Abstract
Objectives
To investigate the experiences of a digital management programme for hip and knee osteoarthritis (OA), including education and exercises as well as an option to chat with an assigned physical therapist for feedback, questions and support.
Setting
This study was conducted at a regional hospital in the southern part of Sweden.
Methods
Nineteen patients (10 women), median age of 66 (q1–q3, 57–71) years, with confirmed hip or knee OA were interviewed after completing their first 6 weeks in the programme, using a semistructured interview guide. The interviews were transcribed verbatim and were qualitatively analysed using systematic text condensation.
Results
Three categories emerged during the interviews:
(1) Management options for mitigating the consequences of OA; (2) Experiences of the digital programme and (3) Perceived effects of the digital programme over time. The participants had mostly positive experiences of the programme. Particularly important for these experiences were no waiting list, the flexibility of taking part in the programme with regards to location and time and the possibility to have daily contact with a physical therapist. These aspects were also emphasised as advantages compared with traditional care.
Conclusions
Digital management of OA, including education and exercise, was experienced as a valid alternative to traditional treatment in enabling the implementation of OA guidelines in a wider community. Easy access, exercising at one’s own convenience, flexible options, daily follow-up and support by a physical therapist were mentioned as the most important features. In addition, the results will contribute to further development and improvement of digital OA management programmes.
Keywords: e-health, digital management, osteoarthritis
Strengths and limitations of this study.
Participants were purposefully selected, including both sexes, who differed in age, osteoarthritis severity and physical function to have rich and varied data, when synthesising shared patterns across cases.
The use of a systematic text condensation analysis method facilitated cross-case synthesis of text and meaning.
Conducting the interviews via telephone may have resulted in less depth of the interviews due to a loss of visual input, but also allowed inclusion of participants from a wide geographic area.
Background
Due to a combination of decreasing healthcare resources, long waiting lists and difficulty to meet the demands of the modern individual who often has a busy schedule, the use of web-based or digital management options in healthcare has increased significantly during the last decade.1–3 Accessibility and flexibility, social motives and an option for anonymity and confidentiality are common arguments for choosing digital options.4–10 A recent review also suggests that it may be easier to seek care and to incorporate the training into daily life when it is accompanied by the flexibility and anonymity that online delivery provides, and that some people even rated their relationship with the online therapist higher than their relationship with their ordinary therapist.6 However, web-based or digital management for musculoskeletal disorders have thus far not been studied to any great extent.11
Individuals with osteoarthritis (OA) constitute one group of patients for whom digital management may be highly beneficial.4 11 As concluded previously in various literature, the guidelines for OA treatment (education, exercise and weight management)12 are not always implemented and few individuals with OA receive adequate management.4 13 14 Lack of healthcare resources, living in rural areas and having a lower level of education are all factors that may reduce the likelihood of receiving appropriate information on management options for OA.4 14 Web-based or digital interventions for OA have been suggested as a way to make the availability of guideline-based OA management accessible to a wider community.4 11 15 Unlike in patients with inflammatory arthritis where digital management does not seem to increase physical activity or quality of life,16 a few studies have shown promising results of digital interventions on physical activity,17 pain and physical function in patients with hip or knee OA.11 15 18–20
Joint Academy19 21 22 was developed in Sweden and is a digital version of the evidence-based face-to-face self-management programme Better Management of Patients with OsteoArthritis (BOA).13 23 The programme, as thoroughly described previously,19 comprises OA education (instructional videos on OA, physical activity and weight management), individualised neuromuscular exercises with increasing difficulty aiming at improving lower extremity strength and neuromuscular control and an option to chat asynchronously with an assigned physical therapist for feedback and questions. Studies have shown that completing the introduction phase of 6 weeks in this digital OA management programme reduces pain and medication intake, increases physical function and walking ability and reduces the willingness for surgery.18 19 24 However, patient experience of digital management for OA has not yet been evaluated. This knowledge may help to further improve digital management options for OA and to facilitate the implementation of OA guidelines in a wider community. Thus, the aim of this qualitative study was to investigate the patients’ experiences of using a digital management programme for hip and knee OA.
