Abstract
Objective:
Individuals aged 90 or older (oldest-old), the fastest growing segment of the population, are at increased risk of developing cognitive impairment compared with younger old. Neuropsychological evaluation of the oldest-old is important yet challenging in part because of the scarcity of test norms for this group. We provide neuropsychological test norms for cognitively intact oldest-old.
Methods:
Test norms were derived from 403 cognitively intact participants of The 90+ Study, an ongoing study of aging and dementia in the oldest-old. Cognitive status of intact oldest-old was determined at baseline using cross-sectional approach. Individuals with cognitive impairment no dementia or dementia (according to DSM-IV criteria) were excluded. Participants ranged in age from 90 to 102 years (Mean=94). The neuropsychological battery included 11 tests (Mini-Mental Status Examination, Modified Mini-Mental State Examination, Boston Naming Test – Short Form, Letter Fluency Test, Animal Fluency Test, California Verbal Learning Test-II Short Form, Trail Making Tests A/B/C, Digit Span Forward and Backwards Test, Clock Drawing Test, CERAD Construction Subtests) and the Geriatric Depression Scale.
Results:
Data show significantly lower scores with increasing age on most tests. Education level, sex and symptoms of depression were associated with performance on a number of tests after accounting for age.
Conclusions:
Provided test norms will help to distinguish cognitively intact oldest-old from those with cognitive impairment.
Keywords: aged, 80 and over, cognition, neuropsychology, reference values, geriatric assessment
INTRODUCTION
The oldest-old (individuals aged 90 or older) are the fastest growing segment of the population. In the United States, the population of 90+ individuals is expected to triple by 2050, reaching 8.1 million people (United Nations Department of Economic and Social Affairs Population Division, 2017). Oldest-old individuals are at high risk of developing dementia (Corrada, Brookmeyer, Paganini-Hill, Berlau, & Kawas, 2010) and the ability to identify cognitive changes in this high-risk group is essential. However, distinguishing individuals with normal cognition from those with impaired cognition remains challenging because of the scarcity of appropriate test norms for this age group. Moreover, available test norms for cognitively normal oldest-old are limited by small sample sizes, small numbers of tests, or tests that are infrequently used by psychologists (Legdeur et al., 2017).
The present work addresses this gap by providing neuropsychological test norms that will help distinguish cognitively normal oldest-old from those with cognitive impairment (cognitively impairment with no dementia (CIND) and dementia). Our earlier publication (Whittle et al., 2007) provided test norms to differentiate oldest-old without dementia (normal and CIND) from those with dementia. Inclusion of CIND participants in our previous normative publication resulted in lower means and larger variances of the normative values compared with norms derived from cognitively normal participants alone, and limited the ability to differentiate cognitively normal from mildly impaired individuals.
Here we report test norms derived from one of the largest well-characterized cohorts of the oldest-old, The 90+ Study. Importantly, these new norms span a comprehensive battery of widely used cognitive tests (Rabin, Paolillo, & Barr, 2016). We developed norms by using a cross-sectional approach to determining cognitive status of the normative group - including individuals with normal cognition at baseline, although they may have later developed cognitive impairment (Sliwinski, Lipton, Buschke, & Stewart, 1996). Using clinical diagnostic criteria we excluded individuals with CIND (Graham et al., 1997) and dementia (DSM-IV) (American Psychiatric Association, 1994) from the normative group.
METHODS
Study Procedures
We report results from a subset of participants of The 90+ Study, an ongoing longitudinal study of aging and dementia in people aged 90 or older. Participants of The 90+ Study were recruited from two groups: (1) survivors of the Leisure World Cohort Study (LWCS) (Paganini-Hill, Ross, & Henderson, 1986), a health survey study in the 1980s of the residents of Leisure World, a retirement community in Orange County, California, who were aged 90 or older on or after January 1, 2003, when enrollment into The 90+ Study commenced, and (2) 90+ residents of Orange County, California, who lived within a two hour drive of the study location, and joined the study through open recruitment (Melikyan et al., 2018).
Eligible individuals could participate in The 90+ Study at any of four levels: (1) in-person, (2) over the telephone, (3) through an informant, (4) LWCS participants who died before they themselves could participate in The 90+ Study were included if an informant provided information on medical, family history and daily functioning. In-person participants undergo comprehensive semi-annual evaluations that include medical and family history, daily functioning, neurological examination, and neuropsychological testing. Based on participant’s choice, visits are done at the study office or at home. We travel across the U.S. to test participants who have moved after enrollment.
The study was approved by the University of California Irvine’s Institutional Review Board and all participants provided signed informed consent. Research was completed in accordance with the Helsinki Declaration.
Participants
Inclusion and exclusion criteria
This paper reports on a subset of The 90+ Study participants who had at least one inperson evaluation and were determined by neurological examiners to have normal cognition at the first in-person evaluation. There were no other inclusion/exclusion criteria.
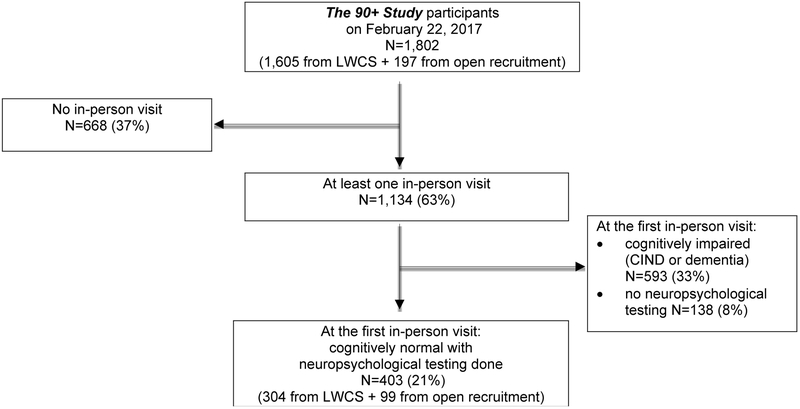
Of the 1,802 participants of The 90+ Study as of February 22, 2017 (figure 1), 1134 (63%) had an in-person visit. Of these, 593 were classified as having CIND/dementia at the first in-person evaluation and an additional 138 had no neuropsychological testing done leaving 403 for analysis. These 403 individuals include 159 cognitively normal participants included in our previous publication (Whittle et al., 2007).
Figure 1.
Flowchart of Participant Inclusion
LWCS – Leisure World Cohort Study.
All percentages are calculated from the total 90+ Study cohort (N=1,802)
Data Collection Instruments
Background information and history
We collected information on demographics, medical history (participants were asked: “Have you ever been diagnosed with cardiovascular, cancer, psychiatric, neurological, or metabolic disorders?”), current mediations, living situation, and instrumental activities of daily living (IADL). Information on subjective cognitive decline was not collected.
Neuropsychological test battery
A neuropsychological test battery of 11 tests indexed language, word list memory, executive function, attention and working memory, psychomotor speed, visual-spatial functions, construction; a questionnaire indexed symptoms of depression. The tests indexed different levels of cognitive ability while minimizing excessive floor and ceiling effects. Tests were administered in the order shown in Table 1 to maximize completion rates of the same tests in oldest-old participants who have high rates of incomplete testing due to fatigue. The average time to complete the entire battery was approximately one hour. Psychometrists, individuals with at least Bachelor’s degree in psychology or related field and trained by a licensed neuropsychologist (M.B.D.), administered the tests in a standardized way.
Table 1.
Neuropsychological test battery in the order of administration
| Tests in order of administration | Range of scores | Units |
|---|---|---|
| MMSE | 0-30 | Points |
| 3MS | 0-100 | Points |
| Animal Fluency | 0-max | No. of words in 1 min. |
| CVLT-II SF | ||
| Trials 1-4 | 0-9 | No. of words |
| Short Delay | 0-9 | No. of words |
| Clock Drawing | 0-8 | Points |
| Trail Making Test | ||
| A | 1-180, 0-max | Seconds, No. of errors |
| B | 1-300, 0-max | Seconds, No. of errors |
| C | 1-150, 0-max | Seconds, No. of errors |
| CVLT-II SF | ||
| Long Delay | 0-9 | No. of words |
| Cued Long Delay | 0-9 | No. of words |
| Recognition | 0-9 | No. of words |
| CERAD Constructions | 0-11 | Points |
| BNT-Short | 0-15 | No. of items |
| Letter F Fluency | 0-max | No. of words in 1 min. |
| Digit Span | ||
| Forward | 0-16 | Points |
| Backward | 0-14 | Points |
| Geriatric Depression Scale | 0-15 | Points |
Notes: MMSE – Mini-Mental State Examination, 3MS - Modified Mini-Mental State Exam, CVLT-II SF – California Verbal Learning Test-II Short Form, CERAD – The Consortium to Establish a Registry for Alzheimer’s Disease, BNT-Short – Boston Naming Test – Short Form (15 items)
Participants were asked to wear their eyeglasses and hearing aids during testing. In case of inability to complete a test due to sensory or motor impairment, a missing code indicated the reason for non-completion. Modifications, such as pairing printed and auditory stimuli and using enlarged boldface font for written information, were made to help compensate for sensory impairments. All test results, whether or not the whole battery was completed, were analyzed. Participants who did not complete the entire test battery were not excluded from analyses.
Cognitive screening tests included Modified Mini-Mental State Examination (3MS) (Teng & Chui, 1987) and Mini-Mental Status Examination (MMSE) (Folstein, Folstein, & McHugh, 1975). Most MMSE items are incorporated in the 3MS and the addition of two items (which floor the participant is on and writing a sentence) to the 3MS made it possible to derive a total score for both tests. Two minor changes were made to the standard administration procedures: (1) the three to-be-remembered words were printed on three separate cards in 90-size font and shown one at a time while the examiner simultaneously repeated the words aloud, (2) the 60-second Animal Fluency test (Morris et al., 1989) was substituted for the 3MS 30-second task of naming fourlegged animals.
Language was indexed using confrontational object naming, category (animals), and letter (F) (Gladsjo, Schuman, Miller, & Heaton, 1999; Heaton, Miller, Taylor, & Grant, 2004) fluencies. Object naming was indexed with the 15-item version of the Boston Naming Test (BNT-Short) (Fastenau, Denburg, & Mauer, 1998) to reduce administration time and fatigue. To avoid confusion with similar-sounding letters, a large “F” printed in 200-size font on a card was presented as a prompt.
