Highlights
-
•
RO teaching is underrepresented in the curriculum of medical students in Europe.
-
•
RO is often taught and examined in modular courses.
-
•
E-learning, computer-based examination and OSCE are used in few institutions.
-
•
Clerkships and policies to enroll students in RO departments should be improved.
Keywords: Undergraduate medical education, Curriculum, Medical students, Radiation oncology
Abstract
Aim
To provide an overview of Radiation Oncology (RO) teaching to medical students around Europe.
Materials and methods
An electronic survey was sent to European academic teachers of RO. The survey focused on the teaching of RO to medical students throughout their undergraduate education.
Results
A total of 87 academic RO teachers from 29 countries were invited to participate in the electronic survey. Thirty-two surveys were completed by respondents from 19 European countries (response rate: 37%). The median number of hours devoted to RO teaching was 10 h (mean 16 h, range 2–60). The number of hours assigned to RO teaching was equal or inferior compared to medical oncology. In two institutions (6%) RO was delivered as a stand-alone course with an individual knowledge assessment. In 30 institutions (94%), the RO course was taught and/or assessed in a modular curriculum with other disciplines. Radiobiology, breast, lung, gastrointestinal, gynecologic malignancies, RO adverse events and palliative RO were taught in 80% of institutions. Pediatric RO, RO for benign conditions and economic topics were taught in less than 30% of institutions. In most institutions, classical written and oral examinations were used. Computer-based examinations and/or objective structured clinical examinations (OSCE) were seldom used. E-learning methods were available in less than 10% of institutions. A clerkship in RO department was available in 28 out of 32 institutions (87%), less than 5% of medical students were involved in research in RO during their undergraduate education. Strategies to encourage medical students to consider RO as a future career were offered in 53% of institutions.
Conclusions
RO teaching to medical students was not uniform in Europe. RO teaching during undergraduate education in Europe was undervalued, and its knowledge and learning tools could be broadened and updated in the core curricula of medical students
1. Introduction
In the last decades, the overall rate of cancer diagnoses has steadily been increasing worldwide. Cancer is the second cause of death after cardiovascular diseases. Approximately 3.4 million of individuals were diagnosed with cancer in Europe in 2012 (excluding non-melanoma skin cancer). At that date, about 80% of those patients were resident in the European Union countries [1].
Almost 50% of patients who have cancer undergo radiotherapy [2]. Tailored treatments are currently being implemented to reduce the adverse effects related to radiotherapy treatment [3], [4]. Radiotherapy has been proven a valuable and cost-effective option in both curative treatment and palliative care [3], [4], [5].
Surprisingly, despite the high number of patients treated with radiotherapy, primary care providers and other specialists are scarcely exposed to RO during their undergraduate education [6], [7], [8], [9], [10]. This lack of education in RO during the undergraduate education was even more concerning than in medical oncology [11]. In a recent article, Mattes and al. analyzed the core curriculum of medical students of 49 different academic institutions in the United States. This survey revealed that only 41% of these institutions declared a faculty participation in educational sessions for medical students focusing on specific oncology topics. Moreover, 25% of these sessions were specifically dedicated to RO [12].
This insufficiency of education in RO during undergraduate curriculum may lead to inadequate patient management, an undervaluation of the toxicity of treatments, a suboptimal communication between patients and general practitioners, radiation oncologists, medical oncologists and palliative or supportive care specialists [10]. As a consequence, recent publications have focused on the potential interest of increasing medical student exposition to RO during their undergraduate education [6], [7], [8], [9], [12], [13], [14], even if the real impact of RO teaching to medical student to lastingly improve their clinical skills is a matter of debate [15].
These studies were designed by RO academic teachers and addressed to medical students to assess different structured core curricula [3], [4], [16]. These initiatives were undertaken to encourage medical students to focus their interest in RO and to develop the skills required to play a useful role in the management of oncologic patients in a multidisciplinary environment.
Unlike USA [6], [8], [9], [17], Canada [11], [13], Australia and New Zealand [18], in Europe data regarding the teaching of RO to medical students was very limited [7], [14]. A European core curriculum implementation initiative was developed only for clinicians, medical physicists and technologist in RO, but not for medical students [19].
In addition, as reported for other related disciplines in Europe, significant differences between the health care systems and medical school curriculum may result in substantial differences of RO teaching amongst European countries [20].
The present survey, addressed to academic teachers of RO was designed to provide an overview of RO teaching to medical students in Europe and to provide a preliminary database to be used, in a second step, to build a pilot reference core curriculum in RO for European Universities.
