Abstract
Purpose:
Contraceptive satisfaction may influence not only contraceptive use, but long-term engagement in care. We investigated the extent to which adolescent and young women’s desired contraceptive features are associated with their current contraceptive method, and if the presence of preferred features in their current method is associated with satisfaction.
Methods:
We performed a secondary analysis of a cross-sectional survey at 5 Northern California family planning clinics, including women ages 13-24. Descriptive statistics and multivariate logistic regression identified associations between desired features and sociodemographic characteristics. Multivariate logistic regression was used to examine associations between desired features and current contraceptive method, as well as the presence of desired features and satisfaction with current method.
Results:
Among 814 participants, the features most frequently rated “very important” included effectiveness (87%, N=685), safety (85%, N=664), and side effects (72%, N=562). Contraceptive feature preferences varied by age, race/ethnicity, intimate partner violence history, and sexually transmitted infection (STI) history. Having a preference for a specific contraceptive feature was not associated with using a method with that feature, except for STI prevention (aOR 1.59 CI [1.18-2.16]). However, respondents with preferences for effectiveness, partner-independence, or privacy who used methods that were congruent with their preferences were more likely to express satisfaction (aOReffectiveness 1.57 CI [1.03-2.37], aORpartner-indpendent 1.75 [1.03-2.96], and aORprivacy 1.81 [1.01-3.23]).
Conclusion:
Adolescent and young women have varied contraceptive preferences that are associated with demographics and reproductive health experiences. Adolescent and young women’s use of contraceptive methods that matched their preferences may improve satisfaction and engagement in care.
Keywords: Adolescents, reproductive health, contraception, patient preference, patient-centered, health disparities
Introduction
Contraceptive satisfaction is an important reason why women initiate, change, or discontinue contraceptive methods. Nearly half of women in the United States (US) report previously discontinuing a contraceptive method due to dissatisfaction [1]. In a study of adolescent and young women ages 15-24 initiating a hormonal contraceptive method, dissatisfaction with side effects was the most commonly reported reason for discontinuation [2]. Although most participants in this study (74%) switched to another method, both method discontinuation and method switching were associated with pregnancy [2].
Contraceptive satisfaction may be an important outcome not only due to its relationship with contraceptive use [3], but also as a meaningful endpoint in itself. Contraceptive satisfaction has been proposed as an important patient-centered outcome, reflecting women’s experiences of family planning care [4,5]. Particularly for adolescent and young women who may be especially encouraged to use long-acting reversible contraception (LARC) [6], and whose early experiences with reproductive healthcare may influence long-term engagement [7], understanding women’s satisfaction with their contraceptive method may facilitate improvements in both short and long-term reproductive health outcomes.
Use of shared decision making in contraceptive counseling may be one way to improve women’s satisfaction with their contraception [8]. In this approach, providers elicit women’s experiences and preferences, provide information about contraceptive options, and help individuals select methods that best meet their needs and values. In one study, the presence of shared decision making in counseling was associated with satisfaction with the chosen contraceptive method [8]. Conversely, in the same study, patients’ perceived provider preference for particular methods was associated with decreased method satisfaction, and younger women were more likely to report that their provider expressed preferences. Furthermore, qualitative studies describe how young Black and Hispanic women perceive subtle provider preferences for particular contraceptive methods, negatively affecting contraceptive use as well as future interactions with health care providers [9,10].
Assisting women with exploring their contraceptive preferences to identify a method that best aligns with those preferences is a key component of shared decision making, and may facilitate women’s satisfaction with their contraceptive methods. However, few studies examine adolescent and young women’s contraceptive preferences, if those preferences align with their contraceptive methods, and their contraceptive method satisfaction. Although one study examined differences in alignment between contraceptive preferences and planned contraceptive method in women as young as fifteen, the variable of interest was planned rather than current method of contraception [11]. This study aims to examine, in adolescent and young women, associations between (1) sociodemographic characteristics and desired contraceptive features; (2) desired contraceptive features and current contraceptive method; and (3) use of method with desired contraceptive features and contraceptive method satisfaction.
Methods
This study is a secondary analysis using data from a previously described cross-sectional survey [12]. The study team recruited participants ages 13-45 in waiting rooms of five family planning clinics in Northern California in 2015-2016. Eligibility criteria for the parent study included individuals who self-identified as women and were English or Spanish speaking, seeking family planning care, and reported negative or unknown HIV status. Participants provided verbal consent. The University of California San Francisco Institutional Review Board approved the study.
Participants self-administered an anonymous, tablet-based survey about demographics, sexual and reproductive health history, contraceptive preferences, current contraceptive method (defined as method(s) in use prior to the visit), and satisfaction with their current method. Prior to distributing the final survey, cognitive testing was performed during which participants described their understanding of questions and responses; the survey was iteratively modified based on feedback. In the final survey, participants identified preferences regarding fifteen contraceptive features: cost, convenience, safety, side effects, effectiveness, other health benefits, sexually transmitted infection (STI) prevention, partner preferences, religious beliefs, partner-independence, privacy, ability to use without going to a doctor or clinic, recommendation of a friend, provider recommendation, and a field to describe other features. Women rated each feature on a 4-point Likert-like scale as “not important at all,” “somewhat not important,” “somewhat important,” or “very important.”