Word list memory was indexed with California Verbal Learning Test - Second Edition, Short Form (CVLT-II SF) (Delis, Kramer, Kaplan, & Ober, 2000). Our modification was to present the words both verbally and visually (one at a time) during the four learning trials. A Short Delay Free Recall was administered following a 30-second interference task of counting backwards from 100 by ones. After approximately 10 minutes of nonverbal tasks, the Long Delay Free Recall was administered and tests of cued-recall and yes/no recognition administered immediately thereafter.
Executive functioning and attention were indexed using the Trail Making Tests (TMT) Parts A and B using standard administration procedures (Reitan & Wolfson, 1993). Completion time limit was 180 seconds for TMT A and 300 seconds for TMT B.
Working memory was indexed using Digit Span Forwards and Backwards from the Wechsler Adult Intelligence Scale-III (Wechsler, 1997). The administration and scoring followed standard procedures.
Psychomotor speed was indexed using a short and less tiring instrument developed by our group that is similar to the original Delis–Kaplan Executive Functioning System (D-KEFS) TMT Part C (Delis, Kaplan, & Kramer, 2001). Using the stimulus page from TMT Part A, we removed the numbers leaving the empty circles that we connected with a dotted line. We reversed the Part A starting and ending points, so that the Part A ending point (i.e., location of number 25) became the beginning position and the Part A starting point (i.e., location of the number 1) became the ending position. The participant’s task was to trace over the dotted line, connecting the circles as quickly as possible using a marker. Completion time limit was 150 seconds.
Visual-spatial and constructional abilities were indexed using the Clock Drawing test and the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Construction Test. In the Clock Drawing test, the participant was asked to fill in a predrawn, 4-inch diameter circle with numbers to represent a clock face and then to draw the hands at “ten after eleven”. In the CERAD Construction Test the participant was asked to copy circle, four-sided diamond, intersecting rectangles, and cube.
Symptoms of depression were characterized using the Geriatric Depression Scale (GDS) (Yesavage et al., 1982-1983).
More detailed information on testing procedures and scoring is provided in Supplementary Material.
Cognitive status assessment and diagnosis
Cognitive status was determined using: (1) a structured neurological examination, (2) the MMSE, 3MS, and Animal Fluency Test, (3) the Clinical Dementia Rating (CDR) scale (Morris, 1993) and (4) the Functional Activities Questionnaire (FAQ) (Pfeffer, Kurosaki, Harrah, Chance, & Filos, 1982). Participants were categorized based on the clinical diagnostic criteria as: (1) dementia, according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association, 1994), i.e., impaired performance on MMSE or 3MS subtests indexing at least two cognitive domains and inability to perform at least one IADL; (2) CIND, i.e., impaired performance on MMSE or 3MS subtests or some difficulty in performing IADLs due to cognition, but not meeting criteria for a dementia diagnosis (Graham et al., 1997); or (3) normal cognition, i.e., no substantial impairment on any cognitive domain (from subtests of MMSE, 3MS, or CDR) and no functional difficulties due to cognitive loss (from FAQ or CDR). Only individuals with normal cognition at their first in-person evaluation were included in the normative group.
Neurological examiners performed the cognitive status assessment and determined diagnostic classification at the end of the evaluation. No consensus diagnosis was used. Neurological examiners were physicians or nurse practitioners trained on the application of CIND and DSM-IV dementia diagnostic criteria by a licensed geriatric neurologist (C.K.).
We report norms on MMSE, 3MS, and animal fluency, that were used in determination of cognitive status, for two reasons: (1) these test scores were not the only criterion for cognitive diagnosis, another being performance in IADLs; (2) these tests are frequently used in aging and dementia settings and have low non-completion rates, making their norms useful.
If 4 or fewer scores on MMSE or 12 or fewer scores on 3MS were missing due to sensory, motor or other difficulties, proportional scores were computed: proportional MMSE score=((30*MMSE total)/(30-MMSE number of missing points)), proportional 3MS score=((100*3MS total)/(100-3MS number of missing points)). This calculation assumes that the score obtained without completing all items would be proportionally equal to the score that would have been obtained if all items had been completed. The fewer scores missing, the more accurately the proportional score represents the theoretical total score; therefore cut-offs for the number of missing items were established. If more than 4 scores in the MMSE or more than 12 scores in the 3MS were missing, proportional scores were not computed.
Data analysis
Means, standard deviations, and percentiles (5, 10, 25, 50, 75, 90, and 95 percentiles) are reported for each test. For ease of use and comparison, norms are provided for the same age groups as in our previous report (Whittle et al., 2007): 90–91, 92–94, and ≥95 years. The effect of age was assessed by regression analysis with age as a continuous variable. The age-adjusted independent effects of sex, education (the same categories as in our previous work (Whittle et al., 2007): high school or less, some college to college graduate, at least some graduate school were used for consistency and ease of comparison), and GDS score (<4 vs. ≥4) were assessed by multivariable regression analyses. Effect sizes are reported using Cohen’s d (Cohen, 1988). To compare characteristics among the age groups, we used Fisher’s exact tests for categorical variables and t-tests and ANOVAs for continuous variables. SAS version 9.4 (SAS Institute Inc., Cary, NC) was used for statistical analyses.
The paper provides age norms, norms by sex and education for the tests with significant sex/education effects after adjusting for age, and missing data. Norms for men and women separately and optional scores (performance on subtests and training samples, cued responses, and errors) are provided in the Supplementary Material (Supplementary Tables 1-7).
RESULTS
Group Demographics and Health
The sample of 403 cognitively normal participants (283 women and 120 men) has an average age of 94 years (range 90-102 years) (Table 2). Most participants were Caucasian (98.5%), well-educated (78% were educated beyond high school), and lived by themselves (63%). Education did not differ significantly among the three age groups (90-91, 92-94, ≥95) (P=.79, Fisher's exact test).
Table 2.
Characteristics of study participants
| Characteristic | Entire sample No (%) |
90-91 years No (%) |
92-94 years No (%) |
≥95 years No (%) |
|---|---|---|---|---|
| Sex | ||||
| Women | 283 (70.2) | 85 (69.1) | 118 (70.7) | 80 (70.8) |
| Men | 120 (29.8) | 38 (30.9) | 49 (29.3) | 33 (29.2) |
| Race | ||||
| Caucasian | 397 (98.5) | 121 (98.4) | 164 (98.2) | 112 (99.1) |
| Asian/Pacific Islander | 3 (.7) | 1 (8) | 1 (6) | 1 (0.9) |
| Spanish/Hispanic/Latino | 3 (.7) | 1 (8) | 2 (1.2) | 0 |
| Age (years) | 403 (100) | 123 (30.5) | 167 (41.4) | 113 (28.1) |
| Residence | ||||
| At home alone | 253 (62.8) | 84 (68.3) | 104 (62.3) | 65 (57.5) |
| At home with spouse/relatives/friends | 103 (25.6) | 33 (26.8) | 43 (25.7) | 27 (23.9) |
| Institution/group home/at home with paid caregiver | 47 (11.7) | 6 (4.9) | 20 (12.0) | 21 (18.6) |
| Education | ||||
| High school graduate or less | 90 (22.3) | 27 (22.0) | 41 (24.6) | 22 (19.5) |
| Some college to college graduate | 195 (48.4) | 62 (50.4) | 74 (44.9) | 58 (51.3) |
| Some graduate school to graduate/professional degree | 118 (29.3) | 34 (27.6) | 51 (30.5) | 33 (29.2) |
| Geriatric Depression Scale | ||||
| <4 depressive symptoms | 268 (79.1) | 87 (70.7) | 115 (68.9) | 66 (58.4) |
| ≥4 depressive symptoms | 71 (20.9) | 17 (13.8) | 26 (15.6) | 28 (24.8) |
| Medical history | ||||
| Hypertension | 248 (62.3) | 75 (61.0) | 104 (62.3) | 69 (61.1) |
| Heart diseasea | 197 (48.9) | 62 (50.4) | 77 (46.1) | 58 (51.3) |
| Cancer (other than skin) | 131 (32.5) | 40 (32.5) | 57 (34.1) | 34 (30.1) |
| Depression | 35 (8.8) | 7 (5.7) | 13 (7.8) | 15 (13.3) |
| Stroke | 27 (6.7) | 8 (6.5) | 11 (6.6) | 8 (7.1) |
| Diabetes | 24 (6.0) | 9 (7.3) | 9 (5.4) | 6 (5.3) |
| Psychoactive medications | ||||
| All psychoactive medicationsb | 83 (20.6) | 25 (20.3) | 33 (19.8) | 25 (22.1) |
| Anti-dementia medicationsc | 6 (1.5) | 2 (1.6) | 2 (1.2) | 2 (1.8) |
All percents are column percentages out of total sample of 403 participants
Heart disease includes: coronary artery disease, myocardial infarction, atrial fibrillation or other arrhythmias, heart valve disease, and congestive heart failure
All psychoactive medications include: narcotic analgesics, general anesthetics, anxiolytics, sedatives, hypnotics, CNS stimulants, antidepressants, antipsychotics, anti-parkinsonian, and anti-dementia medications
Anti-dementia medications include: cholinesterase inhibitors and/ or NMDA antagonist
The most frequent health problems were history of hypertension (62%), heart disease (49%) and non-skin cancer (33%), with no significant differences in prevalence among the three age groups (P=.52, Fisher's exact test). Although 9% of participants reported receiving a diagnosis of depression, over 20% had an elevated depression score (GDS≥ 4). The proportion of participants with GDS≥ 4 increased significantly with age (F(1, 233)=5.68, p=.02). Reporting a diagnosis of depression also increased with age, although not significantly (P=.11, Fisher's exact test).
At the time of testing 83 (21%) participants reported taking psychoactive medications (narcotic analgesics, general anesthetics, anxiolytics, sedatives, hypnotics, CNS stimulants, antidepressants, antipsychotics, antiparkinsonian) or anti-dementia medications (cholinesterase inhibitors or NMDA antagonist). Use of psychoactive medication was not significantly different among the three age groups (P=.88, Fisher's exact test). Only 6 (1.5%) participants were taking anti-dementia medications with no difference among the three age groups (P=.11, Fisher's exact test).
Effects of Age and Age-Adjusted Effects of Education, Sex, and Depressive Symptoms on Test Scores
With increasing age, total scores on MMSE, 3MS, BNT-Short number of spontaneous correct responses (henceforth listed as BNT-Short for brevity), animal fluency, free recall trials (including short and long delays) in CVLT-II SF, TMT A, and clock drawing test were significantly lower (Table 3).
