Abstract
Background:
Studies have found age-specific effects of medical cannabis laws (MCLs), particularly affecting adult cannabis use but not adolescent use. We examined whether age differences in MCL knowledge are in accordance with age differences in MCL effects on cannabis use.
Methods:
Data from the 2004-2013 repeated cross-sectional National Surveys on Drug Use and Health included people ages 12 and older in the United States. State-aggregated MCL knowledge was the proportion of people that correctly identified living in a state that did not allow medical cannabis prior to MCL enactment, or that allowed medical cannabis after MCL enactment. We regressed state-aggregated MCL knowledge on time-varying MCL enactment (i.e., no MCL by 2015, before MCL, after MCL), testing associations by age strata (12-17, 18-25, 26+), open dispensary status, and adjusting for time and state-level demographics.
Results:
Model-based MCL knowledge was significantly lower among adolescents than adults; after enactment, 36.8% of ages 12-17, 48.8% of ages 18-25, and 45.4% of ages 26+ were aware of their state’s MCL status. Correct MCL status knowledge decreased across all age groups after MCL enactment (i.e., low knowledge of MCL changes at the time they occurred). Open cannabis dispensaries significantly increased correct MCL knowledge, with a 7.7-point increase for adolescents and a 17.5-point increase for adults 26+.
Conclusions:
Lower MCL knowledge among adolescents than adults was in accordance with MCL effects on cannabis use previously observed among adults only. Studies should assess whether MCL knowledge is a consequence or predictor of individual-level cannabis use across age groups.
Keywords: medical cannabis laws, cannabis, knowledge, adolescents, marijuana policy, dispensaries
1. INTRODUCTION
The changing cannabis policies in the United States (US) have led to important public health questions about their potential consequences concerning cannabis use prevalence, cannabis use disorder, and cannabis-related injury at the population level (Cerdá, Wall, Keyes, Galea, & Hasin, 2012; Compton, Volkow, & Lopez, 2017; Maxwell & Mendelson, 2016). Various studies have assessed the impact of medical cannabis laws (MCLs) on changes in the prevalence of cannabis use and perceived availability (Chu, 2014; D. Hasin et al., 2017; Martins et al., 2016; Wen, Hockenberry, & Cummings, 2015), and reported age differences in the effects of MCLs (Wen et al., 2015). Of particular interest is understanding why MCLs have not been associated with causal increases in cannabis use among adolescents (D. M. Anderson, Rees, & Sabia, 2014; M. D. Anderson, Hansen, & Rees, 2015; Choo et al., 2014; Harper, Strumpf, & Kaufman, 2012; D. S. Hasin et al., 2015; Johnson, 2015; Johnson, Hodgkin, & Harris, 2017; Keyes et al., 2016; Pacula, Powell, Heaton, & Sevigny, 2015; Smart, 2015; Wall et al., 2016; Wen et al., 2015) but have been associated with increases among adults (Chu, 2014; D. Hasin et al., 2017; Martins et al., 2016; Wen et al., 2015). In this manuscript, we assess whether age differences in knowledge of MCL could contribute to the observed age-specific effects of MCLs on cannabis use.
Studies assessing the relationship between MCL and cannabis use could implicitly assume that people know the MCL status in their state and therefore change their behavior as one potential mechanism of change. However, little is known about MCL awareness and knowledge in the US across age groups. Age differences in knowledge of MCL could contribute to age differences in absence or delay in MCL effects. If younger age groups are less aware of the changing status of cannabis use for medical purposes, they may be less likely to change their attitudes or behaviors as a result of these laws than older ages. Limited knowledge of cannabis decriminalization (MacCoun, Pacula, Chriqui, Harris, & Reuter, 2009), for example, has been found to contribute to mixed or delayed effects of that policy. Based on assessments of other substance use policies such as cannabis decriminalization (Erickson, Van Der Maas, & Hathaway, 2013; MacCoun et al., 2009), cannabis legalization (Mason, Hanson, Fleming, Ringle, & Haggerty, 2015), or zero tolerance policies related to alcohol use (Ferguson & Williams, 2002), there is reason to hypothesize that awareness of MCL status at the state level would be low. To our knowledge, no study has assessed the degree of correspondence of perceived legal status of medical cannabis and actual MCL status in their state, that is, correct knowledge of MCL status.
