Abstract
Intimate partner violence (IPV) is highly prevalent among sexual and gender minority youth. Yet, due to a lack of longitudinal research, little is known regarding the developmental patterns, risk factors, or health-related consequences of IPV among lesbian, gay, bisexual, and transgender (LGBT) adolescents and young adults. In this study, we examined IPV victimization in an ethnically diverse community-based convenience sample of 248 LGBT youth in Chicago (aged 16–20 at study outset) who provided six waves of data across a 5-year period. Results from multilevel models with Bernoulli distributions indicated high, stable rates of IPV victimization across this developmental period (ages 16–25 years) that differed between demographic groups. Overall, 45.2% of LGBT youth were physically abused and 16.9% were sexually victimized by a dating partner during the study period. Odds of physical victimization were 76% higher for female than for male LGBT youth, 2.46 times higher for transgender than for cisgender youth, and 2–4 times higher for racial-ethnic minorities than for White youth. The prevalence of physical IPV declined with age for White youth but remained stable for racial-ethnic minorities. Odds of sexual victimization were 3.42 times higher for transgender than for cisgender youth, 75% higher for bisexual or questioning than for gay or lesbian youth, and increased more with age for male than female participants. Within-person analyses indicated that odds of physical IPV were higher at times when youth had more sexual partners, engaged in more marijuana use, and perceived lower social support; odds of sexual IPV were higher at times when youth had more sexual partners and experienced more LGBT-specific victimization. In prospective analyses, sexual IPV significantly predicted increased psychological distress; both IPV types marginally predicted increased marijuana use. Other traditional correlates (e.g., alcohol use) were not associated with IPV trajectories.
A Longitudinal Study of Intimate Partner Violence Victimization among LGBT Youth
Psychological abuse, physical aggression, and sexual violence between dating partners (i.e., intimate partner violence; IPV) is disturbingly prevalent among adolescents and young adults (Ackerman & Field, 2011; Halpern, Young, Waller, Martin, & Kupper, 2004; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012; Murray & Mobley, 2009). Lesbian, gay, bisexual, and transgender (LGBT) youth, in particular, are at high risk for being victims of IPV. Studies based on U.S. probability samples estimate that in the past year 59% of sexual minority youth (i.e., lesbian, gay, and bisexual youth) and 59% of transgender youth experienced psychological IPV victimization (Dank et al., 2013; Zweig et al., 2013), 17–43% of sexual minority youth and 89% of transgender youth experienced physical IPV victimization (Dank et al., 2013; Kann et al., 2011; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012; Zweig et al., 2013), and 23% of sexual minority youth and 61% of transgender youth experienced sexual IPV victimization (Dank et al., 2013; Zweig et al., 2013).
Research suggests that these prevalence rates of IPV among LGBT youth are significantly higher than those among heterosexual youth. U.S. probability samples have been used to compare lifetime IPV victimization rates between sexual minority versus heterosexual young adults (Rhodes, McCoy, Wilkin, & Wolfson, 2009) and high school students (Martin-Storey, 2014), as well as to compare past year IPV victimization among young adults (Porter & Williams, 2011), high school students (Kann et al., 2011; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012), and middle and high school students (Dank et al., 2013; Zweig et al., 2013). Additionally, several studies using large U.S. non-probability samples have explored lifetime IPV victimization among adolescents and young adults (Freedner et al., 2002) or high school students (Reuter et al., 2015). This substantial literature has revealed that sexual minorities are up to twice as likely to experience psychological IPV victimization (Dank et al., 2013; Freedner et al., 2002; Porter & Williams, 2011; Reuter et al., 2015; Zweig et al., 2013), up to three times as likely to experience physical IPV victimization (Dank et al., 2013; Freedner et al., 2002; Kann et al., 2011; Martin-Storey, 2014; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012; Porter & Williams, 2011; Reuter et al., 2015; Rhodes, McCoy, Wilkin, & Wolfson, 2009; Zweig et al., 2013), and up to five times as likely to experience sexual IPV victimization (Dank et al., 2013; Freedner et al., 2002; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012; Porter & Williams, 2011; Reuter et al., 2015; Zweig et al., 2013).
Much less research has been conducted on IPV among transgendered individuals. The little research on adults has yielded some evidence that transgendered men and women are at higher risk for physical IPV, and that transgendered women are at higher risk of psychological IPV, than are cisgender adults (Pitts et al., 2006); however, these differences were not observed in another study (Turell, 2000). The one study to date on youth – a multi-school, multi-state probability sample of 5,647 U.S. middle and high school students – concluded that transgender youth are at greater risk than both male and female cisgender youth for psychological, physical, and sexual IPV victimization in the past year (Dank, Lachman, Zweig, & Yahner, 2013).
The elevated prevalence of IPV among LGBT youth is particularly concerning in light of its serious negative health and social consequences. It is well established that, beyond injuries, IPV victimization raises risk for a wide range of adverse academic, health, and mental health outcomes among all adolescents (Exner-Cortens, Eckenrode, & Rothman, 2013; Temple, Le, Muir, Goforth, & McElhany, 2013) and specifically among sexual minorities (Messinger, 2014), and transgendered individuals (Pitts et al., 2006; Roch et al., 2010). LGBT youth who are victimized by a dating partner may be particularly vulnerable to negative outcomes: A national U.S. study found that sexual minority IPV victims were more likely than heterosexual IPV victims to experience injury, require medical care, be fearful for their safety, and have PTSD symptoms (Walters, Chen, & Breiding, 2013). Further, data suggest that, among IPV victims, transgender women are at higher risk of injury than cisgender people (Pitts et al., 2006). This may be because LGBT individuals have fewer protective resources (e.g., social support from families, schools, and communities; Eisenberg & Resnick, 2006; Safren & Heimberg, 1999) to buffer them from adverse consequences of violence (Beeble et al., 2009; Hammack et al., 2004). Further, certain unique LGBT-related stressors (e.g., internalized heterosexism and transphobia) faced by LGBT youth may exacerbate negative reactions to IPV (Carvalho et al., 2011).
Clearly, IPV among LGBT youth represents a pressing public health concern. To inform policy and practice, information is needed regarding its developmental patterns, risk factors, and health-related consequences. Unfortunately, very little research has examined IPV among LGBT people, especially youth (see review by Messinger, 2014). There is a particular lack of longitudinal studies: To our knowledge, no longitudinal study has ever assessed IPV among transgender people and the only published longitudinal study of IPV among sexual minority adults focused specifically on re-assault among women who had experienced recent IPV by a same-sex partner (Glass et al., 2008). There has been one published longitudinal study of IPV among sexual minority youth, in which IPV perpetration and victimization were assessed twice, 2 years apart, in heterosexual and self-identified sexual minority U.S. adolescents (Reuter, Sharp, & Temple, 2015). (Note that although the National Longitudinal Study of Adolescent Health assessed sexual orientation and IPV at multiple waves, the only published analyses of sexual minority IPV from this dataset used cross-sectional data; Ackerman & Field, 2011; Halpern, Young, Waller, Martin, & Kupper, 2004; McLaughlin, Hatzenbuehler, Xuan, & Conron, 2012).
The paucity of longitudinal research on IPV among sexual minority and transgender youth leaves several important gaps in our knowledge. First, we know little about the developmental trajectories of IPV among LGBT individuals across adolescence and young adulthood. Reviews of the broader IPV literature (Capaldi et al., 2012) suggest that IPV increases across adolescence, peaks in late adolescence or the early twenties, then declines from age 21 to 26 years and on into adulthood (Kim et al., 2008; Shortt et al., 2012). However, because LGBT youth live within a heterosexist and transphobic social climate, many may delay engaging in sexual and romantic activities and their relationships may differ from those of heterosexual and cisgender youth in important ways (e.g., concealment from family and supportive others). Consequently, IPV among LGBT youth may follow a unique developmental trajectory. Indeed, in the one longitudinal study of youth, rates of IPV perpetration were higher and showed more stability from age 15 to 17 years in sexual minority than in heterosexual adolescents; IPV victimization was higher but not more stable (Reuter et al., 2015). Studies with multiple waves of data across adolescence and young adulthood are needed to more fully assess the developmental trajectories of IPV among LGBT youth.
Second, it remains unclear which demographic groups of LGBT youth are most at risk for IPV onset, continuation, or escalation over time. It is of particular interest whether there are racial-ethnic or sex differences in IPV victimization among LGBT youth, given calls from the Institute of Medicine for research on how co-occurring social identities may intersect to impact sexual minority health (Institute of Medicine, 2011). It is possible that LGBT youth who are members of a minority (i.e., non-White) race or who are not of the dominant sex (i.e., those whose biological sex is female) may be at heightened risk for IPV, due to their multiple minority statuses. Regarding race, LGBT people of color experience more discrimination, harassment, and non-IPV violence than do LGBT Whites (Balsam, Molina, Beadnell, & Walters, 2011; Grant, Mottet, & Tanis, 2011; Katz-Wise & Hyde, 2012). Some scholars speculate that this, in turn, contributes to an internalization of racist, homophobic, and transphobic attitudes that may raise vulnerability to IPV among LGBT people of color (Poon, 2000; Waldron, 1996). Further, racial-ethnic minority LGBT victims of IPV experience multiple barriers to seeking help, often from within their own communities (Bograd, 1999; Kanuha, 1990), which might lead to more continued or escalating victimization than is present for White LGBT victims. However, this remains an empirical question, because no published study has examined racial or ethnic differences in IPV risk among LGBT adolescents. Research on sexual minority adults, which may generalize to youth, has yielded conflicting findings about whether race-ethnicity is associated with IPV risk (see Balsam & Szymanski, 2005; Finneran et al., 2012; Greenwood et al., 2002; Messinger, 2011; Siemieniuk et al., 2013; Stall et al., 2003; Strasser et al., 2012; Turell, 2000; Wong, Weiss, Ayala, & Kipke, 2010). The one study that has explored racial-ethnic differences in IPV victimization rates of transgender individuals used a sample of adult transgender women with a history of sex work. According to that study, transgender women who identify as White were more likely than African Americans to experience physical IPV, followed by Latinas and then Asian and Pacific Islanders; there were no racial-ethnic differences in sexual IPV victimization (Nemoto, Bödeker, & Iwamoto, 2011). Given the highly select nature of this sample, and the conflicting findings from samples of sexual minority adults, there is a clear need for research assessing racial differences in more representative samples of LBGT individuals, particularly youth.