Methods
Patient and public involvement statement
The Joint Academy treatment programme for OA is based on the evidence-based BOA concept.13 In addition to the interviews in the present study, the digital platform has previously been further developed and improved by analysing questionnaires and opinions from patients recruited via the Swedish Rheumatism Association. These patients were able to test Joint Academy and were extensively interviewed about their opinions. All other aspects of this research were performed without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Setting and sampling
This study was conducted at a regional hospital in the southern part of Sweden. From a total sample of 462 individuals who had completed 6 weeks in the digital OA management programme between 2015 and 2018, 73 invitations with written information about the study were sent out by email by the first author (AC). The inclusion criterion was clinical hip or knee OA, previously confirmed or diagnosed according to the American College of Radiology criteria25 26 by an orthopaedic surgeon involved in the programme. The exclusion criteria were the following: (1) reporting other joints than hip or knee as the primary joint for OA symptoms and (2) not understanding and/or speaking Swedish. The participants were purposefully selected to represent both sexes, different age groups, perceived pain and physical function.27 Twenty-one participants accepted the invitation to participate in this study. Two were excluded as one did not speak Swedish and one did not return our phone calls. Ten women and nine men, median age of 66 (q1–q3, 57–71) years were consecutively included in the study. Their primary OA joint location was either in the knee (48%) or hip (52%) (see table 1 for participant characteristics). All participants in this study completed the programme via stationary computers, laptops or mobile phones.
Table 1.
Characteristics of the participants
| Characteristics | n=19 |
| Age mean (minimum–maximum) | 65 (45–80) |
| Sex | |
| Women, n | 10 |
| Men, n | 9 |
| Retired, n | 10 |
| OA location | |
| Hip, n | 10 |
| Knee, n | 9 |
| Pain baseline (minimum–maximum) | 6.1 (1–9) |
| Physical function baseline (minimum–maximum) | 8.6 (1–14) |
| EQ-5D-3L index baseline (minimum–maximum) | 0.59 (0.29–0.76) |
| Activity in the programme mean % (minimum–maximum) | 80.7 (19–93) |
Pain was assessed with the Numeric Rating Scale from 0 to 10, where 0 indicate no pain with higher numbers indicating more severe pain; physical function was assessed using the 30 s Chair Stand Test reflecting the number of repetitions of sitting to standing from a chair during a period of 30 s; a higher EQ-5D-3L index indicates better health-related quality of life. Activity level was defined as the proportion of completed videos, exercises and questionnaires offered in the programme.
EQ-5D-3L, EuroQol–five-dimension descriptive system assessing health-related quality of life; OA, osteoarthritis.
Data collection
The interviews were conducted by two of the authors (JE, physical therapy student, and AC, physical therapist and PhD), as face-to-face interviews, by Skype or by telephone, depending on the participant’s location and access to Skype. The semistructured interview guide included areas of interest such as (1) experiences of living with OA, (2) prior experiences of OA management, (3) experiences of the digital management programme (eg, set-up, educational contents, feedback, feed-forward, availability and design) and (4) experiences of factors that may have increased their motivation, persistence and emotional reactions. In addition, the participants were asked to suggest possible improvements to the programme. Follow-up questions were used to encourage the participants to elaborate on the subject and to explain or clarify the meaning and consequences of their experiences. The interview guide and follow-up questions were pilot tested on three older individuals with OA, not included in the study and was then subjected to minor editing. The two interviewers completed basic training in interview technique prior to data collection and had no relation to the participants in this study. The interviews, which lasted approximately 30–40 min, were recorded and transcribed verbatim. Data collection stopped when no further information was added, that is, the interviews did not add any new information to the results. See online appendix 1 for interview guide.
bmjopen-2018-028388supp001.pdf (263.1KB, pdf)
Data analysis
The transcripts were analysed using systematic text condensation (STC) according to Malterud,28 which is based on Giorgi’s phenomenological analysis.29 The procedure of the analysis consists of the following steps: (1) creating an overall impression and identifying themes; (2) distinguishing and sorting meaning units to codes; (3) formulating the meaning of each code meaning and (4) synthesising the condensed meaning into descriptions and concepts (see online appendix 2 for examples). STC was chosen as the procedure facilitates cross-case synthesis of text and meaning.28 Consequently, in the first step, the interview transcripts were read to get a general impression of the whole and to identify primary themes. Then, meaning units were identified and formulated into codes that represented the core of the statements. During this phase, three of the authors (JE, AC and CSH) worked individually to identify as many perspectives and perceptions as possible in the material. Next, all authors worked together with the coded data to produce one set of data, extracting duplicates and data that were not relevant for the aim of the study. The coded data were then organised into subcategories, and the content of the meaning units of each category was re-examined. The meaning and representation of the data were formulated into aspects representing the content. Thereafter, the subcategories were organised into categories. To validate the categories and make sure that no important aspects had been overlooked, the clusters were referred back to the raw data, and read through once again by the authors. Finally, the recontextualised data were expressed as interpretations of the meaning of each category and representative quotes were selected for each category/subcategory.
