Abstract
Background:
Following blunt abdominal trauma, bowel injuries are often missed on admission computed tomography (CT) scan.
Methods:
Multicenter retrospective analysis of 176 adults with moderate-critical blunt abdominal trauma and admission CT scan who underwent operative exploration. Patients with a bowel injury missed on CT (n =36, 20%) were compared to all other patients (n=140, 80%).
Results:
The missed injury group had greater incidence free fluid without solid organ injury on CT scan (44% vs. 25%, p=0.038) and visceral adhesions (28% vs. 6%, p=0.001). Independent predictors of missed bowel injury included prior abdominal inflammation (OR 3.74, 95% CI 1.37–10.18), CT evidence of free fluid in the absence of solid organ injury (OR 2.31, 95% CI 1.03–5.19) and intraoperative identification of visceral adhesions (OR 4.46, 95% CI 1.52–13.13).
Conclusions:
Patients with visceral adhesive disease and indirect evidence of bowel injury on CT scan were more likely to have occult bowel injury.
Keywords: Surgery, adhesions, computed tomography, trauma, bowel injury
Summary:
Following blunt abdominal trauma, bowel injuries are often missed on admission computed tomography (CT) scan. In this multicenter retrospective analysis of 176 adults with moderate-critical blunt abdominal trauma and admission CT scan who underwent operative exploration, patients with visceral adhesive disease and indirect evidence of bowel injury on CT scan were more likely to have occult bowel injury.
Introduction
The prevalence of intra-abdominal injury among adult patients with blunt abdominal trauma is approximately 13%.1 Selecting patients who will benefit from operative exploration remains difficult, with serious consequences associated with non-therapeutic laparotomy as well delayed recognition of conditions requiring operative intervention. At level I trauma centers, the rate of non-therapeutic laparotomy has ranged from to 27.1%, reported in 1995 by Renz and Feliciano,2 down to 3.9%, reported in 2012 by Schnuriger, Demetirades, et al.3 In the more recent study, 14.5% of all non-therapeutic laparotomies had associated complications, underscoring the importance of patient selection. A missed injury may be an even greater detriment, particularly when a bowel injury is missed on initial workup, resulting in delayed operative exploration after the patient develops peritonitis.4–7 Although multidetector computed tomography (CT) has improved the diagnosis of bowel injury,8, 9 its sensitivity and specificity have been reported as 55–64% and 80–92%, respectively.10, 11 Therefore, better methods are needed to accurately identify patients with bowel injury following blunt abdominal trauma.
The purposes of this study were to assess the incidence of bowel injury missed on CT scan and to identify predictors of missed bowel injury among adult blunt trauma patients who undergo CT scan with subsequent operative exploration to confirm the presence or absence of bowel injury. Based on previous work,4, 11 we hypothesized that patients who are likely to have adhesive disease secondary to prior abdominal inflammation or surgery and patients with indirect evidence of bowel injury on CT scan (e.g. free fluid in the absence of solid organ injury) would be at increased risk for missed bowel injury.
Methods
We performed a retrospective cohort analysis of 176 consecutive adult (age≥18 years) patients admitted to St. Mary’s Medical Center in West Palm Beach, Florida or University of Florida Health in Gainesville, Florida following blunt trauma with abdominal injury severity score ranging from 2 (moderate) to 5 (critical) and had preoperative CT scan of the abdomen and pelvis with subsequent operative exploration by laparoscopy or laparotomy. Patients were identified by searching institutional data registries at both participating institutions. Patients with abdominal injury severity score 1 (mild) or 6 (non-survivable) were not included because prediction of missed bowel injury would not be clinically useful for these patients. Patients were excluded if they had penetrating or burn injuries. Derivation of the study population is illustrated in Figure 1. Patients with a bowel injury that was missed on preoperative CT scan and identified during operative exploration (n =36) were compared to patients who did not have a bowel injury that was missed on preoperative CT scan (n=140).