Regarding sex, research on probability samples of sexual minority youth in the U.S. have found that females are more likely than males to report having ever experienced either physical or sexual IPV (Martin-Storey, 2014), psychological and physical IPV in the past 18 months (Halpern et al., 2004), and psychological and sexual IPV but not physical IPV in the past year (Dank et al., 2013; Zweig et al., 2013). No probability sampled studies of transgender IPV have yet been published. However, one study of 100 transgender adults in Australia found that, compared to transgender men, transgender women reported more psychological IPV, less sexual IPV, and equal rates of physical IPV in their lifetime (Pitts et al., 2006). In sum, existing research suggests that being female may be associated with greater risk for IPV victimization among sexual minority youth. However, no longitudinal studies have examined sex differences in the developmental trajectories of IPV among sexual minority youth and no research to date has assessed sex differences in IPV among transgender youth.
Third, the lack of longitudinal research has limited our ability to identify risk factors and consequences of IPV among LGBT Youth. Longitudinal studies using heterosexual samples have indicated a number of risk factors for IPV, including individual characteristics (e.g., family-of-origin violence), health-related factors (e.g., psychological symptoms; alcohol and substance use) and contextual factors (e.g., low social support; Capaldi et al., 2012). Similarly, IPV has demonstrated negative effects on psychological health (including stress, anxiety, and depression; Coker et al., 2002) and sexual health, including sexual risk-taking behaviors, in heterosexuals (Coker, 2007). However, it is unclear whether these findings will generalize to LGBT individuals. In fact, certain traditional risk factors such as exposure to interparental violence have not predicted IPV in some samples of sexual minority adolescents (Reuter et al., 2015). In recent years, a small number of studies have used LGBT samples to identify individual characteristics that are cross-sectionally associated with IPV victimization. Psychological distress – including stress and anxiety, sadness, depression, and post-traumatic stress disorder symptoms – has shown concurrent associations with IPV in several samples of LGBT people (Dank, Lachman, Zweig, & Yahner, 2014; Descamps, Rothblum, Bradford, & Ryan, 2000; Dyer et al., 2012; Leung, Cheung, & Luu, 2013; Mustanski et al., 2014; Pantalone, Hessler, & Simoni, 2010; Pantalone et al., 2012; Roch et al., 2010; Stall et al., 2003). Similarly, alcohol and drug use – in particular, cigarettes, alcohol, and illicit drugs including cocaine, downers, ecstasy, GHB, heroin, LSD, methamphetamines, and opium – have been linked to concurrent LGBT IPV victimization (Bimbi, Palmadessa, & Parsons, 2008; Descamps, Rothblum, Bradford, & Ryan, 2000; Kelly, Izienicki, Bimbi, & Parson, 2011; Klitzman et al., 2002; Koeppel & Bouffard, 2014; McClennen, Summers, & Vaughan, 2002; Mustanski et al., 2014; Pyra et al., 2014; Schilit, Lie, and Montagne, 1990; Siemieniuk et al., 2013; Stall et al., 2003; Strasser et al., 2012; Tran et al., 2014; Wong, Weiss, Ayala, & Kipke, 2010; Yu et al., 2013). Sexual risk-taking behaviors have also been cross-sectionally associated with LGBT IPV victimization (Feldman, Diaz, Ream, & El-Bassel, 2007; Houston & McKirnan, 2007). However, because these studies have exclusively used cross-sectional data, they cannot speak to direction of effects—that is, whether these health-related factors are causal risk factors of IPV or are outcomes that arise following the experience of IPV. It is plausible that LGBT individuals who are struggling with psychological issues, are frequently under the influence of drugs or alcohol, or engage in risky sexual behaviors are more vulnerable to abuse from dating and sexual partners. Alternately, it is also possible that LGBT youth who are victimized consequently develop psychological distress and may begin using substances or engaging in risky sex to cope with the experience. Longitudinal data is needed to clarify the temporal and causal nature of these associations.
There are other potential psychosocial risk factors for IPV that may be unique to, or particularly salient for, LGBT youth. There is growing evidence that, among sexual minorities, specific sexual orientation (i.e., bisexual vs. gay or lesbian) may be important to consider in understanding risk profiles. Specifically, bisexual individuals appear to differ from gay men and lesbians in important ways, often exhibiting more identity confusion and poorer mental health outcomes (Balsam et al., 2005; Blosnich &Bossarte, 2012). Regarding IPV, there is some evidence that bisexual adults, particularly women, experience higher rates of physical and sexual victimization than gay or lesbian adults (Walters et al., 2013). However, studies on adolescents and young adults have yielded inconsistent findings regarding if bisexual youth report more IPV victimization than gay and lesbian youth (Blosnich & Bossarte, 2012; Freedner et al., 2002; Reuter et al., 2015); further research is needed to examine this possibility. Low social support, a documented risk factor for IPV victimization among heterosexual adults and adolescents (Capaldi et al., 2012), may be particularly important to evaluate among LGBT youth, given that they are often rejected by their parents, families, and school communities based on their sexual orientation or transgender identity (e.g., Safren & Heimberg, 1999). Those youth who experience such rejection may be particularly vulnerable to IPV victimization. Finally, LGBT youth commonly face the unique stressor of LGBT-specific victimization (e.g., being insulted, threatened, or attacked due their sexual orientation and/or gender identity). Because such experiences predict psychological distress (Birkett, Newcomb, & Mustanski, 2015) and may pressure youth to conceal their same-sex relationships, they may also heighten vulnerability to victimization by intimate partners.
The Present Study
In the present study, we examined IPV victimization in a multiwave longitudinal study of ethnically diverse LGBT youth. We had several specific aims. First, we aimed to describe the prevalence and trajectories of physical and sexual IPV victimization across adolescence and emerging adulthood (ages 16–25). Second, we sought to assess differences by sex, race, sexual orientation (particularly bisexual vs. gay or lesbian), and transgender identity in the prevalence and trajectories of IPV victimization. Third, we aimed to evaluate potential risk factors for IPV, including psychological distress, alcohol and drug use, sexual risk-taking, low social support, and experience of LGBT-specific victimization. Capitalizing on our multi-wave longitudinal data, we used within-person associations to assess whether individuals experience higher odds of IPV during the same waves that they report higher levels of these factors, which would suggest that the factors might raise risk for IPV. Finally, we evaluated whether IPV victimization at one wave prospectively predicted health-related factors (psychological distress, alcohol and drug use, sexual risk-taking) at the next wave, which would suggest they are consequences of IPV.
Methods
Participants
Participants were a community sample of 248 sexual minority youth from the Chicago area (ages 16 – 20 years at baseline). Two participants were removed owing to missing demographic data. Of note, participants self-reported age and date of birth at baseline, but identification checks conducted at later waves of data collection resulted in an adjusted sample size compared with previous reports. Table 1 displays demographic characteristics of the sample.
Table 1.
Description of LGBT Youth Sample at Baseline (N=246); n (%)
| Variable | Value |
|---|---|
| Birth Sex | |
| Male | 121 (49.2) |
| Female | 125 (50.8) |
| Transgender Identity | |
| Cisgender | 226 (91.9) |
| Male-to-Female Transgender | 12 (4.9) |
| Female-to-Male Transgender | 8 (3.3) |
| Sexual Orientation | |
| Gay | 83 (34.0) |
| Lesbian | 68 (27.9) |
| Bisexual | 70 (28.7) |
| Questioning/Unsure/Other | 23 (9.4) |
| Race/Ethnicity | |
| White/Caucasian | 34 (13.8) |
| Black/African American | 141 (57.3) |
| Hispanic/Latino | 28 (11.4) |
| Other | 43 (17.5) |
| Living Situation | |
| Living with Parents | 146 (59.8) |
| Other Stable Housing | 86 (34.5) |
| Unstable Housing | 14 (5.7) |
| Highest Level of Education | |
| College | 14 (5.7) |
| Partial College | 55 (22.5) |
| High School | 64 (26.2) |
| Partial High School | 98 (40.2) |
| Less than High School | 13 (5.3) |
Note. LGBT = lesbian, gay, and bisexual and transgender.