Age differences in MCL knowledge could be exacerbated in states with open cannabis dispensaries if the presence of these dispensaries differentially increases MCL knowledge among certain age groups. Cannabis dispensaries may act as a visual cue of MCL status, which could lead to increased knowledge of changing MCL status. Opening of cannabis dispensaries may be accompanied with press coverage that could increase awareness of MCL status in a state. If there are also age differences in the effect of dispensaries on MCL knowledge, these could further contribute to age differences in MCL effects at the population level.
We therefore investigated the following research questions. First, does correct MCL knowledge vary by age? Second, does correct MCL knowledge vary by MCL status, and are relationships comparable across age categories? Third, do dispensaries increase MCL knowledge as expected, and are these increases comparable across age categories? Findings from this study aim to determine whether population-level knowledge of changing MCLs are consistent with the observed effects of MCLs on cannabis use among adults and no effects among adolescents.
2. MATERIALS AND METHODS
2.1. Sample
The National Survey on Drug Use and Health (NSDUH) is a nationally representative cross-sectional survey series in the US sponsored by the Substance Abuse and Mental Health Services Administration (CBHSQ, 2014; SAMHSA, 2005, 2014). The NSDUH multi-stage complex survey design sampled community-based individuals ages 12 and older, oversampling young people. The 2004-2013 NSDUH restricted-use data portal included state-representative NSDUH estimates. Weighted response rates for the years assessed ranged from 71.7 to 77.0% (SAMHSA, 2005, 2014). All 50 states were included in the sampling frame.
2.2. Measures
2.2.1. Participant-reported medical cannabis status in one’s state.
Participants responded to the prompt: “In [your state], has marijuana been legally approved for medical use?” Responses included yes, no, and don’t know. Aggregate state-level estimates of the proportion of responses indicating “yes” (i.e., reporting their state approved medical cannabis), “no” (i.e., reporting their state did not approve medical cannabis) and “don’t know” (i.e., did not know the state MCL status) were obtained for each state-year.
2.2.2. Year of MCL enactment and cannabis dispensary.
Year of MCL enactment was determined by policy reviews conducted by economists, legal scholars, and policy analysts at RAND Corporation. We used enactment date in all 50 states instead of passage date in order to capture the time period when the law was in effect. We also obtained the year that cannabis dispensaries were open or operational regardless of whether the MCL explicitly provided legal protections for the dispensaries (Pacula et al., 2015; Sevigny, Pacula, & Heaton, 2014).
2.2.3. State MCL enactment.
We created a three-level time-varying categorical variable to classify each state-year by MCL enactment status: no MCL by 2015, before MCL, and after MCL. This differentiated state-years before enacting MCLs (e.g., Rhode Island 2004-05) and after enacting MCLs (e.g., Rhode Island 2006-13) from the 27 states that had not passed MCLs by 2015.
2.2.4. State MCL-dispensary status.
We created a four-level time-varying categorical variable further distinguishing states that had enacted MCL by their dispensary status. State-years with MCLs and open dispensaries were differentiated from state-years with MCLs but no open dispensaries. Among the 13 states with open dispensaries before 2015, the lag time between MCL enactment and opening of dispensaries for ranged from 0 (i.e., Michigan) to 11 years (i.e., Maine), with a median of 7 years and mean of 6 years (SD=3.67). State-years before MCL enactment and states without MCL by 2015 were in their own respective categories, as defined in the MCL enactment status variable.
2.2.5. State characteristics.
State-level demographic variables were obtained from the 2000 and 2010 US Census. This included the proportions of males, non-Hispanic whites, people with at least high school education among ages 25+, as well as the unemployment rate, and median household income. Proportions of civilians ages 12-17 and 18-25 were calculated using the 2000-2010 State Characteristics Intercensal Population Estimates Files with single year of age estimates released by the US Census in October 2012.