In this sub-study, we limited analyses to participants ages 13-24 who reported ever having vaginal sex with a male partner. We chose the upper age limit based on a definition of adolescence as the developmental period of transition up to age 24 [13]. To make comparisons between age groups, we use the term “adolescents” when referring to participants ages 13-19 and “young adults” when referring to participants ages 20-24. When grouping participants by contraceptive method, we defined dual-method use as using condoms plus an intrauterine device (IUD), implant, injectable, pill, patch, ring or sterilization. Finally, we refer to emergency contraception (EC) only as pill formulations and exclude copper IUDs.
To answer the primary study question of whether participant preferences matched current contraceptive characteristics, our analyses focused on five features: effectiveness, STI prevention, partner-independence, privacy, and ability to use without going to a doctor or clinic. We identified these characteristics as ones for which we could more objectively determine a match between participants’ contraceptive method and preference(s). Specifically, we defined methods that matched a preference for effectiveness as use of an IUD, implant, sterilization, injectable, pill, patch, or ring based on pilot testing of the survey exploring women’s understanding of “effectiveness” and because these methods have an effectiveness of at least 90% [14]. We defined methods that matched a preference for STI prevention as any condom use in the last month. We defined methods that matched a preference for privacy as use of an IUD, implant, female sterilization, injectable, or EC. We defined methods that matched a preference for partner-independence as use of an IUD, implant, female sterilization, injectable, pill, patch, ring, diaphragm, or EC. Lastly, we defined methods that matched a preference for ability to use the method without going to a doctor or clinic as use of condoms, EC (participants could go to a pharmacy and obtain it without a prescription), fertility awareness-based methods, or withdrawal. Because some of these categories may be defined in different ways (for example, effectiveness may be defined to only include highly effective methods such as the IUD, implant or sterilization), we performed additional analyses using a narrower definition of effectiveness (only use of an IUD, implant or sterilization). We also conducted analyses expanding the list of methods defined as “private” to include the pill or ring, given some women may define these methods as “private.”
We used Pearson’s chi-squared test for bivariate analysis of sociodemographic variables and rating of contraceptive features as “very important.” In multivariate logistic regression analysis of contraceptive preferences, we planned a priori to adjust for age, race/ethnicity, education, currently in school or working, ever pregnant, stable housing, history of an STI, and history of intimate partner violence (IPV) based on prior research findings [11,15-17]. Variables associated with rating a feature “very important” in bivariate analysis with a p-value ≤ 0.1 were also included in adjusted models. Household income was not evaluated as a potential covariate as it is often inaccurately reported by teens [18].
We performed multivariate logistic regression to assess associations between rating a feature “very important” and use of a current method with that feature, defining both as binary variables and adjusting a priori for age, race/ethnicity, education, currently in school or working, ever pregnant, history of IPV, and history of STI based on literature review [19,20]. Among adolescent and young women with a strong preference for a feature, we examined associations between current use of a contraceptive method matching this preference and satisfaction with current contraceptive method, defining both as binary variables and a priori adjusting for age, race/ethnicity, education, and currently in school or working based on literature review [3, 21-25]. For covariates in the models, we defined race/ethnicity and education as categorical, and remaining covariates as binary. We defined statistical significance for multivariate analyses as p≤0.05.
Results
Out of 2,389 women approached in the overall study, 271 declined participation and 149 were ineligible. Of the 1,969 women who completed surveys, 814 met eligibility criteria for this sub-analysis.
One third of respondents in this sub-study were adolescents (ages 13-19) and two thirds were young adults (ages 20-24, Table 1). Forty-one percent (N=336) identified as Hispanic, 24% identified as Black (N=199), 20% identified as Asian (N=160), and 15% identified as White (N=119). The majority (81%, N=661) lived in households with a self-reported total income less than $60,000 per year, and 7% (N=55) endorsed unstable housing.
Table 1.