Procedure and Design
We employed an accelerated longitudinal design (Tonry, Ohlin, & Farrington, 1991), in which participants who varied in age at baseline (from 16–20 years) provided six waves of data over a 5 year period (baseline and 6-, 12-, 42-, 48-, and 60-month follow-up). This design allowed us to assess developmental change across a wider age range (16–25 years) than if all participants were of the same age at baseline. The intervals between assessments varied from 6- to 30-months; however, at each assessment participants were instructed to report on the preceding 6-month period. Baseline data was collected from 2007–2009. Retention at each wave was 85%, 90%, 82%, 83%, and 82%, respectively. Compared to participants who missed one or more assessments, those who completed all waves reported less physical IPV, less marijuana and other drug use, less LGBT victimization, and more social support. This indicates some selective attrition of lower functioning youth, possibly reducing power to detect effects due to reduced variability. However, rates of attrition were lower than in many studies and our analytic strategy (using multilevel models) used all data provided by any participant.
An incentivized snowball sampling approach (Heckathorn, 1997) was used for recruitment that involved an initial convenience sample (i.e., flyers in LGBT neighborhoods and college listservs; 38%) and subsequent waves of incentivized peer recruitment (62%). Recruitment materials identified this as a study of the health of lesbian, gay, bisexual, transgender, queer and questioning youth. To allow for the inclusion of youth who did not identify with LGBT labels but who had same-gender attractions, eligibility screening asked, “Project Q2 is a study for lesbian, gay, bisexual, transgender youth, as well as other youths who do not use these terms but have same-sex attractions. Does this include you?”
Prior to enrollment, trained staff used a two-step process to determine decisional capacity to consent (Dunn & Jeste, 2001), first assessing the youth’s understanding of the study goals and then their capacity to understand, appreciate, thoughtfully consider, and express a choice about participation. Interviewers with any doubts about decisional capacity consulted with the study principal investigator before proceeding. The Institutional Review Board at University of Illinois at Chicago approved a waiver of parental permission for minor participants under 45 CFR 46.408(c), and appropriate mechanisms for protecting youths were put in place (i.e., a youth advocate, a federal Certificate of Confidentiality). Written informed consent was obtained.
Assessments were conducted in a private room at a youth center affiliated with a large LGBT community-based health center in Chicago or at the University of Illinois at Chicago by a trained research assistant. Later waves were conducted at Northwestern University in Chicago. At each visit, participants completed self-report measures of health behaviors, mental health, and psychosocial variables. Participants completed measures using audio computer-assisted self-interview (ACASI) technology. Participants were paid $25 to $50 at each time point. Upon completion of the interview, all participants were provided a list of community resources, including for mental health and domestic violence issues. Participants who endorsed suicidality or IPV were flagged for further assessment of safety. Supervised by a licensed Clinical Psychologist, we utilized a “clinician-on-call” system to provide support and make mandated reported decisions.
Measures
Demographics.
At baseline, a demographic questionnaire assessed participant age, birth sex (coded 0 for male and 1 for female), transgender identity (coded 0 for cisgender and 1 for transgender), race/ethnicity (using dummy variables for Black, Latino, and Other, and excluding White as the reference group), self-reported sexual orientation (coded 0 for gay or lesbian and 1 for bisexual or questioning, unsure, or other), living situation, and education.
All of the following measures were collected at each assessment wave:
Intimate Partner Violence.
The presence of physical and sexual IPV victimization was assessed within the HIV-Risk Assessment for Sexual Partnerships (H-RASP; Mustanski, Starks, & Newcomb, 2014). The H-RASP is a computerized self-administered interview designed to assess sexual behavior and associated situational/contextual variables (e.g., IPV) at the level of the sexual partnership. Physical IPV in the past 6 months was defined as being “hit, slapped, punched, or hurt in a physical way” by a dating or sexual partner, and sexual IPV in the past 6 months was defined as being forced by a partner to “have sex or oral sex when you didn’t want to (force includes physical and non-physical pressure, such as pushing, arguing or threatening).” Participants’ response options were either yes (1) or no (0) to assess whether they had experienced each of these forms of IPV during the past 6 months within each partnership reported at each wave in the H-RASP (up to 3 total per wave). We created dichotomous variables to indicate presence of physical and sexual IPV victimization at each wave (1 = IPV victimization within any partnership at the given wave; 0 = no IPV victimization).
Psychological Distress.
The Global Severity Index of the Brief Symptom Inventory (BSI 18; Derogatis, 2001) is a self-report measure of psychological distress during the previous week. The BSI 18 is a widely used psychiatric screening tool in epidemiological studies and clinical settings, with adequate reliability and validity (Zabora et al., 2001). A composite score was generated by calculating the mean of all items, with possible values ranging from 0 to 4. The BSI 18 demonstrated strong internal consistency across waves (Cronbach α ranged from .91 to .94).
Alcohol and Drug Use.
Frequency and quantity of alcohol use were assessed for the 6 months before each interview. Individuals who endorsed any lifetime use of alcohol were asked to report the number of days they had consumed alcohol during the 6-month assessment period (frequency [range: 0–180]), and the amount used on average while drinking (quantity [1 = one drink to 6 = six or more drinks]). Those indicating no lifetime alcohol use were coded as “0” for both items. A quantity/frequency (QF) variable was calculated by multiplying the number of days when alcohol was consumed by the average amount consumed per episode (Bartholow & Heinz, 2006; Greenfield, 2000). The QF variable provides an approximation of the total number of drinks consumed in the past 6 months. Frequency of marijuana use was assessed by asking participants to indicate the number of days on which they used marijuana during the previous 6 months. Prevalence of other illicit drug use at each wave was a dichotomous variable indicating whether or not participants had used any other illicit drugs on at least one day during the 6 months before each interview (1 = yes; 0 = no). Other illicit drugs included: cocaine/crack, heroin/other opiates, methamphetamines, club drugs (ecstasy, GHB, etc.), prescriptions stimulants and depressants, psychedelics, and inhalants.
Social Support.
The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Powell, Farley, Werkman, & Berkoff, 1990) is a 12-item validated measure of perceived social support, with subscales for family, peer, and significant other support. Example items include “I get the emotional help and support I need from my family” and “I can talk about my problems with my friends.” A composite score is generated by calculating the mean of all items, with possible values ranging from 1 to 7. The MSPSS demonstrated high internal consistency across all waves (Cronbach α ranged from .88 to .95).
Lesbian, gay, bisexual, and transgender (LGBT) victimization.
A 10-item measure based on D’Augelli, Hershberger, and Pilkington (1998) assessed frequency of various victimization experiences (e.g., verbal threats, physical assault) “because you are, or were thought to be, gay, lesbian, bisexual, or transgender” during the previous 6 months. Frequency ratings ranged from never (coded 0) to three or more times (coded 3). A composite variable was created with the mean of all items. Possible values ranged from 0 to 3 (Newcomb, Heinz, Birkett, & Mustanski, 2014; Newcomb, Heinz, & Mustanski, 2012). Cronbach α in our sample ranged from .77 to .93.
Sexual Risk Behavior.
The H-RASP computer-assisted interview (described above) gathered information on the total number of sexual partners each participant had during the 6 months prior to each wave of data collection, which was used to index sexual risk behavior. Number of sexual partners is a commonly used indicator of sexual risk-taking behaviors in adolescents and young adults (e.g., O’Hara & Cooper, 2015).
Analyses
Data analyses were conducted using hierarchical linear modeling (HLM; Raudenbush, Bryk, Cheong, Congdon, & du Toit, 2011). HLM accounts for dependency in observations in data that contain a nested or multilevel structure. In this case, measures collected at each wave, including IPV and time-varying health and social factors (e.g., psychological distress, substance use, social support) were modeled as Level 1 variables that are nested within participants. Time-invariant characteristics of participants, such as demographic characteristics, are modeled at Level 2. Physical and sexual IPV victimization were modeled separately in parallel analyses using a Bernoulli distribution, which is appropriate for dichotomous dependent variables; results are presented as odds ratios (OR). All models accounted for overdispersion in the outcome variable. Maximum likelihood estimation was used to model both outcome variables, and estimates are from the population-average model using robust standard errors.
First, to describe IPV in this sample, we calculated the percentage of participants who reported physical and sexual IPV victimization during the study period and used unconditional HLM models (with no predictors) to examine the extent to which variability in IPV was due to individual/group differences versus within-person change over time. Second, to estimate demographic differences in the prevalence of IPV, we entered demographic variables at Level 2 (i.e., birth sex, transgender identity, sexual orientation and race) as predictors of individuals’ odds of experiencing IPV, averaged across all data waves (i.e., as predictors of the intercept). Third, we estimated the developmental trajectory of IPV victimization across the observed age range (16–25 years) by entering age at each wave into Level 1 as a random effect, and entered each demographic variable as a Level 2 predictor of this random effect to estimate demographic differences in the developmental trajectory. Fourth, we tested for within-person associations between IPV and psychosocial/ health variables by simultaneously entering psychological distress, victimization, social support, alcohol use, marijuana use, drug use, and sexual risk behavior as Level 1 predictors, controlling for demographic effects. These analyses examine whether, within-individuals, odds of IPV are higher at waves when the given predictor is higher (e.g., when the youth’s drug use is higher than at other waves). Finally, to examine whether IPV predicts health outcomes, we ran a lagged model in which each of the health outcome variables (psychological distress, alcohol use, marijuana use, illicit drug use, and sexual risk behavior) at a given wave was predicted by physical and sexual IPV at the previous wave, controlling for the health variable at the previous wave and demographic effects. These analyses test whether IPV prospectively predicts change in the health outcomes.
