Abstract
Patients with low-density lipoprotein cholesterol (LDL-C) ≥190 mg/dl have severe hypercholesterolemia and are at markedly increased risk for adverse cardiovascular events. This study sought to examine the prevalence and treatment of patients with uncontrolled severe hypercholesterolemia in the Veterans Affairs (VA) Health System. The study population was comprised of VA outpatients ≥21 years of age without atherosclerotic disease or diabetes mellitus and an index LDL-C ≥190 mg/dl during April 2011 to March 2014. Patients needed to have filled medications at the VA within the past 6 months. Patient and facility-level predictors of statin use, high-intensity statin use, and statin intensification were analyzed using multivariate logistic regressions. There were a total of 63,576 patients meeting inclusion criteria, including 8,553 (13.5%) women and 26,879 (29.0%) nonwhite patients. The mean (±S.D.) age was 55 (§13) years and the mean of the most recent LDL-C values was 207 ± 22 mg/dl. Only 52% of all eligible patients were on any statin therapy and 9.7% received high-intensity statin therapy. High-intensity statin use increased from 8.6% in 2011 to 13.6% in 2014 (p < 0.001). In adjusted analysis, patients <35 or >75 years of age were less likely to be on a statin (p < 0.001). Women were less likely to be treated than men, odds ratio = 0.88; 95% confidence interval (0.83, 0.92). Similar patterns were observed for predictors of high-intensity statin use and statin intensification. In conclusion, only half of high-risk VA patients with uncontrolled severe hypercholesterolemia were treated with statins and a small minority was on high-intensity statin therapy.
Severe hypercholesterolemia, defined as low-density lipoprotein cholesterol (LDL-C) concentration 190 mg/ dl or above, affects approximately 5% of the US population.1–3 Although familial hypercholesterolemia (FH) is a well-known cause of severe hypercholesterolemia, most patients with an LDL-C above 190 mg/dl will not have an LDL receptor (LDLR) mutation.4 However, those with LDL-C values above this threshold have a marked increased risk of atherosclerotic cardiovascular disease (ASCVD),1,2 and the 2013 American College of Cardiology/American Heart Association (ACC/AHA) cholesterol treatment guideline and the previous treatment guidelines have recommended early initiation of high-intensity statin therapy for primary prevention.5 We thus sought to document patterns of statin use in patients with uncontrolled severe hypercholesterolemia in the Veterans Affairs (VA) Health System.
Methods
We first identified all VA outpatients ≥21 years of age without established ASCVD or diabetes mellitus from April 2011 to March 2014. We examined cohorts at quarterly intervals (index date on the first of January, April, July, and October) and determined all LDL-C values in the previous 6 months. We included those with their most recent LDL-C ≥190 mg/dl. Patients were excluded if they filled no medications at the VA during the 6 months before and after the index date.
Statin intensity was classified according to the ACC/AHA cholesterol guidelines.5 Statin use was defined as a filled prescription in the 6 months following the index date of an LDL-C ≥190 mg/dl. Low-intensity statin therapy was defined as fluvastatin 20 to 40 mg, lovastatin 20 mg, simvastatin 10 mg, pitavastatin 1 mg, and pravastatin 10 to 20 mg. Moderate-intensity statin therapy was defined as atorvastatin 10 to 20 mg, fluvastatin 40 mg twice a day or 80 mg once a day (extended-release formulation), lova-statin 40 mg, pitavastatin 2 to 4 mg, pravastatin 40 to 80 mg, rosuvastatin 5 to 10 mg, and simvastatin 20 to 40 mg. Finally, high-intensity statin therapy was defined as atorvastatin 40 to 80 mg or rosuvastatin 20 to 40 mg. Simvastatin 80 mg was also included as a high-intensity statin dose because it typically lowers LDL-C levels by nearly 50%.6 If patients were prescribed more than 1 type of statin during the previous 6 months, the highest intensity and dose were utilized in the analyses. Statin intensification was determined for those patients who were on no statin or a low- or moderate-intensity statin 6 months before the index date compared with statin intensity 6 months after the index date.
