easily accessible areas.2 3 In another Australian study, Bergin et al 25 reported higher rates of diabetic-foot-related hospitalisations among residents of socially disadvantaged areas. Furthermore, limb amputations due to diabetes are lowest in major cities and inner regional areas and highest in remote and disadvantaged areas.41 These social patterns of hospitalisations have been observed in other countries, for instance, in a Scottish study of 35 935 individuals with diabetes reported a significantly higher proportion of hospital admissions for people presenting with both acute and chronic complications of diabetes in the lowest socioeconomic quintile as compared with those in the highest.24
Social disadvantage has been identified as a barrier to treatment-seeking.42 Given that admission to a hospital may result in loss of income, people, particularly those self-employed, such as farmers and small business owners, may delay necessary inpatient treatment only to end up in the hospital at a later stage with serious complications. A possible explanation for our findings could be that socioeconomic disadvantage and geographic remoteness act as risk factors for ‘emergency’ hospitalisation while acting as barriers to ‘elective’ hospitalisation. Our data, however, did not have the necessary detail to distinguish between elective and emergency hospitalisations, specific reasons for admission or whether there were delays in treatment seeking.
Our results are consistent with previous data showing that six out of every seven hospital admissions for diabetes are T2DM-related.3 In our study, approximately 90% of diabetes-hospitalisations were T2DM-related, which could reflect a similarly higher proportion of T2DM as compared with T1DM in the population. The association between advancing age and hospitalisation was different for T1DM-hospitalisation and T2DM-hospitalisation where more than one-third of T1DM-hospitalisations were in individuals under 40 years of age, compared with less than 2% of T2DM-hospitalisations. This is not surprising as T2DM is less common in this age group and until recently, survival into old age for those with T1DM has been rare. Adolescents and young adults with diabetes, predominantly T1DM, represent a particularly high-risk group for acute hospitalisations.6 Younger persons with diabetes are more likely to miss medical appointments, have worse self-care practices and behaviours, and are less likely to follow medication regimes.43 44 Similarly, elderly persons with diabetes often present with multiple and advanced complications, and are more likely to be readmitted, have longer lengths of hospital stay and higher risk of mortality as compared with younger counterparts.35
Our study has some strengths and limitations. A major strength of our study is that we acquired hospitalisation data from the Victorian Admitted Episodes Dataset, a comprehensive register that collates data from both public and private hospitals and maintains standards for quality and consistency.45 Furthermore, our study region includes areas with a wide range of SES, which makes it suitable to investigate this factor. One of the limitations of our study is that the data presented do not represent ‘individuals’ or ‘separations’ but the total number of admission records with a diagnosis of diabetes. This could have resulted in an overestimation of hospitalisation rates where small numbers of individuals were admitted multiple times. Furthermore, diabetes coding standards in Australian hospitals have undergone significant changes between 2009–2010 and 2013–2014,2 which may have caused inaccuracies in estimation of diabetes-related hospitalisations. Our purpose, however, was not to compare hospitalisation rates over time; therefore, changes in the coding standards would not have had an impact on the interpretation of our data. Moreover, although our study region had no LGAs in the ‘remote’ or ‘very remote’ category, it resembles the accessibility pattern of the state of Victoria, which also does not have any LGAs in these categories. In the absence of reliable diabetes prevalence estimates, we are unable to compare diabetes hospitalisation rates with its prevalence in our study region. However, in the Victorian Population Health Survey (2011–2012),21 the adult prevalence of self-reported, doctor-diagnosed type 2 diabetes was reported. According to the survey, the LGA of Surf Coast (highest SES) had the lowest type 2 diabetes prevalence (2.8%; 95% CI 1.7 to 4.5), whereas Central Goldfields (lowest SES) had the highest (6.1%; 95% CI 4.5 to 8.3). The prevalence was significantly higher among men ‘not in labour force’ or earning <$A40 000 annually (higher socioeconomic disadvantage). The survey did not find any differences in the prevalence of type 2 diabetes between LGAs, or metropolitan versus rural areas. Finally, our study is ecological in nature and uses area-level measures of SES and accessibility/remoteness, which may not capture the socioeconomic diversity among individuals in the community. Results of ecological studies need to be interpreted with caution to avoid making assumptions about individuals based on aggregated population data.