Results
Descriptive Statistics and Preliminary Analyses
Almost half (45.2%) of participants reported at least one incident of physical IPV during the 5-year study period. A substantial number of participants reported physical IPV at multiple waves: 22.6% during at least 2 waves and 10.5% during at least 3 waves. In terms of sexual IPV, 16.9% of the sample reported victimization at least once; 3.2% reported victimization at more than one wave. Participants reported means of 0.67 (SD = .71; range, 0–4) for psychological distress, 5.16 (SD = 1.34; range, 1–7) for social support, and 0.27 (SD = .48; range, 0–3) for LGBT victimization across waves.
To evaluate the extent to which variability in IPV was due to individual/group differences (between-subject factors) versus change over time (within-subject factors), we ran unconditional models for each of the IPV outcome variables with no predictors. For dichotomous outcomes, this yields a weighted Kappa that estimates the proportion of variance across all IPV scores attributable to differences between participants rather than differences across waves within individuals. Results indicated that participants were largely consistent in endorsement of both physical IPV (weighted Kappa = .80) and sexual IPV across waves (weighted Kappa = .94); only 20% of the variability in physical IPV and 6% in sexual IPV was accounted for by within-participant changes over time, largely due to the many participants who never reported IPV.
Demographic Differences in the Prevalence of IPV Victimization
To evaluate group differences in the odds of IPV victimization, all demographic variables were simultaneously entered into multivariate models predicting the intercept of each IPV outcome. As shown in Table 2, female-born participants were approximately 76% more likely than males to experience physical IPV (OR = 1.76; p < .01). Transgender youth were more than twice as likely to experience physical IPV than cisgender youth (OR = 2.46, p < .05). Black and Other race youth were approximately 3–4 times more likely to experience physical IPV compared to Whites (p < .001 and p < .01, respectively). Although Latino youth were approximately twice as likely to experience physical victimization than Whites, this difference was not statistically significant. Self-reported sexual orientation was not associated with odds of physical IPV. With regard to sexual IPV, transgender youth were more than three times more likely than cisgender youth to experience sexual IPV (OR = 3.42, p < .001). Additionally, youth who identified as bisexual, questioning, or unsure were 75% more likely than youth who identified as gay or lesbian to experience sexual IPV (OR = 1.75, p < .050). No significant differences were observed in the odds of experiencing sexual IPV by birth sex or race.
Table 2.
Demographic Differences in Odds of Experiencing Physical and Sexual Intimate Partner Violence
| Fixed Effects | Physical IPV | Sexual IPV | |||||
|---|---|---|---|---|---|---|---|
| Odds Ratio (OR) |
Confidence Interval (95%) | p-value | Odds Ratio (OR) |
Confidence Interval (95%) | p-value | ||
| Birth Sex: Female | 1.76 | 1.17–2.66 | <0.01 | 1.27 | 0.83–1.96 | 0.27 | |
| Transgender Identity | 2.46 | 1.24–4.92 | <0.05 | 3.42 | 1.85–6.33 | <0.001 | |
| Sexual Orientation: Bisexual | 0.91 | 0.58–1.41 | 0.66 | 1.75 | 1.06–2.90 | <0.05 | |
| Race: Black/African American | 3.84 | 1.84–8.02 | <0.001 | 1.33 | 0.62–2.84 | 0.46 | |
| Race: Latino/Hispanic | 2.03 | 0.74–5.57 | 0.17 | 2.25 | 0.76–6.72 | 0.14 | |
| Race: Other | 3.18 | 1.38–7.33 | <0.01 | 1.68 | 0.71–3.96 | 0.24 | |
Note. IPV = intimate partner violence. For race, the reference group is White. Estimates are from multivariate models including all demographic variables as predictors.
Trajectories of IPV (Change Over Time)
To describe the trajectories of physical and sexual IPV victimization in LGBT youth, Level 1 models were estimated predicting each type of IPV with time (as indexed by age in months at each wave). Time was modeled as a random effect (i.e., its slope could vary across participants) to allow for evaluation of heterogeneity between individuals in their IPV trajectories. Based on evidence from heterosexual samples that IPV increases in adolescence, peaking in early adulthood before declining, we first examined a curvilinear growth trajectory for change over time (i.e., including linear and quadratic time parameters). However, for physical IPV the quadratic term was non-significant and did not improve model fit according to deviance statistics, which together indicated that IPV did not follow a curvilinear trajectory across the observed age range. Further, the quadratic term for time did not vary significantly across participants and was not associated with demographic variables. For sexual IPV, the random model including a quadratic term would not converge, likely due to too few reported incidents. We therefore removed the quadratic terms, estimating linear developmental trajectories of each IPV outcome. For physical IPV, the coefficient associated with time was not significant (p = .23); however, the χ2 test of its Level 1 random effect was significant, χ2 (228, N = 246) = 443.78 (p < .001), indicating significant between-person differences in the linear slope over time. That is, although odds of victimization did not significantly change with age in the full sample (OR = .97; p = .230), the linear slope of physical IPV differed between individuals, suggesting that the developmental trajectory in physical IPV may be dependent upon demographic or other characteristics of the individual. Results followed a similar pattern for sexual IPV. Odds of sexual IPV increased marginally with age (OR = 1.06; p = .077), and the linear developmental trajectories of sexual IPV differed between individuals, χ2 (228, N = 246) = 625.15 (p < .001).
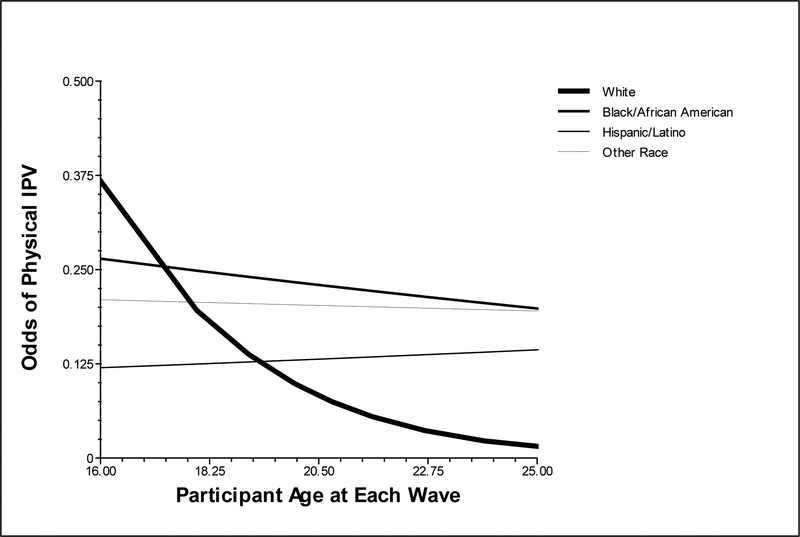
Next, baseline demographic variables were tested as moderators of the developmental trajectory of each IPV outcome variable. There were significant racial differences in developmental trajectories of physical IPV. White youth experienced a decrease in odds of physical IPV relative to Black (OR = 1.43, p < .01), Latino (OR = 1.52, p < .01), and Other race (OR = 1.47, p < .01) youth. Simple slopes analysis for each racial group revealed that whereas White youth experienced a decrease in odds of physical IPV across the observed age range, none of the other racial groups experienced significant change in odds of IPV. This race by age interaction is depicted in Figure 1. Birth sex, transgender identity, and self-reported sexual orientation (bisexual vs. other) did not moderate developmental trajectories of physical IPV.
Figure 1.
Moderating effect of race/ethnicity on trajectories of physical IPV.
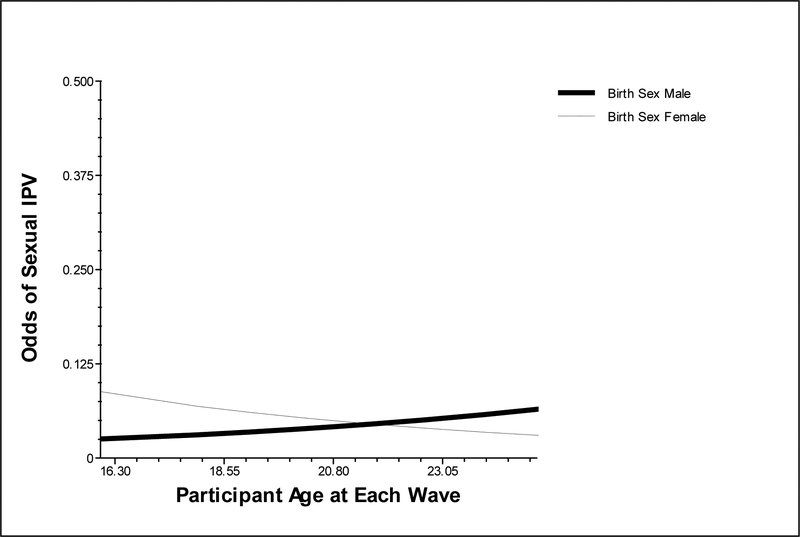
The developmental trajectory of sexual IPV was not moderated by age at baseline, race, transgender identity, or self-reported sexual orientation, but was moderated by birth sex (female OR = .79, p <.05). As displayed in Figure 2, male-born youth experienced an increase in sexual IPV over time relative to female-born youth, whose odds of sexual IPV decreased slightly over time (however, neither of the simple slopes for each sex was significantly different from zero).
Figure 2.
Moderating effect of birth sex on trajectories of sexual IPV.