Figure 1:
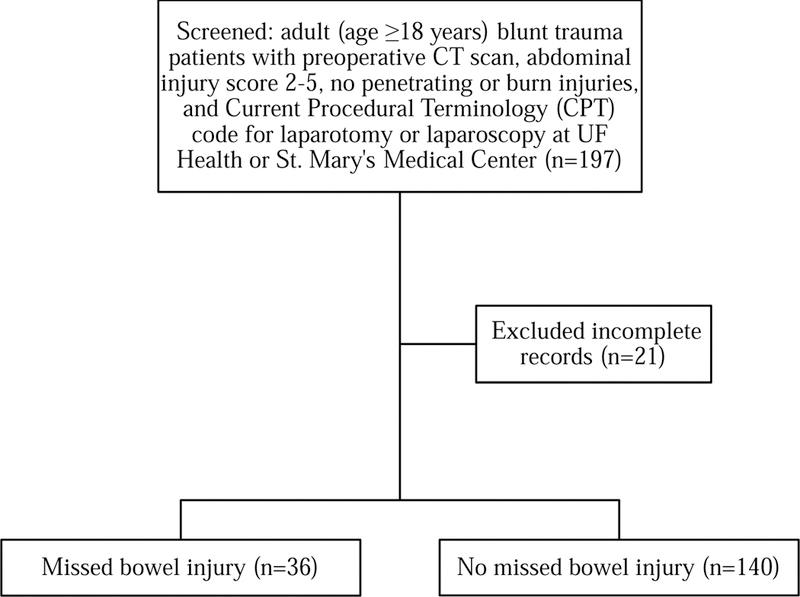
Derivation of the study population (CT: computed tomography).
Data were collected from institutional databases and by retrospective review of electronic medical records. Factors associated with intra-abdominal injury described by previous studies were assessed, including prior abdominal inflammation (documentation of an infectious or non- infectious inflammatory intra-abdominal process, e.g. diverticulitis, Crohn’s disease, spontaneous bacterial peritonitis), prior abdominal surgery, low GCS, endotracheal intubation, hypotension, acidosis, anemia, focused assessment with sonography for trauma (FAST) exam findings, diagnostic peritoneal aspirate/lavage (DPA/DPL), and pelvic facture.12–19 Abdominal pain and tenderness were not considered in this analysis because the accuracy of this data on retrospective review cannot be assured. They are often confounded by medications administered prior to arrival in the trauma bay, and the absence of abdominal pain and tenderness has limited utility in ruling out abdominal injury.18 CT scan findings were obtained from radiology reports signed by board-certified radiologists. Management parameters included laparoscopic versus open operative approach, the interval from admission to surgery, performance of a bowel resection or repair, and the performance of a non-therapeutic laparotomy. The decision to perform operative exploration was at the discretion of the attending surgeon, informed by the presence or development of peritonitis as well as concern for hemorrhage from an intra- abdominal source or hollow visceral injury per clinical presentation or radiographic findings. Operative findings were obtained from operative reports signed by board-certified surgeons. Operative findings included the identification of adhesive disease, solid organ injury, mesenteric injury, and bowel injury.
Statistical analysis was performed in SPSS (version 24; Armonk, NY). Continuous variables were compared by the Kruskal-Wallis test and reported as median [interquartile range]. Discrete variables were compared by Fisher’s Exact test and reported as n (%). Correlations were assessed by Pearson’s r. Univariate logistic regression was performed to identify risk factors for bowel injury missed on CT scan. Factors that were significant on univariate analysis were entered into a multivariate regression model to identify independent predictors of missed bowel injury. A multivariable regression model should contain approximately ten outcome events for each variable in the model.20 In this study, there were 36 cases of bowel injury missed on CT scan. Therefore, this study was adequately powered to include up to three covariates in multivariable modeling. Two models were created: one based on findings available only in the preoperative setting, and one based on preoperative and intraoperative findings, including the presence of visceral adhesive disease on initial exploration. Model strength was assessed by calculating area under the receiver operating characteristic curve (AUROC).