2.3. Analytic strategy
First, we sought to estimate the proportion of people with correct knowledge of their state’s MCL status. Yearly state-specific aggregated estimates of participant-reported medical cannabis status in one’s state were obtained for respondents ages 12-17, 18-25, and 26 and older using survey weights taking into account the effects of the NSDUH complex survey design and oversampling of ages 12-17 and 18-25. Standard errors were derived using a Taylor series linearization approach (Chromy & Abeyasekera, 2005). We combined estimates of participant-reported medical cannabis status and actual state MCL enactment status to estimate the proportion of people with correct knowledge of their state’s MCL status. In state-years with MCL (i.e., after MCL enactment), responding “yes” to the MCL status question indicated correct MCL knowledge. In state-years without MCL (i.e., before MCL enactment or states that never passed MCL), responding “no” to the MCL status question was considered correct MCL status identification. “Don’t know” responses were considered incorrect regardless of MCL status. We graphed non-parametric lowess curves by age to describe overall trends over time in correct MCL knowledge for people 12-17 years old, 18-25 years old, and 26 years and older. Lowess curves were age-specific linear functions (alpha=0.8) locally-weighted using Cleveland’s tricube weighting function (Cleveland, 1979), graphed using Stata14SE (StataCorp, 2015). For states that enacted an MCL by 2015, we also graphed MCL knowledge in relation to MCL enactment year. Years to/since MCL enactment was calculated by subtracting the year of MCL enactment from the NSDUH year.
Then, we estimated model-based age differences in knowledge of MCL status, and compared knowledge in states with and without MCLs. We fit a multilevel adjusted model to estimate MCL knowledge by age and MCL status, accounting for time trends and state demographics. In Model 1, we fit a two-level (i.e., state, year) linear model (Diggle, Heagerty, Liang, & Zeger, 2002) regressing correct MCL status knowledge on the three-level MCL enactment status (residual intraclass correlation [ICC]=0.58). A random intercept for state was used to account for repeated measurements of state over time. This modeling strategy using the three-level MCL enactment status variable allowed us to determine the change in correct MCL status knowledge before and after MCL enactment. Because there was a marked change in the trend of the prevalence of marijuana use in 2008, a piecewise cubic spline function with a knot in 2008 was used for time to account for national trends over time (de Boor, 1978). Interaction terms between age and MCL status as well as age and time allowed for age-specific effects. Estimates adjusted for state demographic variables from the 2000 and 2010 US Census for years 2004-2005 and 2006-2013, respectively. Differences in the predicted mean values were calculated from the adjusted models to estimate whether there were any statistically significant differences in means of correct MCL status knowledge by age and MCL status.
In a separate model, we estimated age differences in knowledge of MCL status, comparing states with and without cannabis dispensaries. In Model 2, we fit a two-level model including the three age categories as done in Model 1, but instead regressing MCL knowledge on the four-category MCL-dispensary status variable. This allowed us to estimate MCL knowledge before and after opening cannabis dispensaries, accounting for before- and never MCL status and other state characteristics. Differences in least squares means were estimated as done in Model 1. Statistical significance was based on two-tailed tests. We used a conservative Bonferroni correction for multiple comparisons at p-value<0.05/30 (i.e., p<0.0017) to account for 30 pairwise comparisons by age and MCL status.
Finally, we conducted sensitivity analyses to determine whether our findings in models 1 and 2 were sensitive to state prevalence of past month cannabis use by age. Importantly, we could not differentiate MCL knowledge by cannabis use, and we conceptualized cannabis use as a potential mediator in the relationship between MCL enactment and MCL knowledge. Analyses were conducted using Stata14SE (StataCorp, 2015).
3. RESULTS
3.1. Age differences in knowledge of legal status of medical cannabis use in one’s state
Overall trends over time in correct MCL knowledge by age are depicted in Figure 1.
Figure 1: Correct knowledge of medical cannabis legal status at the state level by age category, NSDUH 2004-2013.
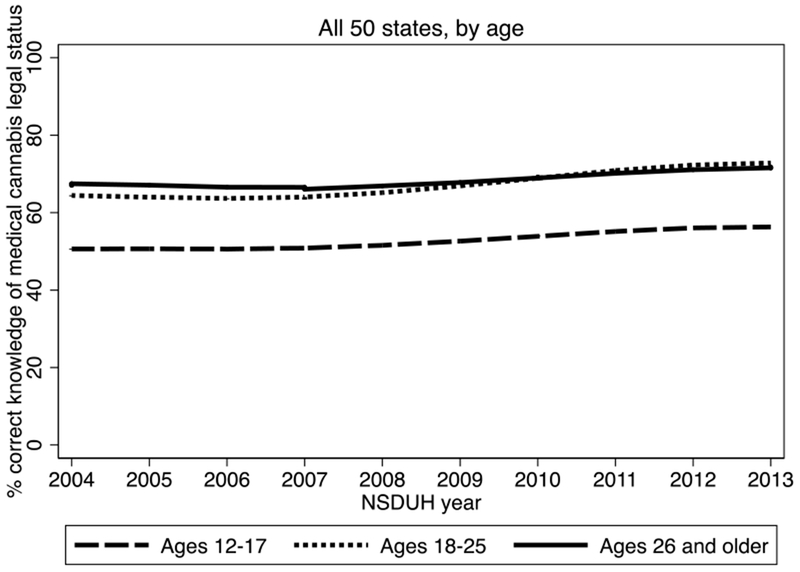
Note: NSDUH=National Survey on Drug Use and Health. Lowess curves were age-specific linear functions (alpha=0.8) locally-weighted using Cleveland’s (1979) tricube weighting function.