2. Materials and methods
2.1. Survey design
The survey was designed to be addressed to academic radiation oncology teachers to investigate how RO was taught to medical students in their institutions. A cluster 19-item questionnaire was developed and transposed in an electronic format using a commercial software (Survey-Monkey®, http://surveymonkey.net) (Appendix 1). The questions were targeted to evaluate critical items including:
-
1)
the duration of medical and RO training;
-
2)
the details of the RO curriculum content;
-
3)
the role of other professionals (e.g. physicists) involved in RO teaching;
-
4)
the availability of an e-learning programme;
-
5)
the availability and the features of clerkship in RO departments;
-
6)
the presence of a programme to involve medical students in research in the field of RO;
-
7)
the presence of a policy to orient medical students towards RO as a career option.
Input fields were made of closed or non-narrative open-ended response to capture accurate standardized answers [21]. Besides, narrative open answers were possible for all of the questions to voluntarily provide additional details on a particular question and/or answer in a narrative format. Respondents were given the possibility to save and complete the survey later, to allow participants to complete responses after verifying the corresponding information, if needed.
2.2. Survey participants selection and survey diffusion
The questionnaire was built by the main author (SBM) on basis of previous articles addressing the same topics for other medical disciplines. Those articles were extensively cited through the manuscript. In order to assess the face validity of the survey, the first draft was sent to a panel of three academic radiation oncologists from different institutions (PC, NJ, PM). They were asked to validate the appropriateness and clarity of the questionnaire.
In addition, their comments and suggestions were included in the provisional survey and, eventually, validated by a consensus session.
The updated version of the survey was resent to the panel and eventually validated by a consensus. This consensus was used to test the intelligibility of the survey.
The final version of the electronic survey was therefore sent to the academic teachers of RO in all European countries.
Because the study did not focus on patients or animals and no medical records were considered in the analysis, the approval of the local ethics committee was not solicited.
To build a comprehensive respondent database, we used the ESTRO site to find the national societies informations including the national representing radiation oncologist (https://www.estro.org/about-us/national-societies/external-audists-in-radiotherapy). Further respondents were found by consulting the database of the UEMS (Union Européenne des Médecins Spécialistes) (https://www.uems.eu/). These databases were worthwhile to identify the first network of responders. The respondents' selection was therefore implemented by a manual search on the Internet, browsing the information provided on the website of the academic hospitals. In addition, in the survey, each respondent was invited to provide to the survey leader (SBM) the name and other details of others RO academic teacher of her/his country by a snowball recruitment.
The goal was to reach at least two university hospitals of each country to assess the teaching differences within the same nation.
The survey was sent by e-mail to all potential respondents with an automatic reminder at one and two months after the first invitation in the attempt to increase the response rate.
The inclusion criteria for the selection of respondents were:
-
1)
being a radiation oncologist actively involved in teaching RO to medical students;
-
2)
the acceptance to provide personal information with the guarantee that the respondent and the university details would be anonymized.
The exclusion criteria for the selection of respondents were:
-
1)
being involved in teaching RO as a Physicist, Radiobiologist, Medical Oncologist;
-
2)
multiple respondents from the same academic institution: to avoid a data redundancy from a single institution, we selected the survey written by the teacher with the highest academic position for the analysis.
2.3. Data collection
The survey data were extracted using the automated system provided by the electronic platform Survey-Monkey (http://surveymonkey.net). All the responses to the survey were collected from June 2015 to June 2017. This time was necessary to wait and collect a representative database. The survey was closed in June 2017 because longer delay would have influenced the temporal coherence of the collected data.
2.4. Statistical analysis
Statistical analysis was carried out using a biostatistics medical software (MedCalc, Morsel, Belgium, Version 18.5) and graphics were obtained by using an Excel worksheet (Office package 365-2018, Microsoft).
3. Results
3.1. Feature of the RO teachers who participated in the survey
Eighty-seven academic teachers from 29 different countries were invited to participate in this study. Of those, 53 completed the questionnaire (rough response rate = 61%). However, 16 questionnaires were excluded because of missing data (16 out of 53 = 30%) and five because two academic teachers of the same university performed the survey (5 out 53 = 10%).
Hence, 32 surveys (rough response rate = 35%) were filled and were therefore included in the final analysis, representing 19 different countries.
The mean response rate per country was 1,9 (range 1–4). Details on the number of respondent academic teachers per country are given in Table 1.
Table 1.
Number of respondents per country and country codes.
| Country | # of respondents |
|---|---|
| Belgium (BE) | 4 |
| Bulgaria (BG) | 1 |
| Czech Republic (CZ) | 1 |
| Croatia (HR) | 1 |
| Denmark (DK) | 2 |
| Hungary (H) | 1 |
| France (FR) | 1 |
| Germany (DE) | 2 |
| Italy (IT) | 4 |
| Netherland (NL) | 2 |
| Norway (NO) | 1 |
| Poland (PL) | 1 |
| Portugal (PT) | 1 |
| Romania (RO) | 1 |
| Serbia (RS) | 1 |
| Slovakia (SK) | 3 |
| Slovenia (SI) | 1 |
| Spain (SP) | 2 |
| Switzerland (CH) | 2 |
| Total: 19 countries | 32 respondents |
3.2. Timing of RO teaching
In all the 19 countries represented in this study, there was a 6-year medical undergraduate curriculum.