Table 3.
Raw neuropsychological test scores (mean, standard deviation, percentiles) by age group
| Test | Age groupa | Nob | Mean | SD | 5% | 10% | 25% | 50% | 75% | 90% | 95% | B±SE /t/pc |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MMSE | 90-91 | 123 | 28.0 | 1.7 | 25 | 26 | 27 | 28 | 29 | 30 | 30 | −.11±.03 /−3.31 /<.01 |
| Total score | 92-94 | 166 | 28.2 | 1.7 | 25 | 26 | 27 | 28 | 30 | 30 | 30 | |
| ≥95 | 113 | 27.4 | 1.9 | 24 | 25 | 26 | 28 | 29 | 30 | 30 | ||
| Overall | 402 | 27.9 | 1.8 | 25 | 26 | 27 | 28 | 29 | 30 | 30 | ||
| 3MS | ||||||||||||
| Total score | 90-91 | 120 | 94.6 | 4.1 | 86 | 89 | 92 | 96 | 98 | 99 | 100 | −.28±.09 /−3.19 /<.01 |
| 92-94 | 155 | 94.4 | 4.4 | 85 | 89 | 92 | 96 | 98 | 99 | 100 | ||
| ≥95 | 102 | 93.1 | 4.9 | 84 | 88 | 91 | 94 | 96 | 98 | 99 | ||
| Overall | 377 | 94.1 | 4.5 | 85 | 88 | 92 | 95 | 97 | 99 | 100 | ||
| BNT-Shorttd | ||||||||||||
| Total correct | 90-91 | 97 | 13.2 | 1.8 | 10 | 11 | 12 | 14 | 14 | 15 | 15 | −.19±.04 /−4.24/<.01 |
| 92-94 | 131 | 12.8 | 1.9 | 9 | 10 | 11 | 13 | 14 | 15 | 15 | ||
| ≥95 | 76 | 12.1 | 2.0 | 9 | 9 | 11 | 12 | 14 | 15 | 15 | ||
| Overall | 304 | 12.8 | 1.9 | 9 | 10 | 11 | 13 | 14 | 15 | 15 | ||
| Animal Fluency | ||||||||||||
| Total correct | 90-91 | 122 | 14.8 | 4.2 | 9 | 10 | 12 | 14 | 17 | 20 | 23 | −.19±.08 /−2.25 /.02 |
| 92-94 | 166 | 14.7 | 3.8 | 9 | 10 | 12 | 14 | 18 | 20 | 22 | ||
| ≥95 | 112 | 13.8 | 4.0 | 8 | 9 | 11 | 13 | 16 | 19 | 22 | ||
| Overall | 400 | 14.5 | 4.0 | 9 | 10 | 12 | 14 | 17 | 20 | 22 | ||
| Letter F Fluency | ||||||||||||
| Total correct | 90-91 | 104 | 12.9 | 4.2 | 6 | 8 | 10 | 13 | 15 | 18 | 20 | .02±.09 /.27 /.79 |
| 92-94 | 138 | 12.7 | 3.9 | 7 | 7 | 10 | 13 | 16 | 17 | 19 | ||
| ≥95 | 93 | 12.7 | 4.5 | 6 | 7 | 10 | 12 | 15 | 19 | 22 | ||
| Overall | 335 | 12.8 | 4.2 | 7 | 8 | 10 | 13 | 15 | 18 | 20 | ||
| CVLT-II SF | ||||||||||||
| Trial 1 Number of words |
90-91 | 107 | 4.9 | 1.5 | 2 | 3 | 4 | 5 | 6 | 7 | 7 | −.08±.03 /−2.65 /.01 |
| 92-94 | 150 | 4.9 | 1.6 | 2 | 3 | 4 | 5 | 6 | 7 | 7 | ||
| ≥95 | 96 | 4.4 | 1.3 | 2 | 3 | 4 | 4 | 5 | 6 | 7 | ||
| Overall | 353 | 4.8 | 1.5 | 2 | 3 | 4 | 5 | 6 | 7 | 7 | ||
| Trial 4 Number of words |
90-91 | 106 | 7.8 | 1.2 | 5 | 6 | 7 | 8 | 9 | 9 | 9 | −.09±.03 /−3.30 /<.01 |
| 92-94 | 149 | 7.7 | 1.2 | 5 | 6 | 7 | 8 | 9 | 9 | 9 | ||
| ≥95 | 96 | 7.2 | 1.3 | 5 | 5 | 6 | 8 | 8 | 9 | 9 | ||
| Overall | 351 | 7.6 | 1.3 | 5 | 6 | 7 | 8 | 9 | 9 | 9 | ||
| Sum Trials1-4 Number of words |
90-91 | 106 | 27.0 | 4.5 | 19 | 20 | 24 | 27 | 30 | 32 | 34 | −.30±.09 /−3.12/<.01 |
| 92-94 | 149 | 26.9 | 4.4 | 18 | 20 | 25 | 27 | 30 | 32 | 33 | ||
| ≥95 | 96 | 24.8 | 4.4 | 17 | 19 | 21 | 25 | 29 | 31 | 32 | ||
| Overall | 351 | 26.3 | 4.5 | 18 | 20 | 23 | 27 | 30 | 32 | 33 | ||
| Short Delay Recall Number of words |
90-91 | 106 | 7.4 | 1.4 | 5 | 5 | 7 | 8 | 9 | 9 | 9 | −.09±.03 /−3.01 /.003 |
| 92-94 | 149 | 7.3 | 1.4 | 5 | 6 | 6 | 8 | 8 | 9 | 9 | ||
| ≥95 | 96 | 6.8 | 1.5 | 4 | 5 | 6 | 7 | 8 | 9 | 9 | ||
| Overall | 351 | 7.2 | 1.5 | 4 | 5 | 6 | 7 | 8 | 9 | 9 | ||
| Long Delay Recall Number of words |
90-91 | 105 | 6.9 | 1.9 | 3 | 4 | 6 | 7 | 8 | 9 | 9 | −.15±.04 /−3.62 /<.01 |
| 92-94 | 148 | 6.7 | 1.8 | 3 | 4 | 6 | 7 | 8 | 9 | 9 | ||
| ≥95 | 96 | 5.8 | 2.1 | 1 | 3 | 5 | 6 | 8 | 8 | 9 | ||
| Overall | 349 | 6.5 | 2.0 | 3 | 4 | 5 | 7 | 8 | 9 | 9 | ||
| Trail Making Test A | ||||||||||||
| Seconds | 90-91 | 102 | 57.2 | 25.1 | 99 | 87 | 71 | 49 | 39 | 35 | 31 | 1.09±.55 /1.99 /.05 |
| 92-94 | 130 | 55.3 | 18.8 | 88 | 82 | 66 | 51 | 42 | 34 | 30 | ||
| ≥95 | 78 | 63.4 | 29.0 | 128 | 103 | 74 | 57 | 45 | 38 | 33 | ||
| Overall | 310 | 58.0 | 24.0 | 104 | 87 | 69 | 53 | 42 | 35 | 31 | ||
| Trail Making Test B | ||||||||||||
| Seconds | 90-91 | 87 | 139.7 | 57.6 | 244 | 216 | 173 | 133 | 94 | 68 | 64 | 2.21±1.50/1.47 /.14 |
| 92-94 | 109 | 141.1 | 55.5 | 243 | 220 | 169 | 127 | 103 | 83 | 75 | ||
| ≥95 | 59 | 151.9 | 61.0 | 261 | 235 | 177 | 143 | 111 | 83 | 74 | ||
| Overall | 255 | 143.2 | 57.5 | 250 | 224 | 173 | 132 | 103 | 78 | 68 | ||
| Trail Making Test C | ||||||||||||
| Seconds | 90-91 | 99 | 24.5 | 9.9 | 45.0 | 37.0 | 31.0 | 22.0 | 18.0 | 14.0 | 13.0 | .46±.29 /1.60 /.11 |
| 92-94 | 124 | 25.8 | 12.7 | 50.0 | 42.0 | 31.5 | 22.0 | 18.0 | 13.0 | 12.0 | ||
| ≥95 | 70 | 27.0 | 12.9 | 55.0 | 44.5 | 32.0 | 24.0 | 18.0 | 14.5 | 13.0 | ||
| Overall | 293 | 25.7 | 11.9 | 48.0 | 40.0 | 31.0 | 23.0 | 18.0 | 14.0 | 13.0 | ||
|
Digit Span Forward+Backwards |
||||||||||||
| Total score | 90-91 | 86 | 15.2 | 3.3 | 10 | 12 | 13 | 15 | 17 | 20 | 22 | .06±.07 /.85 /.39 |
| 92-94 | 103 | 14.7 | 2.8 | 11 | 12 | 13 | 14 | 16 | 18 | 20 | ||
| ≥95 | 65 | 15.4 | 2.7 | 11 | 11 | 14 | 16 | 17 | 19 | 20 | ||
| Overall | 254 | 15.0 | 3.0 | 11 | 12 | 13 | 15 | 16 | 19 | 21 | ||
| Clock Drawing | ||||||||||||
| Total score | 90-91 | 110 | 6.2 | 1.7 | 4 | 4 | 5 | 7 | 8 | 8 | 8 | −.12±.04 /−3.13 /<.01 |
| 92-94 | 141 | 5.9 | 1.7 | 3 | 3 | 5 | 6 | 7 | 8 | 8 | ||
| ≥95 | 90 | 5.3 | 1.9 | 2 | 3 | 4 | 5 | 7 | 8 | 8 | ||
| Overall | 341 | 5.8 | 1.8 | 3 | 3 | 4 | 6 | 7 | 8 | 8 | ||
| CERAD Construction | ||||||||||||
| Total score | 90-91 | 99 | 9.0 | 1.4 | 7 | 7 | 8 | 9 | 10 | 11 | 11 | −.01±.03 /−.42 /.68 |
| 92-94 | 125 | 9.4 | 1.2 | 7 | 8 | 8 | 10 | 10 | 11 | 11 | ||
| ≥95 | 81 | 9.1 | 1.1 | 8 | 8 | 8 | 9 | 10 | 11 | 11 | ||
| Overall | 305 | 9.2 | 1.3 | 7 | 8 | 8 | 9 | 10 | 11 | 11 |
Notes: MMSE – Mini-Mental State Examination, 3MS - Modified Mini-Mental State Exam, BNT-Short – Boston Naming Test – Short Form (15 items), CVLT-II SF – California Verbal Learning Test-II Short Fonn, CERAD – The Consortium to Establish a Registry for Alzheimer’s Disease.