bmjopen-2018-028388supp002.pdf (348KB, pdf)
Results
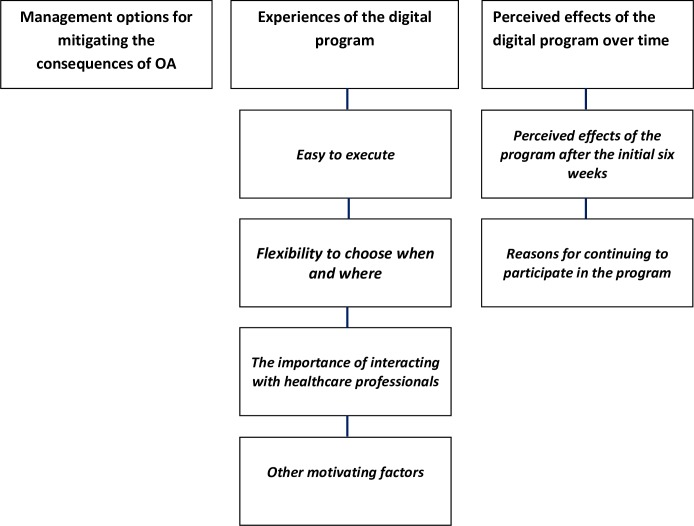
Three main categories were uncovered during the analysis:
Management options for mitigating the consequences of OA.
Experiences of the digital programme, with four subcategories: (1) Easy to execute, (2) Flexibility to choose when and where, (3) The importance of interacting with healthcare professionals and (4) other motivating factors.
Perceived effects of the digital programme over time, with two subcategories: (1) Perceived effects of the programme after the initial 6 weeks and (2) Reasons for continuing to participate in the programme (figure 1).
Figure 1.
Overview of the categories and subcategories describing the participants’ experiences of the digital. OA, osteoarthritis.
Participants’ suggestions for improving the digital programme were also analysed.
Management options for mitigating the consequences of OA
This category entailed the experiences of the perceived consequences of OA leading to the patients’ eager search for a cure that would reduce their symptoms. All participants described symptoms such as pain, disrupted sleep, deteriorating ability to walk, being immobile and activity limitations. Pain was the main motivation for seeking professional management. The participants also found that their decreased functioning was not only affecting themselves but was also a burden on their partners and family. They were trying all sorts of ways to ease the pain and to regain motor function. They were eager to try any treatment hoping that the programme could reduce their symptoms and improve their quality of life.
I felt that it was impossible to continue in this way as I was in such intense pain … (I18)
… you know … I wasn’t able to go downtown without thinking about how I would get back home again, when it was at its worst. I was also considering having surgery and other options, but only to get better. I was feeling really bad … (I12)
You take every chance for improvement that you get. In the end you know it’ll be beneficial.(I3)
Experiences of the digital programme
This category includes four subcategories: (1) Easy to execute, (2) Flexibility to choose when and where, (3) The importance of interacting with healthcare professionals and (4) Other motivating factors. In general, the participants’ experiences of the programme were positive. They found the programme very easy to execute, flexible and motivational. The interaction with the physical therapist was described as important for support and encouragement.
Easy to execute
Most participants were satisfied with the set-up of the programme. The programme was perceived as structured, educational and very simple to execute. Other elements that facilitated participation were instructional videos, email reminders, and that the exercises were individually customised with increasing difficulty but also quickly accomplished.
This is such a great set-up. Not only the exercises, it’s really educational and you learn what osteoarthritis is really about. (I13)
I found it really easy to follow. It does not take long and it’s really good to receive these reminders by email (I18)
However, a few participants perceived some difficulties in understanding how the programme worked. They found that the progression of the exercises was not clearly described or that it was difficult to understand specific words used in the videos.
To me it was hard to follow in the beginning and it actually took some time before I understood it correctly. It took like a few weeks until I really got the system. And that was a pity I think. (I8)
Flexibility to choose when and where
All participants acknowledged the flexibility that was associated with this digital management programme. The ability to execute the exercises at home or at any place at any time without any use of equipment was highly appreciated. The ability to control the time point for when to perform the exercises and not having to make a scheduled appointment at a specific location was described as an advantage compared with traditional management, and was further expressed as time-saving and less stressful since participants did not have to take time off from work for OA management. One participant even expressed that she would never have completed such a programme if it had not been digital.
The flexibility, that I could decide on my own when to perform the exercises was really good. That I didn’t have any scheduled time point when I had to dress, go out, and at this exact time point meet a physical therapist. That I could decide on my own … (I11)
I don’t think this is bad at all, to have it on the internet like this. I would never have done it if it hadn’t been digital (I17)
Some participants described that there were long waiting-lists for traditional OA management in primary care and that the digital programme was, thus, a flexible alternative that they could start at once.