RO courses were delivered to medical students either during their 2nd year (n = 1, BE), 3rd year (n = 4: NL, SP, NL, BE), 4th year (n = 10: IT, BE, SI, SL,SL, FR, CH, HR, DK, BG), 5th year (n = 5: IT, BE, CZ, HU, RO) or 6th year of the undergraduate cursus (n = 3: PO, DK, NO).
Noticeably, in 9 institutions (28%) RO was delivered at different periods during the curriculum:
-
-
Three different periods: at the 2nd, 4th and 6th year (n = 1: CH) and 4th, 5th and 6th year (n = 3: SP, DE, DE)
-
-
Two different periods: at the 3rd and 5th year (n = 2: PL, IT), 3rd and 4th year (n = 1: IT), 4th and 6th (n = 1: SL), 3rd year and 6th (n = 1: RS).
3.3. Specialists involved in RO teaching
The number of teachers involved in the teaching of RO to medical students ranged from 1 to 12 academic teachers (mean 3,8; SD 3,3).
All the respondents provided the number of teachers involved in teaching RO to medical students in their institutions.
In nearly half of the institutions (15/32 = 47% of all institutions), RO specialists were the only teachers involved in delivering the RO courses to medical students (PO, CH, BE, FR, IT, IT, SK, IT, IT, SK, RS, NL, BE, BG, CZ).
In 10 institutions, medical oncologists also participated in the RO teaching in the same sessions with RO specialists and/or specialists from other medical disciplines (31% of all institutions participating in the survey: DK, DK, HR, BE, SW, BE, SP, SL, NO, RO).
In 8 institutions (HR, DE, SP, SL, SP, DE, PL, HU) medical physicists were also involved in the RO teaching to medical students.
Radiobiologists participated in the teaching of radiation oncology in only five institutions (DE, DE, BE, SP, NL).
3.4. Feature of RO teaching
RO was a stand-alone course with an individual examination in two institutions (6%: PL, RO). In 11 institutions (35%, PO, HR, BE, BE, BE, DE, DE, FR, IT, IT, IT) RO was taught as an independent discipline, but the knowledge assessment was embedded in a multidisciplinary examination. In 17 (BE, DK, DK, CH, CH, SP, SL, SL, SL, IT, NL, NL, RS, NO, HU, BG, CZ) out of 32 institutions (53%) the RO teaching was part of a modular course along with other disciplines (e.g. oncology, internal medicine, surgical oncology, neurology, nuclear medicine) with a final overall examination (RO and other disciplines).
In two institutions, (6%: SL, SP) RO was also taught as a modular course along with other disciplines but with a final stand-alone examination for RO.
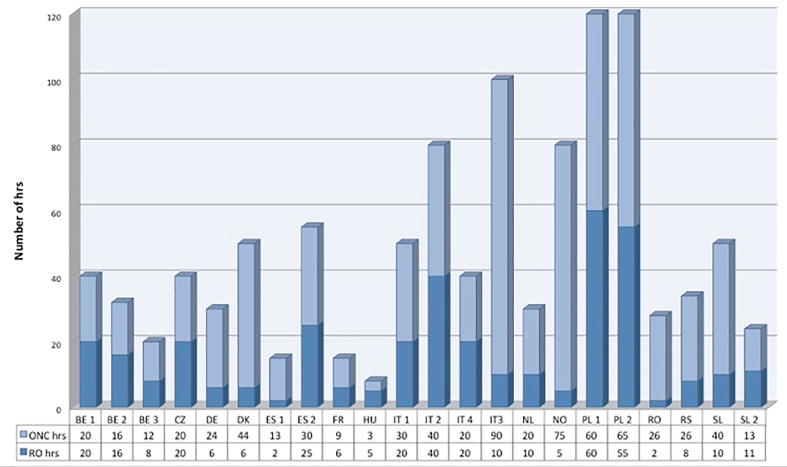
Twenty-two respondents (22 out of 32 = 69%) specified the total numbers of hours devoted to RO teaching and the overall number of hours devoted to oncology (RO along with Medical Oncology) (Fig. 1). The mean time allocated to RO was of 16 h, but there were significant differences amongst the different centers, with a range from 2 to 60 h and a median of 10 h.
Fig. 1.
Number of hours of teaching devoted to RO (RO hrs) in deep blue and the number of hours devoted to the teaching of medical oncology for each respondent institution (ONC hrs) in light blue.
The key topics assessed in the present survey were not taught in all of the institutions. The percentage for each specific key topic is detailed in Fig. 2.
Fig. 2.
Percentage of institutions in which each key topic in RO was taught to medical students during their core curriculum.
Concerning the final assessment of acquired knowledge, the final examination format for each particular topic is detailed in Table 2.
Table 2.