Sociodemographic and reproductive health characteristics of 13-24 year old women who are sexually active with men (N=814)
| Characteristic | N (%) |
|---|---|
| Sociodemographic characteristics | |
| Age | |
| 13-19 years old | 272 (33) |
| 20-24 years old | 542 (67) |
| Race/ethnicity | |
| White | 119 (15) |
| Black | 199 (24) |
| Hispanic | 336 (41) |
| Asian | 160 (20) |
| Cisgender | 794 (98) |
| Completed high school/GED or less | 498 (61) |
| Currently in school | 258 (32) |
| Currently employed (part or full time) | 327 (40) |
| Household income <$60,000 | 661 (81) |
| English is primary language | 603 (74) |
| Has a primary care provider | 456 (56) |
| Only access reproductive health care1 | 218 (27) |
| Stable housing | 727 (89) |
| Reproductive Health | |
| Sexually active in last 6 months | 785 (96) |
| Ever had anal sex | 280 (34) |
| Ever pregnant | 344 (42) |
| Ever had a sexually transmitted infection2 | 232 (29) |
| Ever experienced intimate partner violence | 170 (21) |
| Ever threatened over condom negotiation | 49 (6) |
| Ever exchanged sex | 23 (3) |
| Current contraceptive method(s) | |
| IUD3 | 86 (11) |
| Implant3 | 54 (7) |
| Sterilization3 | 2 (0.3) |
| Pill3 | 169 (21) |
| Ring3 | 18 (2) |
| Patch3 | 25 (3) |
| Injectable3 | 109 (13) |
| Condoms4 | |
| Condoms exclusively | 185 (23) |
| Condoms + IUD, implant, pill, ring, patch, or injectable | 153 (19) |
| Condoms + withdrawal or rhythm method | 47 (6) |
| Condoms + emergency contraception | 10 (1) |
| Diaphragm3 | 3 (0.4) |
| Withdrawal/rhythm method3 | 102 (13) |
| Emergency contraception3 | 46 (6) |
| No method | 93 (11) |
Answered affirmatively to either of the following statements: “I ONLY see a doctor when I’m pregnant” or “I ONLY see a doctor at the time of my birth control visit”
Sexually transmitted infections included history of chlamydia, gonorrhea, syphilis, trichomonas, herpes, molluscum, genital warts/human papilloma virus (HPV), hepatitis B, or hepatitis C. All participants had negative or unknown HIV status based on eligibility criteria.
Using this method exclusively or with another method.
Any condom use within the last month.
IUD: intrauterine device. GED: General education development test
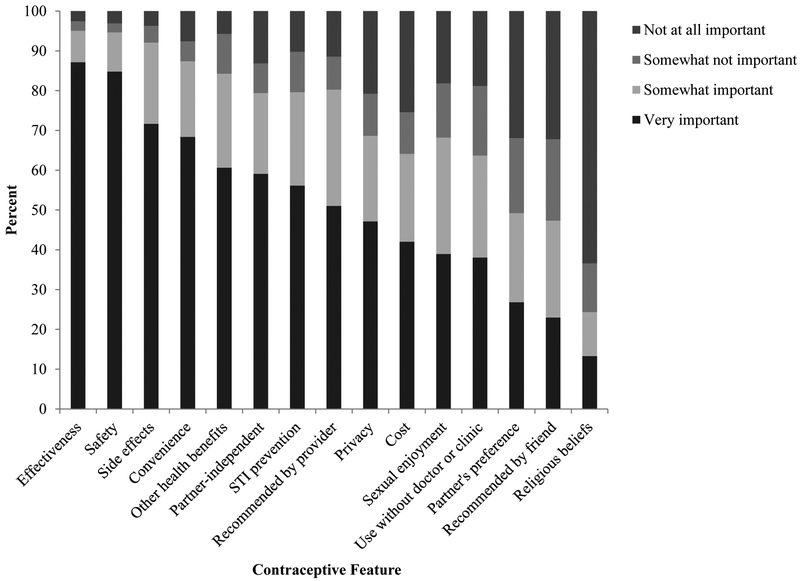
The contraceptive features rated “very important” by the largest proportion of participants included effectiveness (87%, N=685), safety (85%, N=664), and having few or no side effects (72%, N=562; Figure 1). When grouped by current contraceptive method, strong preferences for specific characteristics generally correlated with the characteristic of the method (Figure A1). For example, almost 90% of LARC users valued effectiveness, and a large proportion of condom users and dual method users valued STI protection (Figure A1).
Figure 1.
Contraceptive features by importance to adolescent and young women
STI: sexually transmitted infection
In multivariate analyses, we found age, race, history of IPV, or history of an STI were associated with features of contraceptive methods that participants considered “very important” (Table 2). Specifically, adolescent and young women who were Black, Hispanic, or Asian were significantly more likely than White women to rate STI prevention and privacy as very important (STI prevention: aORBlack 2.70 CI (1.60-4.55), aORHispanic 2.52 CI (1.54-4.11), aORAsian 2.20 CI (1.29-3.76); Privacy: aORblack 4.85 CI (2.75-8.58), aORHispanic 3.22 CI (1.88-5.51), aORAsian 2.79 CI (1.57-4.98)). In addition, Black and Hispanic women were more likely to consider ability to use a method without a doctor or clinic as very important (aORblack: 2.22 CI [1.28-3.84], aORHispanic: 1.96 CI [1.18-3.24]). Compared to teens, young adults were more likely to rate partner independence (aOR 1.89 CI [1.31-2.73]), few or no side effects (Table A1: aOR: 2.07 CI [1.41-3.05]), convenience (Table A1: aOR 1.49 CI [1.02-2.17]), and other health benefits (Table A1: aOR 1.58 CI [1.09-2.29]) as very important. Finally, adolescent and young women with a history of IPV were significantly more likely to rate partner independence as very important (aOR 1.58 CI [1.07-2.33]), while participants with a history of an STI were less likely to consider STI prevention (aOR 0.64 CI [0.45-0.90]) and privacy (aOR 0.66 CI [0.46-0.94]) as very important (Table 2).
Table 2.