Yes, it was also like, there was such a long waiting list for primary care. So I thought … this … this I can start doing right away. (I10)
Importance of interacting with healthcare professionals
Receiving an OA diagnosis without any physical meeting was perceived as a bit awkward to some participants. Some concerns were revealed regarding the risk of missing serious diseases if the diagnosis was given by phone or internet.
It’s somewhat hard to give a diagnosis over the phone. You can do it, but it’s more difficult and you can miss things … there could have been a tumor there … (I14)
The majority of the participants had a very positive experience of the interaction with their online physical therapist. They described that they received fast responses to their questions, as well as information and encouragement, and that they often received feedback within a few hours. Some expressed that the engagement from their physical therapist was valuable for support and encouragement, especially if they experienced pain during the exercises. The daily contact with their physical therapist encouraged them to perform their exercises every day, which was also perceived as an advantage compared with traditional care management.
I think it’s excellent to have daily contact. I think it’s outstanding. That puts pressure on me to really do these exercises and to answer him [the physical therapist] and to give him an opportunity to give feedback and information about other things … You can’t go to a physical therapist every day, every day, every day. That won’t work. They won’t have time for me, they have others to take care of as well. (I12)
In contrast, some participants experienced the contact with their online physical therapist to be unsatisfactory or even non-existent. They described that it could take a week before they received any response, that the questions were only partly answered or that they received no answer at all. Continuous follow-up with feedback and encouragement on their performance in the programme was also lacking.
In the beginning they said that someone would get in touch with me on a regular basis and things like that. But this hasn’t happened as I expected (I9)
Other motivating factors
The daily email reminders were typically highlighted as a motivator since they ensured that participants did not forget about the exercises and pushed them to perform the activities every day. Improved OA symptoms and the measurement feedback system provided by the programme were other factors that were mentioned as contributing to the participants’ motivation to perform the exercises.
It was there, popped up in my email box every day. OK, today I’ll do this exercise … it was something that pushed me. That was good I think … I needed that. (I8)
Perceived effects of the digital programme over time
This category includes two subcategories: (1) Perceived effects of the programme after the initial 6 weeks and (2) Reasons for continuing to participate in the programme. The majority of the participants reported improved functioning and reduced pain. However, some people felt no improvements and that their symptoms were the same as before entering the programme. Many continued to participate in the program after the initial 6 weeks to maintain the positive improvements.
Perceived effects of the digital programme after the initial 6 weeks
Several participants experienced significant reductions in OA symptoms after completing the programme. Improvements commonly mentioned were reduced pain, increased flexibility and improved walking abilities. In many cases, the symptoms were still present but were perceived to have improved significantly, leading to increased quality of life and less focus on the disease. Many described that they had recommended the programme to friends and relatives suffering from hip or knee OA, since they were satisfied with the result and wished that more people could undergo the same management programme.
It has helped me fantastically. I don’t think I could have walked the way I do today if I hadn’t done this … I don’t think so … I think this program has had an absolute crucial role in the fact that I can manage my everyday life as well as I can now, even though I have quite big problems. (I2)
Not all participants perceived that they had reduced symptoms or improvements after 6 weeks in the programme. Some described that their symptoms were still the same or had initially improved, and then worsened with deteriorating physical function and increased pain. However, several of these participants still believed in the set-up despite not experiencing the results they wished for. This lack of positive results was attributed to a belief that they entered the programme too late, that is, that the exercises might have helped if they had started at an earlier stage of the disease or that the exercises may have slowed down the disease progression.
The sad thing is that even if I do these exercises, every day, every week, every month, every year … nothing happens … I don’t get any better. (I4)
It felt really good in the beginning. The reason that it didn’t help me is probably because I started too late. (I12)
Reasons for continuing to participate in the programme
Many continued to do their exercises after the 6-week evaluation. Perceived functional improvements and pain reduction as well as fear of the symptoms worsening were highly motivating factors for continuing to perform the exercises. Another reason was that it might help them to be well prepared for any upcoming surgery.
I believe in these exercises. I believe that exercise is good for osteoarthritis. I am convinced. And I think … if I stop doing this … then this terrible pain will start again. (I8)
On the other hand, reduced pain and scheduled surgery were described by some participants as reasons for not continuing the programme.
The pain was generally reduced … and then I did not feel as motivated as before so I quit doing the exercises … yes I did. Generally, in physical therapy, it’s hard to keep your motivation up if you don’t have a lot of pain. (I19)
I have met with my orthopedist and I’m scheduled for surgery … I feel that the end of this problem is near. That’s why I’m not performing the exercises as I should anymore. (I18)
Suggestions for improving the digital programme
The participants suggested a few possible improvements to the digital programme. For example, many experienced that there were too few exercises with little variation, and the exercises were perceived as somewhat monotonous after a while, especially if the participants were highly active in the programme, that is, carried out exercises several days a week. It was suggested that varying and/or adding more exercises would increase motivation to perform them.