Within-person Associations
Next, we estimated the within-person associations between each IPV outcome and the health-related and psychosocial variables at the same wave, adjusted for the main effects of demographic characteristics, in multivariate models (i.e., including all predictors). As shown in Table 3, within-persons, LGBT victimization was not associated with physical IPV but was associated with increased odds of sexual IPV (OR = 2.15, p < .001). Perceived social support was associated with decreased odds of physical IPV (OR = 0.85, p < .05) but was not associated with odds of sexual IPV. Alcohol use was not associated with odds of physical IPV but, unexpectedly, was associated with decreased odds of sexual IPV (OR = 0.998, p < .001). This was likely due to the effect of another variable in the model, because alcohol was not associated with sexual IPV in a bivariate model. Marijuana use was associated with increased odds of physical IPV (OR = 1.002, p < .05) but not with sexual IPV. Total number of sexual partners at each wave was associated with increased odds of both physical (OR = 1.12, p < .01) and sexual IPV (OR = 1.25, p < .001). Psychological distress and illicit drug use were not associated with either IPV type.
Table 3.
Within-Person Associations between Intimate Partner Violence and Health-Related and Psychosocial Factors
| Fixed Effects | Physical IPV | Sexual IPV | ||||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (OR) |
Confidence Interval (95%) | p-value | Odds Ratio (OR) |
Confidence Interval (95%) | p-value | |||
| Psychological Distress | 1.00 | 0.77 – 1.29 | 0.986 | 1.28 | 0.79 – 2.07 | 0.317 | ||
| Alcohol Quantity-Frequency | 1.00 | 1.00 – 1.00 | 0.975 | 0.99 | 0.99 – 0.99 | <.001 | ||
| Marijuana Use | 1.00 | 1.00 – 1.00 | <0.05 | 1.00 | 1.00 – 1.00 | 0.354 | ||
| Illicit Drug Use | 1.46 | 0.89 – 2.41 | 0.135 | 1.10 | 0.38 – 3.20 | 0.859 | ||
| Number Sexual Partners | 1.12 | 1.04 – 1.21 | <0.01 | 1.25 | 1.12 – 1.39 | <0.001 | ||
| Perceived Social Support | 0.85 | 0.73 – 0.99 | <0.05 | 0.93 | 0.76 – 1.14 | 0.480 | ||
| LGBT Victimization | 1.18 | 0.90 – 1.56 | 0.230 | 2.15 | 1.43 – 3.22 | <0.001 | ||
Note. Estimates are from multivariate models including all predictors and adjusted for the main effects of demographic characteristics (birth sex, race/ethnicity, self-reported sexual orientation). IPV = intimate partner violence.
Lagged Analyses
Finally, we conducted longitudinal lagged analyses in which each of the health outcome variables (psychological distress, alcohol use, marijuana use, illicit drug use, and sexual risk behavior) at a given wave was predicted by physical and sexual IPV at the previous wave, controlling for the health variable at the previous wave. These analyses test whether IPV prospectively predicts change in the health outcomes from one wave to the next. Results are shown in Table 4. Physical IPV was not associated with psychological distress at the subsequent wave, but sexual IPV predicted higher levels of distress (coefficient = 0.32, p < .01). Both physical and sexual IPV were associated with increased marijuana use at the subsequent wave (ERRs = 1.21 and 1.30, respectively); these associations were marginally significant. Similarly, both physical and sexual IPV were associated with increased odds of drug use at the next wave (ORs = 1.27 and 1.21, respectively), but these associations did not reach significance (ps > .10). Neither physical nor sexual IPV was associated with alcohol use or sexual risk behavior.
Table 4.
Results of Lagged Analyses: Prospective Effects of Physical and Sexual Intimate Partner Violence on Health-Related Factors
| Psych. Distress | Alcohol QF | Marijuana Use | Illicit Drug Use | No. Sexual Partners | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coeff. | SE | ERR | 95% CI | ERR | 95% CI | OR | 95% CI | ERR | 95% CI | |
| Physical IPV | −0.01 | 0.05 | 1.14 | 0.82 – 1.60 | 1.21 | 0.96 – 1.52 | 1.27 | 0.68 – 2.37 | 1.05 | 0.91 – 1.20 |
| Sexual IPV | 0.32* | 0.12 | 0.98 | 0.57 – 1.69 | 1.30 | 0.81 – 2.11 | 1.21 | 0.47 – 3.08 | 1.04 | 0.76 – 1.42 |
Note. Each of the above models adjusted for the main effects of participant demographic characteristics (birth sex, race/ethnicity, self-reported sexual orientation). IPV = intimate partner violence; Psych = psychological; QF = quantity frequency; No = number. Coeff. = standardized coefficient; SE = standard error; ERR = event-rate ratio; CI = confidence interval; OR = odds ratio.
Sensitivity Analyses
In our primary analyses, the dichotomous sexual orientation variable grouped all youth who identified as gay or lesbian (i.e., homosexual) together, and combined all others, including those who identified as bisexual (n = 39) and those who were questioning, unsure, or other (n = 26). This strategy was selected because we lacked power to examine groups individually and because by including all participants in one of the two categories we avoided dropping any youth from the analyses. However, because based on past findings we were most interested in comparing bisexual to gay/lesbian youth, we conducted a sensitivity analysis in which we dropped the questioning/unsure/other youth. Using this variable, the overall pattern of effects remained intact. Most notably, paralleling results from primary analyses, bisexual youth had higher odds of experiencing sexual IPV than gay/lesbian youth (OR = 1.91, p < .05) but did not differ in odds of physical IPV or the trajectories of physical and sexual IPV. Only two effects (both from the lagged analyses) changed significance. Sexual IPV became a marginal (p < .10) rather than significant predictor of psychological distress at the next wave and physical IPV became a statistically significant predictor of marijuana use at the next wave (this effect was previously a trend).
Discussion
Echoing findings from population-based studies (e.g., Dank et al., 2013; Zweig et al., 2013), our findings show that physical and sexual IPV victimization is highly prevalent among LGBT adolescents and young adults. Approximately 45% of our sample reported experiencing physical dating violence and 17% sexual dating violence during the 5-year study period. This study also extends the existing literature, which has estimated IPV prevalence in LGBT youth at one time point only, by examining the trajectories of physical and sexual victimization across the age range of 16–25 years. Results indicate that the odds of victimization remained stable across the observed age range, rather than declining in young adulthood (from 21 to 26 years) as has been observed in heterosexual samples (Kim et al, 2008; Shortt et al., 2012). This highlights the unique IPV experiences of sexual minority youth and suggests that prevention and intervention models should be directed to both adolescent and young adult sexual minorities.
Demographic Differences in Prevalence and Trajectories of IPV Among LGBT Youth
It is important to note, however, that the trajectories of physical IPV differed between demographic groups, echoing sex and racial differences observed in national adolescent samples (CDC, 2014; Tajima, Herrenkohl, Moylan, & Derr, 2010). Results indicated that female sexual minorities were consistently at higher risk for physical IPV victimization than male sexual minorities across adolescence and young adulthood. In addition, the youth in our sample who identified as African-American or Other races (but not Latino) were approximately 3–4 times more likely to have experienced physical IPV than their White counterparts. Further, rates of physical IPV remained stable across the age range of 16–25 years among Black, Latino, or Other race youth, whereas White youths’ rates of physical IPV decreased across this developmental period. Overall, findings suggest that having a minority racial or sex status may increase risk for physical IPV among LGBT youth, highlighting the potential vulnerabilities associated with having multiple minority social identities (Cole, 2009; IOM, 2011). The higher rates of dating violence victimization observed among LGBT youth of color may, for example, represent a downstream effect of the prejudice and discrimination they face based in both their race/ethnicity and their LGBT status (Meyer, Dietrich, & Schwartz, 2008).
Interestingly, we did not observe differences by birth sex or race in rates of sexual IPV reported by LGBT youth. This contrasts with national data indicating that female and ethnic minority adolescents report sexual IPV at higher rates than do male and White youth, respectively (CDC, 2014). Our findings suggest that, in contrast to heterosexual female youth, female sexual minority youth are not at higher risk than males for sexual victimization by dating partners. Past research is mixed on this topic. In one study, equal percentages of male and female sexual minorities experienced sexual IPV (Turell, 2000). However, other studies of sexual minority adults have found that women were at greater risk of sexual IPV victimization than men (Blosnich & Bossarte, 2009; Walters et al., 2013). It is possible that, due to low incidence of sexual IPV in this sample, we lacked power to detect true population-level sex differences in LGBT youth. Alternately, the differences in findings between studies may be due to age differences in the samples, reflecting that female sexual minorities are not at greater risk for sexual IPV than males until adulthood. However, consistent with previous evidence that bisexual women’s risk of rape is higher in adolescence than young adulthood (Walters et al., 2013), we found that that females experienced a slight (though non-significant) decrease in odds of sexual IPV from age 16 to 25 and the odds of sexual IPV actually increased more with age for male than for female participants.
The pattern of findings for male participants suggests that sexual minority status is a key risk factor for sexual abuse among male youth. Unlike heterosexual male youth (CDC, 2014), the male sexual minority youth in this sample experienced rates of sexual victimization similar to that of females. Further, male sexual minority youth showed a slight increase in odds of sexual IPV across the ages of 16–25 years; this increase was significantly greater than that of the female participants. Although the mechanisms behind these findings are unclear, partnering with males versus with females may raise risk for sexual IPV among both sexual minority male and heterosexual female youth. It is also possible that age-specific masculinity norms among sexual minority men may drive their increasing risk of sexual IPV across time. Clearly, further research is needed to clarify how sex and sexual minority status intersect in risk for sexual victimization, how this may differ across developmental stage, and explanatory mechanisms.