Race/ethnicity was self-reported in the VA Health System Records. Participants were classified as white, Hispanic, black, Asian, Pacific Islander, or other. Participants’ age and gender were also included. Clinical comorbidities included the presence of hypertension, renal disease, malignancy, or a hospitalization within 1-year from the index date. Hospital characteristics were obtained from the American Hospital Association database. These characteristics included geographic region (divided into Northeast, Midwest, South, and West) and academic teaching status defined as membership in the Council of Teaching Hospitals (COTH).
Baseline characteristics of participants were compared by use of statins (no statin, low-intensity, moderate-intensity, and high-intensity) using either analysis of variance for continuous variables or the chi-square test for categorical variables, during each study period. Missing patient characteristics data were rare (<0.1%), except for race, which then included a missing category. The hospital COTH data were missing for 6% of the study sample. For multivariate analyses, we imputed continuous variables using the mean and most common value for categorical variables. Multivariate logistic regression models were constructed to calculate adjusted odds ratios and 95% confidence intervals predicting use of any statin, high-intensity statin therapy, and statin dose intensification.
Variables included in the models included demographics (age, gender, and race), previous diagnoses (hypertension, renal disease, liver disease, and malignancy), filled prescriptions (angiotensin-converting enzyme inhibitors and angiotensin receptor blockers), laboratory values (baseline LDL-C, HDL-C, total cholesterol, triglycerides, and creatinine), region of the country (Northeast, Midwest, South, and West), hospital membership in the COTH, and time period for entry into the cohort (year/quarter). We then adjusted for potential clustering of patients with VA facilities using a robust sandwich covariance matrix estimate. All statistical testing was 2-sided, at a significance level of 0.05. Analyses were performed using SAS statistical software (version 9.4; SAS Institute Inc., Cary, North Carolina).
Results
The study population included a total of 63,576 patients with an index LDL-C ≥190 mg/d (Table 1). Fifteen percent of the sample were women and 29% of the sample was non-white. The mean ± S.D. age was 55 ± 13 years, and the mean of the most recent LDL-C values was 207 ± 22 mg/dl. Fifty-two percent of all eligible patients were on any statin therapy and 9.1% received high-intensity statin therapy. Women were less likely to be taking statins as compared with men. Black patients were significantly more likely to be on high-intensity statin therapy as compared with whites (11.5% vs 8.6%), as were those with hypertension (10.5% vs 7.8%) and renal disease (11.5% vs 9.0%). Veterans treated at VA facilities located in the West were least likely to have a statin prescription, particularly high-intensity statin therapy, as compared with veterans cared for in other geographic regions.