Results
Patient characteristics are listed in Table 1. Median age was 40 years. Thirty-two percent of all patients were female. Twenty-three percent of all patients had a history of an abdominal inflammatory process, 17% had previous abdominal surgery, and 12% had previous open abdominal surgery. The prevalence of prior abdominal inflammation was significantly higher in the missed injury group (42% vs. 19%, p=0.007). The prevalence of prior laparotomy was similar between groups (19% vs. 10%, p=0.148). Twenty-one percent of all patients were intubated in the field, 13% were intubated in the trauma bay, and only two patients (1%) had a cardiac arrest in the field or trauma bay. A seatbelt sign was noted in 13% of all patients, with similar incidence between groups (17% vs. 12%, p=0.579). A FAST exam was performed in 63% of all patients, with equivocal or positive findings in 24% of all patients.
Table 1:
Summary of baseline characteristics for the study population.
| Patient characteristics | All patients (n=176) |
CT missed Bowel injury (n=36) |
No missed Bowel injury (n=140) |
p |
|---|---|---|---|---|
| Age (years) | 40 [27–58] | 36 [26–51] | 41 [27–58] | 0.356 |
| Female | 56 (32%) | 14 (39%) | 42 (30%) | 0.321 |
| Prior abdominal inflammation | 41 (23%) | 15 (42%) | 26 (19%) | 0.007 |
| Prior abdominal surgery | 29 (16%) | 8 (22%) | 21 (15%) | 0.317 |
| Open abdominal surgery | 21 (12%) | 7 (19%) | 14 (10%) | 0.148 |
| Injury severity score | 26 [16–35] | 21 [13–34] | 27 [17–36] | 0.112 |
| Abdominal injury score | 3 [2–4] | 3 [2–3] | 3 [2–4] | 0.073 |
| Glasgow coma scale score | 15 [13–15] | 15 [13–15] | 15 [11–15] | 0.164 |
| Intubated in field | 36 (20%) | 5 (14%) | 31 (22%) | 0.357 |
| Intubated in trauma bay | 23 (13%) | 4 (11%) | 19 (14%) | >0.999 |
| Cardiac arrest in field | 1 (1%) | 0 (0%) | 1 (1%) | >0.999 |
| Cardiac arrest in trauma bay | 1 (1%) | 0 (0%) | 1 (1%) | >0.999 |
| Admission heart rate | 98 [80–115] | 97 [84–116] | 98 [80–115] | 0.915 |
| Admission SBP (mmHg) | 121 [103–140] | 132 [112–142] | 120 [102–139] | 0.071 |
| Admission lactate (mmol/L) | 2.5 [1.9–3.8] | 2.2 [1.8–4.0] | 2.8 [2.0–3.7] | 0.292 |
| Admission Hb (g/dL) | 12.3 [10.6–13.8] | 12.5 [11.2–13.7] | 12.3 [10.5–13.8] | 0.338 |
| Seatbelt sign | 23 (13%) | 6 (17%) | 17 (12%) | 0.579 |
| FAST performed | 111 (63%) | 20 (56%) | 91 (65%) | 0.335 |
| Negative | 69 (39%) | 15 (42%) | 54 (39%) | 0.850 |
| Equivocal | 6 (3%) | 0 (0%) | 6 (4%) | 0.346 |
| Positive | 36 (20%) | 5 (14%) | 31 (22%) | 0.356 |
| DPA/DPL performed | 8 (5%) | 2 (6%) | 6 (4%) | 0.667 |
| Negative | 2 (1%) | 1 (3%) | 1 (1%) | 0.368 |
| Positive | 6 (3%) | 1 (3%) | 5 (4%) | >0.999 |
| FAST or DPA/DPL positive | 38 (22%) | 6 (17%) | 32 (23%) | 0.502 |
| Abdominal X-ray performed | 142 (81%) | 29 (81%) | 113 (81%) | >0.999 |
| Normal | 104 (59%) | 24 (67%) | 80 (57%) | 0.345 |
| Pelvic fracture | 33 (19%) | 5 (14%) | 28 (20%) | 0.480 |
| Open book deformity | 10 (6%) | 2 (6%) | 8 (6%) | >0.999 |
SBP: systolic blood pressure, Hb: hemoglobin, FAST: focused assessment with sonography for trauma, DPA: diagnostic peritoneal aspirate, DPL: diagnostic peritoneal lavage. Data are presented as median [interquartile range] or n (%).