Contraceptive method feature preferences reported to be “very important” by sociodemographic and reproductive health characteristics
| Strongly Desired Feature | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Effectiveness (N=685) |
STI prevention (N=435) |
Partner-independent (N=454) |
Privacy (N=361) |
Use without doctor or clinic (N=291) |
||||||
| OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | |
| Sociodemographic | ||||||||||
| Age | ||||||||||
| 13-19 | Reference | Reference | Reference | Reference | Reference | Reference | Reference | |||
| 20-24 | 1.42 (0.92-2.17) | 1.21 (0.90-1.63) | 1.92 (1.42-2.60)* | 1.89 (1.31-2.73) | 0.99 (0.73–1.33) | 1.38 (1.01-1.89)* | 1.36 (0.94-1.97) | |||
| Race/ethnicity | ||||||||||
| White | Reference | Reference | Reference | Reference | Reference | Reference | Reference | Reference | ||
| Black | 0.59 (0.29-1.21) | 2.52 (1.55-4.08)* | 2.70 (1.60-4.55) | 0.99 (0.61-1.60) | 4.52 (2.66-7.70)* | 4.85 (2.75-8.58) | 2.36 (1.41-3.96)* | 2.22 (1.28-3.84) | ||
| Hispanic | 0.78 (0.40-1.54) | 2.69 (1.73-4.20)* | 2.52 (1.54-4.11) | 0.97 (0.63-1.51) | 3.59 (2.19-5.90)* | 3.22 (1.88-5.51) | 1.98 (1.22-3.22)* | 1.96 (1.18-3.24) | ||
| Asian | 1.11 (0.50-2.46) | 2.27 (1.38-3.73)* | 2.20 (1.29-3.76) | 0.93 (0.57-1.52) | 3.02 (1.75-5.21)* | 2.79 (1.57-4.98) | 1.64 (0.96-2.82)* | 1.70 (0.97-2.96) | ||
| Completed high school/GED or less | 0.52 (0.32-0.85)* | 0.72 (0.41-1.25) | 1.00 (0.75-1.35) | 0.62 (0.45-0.84)* | 0.88 (0.61-1.26) | 1.08 (0.81-1.46) | 0.94 (0.69-1.27) | |||
| In school or working | 1.94 (1.23-3.06)* | 1.53 (0.93-2.50) | 0.90 (0.64-1.27) | 1.42 (1.01-2.00)* | 1.25 (0.86-1.80) | 0.91 (0.65-1.27) | 1.13 (0.79-1.61) | |||
| Stable housing | 1.89 (0.94-3.81)* | 1.45 (0.70-3.01) | 1.32 (0.76-2.30) | 1.41 (0.81-2.45) | 1.10 (0.63-1.93) | 1.10 (0.62-1.98) | ||||
| English is primary language | 1.11 (0.68-1.79) | 0.68 (0.48-0.95)* | 0.79 (0.54-1.18) | 0.92 (0.66-1.29) | 0.71 (0.51-0.98)* | 0.76 (0.51-1.11) | 0.81 (0.58-1.13) | |||
| Reproductive Health | ||||||||||
| Ever experienced IPV | 1.12 (0.66-1.88) | 0.73 (0.52-1.03)* | 0.80 (0.56-1.16) | 1.67 (1.15-2.41)* | 1.58 (1.07-2.33) | 1.21 (0.86-1.72) | 0.97 (0.68-1.38) | |||
| History of STI | 0.65 (0.42-1.01)* | 0.67 (0.41-1.10) | 0.69 (0.50-0.95)* | 0.64 (0.45-0.90) | 0.77 (0.56-1.06) | 0.76 (0.55-1.04)* | 0.66 (0.46-0.94) | 0.94 (0.68-1.30) | ||
CI: confidence interval; GED: General education development test; IPV: intimate partner violence; STI: sexually transmitted infection.
p≤0.1, with p-values calculated using a chi-squared test examining the proportion of young women rating each feature “very important.”
Bolded values are p≤0.05 with p-values calculated using logistic regression adjusting for age, race/ethnicity, education, currently in school or working, stable housing, ever pregnant, history of IPV, and history of STI.
In multivariate analyses assessing for association between rating a feature as “very important” and current use of a method matching that feature, only desiring STI prevention was associated with using a method that fit that description – in this case, using condoms (Table 3, aOR 1.59 CI [1.18-2.16]). The association between desired effectiveness and use of an effective contraceptive method was not statistically significant, and remained so when analyses were repeated with a narrower definition of effective method use (IUD, implant, or sterilization).
Table 3.
Use of a contraceptive method congruent with strongly desired contraceptive features
| Using a contraceptive method that fits preference | ||||
|---|---|---|---|---|
| Desired feature | OR (95% CI) | p-value | aOR6 (95% CI) | p-value |
| Effectiveness1 | 1.21 (0.76-1.92) | 0.42 | ||
| STI prevention2 | 1.59 (1.20-2.12) | 0.001* | 1.59 (1.18-2.16) | 0.003 |
| Partner independence3 | 1.10 (0.80-1.53) | 0.56 | ||
| Privacy4 | 1.32 (0.97-1.79) | 0.08* | 1.16 (0.83-1.62) | 0.38 |
| Can use without going to doctor or clinic5 | 1.08 (0.78-1.49) | 0.64 | ||
Strongly desired contraceptive features refer to those preferences that participants denoted as “very important” features to have in a contraceptive method. aOR: adjusted odds ratio; CI: confidence interval; STI: sexually transmitted infection; IUD: intrauterine device
Any use of an IUD, implant, sterilization, ring, pill, patch, or injectable (N=436).