Final assessment of knowledge for each key topic in RO: the total number of respondents for each topic is detailed in the table. For Each topic the number of institutions using a certain method is expressed as an absolute number and in percentage. Abbreviation used in the table: N: No examination; W: Written examination, CBE: Computer based Examination; OSCE: Objective Structured Clinical Examination.
| Topics | N | O | W | OSCE | CBE | Number of respondents |
|---|---|---|---|---|---|---|
| Radiobiology | 5 (16,66%) | 7 (23,33%) | 14 (46,66%) | 1 (3,33%) | 3 (10%) | 30 |
| Radiation physics | 5 (20,83%) | 4 (16,66%) | 11 (45,83%) | 1 (4,16%) | 3 (12,5%) | 24 |
| Radiosurgery | 5 (20%) | 8 (32%) | 9 (36%) | 0 (0%) | 3 (12%) | 25 |
| Brachytherapy | 3 (11,53%) | 10 (38,46%) | 10 (38,46%) | 0 (0%) | 3 (11,5″%) | 26 |
| Palliative RT | 2 (7,4%) | 10 (37,03%) | 11 (40,74%) | 2 (7,40%) | 2 (7,40%) | 27 |
| Breast RT | 3 (10%) | 10 (33,33%) | 12 (40%) | 2 (6,66%) | 3 (10%) | 30 |
| CNS RT | 2 (7,69%) | 8 (30,76%) | 11 (42,30%) | 2 (7,69%) | 3 (11,53%) | 26 |
| Head and neck RT | 3 (10,71%) | 9 (32,14%) | 11 (39,28%) | 2 (7,14%) | 3 (10,71%) | 28 |
| Lung RT | 2 (6,89%) | 9 (31,03%) | 13 (44,82%) | 2 (6,89%) | 3 (10,34%) | 29 |
| Gastro-intestinal RT | 2 (7,4%) | 9 (33,33%) | 11 (40,74%) | 2 (7,'%) | 3 (11,11%) | 27 |
| Genito-urinary RT | 2 (7,14%) | 9 (32,14%) | 12 (42,85%) | 2 (7,14%) | 3 (10,71%) | 28 |
| Gynaecologic RT | 3 (10,34%) | 10 (34,48%) | 11 (37,93%) | 2 (6,89%) | 3 (10,34%) | 29 |
| Skin RT | 6 (28,57%) | 5 (23,80%) | 8 (38,09%) | 1 (4,76%) | 1 (4,76%) | 21 |
| Bone and soft tissue RT | 5 (26,31%) | 7 (36,84%) | 6 (31,57%) | 0 (0%) | 1 (5,26%) | 19 |
| Benign conditions RT | 7 (53,84%) | 2 (15,38%) | 3 (23,07%) | 0 (0%) | 1 (7,69%) | 13 |
| Pediatric RT | 8 (50%) | 1 (6,25%) | 5 (31,25%) | 0 (0%) | 2 (12,5%) | 16 |
| Toxicities of RT | 4 (15,38%) | 7 (26,92%) | 11 (42,30%) | 2 (7,69%) | 2 (7,69%) | 26 |
| Toxicities management | 5 (25%) | 6 (30%) | 6 (30%) | 1 (5%) | 2 (10%) | 20 |
| RT for Hematologic malignancies | 7 (36,84%) | 4 (21,05%) | 4 (21,05%) | 1 (5,26%) | 3 (15,78%) | 19 |
| Economic aspects of RT | 8 (72,72%) | 1 (9,09%) | 1 (9,09%) | 0 (0%) | 1 (9,09%) | 11 |
| Radiation protection | 5 (31,25%) | 4 (25%) | 5 (31,25%) | 0 (0%) | 2 (12,5%) | 16 |
E-learning for RO was available to medical students in 10 out of 32 institutions (31%). Medical students were able to access learning cases on the Internet on a specific website in 5 institutions (RO, DK, DK, BE, SP). In 2 institutions the learning cases were available on computers located in a University facility (NO, IT) and they were not available on the web. Interactive webinars in RO were delivered in 2 institutions.
Medical students involved in research programmes or scientific programmes reported by the institutions represent less than 5% of the entire medical student population, except for two institutions (HR, SL) that reported higher rates ranging from 5% to 20%.
In most of the institutions i.e. 28 out of 32 (90%), a clerkship for medical students was available on demand.
The clerkship period was unavailable for medical students in 4 institutions out of 32 (10%) (DK, PO, SL, CZ).
A clerkship in radiation oncology was mandatory in one institution (IT).
A policy to encourage medical students to consider RO as a career option was present in 17 out of 32 institutions (53%) (DK, PO, SW, BE, BE, SW, DE, FR, BE, IT, SI, DE, NO, PL, HU, BE, CZ), while there was no such a policy in 15 out of 32 institutions (47%) (DK, HR, SP, SL, IT, IT, SL, IT, NL, SL, SP, HR, RO, NL, BG).