MMSE and 3MS were used in determination of cognitive status.
In years
Nmnber of participants does not always total 403 as not all the participants completed all the tests
B±SE /t /p – Parameter Estimate±Standard Error /t-value /p-value from linear regression analysis with age as a continuous variable
After adjusting for age, individuals with more education scored significantly higher than those with less education on MMSE, 3MS, BNT-Short, animal and letter F fluencies, and CERAD Construction (Table 4).
Table 4.
Raw neuropsychological test scores (mean, standard deviation) by age group for different education levels.
| Education Level | B±SE/t/pa | ||||
|---|---|---|---|---|---|
| Test | Age group | ≤ High school (HS) |
≤ College | > College | |
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| MMSE | N=90 | N=194 | N=118 | .29±.12 /2.39 /.02 | |
| Total score | 90-91 | 27.5 (2.1) | 28.0 (1.6) | 28.3 (1.3) | |
| 92-94 | 27.8 (1.9) | 28.2 (1.7) | 28.3 (1.7) | ||
| ≥95 | 26.9 (2.1) | 27.6 (1.7) | 27.5 (2.2) | ||
| Overall | 27.5 (2.0) | 28.0 (1.7) | 28.1 (1.8) | ||
| 3MS | N=85 | N=185 | N=109 | 1.45±.31 /4.62 /<.01 | |
| Total score | 90-91 | 92.5 (4.3) | 94.7 (4.3) | 96.1 (3.0) | |
| 92-94 | 92.5 (5.2) | 94.6 (3.9) | 95.8 (4.0) | ||
| ≥95 | 91.7 (7.2) | 93.4 (4.2) | 93.3 (4.3) | ||
| Overall | 92.3 (5.4) | 94.3 (4.2) | 95.2 (4.0) | ||
| BNT-Short | N=61 | N=157 | N=86 | .44±.16 /2.80 /<.01 | |
| Total correct | 90-91 | 12.3 (2.7) | 13.6 (1.4) | 13.1 (1.5) | |
| 92-94 | 12.3 (2.0) | 12.8 (2.0) | 13.3 (1.6) | ||
| ≥95 | 11.2 (2.1) | 12.3 (1.8) | 12.2 (2.0) | ||
| Overall | 12.1 (2.3) | 12.9 (1.9) | 13.0 (1.8) | ||
| Animal Fluency | N=90 | N=193 | N=117 | .79±.28 /2.86 /<.01 | |
| Total correct | 90-91 | 13.3 (4.0) | 14.5 (4.1) | 16.6 (4.2) | |
| 92-94 | 14.2 (3.8) | 14.6 (3.7) | 15.3 (4.0) | ||
| ≥95 | 13.8 (3.5) | 13.7 (3.3) | 14.1 (5.3) | ||
| Overall | 13.8 (3.8) | 14.3 (3.7) | 15.4 (4.5) | ||
| Letter F Fluency | N=68 | N=168 | N=99 | .99±.32 /3.10 /<.01 | |
| Total correct | 90-91 | 11.1 (3.1) | 13.4 (4.4) | 13.1 (4.4) | |
| 92-94 | 11.1 (3.8) | 13.1 (4.0) | 13.2 (3.5) | ||
| ≥95 | 11.1 (4.5) | 12.8 (4.5) | 13.6 (4.3) | ||
| Overall | 11.1 (3.8) | 13.1 (4.3) | 13.3 (3.9) | ||
| CERAD Construction | N=90 | N=195 | N=118 | .22±.10 /2.17 /.03 | |
| Total score | 90-91 | 8.8 (1.4) | 9.4 (1.3) | 8.8 (0.8) | |
| 92-94 | 8.9 (1.4) | 9.2 (1.3) | 9.2 (1.2) | ||
| ≥95 | 9.5 (1.1) | 9.6 (1.2) | 9.2 (1.1) | ||
| Overall | 9.1 (1.2) | 9.1 (1.3) | 9-5 (1.1) | ||
Notes: Scores are provided only for tests for which education level significantly contributed to test performance after controlling for age. MMSE – Mini-Mental State Examination, 3MS - Modified Mini-Mental State Exam, BNT-Short – Boston Naming Test – Short Form (15 items)
B±SE /t /p – Parameter Estimate±Standard Error /t-value /p-value from linear regression analysis with age as continuous and education as categorical variable (high school or less, some college to completed college, some graduate school to completed graduate school)
After adjusting for age, men scored higher than women on BNT-Short, whereas women scored significantly higher than men on the MMSE and CVLT-II SF (Trials 2, 3, 4, Sum of Trials 1-4, short- and long-delay free recall). Effect sizes as measured by Cohen’s d were small to medium (.25 to .36) (Table 5).
Table 5.
Raw neuropsychological test scores (mean, standard deviation) by age group for women and men.
| Sex | B±SE /t /pa |
Effect size
Cohen’s d |
|||
|---|---|---|---|---|---|
| Test | Age group | Women | Men | ||
| Mean (SD) | Mean (SD) | ||||
| MMSE | N=282 | N=120 | .59±.19 /3.11 /<.01 | −.33 | |
| Total score | 90-91 | 28.0 (1.7) | 28.0 (1.7) | ||
| 92-94 | 28.5 (1.5) | 27.4 (2.0) | |||
| ≥95 | 27.6 (1.9) | 27.0 (2.0) | |||
| Overall | 28.1 (1.7) | 27.5 (1.9) | |||
| BNT-Short | N=212 | N=103 | −.65±.23 /−2.76 /<.01 | .34 | |
| Total correct | 90-91 | 13.0 (2.0) | 13.5 (1.3) | ||
| 92-94 | 12.7 (2.0) | 13.2 (1.8) | |||
| ≥95 | 11.8 (2.0) | 12.8 (1.7) | |||
| Overall | 12.6 (2.0) | 13.2 (1.6) | |||
| CVLT-II SF Trial 2 | N=283 | N=120 | .36±.16 /2.23 /.03 | −.25 | |
| Number of words | 90-91 | 7.0 (1.4) | 6.3 (1.4) | ||
| 92-94 | 6.9 (1.3) | 6.6 (1.2) | |||
| ≥95 | 6.2 (1.5) | 6.3 (1.3) | |||
| Overall | 6.8 (1.4) | 6.4 (1.3) | |||
| CVLT-II SF Trial 3 | N=283 | N=120 | .46±.15 /3.04 /<.01 | −.35 | |
| Number of words | 90-91 | 7.6 (1.3) | 7.1 (1.3) | ||
| 92-94 | 7.6 (1.1) | 7.0 (1.4) | |||
| ≥95 | 7.1 (1.4) | 6.8 (1.3) | |||
| Overall | 7.4 (1.3) | 7.0 (1.4) | |||
| CVLT-II SF Trial 4 | N=283 | N=120 | .45±.14 /3.14 /<.01 | −.36 | |
| Number of words | 90-91 | 8.0 (1.1) | 7.5 (1.1) | ||
| 92-94 | 7.9 (1.2) | 7.4 (1.2) | |||
| ≥95 | 7.3 (1.2) | 7.0 (1.5) | |||
| Overall | 7.7 (1.2) | 7.3 (1.3) | |||
| CVLT-II SF Trials 1-4 | N=248 | N=103 | 1.53±.52 /2.97 /<.01 | −.33 | |
| Number of words | 90-91 | 27.6 (4.4) | 25.5 (4.5) | ||
| 92-94 | 27.3 (4.3) | 25.7 (4.4) | |||
| ≥95 | 25.1 (4.6) | 24.2 (3.9) | |||
| Overall | 26.8 (4.5) | 25.3 (4.3) | |||
| CVLT-II SF Short Delay | N=248 | N=103 | .55±.17 /3.34 /<.01 | −.38 | |
| Number of words | 90-91 | 7.7 (1.4) | 6.9 (1.5) | ||
| 92-94 | 7.5 (1.4) | 6.9 (1.2) | |||
| ≥95 | 6.8 (1.4) | 6.6 (1.9) | |||
| Overall | 7.4 (1.4) | 6.8 (1.5) | |||
| CVLT-II SF Long Delay | N=246 | N=103 | .80±.22 /3.55 /<.01 | −.40 | |
| Number of words | 90-91 | 7.4 (1.7) | 5.9 (2.0) | ||
| 92-94 | 6.9 (1.8) | 6.1 (1.8) | |||
| ≥95 | 5.7 (2.1) | 5.8 (2.3) | |||
| Overall | 6.7 (1.9) | 5.9 (2.0) | |||
Notes: Scores provided only for tests for which gender significantly contributed to test performance after controlling for age. MMSE – Mini-Mental State Examination, BNT-Short – Boston Naming Test – Short Form, CVLT-II SF – California Verbal Learning Test-II Short Form
B±SE /t /p – Parameter Estimate±Standard Error /t-value /p-value from linear regression analysis with age as continuous and sex as categorical variable
A higher GDS score was significantly associated with lower scores on 3MS, BNT-Short, animal and letter F fluencies, CVLT-II SF Trial 4, short- and long-delay free recall, and TMT A (results not shown).
Adjustment for education did not alter the effects of sex and GDS score on test scores.
Comparison of Participants Who Did and Did Not Complete All the Tests
Not all participants completed all tests, primarily due to fatigue, sensory impairments or time constraints (Table 6). Hearing problems accounted for non-completion in 0.8-3.5% of participants (depending on the test), but the non-completion rate did not differ among the three age groups (P=.33, Fisher's exact test) (Table 7). Non-completion due to motor symptoms (such as tremor) significantly increased with age from 0% in the 90-91 group to 1-2.4% in the two older age groups (P<.01, Fisher's exact test). Vision impairment accounted for about 6% of non-completion in the two younger groups and significantly increased to about 16% in the ≥95 age group (P=.01, Fisher's exact test).
Table 6.