Any use of condoms (N=384).
Any use of an IUD, implant, sterilization, injectable, ring, patch, pill, diaphragm, or emergency contraception (N=466).
Any use of an IUD, implant, injectable, sterilization, or emergency contraception (N=285).
Any use of condoms, emergency contraception, rhythm method, or withdrawal (N=438).
Adjusted for age, race/ethnicity, education, currently in school or working, ever pregnant, history of IPV, and history of STI.
p≤0.1
Bolded values: p≤0.05
However, adolescent and young women’s satisfaction with their contraceptive method was frequently associated with having a match between their preference and current contraceptive method (Table 4). Specifically, adolescent and young women using a contraceptive method that was consistent with their preferences for effectiveness (aOR 1.57 CI [1.03-2.37]), partner independence (aOR 1.75 CI [1.03-2.96]), or privacy (aOR 1.81 CI [1.01-3.23]) had increased odds of reporting contraceptive satisfaction (Table 4). When a narrower definition of effectiveness was used, this association remained true in univariate analyses (OR 1.91 CI [1.14-3.20]) and multivariate analyses (aOR 1.93 CI [1.13-3.29]). When we expanded the definition of methods meeting a preference for privacy to also include the pill or ring, the association between using a method that was consistent with a preference for privacy was no longer statistically significant in univariate analyses (OR 1.46 CI [0.84-2.54]).
Table 4.
Satisfaction among adolescent and young women whose current contraceptive method includes strongly desired contraceptive features
| Satisfaction, given method fits preference | ||||
|---|---|---|---|---|
| Method matches preference for feature | OR (95% CI) | p-value | aOR6 (95% CI) | p-value |
| Effectiveness1 | 1.49 (1.00-2.23) | 0.05* | 1.57 (1.03-2.37) | 0.03 |
| STI prevention2 | 1.04 (0.63-1.70) | 0.89 | ||
| Partner independence3 | 1.68 (1.01-2.79) | 0.04* | 1.75 (1.03-2.96) | 0.04 |
| Privacy4 | 1.88 (1.09-3.24) | 0.02* | 1.81 (1.01-3.23) | 0.05 |
| Can use without going to doctor or clinic5 | 0.82 (0.45-1.49) | 0.51 | ||
Strongly desired contraceptive features refer to those preferences that participants denoted as “very important” features to have in a contraceptive method aOR: adjusted odds ratio; CI: confidence interval; STI: sexually transmitted infection
Any use of an IUD, implant, sterilization, ring, pill, patch, or injectable (N=436).
Any use of condoms (N=384).
Any use of an IUD, implant, sterilization, injectable, ring, patch, pill, diaphragm, or emergency contraception (N=466).
Any use of an IUD, implant, injectable, sterilization, or emergency contraception (N=285).
Any use of condoms, emergency contraception, rhythm method, or withdrawal (N=438).
Adjusted for age, race/ethnicity, education, and currently working or in school.
p≤0.1
Bolded values: p≤0.05
Discussion
Among a racially and ethnically diverse sample of sexually-active adolescent and young women presenting for family planning care in Northern California, we found that participants had multiple and varied preferences for contraceptive features. Participants’ preferences varied by race/ethnicity, age group, history of IPV, and history of STI. Preferences also differed qualitatively by type of contraceptive method used. In multivariate analyses, only adolescent and young women with a strong preference for STI prevention had increased odds of using a method congruent with their preferences. However, adolescent and young women whose current contraceptive method matched their preference for effectiveness, partner independence, or privacy had increased odds of satisfaction with their method.
We found that Black, Hispanic, and Asian participants were more likely than White participants to rate STI prevention and privacy as very important, with Black and Hispanic participants additionally rating ability to use a method without going to a doctor or clinic as very important. These results are consistent with prior studies suggesting that Black and Hispanic women are more likely than White women to consider STI prevention as very important [11,26], and are contextualized by striking racial/ethnic disparities in STI prevalence among adolescent and young women in the US [27]. Jackson also found that Black women were more likely than White women to want to use a method without going to a doctor or clinic, and concluded that women of color’s valuing contraceptive features related to patient control may reflect broader historical contexts of reproductive abuses in the US [11]. Together, these findings highlight the lack of methods that meet the needs of adolescent and young women of color for STI prevention, privacy, and use without attending a clinic.
We also found that in comparison with adolescents, young adults were more likely to rate partner independence, few or no side effects, convenience, and other health benefits as very important. A qualitative study of women ages 18-24 found that contraceptive decision making was an iterative process with most respondents using multiple forms of contraception at different times in their lives and frequently re-evaluating contraceptive decisions in the context of relationships, pregnancies and personal values [28]. We hypothesize that over time, adolescent and young women may learn more about and experience contraceptive options, including potential side effects and health benefits of various methods and/or pressure from partners. These experiences, as well as changing life circumstances and priorities, may lead to stronger preferences for certain features.