CT scan findings are listed in Table 2. Four patients (2%) had a normal CT scan. Solid organ injuries were identified in 60% of all patients, with a lower proportion of solid organ injuries occurring in patients with a missed bowel injury (44% vs. 64%, p=0.036). Free fluid was identified in 74% of all patients, with no significant differences between groups. Free fluid occurred in the absence of solid organ injury in 44% of all patients with a missed bowel injury, compared with 25% of all other patients (p=0.038). Rates of pelvic fracture, bladder injury, and mesenteric injury were similar between groups.
Table 2:
Summary of abdominal and pelvic computed tomography (CT) scan findings.
| CT findings | All patients (n=176) |
CT missed bowel injury (n=36) |
No missed bowel injury (n=140) |
p |
|---|---|---|---|---|
| Normal CT scan | 4 (2%) | 2 (6%) | 2 (1%) | 0.186 |
| Solid organ injury | 106 (60%) | 16 (44%) | 90 (64%) | 0.036 |
| Bleeding pseudoaneurysm | 29 (16%) | 2 (6%) | 27 (19%) | 0.074 |
| Free fluid | 131 (74%) | 24 (67%) | 107 (76%) | 0.284 |
| Without solid organ injury | 51 (29%) | 16 (44%) | 35 (25%) | 0.038 |
| Bowel injury | 26 (15%) | 0 (0%) | 26 (19%) | 0.003 |
| Pelvic fracture | 47 (27%) | 8 (22%) | 39 (28%) | 0.673 |
| Bladder injury | 9 (5%) | 1 (3%) | 8 (6%) | 0.684 |
| Intraperitoneal | 6 (3%) | 1 (3%) | 5 (4%) | >0.999 |
| Extraperitoneal | 3 (2%) | 0 (0%) | 3 (2%) | >0.999 |
| Mesenteric stranding | 29 (16%) | 9 (25%) | 20 (14%) | 0.135 |
| Mesenteric hematoma | 28 (16%) | 7 (19%) | 21 (15%) | 0.609 |
Data are presented as n (%).
Operative findings and outcomes are listed in Table 3. The median number of days between admission and operative exploration was zero days in both groups. Intraoperative identification of visceral adhesions was significantly more common in the missed injury group (28% vs. 6%, p=0.001). The presence of adhesive disease correlated with history of an abdominal inflammatory process (r=0.269, p<0.001) and history of laparotomy (r=0.396, p < 0.001) but not history of laparoscopy (r=0.145, p=0.054). Similar to CT findings, there was a lower proportion of patients with solid organ injury in the missed bowel injury group (39% vs. 64%, p=0.008). There were 14 patients (10% of the cohort) in the no missed injury group with a bowel injury that was identified on preoperative CT scan by free air, bowel wall thickening, or bowel wall stranding and inflammation. Hospital length of stay was longer in the missed injury group (13 vs. 9 days, p=0.029), though this observation does not establish or imply causality. Overall inpatient mortality was 13%, with no significant differences between groups.
Table 3:
Summary of operative findings and outcomes.