Table 1.
Baseline characteristics of veterans with a severe hypercholesterolemia phenotype by statin intensity (n = 63,576)
| Variable | High intensity | Moderate intensity | Low intensity | No statin | p value |
|---|---|---|---|---|---|
| n = 5,768 | n = 21,874 | n = 5,208 | n = 30,726 | ||
| Age (years), mean (S.D.) | 56.8(11.4) | 55.7 (11.8) | 55.8 (12.3) | 54.1 (14.0) | <0.001 |
| Women | 644(11.2%) | 2,741 (12.5%) | 834 (16.0%) | 4,334(14.1%) | <0.001 |
| White | 3,602 (66.4%) | 14,169 (70.1%) | 3,480 (72.8%) | 20,550 (72.7%) | <0.001 |
| Black | 1,368 (25.2%) | 4,383 (21.7%) | 909 (19.0%) | 5,282(18.7%) | <0.001 |
| Hispanic | 309(5.7%) | 1,154(5.7%) | 273 (5.7%) | 1,635(5.8%) | <0.001 |
| Asian | 37 (0.7%) | 188 (0.9%) | 38 (0.9%) | 255 (0.9%) | <0.001 |
| Native American | 42 (9.6%) | 136 (31.0%) | 34 (7.7%) | 227 (51.7%) | <0.001 |
| Hypertension | 3,192 (55.3%) | 10,933 (50.0%) | 2,561 (49.2%) | 13,651 (44.4%) | <0.001 |
| Renal disease | 203 (3.5%) | 614 (2.8%) | 139 (2.7%) | 811 (2.6%) | p = 0.003 |
| Prior malignancy | 363 (6.3%) | 1,368 (6.3%) | 334 (6.4%) | 1,892 (6.2%) | p = 0.89 |
| Liver disease | 12 (0.2%) | – 53 (0.2%) | 27 (0.5%) | 218(0.7%) | p = 0.003 |
| Hospitalization 1 year prior | 231 (6.2%) | – 716(6.9%) | 154 (7.0%) | 1,237 (7.9%) | <0.001 |
| Council of teaching hospitals | 2,429 (45.3%) | 9,387(45.8%) | 2,060 (42.3%) | 12,685 (44.3%) | <0.001 |
| Midwest | 1,153 (20.0%) | 4,210 (19.3%) | 1,062 (20.4%) | 6,327 (20.6%) | <0.001 |
| Northeast | 789 (13.7%) | 2,878 (13.2%) | 688 (13.2%) | 12,428 (13.2%) | <0.001 |
| South | 2,636 (45.7%) | 9,622 (44.0%) | 2,223 (42.7%) | 12,428 (40.5%) | <0.001 |
| West | 1,190 (20.6%) | 5,164(23.6%) | 1,235 (23.7%) | 7,921 (25.8%) | <0.001 |
| LDL-C (mg/dl), mean (S.D.) | 213.8 (28.3%) | 208.8 (21.3%) | 206.5 (48.1%) | 207.4 (22.3%) | <0.001 |
LDL-C = low-density lipoprotein cholesterol.
High-intensity statins include atorvastatin 40 to 80 mg or rosuvastatin 20 to 40 mg.
Moderate-intensity statins include atorvastatin 10 to 20 mg, fluvastatin 40 g twice a day or 80mg once a day (extended-release formulation), lovastatin 40 mg, pitavastatin 2 to 4 mg, pravastatin 40 to 80 mg, rosuvastatin 5 to 10 mg, and simvastatin 20 to 40 mg.
Low-intensity statins include fluvastatin 20 to 40 mg, lovastatin 20 mg, simvastatin 10 mg, pitavastatin 1mg, and pravastatin 10 to 20 mg.
There was an inverted U-shaped association between statin use and age (Figure 1). Patients under 35 or over 75 years of age were less likely to be on a statin as compared with other age groups (p < 0.001). They were also less likely to be prescribed high-intensity statin therapy. High-intensity statin use increased from 8.6% in 2011 to 13.6% in 2014 (Figure 2).
Figure 1.
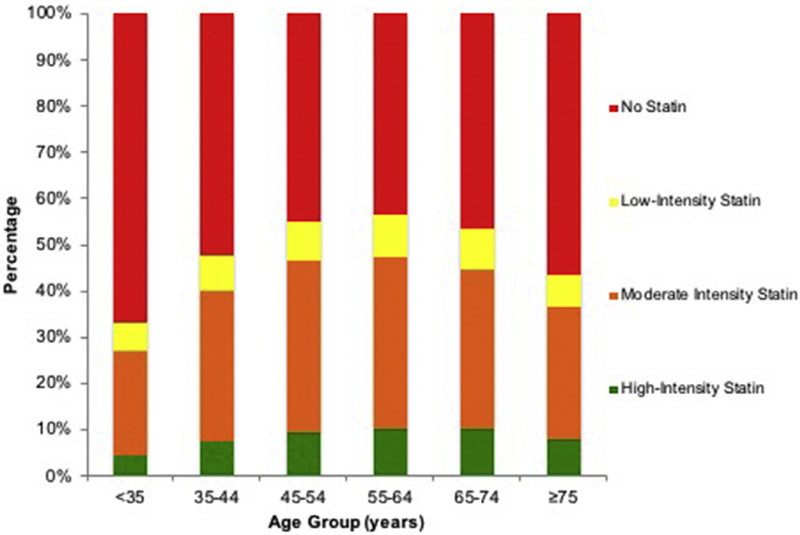
Statin use by age group in Veterans with severe hypercholesterolemia. Overall, there was a U-shaped relation between statin use and age, with younger and older patients’ less likely to be on any statin intensity.