A notable proportion of participants in this study reported a history of IPV, consistent with a prior study of a similar population which demonstrated that sexual and reproductive violence and reproductive control are common among adolescent and young women attending family planning clinics [29]. Participants with a history of IPV were more likely to express strong preferences for methods that could be used independent of partners, which is consistent with research demonstrating a history of violence is associated with decreased condom or oral contraceptive use [30]. Together, these data suggest how trauma history may affect adolescent and young women’s contraceptive preferences and use, and reinforce the importance of equipping staff to provide trauma-informed care in family planning settings [31].
A significant proportion of respondents reported a history of an STI, and these participants surprisingly had decreased odds of reporting STI prevention as “very important” (Table 2). The absence of a strong preference for STI prevention may affect adolescent and young women’s condom use, in turn leading to STI acquisition. STI history may be a marker of limited STI knowledge and barriers to accessing condoms, contributing to both participants’ STI risk and valuation of STI prevention. Furthermore, we previously described, in this population, that most respondents were more likely to rate their STI risk as lower than that of their peers, which may contribute to decreased condom use and reporting STI prevention as “very important” [12].
Notably, a strong desire for STI prevention was the only contraceptive feature that corresponded with being more likely to use a method that matched this preference in adjusted analyses. This finding is consistent with Marshall et al.’s 2016 study using data from a nationally representative survey of women age 18-29, which found that rating STI protection as important was associated with condom use [15]. Our data suggest that adolescent and young women who value STI prevention can effectively translate this preference into action, possibly because condoms are more accessible than other contraceptive methods, or because this preference is particularly powerful.
We found no association between a strong desire for contraceptive effectiveness and current use of a highly effective method, which is again consistent with Marshall et al.’s study described above [15]. These results are in contrast to the CHOICE study, which found that reproductive-age women who ranked effectiveness as important were more likely to choose an IUD versus pill when cost was not a barrier [32]. The CHOICE data have been used to demonstrate how education, access, and cost barriers impede obtaining highly effective methods for some women despite strong desires for effectiveness [33]. In contrast, our study was in California, where the Family PACT program reduces access barriers by providing free contraception to adolescent and young women who cannot access contraception [34]. In this setting, the disconnect between a strong preference for effectiveness and lack of use of “effective” methods is notable. This apparent paradox may be due to other access barriers, complex ways that individuals weigh competing priorities and make decisions, or changes in preferences since initiating a method. Alternatively, although we pre-tested the survey to explore women’s understanding of “effectiveness,” adolescent and young women may interpret the magnitude of effectiveness differently, potentially understanding use of any method, including marginally effective methods, as “effective” pregnancy prevention.
In addition, the lack of association between respondents’ preferences for partner independence, privacy, and use without going to a doctor or clinic (Table 4) and use of a method that has these features may result from similar reasons. Further research is needed to explore why adolescents and young women’s current contraceptive method may not match their preferences, providing opportunities to not only combat potential access barriers, but also improve counseling strategies and inform the development of contraceptive methods that better meet women’s needs.
Adolescent and young women who strongly desired effectiveness, partner-independence, or privacy and were also using a method matching this preference were more likely to be satisfied with their current contraceptive method. These results suggest that asking adolescent and young women open-ended questions about their contraceptive preferences, including but not limited to effectiveness, may facilitate women choosing methods that result in higher satisfaction. These findings support counseling recommendations that are patient-centered, focused on eliciting adolescent and young women’s varied preferences and helping women identify methods that best meet their needs [35,36], rather than emphasizing specific methods based on provider preferences [5,6].
Finally, our findings contribute to interpretations of contraceptive use data among adolescent women. Nearly one in five sexually active, 15-19 year-old women in the US report using no contraception despite not desiring pregnancy [19]. This finding has been attributed to many access barriers including cost, consent laws, confidentiality concerns, limited provider training, provider and patient misconceptions, and lack of awareness of contraceptive options [37]. The concept of pregnancy intentions as a dichotomous decision has also been challenged, and women’s nuanced feelings about pregnancy and abortion may also influence decisions to use contraception [4,35]. Our findings contribute to this evolving understanding of contraceptive use by suggesting that in addition to critical access barriers, adolescents and young women’s contraceptive use may be influenced by their preferences and values, and whether or not they have identified contraceptive methods that fits their needs.
Limitations of this study include its being a cross-sectional analysis of self-reported data in Northern California where many access barriers are minimized due to state contraceptive access programs. Therefore, results may not be generalizable to other settings. While 88% of eligible individuals participated in the study, participants may have differed from those who declined. Moreover, the sample size (N=814) may have limited power to identify statistical significance. Finally, we were unable to include a reliable measure of socioeconomic status in analyses, potentially confounding results.
We were only able to correlate contraceptive preferences with features that could be “objectively” assessed, and could not match preferences for cost, convenience and side effects with specific methods. Although we pretested participants’ understanding of terms in study questions, we did not explore with each participant her personal definition of each characteristic, and whether her contraceptive method specifically aligned with her preferred contraceptive features. While we performed additional analyses to expand and contract definitions of “effectiveness” and “privacy,” studies are needed to further explore alignment or mismatch between adolescent and young women’s preferences and method use, and how those relate to satisfaction. Finally, in this study, we were not able to assess how women prioritize competing preferences, or how these preferences and priorities change over time. Particularly for adolescent and young women whose experiences and situational contexts may change rapidly, longitudinal studies are needed to understand how family planning services can best meet women’s needs over time.