In the end it became a bit boring since there were so few movements … so I added some extra on my own … It was a bit boring to do the same thing every day. (I14)
Some participants who were not satisfied with the communication with the online physical therapist suggested improved patient–physical therapist interaction using increased feedback and encouragement. Another suggestion included follow-ups by video calls or Skype to enhance feedback on the individual performance of specific exercises.
You could send a video via internet and the physical therapist will then check that you have performed the exercise and performed it correctly and correct you if you have performed it incorrectly. (I19)
Discussion
We sought to investigate participant experiences of a digital management programme for hip and knee OA. The majority of the participants reported improvements after the initial 6 weeks, such as reduced pain, increased mobility and a sense of improved quality of life. In general, the participants found that the programme was easy to execute. The flexibility of being able to perform the exercises anywhere and at any time point was highly appreciated. The daily contact with the physical therapist was considered very important and an advantage compared with traditional care and the participants felt that the support and encouragement they received was important to continue exercising. In addition, the participants suggested more variation in the exercises and follow-up by video-calls.
Despite international guidelines,12 many patients with hip and knee OA do not receive appropriate treatment and information regarding OA management options.4 13 14 Web-based or digital management programmes have been proposed as an option for facilitating the implementation of non-surgical treatment as they have the potential to reach more individuals in need of OA treatment.4 The participants in the current study were mostly positive to the set-up of the programme. Being able to perform the exercises whenever and wherever they desired, without needing to take time off from work, was described as valuable. Several participants also mentioned that the digital programme was something they could start doing right away instead of being put on a waiting-list. They also experienced the programme to be educational and they felt motivated by the daily email reminders and the feedback system that were provided by the programme. This result is in line with previous studies investigating patient perceptions of digital OA management, for example, through internet or telerehabilitation, where the participants experienced such programmes to be convenient and time-saving.30 31
Exercise is one of the cornerstones of OA management.12 However, the outcome of the OA management programme is highly dependent on adherence to the exercises. People with OA is reported to be among those with particularly poor adherence to this type of treatment,32 although there seem to be good adherence to treatment delivered online in these patients.33 A recent systematic review of people with hip and knee OA identified factors such as increased knowledge of the disease and benefits of exercise, reduced symptoms, easy access to training facilities and the ability to fit the exercises into daily life as facilitating exercise participation, whereas long travel time and parking difficulties were considered as barriers.34 The results from the current study indicate that a digital programme may facilitate participation in OA management programmes and eliminate some of the barriers associated with exercise participation, such as access and time constrains, and further highlight the importance of adequate information and education regarding the benefits of exercise and different treatment options in OA. There were, however, some contrasting experiences of the digital programme, mostly related to perceived symptom improvement and contact with the physical therapist. Future quantitative investigations may reveal if such differences are related to adherence, that is, activity level in the programme. Previous research conclude that including behavioural change techniques may increase adherence to exercise35 and a digital delivery may enable the patients to continue their treatment week after week to further improvements and to sustain their achieved behavioural change.
Previous research indicates that support and encouragement from healthcare staff are important factors in facilitating exercise participation in people with hip and knee OA.34 This was also reflected in the current study. Interaction with the physical therapist was another important aspect that was highlighted by the participants. Most participants had a positive experience of the contact with their assigned physical therapist and they were highly motivated by the daily contact and the support and encouragement that were provided. This result further emphasises previous findings that a strong therapeutic alliance can be established without meeting in person.36–38 However, some participants were not satisfied with the contact, which in turn lowered their motivation to perform the exercises. This may indicate that support and encouragement from the physical therapist are prerequisites for a satisfactory experience of a digital OA management programme.
In accordance with studies on telerehabilitation,30 31 some concerns were expressed in our interviews about being diagnosed online. A few patients were afraid that they may have been suffering from a more serious disease, such as cancer, and that a differential diagnosis may be difficult via the internet. It is, therefore, important to respond to these worries accordingly and provide the patients with information that explains that OA is primarily diagnosed by symptoms and signs without any use of radiography or laboratory equipment.39 Also, some participants wished to have follow-ups via video call to eliminate the risk of performing the exercises incorrectly. This is consistent with previous studies reporting that non-supervised home-based exercises can give rise to concerns regarding the correct performance of the exercises.5 31 40 Video calls may, thus, be one way to develop the programme further and to optimise the experiences of digital programmes without any physical meeting. However, the influence of video conversations needs further study.