4. Discussion
Medical students have been traditionally reported to be poorly exposed to oncology-related topics during their undergraduate education in both North American and European Universities [22]. In Europe, a survey involving 100 universities revealed that oncology was present in medical students’ core curricula in only 40% of those institutions [23].
Besides, a steady decrease of the involvement of radiation oncologists as teachers in academic institution has been reported over the last decades, with as little as 30% of academic Radiation oncologists involved in medical students’ education with a mean teaching frame of 7 h [24].
It was reported that RO education was even more limited than medical oncology education [8]. Besides, the lack of a mandatory clerkship in RO hinders a practical approach to RO [25].
These observations should stimulate a bigger effort to broaden the visibility of RO. Local and multi-institutional pilot initiatives were undertaken to include RO into the core curriculum for medical students [6], [8], [9], [12], [14], [17], [25], [26]. These initiatives paralleled similar processes implemented for medical students in other medical disciplines such as internal medicine [27], surgery [28], emergency medicine [29], dermatology [30], uro-nephrology [31], [32], palliative care medicine [33], radiology [20] and nuclear medicine [34].
The present survey revealed some interesting results that provide an overview of RO teaching to medical students in Europe. There was a lack of a systematic investigation for this topic.
First, the present survey showed that in most European academic institutions (10/32, 31%) RO education was delivered to medical students during their fourth year. However, in almost one-third of the respondent institutions (9/32, 28%) RO courses were delivered at different periods of the core curriculum, usually from the third year onward.
Second, RO was a stand-alone course with a focused knowledge assessment in 6% of the institutions participating in the survey. In most European academic institutions, RO was taught in modular courses and the final examination was part of a broader knowledge assessment.
Third, the time devoted to oncology-related topics significantly varies amongst the different institutions, ranging from 2 to 60 h. However, the ratio of the time assigned to RO teaching was always equal or inferior to that scheduled to medical oncology. Interestingly, this variability regarding hours was also present amongst universities in the same country. These data confirm that RO was even more neglected than medical oncology in European universities.
Fourth, the critical topics in RO education were: Radiobiology, RO for breast, gynecologic, lung malignancies and RO toxicities, taught in at least 80% of the responding institutions.
The choice to focus on particular cancers in the RO teaching seemed to be in accordance, at least partly, with cancer incidence in Europe and radiation oncology efficacy in those diseases. Hence, the selection of topics was influenced by other factors (differences between institutional/country guidelines, competition with other established treatments (chemotherapy, surgery), RO availability, different techniques of RO availability, socioeconomic factors…). Investigating this observation even further in another study would be interesting.
Fifth, new teaching and knowledge evaluation tools such as e-learning techniques, OSCE and computer-based examination were available in only few institutions.
E-learning techniques were proven to improve the learning in other disciplines individually and when used in groups of students in case-based sessions [35].
Clerkship in RO was available in most of the institutions but only on demand.
Sixth, there was a minor involvement of medical students in research programs in the field of RO. In the present survey a policy to encourage medical students to consider RO as a future career option was present in only half of the respondent institutions.
Because medical schools are in charge of the quality of education provided to medical students, as suggested by previous articles on this matter [12], the teaching of radiation oncology to medical students should be improved at institutional and university level in the environment of the local medical schools. The European societies such as the ESTRO and the UEMS along with the national societies could play a role in this process in promoting and backing the local initiatives.
This could be of help to build a template core curriculum of RO for medical students as a reference for the local institutions.
However, the present study has several limitations.
First, the collected data were provided by teachers willing to participate in this initiative with a low rate of valid respondents (30%). In addition, not all the European countries are represented in the survey and some countries were overrepresented. This bias could have substantially influenced our results. Noticeably, a survey performed in a hundred institutions in the USA [12] revealed that only 30% of the institutions offered a RO education in their mandatory core curriculum, while in the present survey, all the respondents declare that there was a RO teaching in their core curriculum.
A more extensive survey should be launched to have access to a more comprehensive data set.
Second, because of the long turn-around time between the electronic invitation and the responses, the collection of the database was long (approximately two years). Nevertheless, the extent of the collected data and the absence of studies on the same matter could be considered related to difficulties to yield data on this particular matter.
Finally, there was a low rate of answers completed in the free text window associated with each particular question. Therefore, the results were likely to be influenced by the inherent structure and/or type of questions established in the survey.
5. Conclusion
The results of our study are in line with the results reported by similar investigations performed in North America indicating the necessity of broadening the visibility and the diffusion of knowledge in RO to medical students around Europe.
A reference core curriculum definition, adapted to European academic institutions, including e-learning techniques and a practical clerkship program are possible ways to improve RO knowledge during the undergraduate education.
Conflict of interest statement
This is an academic study performed without any funding. The authors declare that they have no conflict of interest.