Estimates from model 1 indicate that overall, 52.8% of ages 12-17, 67.2% of ages 18-25, and 68.3% of ages 26+ had correct knowledge of their state’s legal status of cannabis use for medical purposes, accounting for MCL status, time trends, and state census demographics. Relative to adolescents, correct knowledge was statistically significantly higher among adults ages 18-25 (adjusted estimate=14.5, 95% confidence interval (CI) [11.7, 17.4], p<0.0001) and adults 26+ (adjusted estimate=18.5, 95% CI [15.6, 21.4], p<0.0001). Correct knowledge was 1.1% higher among adults 26+ than adults 18-25 (95% CI [0.2, 2.0], p=0.012).
3.2. Age differences in knowledge of legality of medical cannabis use by MCL status
Unadjusted trends in MCL knowledge by age before and after MCL enactment are depicted in Figure 2, excluding states without MCL by 2015.
Figure 2: Correct knowledge of medical cannabis legal status at the state level before and after medical cannabis law enactment by age category, NSDUH 2004-2013.
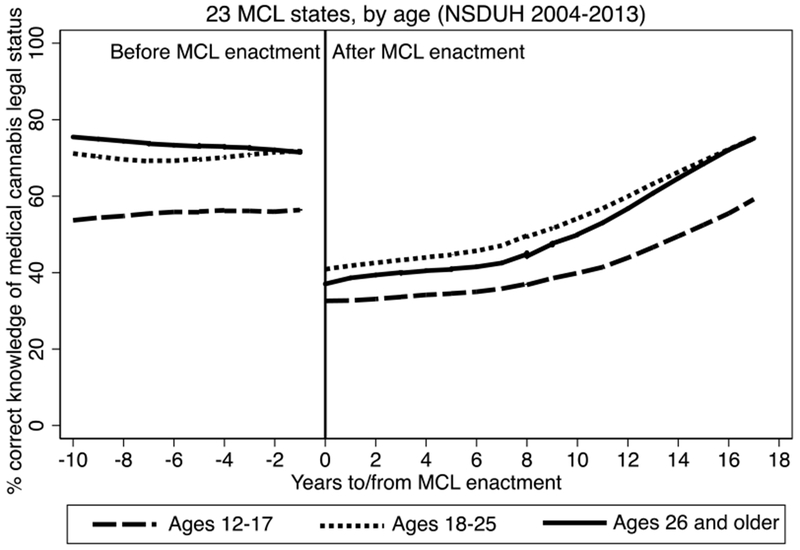
Note: NSDUH=National Survey on Drug Use and Health; MCL= Medical Cannabis Law. Lowess curves were age-specific linear functions (alpha=0.8) locally-weighted using Cleveland’s (1979) tricube weighting function, and fit separately before and after MCL enactment.
In Table 1, we reported correct MCL status knowledge by age and MCL status, adjusting for state demographic covariates and time (Model 1a). Among adolescents, 36.8% reported correct MCL knowledge following MCL enactment in adjusted models. Among adults, correct MCL knowledge after MCL enactment was 48.8% for ages 18-25 and 45.4% for ages 26 and older. Correct MCL knowledge was lower after MCL enactment compared to before enactment for all three age groups. Specifically, correct MCL knowledge was 24.0 points lower after MCL enactment compared to before enactment for ages 12-17 years old, 27.0 points lower for ages 18-25, and 32.5 points lower for ages 26+ (p’s<0.0001). There was no difference in adjusted correct MCL knowledge comparing states before MCL enactment to states that never enacted MCL for any of the age categories.