Percent of participantsa who completed and did not complete each neuropsychological test and reasons for non-completion
| Reasons for non-completion | ||||||||
|---|---|---|---|---|---|---|---|---|
| Cognitive Tests and Domains they index | Completed | Fatigue | Hearing | Vision | Cognitionb | Refused | Out of Timec |
Otherd |
| Cognitive Screening Tests | ||||||||
| MMSE Total score | 99.8 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 |
| 3MS Total score | 93.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 6.5 |
| Language | ||||||||
| BNT-Short Total correct | 75.4 | 4.5 | 0.0 | 7.9 | 0.0 | 1.0 | 10.2 | 0.3 |
| Animal Fluency Total correct | 99.3 | 0.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.3 |
| Letter F Fluency Total correct | 83.1 | 5.5 | 0.0 | 0.0 | 0.0 | 1.5 | 9.4 | 0.5 |
| Verbal Memory | ||||||||
| CVLT-II SF Number of words | 87.6 | 2.5 | 0.5 | 0.0 | 0.0 | 0.7 | 8.7 | 0.0 |
| Executive Function/Attention | ||||||||
| Trail Making Test A Seconds | 76.9 | 3.2 | 0.0 | 9.2 | 0.0 | 1.5 | 7.4 | 1.7 |
| Trail Making Test B Seconds | 63.3 | 3.2 | 0.0 | 9.7 | 7.4 | 2.0 | 9.9 | 4.5 |
| Psychomotor Speed | ||||||||
| Trail Making Test C Seconds | 72.7 | 3.7 | 0.0 | 8.9 | 0.0 | 3.0 | 10.4 | 1.2 |
| Working Memory | ||||||||
| Digit Span Test Total score | 63.0 | 5.7 | 2.2 | 0.0 | 0.0 | 1.0 | 27.5 | 0.5 |
| Construction | ||||||||
| Clock Drawing Total score | 84.6 | 2.5 | 0.0 | 6.7 | 0.0 | 1.0 | 4.2 | 1.0 |
| CERAD Construction Total score | 75.7 | 4.0 | 0.0 | 7.7 | 0.0 | 1.7 | 9.4 | 1.5 |
Notes: MMSE – Mini-Mental State Examination, 3MS - Modified Mini-Mental State Exam, BNT-Short – Boston Naming Test – Short Form (15 items), CVLT-II SF – California Verbal Learning Test-II Short Form, CERAD – The Consortium to Establish a Registry for Alzheimer’s Disease
Percent of participants out of the total 403 participants in the study sample
Could not understand instructions, became confused, forgot instructions
Ran out of time for the entire neuropsychological assessment, not individual test
Equipment error, tester error, other physical impairment of participant, e.g., tremor, alternate test given, quit after starting
Table 7.
Percent of participants who did not complete tests due to sensory or motor impairment by age groupa
| Reasons for non completion | ||||
|---|---|---|---|---|
| Cognitive Test | Age group | Hearing (%) | Vision (%) | Physical impairment (%) |
| BNT-Short Total correct | 90-91 | - | 5.7 | - |
| 92-94 | - | 5.4 | - | |
| ≥95 | - | 14.2 | - | |
| Trail Making Test A Seconds | 90-91 | 5.7 | 0.0 | |
| 92-94 | - | 6.6 | 2.4 | |
| ≥95 | - | 16.8 | 1.8 | |
| Trail Making Test B Seconds | 90-91 | - | 6.5 | 0.0 |
| 92-94 | - | 7.2 | 2.4 | |
| ≥95 | - | 16.8 | 1.8 | |
| Trail Making Test C Seconds | 90-91 | - | 6.5 | 0.0 |
| 92-94 | - | 6.0 | 2.4 | |
| ≥95 | - | 15.9 | 0.9 | |
| CVLT-II SF Number of words | 90-91 | 0.8 | - | - |
| 92-94 | 0.0 | - | - | |
| ≥95 | 0.9 | - | - | |
| Digit Span Test Total score | 90-91 | 2.4 | - | - |
| 92-94 | 1.2 | - | - | |
| ≥95 | 3.5 | - | - | |
Notes: BNT-Short – Boston Naming Test – Short Form (15 items), CVLT-II SF – California Verbal Learning Test-II Short Form,
Percent of participants out of the total 403 in the study sample
On the cognitive screening tests, 363 participants (90%) completed all MMSE items and 39 participants (10%) had 1-4 missing scores. The average MMSE score for participants who completed all items (Mean=27.9, SD=1.7) did not differ from the proportional MMSE score computed for participants with 1-4 missing scores (Mean=27.4, SD=2.2; t(43)=1.54, p=.13). All 3MS items were completed by 362 participants (96%); 15 participants (4%) had 1-12 missing scores. The average 3MS score for participants who completed all 3MS items (Mean=94.2, SD=4.4) was higher than the proportional 3MS score computed for participants with 1-12 missing scores (Mean=91.3, SD=5.6; t(375)=2.49, p=.01).
Within the entire testing battery, completion rates were high for tests administered first: MMSE (>99%), 3MS (94%) and Animal Fluency (99%). In comparison, tests administered towards the end of the battery were least likely to be completed: TMT B (63%) and Digit Span Test (63%). MMSE and 3MS scores were significantly higher among those who completed compared with those who did not complete select neuropsychological tests (BNT-Short, CVLT, TMT B and C, Digit Span, CERAD for MMSE and 3MS; TMT A also for 3MS) (Table 8).
Table 8.
Raw MMSE and 3MS scores for participants who completed and did not complete specific neuropsychological tests
| MMSE |
3MS |
|||||||
|---|---|---|---|---|---|---|---|---|
| Test Missing | Mean for completed |
Mean for missing |
t-test | p-value | Mean for completed |
Mean for missing |
t-test | p-value |
| BNT-Short Total correct | 28.0 | 27.4 | −2.98 | <.01 | 94.5 | 92.7 | −2.85 | <.01 |
| Animal Fluency Total score | 27.9 | 27.7 | 1.73 | .08 | 94.1 | 94.0 | −0.03 | .97 |
| Letter F Fluency Total score | 27.9 | 29.7 | −0.98 | .33 | 94.2 | 93.5 | −1.28 | .20 |
| CVLT-II SF Number of words | 28.0 | 27.4 | −2.23 | .03 | 94.5 | 91.4 | −3.67 | <.01 |
| Trail Making Test A Seconds | 28.0 | 27.6 | −1.81 | .07 | 94.5 | 92.4 | −3.42 | <.01 |
| Trail Making Test B Seconds | 28.1 | 27.4 | −3.77 | <.01 | 95.0 | 92.3 | −5.48 | <.01 |
| Trail Making Test C Seconds | 28.0 | 27.5 | −2.42 | .02 | 94.7 | 92.2 | −3.92 | <.01 |
| Digit Span Total score | 28.1 | 27.6 | −2.80 | <.01 | 94.8 | 93.0 | −3.56 | <.01 |
| Clock Drawing Total score | 27.9 | 27.8 | −0.22 | .82 | 94.2 | 92.9 | −1.70 | .09 |
| CERAD Construction Total score | 28.0 | 27.5 | −2.27 | .02 | 94.5 | 92.3 | −3.85 | <.01 |
Notes: BNT-Short – Boston Naming Test – Short Form (15 items), CVLT-II SF – California Verbal Learning Test-II Short Form, CERAD – The Consortium to Establish a Registry for Alzheimer’s Disease
DISCUSSION
This report extends the available neuropsychological test norms for cognitively normal individuals aged 90 or older. We report norms by age group, sex and education which, along with symptoms of depression, influence test performance. These norms allow differentiation of cognitively normal individuals from those with cognitive impairment (CIND or dementia). In contrast, the norms in our earlier publication (Whittle et al., 2007) were helpful in distinguishing between oldest-old with dementia and those without dementia (cognitively normal and CIND).
Consistent with our previous publication (Whittle et al., 2007) and other reports (Dore, Elias, Robbins, Elias, & Brennan, 2007; Elias, Elias, D'Agostino, Silbershatz, & Wolf, 1997; Harada, Natelson Love, & Triebel, 2013), the current analysis shows that performance on screening measures and on tests indexing attention, language, verbal memory, and construction declines significantly with advancing age. Age-related change in cognitive performance including decline in speeded aspects of activity (Eckert, Keren, Roberts, Calhoun, & Harris, 2010), failure to suppress irrelevant information (Dumas & Hartman, 2008), and decreased use of strategies to improve learning and memory (Davis et al., 2013) is thought to be associated with structural and functional brain changes in older adults (Hafkemeijer et al., 2014; Liu et al., 2017). Counter to our previous report (Whittle et al., 2007), the current sample showed no age effect on TMT B or Digit Span Backwards. In The 90+ Study group and others (Rasmusson, Zonderman, Kawas, & Resnick, 1998) CIND explains larger proportion of variance in test performance than age.
In the current sample, education, sex and symptoms of depression contributed to test performance independently of age. Similarly to others (Au et al., 2004; Dore et al., 2007; Elias et al., 1997; Ganguli et al., 2010; Saykin et al., 1995), we found an effect of education on cognitive screening tests and on tests that index naming, verbal fluency and construction. As education is implicated in cognitive reserve, slower age-related cognitive decline and overall test-wiseness (de Azeredo Passos et al., 2015; Gasquoine, 2009; Stern, 2012), it can contribute to test performance.
In the current group, men scored significantly higher than women on the test indexing naming, but lower on the cognitive screening tests and verbal memory. Higher scores on the naming test in men than women have been reported previously, with no consensus on the mechanisms of these differences. Factors that have been explored include IQ and white matter changes (Hall, Vo, Johnson, Wiechmann, & O'Bryant, 2012). Though men in our group were slightly more educated than women, education did not explain sex differences in test performance. Higher performance of women than men on cognitive screening tests and tests indexing verbal memory has been demonstrated previously and ascribed to different approaches to encoding and learning in men and women or hormonal factors (Gale, Baxter, Connor, Herring, & Comer, 2007; Hogervorst, Rahardjo, Jolles, Brayne, & Henderson, 2012; Rosselli, Tappen, Williams, & Salvatierra, 2006). Although the observed effect sizes of sex differences in test performance were not large, use of sex-specific norms is recommended when available.
The well-documented association of elevated scores on depression measures with lower cognitive performance (Koenig, Bhalla, & Butters, 2014; Morimoto & Alexopoulos, 2013) was observed in our group on cognitive screening tests and on tests that index memory, verbal fluency, and attention. This could be related to poor effort, underlying subclinical dementia, or disruption in structural and functional brain integrity due to factors such as cerebrovascular pathology (Weisenbach, Boore, & Kales, 2012).