Appendix 1
Survey Questions:
-
1.Personal informations
-
-First name
-
-Family name
-
-University
-
-Department
-
-Position: Full Professor, Associate Professor, Lecturer…)
-
-City/town
-
-Country
-
-Email address
-
-Phone number
-
-
-
2.
How is undergraduate teaching in radiation oncology structured in your medical school?
- Possible answers:
-
-Classical type with its own exam: RO as independent discipline with its own exam
-
-Classical type but part of a large exam: RO as an independent discipline and part of a large exam (E.G internal medicine, surgery, oncology, radiology)
-
-Modular type with its own exam: RO taught as part of other disciplines but with its own exam
-
-Modular type and part of a large exam
-
-Other teaching methods: specify
-
-
-
3.
Are e-learning methods available in your university for the teaching of radiation oncology?
- Possibles answers:
-
-Web-based case-based learning
-
-Case-based learning on computers in a university facility
-
-Online courses and/or webinars on particular topics (MOOC, SPOC…)
-
-No e-learning available in my university?
-
-Other: please specify
-
-
-
4.
How long is medical school in your country (to be qualified as medical doctor)
- Possibles answers:
-
-3Y
-
-4Y
-
-5Y
-
-6Y
-
-7Y
-
-8Y
-
-Other: please specify
-
-
-
5.In which year(s) of medical school do students have radiation oncology classes (more than one answer possible)
-
-first year
-
-second year
-
-3rd year
-
-4th year
-
-5th year
-
-6th year
-
-7th year
-
-8th year
-
-
-
6.How many hours are devoted to Radiation Oncology in your Medical School?(please sum up the number of hours in the curriculum of medical students)
-
-Open answer
-
-
-
7.How many hours are devoted to oncology in general in your medical school: (Medical oncology + Radiation oncology)
-
-Open answer
-
-
-
8.
Who teaches radiation oncology in your medical school (more than one answer is allowed)
- Possibles answers:
-
-radiation oncologist
-
-medical oncologist
-
-physicist
-
-Radiobiologist
-
-Each organ specialist (i.e. gastroenterologist, neurologist, pneumologist) in its own course
-
-Other: specify
-
-
-
9.
What domains of radiation oncology are discussed in the course?
- Possible answers, more than one answer is possible:
-
-Radiobiology
-
-Radiation physics
-
-Radiosurgery
-
-Brachytherapy
-
-Palliative radiotherapy
-
-Breast radiotherapy
-
-Central Nervous system radiotherapy
-
-Head and neck radiotherapy
-
-Lung radiotherapy
-
-Gastro-intestinal radiotherapy
-
-Genito-urinary radiotherapy
-
-Gynecologic radiotherapy
-
-Skin radiotherapy
-
-Bone and soft tissue radiotherapy
-
-Benign conditions radiotherapy
-
-Pediatric radiotherapy
-
-Complications of radiotherapy
-
-Economical aspects of radiotherapy
-
-Radiotherapy for hematologic malignancies
-
-Radioprotection
-
-
-
10.
What domaines of radiation oncology are assessed in the final exam and how: Oral exam, Written exam, OSCE: objective structured clinical examination or CBE: computer based examination.
- Possibles answers:
-
-Radiobiology
-
-Radiation physics
-
-Radiosurgery
-
-Brachytherapy
-
-Palliative radiotherapy
-
-Breast radiotherapy
-
-Central Nervous system radiotherapy
-
-Head and neck radiotherapy
-
-Lung radiotherapy
-
-Gastro-intestinal radiotherapy
-
-Genito-urinary radiotherapy
-
-Gynecologic radiotherapy
-
-Skin radiotherapy
-
-Bone and soft tissue radiotherapy
-
-Benign conditions radiotherapy
-
-Pediatric radiotherapy
-
-Complications of radiotherapy
-
-Economical aspects of radiotherapy
-
-Radiotherapy for hematologic malignancies
-
-Radioprotection
-
-
-
11.
How many teachers are involved in teaching radiation oncology in your medical school?
Possibles answers:
-
-
1 dedicated teacher
-
-
2 dedicated teachers
-
-
Other: please specify
-
12.
Is there an online course of radiation oncology in your university?
Yes/no
-
13.
: If yes, please provide the link below.
-
14.
What percentage of medical students enrolled in your university are involved in a research or scientific program in RO each year (e.g. scientific article, communication, poster…)
- Possibles answers:
-
-less than 5%
-
-between 5–20%
-
-between 21–40%
-
-more than 41%
-
-
-
15.
Describe the radiation oncology clerkship in your medical school:
- Possibles answers :
-
-there is no clerkship in RO
-
-Clerkship in RO is optional
-
-Clerkship in RO is mandatory
-
-Other : please specify
-
-
-
16.From what year of medical school onward can internship in radiation oncology be attended by medical students:
-
-3
-
-4
-
-5
-
-6
-
-7
-
-8
-
-never
-
-
-
17.
Is there a policy to attract students to consider RO as a career option?