Self-identified sexual orientation was associated with risk for sexual, but not physical, IPV in this sample of LGBT youth. Specifically, youth who identified as bisexual or questioning had greater odds of experiencing sexual IPV than those who identified as gay or lesbian. Further, the trajectories of sexual IPV over time did not differ by sexual orientation, suggesting that those who identified as bisexual or questioning may continue to be at elevated risk of sexual IPV throughout late adolescence and young adulthood. This result is consistent with previous findings that, among adolescents, bisexual girls are at higher risk than lesbians of sexual abuse by a dating partner (Freedner et al., 2002). It also aligns with findings from the National Intimate Partner and Sexual Violence Survey, in which adult bisexual women reported significantly higher rates of rape (46%) and of other sexual violence (75%) – the majority of which occurred between the ages of 11 and 24 years – than did lesbian women (13% and 46%, respectively; Walters et al., 2013). We did not have power to test gender differences in the associations between bisexuality and sexual victimization; however, given that some previous research did not find bisexuality to raise risk for sexual IPV among male sexual minority adolescents (Freedner et al., 2002) or adults (Walters et al., 2013), this is an important area for future study. Although it is not clear why odds of sexual victimization are elevated for bisexual youth, it may be related to their experiences of “dual marginalization,” in which they face discrimination from both the dominant heterosexist culture (Herek, 2002) and from within the sexual minority community (Weiss, 2004). This may lead to increased minority stress, marginalization, and social isolation, which in turn raises vulnerability to sexual victimization.
It is interesting that we did not observe bisexual youth to have comparatively higher odds of physical abuse, given that the lifetime prevalence of physical IPV victimization is estimated to be higher among adult bisexual women than lesbians (57% vs. 32%) and non-significantly higher among bisexual than gay men (37% vs. 25%; Walters et al., 2013). It is possible that bisexuality does not become a risk factor for physical IPV victimization until adulthood. Two other studies of adolescents have yielded findings similar to ours, indicating that bisexual youth are not at higher risk than gay or lesbian youth of physical IPV (Freedner et al., 2002) or of experiencing any IPV victimization (including physical, sexual, or emotional abuse; Reuter et al., 2015). In contrast, bisexual college students (age 18–24) have shown higher rates of any IPV victimization than their gay and lesbian counterparts (Blossnich & Bosarte, 2011).
Transgender youth were at markedly elevated risk for victimization by a dating partner; compared to cisgender sexual minority youth, they were around 2.5 times more likely to have experienced physical IPV and nearly four times more likely to have experienced sexual IPV. Because our sample of transgender youth was small (n=20) these results should be viewed with caution until replicated in a larger sample. Nevertheless, they are consistent with the only other published study of IPV victimization in transgender youth, which similarly found transgender identity to predict an elevated risk of all forms of IPV (Dank, Lachman, Zweig, & Yahner, 2013). Together, these findings raise significant concerns about the wellbeing of transgender youth, especially in light of evidence that transgender IPV victims may experience more injury than cisgender victims (Pitts et al., 2006) and that forced sex is predictive of suicide attempts among transgendered persons (Clements-Nolle, Marx, & Katz, 2006). Youth who identify with a gender different from the one assigned at birth often experience social isolation, discrimination, and other types of victimization (APA, 2009) which may help explain their greater vulnerability to IPV and possibly exacerbate its negative consequences on their wellbeing.
Risk Factors and Consequences of IPV among LGBT Youth
A key aim of the present study was to examine the temporal sequencing of IPV and health-related factors among LGBT youth, to clarify directionality of effects. Of the three primary IPV health factors studied – psychological distress, substance use, and sexual risk-taking – only psychological distress exhibited a clear time order with IPV, and only for sexual IPV. Specifically, psychological distress was not associated with sexual IPV victimization in the same wave, but sexual IPV victimization prospectively predicted psychological distress in the subsequent wave. This suggests that psychological distress may be a consequence of, rather than a risk factor for, sexual IPV victimization. Future research is needed to examine factors that might exacerbate or buffer sexual IPV victims from psychological distress. For example, the lack of culturally-competent services for victims of same-sex IPV and heterosexism within existing services (reviewed in Messinger, 2014) may enhance and maintain psychological distress. Somewhat unexpectedly, physical IPV victimization was not associated with psychological distress in the same or subsequent wave. It is possible that psychological distress did arise from physical IPV for many respondents, but dissipated more quickly than it did for sexual IPV victims and was not captured by our measure, which only assessed psychological distress within the past week.
The time ordering of IPV and substance use was less clear and differed by the particular substance. Regarding alcohol, neither physical nor sexual IPV victimization prospectively predicted alcohol use in the subsequent 6-month period. Further, when looking at the odds of co-occurrence within the same time period, surprisingly, alcohol use was not associated with physical IPV victimization or with higher odds of sexual IPV victimization. These findings run counter to previous research indicating a cross-sectional association between alcohol and IPV in sexual minority samples (Kelly et al., 2011; McClennen et al., 2002). Interestingly, a recent review of the broader IPV literature also found that the association between alcohol use and IPV was weak and inconsistently observed in longitudinal studies (Capaldi et al., 2012). More longitudinal research is needed to test the validity of common notions that alcohol use is both a major risk factor for IPV and a consequence of victimization. Regarding illicit drugs, physical IPV was associated with marijuana use- but not use of other drugs- both in the same wave and prospectively in the following wave. These findings suggest that use of marijuana may be a coping mechanism for victims of physical IPV, which emerges fairly quickly and is sustained into the future. Together with evidence from other studies that marijuana use, but not alcohol use, is associated with dating violence victimization (Testa, Livingston, & Leonard, 2003), these results support further study into how use of marijuana specifically may be linked with IPV.
Sexual risk-taking, as indexed by the number of sexual partners in the past 6 months, was associated with both physical and sexual IPV victimization in the same time period. This finding might indicate that engaging in sexual activity with more partners raises risk for victimization, perhaps because it increases the opportunities to encounter an abuser. Alternately, victimization may raise risk for sexual risk-taking, consistent with evidence that forced sex and physical abuse by a dating partner predict unprotected sex, another index of sexual risk-taking, among young sexual minority men (Mustanski et al., 2011). That is, the experience of abuse may be followed, within the same 6-month period, by increased sexual risk-taking with others, perhaps as a short-term maladaptive coping mechanism. However, neither physical nor sexual IPV victimization was prospectively associated sexual risk-taking in the subsequent time period, which does not support this directionality of effects. Further research that more closely pinpoints the timing of IPV and sexual behaviors is needed to confidently infer causality.
Beyond health-related factors, we also tested hypotheses that two psychosocial factors commonly experienced by LGBT youth (low social support and victimization due to being LGBT) might raise risk for IPV victimization. Findings yielded mixed support for these hypotheses. Tests of within-person associations across time indicated that the likelihood of physical IPV, but not sexual IPV, was higher at times when participants had lower than usual social support. In contrast, LGBT-specific victimization was associated with increased odds of sexual IPV, but not physical IPV, within the same 6-month time period. This suggests that LGBT youth are at greater risk for sexual victimization by a dating partner during times when they have been bullied, threatened, or hurt due to their sexual orientation. Together these findings suggest that the elevated rates of IPV among LGBT youth may be partially explained by particular hardships they commonly face due to their sexual minority status – namely, rejection by parents and other social support (e.g., Safren & Heimberg, 1999) and LGBT-specific victimization, which is alarmingly prevalent (D’Augelli, Grossman, & Starks, 2006). Policy and intervention efforts should focus on improving social support and preventing bullying and other LGBT-specific victimization.
Study Limitations and Strengths
Several limitations of the study should be noted. First, the non-probability sample limits the extent to which findings can be viewed as representative of the general population of LGBT youth. However, it was community-based, racially diverse, and more representative than samples drawn from courts, shelters, or clinics, which may overestimate the prevalence of IPV and risk factors. Second, the numbers of participants in some groups of interest were small (e.g., transgender youth) and in some instances necessitated merging subgroups (e.g., bisexual, questioning, and unsure/other), limiting power to detect effects and raising questions of generalizability to the population. Third, our assessment of IPV was limited to one-item measures capturing the presence or absence of physical and sexual victimization from sexual partners. Future research should assess other forms of IPV (e.g., emotional or psychological abuse), its frequency and severity, and perpetration as well as victimization, especially given that bidirectional violence is common (e.g., Kelly et al., 2011). The fairly low proportion of variability in IPV that was due to within-person changes over time, driven by the large number of individuals who did not experience IPV at any waves, likely limited power to detect within-person associations between IPV and other variables. There were also too few observations of sexual IPV to estimate a quadratic effect of time, despite an apparent curvilinear trajectory among female-born youth. Future research with more time points and a more inclusive definition of sexual IPV (i.e., not just forced sex) could more powerfully estimate this trajectory. The 6-month recall periods made it challenging to discern the temporal order of IPV and other behaviors (e.g., substance use) that occurred in the same wave. In future studies, real-time data collection or diary methods would help disentangle the direction of effects. In addition, because IPV was assessed at particular time intervals, during which participants could have had multiple partnerships, we were unable to examine relationship-specific factors (e.g., partner sex, couple conflict) associated with IPV. Finally, because the measure of socio-economic status was limited to education, there may have been confounding between race and other factors (e.g., income).