The prevalence of self-reported health problems in our group is similar to other reports for the oldest-old (Lee, Go, Lindquist, Bertenthal, & Covinsky, 2008; Nosraty, Sarkeala, Hervonen, & Jylhä, 2012). We found no differences among the three age groups, which agrees with reports of no age change or a decline with age in nonagenarians and centenarians (Kheirbek et al., 2017; Selim et al., 2005). Therefore decline in test performance with age cannot be ascribed to differential impact of health problems in our three age groups.
The prevalence of psychoactive medication use in our group was similar to that reported in other studies of the oldest-old (Blumstein, Benyamini, Chetrit, Mizrahi, & Lerner-Geva, 2012; Wastesson, Parker, Fastbom, Thorslund, & Johnell, 2012). We observed no age difference in intake which is consistent with other reports (Wastesson et al., 2012). Therefore we cannot ascribe the decline in test performance with age to the differential impact of psychoactive medication.
The decline in test scores with age may be related to neurodegeneration, as discussed above, but also to sensory or motor impairments. Indeed, in our sample, test non-completion due to visual or motor impairments increased with age. Cross-sectional and longitudinal studies report increased prevalence and risk of cognitive impairment in individuals with sensory impairments (Maharani et al., 2018; Mitoku, Masaki, Ogata, & Okamoto, 2016).
Scores in this paper are generally comparable with other reports on cognitively normal oldest-old (Boeve et al., 2003; Fine, Kramer, Lui, Yaffe, & Group, 2012; Iacono et al., 2014; Ivnik, Malec, Smith, Tangalos, & Petersen, 1996; I. N. Miller et al., 2015; National Alzheimer's Coordinating Center, 2017; Tombaugh, Kozak, & Rees, 1999; Weintraub et al., 2018; Zubenko, Zubenko, Maher, & Wolf, 2007). As expected, our scores are consistently higher than in studies of non-demented oldest-old that included both normal individuals and those with mild forms of cognitive impairment (Brayne, Gill, Paykel, Huppert, & O'Connor, 1995; Carrión-Baralt, Meléndez-Cabrero, Schnaider Beeri, Sano, & Silverman, 2009; Cherry et al., 2011; Elias et al., 2011; Iacono et al., 2014; Pioggiosi, Berardi, Ferrari, Quartesan, & De Ronchi, 2006; Steen, Sonn, Hanson, & Steen, 2001; Wahlin et al., 1993; Whittle et al., 2007). This is most likely due to the inclusion of individuals with mild forms of cognitive impairment in other studies as well as possible age and education differences between cohorts. Reports on centenarians and near centenarians provide lower test scores compared with our group, which could be due to higher age and the possible inclusion of cognitively impaired individuals in other cohorts (Beker et al., 2018; Davey et al., 2013; Davey et al., 2010; Ganz et al., 2018; Hagberg, Bauer Alfredson, Poon, & Homma, 2001; Jopp, Park, Lehrfeld, & Paggi, 2016; L. S. Miller et al., 2010).
Compared with the oldest-old population in the U.S. (He & Muenchrath, 2011), our sample differs little by sex (70% vs. 74% female), has a higher proportion of Caucasians (98.5% vs. 88%) and is much more highly educated (78% vs. 28% having more than a high school education). Although our group is not representative of other races, Caucasians are currently the overwhelming majority of the oldest-old in the U.S., which makes our work relevant for most U.S. oldest-old at the present time. Our greater proportion of Caucasians is likely related to the ethnic composition of the recruitment area and highlights challenges associated with recruitment of underrepresented racial groups (Zhou et al., 2017). Our sample does not adequately represent cultural parameters, approximated by race, that are critical for test performance (Harris & Llorente, 2005). Therefore applicability of present norms to other racial and ethnic groups is limited. In the absence of appropriate norms it is advisable to use norms from samples most closely matching characteristics of a test-taker and to be aware of the sources of variation of test performance in different cultural groups (Ardila, 2007).
We report norms by sex and education for cognitively unimpaired oldest-old. Although in older adults quality of education (measured by reading level) (Manly, Jacobs, Touradji, Small, & Stern, 2002) or IQ score (Steinberg, Bieliauskas, Smith, Langellotti, & Ivnik, 2005) is more closely associated with neuropsychological test performance than level of education, we believe that by stratifying norms by education level we likely accounted for some environmental and individual characteristics related to quality of education and IQ.
Like the majority of previously reported neuropsychological test norms, the present norms were derived from a group of participants whose cognitive status was determined cross-sectionally at the baseline evaluation. Despite our best attempt to exclude individuals with cognitive difficulties by applying clinical diagnostic criteria, a weakness of the cross-sectional approach is that individuals who go on to develop dementia may still be included into the normative sample (Sliwinski et al., 1996). In contrast, deriving norms from individuals who are cognitively normal at baseline and remain normal for several years minimizes the inclusion of individuals with preclinical dementia. This longitudinal approach to cognitive status determination likely provides greater sensitivity for the detection of cognitive impairment (Masur, Sliwinski, Lipton, Blau, & Crystal, 1994; Sliwinski et al., 1996). While attractive, this approach has a number of drawbacks, including the limited life expectancy in the oldest-old. However, given the potential advantages of longitudinally-determined norms, we plan to explore their utility for the oldest-old.
Strengths and limitations
This paper has several notable strengths. First, we report data on one of the largest well-characterized groups of cognitively normal 90+ year-olds. The large sample size made it possible to provide norms by sex and education in each of the three relatively narrow age groups. In most cases our cell size is 50 or more participants, a desirable number for stable estimate of population mean (D'Elia, Satz, & Schretlen, 1989). Most, but not all (Ivnik et al., 1996), normative reports collapse individuals aged 90 and older into one age group or have much smaller cell sizes. With no upper age limit, we have a wider age range than age-restricted studies (Boeve et al., 2003). Second, this paper, like some (Davey et al., 2010; Iacono et al., 2014; Ivnik et al., 1996; Pioggiosi et al., 2006; Tombaugh et al., 1999; Wahlin et al., 1993; Weintraub et al., 2018), but not all (Au et al., 2004; Elias et al., 2011; Fine et al., 2012) normative publications, is based on data from a study specifically designed as a cognitive aging study and uses tests well suited for the oldest-old. The tests are relatively short and involve modifications of procedures and stimuli to accommodate the sensory deficits and reduced stamina that often confound cognitive testing in old age. Third, norms are reported for tests indexing a wide range of cognition and are most frequently used by neuropsychologists. Fourth, we provide more detailed normative information, including several percentile ranges, than the majority of publications on the topic. Fifth, the detailed description of our testing procedures and scoring system facilitates data replication and tests usage. Sixth, every effort was made to collect as much testing data as possible by testing participants in their homes including travelling to other states. Seventh, cognitive status determination was based on clinical diagnostic criteria applied by trained clinicians (and not on self-report or a screening measure cut-off score) ensuring that only individuals with normal cognition were included.
We acknowledge several limitations. First, our sample represents mostly well-educated Caucasians, which limits the applicability of reported norms. Second, not all participants completed the entire test battery. Had those tests been completed, they might have affected the reported normative values. Supporting this, our analysis showed lower scores in the cognitive screening tests in individuals who did not complete individual tests compared with those who did. One of the reasons for test non-completion might be that some of the tests were more challenging than others. While we chose tests of various levels of difficulty in order to assess a wide range of cognitive abilities, other projects may benefit from a limited battery to decrease frustration, provide more valid results, and increase completion rates. Third, fixed, compared to counterbalanced test order did not allow us to account for potential effects of the order of test administration. For instance, anxiety at the beginning and fatigue at the end of the testing may impact test performance, as may order effects such that tests administered earlier might facilitate or halt performance on subsequent tests (Franzen, Smith, Paul, & MacInnes, 1993; Llorente, Sines, Rozelle, Turcich, & Casatta, 2000). Despite the disadvantages, in The 90+ Study we elected to use a fixed order to ensure high completion rates of at least a few tests, given that fatigue is a major reason for test non-completion in the oldest-old. Fourth, although we strived to make our test battery comprehensive, we did not index all possible domains (e.g., fine motor skills or visual memory) in order to keep the battery short. Fifth, we report norms on the MMSE, 3MS, and Animal Fluency, even though these tests were used as criteria for normal cognition. We report these norms because the tests are frequently used in aging and dementia settings and their norms for the oldest-old are much needed, but the users need to be aware of the potential circularity. Sixth, the number of centenarians is limited in our group therefore we combined them with those aged 95 and older. We hope to provide norms for centenarians in the future as more 90+ Study participants survive to this age.
CONCLUSIONS
Cross-sectional test norms derived from a group of cognitively normal individuals aged 90+ are instrumental in differentiating cognitively normal from impaired oldest-old. To our knowledge, this is one of the few reports on cognitive test norms derived from a large and well-characterized group of oldest-old individuals without cognitive impairment.
Supplementary Material
ACKNOWLEDGEMENTS:
The authors do not have any conflicts of interest to disclose. This work was supported by the National Institute on Aging (C.H.K., M.M.C., Z.A.M., A.P-H., C.W. grant # R01AG021055; MBD, grant # P50 AG016573). The authors thank the participants and their relatives, testers, examiners and staff of The 90+ Study.