Conclusion
This is the first report of age-related, sex-related, SES-related and accessibility-related variations in rates of diabetes hospitalisation across Western Victoria, Australia. We report that higher SES and accessibility were associated with increased rates for diabetes hospitalisation for both T1DM and T2DM. These results contradict previous reports linking social disadvantage and lower accessibility with higher diabetes-related hospitalisation rates. Health service use for chronic conditions is determined by complex individual, organisational and ecological factors, which need to be addressed in more detail. While we speculate that higher diabetes-related hospitalisation rates may indicate better access to hospital services and social advantage as discussed in this paper, other factors, such as availability of specialists and hospital beds, physicians’ care preferences, health literacy and policies/protocols guiding hospital admissions, also play a role. We have discussed possible explanations of variations in diabetes hospitalisation rates by place of residence, and provided direction for further inquiry into specific determinants, which will inform future planning of hospital services for diabetes.
Supplementary Material
Acknowledgments
We are grateful to the Victorian Admitted Episodes Dataset for providing hospitalisation data for the study.
Footnotes
Contributors: MAS and JAP conceived the study. MAS acquired data and drafted the manuscript. MM performed the data analysis. MAS, KLH-K, MM, MAK, LLFdA, PML, MK, SH, TLD, SB, RSP, AGS, SV, LJW, SLB-O and JAP provided intellectual feedback into the design of the study, critically appraised the manuscript and approved its final version.
Funding: This study was funded by the Western Alliance Academic Health Science Centre, a partnership for research collaboration between Deakin University, Federation University and 13 health service providers across Western Victoria, Australia. MAS and LLFdA were supported by postgraduate scholarships from Deakin University. KLH-K was supported by an Alfred Deakin Postdoctoral Research Fellowship, Deakin University. SLB-O and LJW were each supported by a National Health and Medical Research Council (NHMRC, Australia) Career Development Fellowship (1107510 and 1064272, respectively).
Competing interests: None declared.
Ethics approval: The study was approved by the Barwon Health Human Research Ethics Committee and Deakin University Human Research Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Deidentified aggregated data are available upon request from the corresponding author at msajjad@barwonhealth.org.au.
Patient consent for publication: Not required.
References
- 1. Clinical Epidemiology and Health Service Evaluation Unit. Potentially preventable hospitalisations: a review of the literature and Australian policies. Final report. 2009.
- 2. Australian Institute of Health and Welfare. Admitted patient care 2013-14: Australian hospital statistics. Health services series no. 60 Cat. no. HSE 156. Canberra: AIHW, 2015. https://www.aihw.gov.au/getmedia/3952555a-83c1-41a2-994b 8e9ca38118ed/18671.pdf.aspx?inline=true (Accessed 15 Jul 2017). [Google Scholar]
- 3. Australian institute of Health and Welfare. Diabetes hospitalisations in Australia, 2003-04. Bulletin no 47. Cat. No. 84. Canberra: AIHW, 2006. https://www.aihw.gov.au/getmedia/bf68af7e-3851-4ecb-bdfb-7111590b32d7/bulletin47.pdf.aspx?inline=true (Accessed 22 Aug 2017). [Google Scholar]
- 4. The Joint British Diabetes Societies for Inpatient Care (JBDS – IP). Admissions avoidance and diabetes: guidance for clinical commissioning groups and clinical teams. 2013. http://passthrough.fw-notify.net/download/203915/http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_Admissions_Avoidance_Diabetes.pdf (Accessed 12 Jun 2017).
- 5. Moss SE, Klein R, Klein BE. Risk factors for hospitalization in people with diabetes. Arch Intern Med 1999;159:2053–7. 10.1001/archinte.159.17.2053 [DOI] [PubMed] [Google Scholar]
- 6. Aro S, Kangas T, Reunanen A, et al. . Hospital use among diabetic patients and the general population. Diabetes Care 1994;17:1320–9. 10.2337/diacare.17.11.1320 [DOI] [PubMed] [Google Scholar]
- 7. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baker IDI, Heart & Diabetes Institute. Diabetes: the silent pandemic and its impact on Australia. 2012. (Accessed 12 May 2018).
- 9. NHS Digital. National Diabetes Inpatient Audit (NaDIA)-2016. 2016. http://www.content.digital.nhs.uk/catalogue/PUB23539 (Accessed 10 Jun 2018).