Yes/no
If yes, please specify
-
18.
In case you have questions or remarks concerning this project, please feel free to add them below
Thank you for completing this survey.
References
- 1.Steliarova-Foucher E., O’Callaghan M., Ferlay J., Masuyer E., Rosso S., Forman D. The European cancer observatory: a new data resource. Eur J Cancer. 2015;51:1131–1143. doi: 10.1016/j.ejca.2014.01.027. [DOI] [PubMed] [Google Scholar]
- 2.Barton M.B., Jacob S., Shafiq J., Wong K., Thompson S.R., Hanna T.P. Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother Oncol. 2014;112:140–144. doi: 10.1016/j.radonc.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 3.Delaney G., Jacob S., Featherstone C., Barton M. The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer. 2005;104:1129–1137. doi: 10.1002/cncr.21324. [DOI] [PubMed] [Google Scholar]
- 4.Delaney G.P., Barton M.B. Evidence-based estimates of the demand for radiotherapy. Clin Oncol (R Coll Radiol) 2015;27:70–76. doi: 10.1016/j.clon.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Cai B., Nickman N.A., Gaffney D.K. The cost-effectiveness of external beam radiation therapy in bone metastases. Curr Opin Supp Palliative Care. 2013;7:278–283. doi: 10.1097/SPC.0b013e328362e8e3. [DOI] [PubMed] [Google Scholar]
- 6.Golden D.W., Spektor A., Rudra S., Ranck M.C., Krishnan M.S., Jimenez R.B. Radiation oncology medical student clerkship: implementation and evaluation of a bi-institutional pilot curriculum. Int J Radiat Oncol Biol Phys. 2014;88:45–50. doi: 10.1016/j.ijrobp.2013.10.041. [DOI] [PubMed] [Google Scholar]
- 7.Haagedoorn E.M., de Vries J. Topic selection in undergraduate medical education and relevance to general practice. J Cancer Educ. 1998;13:137–140. doi: 10.1080/08858199809528534. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch A.E., Mulleady Bishop P., Dad L., Singh D., Slanetz P.J. An increase in medical student knowledge of radiation oncology: a pre–post examination analysis of the oncology education initiative. Int J Radiat Oncol Biol Phys. 2009;73 doi: 10.1016/j.ijrobp.2008.12.012. 1003-8.e2. [DOI] [PubMed] [Google Scholar]
- 9.Hirsch A.E., Singh D., Ozonoff A., Slanetz P.J. Educating medical students about radiation oncology: initial results of the oncology education initiative. J Am Coll Radiol. 2007;4:711–715. doi: 10.1016/j.jacr.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Samant R., Malette M., Tucker T., Lightfoot N. Radiotherapy education among family physicians and residents. J Cancer Educ. 2001;16:134–138. doi: 10.1080/08858190109528754. [DOI] [PubMed] [Google Scholar]
- 11.Tam V.C., Berry S., Hsu T., North S., Neville A., Chan K. Oncology education in Canadian undergraduate and postgraduate medical programs: a survey of educators and learners. Curr Oncol. 2014;21:e75–e88. doi: 10.3747/co.21.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mattes M.D., Small W., Jr., Vapiwala N. Out of the basement and into the classroom: pathways for expanding the role of radiation oncologists in medical student education. J Am Coll Radiol. 2018 doi: 10.1016/j.jacr.2017.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwan J.Y., Nyhof-Young J., Catton P., Giuliani M.E. Mapping the future: towards oncology curriculum reform in undergraduate medical education at a Canadian medical school. Int J Radiat Oncol Biol Phys. 2015;91:669–677. doi: 10.1016/j.ijrobp.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 14.Niemiec M., Kepka L., Maciejewski B., Lindner B., Bujko K. Radiation oncology training in Poland: results of a national survey (2007) Clin Oncol (R Coll Radiol) 2009;21:74–75. doi: 10.1016/j.clon.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Barton M.O. What do undergraduate doctors really need to know about radiation oncology? J Med Imaging Radiat Oncol. 2018;62:823–825. doi: 10.1111/1754-9485.12834. [DOI] [PubMed] [Google Scholar]
- 16.Begg A.C., Stewart F.A., Vens C. Strategies to improve radiotherapy with targeted drugs. Nat Rev Cancer. 2011;11:239–253. doi: 10.1038/nrc3007. [DOI] [PubMed] [Google Scholar]
- 17.Hirsch A.E., DeNunzio N., Levin-Epstein R., Bishop P.M. In regards to Dennis and Duncan: radiation oncology in undergraduate medical education: a literature review. Int J Radiat Oncol Biol Phys. 2010;76:649–655. doi: 10.1016/j.ijrobp.2009.08.038. [DOI] [PubMed] [Google Scholar]