The results confirmed the findings of previous studies, in that the participants reported that the most important results of the programme were improvements such as reduced pain, increased flexibility and improved walking abilities,18 19 which brought a sense of improved quality of life and less focus on the disease. Interestingly, reduced pain and being scheduled for surgery were two factors described as both facilitators and barriers to continuing in the programme. Some participants continued to exercise because they experienced that the programme had reduced their pain and they were afraid that the pain would come back if they stopped doing the exercises. In contrast, some felt that reduced pain was a reason to stop doing the exercises, as their motivation was lost when pain no longer was an issue. Likewise, some participants continued to exercise since they wanted to be ready and as fit as possible for a total joint replacement (TJR), whereas others quit doing the exercises when they were scheduled for TJR as they believed the surgery would solve their problems anyway. Presurgery exercise is known to improve outcomes such as length of hospitalisation, knee range of motion and physical function after total knee replacements41 and such information is, therefore, important to include in the educational material to facilitate recovery after any future TJRs in these patients.
One strength of this study is that the participants were purposefully selected, including both men and women who differed in age, OA severity, physical function and OA location (hip or knee) from different parts of Sweden. However, since the participants were located all over Sweden, the interviews were mostly conducted by telephone or via Skype. This approach may have resulted in less depth of the interviews due to a loss of visual input. Also, two of the participants completed the programme more than 1 year prior to the interviews, which may have influenced their recollection of the programme and thereby also the experiences expressed during the interviews. Another limitation may be that some demographic data of the participants, such as education level, previous experience of using digital applications and year of OA diagnosis were not recorded. This information may have increased the generalisability of the results.
Throughout the data analysis, reflexivity has been considered, that is, we have been aware that the pre-understanding that the authors may have as clinicians and researchers could affect the data, if one is not fully aware of previous experiences.42 All authors worked separately during the data processing and there were continuous discussions during the analysis aimed at eliminating possible influences of previous experiences, which helped us to stay neutral to the data. In addition, we have also presented a signature after each quotation to show the representation of our participants, and to add transparency and trustworthiness to our findings and interpretations of the data.
Conclusions
A digital management programme for OA, including education and exercise as well as an option to chat with an assigned physical therapist for feedback, questions and engagement, may be an alternative to traditional treatment and further facilitate the implementation of OA guidelines in a wider community. The participants had mostly positive experiences of the programme, the flexibility of the programme with regards to location and time. Regular and frequent contact with a physical therapist was deemed particularly important for a positive experience of the programme and was also emphasised as an advantage compared with traditional care. In addition, the result of this study will contribute to the further development and improvement of digital management for OA.
Supplementary Material
Footnotes
Contributors: AC contributed to the design of the study, conducted part of the interviews, was responsible for the analysis and interpretation of the data and was in charge of writing the manuscript. LED contributed to the conception and design of the study, contributed to the interpretation of the data and provided feedback on drafts of this paper. HN contributed to the conception and design of the study, contributed to the analysis and interpretation of the data and provided feedback on drafts of this paper. JE contributed to the conception and design of the study, conducted part of the interviews, contributed to the analysis and interpretation of the data and provided feedback on drafts of this paper. CSH contributed to the conception and design of the study, contributed to the analysis and interpretation of the data and provided feedback on drafts of this paper. All authors have read and approved the final manuscript.
Funding: This research was funded by Vinnova, Sweden’s Innovation Agency, by Governmental Funding of Clinical Research within the National Health Service (ALF), the Faculty of Medicine, Lund University and by Region Skåne.
Competing interests: HN is a physical therapist and part time consultant at Joint Academy and LED is the cofounder and Chief Medical Officer in the corporation behind the same programme.
Ethics approval: The Regional Ethical Review Board in Lund, Sweden (Dnr 2017/651; Dnr 2017/980) approved the study and all patients gave their written informed consent prior to participation.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Patient and public involvement: Obtained.