Nevertheless, this study has numerous strengths, which strengthen confidence in the findings and highlight its contribution to the literature. To our knowledge, this study is only the second published longitudinal analysis of IPV in sexual minority youth, the first to longitudinally study IPV among transgender youth, and the first to examine trajectories of IPV among any LGBT subpopulation with multiwave data. As such, it represents a significant advancement beyond the cross-sectional studies that comprise the bulk of the existing literature. The accelerated longitudinal design, with multiple assessments covering the age ranges of 16–25 years, allowed us to model the developmental trajectories of LGBT IPV across adolescence and young adulthood and to examine its risk factors and health-related consequences. Further, the highly diverse sample enabled us to identify demographic differences in these trajectories.
Conclusions
This study extends a growing literature documenting the prevalence of IPV among LGBT youth, by estimating the trajectories of physical and sexual victimization across adolescence and young adulthood for various demographic groups. Findings indicate that the odds of physical IPV are particularly high for female and racial-ethnic minority LGBT youth and, although risk for physical IPV decreases for White sexual minorities between adolescence and young adulthood, it remains high for racial/ethnic minority LGBT individuals. These findings contribute to the limited literature on intersectionality of multiple identities (Cole, 2009), highlighting how an LGBT identity may interact with a minority racial or sex status to exacerbate vulnerability to negative life experiences, including victimization by dating partners. Clinically, these results suggest that screening for physical IPV victimization – as well as prevention and intervention efforts-- may be especially important for young female sexual minorities and for LGBT youth of color, not only in adolescence but also in young adulthood. Odds of both physical and sexual IPV were particularly high among transgendered participants, adding to a growing literature documenting the multitude of challenges that these youth face.
The unique multiwave data identified that LGBT youth may be most at risk for victimization by dating partners when they are experiencing low social support from friends and family and when they experience general victimization based on their sexual or gender identity. These findings, which add to a growing literature documenting the negative effects of such minority stressors for LGBT youth, emphasize the need for policies and interventions aimed at reducing the social rejection and discrimination often faced by LGBT youth. The results also illuminate the negative consequences of IPV in this population. Physical victimization was associated with increased use of marijuana, but not alcohol or other drugs, suggesting that researchers, policy makers and clinicians should focus more attention on marijuana use among sexual minority victims of dating violence. Finally, the data indicated a pattern of sustained psychological distress as an outcome of sexual IPV victimization for sexual minority youth, suggesting that mental health services may be needed immediately and many months after the abuse has occurred.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (R21MH095413; PI: Mustanski), an American Foundation for Suicide Prevention grant (PI: Mustanski), the William T. Grant Foundation Scholars Award (PI: Mustanski), and the David Bohnett Foundation (PI: Mustanski).
References
- Ackerman J, & Field L (2011). The gender asymmetric effect of intimate partner violence on relationship satisfaction. Violence and victims, 26(6), 703–724. [DOI] [PubMed] [Google Scholar]
- American Psychological Association (2009). Report of the Task Force on Gender Identity and Gender Variance. Washington, DC: American Psychological Association. [Google Scholar]
- Balsam KF, Beauchaine TP, Mickey RM, & Rothblum ED (2005). Mental health of lesbian, gay, bisexual, and heterosexual siblings: Effects of gender, sexual orientation, and family. Journal of Abnormal Psychology, 114, 471–476. [DOI] [PubMed] [Google Scholar]
- Balsam KF, & Szymanski DM (2005). Relationship quality and domestic violence in women’s same‐sex relationships: the role of minority stress. Psychology of Women Quarterly, 29(3), 258–269. [Google Scholar]
- Bartholow BD, & Heinz A (2006). Alcohol and aggression without consumption alcohol cues, aggressive thoughts, and hostile perception bias. Psychological Science, 17, 30–37. [DOI] [PubMed] [Google Scholar]
- Beeble ML, Bybee D, Sullivan CM, Adams AE. (2009). Main, mediating, and moderating effects of social support on the well-being of survivors of intimate partner violence across 2 years. J Consult Clin Psychol. 2009;77:718–729. [DOI] [PubMed] [Google Scholar]
- Blosnich J, & Bossarte R (2012). Drivers of disparity: Differences in socially based risk factors of self-injurious and suicidal behaviors among sexual minority college students. Journal of American College Health, 60(2), 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkett M, Newcomb ME, & Mustanski B (2015). Does it get better? A Longitudinal Analysis of Psychological Distress and Victimization in Lesbian, Gay, Bisexual, Transgender, and Questioning Youth. Journal of Adolescent Health, 53, 280–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bograd M (1999). Strengthening domestic violence theories: Intersections of race, class, sexual orientation, and gender. Journal of Marital and Family Therapy, 25(3), 275–289. [DOI] [PubMed] [Google Scholar]
- Burke LK, & Follingstad DR (1999). Violence in lesbian and gay relationships: Theory, prevalence, and correlational factors. Clinical Psychology Review, 19(5), 487–512. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, Kim HK (2012). A systematic review of risk factors for intimate partner violence. Partner Abuse, 3(2), 231–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho AF, Lewis RJ, Derlega VJ, Winstead BA, Viggiano C. (2011). Internalized sexual minority stressors and same-sex intimate partner violence. J Fam Violence. 26, 501–509. [Google Scholar]
- Center for Disease Control (2014). High School Youth Risk Behavior Survey Data. 2013. Accessed 3/4/2015. [Google Scholar]
- Charles D, Whitaker DJ, Le B, Swahn M, & DiClemente RJ (2011). Differences between perpetrators of bidirectional and unidirectional physical intimate partner violence. Partner Abuse, 2, 344–364. [Google Scholar]
- Clements-Nolle K, Marx R, Katz M. (2006). Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. Journal of Homosexuality, 51, 53–69. [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias IA, Desai S, Sanderson M, Brandt HM, et al. (2002). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23, 260–268. [DOI] [PubMed] [Google Scholar]
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64, 170. [DOI] [PubMed] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100(10), 1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Augelli AR, Grossman AH, & Starks MT (2006). Childhood gender atypicality, victimization, and PTSD among lesbian, gay, and bisexual youth. Journal of Interpersonal Violence, 21(11), 1462–1482. [DOI] [PubMed] [Google Scholar]
- D’augelli AR, Hershberger SL, & Pilkington NW (1998). Lesbian, gay, and bisexual youth and their families: Disclosure of sexual orientation and its consequences. American Journal of Orthopsychiatry, 68(3), 361. [DOI] [PubMed] [Google Scholar]
- Dank M, Lachman P, Zweig JM, & Yahner J (2014). Dating violence experiences of lesbian, gay, bisexual, and transgender youth. Journal of Youth & Adolescence, 43, 8467. [DOI] [PubMed] [Google Scholar]
- Derogatis LR (2001). BSI 18, Brief Symptom Inventory 18: Administration, scoring and procedures manual. NCS Pearson, Incorporated. [Google Scholar]
- Descamps MJ, Rothblum E, Bradford J, & Ryan C (2000). Mental health impact of child sexual abuse, rape, intimate partner violence, and hate crimes in the National Lesbian Health Care Survey. Journal of Gay & Lesbian Social Services, 11(1), 27–55. [Google Scholar]
- Dunn LB, & Jeste DV (2001). Enhancing informed consent for research and treatment. Neuropsychopharmacology, 24, 595–607. [DOI] [PubMed] [Google Scholar]
- Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, … & Stall R (2012). Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. Journal of Urban Health, 89(4), 697–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg ME, & Resnick MD (2006). Suicidality among gay, lesbian and bisexual youth: the role of protective factors. Journal of Adolescent Health, 39(5), 662–668. [DOI] [PubMed] [Google Scholar]
- Exner-Cortens D, Eckenrode J, & Rothman E (2013). Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics, 131(1), 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman MB, Díaz RM, Ream GL, & El-Bassel N (2007). Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men. Journal of LGBT health research, 3(2), 9–19. [DOI] [PubMed] [Google Scholar]
- Finneran C, Chard A, Sineath C, Sullivan P, & Stepheneon R (2012). Intimate partner violence and social pressure among gay men in six countries. Western Journal of Emergency Medicine, 13(3), 260–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedner N, Freed LH, Yang YW, Austin SB (2002). Dating violence among gay, lesbian, and bisexual adolescents: Results from a community survey. Journal of Adolescent Health, 31(6), 469–474. [DOI] [PubMed] [Google Scholar]
- Glass N, Perrin N, Hanson G, Bloom T, Gardner E, & Campbell JC (2008). Assessing risk for repeat violence in abusive female same-sex relationships. American Journal of Public Health, 98(6), 1021–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JM, Mottet LA, & Tanis J (2011). Injustice at every turn: A report from the National Transgender Discrimination Survey – Executive summary. National Center for Transgender Equality and National Gay and Lesbian Task Force. [Google Scholar]
- Greenfield TK (2000). Ways of measuring drinking patterns and the difference they make: Experience with graduated frequencies. Journal of Substance Abuse, 12(1), 33–49. [DOI] [PubMed] [Google Scholar]
- Greenwood GL, Relf MV, Huang B, Pollack LM, Canchola JA, & Catania JA (2002). Battering victimization among a probability-based sample of men who have sex with men. American Journal of Public Health, 92(12), 1964–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern CT, Young ML, Waller MW, Martin SL, & Kupper LL (2004). Prevalence of partner violence in same-sex romantic and sexual relationships in a national sample of adolescents. Journal of Adolescent Health, 35(2), 124–131. [DOI] [PubMed] [Google Scholar]