- 18.Nicholls L., Bravery B., Chelvarajah R., Shi K., Tieu M.T., Turner S. The status of radiation oncology teaching in Australian and New Zealand medical schools. J Med Imaging Radiat Oncol. 2018;62:828–834. doi: 10.1111/1754-9485.12788. [DOI] [PubMed] [Google Scholar]
- 19.Eriksen J.G., Beavis A.W., Coffey M.A., Leer J.W., Magrini S.M., Benstead K. The updated ESTRO core curricula 2011 for clinicians, medical physicists and RTTs in radiotherapy/radiation oncology. Radiother Oncol. 2012;103:103–108. doi: 10.1016/j.radonc.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Kourdioukova E.V., Valcke M., Derese A., Verstraete K.L. Analysis of radiology education in undergraduate medical doctors training in Europe. Eur J Radiol. 2011;78:309–318. doi: 10.1016/j.ejrad.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 21.Connor Desai S., Reimers S. Comparing the use of open and closed questions for Web-based measures of the continued-influence effect. Behav Res Methods. 2018 doi: 10.3758/s13428-018-1066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dennis K.E., Duncan G. Radiation oncology in undergraduate medical education: a literature review. Int J Radiat Oncol Biol Phys. 2010;76:649–655. doi: 10.1016/j.ijrobp.2009.08.038. [DOI] [PubMed] [Google Scholar]
- 23.Pilleron S., Sarfati D., Janssen-Heijnen M., Vignat J., Ferlay J., Bray F. Global cancer incidence in older adults, 2012 and 2035: a population-based study. Int J Cancer. 2018 doi: 10.1002/ijc.31664. [DOI] [PubMed] [Google Scholar]
- 24.Lewis R.S., Sunshine J.H. Radiation oncologists in the United States. Int J Radiat Oncol Biol Phys. 2007;69:518–527. doi: 10.1016/j.ijrobp.2007.02.053. [DOI] [PubMed] [Google Scholar]
- 25.Golden D.W., Kauffmann G.E., McKillip R.P., Farnan J.M., Park Y.S., Schwartz A. Objective evaluation of a didactic curriculum for the radiation oncology medical student clerkship. Int J Radiat Oncol Biol Phys. 2018;101:1039–1045. doi: 10.1016/j.ijrobp.2018.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevens G. The new curriculum in radiation oncology-everyone should win! J Med Imaging Radiat Oncol. 2008;52:533–534. doi: 10.1111/j.1440-1673.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- 27.Jablonover R.S., Blackman D.J., Bass E.B., Morrison G., Goroll A.H. Evaluation of a national curriculum reform effort for the medicine core clerkship. J Gen Intern Med. 2000;15:484–491. doi: 10.1046/j.1525-1497.2000.06429.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kumar A.B., Hata J.S., Bayman E.O., Krishnan S. Implementing a hybrid web-based curriculum for an elective medical student clerkship in a busy surgical intensive care unit (ICU): effect on test and satisfaction scores. J Surg Educ. 2013;70:109–116. doi: 10.1016/j.jsurg.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 29.Tews M.C., Wyte C.M., Coltman M., Grekin P.A., Hiller K., Oyama L.C. Developing a third-year emergency medicine medical student curriculum: a syllabus of content. Acad Emerg Med. 2011;18(Suppl 2):S36–S40. doi: 10.1111/j.1553-2712.2011.01161.x. [DOI] [PubMed] [Google Scholar]
- 30.Cipriano S.D., Dybbro E., Boscardin C.K., Shinkai K., Berger T.G. Online learning in a dermatology clerkship: piloting the new American academy of dermatology medical student core curriculum. J Am Acad Dermatol. 2013;69:267–272. doi: 10.1016/j.jaad.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 31.Kerfoot B.P., Baker H., Volkan K., Church P.A., Federman D.D., Masser B.A. Development and initial evaluation of a novel urology curriculum for medical students. J Urol. 2004;172:278–281. doi: 10.1097/01.ju.0000132157.84026.ea. [DOI] [PubMed] [Google Scholar]
- 32.Kaplan A.G., Kolla S.B., Gamboa A.J., Box G.N., Louie M.K., Andrade L. Preliminary evaluation of a genitourinary skills training curriculum for medical students. J Urol. 2009;182:668–673. doi: 10.1016/j.juro.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 33.Parikh P.P., White M.T., Buckingham L., Tchorz K.M. Evaluation of palliative care training and skills retention by medical students. J Surg Res. 2017;211:172–177. doi: 10.1016/j.jss.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 34.Lass P., Scheffler J. Undergraduate teaching of nuclear medicine in European universities. Eur J Nucl Med Mol Imaging. 2003;30:1018–1023. doi: 10.1007/s00259-003-1191-4. [DOI] [PubMed] [Google Scholar]
- 35.Schellens T., Van Keer H., De Wever B., Valcke M. Scripting by assigning roles: does it improve knowledge construction in asynchronous discussion groups? Int J Comput Supp Collab Learn. 2007;2:225–246. [Google Scholar]