Figure 2.
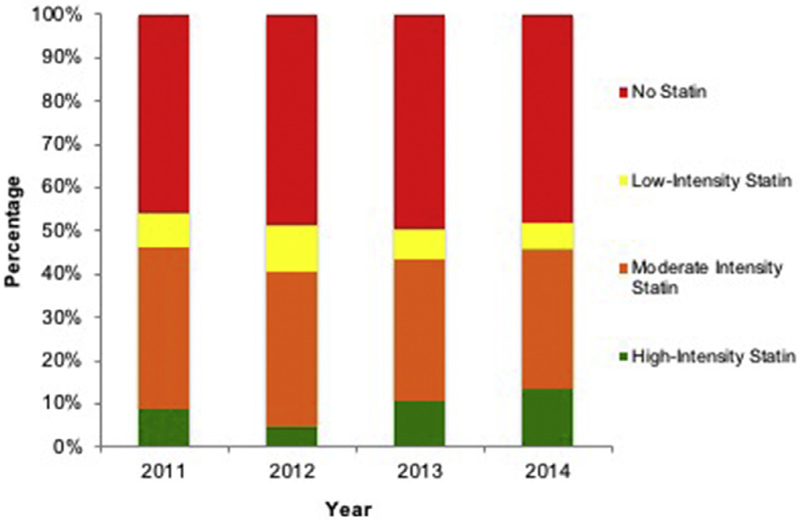
Statin use by year in veterans with severe hypercholesterolemia. Following the release of the 2013 American College of Cardiology/American Heart Association cholesterol management guidelines, there was an increase in high-intensity statin use in this population.
In multivariate-adjusted logistic regression models, this pattern persisted with adults 45 to 54 more likely to be on a statin compared with older and younger age groups. Patients under 35 had 58% lower odds of being on any statin therapy as compared with those age 45 to 54. Women were also less likely to be on a statin as compared with men, odds ratio = 0.88; 95% confidence interval (0.84, 0.92). Blacks, Asians, and Hispanics were more likely to be on statins as compared with whites, as were those with a diagnosis of hypertension (Table 2). Those in facilities located in the West were least likely to receive a statin as were those treated at hospitals that were not members of the COTH.
Table 2.
Multivariate-adjusted predictors of any or high-intensity statin use
| Adjusted odds ratio (95% CI) |
||
|---|---|---|
| Predictors | Any statin use | High-intensity statin use* |
| Age groups (years)** | ||
| <35 | 0.42 (0.40, 0.45) | 0.75 (0.65, 0.87) |
| 35–44 | 0.76 (0.72, 0.80) | 0.92 (0.83, 1.02) |
| 55–64 | 1.06(1.02, 1.11) | 1.12(1.04, 1.21) |
| 65–74 | 0.93 (0.88,0.98) | 1.12(1.02, 1.23) |
| ≥75 | 0.63 (0.57, 0.66) | 1.05 (0.91, 1.22) |
| Women | 0.88 (0.84, 0.92) | 0.81 (0.73, 0.89) |
| Asian† | 1.17 (0.98, 1.40) | 0.91 (0.64, 1.30) |
| Black† | 1.14(1.09, 1.19) | 1.31 (1.22, 1.41) |
| Hispanic† | 1.13 (1.09,1.19) | 1.17(1.02,1.33) |
| Native American† | 0.95 (0.79, 1.15) | 1.30 (0.92, 1.84) |
| Hypertension | 1.19 (1.15, 1.23) | 1.19(1.12, 1.27) |
| Prior malignancy | 1.01 (0.95, 1.09) | 1.08 (0.99, 1.17) |
| Renal disease | 1.05 (0.95, 1.16) | 1.20(1.01, 1.42) |
| Hospitalization in prior year | 0.87 (0.80, 0.95) | 0.87 (0.75, 1.01) |
| Council on teaching hospitals | 1.00(0.97, 1.02) | 1.00 (0.95, 1.06) |
| Midwest‡ | 1.06(1.01, 1.11) | 1.20(1.10, 1.32) |
| Northeast‡ | 1.13 (1.07, 1.19) | 1.20(1.08, 1.32) |
| South‡ | 1.19 (1.14, 1.24) | 1.17(1.09, 1.27) |
Analysis limited to those on any statin (n = 32,850).