- 10. Bach LA, Ekinci EI, Engler D, et al. . The high burden of inpatient diabetes mellitus: the Melbourne Public Hospitals Diabetes Inpatient Audit. Med J Aust 2014;201:334–8. 10.5694/mja13.00104 [DOI] [PubMed] [Google Scholar]
- 11. International Diabetes Federation. IDF Diabetes Atlas-8th Edition. 2017. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas.html (Accessed 5 June 2018). [PubMed]
- 12. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14. 10.1016/j.diabres.2009.10.007 [DOI] [PubMed] [Google Scholar]
- 13. Rosella LC, Lebenbaum M, Fitzpatrick T, et al. . Impact of diabetes on healthcare costs in a population-based cohort: a cost analysis. Diabet Med 2016;33:395–403. 10.1111/dme.12858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khalid JM, Raluy-Callado M, Curtis BH, et al. . Rates and risk of hospitalisation among patients with type 2 diabetes: retrospective cohort study using the UK General Practice Research Database linked to English Hospital Episode Statistics. Int J Clin Pract 2014;68:40–8. 10.1111/ijcp.12265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leibson CL, Venkat Narayan KM, Fox CS, et al. . Trends in cardiovascular complications of diabetes [1] (multiple letters). JAMA 2005;293:1723–4. [DOI] [PubMed] [Google Scholar]
- 16. Struijs JN, Baan CA, Schellevis FG, et al. . Comorbidity in patients with diabetes mellitus: impact on medical health care utilization. BMC Health Serv Res 2006;6:6 10.1186/1472-6963-6-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vasconcelos JP, de Bruin VMS, Daniele TMC, et al. . Physical activity reduces the risk for hospitalizations in patients with type 2 diabetes. Int J Diabetes Dev Ctries 2015;35:237–9. 10.1007/s13410-015-0309-0 [DOI] [Google Scholar]
- 18. Zhao Y, Wright J, Guthridge S, et al. . The relationship between number of primary health care visits and hospitalisations: evidence from linked clinic and hospital data for remote Indigenous Australians. BMC Health Serv Res 2013;13:13 10.1186/1472-6963-13-466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smith KB, Humphreys JS, Wilson MG. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Aust J Rural Health 2008;16:56–66. 10.1111/j.1440-1584.2008.00953.x [DOI] [PubMed] [Google Scholar]
- 20. Chondur R, Li SQ, Guthridge S, et al. . Does relative remoteness affect chronic disease outcomes? Geographic variation in chronic disease mortality in Australia, 2002–2006. Aust N Z J Public Health 2014;38:117–21. 10.1111/1753-6405.12126 [DOI] [PubMed] [Google Scholar]
- 21. Department of Health State Government of Victoria. Victorian Population Health Survey 2011-2012 survey findings. 2015. http://www.health.vic.gov.au/healthstatus/survey/vphs.htm (Accessed 12 Sep 2017).
- 22. Health Workforce Australia. Health Workforce Australia annual report 2012-2013. Adelaide: HWA, 2013. [Google Scholar]
- 23. Australian Institute of Health and Welfare. Australia’s Health 2016. Australia’s health series no. 15. Cat. no. AUS 199. Canberra: AIHW, 2016. (Accessed 12 September 2017). [Google Scholar]
- 24. Wild SH, McKnight JA, McConnachie A, et al. . Socioeconomic status and diabetes-related hospital admissions: a cross-sectional study of people with diagnosed diabetes. J Epidemiol Community Health 2010;64:1022–4. 10.1136/jech.2009.094664 [DOI] [PubMed] [Google Scholar]
- 25. Bergin SM, Brand CA, Colman PG, et al. . The impact of socio-economic disadvantage on rates of hospital separations for diabetes-related foot disease in Victoria, Australia. J Foot Ankle Res 2011;4:17 10.1186/1757-1146-4-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Booth GL, Hux JE, Fang J, et al. . Time trends and geographic disparities in acute complications of diabetes in Ontario, Canada. Diabetes Care 2005;28:1045–50. 10.2337/diacare.28.5.1045 [DOI] [PubMed] [Google Scholar]
- 27. Sajjad MA, Holloway KL, Kotowicz MA, et al. . Ageing, Chronic Disease and Injury: A Study in Western Victoria (Australia). J Public Health Res 2016;5:678 10.4081/jphr.2016.678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Western Alliance Academic Health Science Centre. Western Alliance. 2015. http://www.westernalliance.org.au/ (Accessed 12 Jun 2017).