Strengths of this study include its describing a large, racially and ethnically diverse group of adolescent and young women’s experiences, behaviors, preferences, and satisfaction, facilitating study of patient-centered family planning outcomes. Our survey’s response rate was high, likely due to the survey’s anonymous nature. Although this study’s setting of relatively low-barrier access to contraception could be viewed as a limitation, it facilitated our focus on patient preferences rather than structural barriers which may dominate other clinical settings.
Contraceptive counseling approaches that elicit adolescent and young women’s preferences and identify methods that best meet their needs may improve contraceptive satisfaction. By identifying adolescent and young women’s needs and preferences, family planning counselors and clinicians also have the opportunity to advocate for development of contraceptive and multipurpose prevention methods that satisfy the diverse needs of young people. This patient-centered approach to family planning services and contraceptive development may facilitate adolescent and young women’s satisfaction not only with their contraceptive method, but potentially also with their care, laying the ground work for engagement in care throughout women’s reproductive life spans.
Supplementary Material
Implications and Contribution:
In a survey of adolescent women in California, respondents had varied preferences for contraceptive features that were associated with race/ethnicity, age, and sexual health history. Participants whose contraception matched their preferences had increased satisfaction. Counseling strategies to match preferences with contraceptive methods may improve adolescents’ satisfaction and long-term engagement.
Acknowledgments:
This research was supported by the Society of Family Planning Research Fund and the UCSF PROF-PATH program funded by the National Institute on Minority Health and Health Disparities (R25MD006832). Amelia Wing Walker was funded by the Clinical and Translational Research Fellowship Program (TL1 TR000144). Dominika Seidman was supported by grant 5K12HD001262-18 from the National Institutes of Health. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of Planned Parenthood Federation of America, Inc. or the National Institute of Health.
Abbreviations:
- STI
sexually transmitted infection
- IPV
intimate partner violence
- aOR
adjusted odds ratio
- US
United States
- HPV
human papilloma virus
- LARC
long-acting reversible contraception
- IUD
intrauterine device
- CI
confidence interval
- GED
general education development test
- EC
emergency contraception
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: None
References
- [1].Moreau C, Cleland K, Trussell J. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception 2007;76:267–72. DOI: 10.1016/j.contraception.2007.06.008. [DOI] [PubMed] [Google Scholar]
- [2].Raine TR, Foster-Rosales A, Upadhyay UD, et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol 2011;117:363–71. DOI: 10.1097/AOG.0b013e31820563d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Am Coll Obstet Gynecol 2011;117:1105–13. DOI: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dehlendorf C, Reed R, Fox E, et al. Ensuring our research reflects our values: The role of family planning research in advancing reproductive autonomy. Contraception (in press) 2018. DOI: 10.1016/j.contraception.2018.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schivone GB, Glish LL. Contraceptive counseling for continuation and satisfaction. Curr Opin Obstet Gynecol 2017;29:443–8. DOI: 10.1097/GCO.0000000000000408. [DOI] [PubMed] [Google Scholar]
- [6].Gubrium AC, Mann ES, Borrero S, et al. Realizing reproductive health equity needs more than long-acting reversible contraception (LARC). Am J Public Health 2016;106:18–9. DOI: 10.2105/AJPH.2015.302900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570 DOI: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Dehlendorf C, Grumbach K, Schmittdiel JA, et al. Shared decision making in contraceptive counseling. Contraception 2017;95:452–5. DOI: 10.1016/j.contraception.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gomez AM, Wapman M. Under (implicit) pressure: young Black and Latina women’s perceptions of contraceptive care. Contraception 2017;96:221–6. DOI: 10.1016/j.contraception.2017.07.007. [DOI] [PubMed] [Google Scholar]
- [10].Higgins JA, Kramer RD, Ryder KM. Provider bias in long-acting reversible contraception (LARC) promotion and removal: Perceptions of young adult women. Am J Public Health 2016;106:1932–7. DOI: 10.2105/AJPH.2016.303393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jackson AV, Karasek D, Dehlendorf C, et al. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception 2016;93:406–11. DOI: 10.1016/j.contraception.2015.12.010. [DOI] [PubMed] [Google Scholar]
- [12].Cipres D, Rodriguez A, Alvarez J, et al. Racial/ethnic differences in young women’s health-promoting strategies to reduce vulnerability to sexually transmitted infections. J Adolesc Heal 2017;60:556–62. DOI: 10.1016/j.jadohealth.2016.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sawyer S, Azzopardi D, Wickremarathne D, et al. The age of adolescence. The Lancet Child and Adolescent Health 2018; 2: 223–228. DOI: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- [14].Centers for Disease Control and Prevention. Effectivenes of Family Planning Methods. Available at: https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/pdf/Family-Planning-Methods-2014.pdf. Accessed October 12, 2018.