Reference group = Age group 45 to 54 years.
Reference group = non-Hispanic white.
Reference group = West.
Restricting our study population to those on any statin therapy, we found similar patterns for predictors of high-intensity statin therapy (Table 2). Notably, patients under 35 had 25% lower odds of being on high-intensity statin therapy as compared with those age 45 to 54. Black, Hispanic, and male patients were more likely to receive high-intensity statin therapy compared with whites and women.
The relation between baseline statin intensity and follow-up intensity (after the LDL-C ≥190 mg/dl value) is shown in Figure 3. An increase in statin intensity was noted in only 16.7% of patients, although there was an improvement from 2011 (14.4% intensification) to 2014 (18.6% intensification, p < 0.001). Only 23% of patients not previously on statins received statin therapy during follow-up after an index LDL-C value above 190 mg/dl.
Figure 3.
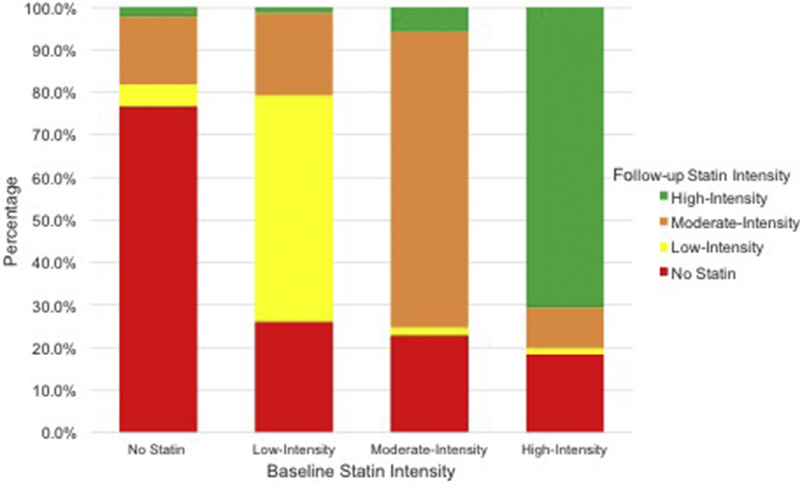
Comparison of baseline statin intensity to follow-up intensity in Veterans with severe hypercholesterolemia. After a documented low-density lipoprotein cholesterol value above 190 mg/dl, less than a quarter of patients previously not on statins were treated with statins. The statin intensity was not increased in most patients.
In multivariate analysis, significant predictors of intensification included being middle-aged (ages 45 to 64 vs other age groups), black (vs white), those with hypertension, those without liver disease, and those in nonwest regions (Table 3).
Table 3.
Multivariate-adjusted predictors of statin intensification*
| Predictors of intensification | Adjusted odds ratio (95% CI) |
|---|---|
| Age groups (years)** | |
| <35 | 0.65 (0.60, 0.72) |
| 35–44 | 0.87 (0.81,0.94) |
| 55–64 | 1.01 (1.01, 1.13) |
| 65–74 | 0.90 (0.83, 0.97) |
| ≥75 | 0.68 (0.61, 0.77) |
| Women | 0.94 (0.88, 1.01) |
| Asian† | 0.87 (0.67, 1.12) |
| Black† | 1.15 (1.08, 1.22) |
| Hispanic† | 1.07 (0.97,1.19) |
| Native American† | 0.95 (0.72, 1.24) |
| Hypertension | 1.08(1.04, 1.14) |
| Renal disease | 1.08 (0.95, 1.24) |
| Hospitalization in prior year | 0.99 (0.88, 1.11) |
| Council on teaching hospitals | 1.01 (0.97, 1.06) |
| Midwest‡ | 1.04(0.98, 1.12) |
| Northeast‡ | 1.10(1.02, 1.19) |
| South‡ | 1.05(0.99, 1.11) |
Analysis limited to patients who were on no statin, low-intensity, or moderate-intensity statin at index date (n = 58,463).