| Operative findings and outcomes | All patients (n=176) |
CT missed bowel injury (n=36) |
No missed bowel injury (n=140) |
p |
|---|---|---|---|---|
| Operative approach | ||||
| Laparotomy | 163 (93%) | 29 (81%) | 134 (96%) | 0.006 |
| Laparoscopy | 3 (2%) | 0 (0%) | 3 (2%) | >0.999 |
| Laparoscopy converted to laparotomy | 10 (6%) | 7 (19%) | 3 (2%) | 0.001 |
| Days from admission to surgery | 0 [0–1] | 0 [0–1] | 0 [0–1] | 0.339 |
| Identified adhesive disease | 18 (10%) | 10 (28%) | 8 (6%) | 0.001 |
| Identified solid organ injury | 104 (59%) | 14 (39%) | 90 (64%) | 0.008 |
| Missed on CT scan | 6 (3%) | 2 (6%) | 4 (3%) | 0.604 |
| Identified mesenteric injury | 60 (34%) | 22 (61%) | 38 (27%) | <0.001 |
| Missed on CT scan | 24 (14%) | 12 (33%) | 12 (9%) | <0.001 |
| Identified bowel injury | 50 (28%) | 36 (100%) | 14 (10%) | <0.001 |
| Partial thickness | 23 (13%) | 18 (50%) | 5 (4%) | <0.001 |
| Full thickness | 27 (15%) | 18 (50%) | 9 (6%) | <0.001 |
| Bowel resection or repair | 53 (30%) | 35 (97%) | 18 (13%) | <0.001 |
| Non-therapeutic laparotomy | 12 (7%) | 0 (0%) | 12 (9%) | 0.130 |
| Hospital length of stay (days) | 10 [5–22] | 13 [8–27] | 9 [5–20] | 0.029 |
| Inpatient mortality | 23 (13%) | 3 (8%) | 20 (14%) | 0.419 |
Data are presented as n (%) or median [interquartile range].
Predictors of missed bowel injury are listed in Table 4. On univariate analysis, prior abdominal inflammation (OR 5.16, 95% CI 2.02–13.20) and CT evidence of free fluid in the absence of solid organ injury (OR 2.40, 95% CI 1.12–5.14) were associated with increased odds of missed bowel injury. Together, these factors each contributed significantly to a preoperative multivariable model with AUROC 0.70, 95% CI 0.60–0.80, p<0.001. The intraoperative identification of visceral adhesions was also associated with increased odds of missed bowel injury (OR 6.35, 95% CI 2.29–17.61, p<0.001). In a combined preoperative/intraoperative model, all three factors contributed significantly as independent predictors of missed bowel injury (AUROC 0.74, 95% CI 0.64–0.84, p<0.001).
Table 4:
Predictors of missed bowel injury. Factors that were statistically significant on univariable analysis were entered into the multivariable regression model.
| Model | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| Factors | OR | 95% CI | p | OR | 95% CI | p |
| Preoperative model | ||||||
| Prior abdominal inflammation | 5.16 | 2.02–13.20 | 0.001 | 5.07 | 1.95–13.21 | 0.001 |
| CT free fluid, no solid organ injury | 2.40 | 1.12–5.14 | 0.024 | 2.35 | 1.06–5.19 | 0.035 |
| Preoperative/intraoperative model | ||||||
| Prior abdominal inflammation | 5.16 | 2.02–13.20 | 0.001 | 3.74 | 1.37–10.18 | 0.010 |
| CT free fluid, no solid organ injury | 2.40 | 1.12–5.14 | 0.024 | 2.31 | 1.03–5.19 | 0.043 |
| Presence of adhesive disease | 6.35 | 2.29–17.61 | <0.001 | 4.46 | 1.52–13.13 | 0.007 |
OR: odds ratio, CI: confidence interval, SBP: systolic blood pressure. Area under the receiver operating characteristic curve for the preoperative multivariate model was 0.70 (95% CI 0.60– 0.80), p <0.001. Area under the receiver operating characteristic curve for the preoperative/intraoperative multivariate model was 0.74 (95% CI 0.64–0.84), p <0.001.