Table 1:
Adjusted multi-level regression of state-level MCL knowledge by age, MCL status, and cannabis dispensaries
| MCL Status | Correct knowledge of MCL status, Est [95% CI] | Differences by age, Est [95% CI] | ||||
|---|---|---|---|---|---|---|
| Ages 12-17 | Ages 18-25 | Ages 26+ | 12-17 vs. 18-25 | 12-17 vs. 26+ | 18-25 vs. 26+ | |
| Model 1 a | ||||||
| Never MCL | 57.66 [54.26, 61.05] | 72.99 [69.60, 76.38] | 75.98 [72.58, 79.37] | −15.33*** [−16.53, −14.14] | −18.32*** [−19.51, −17.13] | −2.99*** [−4.18, −1.79] |
| Before MCL | 60.81 [56.80, 64.82] | 75.82 [71.81, 79.83] | 77.89 [73.88, 81.90] | −15.01*** [−17.01, −13.01] | −17.09*** [−19.08, −15.09] | −2.08* [−4.07, −0.08] |
| After MCL | 36.84 [33.01, 40.68] | 48.82 [44.98, 52.66] | 45.41 [41.57, 49.25] | −11.98*** [−13.69, −10.26] | −8.57*** [−10.28, −6.85] | +3.41** [1.70, 5.13] |
| After vs. before MCL | −23.96*** [−26.54, −21.39] | −26.99*** [−29.57, −24.42] | −32.48*** [−35.06, −29.91] | -- | -- | -- |
| Before vs. never MCL | +3.15 [−2.30, 8.60] | +2.83 [−2.62, 8.28] | +1.92 [−3.54, 7.37] | -- | -- | -- |
| Model 2 a | ||||||
| Never MCL | 58.28 [55.72, 60.84] | 73.61 [71.05, 76.17] | 76.60 [74.04, 79.16] | −15.33*** [−16.45, −14.21] | −18.32*** [−19.44, −17.20] | −2.99*** [−4.11, −1.87] |
| Before MCL | 59.12 [55.97, 62.26] | 74.04 [70.89, 77.19] | 76.07 [72.92, 79.22] | −14.92*** [−16.80, −13.05] | −16.95*** [−18.83, −15.08] | −2.03* [−3.90, −0.16] |
| After MCL, no dispensaries | 33.79 [30.68, 36.91] | 43.40 [40.28, 46.51] | 38.61 [35.50, 41.73] | −9.61*** [−11.66, −7.55] | −4.82*** [−6.88, −2.77] | +4.78*** [2.73, 6.84] |
| After MCL with dispensaries | 41.52 [38.14, 44.90] | 57.30 [53.92, 60.68] | 56.09 [52.71, 59.47] | −15.79*** [−18.39, −13.18] | −14.57*** [−17.18, −11.96] | +1.21 [−1.40, 3.82] |
| After vs. before dispensaries | +7.73*** [5.09, 10.37] | +13.91*** [11.26, 16.55] | +17.48*** [14.84, 20.12] | -- | -- | -- |
Notes: state-level aggregated data were obtained from the National Survey on Drug Use and Health 2004-2013. MCL=medical cannabis law; Est=estimate; CI=confidence interval. Models were adjusted for state demographic variables from the 2000 and 2010 US Census, and time.
p<0.0001
p<0.01
p<0.05.
Bonferroni correction significance level p<0.0017 (i.e., p<0.05/30) in bold.
3.3. Age differences in knowledge of MCL status before and after opening cannabis dispensaries
In Model 2a, we estimated the effect of cannabis dispensaries on state-level MCL knowledge by age. A third of adolescents (33.8%) and less than half of adults (43.4% of ages 18-25 and 38.6% of ages 26+) correctly identified living in a state that had legalized medical use of cannabis when there were no open cannabis dispensaries. In states with open dispensaries, 41.5% of adolescents, 57.3% of ages 18-25, and 56.1% of ages 26+ correctly identified living in a state permitting legal use of medical cannabis.
After adjusting for state demographics and time, presence of cannabis dispensaries following MCL enactment was associated with increases in MCL knowledge across age groups (p’s<0.0001). That is, larger proportions of people correctly reporting that medical cannabis was legal in their state when there were cannabis dispensaries. In particular, cannabis dispensaries in states that had enacted MCLs were associated with a 7.7-point increase in MCL knowledge among ages 12-17, a 13.9-point increase among ages 18-25, and a 17.5-point increase among ages 26 and older (p’s<0.0001). MCL knowledge remained statistically significantly lower for adolescents 12-17 than adults in MCL states with open dispensaries, and was not statistically significantly different comparing adults 18-25 and 26 and older after accounting for multiple comparisons. Findings were robust to model specification changes, particularly including state prevalence of past month cannabis use (see supplemental table A for detailed results) as well as state population totals.