Reference group = Age group 45 to 54 years.
Reference group = nonHispanic white.
Reference group = West.
Discussion
In a national sample of veterans, we identified over 60,000 patients with uncontrolled, severe hypercholesterolemia based on an index LDL-C value at or above 190 mg/dl. We found that within 6 months of this abnormal lab value, only half of these high-risk patients were being treated with statins, and less than 10% were on high-intensity statin therapy as recommended by the 2013 ACC/AHA guidelines. We also found an inverted U-shaped relation between age and statin treatment, with older and younger patients less likely to be treated. Women were less likely to be treated with statins, whereas minority groups and those with a diagnosis of hypertension were more likely to be treated.
Patients with LDL-C values of 190 mg/dl, if left untreated, are at high-risk for cardiovascular events. A recent study by Khera et al showed that LDLR mutations were found in 2% of U.S. adults with LDL-C levels ≥190 mg/dl.4 In those with an LDLR mutation the risk of ASCVD was up to 20-fold higher than in those with normal LDL-C levels. Nevertheless, even in the absence of genetic testing results, the direct relation between elevated LDL-C and risk of ASCVD is compelling; LDL-C >190mg/dl confers a fivefold increase in the long-term risk of ASCVD.7
Although it may not be surprising that providers are less likely to treat older patients with statin therapy that is considered preventive, the reasons for the low rates of treatment in the youngest patients are less clear. Providers may be reluctant to commit young patients to drug therapy, reflecting a “treatment-risk paradox,” where patients at the greatest cardiovascular risk should (but are often not) treated most aggressively.8 Unfortunately, many young patients with hypercholesterolemia fail to be identified and treated until they have experienced an adverse cardiovascular event.9,10 In fact, close to half of providers surveyed were not aware of treatment recommendations for a patient with LDL-C ≥190 mg/dl.11
Adherence to the 2013 ACC/AHA guideline recommendation for high-intensity statin therapy for the primary prevention of adults with an LDL-C ≥190 mg/dl has been similarly low in other populations.5,9,12 Even in patients with diagnosed heterozygous FH receiving care in lipid clinics, only 39% were receiving high-intensity statins and almost a quarter were on no statin therapy.13 The lower use in the VA general population is likely more representative of community care where patients are less likely to be aware of their hypercholesterolemia diagnosis or of the risks associated with not being treated.
Our study has several strengths including our large national population receiving care primarily in general medicine clinics. There are also several limitations that warrant mention. First, we were unable to determine if patients were receiving statin treatment outside of the VA system, although most of these would have been excluded from our analysis, which required at least one medication filled in the VA during the 6-month window. Although this excluded some patients not on any medications, it helped to limit the population to those patients receiving most of their care within the VA system. Our study was not designed to determine the prevalence of severe hypercholesterolemia overall. Our analysis is limited to those with hypercholesterolemia that was uncontrolled. In addition, genetic testing data were not available, so the prevalence of FH in this population is unclear. Finally, we could not determine if lack of treatment was due to patient preferences including statin intolerance.
In conclusion, we evaluated the use of statins for veterans with uncontrolled severe hypercholesterolemia. We found marked underuse of statins in this high-risk patient cohort, with lower use in women as well as younger and older adults. Our findings suggest that significant improvement is needed in order to meet guideline recommended care for these patients.