References
- 1. Olthuis JV, Watt MC, Bailey K, et al. . Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev 2016;3:Cd011565 10.1002/14651858.CD011565.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. van Beugen S, Ferwerda M, Hoeve D, et al. . Internet-based cognitive behavioral therapy for patients with chronic somatic conditions: a meta-analytic review. J Med Internet Res 2014;16:e88 10.2196/jmir.2777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Boogerd EA, Noordam C, Kremer JA, et al. . Teaming up: feasibility of an online treatment environment for adolescents with type 1 diabetes. Pediatr Diabetes 2014;15:394–402. 10.1111/pedi.12103 [DOI] [PubMed] [Google Scholar]
- 4. Li LC, Cott C, Jones CA, et al. . Improving Primary Health Care in Chronic Musculoskeletal Conditions through Digital Media: The PEOPLE Meeting. JMIR Res Protoc 2013;2:e13 10.2196/resprot.2267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Björk AB, Sjöström M, Johansson EE, et al. . Women’s experiences of internet-based or postal treatment for stress urinary incontinence. Qual Health Res 2014;24:484–93. 10.1177/1049732314524486 [DOI] [PubMed] [Google Scholar]
- 6. Verhoeks C, Teunissen D, van der Stelt-Steenbergen A, et al. . Women’s expectations and experiences regarding e-health treatment: A systematic review. Health Informatics J 2017:146045821772039 10.1177/1460458217720394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bidmon S, Terlutter R. Gender Differences in Searching for Health Information on the Internet and the Virtual Patient-Physician Relationship in Germany: Exploratory Results on How Men and Women Differ and Why. J Med Internet Res 2015;17:e156 10.2196/jmir.4127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Powell J, Inglis N, Ronnie J, et al. . The characteristics and motivations of online health information seekers: cross-sectional survey and qualitative interview study. J Med Internet Res 2011;13:e20 10.2196/jmir.1600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sánchez-Ortiz VC, House J, Munro C, et al. . "A computer isn’t gonna judge you": a qualitative study of users' views of an internet-based cognitive behavioural guided self-care treatment package for bulimia nervosa and related disorders. Eat Weight Disord 2011;16:e93–e101. 10.1007/BF03325314 [DOI] [PubMed] [Google Scholar]
- 10. Roettl J, Bidmon S, Terlutter R. What Predicts Patients' Willingness to Undergo Online Treatment and Pay for Online Treatment? Results from a Web-Based Survey to Investigate the Changing Patient-Physician Relationship. J Med Internet Res 2016;18:e32 10.2196/jmir.5244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pietrzak E, Cotea C, Pullman S, et al. . Self-management and rehabilitation in osteoarthritis: is there a place for internet-based interventions? Telemed J E Health 2013;19:800–5. 10.1089/tmj.2012.0288 [DOI] [PubMed] [Google Scholar]
- 12. Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg 2013;21:571–6. 10.5435/JAAOS-21-09-571 [DOI] [PubMed] [Google Scholar]
- 13. Thorstensson CA, Garellick G, Rystedt H, et al. . Better Management of Patients with Osteoarthritis: Development and Nationwide Implementation of an Evidence-Based Supported Osteoarthritis Self-Management Programme. Musculoskeletal Care 2015;13:67–75. 10.1002/msc.1085 [DOI] [PubMed] [Google Scholar]
- 14. Li LC, Sayre EC, Kopec JA, et al. . Quality of nonpharmacological care in the community for people with knee and hip osteoarthritis. J Rheumatol 2011;38:2230–7. 10.3899/jrheum.110264 [DOI] [PubMed] [Google Scholar]
- 15. Bossen D, Veenhof C, Van Beek KE, et al. . Effectiveness of a web-based physical activity intervention in patients with knee and/or hip osteoarthritis: randomized controlled trial. J Med Internet Res 2013;15:e257 10.2196/jmir.2662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Griffiths AJ, White CM, Thain PK, et al. . The effect of interactive digital interventions on physical activity in people with inflammatory arthritis: a systematic review. Rheumatol Int 2018;38:1623–34. 10.1007/s00296-018-4010-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berry A, McCabe CS, Muir S, et al. . Digital behaviour change interventions to facilitate physical activity in osteoarthritis: a systematic review. Physical Therapy Reviews 2018;23:197–206. 10.1080/10833196.2018.1470747 [DOI] [Google Scholar]
- 18. Nero H, Dahlberg J, Dahlberg LE. A 6-Week Web-Based Osteoarthritis Treatment Program: Observational Quasi-Experimental Study. J Med Internet Res 2017;19:e422 10.2196/jmir.9255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dahlberg LE, Grahn D, Dahlberg JE, et al. . A Web-Based Platform for Patients With Osteoarthritis of the Hip and Knee: A Pilot Study. JMIR Res Protoc 2016;5:e115 10.2196/resprot.5665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Smittenaar P, Erhart-Hledik JC, Kinsella R, et al. . Translating Comprehensive Conservative Care for Chronic Knee Pain Into a Digital Care Pathway: 12-Week and 6-Month Outcomes for the Hinge Health Program. JMIR Rehabil Assist Technol 2017;4:e4 10.2196/rehab.7258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joint Academy. [https://www.jointacademy.com/se/en/]