4. DISCUSSION
In this study, we assessed whether there were age differences in MCL knowledge by MCL and dispensary status using state-level aggregated data from 2004-2013, a 10-year period with substantial cannabis policy change across states. Knowledge of MCLs was lower among adolescents than adults and remained significantly lower after accounting for the effect of enacting MCLs, open dispensaries, and state cannabis use prevalence. Our findings are in accordance with age differences in MCL effects across states, both in MCL states with and without cannabis dispensaries. We also found that across age groups, correct MCL status knowledge was significantly lower after MCL enactment, suggesting low levels of information about medical cannabis status at the time of the policy change, particularly among adolescents. Correct MCL knowledge seems to increase over time and with opening of cannabis dispensaries, and could be influenced by various factors such as media attention on the policy change.
Our study fills an important gap in the literature, and contributes to potential explanations of the discrepancy MCL age effects observed in previous studies. Studies assessing the causal effect of MCL on cannabis use through difference-in-difference methodology in large survey samples of adolescents found no increases in cannabis use after MCL passage or enactment (D. M. Anderson et al., 2014; Choi, 2014; Choo et al., 2014; Harper et al., 2012; D. S. Hasin et al., 2015; Johnson, 2015; Johnson et al., 2017; Keyes et al., 2016; Martins et al., 2016; Pacula et al., 2015; Sarvet et al., 2018; Smart, 2015; Wall et al., 2016; Wen et al., 2015). In contrast, four studies using large surveys and similar methodology found MCLs to be associated with increases in cannabis use among adults (Chu, 2014; D. Hasin et al., 2017; Martins et al., 2016; Wen et al., 2015). Similarly, a recent study reported increases in perceived availability of cannabis among adults, not adolescents, following MCL enactment (Martins et al., 2016). Age differences in MCL knowledge are in accordance with age differences in MCL effects on cannabis use, similar to how limited awareness of cannabis decriminalization policies partially explained the policies’ inconsistent effects in the US from 2001-2003 (MacCoun et al., 2009). MCLs could impact adults’ cannabis use since adults are more aware of their state’s MCL status, and are, therefore, more likely to be affected by changes in its legal status than adolescents. This could be due to adolescents not being able to vote and therefore being less aware of state-level legislation in cases when the law was passed by a ballot initiative, for example. Alternatively, people who use cannabis may be more aware of MCLs, though this was not assessed in the current study due to data access limitations. In the context of increasing daily and non-daily cannabis use among adults, particularly since 2007 (Mauro et al., 2018), future studies should assess individual-level correlates and predictors of MCL knowledge to determine whether knowledge of MCL is in the causal pathway between MCL enactment and cannabis use.
Significant age differences in MCL knowledge remained even after accounting for open cannabis dispensaries. As expected, MCL knowledge was higher in states with open cannabis dispensaries than in MCL states without dispensaries. However, the effect of open dispensaries on MCL knowledge also varied by age. Dispensaries were associated with a 17-point increase in MCL knowledge among adults 26+ in states that had enacted MCLs; this change in MCL knowledge was more than twice the magnitude of the change observed among adolescents after dispensaries opened. Opening of dispensaries could increase knowledge of MCL status through advertising or media coverage, which could be affected by age differences in media consumption patterns (Newman, 2017). Dispensaries could also increase actual availability of cannabis among adults, and therefore increase an individual’s exposure to cannabis among adults and their social networks, leading to age differences in the effects of dispensaries on MCL status knowledge.
Understanding MCL knowledge is of public health interest, as it could potentially modify attitudes and behavior. For example, people with accurate knowledge of a cannabis decriminalization law had a higher probability of saying that legal sanctions affected cannabis use patterns than those with inaccurate knowledge of the law (Erickson et al., 2013). As perceived state legalization of medical cannabis has been associated with any and more frequent cannabis use (Compton, Han, Jones, Blanco, & Hughes, 2016), knowledge of actual MCL status following MCL enactment could also be associated with these outcomes. However, changing state MCL status is occurring in the context of unchanging federal classification of cannabis as a Schedule I substance, indicating no medical use and high abuse potential as determined by the Drug Enforcement Agency. The tension between state and federal legal status of cannabis could be contributing to delays in correct knowledge of MCL following enactment of these laws.