Footnotes
Disclosures
The authors have no relevant disclosures or relations with industry to report. The views expressed in this manuscript represent those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Sniderman AD, Tsimikas S, Fazio S. The severe hypercholesterolemia phenotype: clinical diagnosis, management, and emerging therapies. J Am Coll Cardiol 2014;63:1935–1949. [DOI] [PubMed] [Google Scholar]
- 2.Gidding SS, Champagne MA, de Ferranti SD, Defesche J, Ito MK, Knowles JW, McCrindle B, Raal F, Rader D, Santos RD, Lopes-Virella M, Watts GF, Wierzbicki AS. American Heart Association Ath-erosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in Young. Council on Cardiovascular and Stroke Nursing. Council on Functional Genomics and Translational Biology. Council on Lifestyle and Cardiometabolic Health. The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation 2015;132:2167–2192. [DOI] [PubMed] [Google Scholar]
- 3.Hopkins PN, Toth PP, Ballantyne CM, Rader DJ. National Lipid Association Expert Panel on Familial Hypercholesterolemia. Familial hypercholesterolemias: prevalence, genetics, diagnosis and screening recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol 2011;5:S9–S17. [DOI] [PubMed] [Google Scholar]
- 4.Khera AV, Won HH, Peloso GM, Lawson KS, Bartz TM, Deng X, van Leeuwen EM, Natarajan P, Emdin CA, Bick AG, Morrison AC, Brody JA, Gupta N, Nomura A, Kessler T, Duga S, Bis JC, van Duijn CM, Cupples LA, Psaty B, Rader DJ, Danesh J, Schunkert H, McPherson R, Farrall M, Watkins H, Lander E, Wilson JG, Correa A, Boerwinkle E, Merlini PA, Ardissino D, Saleheen D, Gabriel S, Kathiresan S. Diagnostic yield of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol 2016;67:2578–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr., Watson K, Wilson PW. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2889–2934. [DOI] [PubMed] [Google Scholar]
- 6.Smith MEB, Lee NJ, Haney E, Carson S. Drug Class Review: HMG-CoA Reductase Inhibitors (Statins) and Fixed-dose Combination Products Containing a Statin: Final Report Update 5. Portlands, OR: Oregon Health & Science University, 2009. [PubMed] [Google Scholar]
- 7.Perak AM, Ning H, de Ferranti SD, Gooding HC, Wilkins JT, Lloyd-Jones DM. Long-term risk of atherosclerotic cardiovascular disease in US adults with the familial hypercholesterolemia phenotype. Circulation 2016;134:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA 2004;291:1864–1870. [DOI] [PubMed] [Google Scholar]
- 9.Casula M, Scotti L, Tragni E, Merlino L, Corrao G, Catapano AL. Drug treatment and adherence of subjects <40 years with diagnosis of heterozygous familial hypercholesterolemia. Atherosclerosis 2016;254:172–178. [DOI] [PubMed] [Google Scholar]
- 10.Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, Wiklund O, Hegele RA, Raal FJ, Defesche JC, Wiegman A, Santos RD, Watts GF, Parhofer KG, Hovingh GK, Kovanen PT, Boileau C, Averna M, Boren J, Bruckert E, Catapano AL, Kuivenhoven JA, Pajukanta P, Ray K, Stalenhoef AF, Stroes E, Taskinen MR, Tybjaerg-Hansen A. European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J 2013;34:3478–3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Virani SS, Pokharel Y, Steinberg L, Chan W, Akeroyd JM, Gowani SA, Kalra A, Polsani V, Miedema MD, Jones PH, Nambi V, Petersen LA, Ballantyne CM. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol 2016;10:497–504. [DOI] [PubMed] [Google Scholar]
- 12.Zafrir B, Jubran A, Lavie G, Halon DA, Flugelman MY, Shapira C. Clinical features and gaps in the management of probable familial hypercholesterolemia and cardiovascular disease. Circ J 2017;82: 218–223. [DOI] [PubMed] [Google Scholar]
- 13.deGoma EM, Ahmad ZS, O’Brien EC, Kindt I, Shrader P, Newman CB, Pokharel Y, Baum SJ, Hemphill LC, Hudgins LC, Ahmed CD, Gidding SS, Duffy D, Neal W, Wilemon K, Roe MT, Rader DJ, Ballantyne CM, Linton MF, Duell PB, Shapiro MD, Moriarty PM, Knowles JW. Treatment gaps in adults with heterozygous familial hypercholesterolemia in the United States: data from the CASCADE-FH registry. Circ Cardiovasc Genet 2016;9:240–249. [DOI] [PMC free article] [PubMed] [Google Scholar]