- 29. Australian Bureau of Statistics. 2033.0.55.001 - Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia. 2014. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2033.0.55.001main+features100042011 (Accessed 19 July 2018).
- 30. Commonwealth Department of Health and Aged Care. Measuring Remoteness: Accessibility/Remoteness Index of Australia (ARIA). Occasional Papers: New Series Number 14. Canberra. 2001. http://www.health.gov.au/internet/main/publishing.nsf/Content/E2EE19FE831F26BFCA257BF0001F3DFA/$File/ocpanew14.pdf (Accessed 9 May 2017).
- 31. National Centre for Classification in Health. The international statistical classification of diseases and related health problems, 10th revision, Australian modification (ICD-10-AM). 2016. (Accessed 26 Nov 2017). [PubMed]
- 32. Australian Bureau of Statistics ABS. Stat. Estimated Resident Population by Sex by Age Group by LGA, 2001-2013. 2015. http://stat.abs.gov.au/ (Accessed 19 Oct 2017).
- 33. Brennan-Olsen S, Vogrin S, Holloway KL, et al. . Geographic region, socioeconomic position and the utilisation of primary total joint replacement for hip or knee osteoarthritis across western Victoria: a cross-sectional multilevel study of the Australian Orthopaedic Association National Joint Replacement Registry. Arch Osteoporos 2017;12:97 10.1007/s11657-017-0396-2 [DOI] [PubMed] [Google Scholar]
- 34. Holloway KL, Sajjad MA, Mohebbi M, et al. . The epidemiology of hip fractures across western Victoria, Australia. Bone 2018;108:1–9. 10.1016/j.bone.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 35. Niefeld MR, Braunstein JB, Wu AW, et al. . Preventable hospitalization among elderly Medicare beneficiaries with type 2 diabetes. Diabetes Care 2003;26:1344–9. 10.2337/diacare.26.5.1344 [DOI] [PubMed] [Google Scholar]
- 36. Rosano A, Loha CA, Falvo R, et al. . The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health 2013;23:356–60. 10.1093/eurpub/cks053 [DOI] [PubMed] [Google Scholar]
- 37. Australian Bureau of Statistics. 4839.0 - Patient Experiences in Australia: Summary of Findings, 2016-17. Canberra: ABS, 2017. http://www.abs.gov.au/ausstats/abs@.nsf/mf/4839.0 (Accessed 9 July 2018). [Google Scholar]
- 38. Lin G, Allan DE, Penning MJ. Examining Distance Effects on Hospitalizations Using GIS: A Study of Three Health Regions in British Columbia, Canada. Environment and Planning A: Economy and Space 2002;34:2037–53. 10.1068/a3528 [DOI] [Google Scholar]
- 39. Roemer MI. Bed supply and hospital utilization: a natural experiment. Hospitals 1961;35:36–42. [PubMed] [Google Scholar]
- 40. Connell FA, Blide LA, Hanken MA. Clinical correlates of small area variations in population-based admission rates for diabetes. Med Care 1984;22:939–49. 10.1097/00005650-198410000-00006 [DOI] [PubMed] [Google Scholar]
- 41. Australian institute of Health and Welfare. Burden of lower limb amputations due to diabetes in Australia: Australian Burden of Disease Study 2011. Australian Burden of Disease Study series no. 10. BOD 11. Canberra: AIHW, 2017. [Google Scholar]
- 42. Billings J, Zeitel L, Lukomnik J, et al. . Impact of socioeconomic status on hospital use in New York City. Health Aff 1993;12:162–73. 10.1377/hlthaff.12.1.162 [DOI] [PubMed] [Google Scholar]
- 43. Bujang MA, Supramaniam P, Haniff J, et al. . The association between self-care practices, HbA1c and quality of life for type 1 DM in children and adolescents. IMJ 2013;20:317–9. [Google Scholar]
- 44. Commissariat PV, Kenowitz JR, Trast J, et al. . Developing a personal and social identity with type 1 diabetes during adolescence: a hypothesis generative study. Qual Health Res 2016;26:672–84. 10.1177/1049732316628835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Department of Health and Human Services. Victorian Admitted Episodes Dataset (VAED). 2015. http://www.health.vic.gov.au/hdss/vaed/ (Accessed 20 April 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.