REFERENCES
- American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association. [Google Scholar]
- Ardila A (2007). The impact of culture on neuropsychological test performance In Uzzell BP, Ponton MO, & Ardila A (Eds.), International Handbook of Cross-Cultural Neuropsychology (pp. 23–45). Mahwah, New Jersey: Lawrence Erlbaum Associates, Publishers. [Google Scholar]
- Au R, Seshadri S, Wolf PA, Elias M, Elias P, Sullivan L, … D'Agostino RB (2004). New norms for a new generation: cognitive performance in the framingham offspring cohort. Exp Aging Res, 30(4), 333–358. doi: 10.1080/03610730490484380 [DOI] [PubMed] [Google Scholar]
- Beker N, Sikkes SAM, Hulsman M, Schmand B, Scheltens P, & Holstage H (2018). Neuropsychological test performance of cognitively healthy centenarians: Normative data from the Dutch 100-plus study. In: bioRxiv The reprint server for biology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumstein T, Benyamini Y, Chetrit A, Mizrahi EH, & Lerner-Geva L (2012). Prevalence and correlates of psychotropic medication use among older adults in Israel: cross-sectional and longitudinal findings from two cohorts a decade apart. Aging Ment Health, 16(5), 636–647. doi: 10.1080/13607863.2011.644262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeve B, McCormick J, Smith G, Ferman T, Rummans T, Carpenter T, … Petersen R (2003). Mild cognitive impairment in the oldest old. Neurology, 60(3), 477–480. [DOI] [PubMed] [Google Scholar]
- Brayne C, Gill C, Paykel ES, Huppert F, & O'Connor DW (1995). Cognitive decline in an elderly population--a two wave study of change. Psychol Med, 25(4), 673–683. [DOI] [PubMed] [Google Scholar]
- Carrión-Baralt JR, Meléndez-Cabrero J, Schnaider Beeri M, Sano M, & Silverman JM (2009). The neuropsychological performance of nondemented Puerto Rican nonagenarians. Dement Geriatr Cogn Disord, 27(4), 353–360. doi: 10.1159/000209213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry KE, Brown JS, Marks LD, Galea S, Volaufova J, Lefante C, … Jazwinski SM (2011). Longitudinal Assessment of Cognitive and Psychosocial Functioning After Hurricanes Katrina and Rita: Exploring Disaster Impact on Middle-Aged, Older, and Oldest-Old Adults. J Appl Biobehav Res, 16(3-4), 187–211. doi: 10.1111/j.1751-9861.2011.00073.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic. [Google Scholar]
- Corrada MM, Brookmeyer R, Paganini-Hill A, Berlau D, & Kawas CH (2010). Dementia incidence continues to increase with age in the oldest old: the 90+ study. Ann Neurol, 67(1), 114–121. doi: 10.1002/ana.21915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Elia L, Satz P, & Schretlen D (1989). Wechsler Memory Scale: a critical appraisal of the normative studies. J Clin Exp Neuropsychol, 11(4), 551–568. doi: 10.1080/01688638908400913 [DOI] [PubMed] [Google Scholar]
- Davey A, Dai T, Woodard JL, Miller LS, Gondo Y, Johnson MA, … Centenarian G (2013). Profiles of cognitive functioning in a population-based sample of centenarians using factor mixture analysis. Exp Aging Res, 39(2), 125–144. doi: 10.1080/0361073X.2013.761869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey A, Elias MF, Siegler IC, Lele U, Martin P, Johnson MA, … Poon LW (2010). Cognitive function, physical performance, health, and disease: norms from the georgia centenarian study. Exp Aging Res, 36(4), 394–425. doi: 10.1080/0361073X.2010.509010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis HP, Klebe KJ, Guinther PM, Schroder KB, Cornwell RE, & James LE (2013). Subjective organization, verbal learning, and forgetting across the life span: from 5 to 89. Exp Aging Res, 39(1), 1–26. doi: 10.1080/0361073X.2013.741956 [DOI] [PubMed] [Google Scholar]
- de Azeredo Passos VM, Giatti L, Bensenor I, Tiemeier H, Ikram MA, de Figueiredo RC, … Barreto SM (2015). Education plays a greater role than age in cognitive test performance among participants of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Neurol, 15, 191. doi: 10.1186/s12883-015-0454-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kaplan E, & Kramer JH (2001). Delis-Kaplan Executive Function System (D-KEFS): Pearson. [DOI] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, & Ober BA (2000). CVLT-II: California Verbal Learning Test. (2nd ed.): The Psychological Corporation. [Google Scholar]
- Dore GA, Elias MF, Robbins MA, Elias PK, & Brennan SL (2007). Cognitive performance and age: norms from the Maine-Syracuse Study. Exp Aging Res, 33(3), 205–271. doi: 10.1080/03610730701319087 [DOI] [PubMed] [Google Scholar]
- Dumas JA, & Hartman M (2008). Adult age differences in the access and deletion functions of inhibition. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn, 15(3), 330–357. doi: 10.1080/13825580701534601 [DOI] [PubMed] [Google Scholar]
- Eckert MA, Keren NI, Roberts DR, Calhoun VD, & Harris KC (2010). Age-related changes in processing speed: unique contributions of cerebellar and prefrontal cortex. Front Hum Neurosci, 4, 10. doi: 10.3389/neuro.09.010.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias MF, Dore GA, Goodell AL, Davey A, Zilioli MK, Brennan S, & Robbins MA (2011). Normative data for elderly adults: the Maine-Syracuse study. Exp Aging Res, 37(2), 142–178. doi: 10.1080/0361073X.2011.554511 [DOI] [PubMed] [Google Scholar]
- Elias MF, Elias PK, D'Agostino RB, Silbershatz H, & Wolf PA (1997). Role of age, education, and gender on cognitive performance in the Framingham Heart Study: community-based norms. Exp Aging Res, 23(3), 201–235. doi: 10.1080/03610739708254281 [DOI] [PubMed] [Google Scholar]
- Fastenau PS, Denburg NL, & Mauer BA (1998). Parallel short forms for the Boston Naming Test: psychometric properties and norms for older adults. J Clin Exp Neuropsychol, 20(6), 828–834. [DOI] [PubMed] [Google Scholar]
- Fine EM, Kramer JH, Lui LY, Yaffe K, & Group, S. o. O. F. S. R. (2012). Normative data in women aged 85 and older: verbal fluency, digit span, and the CVLT-II short form. Clin Neuropsychol, 26(1), 18–30. doi: 10.1080/13854046.2011.639310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 12(3), 189–198. [DOI] [PubMed] [Google Scholar]
- Franzen MD, Smith SS, Paul DS, & MacInnes WD (1993). Order effects in the administration of the Booklet Category Test and Wisconsin Card Sorting Test. Arch Clin Neuropsychol, 8(2), 105–110. [PubMed] [Google Scholar]
- Gale SD, Baxter L, Connor DJ, Herring A, & Comer J (2007). Sex differences on the Rey Auditory Verbal Learning Test and the Brief Visuospatial Memory Test-Revised in the elderly: normative data in 172 participants. J Clin Exp Neuropsychol, 29(5), 561–567. doi: 10.1080/13803390600864760 [DOI] [PubMed] [Google Scholar]
- Ganguli M, Snitz BE, Lee CW, Vanderbilt J, Saxton JA, & Chang CC (2010). Age and education effects and norms on a cognitive test battery from a population-based cohort: the Monongahela-Youghiogheny Healthy Aging Team. Aging Ment Health, 14(1), 100–107. doi: 10.1080/13607860903071014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz AB, Beker N, Hulsman M, Sikkes S, Netherlands Brain Bank, Scheltens P, … Holstege H (2018). Neuropathology and cognitive performance in self-reported cognitively healthy centenarians. Acta Neuropathol Commun, 6(1), 64. doi: 10.1186/s40478-018-0558-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasquoine PG (2009). Race-norming of neuropsychological tests. Neuropsychol Rev, 19(2), 250–262. doi: 10.1007/s11065-009-9090-5 [DOI] [PubMed] [Google Scholar]
- Gladsjo JA, Schuman CC, Miller SW, & Heaton RK (1999). Norms for letter and category fluency: Demographic correction for age, education, and ethnicity. Odessa, FL: PAR. [DOI] [PubMed] [Google Scholar]
- Graham JE, Rockwood K, Beattie BL, Eastwood R, Gauthier S, Tuokko H, & McDowell I (1997). Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet, 349(9068), 1793–1796. doi: 10.1016/S0140-6736(97)01007-6 [DOI] [PubMed] [Google Scholar]
- Hafkemeijer A, Altmann-Schneider I, de Craen AJ, Slagboom PE, van der Grond J, & Rombouts SA (2014). Associations between age and gray matter volume in anatomical brain networks in middle-aged to older adults. Aging Cell, 13(6), 1068–1074. doi: 10.1111/acel.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagberg B, Bauer Alfredson B, Poon LW, & Homma A (2001). Cognitive functioning in centenarians: a coordinated analysis of results from three countries. J Gerontol B Psychol Sci Soc Sci, 56(3), P141–151. [DOI] [PubMed] [Google Scholar]
- Hall JR, Vo HT, Johnson LA, Wiechmann A, & O'Bryant SE (2012). Boston Naming Test: Gender Differences in Older Adults with and without Alzheimer's Dementia. Psychology, 3(6), 485–488. [Google Scholar]
- Harada CN, Natelson Love MC, & Triebel KL (2013). Normal cognitive aging. Clin Geriatr Med, 29(4), 737–752. doi: 10.1016/j.cger.2013.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JG, & Llorente AM (2005). Cultural consideration in the use of the Wechsler Intelligence Scale for Children - Fourth Edition (WISC-IV). In Prifitera A, Saklofske DH, & Weiss LG (Eds.), WISC-IV clinical use and interpretation: Scientist-practitioner perspectives (pp. 382–413). Burlington: Elsevier Academic. [Google Scholar]
- He W, & Muenchrath M (2011). ACS-17 90+ in the United States: 2006-2008 American Community Survey Reports. Retrieved from Washington, D.C.: [Google Scholar]
- Heaton RK, Miller SW, Taylor MJ, & Grant I (2004). Revised comprehensive norms for an expanded Halstead-Reitan battery: Demographically adjusted neuropsychological norms for African American and Caucasian adults. Lutz, FL: PAR. [Google Scholar]
- Hogervorst E, Rahardjo TB, Jolles J, Brayne C, & Henderson VW (2012). Gender differences in verbal learning in older participants. Aging Health, 8(5), 1–15. [Google Scholar]
- Iacono D, Resnick SM, O'Brien R, Zonderman AB, An Y, Pletnikova O,… Troncoso JC (2014). Mild cognitive impairment and asymptomatic Alzheimer disease subjects: equivalent β -amyloid and tau loads with divergent cognitive outcomes. J Neuropathol Exp Neurol, 73(4), 295–304. doi: 10.1097/NEN.0000000000000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivnik RJ, Malec JF, Smith GE, Tangalos EG, & Petersen RC (1996). Neuropsychological Tests' Norms Above Age 55: COWAT, BNT, MAE Token, WRAT-R Reading, AMNART, STROOP, TMT, and JLO. The Clinical Neuropsychologist, 10(3), 262–278. [Google Scholar]