Discussion
These findings suggest that blunt traumatic bowel injuries are commonly missed on preoperative CT scan, and that patients with a predilection for visceral adhesive disease and indirect evidence of bowel injury on CT scan are at increased risk for occult bowel injury. These findings, along with the low sensitivity of CT scan in identifying bowel injuries, suggest that assessing likelihood of intra-abdominal adhesions may be a valuable adjunct in weighing the risks and benefits of operative exploration for patients with blunt abdominal trauma.10, 11 As expected, intraoperative identification of adhesive disease correlated with prior abdominal inflammation and prior laparotomy, but not prior laparoscopy. Although this study was not designed to assess pathophysiologic mechanisms, it seems plausible that visceral adhesions tether the bowel and create shearing forces during blunt abdominal trauma, similar to the mechanism by which traumatic aortic injury occurs near the ligamentum arteriosum in deceleration injuries. The same adhesions may then obscure CT scan evidence of bowel wall injury, apart from the finding of free fluid in the absence of solid organ injury. Although missed injury was not associated with a significant delay in operative exploration or increased mortality, it was associated with longer hospital length of stay, which may have been attributable to the increased incidence of bowel resection or repair in this group.
A recent study reported similar rates of missed injury. In a retrospective review of patients who underwent CT scan following motor vehicle crashes at a single center in Virginia, 24% of all patients had a delay of at least 24 hours before the diagnosis of bowel or mesenteric injury was established.21 Based on previous work,4–7 such delays are associated with increased morbidity and mortality. Until imaging technology improves, the ability to accurately identify patients who will benefit from operative exploration remains highly dependent on clinical suspicion. Unfortunately, the absence of abdominal pain and tenderness has limited utility in ruling out abdominal injury.18 However, clinical assessment may be improved by incorporating other elements of the history and physical exam. Based on our findings, we propose that eliciting a history of an abdominal inflammatory process or prior laparotomy may be a useful adjunct in the decision for or against operative exploration.
This study was limited by selection bias inherent to retrospective review. Selection bias was limited as much as possible by including all consecutive cases meeting study criteria at two institutions. In addition, although including only patients with abdominal injury severity score ranging from 2 (moderate) to 5 (critical) was advantageous for the purposes of this study by focusing the analysis on patients for whom the decision for or against operative exploration is relevant, this design also limits the generalizability of these findings. For example, the observation that solid organ injuries were identified on CT and by intraoperative assessment in a lower proportion of patients with a missed bowel injury is likely attributable to study design, i.e. all patients had a moderate-critical abdominal injury, the incidence of bowel injury must be higher (100%) in the cohort of patients with a missed bowel injury, and so the control group must have other injuries to obtain similar abdominal injury severity scores. Future investigations should seek to validate these findings in a prospective fashion including a broad cohort of patients with blunt abdominal trauma, and to ascertain whether acceleration and deceleration visceral shearing forces cause bowel injuries among patients with abdominal adhesions.
Conclusions
Bowel injuries were missed on preoperative CT scan in one out of five patients with moderate-critical blunt abdominal trauma. Patients with a predilection for visceral adhesive disease and indirect evidence of bowel injury on CT scan were at increased risk for occult bowel injury. Future research should validate these findings in a prospective fashion and ascertain whether visceral shearing forces due to adhesive disease predispose to bowel injury.
Highlights.