Limitations are noted. First, the use of aggregated state-level estimates limited any individual-level conclusions that can be drawn from these analyses. Despite the fact that NSDUH is a repeated cross-sectional study of individuals, when state is treated as the unit of observation, as is the case here, the data is longitudinal and strengthens the findings. The use of state-level estimates of MCL knowledge is a major strength of the study. While we adjusted for many state-level characteristics from the US census, residual confounding could result from unobserved characteristics such as state-led substance use prevention efforts, information campaigns, and variability in voting practices. Future studies should assess whether ballot-led initiatives are associated with higher MCL knowledge, accounting for percentage of voters in a state. Due to limitations in years available for analysis, we were not able to include recreational cannabis use laws, as these were enacted at the end of 2012 or later and we therefore did not have enough data to investigate their impact. Future studies should address this issue when more data become available. It could be that MCL knowledge was different in states that enacted recreational cannabis (e.g., Colorado, Washington). An important next step is to identify individual-level factors associated with increased MCL knowledge, such as self-reported medical cannabis use or having a medical condition for which medical cannabis might be indicated.
5. CONCLUSIONS
Our findings are in accordance with other studies reporting MCL effects among adults, not adolescents. A larger proportion of adults than adolescents knew their state’s MCL status between 2004 and 2013, even after accounting for cannabis dispensaries and state prevalence of past month cannabis use. The ecological design warrants caution when interpreting results. Future research should assess whether knowledge of MCL status is associated with higher medical or non-medical cannabis use at the individual-level following MCL enactment. The tension between different state and federal legal status of medical cannabis use could indeed be contributing to this gap in MCL knowledge. If MCL knowledge predicts cannabis use across age groups, future changes in knowledge could lead to further changes in cannabis use at the population level, particularly among adults. Continued assessment of MCL is needed as the legal status of cannabis continues to change, and as more states consider recreational cannabis legislation. To assess the full effect of policy interventions, studies should assess knowledge of these policies once they are enacted.
Supplementary Material
HIGHLIGHTS.
We assessed correct knowledge of medical cannabis law, comparing adolescents and adults in the US
45.6%-49.0% of adults were aware that their state allowed medical use of cannabis after enactment
37.0% of adolescents were aware of their state’s MCL status after policy enactment
Across age categories, correct policy knowledge increased after opening of cannabis dispensaries
Lower MCL knowledge among adolescents than adults was in accordance with studies reporting MCL effects among adults only
Footnotes
Declaration of competing interests: None.
References
- Anderson DM, Rees DI, & Sabia JJ (2014). Medical marijuana laws and suicides by gender and age. Am J Public Health, 104(12), 2369–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson MD, Hansen B, & Rees DI (2015). Medical marijuana laws and teen marijuana use. American Law and Economics Review, 17(2), 495–528. [Google Scholar]
- CBHSQ. (2014). Summary of Methodological Studies, 1971–2014. Retrieved from Rockville, MD. [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, & Hasin D (2012). Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence, 120(1–3), 22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi A (2014). The impact of medical marijuana laws on marijuana use and other risky health behaviors. Health & healthcare in america: From economics to policy. [Google Scholar]
- Choo EK, Benz M, Zaller N, Warren O, Rising KL, & McConnell KJ (2014). The impact of state medical marijuana legislation on adolescent marijuana use. Journal of Adolescent Health, 55(2), 160–166. [DOI] [PubMed] [Google Scholar]
- Chromy JR, & Abeyasekera S (2005). Statistical analysis of survey data. New York, NY: United Nations Publications. [Google Scholar]
- Chu YW (2014). The effects of medical marijuana laws on illegal marijuana use. Journal of Health Economics, 38, 43–61. [DOI] [PubMed] [Google Scholar]
- Cleveland WS (1979). Robust locally weighted regression and smoothing scatterplots. Journal of the American Statistical Association, 74, 829–836. [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, & Hughes A (2016). Marijuana use and use disorders in adults in the USA, 2002-14: analysis of annual cross-sectional surveys. The Lancet Psychiatry, 3(10), 954–964. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkow ND, & Lopez MF (2017). Medical Marijuana Laws and Cannabis Use: Intersections of Health and Policy. JAMA Psychiatry, 74(6), 559–560. [DOI] [PubMed] [Google Scholar]