- 22. Nero H, Dahlberg JE. Dahlberg LE: Joint academy - a six-week online treatment program for osteoarthritis Osteoarthritis Research Society International (OARSI. Liverpool, England: Osteoarthritis and Cartilage, 2018. [Google Scholar]
- 23. Jönsson T, Ekvall Hansson E, Thorstensson CA, et al. . The effect of education and supervised exercise on physical activity, pain, quality of life and self-efficacy - an intervention study with a reference group. BMC Musculoskelet Disord 2018;19:198 10.1186/s12891-018-2098-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cronström A, Nero H, Dahlberg LE. Factors associated with patients' willingness to consider joint surgery after completion of a digital osteoarthritis treatment program: A prospective cohort study. Arthritis Care Res 2018. 10.1002/acr.23772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Altman R, Alarcón G, Appelrouth D, et al. . The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 1991;34:505–14. 10.1002/art.1780340502 [DOI] [PubMed] [Google Scholar]
- 26. Altman R, Asch E, Bloch D, et al. . Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986;29:1039–49. [DOI] [PubMed] [Google Scholar]
- 27. Patton M. Qualitative evaluation and research methods. 3rd edn Thousand Oaks, CA: Sage Publications, Inc, 2002. [Google Scholar]
- 28. Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health 2012;40:795–805. 10.1177/1403494812465030 [DOI] [PubMed] [Google Scholar]
- 29. Giorgi A. Phenomenology and psychological research. Pittsburgh, PA: Duquesne University Press, 1985. [Google Scholar]
- 30. Lawford BJ, Bennell KL, Hinman RS. Consumer Perceptions of and Willingness to Use Remotely Delivered Service Models For Exercise Management of Knee and Hip Osteoarthritis: A Cross-Sectional Survey. Arthritis Care Res 2017;69:667–76. 10.1002/acr.23122 [DOI] [PubMed] [Google Scholar]
- 31. Lawford BJ, Delany C, Bennell KL, et al. . "I was really sceptical… But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis Cartilage 2018;26:741–50. 10.1016/j.joca.2018.02.909 [DOI] [PubMed] [Google Scholar]
- 32. Pisters MF, Veenhof C, Schellevis FG, et al. . Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res 2010;62:1087–94. 10.1002/acr.20182 [DOI] [PubMed] [Google Scholar]
- 33. de Vries HJ, Kloek CJJ, de Bakker DH, et al. . Determinants of Adherence to the Online Component of a Blended Intervention for Patients with Hip and/or Knee Osteoarthritis: A Mixed Methods Study Embedded in the e-Exercise Trial. Telemed J E Health 2017;23:1002–10. 10.1089/tmj.2016.0264 [DOI] [PubMed] [Google Scholar]
- 34. Dobson F, Bennell KL, French SD, et al. . Barriers and Facilitators to Exercise Participation in People with Hip and/or Knee Osteoarthritis: Synthesis of the Literature Using Behavior Change Theory. Am J Phys Med Rehabil 2016;95:372–89. 10.1097/PHM.0000000000000448 [DOI] [PubMed] [Google Scholar]
- 35. Meade LB, Bearne LM, Sweeney LH, et al. . Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: Systematic review. Br J Health Psychol 2019;24:10–30. 10.1111/bjhp.12324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lingely-Pottie P, McGrath PJ. A therapeutic alliance can exist without face-to-face contact. J Telemed Telecare 2006;12:396–9. 10.1258/135763306779378690 [DOI] [PubMed] [Google Scholar]
- 37. Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: a randomized controlled clinical trial. BMC Psychiatry 2007;7:13 10.1186/1471-244X-7-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Muller I, Kirby S, Yardley L. The therapeutic relationship in telephone-delivered support for people undertaking rehabilitation: a mixed-methods interaction analysis. Disabil Rehabil 2015;37:1060–5. 10.3109/09638288.2014.955134 [DOI] [PubMed] [Google Scholar]
- 39. Abhishek A, Doherty M. Diagnosis and clinical presentation of osteoarthritis. Rheum Dis Clin North Am 2013;39:45–66. 10.1016/j.rdc.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 40. Cranen K, Drossaert CH, Brinkman ES, et al. . An exploration of chronic pain patients' perceptions of home telerehabilitation services. Health Expect 2012;15:339–50. 10.1111/j.1369-7625.2011.00668.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chen H, Li S, Ruan T, et al. . Is it necessary to perform prehabilitation exercise for patients undergoing total knee arthroplasty: meta-analysis of randomized controlled trials. Phys Sportsmed 2018;46:36–43. 10.1080/00913847.2018.1403274 [DOI] [PubMed] [Google Scholar]
- 42. Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet 2001;358:483–8. 10.1016/S0140-6736(01)05627-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-028388supp001.pdf (263.1KB, pdf)
bmjopen-2018-028388supp002.pdf (348KB, pdf)