Occult bowel injury after blunt trauma is common and delayed diagnosis is morbid
At two centers, the incidence of bowel injury missed on admission CT scan was 20%
Free fluid without solid organ injury was associated with occult bowel injury
Visceral adhesions were associated with occult bowel injury
Acknowledgements
This work was supported in part by grants R01 GM113945–01 (PAE), R01 GM105893– 01A1 (AMM), and P50 GM111152–01 (SCB, PAE, AMM) awarded by the National Institute of General Medical Sciences (NIGMS). TJL was supported by a post-graduate training grant (T32 GM-008721) in burns, trauma and perioperative injury by NIGMS. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nishijima DK, Simel DL, Wisner DH, Holmes JF. Does this adult patient have a blunt intra-abdominal injury? JAMA, 2012. April 11;307(14):1517–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma, 1995. March;38(3):350–6. [DOI] [PubMed] [Google Scholar]
- 3.Schnuriger B, Lam L, Inaba K, et al. Negative laparotomy in trauma: are we getting better? Am Surg, 2012. November;78(11):1219–23. [PubMed] [Google Scholar]
- 4.Matsushima K, Mangel PS, Schaefer EW, Frankel HL. Blunt hollow viscus and mesenteric injury: still underrecognized. World J Surg, 2013. April;37(4):759–65. [DOI] [PubMed] [Google Scholar]
- 5.Allen GS, Moore FA, Cox CS Jr., et al. Hollow visceral injury and blunt trauma. J Trauma, 1998. July;45(1):69–75; discussion −8. [DOI] [PubMed] [Google Scholar]
- 6.Fakhry SM, Brownstein M, Watts DD, et al. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma, 2000. March;48(3):408–14; discussion 14–5. [DOI] [PubMed] [Google Scholar]
- 7.Watts DD, Fakhry SM, Group EM-IHVIR. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma, 2003. February;54(2):289–94. [DOI] [PubMed] [Google Scholar]
- 8.Atri M, Hanson JM, Grinblat L, et al. Surgically important bowel and/or mesenteric injury in blunt trauma: accuracy of multidetector CT for evaluation. Radiology, 2008. November;249(2):524–33. [DOI] [PubMed] [Google Scholar]
- 9.Park MH, Shin BS, Namgung H. Diagnostic performance of 64-MDCT for blunt small bowel perforation. Clin Imaging, 2013. Sep-Oct;37(5):884–8. [DOI] [PubMed] [Google Scholar]
- 10.Landry BA, Patlas MN, Faidi S, et al. Are We Missing Traumatic Bowel and Mesenteric Injuries? Can Assoc Radiol J, 2016. November;67(4):420–5. [DOI] [PubMed] [Google Scholar]
- 11.Bhagvan S, Turai M, Holden A, et al. Predicting hollow viscus injury in blunt abdominal trauma with computed tomography. World J Surg, 2013. January;37(1):123–6. [DOI] [PubMed] [Google Scholar]
- 12.Beck D, Marley R, Salvator A, Muakkassa F. Prospective study of the clinical predictors of a positive abdominal computed tomography in blunt trauma patients. J Trauma, 2004. August;57(2):296–300. [DOI] [PubMed] [Google Scholar]
- 13.Udekwu PO, Gurkin B, Oller DW. The use of computed tomography in blunt abdominal injuries. Am Surg, 1996. January;62(1):56–9. [PubMed] [Google Scholar]
- 14.Nelson JB, Bresticker MA, Nahrwold DL. Computed tomography in the initial evaluation of patients with blunt trauma. J Trauma, 1992. November;33(5):722–7. [DOI] [PubMed] [Google Scholar]
- 15.Mackersie RC, Tiwary AD, Shackford SR, Hoyt DB. Intra-abdominal injury following blunt trauma. Identifying the high-risk patient using objective risk factors. Arch Surg, 1989. July;124(7):809–13. [DOI] [PubMed] [Google Scholar]
- 16.Grieshop NA, Jacobson LE, Gomez GA, et al. Selective use of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma, 1995. May;38(5):727–31. [DOI] [PubMed] [Google Scholar]
- 17.Richards JR, Derlet RW. Computed tomography for blunt abdominal trauma in the ED: a prospective study. Am J Emerg Med, 1998. July;16(4):338–42. [DOI] [PubMed] [Google Scholar]
- 18.Poletti PA, Mirvis SE, Shanmuganathan K, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma, 2004. November;57(5):1072–81. [DOI] [PubMed] [Google Scholar]
- 19.Holmes JF, Wisner DH, McGahan JP, et al. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med, 2009. October;54(4):575–84. [DOI] [PubMed] [Google Scholar]
- 20.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol, 1996. December;49(12):1373–9. [DOI] [PubMed] [Google Scholar]
- 21.Zingg T, Agri F, Bourgeat M, et al. Avoiding delayed diagnosis of significant blunt bowel and mesenteric injuries: Can a scoring tool make the difference? A 7-year retrospective cohort study. Injury, 2017. September 6. [DOI] [PubMed] [Google Scholar]