- de Boor C (1978). A Practical Guide to Splines (Vol. 27). New York, NY: Springer-Verlag. [Google Scholar]
- Diggle PJ, Heagerty PJ, Liang K-Y, & Zeger SL (2002). Analysis of longitudinal data (2 ed. Vol. 1). [Google Scholar]
- Erickson PG, Van Der Maas M, & Hathaway AD (2013). Revisiting Deterrence: Legal Knowledge, Use Context and Arrest Perception for Cannabis*. Sociologicky Casopis, 49(3), 427. [Google Scholar]
- Ferguson SA, & Williams AF (2002). Awareness of zero tolerance laws in three states. Journal of Safety Research, 33(3), 293–299. [DOI] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, & Kaufman JS (2012). Do Medical Marijuana Laws Increase Marijuana Use? Replication Study and Extension. Annals of Epidemiology, 22(3), 207–212. [DOI] [PubMed] [Google Scholar]
- Hasin D, Sarvet A, Cerdá M, Keyes K, Stohl M, Galea S, & Wall M (2017). US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry, 74(6), 579–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Feng T (2015). Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. The Lancet Psychiatry, 2(7), 601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J (2015). Do state liberalized marijuana policies affect adolescent marijuana and alcohol use? A state-level analysis. Brandeis University, Waltham, Mass. [Google Scholar]
- Johnson J, Hodgkin D, & Harris SK (2017). The design of medical marijuana laws and adolescent use and heavy use of marijuana: Analysis of 45 states from 1991 to 2011. Drug and Alcohol Dependence, 170, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Wall M, Cerdá M, Schulenberg J, O’malley PM, Galea S, Hasin DS (2016). How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction, 111(12), 2187–2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoun R, Pacula RL, Chriqui J, Harris K, & Reuter P (2009). Do Citizens Know Whether Their State Has Decriminalized Marijuana? Assessing the Perceptual Component of Deterrence Theory. Review of Law and Economics, 5(1). [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Wall M (2016). State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend, 169, 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hanson K, Fleming CB, Ringle JL, & Haggerty KP (2015). Washington State recreational marijuana legalization: parent and adolescent perceptions, knowledge, and discussions in a sample of low-income families. Subst Use Misuse, 50(5), 541–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauro PM, Carliner H, Brown QL, Hasin DS, Shmulewitz D, Rahim-Juwel R, Martins SS (2018). Age differences in daily and non-daily cannabis use in the United States, 2002-2014. Journal of studies on alcohol and drugs, 79(3), 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JC, & Mendelson B (2016). What Do We Know Now About the Impact of the Laws Related to Marijuana? J Addict Med, 10(1), 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman N, Richard F; Kalogeropoulos Antonis; Levy David A. L.; Nielsen Rasmus Kleis. (2017). Reuters Institute Digital News Report 2017. Retrieved from Oxford, UK. [Google Scholar]
- Pacula RL, Powell D, Heaton P, & Sevigny EL (2015). Assessing the Effects of Medical Marijuana Laws on Marijuana Use: The Devil is in the Details. Journal of policy analysis and management, 34(1), 7–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. (2005). Results from the 2004 National Survey on Drug Use and Health: National Findings (DHHS Publication No. SMA 05-4062). Retrieved from Rockville, MD. [Google Scholar]
- SAMHSA. (2014). Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings (DHHS Publication No. SMA 14-4863). Retrieved from Rockville, MD. [Google Scholar]
- Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, Hasin DS (2018). Medical marijuana laws and adolescent marijuana use in the United States: A systematic review and meta-analysis. Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevigny EL, Pacula RL, & Heaton P (2014). The effects of medical marijuana laws on potency. International Journal of Drug Policy, 25(2), 308–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R (2015). The Kids Aren’t Alright but Older Adults Are Just Fine: Effects of Medical Marijuana Market Growth on Substance Use and Abuse. Social Science Research Network; Available from: http://ssrn.com/abstract=2574915 or 10.2139/ssrn.2574915. [DOI] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Wall MM, Mauro C, Hasin DS, Keyes KM, Cerda M, Martins SS, & Feng T (2016). Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: Commentary on Stolzenberg et al. (2015) and reanalysis of US National Survey on Drug Use in Households data 2002–2011. International Journal of Drug Policy, 29, 9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, & Cummings JR (2015). The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health Economics, 42, 64–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