- Jopp DS, Park MK, Lehrfeld J, & Paggi ME (2016). Physical, cognitive, social and mental health in near-centenarians and centenarians living in New York City: findings from the Fordham Centenarian Study. BMC Geriatr, 16, 1. doi: 10.1186/s12877-015-0167-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kheirbek RE, Fokar A, Shara N, Bell-Wilson LK, Moore HJ, Olsen E, … Llorente MD (2017). Characteristics and Incidence of Chronic Illness in Community-Dwelling Predominantly Male U.S. Veteran Centenarians. J Am Geriatr Soc, 65(9), 2100–2106. doi: 10.1111/jgs.14900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig AM, Bhalla RK, & Butters MA (2014). Cognitive functioning and late-life depression. J Int Neuropsychol Soc, 20(5), 461–467. doi: 10.1017/S1355617714000198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Go AS, Lindquist K, Bertenthal D, & Covinsky KE (2008). Chronic conditions and mortality among the oldest old. Am J Public Health, 98(7), 1209–1214. doi: 10.2105/AJPH.2007.130955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legdeur N, Binnekade TT, Otten RH, Badissi M, Scheltens P, Visser PJ, & Maier AB (2017). Cognitive functioning of individuals aged 90 years and older without dementia: A systematic review. Ageing Res Rev, 36, 42–49. doi: 10.1016/j.arr.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Liu H, Yang Y, Xia Y, Zhu W, Leak RK, Wei Z, … Hu X (2017). Aging of cerebral white matter. Ageing Res Rev, 34, 64–76. doi: 10.1016/j.arr.2016.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llorente AM, Sines MC, Rozelle JC, Turcich MR, & Casatta A (2000). Effects of test administration order on children's neuropsychological performance: emerging one-word expressive and receptive language skills. Clin Neuropsychol, 14(2), 162–172. doi: 10.1076/1385-4046(200005)14:2;1-Z;FT162 [DOI] [PubMed] [Google Scholar]
- Maharani A, Dawes P, Nazroo J, Tampubolon G, Pendleton N, & group, S.-C. W. (2018). Visual and hearing impairments are associated with cognitive decline in older people. Age Ageing. doi: 10.1093/ageing/afy061 [DOI] [PubMed] [Google Scholar]
- Manly JJ, Jacobs DM, Touradji P, Small SA, & Stern Y (2002). Reading level attenuates differences in neuropsychological test performance between African American and White elders. J Int Neuropsychol Soc, 8(3), 341–348. [DOI] [PubMed] [Google Scholar]
- Masur DM, Sliwinski M, Lipton RB, Blau AD, & Crystal HA (1994). Neuropsychological prediction of dementia and the absence of dementia in healthy elderly persons. Neurology, 44(8), 1427–1432. [DOI] [PubMed] [Google Scholar]
- Melikyan ZA, Greenia DE, Corrada MM, Hester MM, Kawas CH, & Grill JD (2018). Recruiting the Oldest-old for Clinical Research. Alzheimer Dis Assoc Disord. doi: 10.1097/WAD.0000000000000260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller IN, Himali JJ, Beiser AS, Murabito JM, Seshadri S, Wolf PA, & Au R (2015). Normative Data for the Cognitively Intact Oldest-Old: The Framingham Heart Study. Exp Aging Res, 41(4), 386–409. doi: 10.1080/0361073X.2015.1053755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LS, Mitchell MB, Woodard JL, Davey A, Martin P, Poon LW, …Siegler IC (2010). Cognitive performance in centenarians and the oldest old: norms from the Georgia Centenarian Study. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn, 17(5), 575–590. doi: 10.1080/13825585.2010.481355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitoku K, Masaki N, Ogata Y, & Okamoto K (2016). Vision and hearing impairments, cognitive impairment and mortality among long-term care recipients: a population-based cohort study. BMC Geriatr, 16, 112. doi: 10.1186/s12877-016-0286-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morimoto SS, & Alexopoulos GS (2013). Cognitive deficits in geriatric depression: clinical correlates and implications for current and future treatment. Psychiatr Clin North Am, 36(4), 517–531. doi: 10.1016/j.psc.2013.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC (1993). The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology, 43(11), 2412–2414. [DOI] [PubMed] [Google Scholar]
- Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, … Clark C (1989). The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology, 39(9), 1159–1165. [DOI] [PubMed] [Google Scholar]
- National Alzheimer's Coordinating Center. (2017). Means and standard deviations for the UDS3 neuropsychological battery in cognitively normal participants - March 2017 - NACC. [Google Scholar]
- Nosraty L, Sarkeala T, Hervonen A, & Jylha M (2012). Is there successful aging for nonagenarians? The vitality 90+ study. J Aging Res, 2012, 868797. doi: 10.1155/2012/868797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paganini-Hill A, Ross RK, & Henderson BE (1986). Prevalence of chronic disease and health practices in a retirement community. J Chronic Dis, 39(9), 699–707. [DOI] [PubMed] [Google Scholar]
- Pfeffer RI, Kurosaki TT, Harrah CH, Chance JM, & Filos S (1982). Measurement of functional activities in older adults in the community. J Gerontol, 37(3), 323–329. [DOI] [PubMed] [Google Scholar]
- Pioggiosi PP, Berardi D, Ferrari B, Quartesan R, & De Ronchi D (2006). Occurrence of cognitive impairment after age 90: MCI and other broadly used concepts. Brain Res Bull, 68(4), 227–232. doi: 10.1016/j.brainresbull.2005.06.039 [DOI] [PubMed] [Google Scholar]
- Rabin LA, Paolillo E, & Barr WB (2016). Stability in Test-Usage Practices of Clinical Neuropsychologists in the United States and Canada Over a 10-Year Period: A Follow-Up Survey of INS and NAN Members. Arch Clin Neuropsychol, 31(3), 206–230. doi: 10.1093/arclin/acw007 [DOI] [PubMed] [Google Scholar]
- Rasmusson X, Zonderman A, Kawas C, & Resnick SM (1998). Effects of age and dementia on Trail Making Test. The Clinical Neuropsychologist, 12(2), 169–178. [Google Scholar]
- Reitan R, & Wolfson D (1993). The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretations. (2nd ed.). Tucson: Neuropsychological Press. [Google Scholar]
- Rosselli M, Tappen R, Williams C, & Salvatierra J (2006). The relation of education and gender on the attention items of the Mini-Mental State Examination in Spanish speaking Hispanic elders. Arch Clin Neuropsychol, 21(7), 677–686. doi: 10.1016/j.acn.2006.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saykin AJ, Gur RC, Gur RE, Shtasel DL, Flannery KA, Mozley LH, … Mozley PD (1995). Normative neuropsychological test performance: effects of age, education, gender and ethnicity. Appl Neuropsychol, 2(2), 79–88. doi: 10.1207/s15324826an0202_5 [DOI] [PubMed] [Google Scholar]
- Selim AJ, Fincke G, Berlowitz DR, Miller DR, Qian SX, Lee A, … Kazis LE (2005). Comprehensive health status assessment of centenarians: results from the 1999 large health survey of veteran enrollees. J Gerontol A Biol Sci Med Sci, 60(4), 515–519. [DOI] [PubMed] [Google Scholar]
- Sliwinski M, Lipton RB, Buschke H, & Stewart W (1996). The effects of preclinical dementia on estimates of normal cognitive functioning in aging. J Gerontol B Psychol Sci Soc Sci, 51(4), P217–225. [DOI] [PubMed] [Google Scholar]
- Steen G, Sonn U, Hanson AB, & Steen B (2001). Cognitive function and functional ability. A cross-sectional and longitudinal study at ages 85 and 95 in a non-demented population. Aging (Milano), 13(2), 68–77. [DOI] [PubMed] [Google Scholar]
- Steinberg BA, Bieliauskas LA, Smith GE, Langellotti C, & Ivnik RJ (2005). Mayo's Older Americans Normative Studies: Age- and IQ-Adjusted Norms for the Boston Naming Test, the MAE Token Test, and the Judgment of Line Orientation Test. Clin Neuropsychol, 19(3-4), 280–328. doi: 10.1080/13854040590945229 [DOI] [PubMed] [Google Scholar]
- Stern Y (2012). Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol, 11(11), 1006–1012. doi: 10.1016/S1474-4422(12)70191-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng EL, & Chui HC (1987). The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry, 48(8), 314–318. [PubMed] [Google Scholar]
- Tombaugh TN, Kozak J, & Rees L (1999). Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch Clin Neuropsychol, 14(2), 167–177. [PubMed] [Google Scholar]
- United Nations Department of Economic and Social Affairs Population Division. (2017). World Population Prospects: The 2017. Revision, custom data acquired via web-site. [Google Scholar]
- Wahlin A, Bäckman L, Mäntylä T, Herlitz A, Viitanen M, & Winblad B (1993). Prior knowledge and face recognition in a community-based sample of healthy, very old adults. J Gerontol, 48(2), P54–61. [DOI] [PubMed] [Google Scholar]
- Wastesson JW, Parker MG, Fastbom J, Thorslund M, & Johnell K (2012). Drug use in centenarians compared with nonagenarians and octogenarians in Sweden: a nationwide register-based study. Age Ageing, 41(2), 218–224. doi: 10.1093/ageing/afr144 [DOI] [PubMed] [Google Scholar]
- Wechsler D (1997). Wechsler Adult Intelligence Scale - Third Edition (WAIS-III) San Antonio, TX: Psychological Corporation. [Google Scholar]
- Weintraub S, Besser L, Dodge HH, Teylan M, Ferris S, Goldstein FC, … Morris JC (2018). Version 3 of the Alzheimer Disease Centers' Neuropsychological Test Battery in the Uniform Data Set (UDS). Alzheimer Dis Assoc Disord, 32(1), 10–17. doi: 10.1097/WAD.0000000000000223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisenbach SL, Boore LA, & Kales HC (2012). Depression and cognitive impairment in older adults. Curr Psychiatry Rep, 14(4), 280–288. doi: 10.1007/s11920-012-0278-7 [DOI] [PubMed] [Google Scholar]
- Whittle C, Corrada MM, Dick M, Ziegler R, Kahle-Wrobleski K, Paganini-Hill A, & Kawas C (2007). Neuropsychological data in nondemented oldest old: the 90+ Study. J Clin Exp Neuropsychol, 29(3), 290–299. doi: 10.1080/13803390600678038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, & Leirer VO (1982-1983). Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res, 17(1), 37–49. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Elashoff D, Kremen S, Teng E, Karlawish J, & Grill JD (2017). African Americans are less likely to enroll in preclinical Alzheimer's disease clinical trials. Alzheimers Dement (N Y), 3(1), 57–64. doi: 10.1016/j.trci.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubenko GS, Zubenko WN, Maher BS, & Wolf NS (2007). Reduced age-related cataracts among elderly persons who reach age 90 with preserved cognition: a biomarker of successful aging? J Gerontol A Biol Sci Med Sci, 62(5), 500–506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.