- [15].Marshall C, Guendelman S, Mauldon J, et al. Young women’s contraceptive decision making: Do preferences for contraceptive attributes align with method choice? Perspect Sex Reprod Health 2016;48:119–27. DOI: 10.1363/48e10116. [DOI] [PubMed] [Google Scholar]
- [16].He K, Dalton VK, Zochowski MK, et al. Women’s contraceptive preference-use mismatch. J Women’s Heal 2017;26:692–701. DOI: 10.1089/jwh.2016.5807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lessard LN, Karasek D, Ma S, et al. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect Sex Reprod Health 2012;44:194–200. DOI: 10.1363/4419412. [DOI] [PubMed] [Google Scholar]
- [18].Martinez G, Copen CE, Abma JC. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2006-2010 National Survey of Family Growth. Vital Heal Stat 2011;23:1–35. [PubMed] [Google Scholar]
- [19].Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Report 2012;60:1–26. [PubMed] [Google Scholar]
- [20].Daniels K, Daugherty J, Jones J, et al. Current contraceptive use and variation by selected characteristics among women aged 15-44: United States, 2011-2013. Natl Health Stat Report 2015;86:1–14. [PubMed] [Google Scholar]
- [21].Friedman JO. Factors associated with contraceptive satisfaction in adolescent women using the IUD. J Pediatr Adolesc Gynecol 2015;28:38–42. DOI: 10.1016/j.jpag.2014.02.015. [DOI] [PubMed] [Google Scholar]
- [22].Dickerson LM, Diaz VA, Jordan J, et al. Satisfaction, early removal, and side effects associated with long-acting reversible contraception. Fam Med 2013;45:701–7. [PubMed] [Google Scholar]
- [23].Ersek JL, Huber LRB, Thompson ME, et al. Satisfaction and discontinuation of contraception by contraceptive method among university women. Matern Child Health J 2011;15:497–506. DOI: 10.1007/s10995-010-0610-y. [DOI] [PubMed] [Google Scholar]
- [24].Rosenstock JR, Peipert JF, Madden T, et al. Continuation of reversible contraception in teenagers and young women. Obs Gynecol 2012;120:1298–1305. DOI: 10.1097/AOG.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gemzell-Danielsson K, Apter D, Hauck B, et al. The effect of age, parity and body mass index on the efficacy, safety, placement and user satisfaction associated with two low-dose levonorgestrel intrauterine contraceptive systems: Subgroup analyses of data from a phase III trial. PLoS One 2015;10:1–14. DOI: 10.1371/journal.pone.0135309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Callegari L, Zhao X, Schwarz E, et al. Racial/ethnic differences in contraceptive preferences, beliefs, and self-efficacy among women veterans. Am J Obstet Gynecol 2017;216:504.e1–504.e10. DOI: 10.1016/j.ajog.2016.12.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016. Alanta, GA: U.S. Department of Health and Human Services, 2017. [Google Scholar]
- [28].Downey MM, Arteaga S, Villaseñor E, et al. More than a destination: Contraceptive decision making as a journey. Women’s Heal Issues 2017;27:539–45. DOI: 10.1016/j.whi.2017.03.004. [DOI] [PubMed] [Google Scholar]
- [29].Miller E, Decker MR, McCauley HL, et al. Pregnancy coercion, intimate partner violence, and unintended pregnancy. Contraception 2010;81:316–22. DOI: 10.1016/j.contraception.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bergmann JN, Stockman JK. How does intimate partner violence affect condom and oral contraceptive use in the United States? A systematic review of the literature. Contraception 2015;91:438–55. DOI: 10.1016/j.contraception.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Decker MR, Flessa S, Pillai R V, et al. Implementing trauma-informed partner violence assessment in family planning clinics. J Women’s Heal 2017;26:957–65. DOI: 10.1089/jwh.2016.6093. [DOI] [PubMed] [Google Scholar]
- [32].Madden T, Secura GM, Nease RF, et al. The role of contraceptive attributes in women’s contraceptive decision making. Am J Obstet Gynecol 2015;213:46e1–46.e6. DOI: 10.1016/j.ajog.2015.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Goodman M, Onwumere O, Milam L, et al. Reducing health disparities by removing cost, access, and knowledge barriers. Am J Obstet Gynecol 2017;216:382.e1–382.e5. DOI: 10.1016/j.ajog.2016.12.015. [DOI] [PubMed] [Google Scholar]
- [34].Family PACT. Available at: http://www.familypact.org/Home/home-page. Accessed May 16, 2018.
- [35].Callegari LS, Aiken ARA, Dehlendorf C, et al. Addressing potential pitfalls of reproductive life planning with patient-centered counseling. Am J Obstet Gynecol 2017;216:129–34. DOI: 10.1016/j.ajog.2016.10.004. [DOI] [PubMed] [Google Scholar]
- [36].Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality commuication and enable effective contraceptive use. Clin Obstet Gynecol 2014;57(4): 659–73. DOI: 10.1097/GRF.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kumar N, Brown JD. Access barriers to long-acting reversible contraceptives for adolescents. J Adolesc Heal 2016;59:248–53. DOI: 10.1016/j.jadohealth.2016.03.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.