- Hammock PL, Richards MH, Luo Z, Edlynn ES, Roy K. (2004). Social support factors as moderators of community violence exposure among inner-city african american young adolescents. J Clin Child Adolesc Psychol. 33, 450–462. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD (1997). Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems, 44(2), 174–199. doi: [DOI] [Google Scholar]
- Herek GM (2002). Heterosexuals’ attitudes toward bisexual men and women in the United States. Journal of Sex Research, 39, 264–274. [DOI] [PubMed] [Google Scholar]
- Houston E, & McKirnan DJ (2007). Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. Journal of Urban Health, 84(5), 681–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. [PubMed] [Google Scholar]
- Kann L, Olsen EO, McManus T, Kinchen S, Chyen D, Harris WA, & Wechsler H (2011). Sexual identity, sex of sexual contacts, and health-risk behaviors among students in grades 9–12: Youth risk behavior surveillance, selected sites, United States, 2001–2009 (Vol. 60, No. 7). DIANE Publishing. [PubMed] [Google Scholar]
- Kanuha V (1990). Compounding the triple jeopardy: Battering in lesbian of color relationships. Women & Therapy, 9(1–2), 169–184. [Google Scholar]
- Kelly BC, Izienicki H, Bimbi DS, & Parsons JT (2011). The intersection of mutual partner violence and substance use among urban gays, lesbians, and bisexuals. Deviant Behavior, 32(5), 379–404. [Google Scholar]
- Kelly BC, Izienicki H, Bimbi DS, & Parsons JT (2011). The intersection of mutual partner violence and substance use among urban gays, lesbians, and bisexuals. Deviant Behavior, 32(5), 379–404. [Google Scholar]
- Kuper LE, Coleman BR, & Mustanski BS (2014). Coping with LGBT and racial–ethnic‐related stressors: A mixed‐methods study of LGBT youth of color. Journal of Research on Adolescence, 24(4), 703–719. [Google Scholar]
- Lanier C, & Maume MO. (2009) Intimate partner violence and social isolation across the rural/urban divide. Violence against Women. 2009; 15(11):1311–1330. [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Banister EM, Ellis WE, & Yeung R (2008). Victimization and relational aggression in adolescent romantic relationships: The influence of parental and peer behaviors, and individual adjustment. Journal of Youth and Adolescence, 37(3), 359–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung P, Cheung M, & Luu TD (2013). Hardships and interpersonal relationships among Asian-Americans with same-sex partners. Journal of GLBT Family Studies, 9(3), 288–301. [Google Scholar]
- Martin-Storey A (2014). Prevalence of dating violence among sexual minority youth: Variation across gender, sexual minority identity and gender of sexual partners. Journal of Youth Adolescence, 44(1), 211–224. [DOI] [PubMed] [Google Scholar]
- McClennen JC, Summers AB, & Vaughan C (2002). Gay men’s domestic violence: Dynamics, help-seeking behaviors, and correlates. Journal of Gay & Lesbian Social Services, 14(1), 23–49. [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Xuan Z, & Conron KJ (2012). Disproportionate exposure to early-life adversity and sexual orientation disparities in psychiatric morbidity. Child abuse & neglect, 36(9), 645–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messinger AM (2014). Marking 35 Years of Research on Same-Sex Intimate Partner Violence: Lessons and New Directions In Handbook of LGBT Communities, Crime, and Justice (pp. 65–85). Springer New York. [Google Scholar]
- Messinger AM (2011). Invisible victims: Same-sex IPV in the national violence against women survey. Journal of interpersonal violence, 26(11), 2228–2243. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2010). Identity, stress, and resilience in Lesbians, Gay Men, and Bisexuals of color. The Counseling Psychologist, 38(3), 442–454. doi: 10.1177/0011000009351601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dietrich J, & Schwartz S (2008). Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. American Journal of Public Health, 98(6), 1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CE, & Mobley AK (2009). Empirical research about same-sex intimate partner violence: A methodological review. Journal of Homosexuality, 56(3), 361–386. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Andrews R, Herrick A, Stall R, & Schnarrs PW (2014). A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. American Journal of Public Health, 104(2), 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B Newcomb ME, & Clerkin EM (2011). Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology, 30, 597–605. doi: 10.1037/a002385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Starks T, & Newcomb ME (2014). Methods for the design and analysis of relationship and partner effects on sexual health. Archives of Sexual Behavior, 43, 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Heinz AJ, Birkett M, & Mustanski B (2014). A longitudinal examination of risk and protective factors for cigarette smoking among lesbian, gay, bisexual, and transgender youth. Journal of Adolescent Health, 54(5), 558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Heinz AJ, & Mustanski B (2012). Examining risk and protective factors for alcohol use in lesbian, gay, bisexual, and transgender youth: A longitudinal multilevel analysis. Journal of Studies on Alcohol and Drugs, 73(5), 783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto T, Bödeker B, & Iwamoto M (2011). Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. American journal of public health, 101(10), 1980–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara RE, & Cooper ML (2015). Bidirectional associations between alcohol use and sexual risk-taking behavior from adolescence into young adulthood. Archives of Sexual Behavior, 44, 857–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantalone DW, Hessler DM, & Simoni JM (2010). Mental health pathways from interpersonal violence to health-related outcomes in HIV-positive sexual minority men. Journal of Consulting and Clinical Psychology, 78(3), 387–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantalone DW, Schneider KL, Valentine SE, & Simoni JM (2012). Investigating partner abuse among HIV-positive men who have sex with men. AIDS and Behavior, 16(4), 1031–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitts M, Mitchell A, Smith A, & Patel S (2006). Private Lives: A report on the health and wellbeing of GLBTI Australians. Australian Research Centre in Sex, Health and Society, La Trobe University. [Retrieved Jan. 2016 from https://www.livingwell.org.au/wp-content/uploads/2012/11/private_lives_report_1_0.pdf] [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, & du Toit M (2011). HLM 7: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: SSI, Inc. [Google Scholar]
- Reuter TR, Sharp C, Temple JR (2015). An exploratory study of teen dating violence in sexual minority youth. Partner Abuse, 6(1), 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes SD, McCoy TP, Wilkin AM, & Wolfson M (2009). Behavioral risk disparities in a random sample of self-identifying gay and non-gay male university students. Journal of Homosexuality, 56(8), 1083–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roch A, Ritchie G, & Morton J (2010). Out of sight, out of mind? Transgender People’s experiences of domestic abuse. Scottish Transgender Alliance and Scotland’s Lesbian, Gay, Bisexual and Transgender Abuse Project. [Retrieved Jan. 2016 from http://www.scottishtrans.org/wp-content/uploads/2013/03/trans_domestic_abuse.pdf] [Google Scholar]
- Safren SA, Heimberg RG (1999). Depression, hopelessness, suicidality, and related factors in sexual minority and heterosexual adolescents. J Consult Clin Psychology, 67(6), 859–866. [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC, & Cohen KM (2007). Development of same-sex attracted youth In The Health of Sexual Minorities (pp. 27–47). Springer US. [Google Scholar]
- Siemieniuk RAC, Miller P, Woodman K, Ko K, Krentz HB, & Gill MJ (2013). Prevalence, clinical associations, and impact of intimate partner violence among HIV-infected gay and bisexual men: A population-based study. HIV medicine, 14(5), 293–302. [DOI] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, … & Catania JA (2003). Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health, 93(6), 939–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasser SM, Smith M, Pendrick-Denney D, Boos-Beddington S, Chen K, & McCarty F (2012). Feasibility study of social media to reduce intimate partner violence among gay men in metro Atlanta, Georgia. Western Journal of Emergency Medicine, 13(3), 298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tajima EA, Herrenkohl TI, Moylan CA, & Derr AS (2010). Moderating the effects of childhood exposure to intimate partner violence: The roles of parenting characteristics and adolescent peer support. Journal of Research on Adolescence, 21(2), 376–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JR, Le VD, Muir A, Goforth L, & McElhany AL (2013). The need for school-based teen dating violence prevention. Journal of Applied Research on Children: Informing Policy for Children at Risk, 4(1), 1–11. [Google Scholar]
- Tonry M, Ohlin LE, & Farrington DP (1991). Human development and criminal behavior: New ways of advancing knowledge. New York, NY, US: Springer-Verlag Publishing. [Google Scholar]
- Turell SC (2000). A descriptive analysis of same-sex relationship violence for a diverse sample. Journal of Family Violence, 15, 281–293. [Google Scholar]
- Walters ML, Chen J, & Breiding MJ (2013). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Findings on Victimization by Sexual Orientation. Atlanta, GA: National Center for Injury Prevention and Control, CDC. [Google Scholar]
- Weiss JT (2004). GL. vs. BT: The archaeology of biphobia and transphobia within the U.S. gay and lesbian community. Journal of Bisexuality, 3, 25–55. [Google Scholar]
- Wong CF, Weiss G, Ayala G, & Kipke MD (2010). Harassment, discrimination, violence and illicit drug use among young men who have sex with men. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education, 22(4), 286–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabora J, Brintzenhofeszoc K, Jacobsen P, Curbow B, Piantadosi S, Hooker C, … & Derogatis L (2001). A new psychosocial screening instrument for use with cancer patients. Psychosomatics, 42(3), 241–246. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, & Berkoff KA (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55(3–4), 610–617. [DOI] [PubMed] [Google Scholar]